1. Introduction
Tooth impaction is defined as the intraosseous retention of a tooth beyond its expected time of eruption, accompanied by the loss of its eruptive potential. It can affect various tooth groups, most commonly the mandibular third molars and maxillary canines, followed by maxillary third molars, premolars, and central incisors [
1,
2]. The etiology is usually multifactorial, involving mechanical obstructions, environmental factors, and genetic predisposition.
Although rare, retention of mandibular second molars (MM2) can significantly compromise occlusion and aesthetics. The most common causes include lack of space in the dental arch or failure of the follicle to initiate bone resorption [
3,
4]. Ectopic positioning of the tooth germ or deviation in its eruptive path may also contribute to impaction [
5,
6]. Iatrogenic factors such as the use of lingual arches, ankylosis, or early extraction of the first molar have also been implicated, although less frequently [
7,
8].
According to various authors prevalence rates vary from 0.8% to 3.6% in the general population to as high as 11.9% in orthodontic patients [
9,
10,
11]. Unilateral impaction is more common, with a higher incidence in males and on the right side [
5,
12]. Clinical symptoms may include pain, pericoronitis, dental caries, cyst formation, and infections [
13].
The standard approach to managing impacted MM2 is surgical–orthodontic intervention, with early diagnosis being critical. Treatment protocols vary depending on the position and inclination of the impacted tooth and may involve surgical exposure with orthodontic uprighting, extraction with autotransplantation, or replacement by the third molar. Other reported options include early prophylactic removal of the third molar bud, surgical uprighting of MM2, or facilitating its eruption by removing eruption-blocking barriers [
4,
5,
7,
14,
15,
16,
17,
18].
Classical orthodontic traction techniques often employ segmental archwires, cantilever loops, coil springs, or temporary anchorage devices (TADs). However, these methods are frequently associated with patient discomfort, risk of anchorage loss, and the need for full arch alignment prior to force application [
4,
19,
20].
In contemporary orthodontic practice, the most stable form of anchorage is skeletal anchorage provided by orthodontic miniscrews (mini-implants). There are three optimal methods for uprighting molars using miniscrew anchorage, with placement between the roots of the premolars, in the mandibular retromolar region, and in the mandibular ramus [
21]. Positioning a miniscrew distally in the regenerated bone at the third-molar extraction site provides an ideal point for distal traction of the second molar [
7,
22,
23]. The limitations of this technique include the time required for osseous regeneration at the extraction site; additionally, the vertical height of the miniscrew may interfere with occlusion [
24,
25]. Another approach involves placing the mini-screw in the mandibular ramus, which offers a substantial amount of bone and favorable mechanical positioning of the implant to facilitate molar traction [
26]. However, treatment in this region can be particularly challenging due to limited visibility in the surgical field [
27].
In recent years, there has been growing interest in the use of digitally designed and three-dimensional (3D) printed orthodontic devices that allow for pretreatment planning, patient-specific customization, and improved predictability of tooth movement [
28,
29,
30,
31]. Computer-Aided Design and Computer-Aided Manufacturing (CAD/CAM) technologies enable the integration of Standard Triangle Language (STL) files from intraoral scans with Digital Imaging and Communication in Medicine (DICOM) data from Cone Beam Computed Tomography (CBCT) imaging, thereby facilitating assessment of the retromolar space, bone quality, and definition of the optimal vector for orthodontic traction. This digital workflow reduces the need for intraoral adjustment of the appliance and shortens chair time [
32].
Furthermore, these individually manufactured appliances do not require surgical insertion into the bone, as is the case with mini-implants, making them less invasive and more acceptable to growing patients. They can be used as a standalone segment of treatment or combined with other orthodontic approaches for example, in patients who underwent early orthodontic therapy and developed MM2 impaction later.
Many orthodontic appliances and techniques are available for uprighting mesial impacted MM2, but each has its advantages in specific clinical cases and disadvantages in others. Modern orthodontics creates conditions for designing appliances with greater predictability of outcomes, with a reduced degree of invasiveness and less need for patient cooperation.
Therefore, the aim of the article is to share data on the design and methodology of working with digitally designed systems for Printed Dento-alveolar Anchorage (PDaA) used in orthodontic traction of MM2. PDaA systems are manufactured by 3D metal printing using Selective Laser Melting and Selective Laser Sintering (SLM/SLS) technology. This method integrates digital precision, biomechanical efficiency and clinical minimal invasiveness, offering a reliable and predictable solution for stable support during traction of impacted MM2.
2. Materials and Methods
2.1. Clinical Protocol
The clinical workflow comprises several phases: diagnostic assessment; team-based formulation and discussion of the surgical–orthodontic protocol; presentation of the treatment plan to the patient or legal guardians; design planning of the personalized dentoalveolar anchorage system (PDaA); technology-assisted device fabrication; and implementation of the surgical–orthodontic procedures
Figure 1. Each phase requires a precise, individualized approach and creative problem-solving. Extensive digitization of the diagnostic and therapeutic stages, particularly device planning and fabrication, maximizes concordance between the planned objectives and the achieved clinical outcomes.
2.1.1. Diagnostic Stage
Clinical experience, which underpins the development and technological fabrication of the (PDaA) system for the traction of impacted MM2, is based on the treatment of 14 patients. All patients were between 14 and 18 years old. Four of them had previously undergone orthodontic treatment. In three cases, the prior treatment had been completed before the eruption of the mandibular second molars, resulting in delayed diagnosis of their impaction. One patient had been treated with aligners. Three of the patients presented with bilateral impaction of the mandibular second molars, while the remaining 11 had unilateral impaction. Ten patients required comprehensive orthodontic treatment. In eight of these cases, the primary reason for seeking orthodontic care was not the impacted MM2 but another orthodontic issue, most commonly related to dental alignment and occlusal discrepancies. The diagnosis of MM2 impaction was made as part of the comprehensive orthodontic assessment of the clinical case. Only two patients had been referred by their general dentists due to failure of eruption of the mandibular second molars.
