Abstract
(1) Background: The static body-weight wall-squat (SBWS) exercise is often included in the early rehabilitation stages of the lower limb. To establish its effectiveness and optimise its application, it is important to precisely quantify the muscle contribution to different versions of this exercise. (2) Methods: We analysed the electromyographic activity of lower limb and lumbar muscles during the SBWS with knees flexed at 45° by manipulating three different variables: horizontal distance of the ankles from the wall; scapular or pelvic location of the centre of pressure Cwall of the force exerted by the wall on the back; rearfoot or forefoot location of the centre of pressure CGR of the ground reaction force. (3) Results: The forefoot-to-rearfoot CGR shift significantly increased the vastus medialis, vastus lateralis, and tibialis anterior activity up to 23%, 26%, and 44% of the maximum voluntary isometric contraction (MVIC). The lumbar muscle activity was maximised (23% MVIC) shifting CGR at the forefoot, Cwall at the scapular zone, and placing the feet far from the wall. (4) Conclusions: These SBWS methods might be effective for quadriceps, tibialis anterior, and lumbar muscles strengthening in the early phase of rehabilitation intervention as soon as the patient can tolerate partial weight-bearing. The exercise appears suitable for patients with low back pain and limited lumbar muscle endurance, or quadriceps weakness and inhibition secondary to a knee injury.
1. Introduction
The ‘static body-weight wall-squat’ (SBWS) exercise is frequently included in lower-limb rehabilitation programmes [1,2,3,4]. It also provides a practical, reliable, and well-tolerated clinical test for the assessment of the quadriceps muscle endurance [5,6]. Given the isometric execution and support provided by the wall, this exercise requires less balance and stability than the common squat exercise. For this reason, the SBWS can be readily included in the early stage of rehabilitation interventions, as soon as the patient can tolerate weight-bearing [1]. The correct SBWS execution requires the subject to hold a partial squat position with the back flat against a vertical wall, spine in a neutral position, arms relaxed along the body, knee in proper alignment (i.e., neutral knee varus/valgus and internal/external rotation) and feet about shoulder-width apart. The knee flexion angle () and the horizontal distance (d) of the ankles from the wall constitute the main exercise variables. These two parameters completely determine the configuration of the body, including the hip and ankle angle, when the subject’s anthropometry is known.
Besides its popularity, information about the muscle contribution to the SBWS performance is lacking. Blanpied [7] recorded electromyographic (EMG) signals during a dynamic version of the body-weight wall squat (wall slide). The participants were required to perform five consecutive exercise repetitions up to 60° of knee flexion meanwhile the feet were aligned with the hip or 50 cm forward and the posterior support was at the hip or scapular level. The author used surface EMG sensors to record the activity of the gluteus maximus, semitendinosus, vastus lateralis, and soleus muscles. The EMG data were used to quantify the mean EMG activity among three consecutive repetitions. Critically, this information has limited impact on the management of the early subacute phase of lower limb rehabilitation, where fine control of muscle activity, joint torques, and joint reaction forces is needed in different phases of the exercise throughout the range of motion (ROM). For example, it is known that quadriceps contraction yields patterns of mechanical loading on the knee joint that change considerably over the range of knee motion and among the different knee joint structures [8,9,10,11,12,13].
To gain a deeper insight into the biomechanics of static wall squat, Biscarini et al. [14] have recently provided a quantitative analysis of this exercise combining biomechanical modelling and force plate measurements. In that study, the lower limb joint torques, and the shear and compressive components of the tibiofemoral reaction force, were determined analytically as a function of and d considering two additional exercise variants: (1) progressive shift between the scapular and the gluteal zone of the centre of pressure Cwall of the supporting force exerted by the wall on the back; (2) progressive shift between the rearfoot and forefoot of the centre of pressure CGR of the ground reaction force. Both variants had an important impact on the joint torques and joint reaction forces in the whole domain of the and d variables.
