Abstract
Urinary incontinence affects approximately 200 million people worldwide. The objective of this study was to investigate the effect of pelvic floor muscle (PFM) training with biofeedback (BF) in women with urinary incontinence in comparison to PFM training alone. The primary outcome was PFM strength with secondary outcomes being the severity of incontinence, other PFM parameters, quality of life (QoL), social life, satisfaction and adherence to treatment. Randomized controlled trials (RCTs) published from 2005 to 2023 in PubMed, MEDLINE, Scopus and Google Scholar were searched and evaluated with the PEDro scale. Nine moderate and two high methodological quality RCTs were selected. There was a statistically significant improvement in all parameters. In five studies, muscle strength and the severity of incontinence were statistically better in the BF group compared to the non-BF group. In most studies, no differences were found for QoL and social life between the groups. For adherence to treatment, the results were ambiguous. Τhe remaining variables (endurance, precontraction, function, adherence and satisfaction) had few studies to support the results. There was moderate level evidence that the group utilizing PFM exercises with BF showed significant improvements in the management of urinary incontinence. Concerning muscle strength and the severity of incontinence, findings were inconclusive, as only in some studies the results were statistically better in the BF group compared to the non-BF group.
1. Introduction
Urinary incontinence is a condition which is characterized as the involuntary loss of urine and affects over 200 million people worldwide [1,2]. Even though it can be found in both genders, it has twice as much prevalence in women than in men [3,4]. It affects the muscular and urinary systems as well as quality of life (QoL), including social and sexual life [5,6]. Most patients prefer to seek conservative treatment, whereas fewer may prioritize surgery [7]. One of the conservative methods widely used is pelvic floor muscle (PFM) exercises, which have long been identified as the first line of treatment for urinary incontinence [8]. This has been supported by several studies, which have found that PFM exercises have a significant positive effect in women suffering from urinary incontinence [9,10,11].
Biofeedback (BF) is regularly used as an adjunct to rehabilitation programs used for urinary incontinence [12]. The role of BF is to convert biological signals into comprehensible visual, auditory and/or vibratory ones. Direct information about the condition of the PFMs is provided, permitting patients to “see inside their body” [13,14,15]. Biofeedback devices educate women on how to correctly contract their muscles during the exercise [13,14]. Indeed, researchers of experimental studies [16,17,18,19,20] found improvements in symptoms in women with urinary incontinence after PFM exercises with BF, whereas according to the results of one systematic review [21], PFM exercises with BF were not superior to alternative interventions, such as no training, PFM exercises alone or vaginal electrostimulation.
However, these studies are restricted to women with stress urinary incontinence (SUI) and, as a result, these conclusions cannot be generalized to other types of urinary incontinence (such as urge or mixed urinary incontinence). Furthermore, in Nunes et al.’s (2018) systematic review [21], not all of the included studies compared PFM exercises with BF to PFM exercise without BF, as some group interventions consisted of electrical stimulation, kinesthetic training, etc., while other comparative groups included no training at all. Thus, it is not clear whether PFM exercises with BF are better than isolated PFM exercises (without BF). In addition, outcomes such as the endurance and functionality of the pelvic floor muscles, satisfaction and commitment to the treatment have not been explored [21]. No other systematic review was found that clearly investigated, according to the above, the effectiveness of PFM exercises in combination with BF training for the treatment of urinary incontinence across women. Thus, this area merits further research.
Given the above, urinary incontinence is a condition that negatively affects the muscular and urinary systems as well as the QoL of a large number of women. According to this, we conducted a systematic review investigating the effects of PFM exercises with biofeedback in women with urinary incontinence (stress, mixed and urge) in PFM strength and other muscular variables, QoL and other clinical and functional parameters compared to PFM exercises alone (without BF).
2. Materials and Methods
2.1. Study Design
This is a systematic review consisting of randomized controlled trials (RCTs) evaluating the effects of PFM exercises with BF in women with urinary incontinence compared to PFM exercises alone (without BF). PRISMA (preferred reporting items for systematic reviews and meta-analyses) instructions were followed for the study [22].
2.2. Search Strategy
The databases that were used for the initial search were PubMed, MEDLINE, Scopus and Google Scholar with the use of specific key words, including «urinary incontinence», «stress incontinence», «urge incontinence», «mixed incontinence», «woman», «women», «pelvic floor muscle exercise», «pelvic floor exercises», «pelvic floor muscle training», «Kegel exercise», «biofeedback», «biofeedback training», «muscle strength», «muscle contraction», «pad test», «quality of life», «social interaction», «patients satisfaction», «personal satisfaction», «symptoms severity», «incontinence severity» and «adherence». The key word combinations are shown in Table 1. Randomized controlled studies, published from January 2005 to July 2023, were searched. Furthermore, citations from previous relevant studies were crosschecked and examined for additional related studies.

Table 1.
Key words for search strategy.
2.3. Inclusion and Exclusion Criteria
Specific inclusion and exclusion criteria were set by two independent researchers who agreed in the selection of the studies.
The inclusion criteria were:
- RCTs published in English and in full text;
- The sample of the studies had to include women over 18 years old;
- Women had to have stress urinary incontinence (SUI) or urge urinary incontinence (UUI) or mixed incontinence (MUI) of any severity;
- PFM exercises combined with BF were part of the therapeutic intervention for at least one (experimental) group and were compared with a control group, which followed PFM exercises alone (without BF).
The exclusion criteria were:
- Studies including men;
- Women who in the past had undergone surgery for their incontinence problem;
- The control group followed a placebo or no intervention or any other kind of ‘passive’ intervention (such as booklets and guides);
- PFM exercises with the combination of BF were part of the intervention in both the experimental and control groups.