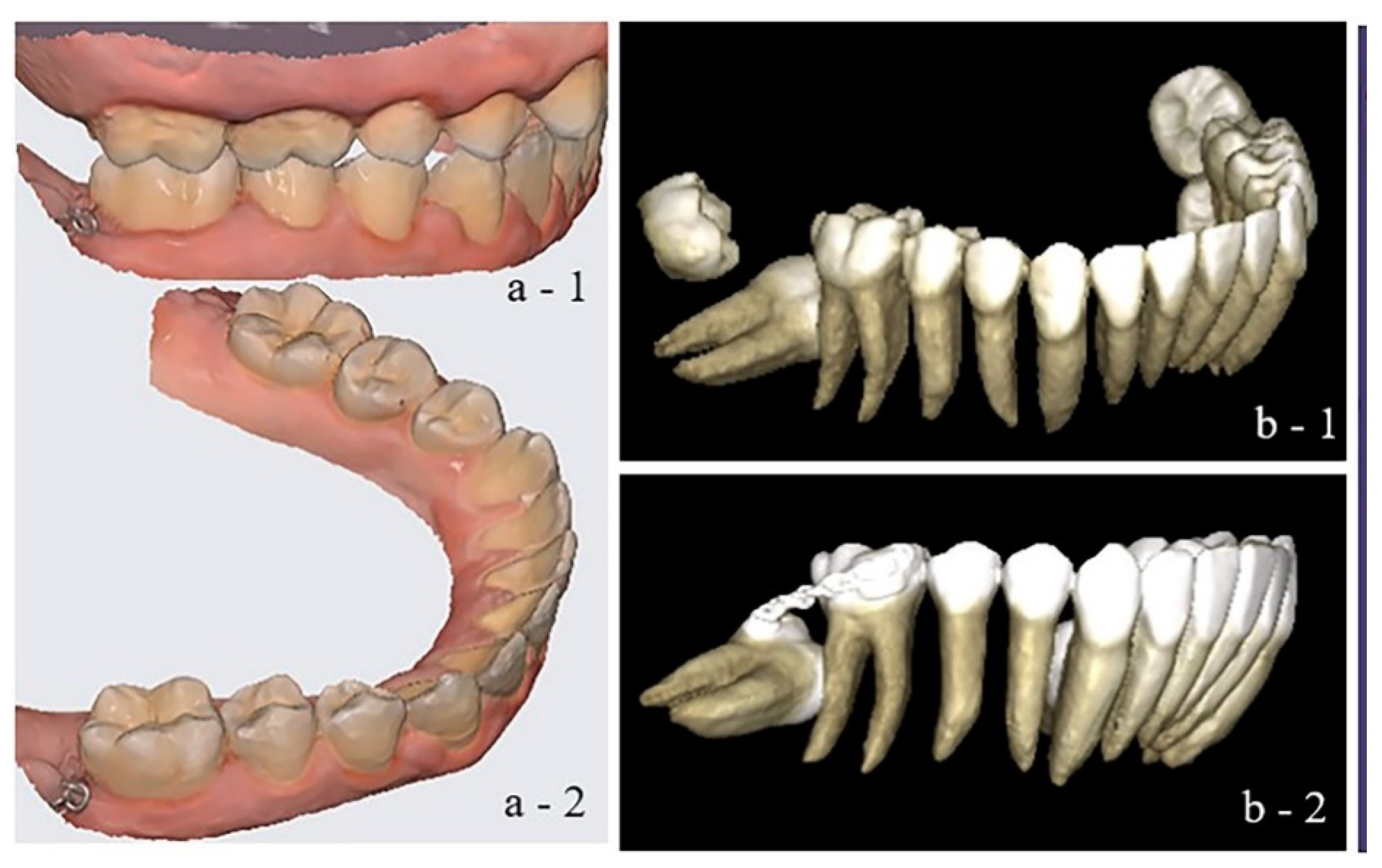
The clinical protocol included patients diagnosed with mandibular second molar (MM2) impaction, confirmed via cone-beam computed tomography (CBCT). Three-dimensional imaging enabled precise assessment of the position of the impacted teeth as well as the presence and location of the developing third molars. In addition, digital intraoral scans of the upper and lower dental arches and their occlusal relationships were performed to generate a complete digital model of the oral cavity, as shown in
Figure 2. Intraoral and extraoral photographs were also obtained as part of a comprehensive orthodontic analysis, along with supplementary diagnostics to evaluate the overall orthodontic condition.
Particular attention is given to refining the traction vector for impacted mandibular second molars (MM2), as this determines the location of the anchorage point in the forthcoming digital construct. Tooth movement commonly begins with buccal
Figure 2 or lingual uprighting, followed by distal crown tipping. Analysis of the planned traction vector determines the PDaA design and the choice of surgical approach for third-molar extraction and second-molar exposure.
In clinical practice, two surgical–orthodontic techniques are recognized: (1) Closed technique: The third molar is extracted, the second molar is exposed, and a button (or chain) is bonded; the surgical site is then primarily closed. The chain emerging from the wound is passively secured to the adjacent teeth (the first molar or the second premolar)
Figure 2(b-2). After a healing period, the orthodontist places the PDaA and actively engages the chain to initiate traction of the impacted MM2. (2) Open technique: This may be performed in one or two stages. In the two-stage approach, the third molar is extracted; following a healing period with osseous fill of the retromolar space, the impacted second molar is exposed, and the site is covered with a surgical dressing. After approximately three days, the orthodontist fixes the PDaA to the mandibular anchorage teeth and begins traction. More commonly, we prefer a single-stage approach in which the third molar extraction and second molar exposure are completed in one session, followed by placement of a surgical dressing. On postoperative day 3–4, the pre-fabricated PDaA is delivered, an attachment (button or traction chain) is bonded to the impacted second molar, and traction is initiated.