To complete the biomechanical analysis of the SBWS, the EMG activity of relevant muscles involved in the exercise (hip, knee, and ankle extensors, erector spinae, and tibialis anterior) should be mapped in the whole domain of the four variables , d, xGR (the location of CGR on the ground, between rearfoot and forefoot) and ywall (the location of CGR on the wall, between the scapular and the pelvic zone). However, this requires massive experimental activity. In this research, we provide the first set of such EMG measurements, selecting values of the four variables that are easily reproducible in clinical settings and of primary interest in rehabilitation applications. Specifically, the measurements were carried out at 45° of knee flexion. In this condition, the mechanical loading on the anterior cruciate ligament (ACL) is negligible (the ACL may experience a significant tensile loading in the final 40° of knee extension) [14], the compressive tibiofemoral and patellofemoral forces are mild (compared with those that can be achieved at a higher degree of knee flexion) [15,16,17,18,19], but the demand of knee-extension muscle torque is sufficiently high (up to 65 Nm) [14] to produce strengthening adaptation in the early phase of rehabilitation interventions. To comply with the principle of exercise individualisation, contrary to the Blanpied protocol [7], the selected d values were referred to as individual anthropometry measurements (i.e., the length of the femur). Finally, as highlighted by the authors in a previous study, the SBWS allows the exerciser to voluntarily perform scapular–pelvic Cwall shifts and rearfoot–forefoot CGR shifts [14]. Only in the static version of the wall-squat exercise can this be readily performed without losing neutral spine and knee alignment, vertical trunk orientation, and forefoot or rearfoot contact with the floor [14].
Therefore, the main aim of this study was to measure the electromyographic activity of the lower limb and lumbar muscles during the SBWS performed at , in different exercise conditions defined by different combinations of the d, xGR, and ywall variables. We hypothesise that the activity of the lumbar muscles and the muscles of the rear part of the lower limb is maximised by shifting Cwall at the scapular zone (i.e., increasing the moment arm of the wall-supporting force about the lumbar and lower limb joints) and shifting CGR at forefoot and placing the feet far from the wall (as this maximises the tendency of gravity to rotate the entire body backward and, consequently, the magnitude of the wall-supporting force). In this condition, the wall-supporting force is expected to develop maximum flexor torque on the hip and lumbar joints and extensor torque on the knee [14]. We also hypothesise that quadriceps activity is maximised by the opposite conditions, which is expected to maximise the knee flexor torque developed by the ground reaction force while minimising the knee extensor torque developed by the wall-supporting force [14]. For both wall-squat configurations, we hypothesise that the prime muscles involved in the exercises reach activation levels effective for muscle strengthening interventions in the early stage of the knee and lumbar rehabilitation programs.
2. Materials and Methods
2.1. Participants
For this study, 8 female and 14 male participants (age 29 ± 7 years, age range 19–47 years, height 1.71 ± 0.09 m, body mass 69 ± 12 kg), without musculoskeletal injuries, were recruited from local fitness centres. All participants were experienced in resistance training (intermediate level), including squat exercises. The complete list of inclusion and exclusion criteria is outlined in Table 1. Informed consent was obtained from all subjects involved in the study, which was conducted in accordance with the Declaration of Helsinki and approved by the ethics committee of the University of Perugia.

Table 1.
Inclusion and exclusion criteria.
2.2. Exercise Conditions and Selected Muscles
All the participants executed the SBWS exercise with in eight different conditions (Figure 1) resulting from the combination of two d values ( and , where is the knee–hip distance), two locations of Cwall (obtained shifting Cwall between the scapular and pelvic zone), and two locations of CGR (obtained shifting CGR between forefoot and rearfoot). To displace Cwall toward the scapular (pelvic) zone, participants had to touch the wall with only the scapular (pelvic) zone while keeping neutral spine alignment and vertical trunk orientation. To displace CGR toward the rearfoot (forefoot), participants had to push against the ground with the rearfoot (forefoot) while keeping the whole foot plant on the ground.
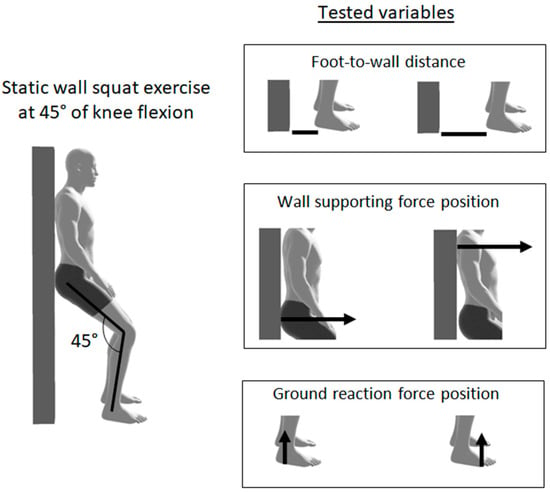
Figure 1.