2.4. Methodological Quality
The methodological quality of the articles was evaluated with the PEDro scale, which is widely used for the evaluation of RCTs and is characterized as a valid and reliable tool [23]. This scale consists of 11 criteria (10 of which are scored). For each criterion, if it was met by the study, a score of 1 was given, and if it the criterion was not met, the article was scored with 0. Scores could range from 0 to 10. Scores between 0 and 3 were characterized as poor in quality, scores between 4 and 6 as moderate and scores between 7 and 10 as high-quality studies. Each study was evaluated independently by two researchers (AEM and EB) and the results were compared. In cases of disagreement, a third assessor (SL) would be involved to solve the disagreement.
2.5. Participants
The included RCTs consisted of adult women who had SUI, UUI or MUI of any severity (mild, moderate or severe) in order to not restrict the generalization of the results. The exclusion criteria involved women with underlying conditions, such as neurological or psychiatric diseases, urinary tract infections, malignancy, etc., which could interfere with the intervention.
2.6. Intervention
The therapeutic intervention consisted of at least one group following PFM exercises combined with BF, whereas the comparative group followed PFM exercises alone (without BF). RCTs involving all types of BF and PFM exercises of any duration, frequency, etc., were all included in the systematic review.
2.7. Outcome Measures
The primary outcome was the PFM strength. Secondary outcomes were the severity of incontinence, other muscular parameters, such as endurance, PFM functionality, QoL, social life, adherence and satisfaction from the intervention. All evaluation tools assessing the aforementioned parameters were considered as acceptable so as not to restrict any RCTs from the systematic review.
3. Results
3.1. Search and Selection
After the initial search, 862 articles published from January 2005 to July 2023 were retrieved. Following the removal of non-RCTs and duplicates, 125 RCTs were selected. From these, 67 RCTs were excluded after a title screening, 26 after an abstract screening and 21 after a full-text screening. Finally, 11 studies were included and evaluated with the PEDro scale [24,25,26,27,28,29,30,31,32,33,34]. The flow chart for the process of the study collection is presented in Figure 1.
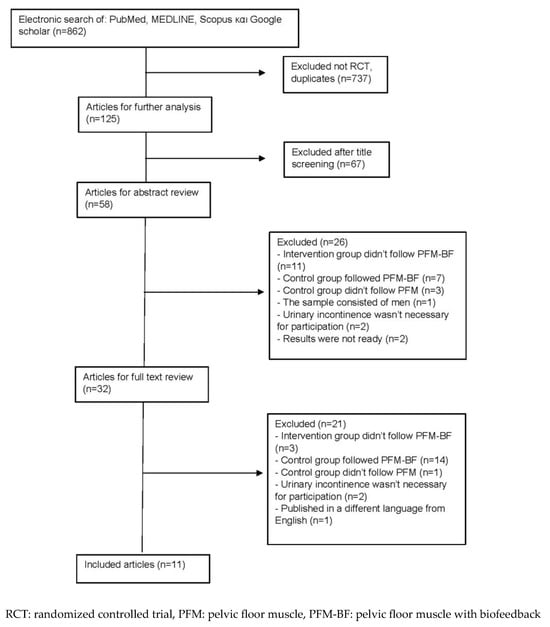
Figure 1.
Flow chart.
3.2. Methodological Quality
According to the PEDro scale, two studies were considered as being high-quality with a score of 8/10 [26] and 7/10 [34], and the remaining nine as moderate with a score of 5/10 [24,27,31] and 6/10 [25,28,29,30,32,33]. The mean score of these studies was six (Table 2). No differences were found in scoring across the two assessors.

Table 2.
Evaluation of studies using PEDro scale.
3.3. Participants
The sample in this systematic review included 1165 women in total, with a mean age of 50–60. From these, 62 (5.3%) dropped out for various reasons. All women were at least 18 years old and were suffering from all types of incontinence (SUI, UUI and MUI); in particular, 546 women had SUI and 386 MUI [24,25,26,27,28,29,31,34]. Out of the MUI women, 217 of them were SUI-symptom dominant, 67 were UUI-symptom dominant, 84 had no SUI or UUI dominance in symptoms, whereas the remaining 18 were without a clear presentation. Fitz et al.’s [30] and Weinstein et al.’s [33] studies included both SUI and MUI women (149 in total) without specifying their proportion dominance. In addition, Sigurdardottir’s et al. [32] study included 84 women with all types of incontinence (SUI, MUI or UUI) without, however, any further specifications. The severity of the incontinence of the participants varied from mild up to severe. Most studies (412 women in total) did not report a level of severity [24,25,26,27,30,32,33]. From the remaining studies, 58.7% of the women had mild to moderate incontinence and 41.3% had severe incontinence.
3.4. Biofeedback Mode
In all eleven studies [24,25,26,27,28,29,30,31,32,33,34] there was at least one group that followed PFM exercises with BF, which was compared to a group that followed PFM exercises alone without BF (Table 3). The experimental group (BF with PFM exercises) presented variety, both in the receiving signal and in the application probes. In six studies, they used electromyographic BF (EMG-BF), receiving visual [25,28,29,31,32,34] and acoustic signals [25], and six studies used pressure BF [24,26,27,30,33,34]. Specifically, Kannan et al. [34] developed their own biofeedback device with wearable EMG sensors in the perineal region that displayed the electrical activity during PFM exercises via a mobile device. In addition, besides the EMG group, they had another BF group using a Kegel intravaginal-probe-based device. Additionally, Özlü et al. [28], besides EMG-BF, had a second experimental group that used pressure BF (measuring intravaginal pressure signals). Furthermore, Fitz et al. [30] also used manometric-based pressure BF equipment. Ong et al. [27] used a vibrance Kegel device with a pressure-sensitive body detecting vaginal squeeze pressures that gave vibrational pulses as an active biofeedback on PFM contractions. In Weinstein et al.’s [33] study, the experimental group used an intravaginal insert with arranged accelerometers. This device communicated wirelessly with an application suitable for mobile phones and provided biofeedback by reflecting muscle contractions. In two other studies [24,26], researchers devolved their own biofeedback devices, both receiving pressure signals. Specifically, Schmidt et al. [24] used a microprocessor-controlled unit via a vaginal probe, which stored vaginal pressure waveforms, and Manonai et al. [26] used an air-pressure balloon to measure pressure changes in the vagina giving feedback displayed on a screen.