Selection of the closed versus open approach is decided jointly by the orthodontist–surgeon team, considering the patient’s emotional and psychological preferences as well as the characteristics of the operative field. For all approaches, the intended position of the PDaA must be preplanned and trial-fitted. Clinically, the position of the extended arm (cantilever) relative to the mandibular alveolar crest is assessed to plan the osseous recontouring and create access to the impacted second molar. Occlusal contacts with antagonists are evaluated to avoid loading the extended arm. The assembly is also checked for unintended stresses arising from contact between the framework and the abutment teeth.
Following the diagnostic assessment, a comprehensive treatment plan was developed for each case. Treatment is sequenced to first resolve the impaction of the MM2 and only thereafter to address leveling of both dental arches and adjustment of occlusal relationships. Traction of the impacted MM2 precedes mandibular arch alignment to minimize the risk of orthodontically induced resorptive changes on the distal root surface of the first molars. This sequencing underpins the individualized treatment plan. Patients and/or their guardians received detailed information regarding the treatment process, procedures involved, and the anticipated outcome. Upon obtaining informed consent, the combined orthodontic-surgical protocol was initiated.
2.1.2. Digital Design and Fabrication of the Printed Dentoalveolar Anchorage System
Therefore, the workflow relies on high-accuracy digital records—CBCT, intraoral scans, and photographs, acquired with calibrated devices and registered through a validated protocol, enabling precise transfer from virtual design to device fabrication and clinical delivery. The digital workflow began with the integration of intraoral scan data (STL files) and segmented CBCT images (DICOM files), enabling comprehensive 3D treatment planning
Figure 3. Accordingly, the CBCT-derived root anatomy of the anchorage teeth and the true position of the impacted MM2 are registered onto the working digital models. Using CAD/CAM software (Exocad 3.0 Galway), the anchorage zone was defined, and a metallic extension was designed to project into the retromolar space. The extended arm (cantilever) emerges from the base of the lingual framework and may be positioned lingually or buccally, or configured to circumferentially encircle the molar site. The position of the extension was adapted to the occlusal plane to avoid interference with interarch relationships and aligned with the alveolar ridge anatomy to prevent irritation of adjacent soft tissues.
The digital planning includes precise assessment of the metallic extension’s position relative to the impacted mandibular second molar, evaluation of occlusal contacts, and analysis of the transverse and sagittal dimensions of the retromolar space. Depending on the position of the impacted molar, one or more hooks for elastic elements were incorporated into the extension, allowing for precise direction of the traction forces and potential vector modification during the course of treatment
Figure 4. The anchorage design could be positioned lingually, buccally, or extended across the entire retromolar area. Once a segment of the extension fulfilled its function, it could be removed by cutting with a carbide bur to reduce the weight and bulk of the appliance.
Design was performed using Exocad 3.0 Galway software, and the final design was exported in a format compatible with 3D metal printing. The anchorage system was fabricated using Wirobond C+ metal powder (BEGO Medical GmbH, Bremen, Germany), composed of 63.3% Cobalt (Co), 24.8% Chromium (Cr), 5.3% Tungsten (W), 5.1% Molybdenum (Mo), and 1.0% Silicon (Si). An offset of 0.08 mm was applied to the rings and contact zones [
32]. The manufacturing process employed laser sintering (SLM/SLS) technology using the TruPrint 1000 system (Trumpf Group, Ditzingen, Germany). During fabrication, the powder was melted layer by layer using a high-energy CO
2 laser until the final structure was completed
Figure 4. After printing, support structures were removed. Based on the team’s six years of experience working with this manufacturing system, we rely on the predictability and accuracy of appliance printing, which prevents the generation of residual stresses. The alloy used contains no nickel, thereby reducing the risk of allergic reactions in patients during orthodontic treatment. Numerous studies have already confirmed the mechanical properties, electrochemical behavior, and biocompatibility of the selected alloy [
33,
34].
The design of the PDaA can incorporate additional elements to support the subsequent phase of orthodontic treatment (i.e., the fixed appliance stage). The integration of printed buccal tubes onto the bands of the lower first molars (as illustrated in one of the PDaA designs in
Figure 4, or printed brackets on bands encompassing the premolars, eliminates the need to remove the anchorage system when transitioning to the next treatment stage. Such integrated elements are particularly advantageous in segmental treatments primarily focused on the traction of MM2.