Sketch illustrating the static wall-squat exercise executed with knees flexed at 45° (left panel) and the two different conditions for each of the three exercise variables (right panels): (1) horizontal distance d of the ankles from the wall ( and ); (2) scapular or pelvic location of the centre of pressure Cwall of the wall-supporting force; (3) rearfoot or forefoot location of the centre of pressure CGR of the ground reaction force.
In each condition, the static wall-squat position was held for 8 s. During each trial, surface EMG signals were recorded from gluteus maximus (GM), vastus lateralis (VL), vastus medialis (VM), biceps femoris long head (BF), semitendinosus (ST), tibialis anterior (TA), and gastrocnemius lateralis (GL), and lumbar part of erector spinae longissimus (ES) of the dominant side of the body.
2.3. Testing Session
After a 10 min warm-up at moderate intensity on a bike ergometer, we recorded the EMG activity during maximum voluntary isometric contractions (MVICs) executed in postural conditions specific for each of the eight muscles of interest [20]. During the MVIC recording procedures, the subjects gradually reached the maximum effort in 2 to 3 s and held it for 3 s. Each MVIC test was executed two times, and we indexed the maximum muscle activation level as the highest EMG activity level across the two tests. Participants were given at least 2 min of rest between maximum contractions. The maximum EMG activity levels determined during the MVIC tests were used for offline normalisation of the EMG signals subsequently recorded during the wall-squat trials.
After the MVIC test and full recovery (of at least 5 min), each participant performed the static wall-squat in the 8 different conditions (see the previous section for details). To avoid potential fatigue-induced biases, the trial sequence was randomised, and 3 min of recovery was allowed between trials.
2.4. Data Recording and Processing
A FREEEMG 1000 apparatus (BTS Bioengineering, Milano, Italy) comprising wireless EMG sensors was used to record the EMG signals in each trail. The surface EMG electrodes were placed according to the surface electromyography for non-invasive assessment of muscles (SENIAM) guidelines. The selected knee angle was determined by a twin axis SG150 electrogoniometer (Biometrics, Newport, UK). The procedure for the electrogoniometer positioning is reported in previous papers [21]. For each muscle, the raw EMG signal was differentially amplified (933 gain), band-pass filtered (10 to 500 Hz), and digitalised (16-bit resolution, 1 kHz sampling frequency) online by the wireless EMG sensor and then sent to the laboratory’s computer for offline processing and analysis. The EMG signals were transformed into amplitude envelopes through a point-to-point moving root-mean-square filter (500-millisecond time interval), normalised to the peak EMG amplitude at MVIC, and expressed as a percentage of the MVIC value. Finally, we computed the mean value of the EMG signals for statistical comparison between task conditions.
2.5. Statistical Analysis
Based on previous reports [7,15], the sample size was estimated by computing a priori power analysis (G*Power 3.1 software) setting a power level of 0.80, an α significance level of 0.05, and a medium-to-large effect size (0.65) for F tests.
Analysis of variance (ANOVA) was performed to evaluate differences among data samples. Normality was assayed using the Shapiro–Wilk test, while the homogeneity of the variance between populations and sphericity by Levene’s test and Mauchly’s sphericity test, respectively. Probabilities were corrected based on Greenhouse–Geisser and Huynh–Feldt epsilon when appropriated. Data did not follow ANOVA assumptions for normality, and variances were transformed by applying an ln function to make transformed data satisfy the ANOVA assumptions. Mean ± SD used for descriptive statistics was always referred to as original data, even when the statistical analysis was carried out on transformed data.
The dependent variables were analysed with a 3-way repeated-measures ANOVA with ( and ), Cwall (Cwall shifted between the scapular and pelvic zone), and CGR (CGR shifted between forefoot and rearfoot) as independent within-subject factors. For significant main effects or interactions, the statistical power and effect size were assessed by the observed power (ω) and partial eta squared () coefficients, respectively (Table 2), and post hoc analysis was run via the Scheffè test (Table 3). For each statistical test, the significance level was designated at .

Table 2.
p-value, effect size (partial eta squared ), and statistical power (observed power ω) for main effects and interactions as deduced by the three-way ANOVA analysis. The statistical parameters are reported only for main effects and interactions with p < 0.05. No statistically significant effect was detected for the d ∗ Cwall ∗ CGR interaction. Main effects: (1) change in ankle–wall distance d between and ; (2) shift in Cwall between the scapular and pelvic zone; (3) shift in CGR between rearfoot and forefoot. ES = erector spinae, GM = gluteus maximus, VM = vastus medialis, VL = vastus lateralis, BF = biceps femoris, ST = semitendinosus, GL = gastrocnemius lateralis, TA = tibialis anterior.