Table 3.
General study characteristics.
3.5. Intervention
In all eleven studies [24,25,26,27,28,29,30,31,32,33,34], there was at least one group that followed PFM exercises with BF, which was compared to a group that followed PFM exercises alone without BF (Table 3). There was a heterogeny of PFM exercise programs between the studies concerning duration, frequency and repetitions. The duration of the exercise programs in most studies was for either 12 [24,25,30] or 16 weeks [26,27,32], with a frequency of two to three times a week [25,28,29,30]. In most studies, the program consisted of slow maximum contractions up to 10 s long holds each with up to 10 s rest time intervals following each contraction, and 2 s hold rapid contractions. Each fast-contraction set included up to 10 repetitions or until fatigue. In two studies [28,32], the exercise program was progressive as the time of contractions, the repetition and the sets increased as the weeks passed. The non-BF group in all studies followed a PFM exercise protocol, which was similar to the experimental group (without, however, the biofeedback).
3.6. Primary Outcome
PFM strength was evaluated either with a perineometer [24,25,28,30,32] or manually with the modified Oxford scale [27,29,30,31,34]. Ιn one study, the maximum voluntary contraction was also examined with electromyography [29]. Statistically significant improvements in muscle strength were found in both the BF and the non-BF groups (p < 0.05) [24,25,26,27,28,29,30]. In five studies, the BF group had statistically significantly improved results compared to the non-BF group (p < 0.05) [27,28,29,32,34]. It should be noted that, even though Kannan et al. had two BF groups [34], only the EMG BF group yielded a significant difference in PFM strength compared to the non-BF group.
3.7. Secondary Outcomes
3.7.1. Severity of Incontinence
Incontinence in most studies was assessed with questionnaires such as the King’s health questionnaire (KHQ) [25]; international consultation on incontinence questionnaire—short form (ICIQ-SF) [25,31,34]; Australian pelvic floor questionnaire (APFQ) [27,32], patient global impression of improvement (PGII) [31,33] and the urinary distress inventory—short version (UDI-6) [33]. Incontinence was also evaluated with pad tests [25,28,30,34], bladder diaries [24,25,30,33], by asking patients if they had seen an improvement [24] and by using the Stamey grading system, a four-level scale ranging from 0 (continent) to 3 (total incontinence) [26,35]. Significant improvements were found in both the BF and non-BF groups (p < 0.05) [24,25,27,28,30,33].
Between-group comparisons yielded five studies with statistically significant differences (p < 0.05) in favor of the BF group [27,28,30,32,34]. To note, in Kannan’s et al. study [34], only the EMG BF group (not the vaginal-probe-based one) yielded significant differences compared to the non-BF group. For the vaginal-probe-based device (BF) group, according to the ICIQ-SF, there were no differences between the groups in contrast to the 1 h pad test, where the non-BF group had better results. It should be stated that in Weinstein et al.’s [33] study, according to the PGII and the UDI-6, there was no significant difference between the groups in contrast to the 3-day bladder diary, where the results were in favor of the BF group.
3.7.2. Other Muscular Parameters
Besides muscle strength, other muscular parameters were evaluated. Muscle endurance was evaluated with the manometer [32], the modified Oxford scale [31] or electromyography (EMG) [29]. Statistically significant improvements (p < 0.05) in endurance were found in two studies for the BF group compared to the non-BF one [29,32], whereas in one study, the difference was not significant (p > 0.05) [31]. For the evaluation of PFM function, Fitz et al. [30] assessed with the modified Oxford scale, vaginal palpation and a visual examination of women’s ability to conduct PFM contractions. They found that, in both groups, muscle function significantly improved after 3 months. Both groups were then instructed to continue the PFM exercises at home, and a re-evaluation at 9 months revealed that improvements in muscle function were maintained for both groups, although the BF group had better subjective improvements [30].
Furthermore, electromyography was also used to evaluate the PFM precontraction, initial and final EMG baseline activity [29], as well as abdominal wall muscle activity in order to see whether the PFM exercises were isolated or performed together with the abdominal muscles [26]. Statistically significant improvements were also found in precontractions, since they were either generated or enhanced in both the BF and non-BF groups (p < 0.05). Between the groups, the results were statistically better in the BF group (p < 0.05). Concerning the initial EMG baseline values, only the non-BF group revealed a significant increase post-treatment (p < 0.05). Furthermore, after the analysis of the difference between the final and initial EMG baselines, the period of rest significantly reduced in the non-BF group [29]. Finally, it was found that the BF group performed the exercises without abdominal cocontractions (p < 0.05) [26].
3.7.3. Quality of Life
QoL was evaluated with different questionnaires, such as the KHQ [24,25], ICIQ-SF [25,29,31], European quality of life (EuroQol) [31], incontinence impact questionnaire (IIQ-7) [28], incontinence quality of life questionnaire (I-Qol) [30] and the pelvic floor impact questionnaire—short form (PFIQ-7) [33]. In most studies, QoL improved significantly in both the BF and non-BF groups (p < 0.05) without significant differences between them [24,25,26,28,29,30], except for in Weinstein et al.’s [33] study, where the BF group had significantly better results compared to the non-BF one.
3.7.4. Social Life
Social life was examined in five RCTs [25,26,27,28,30]. The same questionnaires regarding QoL were used with the addition of the «social activity index (SAI)» [28] and the APFQ (question 14) [27]. Four studies found substantial improvements in social life (p < 0.05) across both studies’ groups [25,26,28,30]. Only one study, which had two BF groups, showed that both groups had significantly better results than the non-BF one (p < 0.05) [28].