2.1.3. Clinical Application of the Printed Dentoalveolar Anchorage System
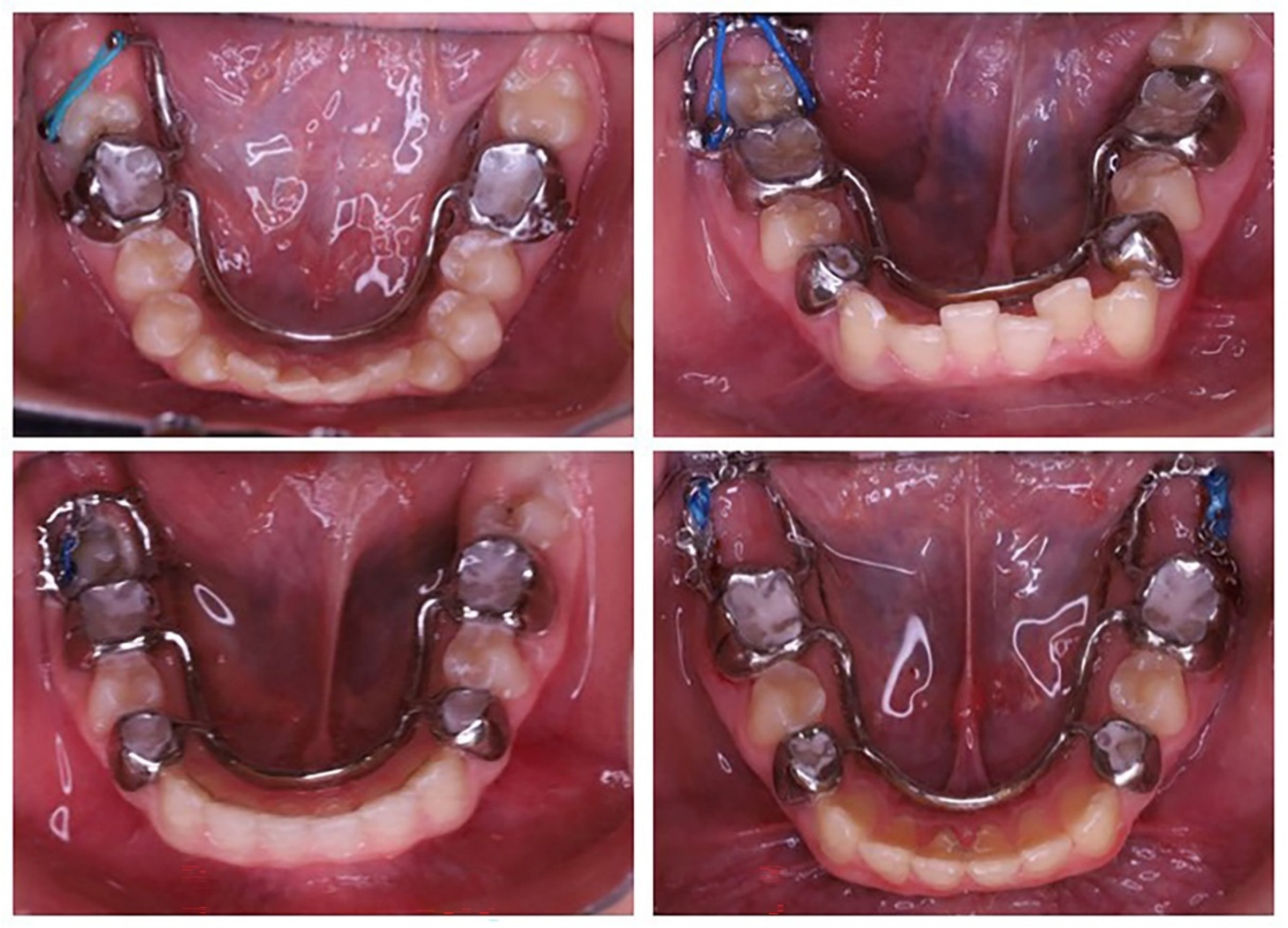
The PDaA system is cemented intraorally using a glass-ionomer cement (GIC), which tolerates a slightly moist field. Upon removal of the surgical dressing, minor exudate is common and may compromise the adhesion of resin-based cements, hence the preference for GIC. The elastomeric element is attached to the extended arm using various techniques
Figure 5, such as an elastomeric ligature with an auxiliary stainless-steel ligature or direct application of an elastomeric chain (single or double strands). As the MM2 is displaced, the elastomeric element is either replaced with a shorter one or the point of attachment is moved to a more distal location along the cantilever.
Placement of a button on the impacted mandibular second molar and activation of an elastic traction element. The traction vector can be modified by attaching the elastic chain to various segments of the metallic extension of the PDaA.
The traction and uprighting of impacted mandibular molars require controlled, light to moderate orthodontic forces to ensure safe and effective tooth movement without causing damage to the surrounding tissues. The uprighting procedure is typically performed using light forces in the range of 50–80 g. These forces can be generated by stretching an elastic continuous chain by 25% to 50%, depending on the material from which the chain is made. Manufacturers usually provide force values for their chains when stretched to a specific extent, most commonly at 25% elongation. However, the most reliable method for determining the applied force is by using a force gauge. In our clinical protocol, we apply the chain stretched to 25%. The greatest amount of force is generated and perceived by the patient within the first 24 hours, after which a gradual decrease in force occurs.
3. Results
The effectiveness of applying orthodontic traction to impacted mandibular second molars using PDaA anchorage was monitored throughout the treatment period using orthopantomograms and intraoral documentation of the clinical stages. Once the MM2 erupted into the dental arch at the level of the clinical crown, its final alignment was continued within the framework of comprehensive orthodontic treatment using a fixed appliance technique. The entire orthodontic treatment was completed upon achieving normal occlusal relationships between the two aligned dental arches. The retention phase did not differ from that of other orthodontic treatments. In patients undergoing a second treatment involving only the traction of impacted mandibular second molars, the final alignment was accomplished using a segmental fixed appliance including the first molar and the two premolars. This approach preserved the patient’s aesthetics.
The clinical outcomes, treatment duration related to the traction of impacted mandibular second molars, and the knowledge gained through clinical experience are summarized in
Table 1.
The clinical sequence and outcomes associated with the management of impacted mandibular second molars (MM2) utilizing customized, metal-printed dentoalveolar anchorage systems (PDaA) are illustrated in
Figure 6 and
Figure 7. Following the extraction of the mandibular third molars and the surgical exposure of the impacted teeth, performed in accordance with the digital treatment plan, orthodontic buttons were bonded to the MM2. After a healing period of 3–4 days, the PDaA was cemented intraorally.
