Diagnosis and Treatment in Asthma and Allergic Rhinitis: Past, Present, and Future
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Asthma
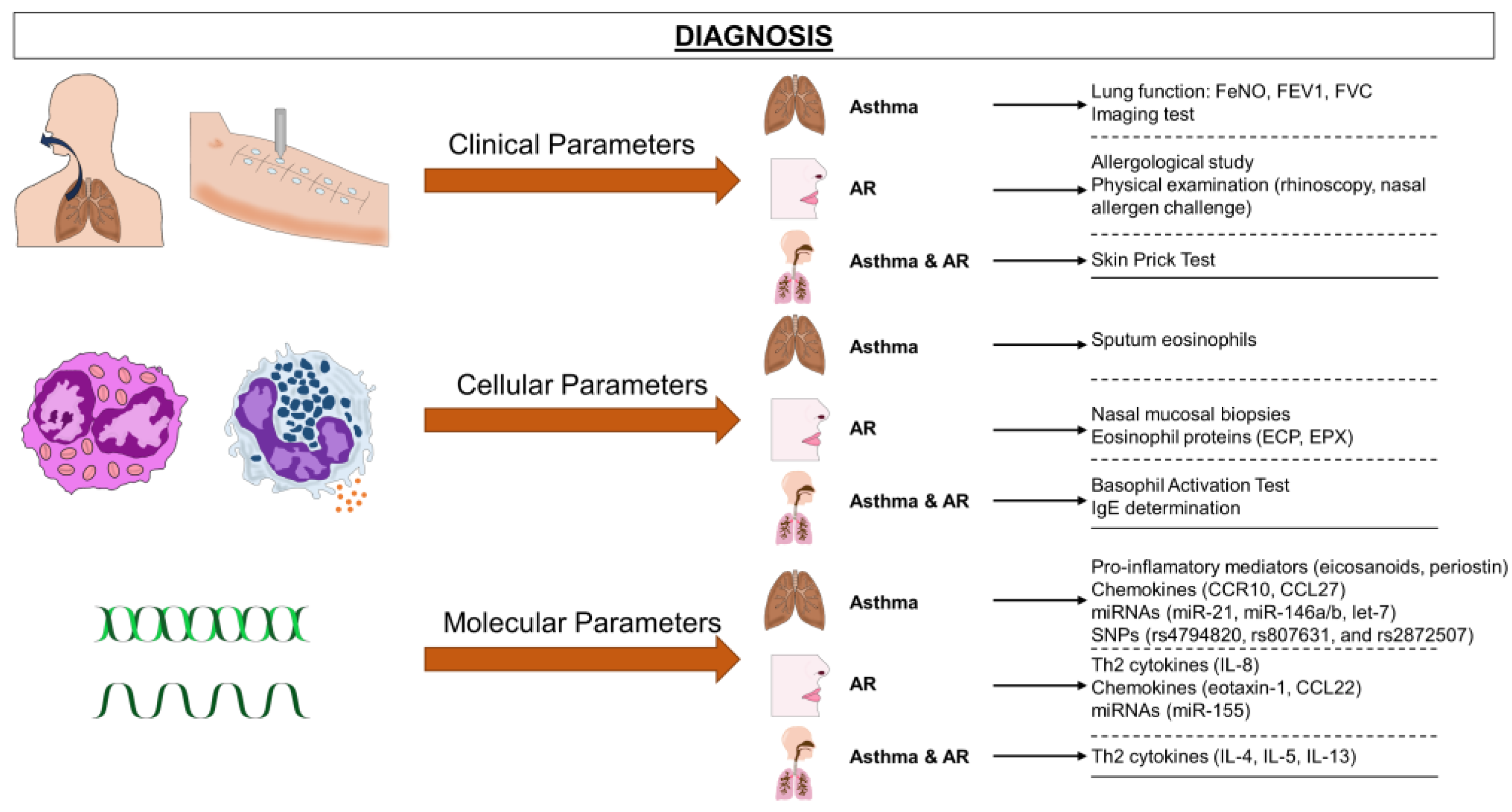
3.1.1. Asthma Diagnosis
Clinical Diagnosis of Asthma
Cellular Diagnostic Parameters and Biomarkers in Asthma
Molecular Diagnostic Parameters in Asthma: Proteomics, Metabolomics, and Transcriptomics Analysis
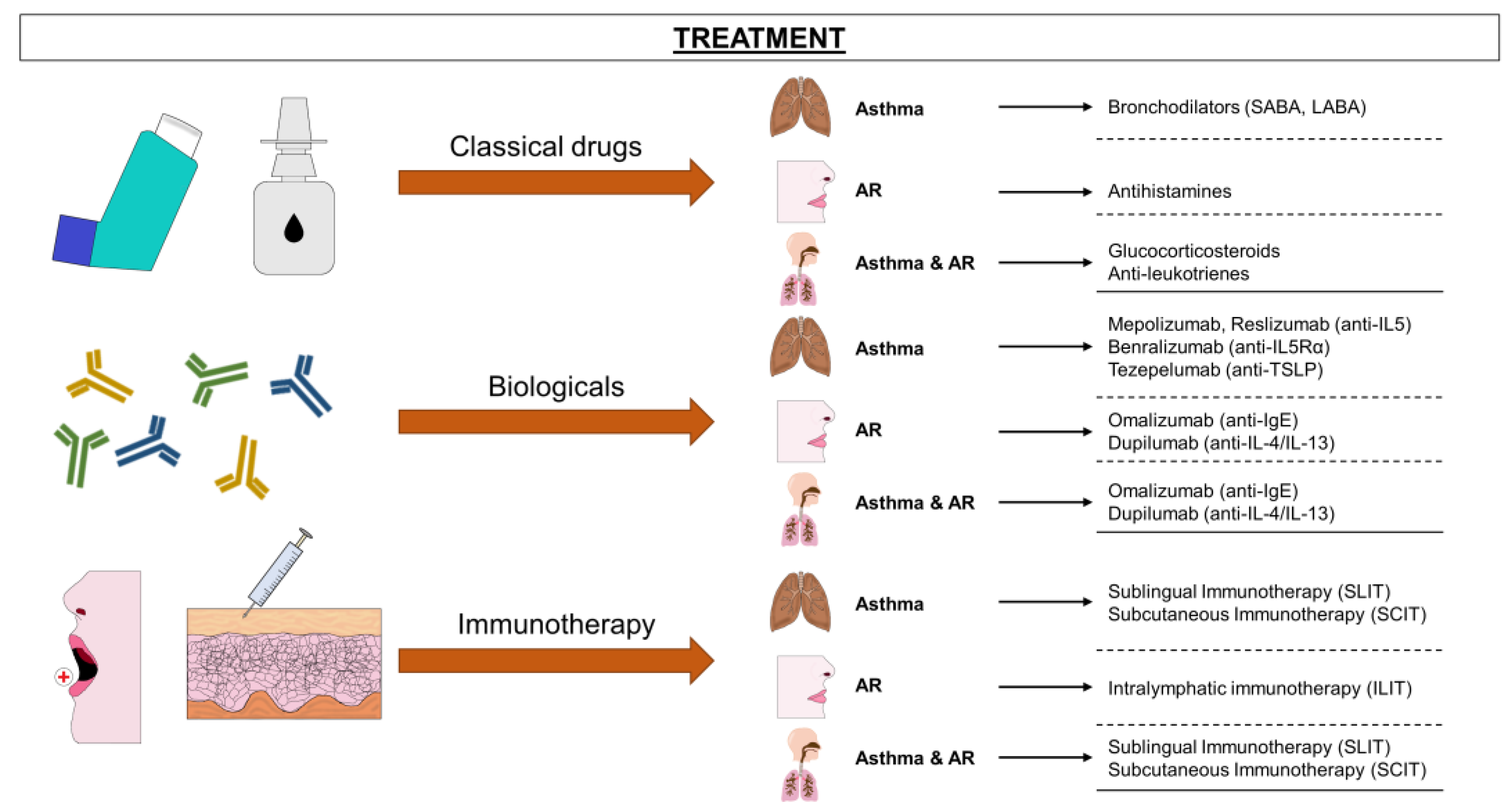
3.1.2. Asthma Treatment
3.2. Allergic Rhinitis
3.2.1. Diagnosis of Allergic Rhinitis
Clinical Tools to Diagnose Allergic Rhinitis
Cellular Diagnostic of Allergic Rhinitis
Molecular Diagnostic Parameters in Allergic Rhinitis
3.2.2. Treatment of Allergic Rhinitis
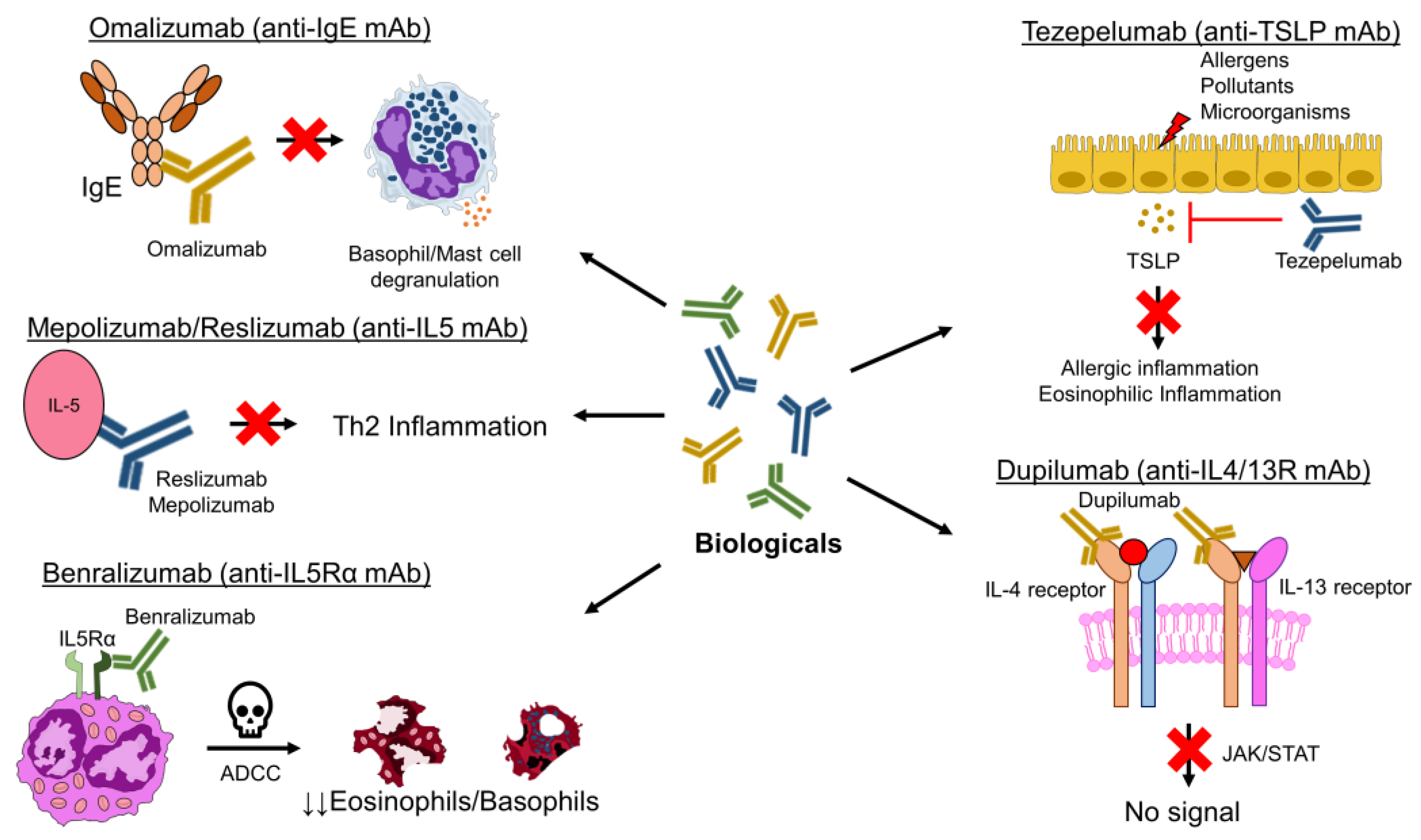
3.3. Biologicals in Asthma and Allergic Rhinitis
3.3.1. Omalizumab (Anti-IgE)
3.3.2. Mepolizumab and Reslizumab (Anti-IL-5)
3.3.3. Benralizumab (Anti-IL-5 Receptor)
3.3.4. Dupilumab (Anti-IL-4/13 Receptor)
3.3.5. Novel Biologic Therapies
3.4. Allergen-Specific Immunotherapy
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- GBD Chronic Respiratory Disease Collaborators. Prevalence and attributable health burden of chronic respiratory diseases, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet Respir. Med. 2020, 8, 585–596. [Google Scholar] [CrossRef]
- Eguiluz-Gracia, I.; Mathioudakis, A.G.; Bartel, S.; Vijverberg, S.J.H.; Fuertes, E.; Comberiati, P.; Cai, Y.S.; Tomazic, P.V.; Diamant, Z.; Vestbo, J.; et al. The need for clean air: The way air pollution and climate change affect allergic rhinitis and asthma. Allergy 2020, 75, 2170–2184. [Google Scholar] [CrossRef] [PubMed]
- Labaki, W.W.; Han, M.K. Chronic respiratory diseases: A global view. Lancet Respir. Med. 2020, 8, 531–533. [Google Scholar] [CrossRef]
- He, Z.F.; Zhong, N.S.; Guan, W.J. Impact of Chronic Respiratory Diseases on the Outcomes of COVID-19. Arch. Bronconeumol. 2022, 58, 5–7. [Google Scholar] [CrossRef]
- Reddel, H.K.; Bacharier, L.B.; Bateman, E.D.; Brightling, C.E.; Brusselle, G.G.; Buhl, R.; Cruz, A.A.; Duijts, L.; Drazen, J.M.; FitzGerald, J.M.; et al. Global Initiative for Asthma Strategy 2021: Executive summary and rationale for key changes. Eur. Respir. J. 2022, 59, 2102730. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Available online: https://www.who.int/news-room/fact-sheets/detail/asthma (accessed on 20 October 2022).