3.7.5. Adherence
Adherence to the exercise intervention was mostly examined with the use of exercise diaries [25,26,30,31,32]. In one study, however, compliance with treatment was calculated as the ratio between the number of attended sessions over the total number of treatments [24]. Additionally, in Kannan et al.’s [34] study, a tool designed to quantify adherence via a 10-point scale was used. The results in two studies showed that adherence to treatment was in favor of the BF group [26,32], in one, it was in favor of the non-BF group [25] and in three, the results were similar across groups [24,30,31]. In Kannan et al.’s [34] study, of the EMG BF group, 18% showed high adherence (score > 8/10), 71% moderate (score of 3–7/10) and 11% low (score < 2). In the vaginal-probe-based BF group, 34% showed moderate adherence and 66% low, and in the non-BF group, 59% showed moderate adherence and 41% low.
3.7.6. Satisfaction from Therapy
Satisfaction from therapy was examined in two studies only. Fitz et al. [30] asked their patients after 3 and 9 months following intervention if they had the desire to follow a different treatment; both groups reported being satisfied and did not wish to have undergone another therapy. Özlü et al. [28] used a three-point Likert scale (not satisfied, no change and satisfied) to assess satisfaction from therapy and showed that both BF groups had significantly better results compared to the non-BF one (p < 0.05).
4. Discussion
This systematic review’s results showed that women after PFM exercises with BF had a statistically significant improvement in muscle strength and other PFM parameters (such as endurance, muscle function and precontraction), severity of incontinence, QoL and social life. These results were mostly based on women with SUI and MUI and, to a lesser extent, on women with UUI. In five studies, out of which four were of moderate-quality [27,28,29,32] and one of high-quality [34], it was shown that PFM exercises with BF had a statistically significant improvement in muscle strength compared to PFM exercises alone. Four out of these five studies included women with SUI [27,28,29,34] and in only one study [32] the sample consisted of women with SUI, MUI and UUI. In the remaining four studies [24,30,31,33], which did not state a significant difference between BF and non-BF groups, the sample consisted of women with SUI or MUI. This could lead to the conclusion that the intervention was more effective in women with SUI for the parameter of PFM strength.
The results of our systematic review were in agreement with another experimental study [36], which found that PFM exercises with BF had a significantly positive impact on PFMs in comparison to a baseline evaluation. In another study [37], it was shown that there was a significant improvement in PFM strength in both BF and non-BF groups. In the systematic review of Nunes et al. [21], PFM exercises with BF were not more effective in terms of muscle strength than other ones (such as isolated PFM exercises, electrostimulation and no training). However, the included studies mostly consisted of low-methodological-quality RCTs, which negatively influenced the results. In contrast, this systematic review consisted mostly of moderate-methodological-quality RCTs [24,25,27,28,29,30,31,32] and two high-quality ones [26,34].
In the study of Ong et al. [27], which was of moderate quality, there was a statistically significant and ‘speedy’ improvement in pelvic floor muscle strength and a reduction in the severity of incontinence in the BF group compared to the non-BF group after the 4-week reassessment. Interestingly, this faster improvement in the BF group after four weeks of intervention was also seen in Weinstein et al.’s study [33]. An explanation for this fast response could be that the biofeedback provided an easy and accurate identification of the PFMs, thus, facilitating the correct contraction of women who were unable to consciously locate or feel the muscles in order to perform the exercises. Interestingly, it was found that approximately 30% of women were not capable of performing isolated pelvic floor contractions after written or verbal guidance [38,39]. Thus, it may be that the BF training during these early stages of PFM rehabilitation may have been beneficial in promoting a faster improvement in muscle tone, better neuromuscular function and also better urethral closure.
One more possible explanation could be that an early improvement gave additional motivation to patients, who were then encouraged to continue the exercises [27]. It is worth noting that positive results from biofeedback may also have been due to the subjects having more interaction with the therapist during the exercise [40]. Such a fast improvement was also shown in the study of Bertortto et al. [29], who also evaluated the participants after 4 weeks of intervention and yielded better results for maximum voluntary contractions and muscle precontractions in the BF group compared to the non-BF one.
Incontinence symptoms improved in most studies. Even though, in some studies, the results were in favor of the BF group [27,28,30,32,34], in other studies, the results were similar between the groups [25,26,30,31,33,34]. It is important to note that in one of the high-quality studies [26], the results between the groups were similar, possibly due to the fact that the intervention group was characterized as a ‘nonintensive’ BF exercise group, since the whole process took 15 min in a single session. As a result, the intervention in both groups was very similar.
In another experimental study, Lee et al. [19] stated that PFM exercises with BF were effective in reducing urine loss and in increasing muscle strength. It has been supported that the increase in muscle strength reduces incontinence symptoms [41]. Bø [42] examined the effectiveness of a PFM exercise program and supported that after the pad test and the urine loss test, there was a correlation between increased strength and decreased urine loss. On the other hand, Sigurdardottir et al. [32] supported that urine loss was not related to muscle strength. It is, therefore, possible that the main clinical benefit in patients with SUI was related to the improvement in the perception of contractions and not necessarily to the improvement in muscle strength. With the application of BF, females improved their body awareness, structural support of the pelvic organs and also reached faster automatic muscle contractions [32]. The biofeedback informed women about their muscle condition, providing them with instant information by giving feedback usually via a screen [43]. By watching physiological data moving towards the right direction, patients felt confidence and satisfaction, thus, enhancing this movement even more [13].
In the systematic review of Nunes et al. [21], the studies mostly found that the volume of urine loss significantly reduced in the BF group compared to the other groups. However, only women with SUI were included compared to this current systematic review, where SUI, MUI and UUI were included. Therefore, the inclusion of only women with SUI could have affected the results because it is known that these women have greater improvements than other types of urinary incontinence [44]. In contrast, one of the RCTs [31] included in the current review mostly consisted of women with MUI and showed that between the BF and non-BF group, there was no significant difference concerning the severity of incontinence. Additionally, Fitz et al. [36] supported that the addition of BF reduced urine loss during exercise.