The position of the extension arm within the retromolar space and the predesigned anchorage points allowed for precise control over the vector and direction of the applied orthodontic force, with the possibility of modification during tooth movement. The arm followed the contour of the alveolar ridge and the course of the ascending ramus, enabling the use of planned hook points to direct vertical movements of the impacted second molar. Thus, control is achieved in the bucco-lingual, vertical, and disto-coronal directions simultaneously. The anchorage point on the PDaA system was adjustable during treatment according to the required direction of tooth movement. Activation of the elastic element was carried out every 3–4 weeks during routine orthodontic follow-ups. The applied force system generated a counterclockwise moment, enabling controlled movement. The roots of the MM2 moved mesially, consistent with their biological eruptive path and toward an area of greater bone volume. Side effects were minimized, and anchorage components were incorporated to offset undesirable forces. Once sufficient uprighting and vertical alignment of the MM2 were achieved, the extension arm or the entire PDaA system was removed. The subsequent treatment phase involved leveling of the dental arch and restoration of functional occlusion. In some clinical cases, brackets or tubes were added to the anchorage teeth on the PDaA, integrating it into the fixed orthodontic appliance.
The effectiveness of PDaA is best illustrated by a clinical case. The treatment stages presented in
Figure 6 were on a 17-year-old female patient diagnosed with impaction of the mandibular right second molar (tooth 47), hyperdontia involving the maxillary right third molar (tooth 18), and rotations in both arches.
Tooth 47 had its crown positioned mesially and buccally, with the roots in contact with the lingual cortical plate of the mandible. The mandibular right third molar (tooth 48) completely blocked the eruptive potential and path of tooth 47, necessitating extraction of tooth 48. To address the supernumerary maxillary molar, extraction of the maxillary right second molar (tooth 17) was planned to create space for eruption of the third molar(s).
The patient was treated using a PDaA to upright the mandibular right second molar (47), combined with extraction of the maxillary right second molar (17) and comprehensive leveling of both arches while preserving Class I relationships. The PDaA phase lasted six months, resulting in complete uprighting and extrusion of tooth 47, shown on
Figure 6. Forces were applied to achieve lingual uprighting, followed by distal crown tipping. The distally extended arm provided an extrusive vector to bring tooth 47 to the occlusal plane. Fixed appliances were subsequently bonded in both arches to complete leveling and alignment
Figure 6 and
Figure 7.
Due to the exceptional manufacturing precision, the custom-designed dentoalveolar anchorage systems (PDaA) did not require any additional adjustment, which significantly reduced the clinical time for placement and activation. The rigidity of the structure provided stable support for biological orthodontic forces, with no observed undesirable movement or changes in the teeth within the anchorage zone. These systems can be used either as a standalone phase of treatment or in combination with fixed orthodontic techniques. Their individualized design also enables their application in segmental interventions, particularly in patients who completed an early phase of orthodontic treatment prior to the eruption of the mandibular second molars. In such cases, where the dental arches and occlusion are already well aligned, the retention of MM2 often remains undetected until a later stage, for which the use of a customized anchorage system offers an efficient and minimally invasive solution. The PDaA system is positioned on the lingual aspect, preserving aesthetics, not affecting speech, and allowing rapid patient adaptation.
4. Discussion
Given the relatively low incidence of mandibular second molar impaction, the clinical experience accumulated by our team provides a solid basis for proposing treatment with PDaA as a reliable and easily applicable method in orthodontic practice. Our previous experience with miniscrews was also successful; however, it required more advanced surgical skills on the part of the orthodontist.
This study demonstrates the clinical effectiveness of a surgical–orthodontic technique for the traction of impacted MM2. The proposed method differs from previously described approaches by incorporating reduced orthodontic invasiveness and an innovative protocol involving individualized pretreatment planning and custom fabrication of orthodontic appliances and auxiliary anchorage systems.
Additionally, in cases where the surgical protocol involves the removal of impacted mandibular third molars to facilitate MM2 uprighting, it would be valuable to discuss the option of coronectomy as an alternative to full extraction when appropriate, particularly in cases with a high risk of inferior alveolar nerve injury. Our clinical experience is limited to the use of a surgical approach involving complete extraction of the mandibular third molar in conjunction with orthodontic traction of the mandibular second molar. However, the scientific literature also presents coronectomy as a safer alternative, especially in cases where the third molar is in close proximity to the mandibular canal [
35].
The presented PDaA design is readily customizable to each clinical case. The extended arm (cantilever) can be contoured to the alveolar ridge and oriented according to the position and inclination of the impacted MM2. Features along the cantilever may range from perforations for passing wire or elastomeric ligatures to a button-type element with a textured surface, shaped to the available space and non-irritating to adjacent soft tissues. The cantilever length can be specified during design and subsequently adjusted chairside by trimming as treatment progresses. Various methods for attaching the elastomeric component are available. For direct distal uprighting of an impacted mandibular second molar, paired elastomeric forces (buccal and lingual) can be applied to control unwanted tipping or rotation of the MM2.
The optimal timing for the management of impacted MM2 is when root development is still incomplete [
36]. Early diagnosis and prompt intervention are key to successful correction, as prolonged contact between the impacted MM2 and the adjacent first molar (MM1) may lead to root resorption, caries, and periodontal complications.
In modern orthodontics, computer-designed appliances can be precisely tailored to the patient’s unique anatomical characteristics, considering surrounding bone structures and the specifics of the location for placement. Superimposing CBCT data and intraoral scans enables accurate localization of the first molars, prediction of MM2 tooth movement, and precise planning of the retromolar space. Dedicated software merges STL files from intraoral scanning with DICOM images from CBCT, facilitating both qualitative and quantitative assessment of the available bone volume. The resulting appliance features a simplified design, yet is highly personalized and adapted to the individual clinical scenario. This level of precision improves the predictability of orthodontic tooth movement and enhances appliance accuracy. Consequently, clinicians can plan with greater confidence, while patients experience increased trust in the diagnostic and treatment process. Furthermore, patients actively engage in the digital planning journey, which enhances cooperation and treatment adherence. The PDaA system is particularly well-accepted among growing patients and their parents, as it does not require local anesthesia or the insertion of skeletal implants, such as mini-screws.