- Kuruvilla, M.E.; Lee, F.E.; Lee, G.B. Understanding Asthma Phenotypes, Endotypes, and Mechanisms of Disease. Clin. Rev. Allergy Immunol. 2019, 56, 219–233. [Google Scholar] [CrossRef] [PubMed]
- Agache, I.; Eguiluz-Gracia, I.; Cojanu, C.; Laculiceanu, A.; Del Giacco, S.; Zemelka-Wiacek, M.; Kosowska, A.; Akdis, C.A.; Jutel, M. Advances and highlights in asthma in 2021. Allergy 2021, 76, 3390–3407. [Google Scholar] [CrossRef]
- Oliveria, J.P.; Agayby, R.; Gauvreau, G.M. Regulatory and IgE(+) B Cells in Allergic Asthma. Methods Mol. Biol. 2021, 2270, 375–418. [Google Scholar] [CrossRef]
- Ricciardolo, F.L.M.; Sprio, A.E.; Baroso, A.; Gallo, F.; Riccardi, E.; Bertolini, F.; Carriero, V.; Arrigo, E.; Ciprandi, G. Characterization of T2-Low and T2-High Asthma Phenotypes in Real-Life. Biomedicines 2021, 9, 1684. [Google Scholar] [CrossRef] [PubMed]
- Sze, E.; Bhalla, A.; Nair, P. Mechanisms and therapeutic strategies for non-T2 asthma. Allergy 2020, 75, 311–325. [Google Scholar] [CrossRef]
- Hudey, S.N.; Ledford, D.K.; Cardet, J.C. Mechanisms of non-type 2 asthma. Curr. Opin. Immunol. 2020, 66, 123–128. [Google Scholar] [CrossRef]
- Wang, R.; Murray, C.S.; Fowler, S.J.; Simpson, A.; Durrington, H.J. Asthma diagnosis: Into the fourth dimension. Thorax 2021, 76, 624–631. [Google Scholar] [CrossRef] [PubMed]
- Guilleminault, L.; Ouksel, H.; Belleguic, C.; Le Guen, Y.; Germaud, P.; Desfleurs, E.; Leroyer, C.; Magnan, A. Personalised medicine in asthma: From curative to preventive medicine. Eur. Respir. Rev. 2017, 26, 160010. [Google Scholar] [CrossRef] [PubMed]
- Asthma, G.I.f. Global Strategy for Asthma Management and Prevention. Available online: www.ginasthma.org (accessed on 16 November 2022).
- Bernstein, I.L.; Li, J.T.; Bernstein, D.I.; Hamilton, R.; Spector, S.L.; Tan, R.; Sicherer, S.; Golden, D.B.; Khan, D.A.; Nicklas, R.A.; et al. Allergy diagnostic testing: An updated practice parameter. Ann. Allergy Asthma Immunol. 2008, 100, S1–S148. [Google Scholar] [CrossRef] [PubMed]
- Coates, A.L.; Wanger, J.; Cockcroft, D.W.; Culver, B.H.; Carlsen, K.-H.; Diamant, Z.; Gauvreau, G.; Hall, G.L.; Hallstrand, T.S.; Horvath, I.; et al. ERS technical standard on bronchial challenge testing: General considerations and performance of methacholine challenge tests. Eur. Respir. J. 2017, 49, 1601526. [Google Scholar] [CrossRef]
- Parsons, J.P.; Hallstrand, T.S.; Mastronarde, J.G.; Kaminsky, D.A.; Rundell, K.W.; Hull, J.H.; Storms, W.W.; Weiler, J.M.; Cheek, F.M.; Wilson, K.C.; et al. An official American Thoracic Society clinical practice guideline: Exercise-induced bronchoconstriction. Am. J. Respir. Crit. Care Med. 2013, 187, 1016–1027. [Google Scholar] [CrossRef]
- Saito, J.; Inoue, K.; Sugawara, A.; Yoshikawa, M.; Watanabe, K.; Ishida, T.; Ohtsuka, Y.; Munakata, M. Exhaled nitric oxide as a marker of airway inflammation for an epidemiologic study in schoolchildren. J. Allergy Clin. Immunol. 2004, 114, 512–516. [Google Scholar] [CrossRef]
- Reddel, H.K. Peak flow monitoring in clinical practice and clinical asthma trials. Curr. Opin. Pulm. Med. 2006, 12, 75–81. [Google Scholar] [CrossRef]
- James, B.N.; Oyeniran, C.; Sturgill, J.L.; Newton, J.; Martin, R.K.; Bieberich, E.; Weigel, C.; Maczis, M.A.; Palladino, E.N.D.; Lownik, J.C.; et al. Ceramide in apoptosis and oxidative stress in allergic inflammation and asthma. J. Allergy Clin. Immunol. 2021, 147, 1936–1948. [Google Scholar] [CrossRef]
- Spanish Asthma Management Guidelines (GEMA 5.0 2022). Available online: https://www.gemasma.com (accessed on 11 January 2023).
- Fahy, J.V. Type 2 inflammation in asthma--present in most, absent in many. Nat. Rev. Immunol. 2015, 15, 57–65. [Google Scholar] [CrossRef]
- Breiteneder, H.; Peng, Y.Q.; Agache, I.; Diamant, Z.; Eiwegger, T.; Fokkens, W.J.; Traidl-Hoffmann, C.; Nadeau, K.; O’Hehir, R.E.; O’Mahony, L.; et al. Biomarkers for diagnosis and prediction of therapy responses in allergic diseases and asthma. Allergy 2020, 75, 3039–3068. [Google Scholar] [CrossRef] [PubMed]
- Agache, I.; Akdis, C.A. Precision medicine and phenotypes, endotypes, genotypes, regiotypes, and theratypes of allergic diseases. J. Clin. Investig. 2019, 129, 1493–1503. [Google Scholar] [CrossRef] [PubMed]
- Ogulur, I.; Pat, Y.; Ardicli, O.; Barletta, E.; Cevhertas, L.; Fernandez-Santamaria, R.; Huang, M.; Bel Imam, M.; Koch, J.; Ma, S.; et al. Advances and highlights in biomarkers of allergic diseases. Allergy 2021, 76, 3659–3686. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Morita, H.; Sokolowska, M.; Tan, G.; Boonpiyathad, T.; Opitz, L.; Orimo, K.; Archer, S.K.; Jansen, K.; Tang, M.L.K.; et al. Gene expression signatures of circulating human type 1, 2, and 3 innate lymphoid cells. J. Allergy Clin. Immunol. 2019, 143, 2321–2325. [Google Scholar] [CrossRef]
- Matsumoto, H. Roles of Periostin in Asthma. Adv. Exp. Med. Biol. 2019, 1132, 145–159. [Google Scholar] [CrossRef] [PubMed]
- Izuhara, K.; Ohta, S.; Ono, J. Using Periostin as a Biomarker in the Treatment of Asthma. Allergy Asthma Immunol. Res. 2016, 8, 491–498. [Google Scholar] [CrossRef]
- Santos, A.F.; Alpan, O.; Hoffmann, H.J. Basophil activation test: Mechanisms and considerations for use in clinical trials and clinical practice. Allergy 2021, 76, 2420–2432. [Google Scholar] [CrossRef]
- Dahlen, B.; Nopp, A.; Johansson, S.G.; Eduards, M.; Skedinger, M.; Adedoyin, J. Basophil allergen threshold sensitivity, CD-sens, is a measure of allergen sensitivity in asthma. Clin. Exp. Allergy 2011, 41, 1091–1097. [Google Scholar] [CrossRef]
- Diamant, Z.; Vijverberg, S.; Alving, K.; Bakirtas, A.; Bjermer, L.; Custovic, A.; Dahlen, S.E.; Gaga, M.; Gerth van Wijk, R.; Giacco, S.D.; et al. Toward clinically applicable biomarkers for asthma: An EAACI position paper. Allergy 2019, 74, 1835–1851. [Google Scholar] [CrossRef]
- Perkins, T.N.; Donnell, M.L.; Oury, T.D. The axis of the receptor for advanced glycation endproducts in asthma and allergic airway disease. Allergy 2021, 76, 1350–1366. [Google Scholar] [CrossRef]
- McDowell, P.J.; Heaney, L.G. Different endotypes and phenotypes drive the heterogeneity in severe asthma. Allergy 2020, 75, 302–310. [Google Scholar] [CrossRef] [PubMed]
- Alving, K.; Diamant, Z.; Lucas, S.; Magnussen, H.; Pavord, I.D.; Piacentini, G.; Price, D.; Roche, N.; Sastre, J.; Thomas, M.; et al. Point-of-care biomarkers in asthma management: Time to move forward. Allergy 2020, 75, 995–997. [Google Scholar] [CrossRef] [PubMed]
- Wasti, B.; Liu, S.K.; Xiang, X.D. Role of Epigenetics in the Pathogenesis, Treatment, Prediction, and Cellular Transformation of Asthma. Mediat. Inflamm. 2021, 2021, 9412929. [Google Scholar] [CrossRef] [PubMed]
- Koenderman, L.; Hassani, M.; Mukherjee, M.; Nair, P. Monitoring eosinophils to guide therapy with biologics in asthma: Does the compartment matter? Allergy 2021, 76, 1294–1297. [Google Scholar] [CrossRef] [PubMed]
- Weidner, J.; Bartel, S.; Kilic, A.; Zissler, U.M.; Renz, H.; Schwarze, J.; Schmidt-Weber, C.B.; Maes, T.; Rebane, A.; Krauss-Etschmann, S.; et al. Spotlight on microRNAs in allergy and asthma. Allergy 2021, 76, 1661–1678. [Google Scholar] [CrossRef] [PubMed]
- Pua, H.H.; Ansel, K.M. MicroRNA regulation of allergic inflammation and asthma. Curr. Opin. Immunol. 2015, 36, 101–108. [Google Scholar] [CrossRef]
- Panganiban, R.P.; Wang, Y.; Howrylak, J.; Chinchilli, V.M.; Craig, T.J.; August, A.; Ishmael, F.T. Circulating microRNAs as biomarkers in patients with allergic rhinitis and asthma. J. Allergy Clin. Immunol. 2016, 137, 1423–1432. [Google Scholar] [CrossRef]
- Kho, A.T.; Sharma, S.; Davis, J.S.; Spina, J.; Howard, D.; McEnroy, K.; Moore, K.; Sylvia, J.; Qiu, W.; Weiss, S.T.; et al. Circulating MicroRNAs: Association with Lung Function in Asthma. PLoS ONE 2016, 11, e0157998. [Google Scholar] [CrossRef]
- Kho, A.T.; McGeachie, M.J.; Moore, K.G.; Sylvia, J.M.; Weiss, S.T.; Tantisira, K.G. Circulating microRNAs and prediction of asthma exacerbation in childhood asthma. Respir. Res. 2018, 19, 128. [Google Scholar] [CrossRef]
- Davis, J.S.; Sun, M.; Kho, A.T.; Moore, K.G.; Sylvia, J.M.; Weiss, S.T.; Lu, Q.; Tantisira, K.G. Circulating microRNAs and association with methacholine PC20 in the Childhood Asthma Management Program (CAMP) cohort. PLoS ONE 2017, 12, e0180329. [Google Scholar] [CrossRef]
- Lefaudeux, D.; De Meulder, B.; Loza, M.J.; Peffer, N.; Rowe, A.; Baribaud, F.; Bansal, A.T.; Lutter, R.; Sousa, A.R.; Corfield, J.; et al. U-BIOPRED clinical adult asthma clusters linked to a subset of sputum omics. J. Allergy Clin. Immunol. 2017, 139, 1797–1807. [Google Scholar] [CrossRef] [PubMed]
- Kuo, C.S.; Pavlidis, S.; Loza, M.; Baribaud, F.; Rowe, A.; Pandis, I.; Sousa, A.; Corfield, J.; Djukanovic, R.; Lutter, R.; et al. T-helper cell type 2 (Th2) and non-Th2 molecular phenotypes of asthma using sputum transcriptomics in U-BIOPRED. Eur. Respir. J. 2017, 49, 1602135. [Google Scholar] [CrossRef] [PubMed]
- Guerra, E.N.S.; Acevedo, A.C.; de Toledo, I.P.; Combes, A.; Chardin, H. Do mucosal biomarkers reveal the immunological state associated with food allergy? Allergy 2018, 73, 2392–2394. [Google Scholar] [CrossRef]