Concerning muscle endurance, two included studies [29,32] showed that the BF group had significantly better results in comparison to the non-BF group, whereas one showed that there was no significant deference between the BF and non-BF groups [31]. In agreement with the significant improvement were the results from Fitz et al.’s [36] study, who found that PFM exercises with BF improved endurance. In regard to muscle function, in both the BF and non-BF groups, there was a statistically significant improvement (compared to the baseline), but across-group comparison results were similar [30]. In agreement with this was also another study [45]. PFM exercise on a dysfunctional pelvic floor was shown to be attributed to the improvement of structural support, prolonging activation time and enhancing precontractions, which, as a result, might have decreased or prevented urine leakage [46,47]. The purpose of BF is to improve voluntary motor function, promoting neuroplasticity or activating functional neural regeneration mechanisms of the central nervous system by exposing them to new demands. This neuroplasticity process may assist people in controlling and in monitoring muscle activities and movements, enabling them to manipulate these physiological events during the activity [48].
Quality of life had significant improvements in both groups, but between-group comparisons yielded similar results in most of the studies [24,25,26,28,29,30]. For the parameter of social life in most studies, there was a significant improvement in both groups; however, in one study, the results were in favor of the BF group (p < 0.05) [28]. In agreement with these latter results of this systematic review were two other systematic reviews [21,49], which found a statistically important improvement in QoL after PFM exercises with BF. Nunes et al. [21] also showed that the combination of BF with PFM exercises in comparison to alternative interventions (PFM exercises alone, electrostimulation and no training) were not better. On the other hand, UK International Guidelines [50] support that the combination of PFM with BF has had better results concerning QoL (than PFM exercises alone).
The results concerning satisfaction to treatment could not be supported because of the lack of studies (only two moderate-quality studies) examining this outcome. However, in one study [30], patients in both groups were satisfied with the treatment and did not desire to participate in a different group. In the study of Özlü et al. [28], women in the BF groups were more satisfied than women in the non-BF group.
Finally, adherence to treatment was found better in the BF group in two studies [26,32], better in the non-BF group in one [25] and similar between groups in three studies [24,30,31]. In Fitz et al.’s [36] study, it was observed that the frequency of exercise followed at home decreased during the nonsupervised exercise period. This came to an agreement with two other studies [51,52], emphasizing the role of supervision in adherence to exercise programs. In Kannan et al.’s [34] high-quality study, the EMG group showed greater adherence compared to the vaginal probe and non-BF groups. Women in the vaginal probe BF group reported adverse effects (burning and painful urination, discomfort, skin damage near the vaginal region), resulting in the discontinuation of the intervention. Additionally, in the Cochrane review [40], it was supported that adverse events were associated with intravaginal probes leading to the discontinuation of the intervention. This fact may have affected the results.
Others supported that the EMG-BF had an advantage over manometric pressure biofeedback due to the fact that it can accommodate new types of electrodes that are lightweight, more sensitive and designed to stay in place, thus, allowing for a more functional body position for assessment and treatment [43]. In one moderate-quality RCT [28], two BF groups (perineal EMG-BF and intravaginal pressure BF) were included. The results concerning muscle strength, QoL, social life and the severity of incontinence were similar between the groups at both 4 and 8 weeks. It should be noted that the level of discomfort was significantly higher in the intravaginal pressure BF group compared to the EMG-BF group at the 4-week reassessment. In contrast, in Kannan et al.’s high-quality study [34], the EMG-BF group was superior to the vaginal probe BF group concerning muscle strength and the severity of incontinence. However, these results must be interpreted with caution due to the underpowered pilot trial.
The findings of this systematic review add novel contributions to the existing literature. As it has been known, the first-line treatment for urinary incontinence is PFM exercises [8]. Most RCTs included in this review showed that PFM exercises with BF had a significant effect in muscle strength and the severity of incontinence compared to PFM exercises without BF. It is also important to note that besides the significant effect of the combination of PFM exercises with BF on muscle strength and the severity of incontinence, a significantly improvement was also shown in other muscle parameters (such as endurance, precontraction and function), Qol and social life compared to the baseline. As a result, PFM exercises with BF had an important therapeutic effect in women with urinary incontinence. However, it should be noted that these results were based on RCTs that showed heterogeny concerning the type of PFM exercise and the follow-up period.
4.1. Clinical Implications
By incorporating biofeedback into a PFM exercises program, patients showed better coordination and muscle control [53], which was probably most important at the beginning of treatment [54]. Additionally, as mentioned above, BF possibly helped in gaining a faster response to PFM contractions [32]. Furthermore, it was found that the addition of BF in women with very low muscle strength helped to enhance maximum vaginal pressures [29]. The advantage that BF had was that the small contraction amplitude caused by a low muscle force could be visualized. On that account, it is believed that BF should be an option in women with very weak PFM strength. Lastly, BF can be considered as supplementary to the PFM exercise program, allowing patients to observe muscle contractions during exercise, which, in fact, could improve motivation [51,55].
4.2. Limitations and Future Considerations
Limitation of this study were that only English studies were included and most of them were of moderate methodological quality. Additionally, six studies [24,26,27,31,32,33], which relied solely on subjective findings (such as the ICIQ-SF questionnaire) for the evaluation of incontinence, were included. Furthermore, not many RCTs examining the long-term effect, as well as many studies assessing treatment satisfaction, were found. Lastly, the examination of the variables was based on their statistical significance and not on their clinical significance. In addition, the included RCTs showed heterogeny between the type of PFM exercises and follow-up periods. However, this was the case across published papers and clinical practice with PFM exercises. Lastly, a meta-analysis would have been useful, but due to the limited number of studies and the heterogeneity of the outcome measures used, this was not implemented.
In future, more qualitative methodology studies should be carried out examining the satisfaction of therapy. Knowledge whether the intervention gives better satisfaction to the participants would help in the choice of treatment. Additionally, more studies should evaluate the effect in women with UUI, which was the least researched patient subgroup. Finally, it would be useful to investigate the comparison of the effectiveness of different BF types.