The anchorage system is rigid and does not permit undesirable movement of adjacent teeth. Side effects are minimized, and supportive elements are incorporated into the design to allow for compensation if needed. In contemporary literature, there is a growing number of reports on support devices for impacted teeth that can be manufactured using 3D printing technology [
30,
31,
32]. These studies report satisfactory treatment outcomes. Predefining the direction of the required orthodontic forces significantly improves the prognosis for successful treatment. Personalized devices follow the patient’s needs, and this provides certainty that this approach will benefit the patient’s treatment [
37].
4.1. Esthetics and Clinical Compatibility
Most individualized PDaA systems are positioned lingually and remain outside the visible aesthetic zone, enhancing treatment acceptability, particularly in cases where the anchorage system is the only appliance in the oral cavity. These devices may function as a standalone phase of treatment or be combined with a fixed orthodontic approach. Their custom design allows for segmental mechanics with archwires, especially in patients who completed early orthodontic therapy prior to the eruption of the MM2. In such cases, impaction often remains undiagnosed until later, as the dental arch appears leveled and occlusion functional. The device is also compatible with aligner-based treatments, where the traction of impacted mandibular second molars can be performed either before or after dental leveling.
4.2. Artificial Intelligence and Future Perspectives
The increasing adoption of digital orthodontic appliances also supports the advancement of artificial intelligence (AI) algorithms in orthodontic diagnostics and treatment planning [
38,
39,
40]. Artificial intelligence (AI) assists in segmenting CBCT images and integrating them with intraoral scan data during appliance design planning. AI may assist in error prediction during the 3D printing workflow, improving reliability and outcome optimization. Furthermore, individualization enhances patient satisfaction and creates new opportunities for patient-centered, cooperative care.
All digital designs of anchorage systems, whether for the traction of impacted MM2 or for the treatment of other impacted teeth, contribute to enriching the software’s library, leading to the self-learning of the AI assistant. At this stage of AI integration into orthodontics, its benefit is particularly evident in the segmentation of structures and teeth from CBCT files and their incorporation into STL files.
CBCT enables clinicians to evaluate anatomical structures from multiple angles, significantly enhancing diagnostic accuracy for both orthodontic treatment and surgical procedures. The development of AI-based systems assists clinicians during diagnostics by identifying problematic areas in scans and supporting clinical decision-making. Their integration has the potential to optimize clinical workflows and reduce reliance on post-procedural diagnostics [
41].
Digitalization in orthodontics affects all levels of practice: diagnosis, treatment planning, fabrication of orthodontic appliances, communication with patients, and even appointment scheduling. In this context, every experience with new digital versions of orthodontic appliances enriches daily clinical practice and broadens the perspective of orthodontic thinking.
4.3. Limitations
The main limitations of custom-fabricated dentoalveolar anchorage systems are related to the planning software and the operator’s training level [
37]. Additionally, clinicians must have a solid understanding of the physicomechanical properties of the selected materials [
38]. These materials must meet the biocompatibility standards for growing patients while ensuring sufficient rigidity and load-bearing capacity.
5. Conclusions
Contemporary orthodontic practice has undergone significant innovation and rapid development with the integration of 3D planning and printing technologies for orthodontic appliances and auxiliary devices. Based on the clinical experience and outcomes presented, several key conclusions can be drawn regarding the application and effectiveness of individualized metal-printed dento-alveolar anchorage systems (PDaA) in the management of impacted mandibular second molars:
The use of a customized, metal-printed dento-alveolar anchorage system (PDaA) provided a stable and adaptable platform for the distal and vertical traction of impacted mandibular second molars without requiring full arch leveling prior to activation.
Accurate CAD/CAM planning allowed the positioning of multiple traction points, enabling precise control of orthodontic force vectors and staged modulation of movement direction during treatment.
Clinical application in late-diagnosed impaction cases, following early-phase orthodontic therapy demonstrated the effectiveness of the segmental approach, which reduced the need for complete dental arch readjustment and shortened treatment duration.
The design of the PDaA is adapted to the occlusal contacts of the antagonists and the morphology of the alveolar ridge, without altering occlusal relationships or causing discomfort to the patient. The planning of the system also includes elements that may be utilized in the subsequent stages of treatment—for example, molar bands can be designed with buccal tubes, while premolar bands may incorporate brackets and other components.
The proposed treatment protocol and system design are non-invasive and well accepted by growing patients.
Author Contributions
Conceptualization, G.Y.; methodology, G.Y.; resources, G.Y.; writing—original draft preparation, G.Y.; writing—review and editing, M.G.; visualization, M.G.; supervision, M.G.; project administration, M.G.; funding acquisition, G.Y. and M.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of KENIMUS, Approval Code: N_ 2873 Approval Date: 4 May 2022.