- Walter, J.; O’Mahony, L. The importance of social networks-An ecological and evolutionary framework to explain the role of microbes in the aetiology of allergy and asthma. Allergy 2019, 74, 2248–2251. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.J.; Nariya, S.; Harris, J.M.; Lynch, S.V.; Choy, D.F.; Arron, J.R.; Boushey, H. The airway microbiome in patients with severe asthma: Associations with disease features and severity. J. Allergy Clin. Immunol. 2015, 136, 874–884. [Google Scholar] [CrossRef]
- Pitsios, C. Allergen Immunotherapy: Biomarkers and Clinical Outcome Measures. J. Asthma Allergy 2021, 14, 141–148. [Google Scholar] [CrossRef]
- Lunjani, N.; Satitsuksanoa, P.; Lukasik, Z.; Sokolowska, M.; Eiwegger, T.; O’Mahony, L. Recent developments and highlights in mechanisms of allergic diseases: Microbiome. Allergy 2018, 73, 2314–2327. [Google Scholar] [CrossRef]
- Ivanova, O.; Richards, L.B.; Vijverberg, S.J.; Neerincx, A.H.; Sinha, A.; Sterk, P.J.; Maitland-van der Zee, A.H. What did we learn from multiple omics studies in asthma? Allergy 2019, 74, 2129–2145. [Google Scholar] [CrossRef]
- Schofield, J.P.R.; Burg, D.; Nicholas, B.; Strazzeri, F.; Brandsma, J.; Staykova, D.; Folisi, C.; Bansal, A.T.; Xian, Y.; Guo, Y.; et al. Stratification of asthma phenotypes by airway proteomic signatures. J. Allergy Clin. Immunol. 2019, 144, 70–82. [Google Scholar] [CrossRef]
- Nieto-Fontarigo, J.J.; Gonzalez-Barcala, F.J.; Andrade-Bulos, L.J.; San-Jose, M.E.; Cruz, M.J.; Valdes-Cuadrado, L.; Crujeiras, R.M.; Arias, P.; Salgado, F.J. iTRAQ-based proteomic analysis reveals potential serum biomarkers of allergic and nonallergic asthma. Allergy 2020, 75, 3171–3183. [Google Scholar] [CrossRef]
- Abdel-Aziz, M.I.; de Vries, R.; Lammers, A.; Xu, B.; Neerincx, A.H.; Vijverberg, S.J.H.; Dagelet, Y.W.F.; Kraneveld, A.D.; Frey, U.; Lutter, R.; et al. Cross-sectional biomarker comparisons in asthma monitoring using a longitudinal design: The eNose premise. Allergy 2020, 75, 2690–2693. [Google Scholar] [CrossRef] [PubMed]
- Sokolowska, M.; Rovati, G.E.; Diamant, Z.; Untersmayr, E.; Schwarze, J.; Lukasik, Z.; Sava, F.; Angelina, A.; Palomares, O.; Akdis, C.A.; et al. Current perspective on eicosanoids in asthma and allergic diseases: EAACI Task Force consensus report, part I. Allergy 2021, 76, 114–130. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Zhao, Q.; Wang, S. The role of serum periostin in the diagnosis of asthma: A meta-analysis. Allergy Asthma Proc. 2020, 41, 240–247. [Google Scholar] [CrossRef] [PubMed]
- Asano, T.; Ohbayashi, H.; Ariga, M.; Furuta, O.; Kudo, S.; Ono, J.; Izuhara, K. Serum periostin reflects dynamic hyperinflation in patients with asthma. ERJ Open Res. 2020, 6, 00347-2019. [Google Scholar] [CrossRef] [PubMed]
- Eguiluz-Gracia, I.; Tay, T.R.; Hew, M.; Escribese, M.M.; Barber, D.; O’Hehir, R.E.; Torres, M.J. Recent developments and highlights in biomarkers in allergic diseases and asthma. Allergy 2018, 73, 2290–2305. [Google Scholar] [CrossRef]
- Hur, G.Y.; Pham, A.; Miller, M.; Weng, N.; Hu, J.; Kurten, R.C.; Broide, D.H. ORMDL3 but not neighboring 17q21 gene LRRC3C is expressed in human lungs and lung cells of asthmatics. Allergy 2020, 75, 2061–2065. [Google Scholar] [CrossRef]
- Yang, I.V.; Pedersen, B.S.; Liu, A.H.; O’Connor, G.T.; Pillai, D.; Kattan, M.; Misiak, R.T.; Gruchalla, R.; Szefler, S.J.; Khurana Hershey, G.K.; et al. The nasal methylome and childhood atopic asthma. J. Allergy Clin. Immunol. 2017, 139, 1478–1488. [Google Scholar] [CrossRef]
- Li, C.Y.; Peng, J.; Ren, L.P.; Gan, L.X.; Lu, X.J.; Liu, Q.; Gu, W.; Guo, X.J. Roles of histone hypoacetylation in LAT expression on T cells and Th2 polarization in allergic asthma. J. Transl. Med. 2013, 11, 26. [Google Scholar] [CrossRef]
- Kidd, C.D.; Thompson, P.J.; Barrett, L.; Baltic, S. Histone Modifications and Asthma. The Interface of the Epigenetic and Genetic Landscapes. Am. J. Respir. Cell Mol. Biol. 2016, 54, 3–12. [Google Scholar] [CrossRef]
- Harb, H.; Raedler, D.; Ballenberger, N.; Bock, A.; Kesper, D.A.; Renz, H.; Schaub, B. Childhood allergic asthma is associated with increased IL-13 and FOXP3 histone acetylation. J. Allergy Clin. Immunol. 2015, 136, 200–202. [Google Scholar] [CrossRef]
- Hirai, K.; Shirai, T.; Shimoshikiryo, T.; Ueda, M.; Gon, Y.; Maruoka, S.; Itoh, K. Circulating microRNA-15b-5p as a biomarker for asthma-COPD overlap. Allergy 2021, 76, 766–774. [Google Scholar] [CrossRef] [PubMed]
- Specjalski, K.; Niedoszytko, M. MicroRNAs: Future biomarkers and targets of therapy in asthma? Curr. Opin. Pulm. Med. 2020, 26, 285–292. [Google Scholar] [CrossRef]
- Simpson, L.J.; Patel, S.; Bhakta, N.R.; Choy, D.F.; Brightbill, H.D.; Ren, X.; Wang, Y.; Pua, H.H.; Baumjohann, D.; Montoya, M.M.; et al. A microRNA upregulated in asthma airway T cells promotes TH2 cytokine production. Nat. Immunol. 2014, 15, 1162–1170. [Google Scholar] [CrossRef] [PubMed]
- Pinkerton, M.; Chinchilli, V.; Banta, E.; Craig, T.; August, A.; Bascom, R.; Cantorna, M.; Harvill, E.; Ishmael, F.T. Differential expression of microRNAs in exhaled breath condensates of patients with asthma, patients with chronic obstructive pulmonary disease, and healthy adults. J. Allergy Clin. Immunol. 2013, 132, 217–219. [Google Scholar] [CrossRef] [PubMed]
- Panganiban, R.P.; Pinkerton, M.H.; Maru, S.Y.; Jefferson, S.J.; Roff, A.N.; Ishmael, F.T. Differential microRNA epression in asthma and the role of miR-1248 in regulation of IL-5. Am. J. Clin. Exp. Immunol. 2012, 1, 154–165. [Google Scholar]
- Polikepahad, S.; Knight, J.M.; Naghavi, A.O.; Oplt, T.; Creighton, C.J.; Shaw, C.; Benham, A.L.; Kim, J.; Soibam, B.; Harris, R.A.; et al. Proinflammatory role for let-7 microRNAS in experimental asthma. J. Biol. Chem. 2010, 285, 30139–30149. [Google Scholar] [CrossRef]
- Nakano, T.; Inoue, Y.; Shimojo, N.; Yamaide, F.; Morita, Y.; Arima, T.; Tomiita, M.; Kohno, Y. Lower levels of hsa-mir-15a, which decreases VEGFA, in the CD4+ T cells of pediatric patients with asthma. J. Allergy Clin. Immunol. 2013, 132, 1224–1227. [Google Scholar] [CrossRef]
- Feketea, G.; Bocsan, C.I.; Popescu, C.; Gaman, M.; Stanciu, L.A.; Zdrenghea, M.T. A Review of Macrophage MicroRNAs’ Role in Human Asthma. Cells 2019, 8, 420. [Google Scholar] [CrossRef]
- Wardzynska, A.; Pawelczyk, M.; Rywaniak, J.; Makowska, J.; Jamroz-Brzeska, J.; Kowalski, M.L. Circulating miRNA expression in asthmatics is age-related and associated with clinical asthma parameters, respiratory function and systemic inflammation. Respir. Res. 2021, 22, 177. [Google Scholar] [CrossRef]
- Torregrosa Paredes, P.; Esser, J.; Admyre, C.; Nord, M.; Rahman, Q.K.; Lukic, A.; Radmark, O.; Gronneberg, R.; Grunewald, J.; Eklund, A.; et al. Bronchoalveolar lavage fluid exosomes contribute to cytokine and leukotriene production in allergic asthma. Allergy 2012, 67, 911–919. [Google Scholar] [CrossRef]
- Sastre, B.; Canas, J.A.; Rodrigo-Munoz, J.M.; Del Pozo, V. Novel Modulators of Asthma and Allergy: Exosomes and MicroRNAs. Front. Immunol. 2017, 8, 826. [Google Scholar] [CrossRef] [PubMed]
- Levanen, B.; Bhakta, N.R.; Torregrosa Paredes, P.; Barbeau, R.; Hiltbrunner, S.; Pollack, J.L.; Skold, C.M.; Svartengren, M.; Grunewald, J.; Gabrielsson, S.; et al. Altered microRNA profiles in bronchoalveolar lavage fluid exosomes in asthmatic patients. J. Allergy Clin. Immunol. 2013, 131, 894–903. [Google Scholar] [CrossRef]
- Kyyaly, M.A.; Vorobeva, E.V.; Kothalawala, D.M.; Fong, W.C.G.; He, P.; Sones, C.L.; Al-Zahrani, M.; Sanchez-Elsner, T.; Arshad, S.H.; Kurukulaaratchy, R.J. MicroRNAs-A Promising Tool for Asthma Diagnosis and Severity Assessment: A Systematic Review. J. Pers. Med. 2022, 12, 543. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.B.; Wang, M.Y.; Zhu, H.Y.; Tang, S.Q.; You, Y.D.; Xie, Y.Q. Overexpression of microRNA-21 and microRNA-126 in the patients of bronchial asthma. Int. J. Clin. Exp. Med. 2014, 7, 1307–1312. [Google Scholar] [PubMed]
- Hammad Mahmoud Hammad, R.; Hamed, D.; Eldosoky, M.; Ahmad, A.; Osman, H.M.; Abd Elgalil, H.M.; Mahmoud Hassan, M.M. Plasma microRNA-21, microRNA-146a and IL-13 expression in asthmatic children. Innate Immun. 2018, 24, 171–179. [Google Scholar] [CrossRef]
- ElKashef, S.; Ahmad, S.E.; Soliman, Y.M.A.; Mostafa, M.S. Role of microRNA-21 and microRNA-155 as biomarkers for bronchial asthma. Innate Immun. 2021, 27, 61–69. [Google Scholar] [CrossRef]
- Maes, T.; Cobos, F.A.; Schleich, F.; Sorbello, V.; Henket, M.; De Preter, K.; Bracke, K.R.; Conickx, G.; Mesnil, C.; Vandesompele, J.; et al. Asthma inflammatory phenotypes show differential microRNA expression in sputum. J. Allergy Clin. Immunol. 2016, 137, 1433–1446. [Google Scholar] [CrossRef]
- Shi, J.; Chen, M.; Ouyang, L.; Wang, Q.; Guo, Y.; Huang, L.; Jiang, S. miR-142-5p and miR-130a-3p regulate pulmonary macrophage polarization and asthma airway remodeling. Immunol. Cell Biol. 2020, 98, 715–725. [Google Scholar] [CrossRef]
- Bartel, S.; Carraro, G.; Alessandrini, F.; Krauss-Etschmann, S.; Ricciardolo, F.L.M.; Bellusci, S. miR-142-3p is associated with aberrant WNT signaling during airway remodeling in asthma. Am. J. Physiol. Lung Cell Mol. Physiol. 2018, 315, 328–333. [Google Scholar] [CrossRef]