5. Conclusions
PFM exercises in combination with biofeedback contributed significantly to all examined muscle parameters, QoL and social life, as well as addressing the severity of incontinence. Concerning muscle strength, five studies showed a significant improvement in the BF group compared to the non-BF group. A similar number of studies showed a significant improvement in favor of the BF group concerning the severity of incontinence. Furthermore, regarding QoL and social life, PFM with BF interventions did not appear to be more effective than PFM exercises alone. For adherence to treatment, the results were ambiguous. Lastly, there were not enough studies to support the results of other PFM parameters and satisfaction to therapy. In conclusion, PFM exercises with BF were proven to be effective for women with urinary incontinence and for the variables of muscle strength and urinary incontinence, shown to be superior to PFM exercises alone. The clinical implications of BF were that it can be used at the beginning of the treatment and in women with very weak or no PFM strength. With the use of BF, patients showed better coordination and muscle control, and the small contraction amplitude caused by muscles with low strength could be visualized. In the future, more studies should emphasize the satisfaction of therapy and investigate which types of BF are better.
Author Contributions
Conceptualization, A.E.M. and E.B.; methodology, A.E.M., E.B. and S.L.; writing—original draft preparation, A.E.M., S.A.X. and M.T.; writing—review and editing, E.B.; project administration, K.F.; All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
Not Applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Abrams, P.; Andersson, K.E.; Birder, L.; Brubaker, L.; Cardozo, L.; Chapple, C.; Cottenden, A.; Davila, W.; de Ridder, D.; Dmochowski, R.; et al. Fourth international consultation on incontinence recommendations of the international scientific committee: Evaluation and treatment of urinary incontinence, pelvic organ prolapse, and fecal incontinence. Neurourol. Urodyn. 2010, 29, 213–240. [Google Scholar] [CrossRef] [PubMed]
- Norton, P.; Brubaker, L. Urinary incontinence in women. Lancet 2006, 367, 57–67. [Google Scholar] [CrossRef] [PubMed]
- Derewiecki, T.; Mroczek, M.; Majcher, P.; Chrusciel, P. Importance of urinary incontinence problem among women over 40 years of age. Hygeia Publ. Health 2015, 50, 219–225. [Google Scholar]
- Zygmunt, R.; Koziol, S.; Hladki, W.; Golec, J. The influence of physiotherapy on incontinence in women. Emerg. Duty 2017, 10, 77–83. [Google Scholar]
- Klimaszewska, K. The social aspects of urinary incontinence of women. Pielęg XXI Wieku 2017, 16, 57–61. [Google Scholar] [CrossRef]
- Saboia, D.M.; Firmiano, M.L.V.; Bezerra, K.d.C.; Neto, J.A.V.; Oriá, M.O.B.; Vasconcelos, C.T.M. Impact of urinary incontinence types on women’s quality of life. Rev. Esc. Enferm. USP 2017, 51, e03266. [Google Scholar] [CrossRef] [PubMed]
- Lukacz, E.S.; Santiago-Lastra, Y.; Albo, M.E.; Brubaker, L. Urinary Incontinence in Women: A Review. JAMA 2017, 318, 1592–1604. [Google Scholar] [CrossRef]
- National Institute for Health Clinical Excellence. Urinary Incontinence: The Management of Urinary Incontinence in Women; Clinical Guideline; NICE: London, UK, 2006; Volume 40. [Google Scholar]
- Curillo-Aguirre, C.A.; Gea-Izquierdo, E. Effectiveness of pelvic floor muscle training on quality of life in women with urinary incontinence: A systematic review and meta-analysis. Medicina 2023, 59, 1004. [Google Scholar] [CrossRef]
- Dumoulin, C.; Hay-Smith, J.; Habée-Séguin, G.M.; Mercier, J. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women: A short version Cochrane systematic review with meta-analysis. Neurourol. Urodyn. 2014, 34, 300–308. [Google Scholar] [CrossRef]
- Tosun, O.C.; Solmaz, U.; Ekin, A.; Tosun, G.; Gezer, C.; Ergenoglu, A.M.; Yeniel, A.O.; Mat, E.; Malkoc, M.; Askar, N. Assessment of the effect of pelvic floor exercises on pelvic floor muscle strength using ultrasonography in patients with urinary incontinence: A prospective randomized controlled trial. J. Phys. Ther. Sci. 2016, 28, 360–365. [Google Scholar] [CrossRef]
- Kopańska, M.; Torices, S.; Czech, J.; Koziara, W.; Toborek, M.; Dobrek, L. Urinary incontinence in women: Biofeedback as an innovative treatment method. Ther. Adv. Urol. 2020, 12, 1756287220934359. [Google Scholar] [CrossRef] [PubMed]
- Frank, D.L.; Khorshid, L.; Kiffer, J.F.; Moravec, C.S.; McKee, M.G. Biofeedback in medicine: Who, when, why and how? Ment. Health Fam. Med. 2010, 7, 85–91. [Google Scholar] [PubMed]
- Giggins, O.M.; Persson, U.M.; Caulfield, B. Biofeedback in rehabilitation. J. NeuroEng. Rehabil. 2013, 10, 60. [Google Scholar] [CrossRef] [PubMed]
- Newman, D.K.; Wein, A.J. Managing and Treating Urinary Incontinence, 2nd ed.; Health Professions Press: Baltimore, MD, USA, 2009; pp. 245–306. [Google Scholar]
- Capelini, M.V.; Riccetto, C.L.; Dambros, M.; Tamanini, J.T.; Herrmann, V.; Muller, V. Pelvic floor exercises with biofeedback for stress urinary incontinence. Int. Braz. J. Urol. 2006, 32, 462–469. [Google Scholar] [CrossRef] [PubMed]