Informed Consent Statement
Written informed consent was obtained from the patient(s) to publish this paper.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, M.G., upon reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| PDaA | Printed Dento-alveolar Anchorage |
| MM2 | Mandibular second molar |
| CBCT | Cone-beam computed tomography |
| 3D | 3-dimensional X-ray examination |
| CAD/CAM | Computer-Aided Design and Computer-Aided Manufacturing. |
| DICOM | Digital Imaging and Communication in Medicine. |
| STL | Standard Triangle Language |
| SLM/SLS | Selective Laser Melting and Selective Laser Sintering |
| AI | Artificial Intelligence |
References
- Yordanova, G.; Stanimirov, P. Impaction of teeth—Frequency and treatment protocols. Stoma. Edu. J. 2017, 4, 53–60. [Google Scholar]
- Yordanova, G.; Gurgurova, G. Impacted upper central incisors—Frequency and factors complicating the treatment protocol. Folia Med. 2021, 63, 405–412. [Google Scholar] [CrossRef]
- Kjær, I. Mechanism of human tooth eruption: Review article including a new theory for future studies on the eruption process. Scientifica 2014, 2014, 341905. [Google Scholar] [CrossRef]
- Yordanova, G. Treatment of impacted lower left second molar and over erupted upper second molar. J. Dent. Health Oral Disord. Ther. 2018, 9, 106–108. [Google Scholar] [CrossRef][Green Version]
- Shapira, Y.; Lai, Y.; Schonberger, S.; Shpack, N.; Finkelstein, T. Mandibular Second Molar Impaction-Part II: Etiology and Role of the Third Molar. Appl. Sci. 2022, 12, 11520. [Google Scholar] [CrossRef]
- Aharon, E.D.; Rushinek, H.; Casap-Caspi, N.; Chaushu, S. Impacted permanent first and second molars and failure of eruption: A comprehensive review for orthodontic practitioner. Semin. Orthod. 2024, 30, 727–741. [Google Scholar] [CrossRef]
- Sbricoli, L.; Ricci, S.; Cattozzo, A.; Favero, R.; Bressan, E.; Sivolella, S. Mandibular Molar Uprighting Using Skeletal Anchorage: A Novel Approach. J. Clin. Med. 2022, 11, 3565. [Google Scholar] [CrossRef]
- Cassetta, M.; Altieri, F.; Di Mambro, A.; Giansanti, M.; Galluccio, G.; Barbato, E. A retrospective study on impaction of mandibular second molar. Dent. Cadmos. 2013, 81, 603–611. [Google Scholar] [CrossRef]
- Chu, F.C.; Li, T.K.; Lui, V.K.; Newsome, P.R.; Chow, R.L.; Cheung, L.K. Prevalence of impacted teeth and associated pathologies--a radiographic study of the Hong Kong Chinese population. Hong Kong Med. J. 2003, 9, 158–163. [Google Scholar]
- Shpack, N.; Kisoss, C.A.; Laviv, A. The Presence of Impacted Teeth (Except for Wisdom Teeth) in Orthodontic Patients in Israel. Appl. Sci. 2022, 12, 10924. [Google Scholar] [CrossRef]
- Shpack, N.; Finkelstein, T.; Lai, Y.H.; Kuftinec, M.M.; Vardimon, A.; Shapira, Y. Mandibular Permanent Second Molar Impaction Treatment options and outcome. Open J. Dent. Oral Med. 2013, 1, 9–14. [Google Scholar] [CrossRef]
- Moca, R.T.; Moca, A.E.; Juncar, M. Prevalence and Symmetry of Positional Anomalies in Second Permanent Molars: Study of Romanian Patients. Pediatr. Rep. 2024, 16, 1149–1160. [Google Scholar] [CrossRef] [PubMed]
- Kuang, Q.; Zhou, H.; Hong, H.; Lin, D.; You, M.; Lai, W.; Long, H. Radiographic Features of Mandibular Second Molars with Eruption Disturbances: A Retrospective Study. J. Clin. Med. 2023, 12, 2798. [Google Scholar] [CrossRef]
- Johnson, J.V.; Quirk, G.P. Surgical repositioning of impacted mandibular second molar teeth. Am. J. Orthod. Dentofac. Orthop. 1987, 91, 242–251. [Google Scholar] [CrossRef] [PubMed]
- Abate, A.; Cavagnetto, D.; Fama, A.; Matarese, M.; Bellincioni, F.; Assandri, F. Efficacy of Operculectomy in the Treatment of 145 Cases with Unerupted Second Molars: A Retrospective Case-Control Study. Dent. J. 2020, 8, 65. [Google Scholar] [CrossRef] [PubMed]
- Han, T.; Christensen, B.J. Surgical Treatment of Impacted Mandibular Second Molars: A Systematic Review. J. Oral Maxillofac. Surg. 2022, 80, 29–36. [Google Scholar] [CrossRef]
- Sangha, T.; Sangha, S.; Hanna, B.; Tayab, T.; Padala, S. Surgical uprighting of impacted mandibular second molar: A narrative review. J. Oral Med. Oral Surg. 2021, 27, 28. [Google Scholar] [CrossRef]
- Tamer, I.; Öztaş, E.; Marşan, G. Up-to-date approach in the treatment of impacted mandibular molars: A literature review. Turk. J. Orthod. 2020, 33, 183–191. [Google Scholar] [CrossRef]
- Morita, Y.; Koga, Y.; Nguyen, T.A.; Yoshida, N. Biomechanical considerations for uprighting impacted mandibular molars. Korean J. Orthod. 2020, 50, 268–277. [Google Scholar] [CrossRef]
- Turley, P.K. The management of mesially inclined/impacted mandibular permanent second molars. J. World Fed. Orthod. 2020, 9, 45–53. [Google Scholar] [CrossRef]