- Comer, B.S.; Camoretti-Mercado, B.; Kogut, P.C.; Halayko, A.J.; Solway, J.; Gerthoffer, W.T. MicroRNA-146a and microRNA-146b expression and anti-inflammatory function in human airway smooth muscle. Am. J. Physiol. Lung Cell Mol. Physiol. 2014, 307, 727–734. [Google Scholar] [CrossRef]
- Malmhall, C.; Johansson, K.; Winkler, C.; Alawieh, S.; Ekerljung, L.; Radinger, M. Altered miR-155 Expression in Allergic Asthmatic Airways. Scand. J. Immunol. 2017, 85, 300–307. [Google Scholar] [CrossRef]
- Rijavec, M.; Korosec, P.; Zavbi, M.; Kern, I.; Malovrh, M.M. Let-7a is differentially expressed in bronchial biopsies of patients with severe asthma. Sci. Rep. 2014, 4, 6103. [Google Scholar] [CrossRef]
- Shaik, N.A.; Nasser, K.; Mohammed, A.; Mujalli, A.; Obaid, A.A.; El-Harouni, A.A.; Elango, R.; Banaganapalli, B. Identification of miRNA-mRNA-TFs regulatory network and crucial pathways involved in asthma through advanced systems biology approaches. PLoS ONE 2022, 17, e0271262. [Google Scholar] [CrossRef]
- Wise, S.K.; Lin, S.Y.; Toskala, E.; Orlandi, R.R.; Akdis, C.A.; Alt, J.A.; Azar, A.; Baroody, F.M.; Bachert, C.; Canonica, G.W.; et al. International Consensus Statement on Allergy and Rhinology: Allergic Rhinitis. Int. Forum Allergy Rhinol. 2018, 8, 108–352. [Google Scholar] [CrossRef]
- Zielen, S.; Devillier, P.; Heinrich, J.; Richter, H.; Wahn, U. Sublingual immunotherapy provides long-term relief in allergic rhinitis and reduces the risk of asthma: A retrospective, real-world database analysis. Allergy 2018, 73, 165–177. [Google Scholar] [CrossRef]
- Dong, X.; Zhong, N.; Fang, Y.; Cai, Q.; Lu, M.; Lu, Q. MicroRNA 27b-3p Modulates SYK in Pediatric Asthma Induced by Dust Mites. Front. Pediatr. 2018, 6, 301. [Google Scholar] [CrossRef]
- Zhang, K.; Liang, Y.; Feng, Y.; Wu, W.; Zhang, H.; He, J.; Hu, Q.; Zhao, J.; Xu, Y.; Liu, Z.; et al. Decreased epithelial and sputum miR-221-3p associates with airway eosinophilic inflammation and CXCL17 expression in asthma. Am. J. Physiol. Lung Cell Mol. Physiol. 2018, 315, 253–264. [Google Scholar] [CrossRef] [PubMed]
- Weidner, J.; Ekerljung, L.; Malmhall, C.; Miron, N.; Radinger, M. Circulating microRNAs correlate to clinical parameters in individuals with allergic and non-allergic asthma. Respir Res 2020, 21, 107. [Google Scholar] [CrossRef] [PubMed]
- Sun, Q.; Liu, L.; Wang, H.; Mandal, J.; Khan, P.; Hostettler, K.E.; Stolz, D.; Tamm, M.; Molino, A.; Lardinois, D.; et al. Constitutive high expression of protein arginine methyltransferase 1 in asthmatic airway smooth muscle cells is caused by reduced microRNA-19a expression and leads to enhanced remodeling. J. Allergy Clin. Immunol. 2017, 140, 510–524. [Google Scholar] [CrossRef] [PubMed]
- Haj-Salem, I.; Fakhfakh, R.; Berube, J.C.; Jacques, E.; Plante, S.; Simard, M.J.; Bosse, Y.; Chakir, J. MicroRNA-19a enhances proliferation of bronchial epithelial cells by targeting TGFbetaR2 gene in severe asthma. Allergy 2015, 70, 212–219. [Google Scholar] [CrossRef] [PubMed]
- Rodrigo-Munoz, J.M.; Canas, J.A.; Sastre, B.; Rego, N.; Greif, G.; Rial, M.; Minguez, P.; Mahillo-Fernandez, I.; Fernandez-Nieto, M.; Mora, I.; et al. Asthma diagnosis using integrated analysis of eosinophil microRNAs. Allergy 2019, 74, 507–517. [Google Scholar] [CrossRef] [PubMed]
- Papi, A.; Brightling, C.; Pedersen, S.E.; Reddel, H.K. Asthma. Lancet 2018, 391, 783–800. [Google Scholar] [CrossRef]
- Tabar, A.I.; Delgado, J.; Gonzalez-Mancebo, E.; Arroabarren, E.; Soto Retes, L.; Dominguez-Ortega, J.; Spanish Allergy and Clinical Immunology Scientific Society (SEAIC). Recent Advances in Allergen-Specific Immunotherapy as Treatment for Allergic Asthma: A Practical Overview. Int. Arch. Allergy Immunol. 2021, 182, 496–514. [Google Scholar] [CrossRef] [PubMed]
- Schoettler, N.; Strek, M.E. Recent Advances in Severe Asthma: From Phenotypes to Personalized Medicine. Chest 2020, 157, 516–528. [Google Scholar] [CrossRef]
- Lommatzsch, M.; Buhl, R.; Korn, S. The Treatment of Mild and Moderate Asthma in Adults. Dtsch. Arztebl. Int. 2020, 117, 434–444. [Google Scholar] [CrossRef] [PubMed]
- Sobieraj, D.M.; Baker, W.L. Medications for Asthma. JAMA 2018, 319, 1520. [Google Scholar] [CrossRef]
- Kwah, J.H.; Peters, A.T. Asthma in adults: Principles of treatment. Allergy Asthma Proc. 2019, 40, 396–402. [Google Scholar] [CrossRef] [PubMed]
- Kume, H.; Fukunaga, K.; Oguma, T. Research and development of bronchodilators for asthma and COPD with a focus on G protein/KCa channel linkage and beta2-adrenergic intrinsic efficacy. Pharmacol. Ther. 2015, 156, 75–89. [Google Scholar] [CrossRef]
- Heffler, E.; Madeira, L.N.G.; Ferrando, M.; Puggioni, F.; Racca, F.; Malvezzi, L.; Passalacqua, G.; Canonica, G.W. Inhaled Corticosteroids Safety and Adverse Effects in Patients with Asthma. J. Allergy Clin. Immunol. Pract. 2018, 6, 776–781. [Google Scholar] [CrossRef]
- Philip, J. The effects of inhaled corticosteroids on growth in children. Open Respir. Med. J. 2014, 8, 66–73. [Google Scholar] [CrossRef]
- Sullivan, P.W.; Ghushchyan, V.H.; Globe, G.; Schatz, M. Oral corticosteroid exposure and adverse effects in asthmatic patients. J. Allergy Clin. Immunol. 2018, 141, 110–116. [Google Scholar] [CrossRef] [PubMed]
- Price, D.B.; Trudo, F.; Voorham, J.; Xu, X.; Kerkhof, M.; Jie, J.L.Z.; Tran, T.N. Adverse outcomes from initiation of systemic corticosteroids for asthma: Long-term observational study. J. Asthma Allergy 2018, 11, 193–204. [Google Scholar] [CrossRef] [PubMed]
- Figueroa, D.J.; Breyer, R.M.; Defoe, S.K.; Kargman, S.; Daugherty, B.L.; Waldburger, K.; Liu, Q.; Clements, M.; Zeng, Z.; O’Neill, G.P.; et al. Expression of the cysteinyl leukotriene 1 receptor in normal human lung and peripheral blood leukocytes. Am. J. Respir. Crit. Care Med. 2001, 163, 226–233. [Google Scholar] [CrossRef] [PubMed]
- Ban, G.Y.; Kim, S.H.; Park, H.S. Persistent Eosinophilic Inflammation in Adult Asthmatics with High Serum and Urine Levels of Leukotriene E4. J. Asthma Allergy 2021, 14, 1219–1230. [Google Scholar] [CrossRef]
- Yokomizo, T.; Nakamura, M.; Shimizu, T. Leukotriene receptors as potential therapeutic targets. J. Clin. Investig. 2018, 128, 2691–2701. [Google Scholar] [CrossRef]
- Chauhan, B.F.; Ducharme, F.M. Anti-leukotriene agents compared to inhaled corticosteroids in the management of recurrent and/or chronic asthma in adults and children. Cochrane Database Syst. Rev. 2012, 2012, CD002314. [Google Scholar] [CrossRef]
- Bleecker, E.R.; Welch, M.J.; Weinstein, S.F.; Kalberg, C.; Johnson, M.; Edwards, L.; Rickard, K.A. Low-dose inhaled fluticasone propionate versus oral zafirlukast in the treatment of persistent asthma. J. Allergy Clin. Immunol. 2000, 105, 1123–1129. [Google Scholar] [CrossRef]
- Gosens, R.; Gross, N. The mode of action of anticholinergics in asthma. Eur. Respir. J. 2018, 52, 1701247. [Google Scholar] [CrossRef]
- Buels, K.S.; Fryer, A.D. Muscarinic receptor antagonists: Effects on pulmonary function. Handb. Exp. Pharmacol. 2012, 208, 317–341. [Google Scholar] [CrossRef]
- Egan, M.; Bunyavanich, S. Allergic rhinitis: The “Ghost Diagnosis” in patients with asthma. Asthma Res. Pract. 2015, 1, 8. [Google Scholar] [CrossRef]
- Akhouri, S.; House, S.A. Allergic Rhinitis; StatPearls: Treasure Island, FL, USA, 2022. [Google Scholar]
- Skoner, D.P. Allergic rhinitis: Definition, epidemiology, pathophysiology, detection, and diagnosis. J. Allergy Clin. Immunol. 2001, 108, 2–8. [Google Scholar] [CrossRef]
- Eguiluz-Gracia, I.; Testera-Montes, A.; Gonzalez, M.; Perez-Sanchez, N.; Ariza, A.; Salas, M.; Moreno-Aguilar, C.; Campo, P.; Torres, M.J.; Rondon, C. Safety and reproducibility of nasal allergen challenge. Allergy 2019, 74, 1125–1134. [Google Scholar] [CrossRef] [PubMed]
- Gomez, E.; Campo, P.; Rondon, C.; Barrionuevo, E.; Blanca-Lopez, N.; Torres, M.J.; Herrera, R.; Galindo, L.; Mayorga, C.; Blanca, M. Role of the basophil activation test in the diagnosis of local allergic rhinitis. J. Allergy Clin. Immunol. 2013, 132, 975–976. [Google Scholar] [CrossRef]
- Gevaert, P.; Omachi, T.A.; Corren, J.; Mullol, J.; Han, J.; Lee, S.E.; Kaufman, D.; Ligueros-Saylan, M.; Howard, M.; Zhu, R.; et al. Efficacy and safety of omalizumab in nasal polyposis: 2 randomized phase 3 trials. J. Allergy Clin. Immunol. 2020, 146, 595–605. [Google Scholar] [CrossRef]
- Emson, C.; Corren, J.; Salapa, K.; Hellqvist, A.; Parnes, J.R.; Colice, G. Efficacy of Tezepelumab in Patients with Severe, Uncontrolled Asthma with and without Nasal Polyposis: A Post Hoc Analysis of the Phase 2b PATHWAY Study. J. Asthma Allergy 2021, 14, 91–99. [Google Scholar] [CrossRef] [PubMed]
- Bachert, C.; Sousa, A.R.; Lund, V.J.; Scadding, G.K.; Gevaert, P.; Nasser, S.; Durham, S.R.; Cornet, M.E.; Kariyawasam, H.H.; Gilbert, J.; et al. Reduced need for surgery in severe nasal polyposis with mepolizumab: Randomized trial. J. Allergy Clin. Immunol. 2017, 140, 1024–1031. [Google Scholar] [CrossRef]
- Bachert, C.; Han, J.K.; Desrosiers, M.; Hellings, P.W.; Amin, N.; Lee, S.E.; Mullol, J.; Greos, L.S.; Bosso, J.V.; Laidlaw, T.M.; et al. Efficacy and safety of dupilumab in patients with severe chronic rhinosinusitis with nasal polyps (LIBERTY NP SINUS-24 and LIBERTY NP SINUS-52): Results from two multicentre, randomised, double-blind, placebo-controlled, parallel-group phase 3 trials. Lancet 2019, 394, 1638–1650. [Google Scholar] [CrossRef] [PubMed]