- Chmielewska, D.; Stania, M.; Kucab–Klich, K.; Błaszczak, E.; Kwaśna, K.; Smykla, A.; Hudziak, D.; Dolibog, P. Electromyographic characteristics of pelvic floor muscles in women with stress urinary incontinence following sEMG-assisted biofeedback training and Pilates exercises. PLoS ONE 2019, 14, e0225647. [Google Scholar] [CrossRef] [PubMed]
- Dannecker, C.; Wolf, V.; Raab, R.; Hepp, H.; Anthuber, C. EMG-biofeedback assisted pelvic floor muscle training is an effective therapy of stress urinary or mixed incontinence: A 7-year experience with 390 patients. Arch. Gyn. Obstet. 2005, 273, 93–97. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.N.; Lee, S.Y.; Lee, Y.S.; Han, J.Y.; Choo, M.S.; Lee, K.S. Pelvic floor muscle training using an extracorporeal biofeedback device for female stress urinary incontinence. Int. Urogynecol. J. 2012, 24, 831–838. [Google Scholar] [CrossRef]
- Rett, M.T.; Simoes, J.A.; Herrmann, V.; Pinto, C.L.; Marques, A.A.; Morais, S.S. Management of Stress Urinary Incontinence with Surface Electromyography–Assisted Biofeedback in Women of Reproductive Age. Phys. Ther. 2007, 87, 136–142. [Google Scholar] [CrossRef]
- Nunes, E.F.C.; Sampaio, L.M.M.; Biasotto-Gonzalez, D.A.; Nagano, R.C.d.R.; Politti, F. Biofeedback for pelvic floor muscle training in women with stress urinary incontinence: A systematic review with meta-analysis. Physiotherapy 2018, 105, 10–23. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int. J. Surg. 2010, 8, 336–341. [Google Scholar] [CrossRef]
- Maher, C.G.; Sherrington, C.; Herbert, R.D.; Moseley, A.M.; Elkins, M. Reliability of the PEDro Scale for Rating Quality of Randomized Controlled Trials. Phys. Ther. 2003, 83, 713–721. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, A.P.; Sanches, P.R.S.; Silva, D.P.; Ramos, J.G.L.; Nohama, P. A new pelvic muscle trainer for the treatment of urinary incontinence. Int. J. Gynecol. Obstet. 2009, 105, 218–222. [Google Scholar] [CrossRef] [PubMed]
- Hirakawa, T.; Suzuki, S.; Kato, K.; Gotoh, M.; Yoshikawa, Y. Randomized controlled trial of pelvic floor muscle training with or without biofeedback for urinary incontinence. Int. Urogynecol. J. 2013, 24, 1347–1354. [Google Scholar] [CrossRef] [PubMed]
- Manonai, J.; Kamthaworn, S.; Petsarb, K.; Wattanayingcharoenchai, R. Development of a pelvic floor muscle strength ecaluation device. J. Med. Assoc. Thai 2015, 98, 219–225. [Google Scholar] [PubMed]
- Ong, T.A.; Khong, S.Y.; Ng, K.L.; Ting, J.R.S.; Kamal, N.; Yeoh, W.S.; Yap, N.Y.; Razack, A.H. Using the Vibrance Kegel Device With Pelvic Floor Muscle Exercise for Stress Urinary Incontinence: A Randomized Controlled Pilot Study. Urology 2015, 86, 487–491. [Google Scholar] [CrossRef] [PubMed]
- Özlü, A.; Yıldız, N.; Öztekin, Ö. Comparison of the efficacy of perineal and intravaginal biofeedback assisted pelvic floor muscle exercises in women with urodynamic stress urinary incontinence. Neurourol. Urodyn. 2017, 36, 2132–2141. [Google Scholar] [CrossRef]
- Bertotto, A.; Schvartzman, R.; Uchôa, S.; Wender, M.C.O. Effect of electromyographic biofeedback as an add-on to pelvic floor muscle exercises on neuromuscular outcomes and quality of life in postmenopausal women with stress urinary incontinence: A randomized controlled trial. Neurourol. Urodyn. 2017, 36, 2142–2147. [Google Scholar] [CrossRef]
- Fitz, F.F.; Stüpp, L.; da Costa, T.F.; Bortolini, M.A.T.; Girão, M.J.B.C.; Castro, R.A. Outpatient biofeedback in addition to home pelvic floor muscle training for stress urinary incontinence: A randomized controlled trial. Neurourol. Urodyn. 2017, 36, 2034–2043. [Google Scholar] [CrossRef]
- Hagen, S.; Elders, A.; Stratton, S.; Sergenson, N.; Bugge, C.; Dean, S.; Hay-Smith, J.; Kilonzo, M.; Dimitrova, M.; Abdel-Fattah, M.; et al. Effectiveness of pelvic floor muscle training with and without electromyographic biofeedback for urinary incontinence in women: Multicentre randomised controlled trial. BMJ 2020, 371, m3719. [Google Scholar] [CrossRef]
- Sigurdardottir, T.; Steingrimsdottir, T.; Geirsson, R.T.; Halldorsson, T.I.; Aspelund, T.; Bø, K. Can postpartum pelvic floor muscle training reduce urinary and anal incontinence? An assessor-blinded randomized controlled trial. Am. J. Obstet. Gynecol. 2020, in press. [CrossRef]
- Weinstein, M.M.; Collins, S.; Quiroz, L.; Anger, J.T.; Paraiso, M.F.R.; DeLong, J.; Richter, H.E. Multicenter randomized controlled trial of pelvic floor muscle training with a motion-based digital therapeutic device versus pelvic floor muscle training alone for treatment of stress-predominant urinary incontinence. Female Pelvic Med. Reconstr. Surg. 2021, 28, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Kannan, P.; Cheing, G.L.Y.; Fung, B.K.Y.; Li, J.; Leung, W.C.; Chung, R.C.K.; Cheung, T.W.; Lam, L.K.; Lee, W.Y.; Wong, W.C.; et al. Effectiveness of pelvic floor muscle training alone or combined with either a novel biofeedback device or conventional biofeedback for improving stress urinary incontinence: A randomized controlled pilot trial. Contemp. Clin. Trials 2022, 123, 106991. [Google Scholar] [CrossRef] [PubMed]