- Yuan, X.; Kuang, Q.; He, X.; Han, X.; Lai, W.; Long, H. Clinical effectiveness of ramus mini-implants in orthodontic traction of impacted mandibular second molars. Eur. J. Orthod. 2025, 47, cjaf015. [Google Scholar] [CrossRef] [PubMed]
- Altieri, F.; Guarnieri, R.; Mezio, M.; Padalino, G.; Cipollone, A.; Barbato, E.; Cassetta, M. Uprighting Impacted Mandibular Second Molar Using a Skeletal Anchorage: A Case Report. Dent. J. 2020, 8, 129. [Google Scholar] [CrossRef]
- Cheng, H.-W.; Kao, C.-T.; Chou, C.-C.; Tsai, C.-Y.; Shen, H.-Y.; Tai, W.K. The Strategy for Uprighting a Deep Horizontally Impacted Mandibular Second Molar. Taiwan. J. Orthod. 2024, 36, 6. [Google Scholar] [CrossRef]
- Lee, K.J.; Park, Y.C.; Hwang, W.S.; Seong, E.H. Uprighting mandibular second molars with direct miniscrew anchorage. J. Clin. Orthod. 2007, 41, 627–635. [Google Scholar]
- Derton, N.; Perini, A.; Mutinelli, S.; Gracco, A. Mandibular molar uprighting using mini-implants: Different approaches for different clinical cases--two case reports. Orthodontics 2012, 13, 138–145. [Google Scholar] [PubMed]
- Mehta, S.; Arqub, S.A.; Sharma, R.; Patel, N.; Tadinada, A.; Upadhyay, M.; Yadav, S. Variability associated with mandibular ramus area thickness and depth in subjects with different growth patterns, gender, and growth status. Am. J. Orthod. Dentofac. Orthop. 2022, 161, e223–e234. [Google Scholar] [CrossRef]
- Baxi, S.; Bhatia, V.; Tripathi, A.; Dubey, M.P.; Kumar, P.; Mapare, S. Temporary Anchorage Devices. Cureus 2023, 15, e44514. [Google Scholar] [CrossRef]
- Germanò, F.; Guarnieri, R.; Mezio, M.; Barbato, E.; Cassetta, M. The Use of CAD/CAM Technology in Mandibular Canine Disimpaction: A Case Report. Dent. J. 2024, 12, 79. [Google Scholar] [CrossRef]
- Kuang, Y.; Wang, C.; Hu, B.; Feng, G.; Wang, C.; Song, J. Biomechanical analysis of reinstating buccally flared maxillary 2nd molars using 3D printing anchorage supports: A 3D finite element study. Comput. Methods Biomech. Biomed. Engin. 2021, 24, 1085–1096. [Google Scholar] [CrossRef]
- Yordanova-Kostova, G.R.; Emiliyanov, E.; Yanev, N. Digital Laser-Sintered Expander in Adolescent Patient with Hyperdontia and Molar Impaction. Case Rep. Dent. 2023, 2023, 8824900. [Google Scholar] [CrossRef]
- Pal’ovčík, M.; Tomášik, J.; Zsoldos, M.; Thurzo, A. 3D-Printed Accessories and Auxiliaries in Orthodontic Treatment. Appl. Sci. 2025, 15, 78. [Google Scholar] [CrossRef]
- Yordanova, G.; Chalyovski, M.; Gurgurova, G.; Georgieva, M. Digital Design of Laser-Sintered Metal-Printed Dento-Alveolar Anchorage Supporting Orthodontic Treatment. Appl. Sci. 2023, 13, 7353. [Google Scholar] [CrossRef]
- Zinelis, S.; Polychronis, G.; Papadopoulos, F.; Kokkinos, C.; Economou, A.; Panayi, N.; Papageorgiou, S.N.; Eliades, T. Mechanical and electrochemical characterization of 3D printed orthodontic metallic appliances after in vivo ageing. Dent. Mater. 2022, 38, 1721–1727. [Google Scholar] [CrossRef] [PubMed]
- Graf, S. Direct printed metal devices—The next level of computer-aided design and computer-aided manufacturing applications in the orthodontic care. APOS Trends Orthod. 2017, 7, 253–259. [Google Scholar] [CrossRef]
- Cosola, S.; Kim, Y.S.; Park, Y.M.; Giammarinaro, E.; Covani, U. Coronectomy of Mandibular Third Molar: Four Years of Follow-Up of 130 Cases. Medicina 2020, 56, 654. [Google Scholar] [CrossRef]
- Selvido, D.I.; Wongsirichat, N.; Arirachakaran, P.; Rokaya, D.; Wongsirichat, N. Surgical Management of Impacted Lower Second Molars: A Comprehensive Review. Eur. J. Dent. 2022, 16, 465–477. [Google Scholar] [CrossRef]
- Tsolakis, I.A.; Gizani, S.; Tsolakis, A.I.; Panayi, N. Three-Dimensional-Printed Customized Orthodontic and Pedodontic Appliances: A Critical Review of a New Era for Treatment. Children 2022, 9, 1107. [Google Scholar] [CrossRef]
- Panayi, N.C.; Efstathiou, S.; Christopoulou, I.; Kotantoula, G.; Tsolakis, I.A. Digital Orthodontics: Present and Future. AJO-DO Clin. Companion 2024, 4, 14–25. [Google Scholar] [CrossRef]
- Tomašik, J.; Zsoldos, M.; Oravcova, L.; Lifkova, M.; Pavleova, G.; Strunga, M.; Thurzo, A. AI and Face-Driven Orthodontics: A Scoping Review of Digital Advances in Diagnosis and Treatment Planning. AI 2024, 5, 158–176. [Google Scholar] [CrossRef]
- Gracea, R.S.; Winderickx, N.; Vanheers, M.; Hendrickx, J.; Preda, F.; Shujaat, S.; de Llano-Pérula, M.C. Artificial intelligence for orthodontic diagnosis and treatment planning: A scoping review. J. Dent. 2025, 152, 105442. [Google Scholar] [CrossRef]
- Meto, A.; Halilaj, G. The Integration of Cone Beam Computed Tomography, Artificial Intelligence, Augmented Reality, and Virtual Reality in Dental Diagnostics, Surgical Planning, and Education: A Narrative Review. Appl. Sci. 2025, 15, 6308. [Google Scholar] [CrossRef]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).