- Dykewicz, M.S.; Wallace, D.V.; Amrol, D.J.; Baroody, F.M.; Bernstein, J.A.; Craig, T.J.; Dinakar, C.; Ellis, A.K.; Finegold, I.; Golden, D.B.K.; et al. Rhinitis 2020: A practice parameter update. J. Allergy Clin. Immunol. 2020, 146, 721–767. [Google Scholar] [CrossRef] [PubMed]
- Alobid, I.; Anton, E.; Armengot, M.; Chao, J.; Colas, C.; del Cuvillo, A.; Davila, I.; Dordal, M.T.; Escobar, C.; Fernandez-Parra, B.; et al. SEAIC-SEORL. Consensus Document on Nasal Polyposis. POLINA Project. J. Investig. Allergol. Clin. Immunol. 2011, 21 (Suppl. 1), 1–58. [Google Scholar]
- Bousquet, P.J.; Combescure, C.; Neukirch, F.; Klossek, J.M.; Mechin, H.; Daures, J.P.; Bousquet, J. Visual analog scales can assess the severity of rhinitis graded according to ARIA guidelines. Allergy 2007, 62, 367–372. [Google Scholar] [CrossRef]
- Seidman, M.D.; Gurgel, R.K.; Lin, S.Y.; Schwartz, S.R.; Baroody, F.M.; Bonner, J.R.; Dawson, D.E.; Dykewicz, M.S.; Hackell, J.M.; Han, J.K.; et al. Clinical practice guideline: Allergic rhinitis executive summary. Otolaryngol. Head Neck Surg. 2015, 152, 197–206. [Google Scholar] [CrossRef]
- Dordal, M.T.; Lluch-Bernal, M.; Sanchez, M.C.; Rondon, C.; Navarro, A.; Montoro, J.; Matheu, V.; Ibanez, M.D.; Fernandez-Parra, B.; Davila, I.; et al. Allergen-specific nasal provocation testing: Review by the rhinoconjunctivitis committee of the Spanish Society of Allergy and Clinical Immunology. J. Investig. Allergol. Clin. Immunol. 2011, 21, 1–12. [Google Scholar]
- Zhang, Y.; Lan, F.; Zhang, L. Advances and highlights in allergic rhinitis. Allergy 2021, 76, 3383–3389. [Google Scholar] [CrossRef] [PubMed]
- Small, P.; Keith, P.K.; Kim, H. Allergic rhinitis. Allergy Asthma Clin. Immunol. 2018, 14, 51. [Google Scholar] [CrossRef] [PubMed]
- Canonica, G.W.; Ansotegui, I.J.; Pawankar, R.; Schmid-Grendelmeier, P.; van Hage, M.; Baena-Cagnani, C.E.; Melioli, G.; Nunes, C.; Passalacqua, G.; Rosenwasser, L.; et al. A WAO—ARIA—GA(2)LEN consensus document on molecular-based allergy diagnostics. World Allergy Organ. J. 2013, 6, 17. [Google Scholar] [CrossRef] [PubMed]
- Luengo, O.; Cardona, V. Component resolved diagnosis: When should it be used? Clin. Transl. Allergy 2014, 4, 28. [Google Scholar] [CrossRef]
- Papadopoulos, N.G.; Bernstein, J.A.; Demoly, P.; Dykewicz, M.; Fokkens, W.; Hellings, P.W.; Peters, A.T.; Rondon, C.; Togias, A.; Cox, L.S. Phenotypes and endotypes of rhinitis and their impact on management: A PRACTALL report. Allergy 2015, 70, 474–494. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, R.G. Allergic sensitization is a key risk factor for but not synonymous with allergic disease. J. Allergy Clin. Immunol. 2014, 134, 360–361. [Google Scholar] [CrossRef] [PubMed]
- Campo, P.; Eguiluz-Gracia, I.; Bogas, G.; Salas, M.; Plaza Seron, C.; Perez, N.; Mayorga, C.; Torres, M.J.; Shamji, M.H.; Rondon, C. Local allergic rhinitis: Implications for management. Clin. Exp. Allergy 2019, 49, 6–16. [Google Scholar] [CrossRef] [PubMed]
- Vlaykov, A.N.; Tacheva, T.T.; Vlaykova, T.I.; Stoyanov, V.K. Serum and local IL-4, IL-5, IL-13 and immunoglobulin E in allergic rhinitis. Postepy Dermatol. Alergol. 2020, 37, 719–724. [Google Scholar] [CrossRef]
- Nur Husna, S.M.; Md Shukri, N.; Tuan Sharif, S.E.; Tan, H.T.T.; Mohd Ashari, N.S.; Wong, K.K. IL-4/IL-13 Axis in Allergic Rhinitis: Elevated Serum Cytokines Levels and Inverse Association With Tight Junction Molecules Expression. Front. Mol. Biosci. 2022, 9, 819772. [Google Scholar] [CrossRef]
- Li, C.; Xu, Y.; Luo, X.; Chen, F. The Effect of IL-18 on Group 2 Innate Lymphoid Cells in Allergic Rhinitis. Iran J. Immunol. 2021, 18, 188–194. [Google Scholar] [CrossRef]
- Kim, D.W.; Kim, D.K.; Eun, K.M.; Bae, J.S.; Chung, Y.J.; Xu, J.; Kim, Y.M.; Mo, J.H. IL-25 Could Be Involved in the Development of Allergic Rhinitis Sensitized to House Dust Mite. Mediat. Inflamm. 2017, 2017, 3908049. [Google Scholar] [CrossRef]
- Qiao, Y.; Chen, J. Serum levels of IL-31, IL-33 and ST2 in allergic rhinitis of children in China. Cell. Mol. Biol. 2018, 64, 52–55. [Google Scholar] [CrossRef]
- Tyurin, Y.A.; Lissovskaya, S.A.; Fassahov, R.S.; Mustafin, I.G.; Shamsutdinov, A.F.; Shilova, M.A.; Rizvanov, A.A. Cytokine Profile of Patients with Allergic Rhinitis Caused by Pollen, Mite, and Microbial Allergen Sensitization. J. Immunol. Res. 2017, 2017, 3054217. [Google Scholar] [CrossRef] [PubMed]
- Luo, X.; Zeng, Q.; Yan, S.; Liu, W.; Luo, R. MicroRNA-375-mediated regulation of ILC2 cells through TSLP in allergic rhinitis. World Allergy Organ. J. 2020, 13, 100451. [Google Scholar] [CrossRef] [PubMed]
- Rondon, C.; Eguiluz-Gracia, I.; Shamji, M.H.; Layhadi, J.A.; Salas, M.; Torres, M.J.; Campo, P. IgE Test in Secretions of Patients with Respiratory Allergy. Curr. Allergy Asthma Rep. 2018, 18, 67. [Google Scholar] [CrossRef]
- Eguiluz-Gracia, I.; Perez-Sanchez, N.; Bogas, G.; Campo, P.; Rondon, C. How to Diagnose and Treat Local Allergic Rhinitis: A Challenge for Clinicians. J. Clin. Med. 2019, 8, 1062. [Google Scholar] [CrossRef] [PubMed]
- Erkan, K.; Bozkurt, M.K.; Artac, H.; Ozdemir, H.; Unlu, A.; Korucu, E.N.; Elsurer, C. The role of regulatory T cells in allergic rhinitis and their correlation with IL-10, IL-17 and neopterin levels in serum and nasal lavage fluid. Eur. Arch. Otorhinolaryngol. 2020, 277, 1109–1114. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Yang, M.; Deng, J.; Wang, K.; Shi, J.; Sun, Y. Elevated Levels of Activated and Pathogenic Eosinophils Characterize Moderate-Severe House Dust Mite Allergic Rhinitis. J. Immunol. Res. 2020, 2020, 8085615. [Google Scholar] [CrossRef]
- Holgate, S.T.; Davies, D.E. Rethinking the pathogenesis of asthma. Immunity 2009, 31, 362–367. [Google Scholar] [CrossRef] [PubMed]
- Semik-Orzech, A.; Barczyk, A.; Wiaderkiewicz, R.; Pierzchala, W. Eotaxin, but not IL-8, is increased in upper and lower airways of allergic rhinitis subjects after nasal allergen challenge. Allergy Asthma Proc. 2011, 32, 230–238. [Google Scholar] [CrossRef] [PubMed]
- Bartemes, K.R.; Kephart, G.M.; Fox, S.J.; Kita, H. Enhanced innate type 2 immune response in peripheral blood from patients with asthma. J. Allergy Clin. Immunol. 2014, 134, 671–678. [Google Scholar] [CrossRef]
- Sun, R.; Yang, Y.; Huo, Q.; Gu, Z.; Wei, P.; Tang, X. Increased expression of type 2 innate lymphoid cells in pediatric patients with allergic rhinitis. Exp. Ther. Med. 2020, 19, 735–740. [Google Scholar] [CrossRef]
- Testera-Montes, A.; Jurado, R.; Salas, M.; Eguiluz-Gracia, I.; Mayorga, C. Diagnostic Tools in Allergic Rhinitis. Front. Allergy 2021, 2, 721851. [Google Scholar] [CrossRef]
- Hemmings, O.; Kwok, M.; McKendry, R.; Santos, A.F. Basophil Activation Test: Old and New Applications in Allergy. Curr. Allergy Asthma Rep. 2018, 18, 77. [Google Scholar] [CrossRef] [PubMed]
- Abbas, M.; Moussa, M.; Akel, H. Type I Hypersensitivity Reaction; StatPearls: Treasure Island, FL, USA, 2022. [Google Scholar]
- Duarte Ferreira, R.; Ornelas, C.; Silva, S.; Morgado, R.; Pereira, D.; Escaleira, D.; Moreira, S.; Valenca, J.; Pedro, E.; Branco Ferreira, M.; et al. Contribution of In Vivo and In Vitro Testing for The Diagnosis of Local Allergic Rhinitis. J. Investig. Allergol. Clin. Immunol. 2019, 29, 46–48. [Google Scholar] [CrossRef]
- Campo, P.; Villalba, M.; Barrionuevo, E.; Rondon, C.; Salas, M.; Galindo, L.; Rodriguez, M.J.; Lopez-Rodriguez, J.C.; Prieto-Del Prado, M.A.; Torres, M.J.; et al. Immunologic responses to the major allergen of Olea europaea in local and systemic allergic rhinitis subjects. Clin. Exp. Allergy 2015, 45, 1703–1712. [Google Scholar] [CrossRef]
- Eguiluz-Gracia, I.; Fernandez-Santamaria, R.; Testera-Montes, A.; Ariza, A.; Campo, P.; Prieto, A.; Perez-Sanchez, N.; Salas, M.; Mayorga, C.; Torres, M.J.; et al. Coexistence of nasal reactivity to allergens with and without IgE sensitization in patients with allergic rhinitis. Allergy 2020, 75, 1689–1698. [Google Scholar] [CrossRef]
- Yanai, M.; Sato, K.; Aoki, N.; Takiyama, Y.; Oikawa, K.; Kobayashi, H.; Kimura, S.; Harabuchi, Y.; Tateno, M. The role of CCL22/macrophage-derived chemokine in allergic rhinitis. Clin. Immunol. 2007, 125, 291–298. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sun, J.; Wong, B.; Cundall, M.; Goncharova, S.; Conway, M.; Dalrymple, A.; Coyle, A.J.; Waserman, S.; Jordana, M. Immunoreactivity profile of peripheral blood mononuclear cells from patients with ragweed-induced allergic rhinitis. Clin. Exp. Allergy 2007, 37, 901–908. [Google Scholar] [CrossRef]
- Baumann, R.; Rabaszowski, M.; Stenin, I.; Tilgner, L.; Scheckenbach, K.; Wiltfang, J.; Schipper, J.; Chaker, A.; Wagenmann, M. Comparison of the nasal release of IL-4, IL-10, IL-17, CCL13/MCP-4, and CCL26/eotaxin-3 in allergic rhinitis during season and after allergen challenge. Am. J. Rhinol. Allergy 2013, 27, 266–272. [Google Scholar] [CrossRef]