- Stamey, T.A. Endoscopic suspension of the vesical neck for urinary incontinence. Surg. Gynecol. Obstet. 1973, 28, 762–764. [Google Scholar] [CrossRef] [PubMed]
- Fitz, F.F.; Resende, A.P.M.; Stupp, L.; Costa, T.F.; Sartori, M.G.F.; Girao, M.J.B.C.; Castro, R.A. Effect the adding of biofeedback to the training of the pelvic floor muscles to treatment of stress urinary incontinence. Rev. Bras. Ginecol. Obstet. 2012, 34, 505–510. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Özengin, N.; Bakar, Y.; Özdemir, C.; Duran, B. The comparison of EMG- biofeedback and extracorporeal magnetic innervation treatments in women with urinary incontinence. Clin. Exp. Obstet. Gynecol. 2016, 43, 550–554. [Google Scholar] [CrossRef]
- Bø, K.; Kvarstein, B.; Hagen, R.R.; Larsen, S. Pelvic floor muscle exercise for the treatment of female stress urinary incontinence: II. Validity of vaginal pressure measurements of pelvic floor muscle strength and the necessity of supplementary methods for control of correct contraction. Neurourol. Urodyn. 1990, 9, 479–487. [Google Scholar] [CrossRef]
- Bump, R.C.; Hurt, W.G.; Fantl, J.A.; Wyman, J.F. Assessment of Kegel pelvic muscle exercise performance after brief verbal instruction. Am. J. Obstet. Gynecol. 1991, 165, 322–329. [Google Scholar] [CrossRef]
- Herderschee, R.; Hay-Smith, E.J.; Herbison, G.P.; Roovers, J.P.; Heineman, M.J. Feedback or biofeedback to augment pelvic floor muscle training for urinary incontinence in women. Cochrane Database Syst. Rev. 2011, in press. [Google Scholar] [CrossRef]
- Knorst, M.R.; Resende, T.L.; Santos, T.G.; Goldim, J.R. The effect of outpatient physical therapy intervention on pelvic floor muscles in women with urinary incontinence. Braz. J. Phys. Ther. 2013, 17, 442–449. [Google Scholar] [CrossRef]
- Bø, K. Pelvic floor muscle training is effective in treatment of female stress urinary incontinence, but how does it work? Int. Urogynecol. J. Pelvic Floor. Dysfunct. 2004, 15, 76–84. [Google Scholar] [CrossRef]
- Newman, D.K. Pelvic Floor Muscle Rehabilitation Using Biofeedback. Urol. Nurs. 2014, 34, 193. [Google Scholar] [CrossRef] [PubMed]
- Kaya, S.; Akbayrak, T.; Gursen, C.; Beksac, S. Short-term effect of adding pelvic floor muscle training to bladder training for female urinary incontinence: A randomized controlled trial. Int. Urogynecol. J. 2014, 26, 285–293. [Google Scholar] [CrossRef] [PubMed]
- Fitz, F.F.; Resende, A.P.; Stüpp, L.; Sartori, M.G.F.; Girao, M.J.B.C.; Castro, R.A. Biofeedback for the treatment of female pelvic floor muscle dysfunction: A systematic review and meta-analysis. Int. Urogynecol. J. 2012, 23, 1495–1516. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.M.; Ashton-Miller, J.A.; DeLancey, J.O. A pelvic muscle precontraction can reduce cough-related urine loss in selected women with mild SUI. J. Am. Geriatr. Soc. 1998, 46, 870–874. [Google Scholar] [CrossRef]
- Price, N.; Dawood, R.; Jackson, S.R. Pelvic floor exercise for urinary incontinence: A systematic literature review. Maturitas 2010, 67, 309–315. [Google Scholar] [CrossRef] [PubMed]
- Goulart, F.; Vasconcelos, K.S.; de Souza, M.R.; Pontes, P.B. Physical therapy for facial paralysis using the biofeedback. Acta Fisiátr. 2002, 9, 134–140. [Google Scholar] [CrossRef]
- Capelini, M.V.; Riccetto, C.L.; Palma, P.C. Treatment of stress urinary incontinence with biofeedback: Objective analysis and impact on quality of life. Rev. Bras. Ginecol. Obstet. 2005, 27, 230. [Google Scholar] [CrossRef]
- National Guideline Alliance UK. Urinary Incontinence and Pelvic Organ Prolapse in Women: Management. 2019. Available online: www.nice.ork.uk/guidance/ng123 (accessed on 24 August 2023).
- Bø, K.; Herbert, R. There is not yet strong evidence that exercises regimens other than pelvic floor muscle training can reduce stress urinary incontinence in women: A systematic review. J. Physiother. 2013, 59, 159–168. [Google Scholar] [CrossRef]
- Hay-Smith, E.J.C.; Herderschee, R.; Dumoulin, C.; Herbison, P.G. Comparisons of approaches to pelvic floor muscle training for urinary incontinence in women. Cochrane Database Syst. Rev. 2015, 48, 689–705. [Google Scholar] [CrossRef]
- Burns, P.A.; Pranikoff, Κ.; Nochajski, T.H.; Hadley, E.C.; Levy, K.J.; Ory, M.G. A comparison of effectiveness of biofeedback and pelvic muscle exercise treatment of stress incontinence in older community-dwelling women. J. Gerontol. 1993, 48, M167–M174. [Google Scholar]
- Berghmans, L.C.M.; Frederiks, C.M.A.; de Bie, R.A.; Weil, E.H.J.; Smeets, L.W.H.; vam Waalwijk vam Doorm, E.S.C.; Jankinegt, R.A. Efficacy of biofeedback, when included with pelvic floor muscle exercise treatment, for genuine stress incontinence. Neurourol. Urodyn. 1996, 15, 37–52. [Google Scholar] [CrossRef]
- Mørkved, S.; Bø, K.; Fjortoft, T. Effect of adding biofeedback to pelvic floor muscle training to treat urodynamic stress incontinence. Obstet. Gynecol. 2002, 100, 730–739. [Google Scholar] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).