- Wu, G.; Yang, G.; Zhang, R.; Xu, G.; Zhang, L.; Wen, W.; Lu, J.; Liu, J.; Yu, Y. Altered microRNA Expression Profiles of Extracellular Vesicles in Nasal Mucus From Patients With Allergic Rhinitis. Allergy Asthma Immunol. Res. 2015, 7, 449–457. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.H.; Zhang, Y.N.; Liu, Z. MicroRNA in chronic rhinosinusitis and allergic rhinitis. Curr. Allergy Asthma Rep. 2014, 14, 415. [Google Scholar] [CrossRef] [PubMed]
- Hammad, N.M.; Nabil, F.; Elbehedy, E.M.; Sedeek, R.; Gouda, M.I.; Arafa, M.A.; Elalawi, S.M.; El Shahawy, A.A. Role of MicroRNA-155 as a Potential Biomarker for Allergic Rhinitis in Children. Can. Respir. J. 2021, 2021, 5554461. [Google Scholar] [CrossRef]
- Suojalehto, H.; Lindstrom, I.; Majuri, M.L.; Mitts, C.; Karjalainen, J.; Wolff, H.; Alenius, H. Altered microRNA expression of nasal mucosa in long-term asthma and allergic rhinitis. Int. Arch. Allergy Immunol. 2014, 163, 168–178. [Google Scholar] [CrossRef] [PubMed]
- Teng, Y.; Zhang, R.; Liu, C.; Zhou, L.; Wang, H.; Zhuang, W.; Huang, Y.; Hong, Z. miR-143 inhibits interleukin-13-induced inflammatory cytokine and mucus production in nasal epithelial cells from allergic rhinitis patients by targeting IL13Ralpha1. Biochem. Biophys. Res. Commun. 2015, 457, 58–64. [Google Scholar] [CrossRef]
- Stelmaszczyk-Emmel, A.; Zawadzka-Krajewska, A.; Kopatys, A.; Demkow, U. Th1, Th2, Th17, and regulatory cytokines in children with different clinical forms of allergy. Adv. Exp. Med. Biol. 2013, 788, 321–328. [Google Scholar] [CrossRef]
- Lee, M.F.; Song, P.P.; Hwang, G.Y.; Lin, S.J.; Chen, Y.H. Sensitization to Per a 2 of the American cockroach correlates with more clinical severity among airway allergic patients in Taiwan. Ann. Allergy Asthma Immunol. 2012, 108, 243–248. [Google Scholar] [CrossRef]
- Kim, J.A.; Cho, J.H.; Park, I.H.; Shin, J.M.; Lee, S.A.; Lee, H.M. Diesel Exhaust Particles Upregulate Interleukins IL-6 and IL-8 in Nasal Fibroblasts. PLoS ONE 2016, 11, e0157058. [Google Scholar] [CrossRef] [PubMed]
- Yu, X.; Wang, M.; Cao, Z. Reduced CD4(+)T Cell CXCR3 Expression in Patients With Allergic Rhinitis. Front. Immunol. 2020, 11, 581180. [Google Scholar] [CrossRef] [PubMed]
- Kant, A.; Terzioglu, K. Association of severity of allergic rhinitis with neutrophil-to-lymphocyte, eosinophil-to-neutrophil, and eosinophil-to-lymphocyte ratios in adults. Allergol. Immunopathol. 2021, 49, 94–99. [Google Scholar] [CrossRef] [PubMed]
- Doherty, T.A.; Scott, D.; Walford, H.H.; Khorram, N.; Lund, S.; Baum, R.; Chang, J.; Rosenthal, P.; Beppu, A.; Miller, M.; et al. Allergen challenge in allergic rhinitis rapidly induces increased peripheral blood type 2 innate lymphoid cells that express CD84. J. Allergy Clin. Immunol. 2014, 133, 1203–1205. [Google Scholar] [CrossRef] [PubMed]
- Dhariwal, J.; Cameron, A.; Trujillo-Torralbo, M.B.; Del Rosario, A.; Bakhsoliani, E.; Paulsen, M.; Jackson, D.J.; Edwards, M.R.; Rana, B.M.J.; Cousins, D.J.; et al. Mucosal Type 2 Innate Lymphoid Cells Are a Key Component of the Allergic Response to Aeroallergens. Am. J. Respir. Crit. Care Med. 2017, 195, 1586–1596. [Google Scholar] [CrossRef]
- Xu, G.; Zhang, L.; Wang, D.Y.; Xu, R.; Liu, Z.; Han, D.M.; Wang, X.D.; Zuo, K.J.; Li, H.B. Opposing roles of IL-17A and IL-25 in the regulation of TSLP production in human nasal epithelial cells. Allergy 2010, 65, 581–589. [Google Scholar] [CrossRef]
- Asaka, D.; Yoshikawa, M.; Nakayama, T.; Yoshimura, T.; Moriyama, H.; Otori, N. Elevated levels of interleukin-33 in the nasal secretions of patients with allergic rhinitis. Int. Arch. Allergy Immunol. 2012, 158, 47–50. [Google Scholar] [CrossRef]
- Zhu, D.D.; Zhu, X.W.; Jiang, X.D.; Dong, Z. Thymic stromal lymphopoietin expression is increased in nasal epithelial cells of patients with mugwort pollen sensitive-seasonal allergic rhinitis. Chin. Med. J. 2009, 122, 2303–2307. [Google Scholar] [CrossRef]
- Kamekura, R.; Kojima, T.; Takano, K.; Go, M.; Sawada, N.; Himi, T. The role of IL-33 and its receptor ST2 in human nasal epithelium with allergic rhinitis. Clin. Exp. Allergy 2012, 42, 218–228. [Google Scholar] [CrossRef]
- Kamekura, R.; Kojima, T.; Koizumi, J.; Ogasawara, N.; Kurose, M.; Go, M.; Harimaya, A.; Murata, M.; Tanaka, S.; Chiba, H.; et al. Thymic stromal lymphopoietin enhances tight-junction barrier function of human nasal epithelial cells. Cell Tissue Res. 2009, 338, 283–293. [Google Scholar] [CrossRef]
- Busse, W.W.; Maspero, J.F.; Lu, Y.; Corren, J.; Hanania, N.A.; Chipps, B.E.; Katelaris, C.H.; FitzGerald, J.M.; Quirce, S.; Ford, L.B.; et al. Efficacy of dupilumab on clinical outcomes in patients with asthma and perennial allergic rhinitis. Ann. Allergy Asthma Immunol. 2020, 125, 565–576. [Google Scholar] [CrossRef]
- Yu, C.; Wang, K.; Cui, X.; Lu, L.; Dong, J.; Wang, M.; Gao, X. Clinical Efficacy and Safety of Omalizumab in the Treatment of Allergic Rhinitis: A Systematic Review and Meta-analysis of Randomized Clinical Trials. Am. J. Rhinol. Allergy 2020, 34, 196–208. [Google Scholar] [CrossRef] [PubMed]
- Tsabouri, S.; Ntritsos, G.; Koskeridis, F.; Evangelou, E.; Olsson, P.; Kostikas, K. Omalizumab for the treatment of allergic rhinitis: A systematic review and meta-analysis. Rhinology 2021, 59, 501–510. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, S.F.; Katial, R.; Jayawardena, S.; Pirozzi, G.; Staudinger, H.; Eckert, L.; Joish, V.N.; Amin, N.; Maroni, J.; Rowe, P.; et al. Efficacy and safety of dupilumab in perennial allergic rhinitis and comorbid asthma. J. Allergy Clin. Immunol. 2018, 142, 171–177. [Google Scholar] [CrossRef]
- Juel-Berg, N.; Darling, P.; Bolvig, J.; Foss-Skiftesvik, M.H.; Halken, S.; Winther, L.; Hansen, K.S.; Askjaer, N.; Heegaard, S.; Madsen, A.R.; et al. Intranasal corticosteroids compared with oral antihistamines in allergic rhinitis: A systematic review and meta-analysis. Am. J. Rhinol. Allergy 2017, 31, 19–28. [Google Scholar] [CrossRef] [PubMed]
- Bousquet, J.; Schunemann, H.J.; Togias, A.; Bachert, C.; Erhola, M.; Hellings, P.W.; Klimek, L.; Pfaar, O.; Wallace, D.; Ansotegui, I.; et al. Next-generation Allergic Rhinitis and Its Impact on Asthma (ARIA) guidelines for allergic rhinitis based on Grading of Recommendations Assessment, Development and Evaluation (GRADE) and real-world evidence. J. Allergy Clin. Immunol. 2020, 145, 70–80. [Google Scholar] [CrossRef] [PubMed]
- Fein, M.N.; Fischer, D.A.; O’Keefe, A.W.; Sussman, G.L. CSACI position statement: Newer generation H1-antihistamines are safer than first-generation H1-antihistamines and should be the first-line antihistamines for the treatment of allergic rhinitis and urticaria. Allergy Asthma Clin. Immunol. 2019, 15, 61. [Google Scholar] [CrossRef]
- Church, M.K.; Maurer, M.; Simons, F.E.; Bindslev-Jensen, C.; van Cauwenberge, P.; Bousquet, J.; Holgate, S.T.; Zuberbier, T.; Global, A.; Asthma European, N. Risk of first-generation H(1)-antihistamines: A GA(2)LEN position paper. Allergy 2010, 65, 459–466. [Google Scholar] [CrossRef]
- Sanchez-Borges, M.; Ansotegui, I.J. Second generation antihistamines: An update. Curr. Opin. Allergy Clin. Immunol. 2019, 19, 358–364. [Google Scholar] [CrossRef]
- Feng, S.; Deng, C.; Li, L.; Liao, W.; Fan, Y.; Xu, G.; Li, H. Efficacy of intranasal antihistamine in the treatment of allergic rhinitis: A meta-analysis. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2014, 49, 832–838. [Google Scholar]
- LaForce, C.F.; Corren, J.; Wheeler, W.J.; Berger, W.E.; Rhinitis Study, G. Efficacy of azelastine nasal spray in seasonal allergic rhinitis patients who remain symptomatic after treatment with fexofenadine. Ann. Allergy Asthma Immunol. 2004, 93, 154–159. [Google Scholar] [CrossRef]
- Kaliner, M.A.; Berger, W.E.; Ratner, P.H.; Siegel, C.J. The efficacy of intranasal antihistamines in the treatment of allergic rhinitis. Ann. Allergy Asthma Immunol. 2011, 106, 6–11. [Google Scholar] [CrossRef]
- Horak, F.; Zieglmayer, U.P.; Zieglmayer, R.; Kavina, A.; Marschall, K.; Munzel, U.; Petzold, U. Azelastine nasal spray and desloratadine tablets in pollen-induced seasonal allergic rhinitis: A pharmacodynamic study of onset of action and efficacy. Curr. Med. Res. Opin. 2006, 22, 151–157. [Google Scholar] [CrossRef]
- Shah, S.R.; Nayak, A.; Ratner, P.; Roland, P.; Michael Wall, G. Effects of olopatadine hydrochloride nasal spray 0.6% in the treatment of seasonal allergic rhinitis: A phase III, multicenter, randomized, double-blind, active- and placebo-controlled study in adolescents and adults. Clin. Ther. 2009, 31, 99–107. [Google Scholar] [CrossRef] [PubMed]
- Sastre, J.; Mosges, R. Local and systemic safety of intranasal corticosteroids. J. Investig. Allergol. Clin. Immunol. 2012, 22, 1–12. [Google Scholar] [PubMed]
- Bensch, G.W. Safety of intranasal corticosteroids. Ann. Allergy Asthma Immunol. 2016, 117, 601–605. [Google Scholar] [CrossRef] [PubMed]
- Kirtsreesakul, V.; Chansaksung, P.; Ruttanaphol, S. Dose-related effect of intranasal corticosteroids on treatment outcome of persistent allergic rhinitis. Otolaryngol. Head Neck Surg. 2008, 139, 565–569. [Google Scholar] [CrossRef] [PubMed]
- Zhang, K.; Li, A.R.; Miglani, A.; Nguyen, S.A.; Schlosser, R.J. Effect of Medical Therapy in Allergic Rhinitis: A Systematic Review and Meta-Analysis. Am. J. Rhinol. Allergy 2022, 36, 269–280. [Google Scholar] [CrossRef]
- Joseph, R.M.; Hunter, A.L.; Ray, D.W.; Dixon, W.G. Systemic glucocorticoid therapy and adrenal insufficiency in adults: A systematic review. Semin. Arthritis Rheum. 2016, 46, 133–141. [Google Scholar] [CrossRef]
- Hox, V.; Lourijsen, E.; Jordens, A.; Aasbjerg, K.; Agache, I.; Alobid, I.; Bachert, C.; Boussery, K.; Campo, P.; Fokkens, W.; et al. Benefits and harm of systemic steroids for short- and long-term use in rhinitis and rhinosinusitis: An EAACI position paper. Clin. Transl. Allergy 2020, 10, 1–27. [Google Scholar] [CrossRef]
- Bousquet, J.; Meltzer, E.O.; Couroux, P.; Koltun, A.; Kopietz, F.; Munzel, U.; Kuhl, H.C.; Nguyen, D.T.; Salapatek, A.M.; Price, D. Onset of Action of the Fixed Combination Intranasal Azelastine-Fluticasone Propionate in an Allergen Exposure Chamber. J. Allergy Clin. Immunol. Pract. 2018, 6, 1726–1732. [Google Scholar] [CrossRef]
- Price, D.; Shah, S.; Bhatia, S.; Bachert, C.; Berger, W.; Bousquet, J.; Carr, W.; Hellings, P.; Munzel, U.; Scadding, G.; et al. A new therapy (MP29-02) is effective for the long-term treatment of chronic rhinitis. J. Investig. Allergol. Clin. Immunol. 2013, 23, 495–503. [Google Scholar]
- Carr, W.; Bernstein, J.; Lieberman, P.; Meltzer, E.; Bachert, C.; Price, D.; Munzel, U.; Bousquet, J. A novel intranasal therapy of azelastine with fluticasone for the treatment of allergic rhinitis. J. Allergy Clin. Immunol. 2012, 129, 1282–1289. [Google Scholar] [CrossRef] [PubMed]
- Meltzer, E.O.; Bachert, C.; Mayer, M.J.; Kopietz, F.; Koltun, A.; Maus, J.; D’Addio, A.D. Deposition characteristics of a novel intranasal formulation of azelastine hydrochloride plus fluticasone propionate in an anatomic model of the human nasal cavity. Allergy Asthma Proc. 2020, 41, 265–270. [Google Scholar] [CrossRef] [PubMed]
- Hossenbaccus, L.; Linton, S.; Garvey, S.; Ellis, A.K. Towards definitive management of allergic rhinitis: Best use of new and established therapies. Allergy Asthma Clin. Immunol. 2020, 16, 39. [Google Scholar] [CrossRef]
- Wilson, A.M.; O’Byrne, P.M.; Parameswaran, K. Leukotriene receptor antagonists for allergic rhinitis: A systematic review and meta-analysis. Am. J. Med. 2004, 116, 338–344. [Google Scholar] [CrossRef] [PubMed]
- Rodrigo, G.J.; Yanez, A. The role of antileukotriene therapy in seasonal allergic rhinitis: A systematic review of randomized trials. Ann. Allergy Asthma Immunol. 2006, 96, 779–786. [Google Scholar] [CrossRef] [PubMed]
- Bousquet, J.; Anto, J.M.; Bachert, C.; Baiardini, I.; Bosnic-Anticevich, S.; Walter Canonica, G.; Melen, E.; Palomares, O.; Scadding, G.K.; Togias, A.; et al. Allergic rhinitis. Nat. Rev. Dis. Prim. 2020, 6, 95. [Google Scholar] [CrossRef]
- Saco, T.; Ugalde, I.C.; Cardet, J.C.; Casale, T.B. Strategies for choosing a biologic for your patient with allergy or asthma. Ann. Allergy Asthma Immunol. 2021, 127, 627–637. [Google Scholar] [CrossRef]
- Geng, B.; Dilley, M.; Anterasian, C. Biologic Therapies for Allergic Rhinitis and Nasal Polyposis. Curr. Allergy Asthma Rep. 2021, 21, 36. [Google Scholar] [CrossRef]
- Casale, T.B.; Condemi, J.; LaForce, C.; Nayak, A.; Rowe, M.; Watrous, M.; McAlary, M.; Fowler-Taylor, A.; Racine, A.; Gupta, N.; et al. Effect of omalizumab on symptoms of seasonal allergic rhinitis: A randomized controlled trial. JAMA 2001, 286, 2956–2967. [Google Scholar] [CrossRef]
- Pelaia, C.; Calabrese, C.; Terracciano, R.; de Blasio, F.; Vatrella, A.; Pelaia, G. Omalizumab, the first available antibody for biological treatment of severe asthma: More than a decade of real-life effectiveness. Ther. Adv. Respir. Dis. 2018, 12, 1753466618810192. [Google Scholar] [CrossRef]
- Bousquet, J.; Humbert, M.; Gibson, P.G.; Kostikas, K.; Jaumont, X.; Pfister, P.; Nissen, F. Real-World Effectiveness of Omalizumab in Severe Allergic Asthma: A Meta-Analysis of Observational Studies. J. Allergy Clin. Immunol. Pract. 2021, 9, 2702–2714. [Google Scholar] [CrossRef] [PubMed]
- Zhu, R.; Zheng, Y.; Putnam, W.S.; Visich, J.; Eisner, M.D.; Matthews, J.G.; Rosen, K.E.; D’Argenio, D.Z. Population-based efficacy modeling of omalizumab in patients with severe allergic asthma inadequately controlled with standard therapy. AAPS J. 2013, 15, 559–570. [Google Scholar] [CrossRef] [PubMed]
- Casale, T.B.; Luskin, A.T.; Busse, W.; Zeiger, R.S.; Trzaskoma, B.; Yang, M.; Griffin, N.M.; Chipps, B.E. Omalizumab Effectiveness by Biomarker Status in Patients with Asthma: Evidence From PROSPERO, A Prospective Real-World Study. J. Allergy Clin. Immunol. Pract. 2019, 7, 156–164. [Google Scholar] [CrossRef]
- Fala, L. Nucala (Mepolizumab): First IL-5 Antagonist Monoclonal Antibody FDA Approved for Maintenance Treatment of Patients with Severe Asthma. Am. Health Drug Benefits 2016, 9, 106–110. [Google Scholar] [PubMed]
- Ortega, H.G.; Liu, M.C.; Pavord, I.D.; Brusselle, G.G.; FitzGerald, J.M.; Chetta, A.; Humbert, M.; Katz, L.E.; Keene, O.N.; Yancey, S.W.; et al. Mepolizumab treatment in patients with severe eosinophilic asthma. N. Engl. J. Med. 2014, 371, 1198–1207. [Google Scholar] [CrossRef]
- Khurana, S.; Brusselle, G.G.; Bel, E.H.; FitzGerald, J.M.; Masoli, M.; Korn, S.; Kato, M.; Albers, F.C.; Bradford, E.S.; Gilson, M.J.; et al. Long-term Safety and Clinical Benefit of Mepolizumab in Patients With the Most Severe Eosinophilic Asthma: The COSMEX Study. Clin. Ther. 2019, 41, 2041–2056. [Google Scholar] [CrossRef]
- Lugogo, N.; Domingo, C.; Chanez, P.; Leigh, R.; Gilson, M.J.; Price, R.G.; Yancey, S.W.; Ortega, H.G. Long-term Efficacy and Safety of Mepolizumab in Patients With Severe Eosinophilic Asthma: A Multi-center, Open-label, Phase IIIb Study. Clin. Ther. 2016, 38, 2058–2070. [Google Scholar] [CrossRef]
- Bel, E.H.; Wenzel, S.E.; Thompson, P.J.; Prazma, C.M.; Keene, O.N.; Yancey, S.W.; Ortega, H.G.; Pavord, I.D.; Investigators, S. Oral glucocorticoid-sparing effect of mepolizumab in eosinophilic asthma. N. Engl. J. Med. 2014, 371, 1189–1197. [Google Scholar] [CrossRef] [PubMed]
- Markham, A. Reslizumab: First Global Approval. Drugs 2016, 76, 907–911. [Google Scholar] [CrossRef]
- Mukherjee, M.; Aleman Paramo, F.; Kjarsgaard, M.; Salter, B.; Nair, G.; LaVigne, N.; Radford, K.; Sehmi, R.; Nair, P. Weight-adjusted Intravenous Reslizumab in Severe Asthma with Inadequate Response to Fixed-Dose Subcutaneous Mepolizumab. Am. J. Respir. Crit. Care Med. 2018, 197, 38–46. [Google Scholar] [CrossRef]
- Corren, J.; Weinstein, S.; Janka, L.; Zangrilli, J.; Garin, M. Phase 3 Study of Reslizumab in Patients With Poorly Controlled Asthma: Effects Across a Broad Range of Eosinophil Counts. Chest 2016, 150, 799–810. [Google Scholar] [CrossRef] [PubMed]
- Markham, A. Benralizumab: First Global Approval. Drugs 2018, 78, 505–511. [Google Scholar] [CrossRef]
- FitzGerald, J.M.; Bleecker, E.R.; Nair, P.; Korn, S.; Ohta, K.; Lommatzsch, M.; Ferguson, G.T.; Busse, W.W.; Barker, P.; Sproule, S.; et al. Benralizumab, an anti-interleukin-5 receptor alpha monoclonal antibody, as add-on treatment for patients with severe, uncontrolled, eosinophilic asthma (CALIMA): A randomised, double-blind, placebo-controlled phase 3 trial. Lancet 2016, 388, 2128–2141. [Google Scholar] [CrossRef] [PubMed]
- Bleecker, E.R.; FitzGerald, J.M.; Chanez, P.; Papi, A.; Weinstein, S.F.; Barker, P.; Sproule, S.; Gilmartin, G.; Aurivillius, M.; Werkstrom, V.; et al. Efficacy and safety of benralizumab for patients with severe asthma uncontrolled with high-dosage inhaled corticosteroids and long-acting beta2-agonists (SIROCCO): A randomised, multicentre, placebo-controlled phase 3 trial. Lancet 2016, 388, 2115–2127. [Google Scholar] [CrossRef] [PubMed]
- Cheraghlou, S.; Cohen, J.M. Early Adoption of Dupilumab in the Medicare Population in 2017. Yale J. Biol. Med. 2020, 93, 675–677. [Google Scholar] [PubMed]
- Eschenbacher, W.; Straesser, M.; Knoeddler, A.; Li, R.C.; Borish, L. Biologics for the Treatment of Allergic Rhinitis, Chronic Rhinosinusitis, and Nasal Polyposis. Immunol. Allergy Clin. N. Am. 2020, 40, 539–547. [Google Scholar] [CrossRef]
- Berger, P.; Menzies-Gow, A.; Peters, A.T.; Kuna, P.; Rabe, K.F.; Altincatal, A.; Soler, X.; Pandit-Abid, N.; Siddiqui, S.; Jacob-Nara, J.A.; et al. Long-term efficacy of dupilumab in asthma with and without chronic rhinosinusitis and/or nasal polyps. Ann. Allergy Asthma Immunol. 2022, S1081-1206(22)01912-3. [Google Scholar] [CrossRef]
- Castro, M.; Corren, J.; Pavord, I.D.; Maspero, J.; Wenzel, S.; Rabe, K.F.; Busse, W.W.; Ford, L.; Sher, L.; FitzGerald, J.M.; et al. Dupilumab Efficacy and Safety in Moderate-to-Severe Uncontrolled Asthma. N. Engl. J. Med. 2018, 378, 2486–2496. [Google Scholar] [CrossRef]
- Rabe, K.F.; Nair, P.; Brusselle, G.; Maspero, J.F.; Castro, M.; Sher, L.; Zhu, H.; Hamilton, J.D.; Swanson, B.N.; Khan, A.; et al. Efficacy and Safety of Dupilumab in Glucocorticoid-Dependent Severe Asthma. N. Engl. J. Med. 2018, 378, 2475–2485. [Google Scholar] [CrossRef]
- Kychygina, A.; Cassagne, M.; Tauber, M.; Galiacy, S.; Paul, C.; Fournie, P.; Simon, M. Dupilumab-Associated Adverse Events During Treatment of Allergic Diseases. Clin. Rev. Allergy Immunol. 2022, 62, 519–533. [Google Scholar] [CrossRef] [PubMed]
- Wenzel, S.; Castro, M.; Corren, J.; Maspero, J.; Wang, L.; Zhang, B.; Pirozzi, G.; Sutherland, E.R.; Evans, R.R.; Joish, V.N.; et al. Dupilumab efficacy and safety in adults with uncontrolled persistent asthma despite use of medium-to-high-dose inhaled corticosteroids plus a long-acting beta2 agonist: A randomised double-blind placebo-controlled pivotal phase 2b dose-ranging trial. Lancet 2016, 388, 31–44. [Google Scholar] [CrossRef]
- Hoy, S.M. Tezepelumab: First Approval. Drugs 2022, 82, 461–468. [Google Scholar] [CrossRef] [PubMed]
- Menzies-Gow, A.; Corren, J.; Bourdin, A.; Chupp, G.; Israel, E.; Wechsler, M.E.; Brightling, C.E.; Griffiths, J.M.; Hellqvist, A.; Bowen, K.; et al. Tezepelumab in Adults and Adolescents with Severe, Uncontrolled Asthma. N. Engl. J. Med. 2021, 384, 1800–1809. [Google Scholar] [CrossRef] [PubMed]
- Kelsen, S.G.; Agache, I.O.; Soong, W.; Israel, E.; Chupp, G.L.; Cheung, D.S.; Theess, W.; Yang, X.; Staton, T.L.; Choy, D.F.; et al. Astegolimab (anti-ST2) efficacy and safety in adults with severe asthma: A randomized clinical trial. J. Allergy Clin. Immunol. 2021, 148, 790–798. [Google Scholar] [CrossRef]
- Penagos, M.; Durham, S.R. Allergen immunotherapy for long-term tolerance and prevention. J. Allergy Clin. Immunol. 2022, 149, 802–811. [Google Scholar] [CrossRef] [PubMed]
- Cox, L.S.; Murphey, A.; Hankin, C. The Cost-Effectiveness of Allergen Immunotherapy Compared with Pharmacotherapy for Treatment of Allergic Rhinitis and Asthma. Immunol. Allergy Clin. N. Am. 2020, 40, 69–85. [Google Scholar] [CrossRef]
- Akkoc, T.; Genc, D. Asthma immunotherapy and treatment approaches with mesenchymal stem cells. Immunotherapy 2020, 12, 665–674. [Google Scholar] [CrossRef] [PubMed]
- Gans, M.D.; Gavrilova, T. Understanding the immunology of asthma: Pathophysiology, biomarkers, and treatments for asthma endotypes. Paediatr. Respir. Rev. 2020, 36, 118–127. [Google Scholar] [CrossRef]
- Rondón, C.; Campo, P.; López-Blanca, N.; Torres, M.J.; Blanca, M. Local Allergic Rhinitis: Is There a Role for Systemic Allergy Immunotherapy? Curr. Treat. Options Allergy 2015, 2, 54–63. [Google Scholar] [CrossRef][Green Version]
- Kouzegaran, S.; Zamani, M.A.; Faridhosseini, R.; Rafatpanah, H.; Rezaee, A.; Yousefzadeh, H.; Movahed, R.; Azad, F.J.; Tehrani, H. Immunotherapy in Allergic Rhinitis: It’s Effect on the Immune System and Clinical Symptoms. Open Access Maced. J. Med. Sci. 2018, 6, 1248–1252. [Google Scholar] [CrossRef]
- Hoshino, M.; Akitsu, K.; Kubota, K.; Ohtawa, J. Efficacy of a house dust mite sublingual immunotherapy tablet as add-on dupilumab in asthma with rhinitis. Allergol. Int. 2022, 71, 490–497. [Google Scholar] [CrossRef] [PubMed]
- Fritzsching, B.; Contoli, M.; Porsbjerg, C.; Buchs, S.; Larsen, J.R.; Elliott, L.; Rodriguez, M.R.; Freemantle, N. Long-term real-world effectiveness of allergy immunotherapy in patients with allergic rhinitis and asthma: Results from the REACT study, a retrospective cohort study. Lancet Reg. Health Eur. 2022, 13, 100275. [Google Scholar] [CrossRef]
- Roberts, G.; Pfaar, O.; Akdis, C.A.; Ansotegui, I.J.; Durham, S.R.; Gerth van Wijk, R.; Halken, S.; Larenas-Linnemann, D.; Pawankar, R.; Pitsios, C.; et al. EAACI Guidelines on Allergen Immunotherapy: Allergic rhinoconjunctivitis. Allergy 2018, 73, 765–798. [Google Scholar] [CrossRef] [PubMed]
- Valenta, R.; Campana, R.; Focke-Tejkl, M.; Niederberger, V. Vaccine development for allergen-specific immunotherapy based on recombinant allergens and synthetic allergen peptides: Lessons from the past and novel mechanisms of action for the future. J. Allergy Clin. Immunol. 2016, 137, 351–357. [Google Scholar] [CrossRef]
- Rondon, C.; Blanca-Lopez, N.; Aranda, A.; Herrera, R.; Rodriguez-Bada, J.L.; Canto, G.; Mayorga, C.; Torres, M.J.; Campo, P.; Blanca, M. Local allergic rhinitis: Allergen tolerance and immunologic changes after preseasonal immunotherapy with grass pollen. J. Allergy Clin. Immunol. 2011, 127, 1069–1071. [Google Scholar] [CrossRef] [PubMed]
- Klimek, L.; Fox, G.C.; Thum-Oltmer, S. SCIT with a high-dose house dust mite allergoid is well tolerated: Safety data from pooled clinical trials and more than 10 years of daily practice analyzed in different subgroups. Allergo J. Int. 2018, 27, 131–139. [Google Scholar] [CrossRef] [PubMed]
- Shamji, M.H.; Ceuppens, J.; Bachert, C.; Hellings, P.; Placier, G.; Thirion, G.; Bovy, N.; Durham, S.R.; Duchateau, J.; Legon, T.; et al. Lolium perenne peptides for treatment of grass pollen allergy: A randomized, double-blind, placebo-controlled clinical trial. J. Allergy Clin. Immunol. 2018, 141, 448–451. [Google Scholar] [CrossRef]
- Epstein, T.G.; Liss, G.M.; Murphy-Berendts, K.; Bernstein, D.I. Risk factors for fatal and nonfatal reactions to subcutaneous immunotherapy: National surveillance study on allergen immunotherapy (2008-2013). Ann. Allergy Asthma Immunol. 2016, 116, 354–359. [Google Scholar] [CrossRef]
- Unal, D. Effects of Perennial Allergen Immunotherapy in Allergic Rhinitis in Patients with/without Asthma: A-Randomized Controlled Real-Life Study. Int. Arch. Allergy Immunol. 2020, 181, 141–148. [Google Scholar] [CrossRef]
- Rondon, C.; Blanca-Lopez, N.; Campo, P.; Mayorga, C.; Jurado-Escobar, R.; Torres, M.J.; Canto, G.; Blanca, M. Specific immunotherapy in local allergic rhinitis: A randomized, double-blind placebo-controlled trial with Phleum pratense subcutaneous allergen immunotherapy. Allergy 2018, 73, 905–915. [Google Scholar] [CrossRef]
- Calderon, M.A.; Simons, F.E.; Malling, H.J.; Lockey, R.F.; Moingeon, P.; Demoly, P. Sublingual allergen immunotherapy: Mode of action and its relationship with the safety profile. Allergy 2012, 67, 302–311. [Google Scholar] [CrossRef]
- Pfaar, O.; Lou, H.; Zhang, Y.; Klimek, L.; Zhang, L. Recent developments and highlights in allergen immunotherapy. Allergy 2018, 73, 2274–2289. [Google Scholar] [CrossRef] [PubMed]
- Virchow, J.C.; Backer, V.; Kuna, P.; Prieto, L.; Nolte, H.; Villesen, H.H.; Ljorring, C.; Riis, B.; de Blay, F. Efficacy of a House Dust Mite Sublingual Allergen Immunotherapy Tablet in Adults With Allergic Asthma: A Randomized Clinical Trial. JAMA 2016, 315, 1715–1725. [Google Scholar] [CrossRef]
- Valovirta, E.; Petersen, T.H.; Piotrowska, T.; Laursen, M.K.; Andersen, J.S.; Sorensen, H.F.; Klink, R.; GAP Investigators. Results from the 5-year SQ grass sublingual immunotherapy tablet asthma prevention (GAP) trial in children with grass pollen allergy. J. Allergy Clin. Immunol. 2018, 141, 529–538. [Google Scholar] [CrossRef]
- Elliott, J.; Kelly, S.E.; Johnston, A.; Skidmore, B.; Gomes, T.; Wells, G.A. Allergen immunotherapy for the treatment of allergic rhinitis and/or asthma: An umbrella review. CMAJ Open 2017, 5, 373–385. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.Y.; Jang, M.J.; Kim, D.Y.; Park, S.W.; Han, D.H. Efficacy of Subcutaneous and Sublingual Immunotherapy for House Dust Mite Allergy: A Network Meta-Analysis-Based Comparison. J. Allergy Clin. Immunol. Pract. 2021, 9, 4450–4458. [Google Scholar] [CrossRef] [PubMed]
- Konradsen, J.R.; Grundstrom, J.; Hellkvist, L.; Tran, T.A.T.; Andersson, N.; Gafvelin, G.; Kiewiet, M.B.G.; Hamsten, C.; Tang, J.; Parkin, R.V.; et al. Intralymphatic immunotherapy in pollen-allergic young adults with rhinoconjunctivitis and mild asthma: A randomized trial. J. Allergy Clin. Immunol. 2020, 145, 1005–1007. [Google Scholar] [CrossRef] [PubMed]
- Werner, M.T.; Bosso, J.V. Intralymphatic immunotherapy for allergic rhinitis: A systematic review and meta-analysis. Allergy Asthma Proc. 2021, 42, 283–292. [Google Scholar] [CrossRef]
- Skaarup, S.H.; Schmid, J.M.; Skjold, T.; Graumann, O.; Hoffmann, H.J. Intralymphatic immunotherapy improves grass pollen allergic rhinoconjunctivitis: A 3-year randomized placebo-controlled trial. J. Allergy Clin. Immunol. 2021, 147, 1011–1019. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Espada-Sánchez, M.; Sáenz de Santa María, R.; Martín-Astorga, M.d.C.; Lebrón-Martín, C.; Delgado, M.J.; Eguiluz-Gracia, I.; Rondón, C.; Mayorga, C.; Torres, M.J.; Aranda, C.J.; et al. Diagnosis and Treatment in Asthma and Allergic Rhinitis: Past, Present, and Future. Appl. Sci. 2023, 13, 1273. https://doi.org/10.3390/app13031273
Espada-Sánchez M, Sáenz de Santa María R, Martín-Astorga MdC, Lebrón-Martín C, Delgado MJ, Eguiluz-Gracia I, Rondón C, Mayorga C, Torres MJ, Aranda CJ, et al. Diagnosis and Treatment in Asthma and Allergic Rhinitis: Past, Present, and Future. Applied Sciences. 2023; 13(3):1273. https://doi.org/10.3390/app13031273
Chicago/Turabian StyleEspada-Sánchez, Marta, Rocío Sáenz de Santa María, María del Carmen Martín-Astorga, Clara Lebrón-Martín, María Jesús Delgado, Ibón Eguiluz-Gracia, Carmen Rondón, Cristobalina Mayorga, María José Torres, Carlos José Aranda, and et al. 2023. "Diagnosis and Treatment in Asthma and Allergic Rhinitis: Past, Present, and Future" Applied Sciences 13, no. 3: 1273. https://doi.org/10.3390/app13031273
APA StyleEspada-Sánchez, M., Sáenz de Santa María, R., Martín-Astorga, M. d. C., Lebrón-Martín, C., Delgado, M. J., Eguiluz-Gracia, I., Rondón, C., Mayorga, C., Torres, M. J., Aranda, C. J., & Cañas, J. A. (2023). Diagnosis and Treatment in Asthma and Allergic Rhinitis: Past, Present, and Future. Applied Sciences, 13(3), 1273. https://doi.org/10.3390/app13031273