Table 3.
Post hoc comparisons among different exercise conditions that differ for the value of one variable (variable 1: change in ankle–wall distance d between and ; variable 2: shift in Cwall between the scapular (S) and pelvic (P) zone; variable 3: shift in CGR between rearfoot (R) and forefoot (F)). The p-value is reported only for comparisons with statistically significant differences (p < 0.05). ES = erector spinae, GM = gluteus maximus, VM = vastus medialis, VL = vastus lateralis, BF = biceps femoris, ST = semitendinosus, GL = gastrocnemius lateralis, TA = tibialis anterior; S: Cwall at the scapular zone, P: Cwall at the pelvic zone, R: CGR at rearfoot, F: CGR at forefoot.
3. Results
3.1. Erector Spinae and Gluteus Maximum
The mean ES activity was significantly affected by all exercise variables (d, Cwall, and CGR), as well as by the interactions between d and Cwall and between Cwall and CGR (Table 2). Post hoc comparison (Table 3) highlighted that ES activity increased significantly by (1) shifting CGR from rearfoot to forefoot with Cwall at the scapular zone, at either (p < 10−3) or (p = 0.001); (2) increasing d with Cwall at the scapular zone, with CGR either at rearfoot (p < 10−3) or forefoot (p < 10−3); (3) shifting Cwall from the pelvic to the scapular zone, at , with CGR either at rearfoot (p < 10−3) or forefoot (p < 10−3), and at , with CGR at the forefoot (p < 10−3). Notably, a peak activity slightly higher than 23% MVIC was reached for , Cwall at the scapular zone, and CGR at the forefoot (Figure 2, Table 4).
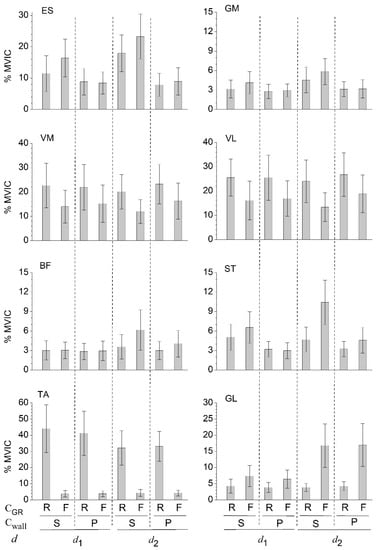
Figure 2.
Mean muscle activation levels (expressed as a percentage of the peak electromyographic amplitude at MVIC) recorded during the SBWS exercise executed with knees flexed at 45° and in two different conditions for each of the three exercise variables: (1) horizontal distance d of the ankles from the wall ( and ); (2) scapular (S) or pelvic (P) location of Cwall; (3) rearfoot (R) or forefoot (F) location of CGR. ES = erector spinae, GM = gluteus maximus, VM = vastus medialis, VL = vastus lateralis, BF = biceps femoris, ST = semitendinosus, GL = gastrocnemius lateralis, TA = tibialis anterior; S: Cwall at the scapular zone, P: Cwall at the pelvic zone, R: CGR at rearfoot, F: CGR at forefoot.

Table 4.
Muscle activation levels (expressed as a percentage of the peak electromyographic amplitude at MVIC) recorded during the SBWS exercise executed with knees flexed at 45° and in two different conditions for each of the three exercise variables: (1) horizontal distance d of the ankles from the wall ( and ); (2) scapular (S) or pelvic (P) location of Cwall; (3) rearfoot (R) or forefoot (F) location of CGR. Data reported as mean (standard deviation). ES = erector spinae, GM = gluteus maximus, VM = vastus medialis, VL = vastus lateralis, BF = biceps femoris, ST = semitendinosus, GL = gastrocnemius lateralis, TA = tibialis anterior; S: Cwall at the scapular zone, P: Cwall at the pelvic zone, R: CGR at rearfoot, F: CGR at forefoot.
The EMG activity of GM displayed the same significant main effects and interactions as those of the ES. However, in any exercise condition, the level of GM activity was always too low (less than 10% MVIC) to be of clinical relevance.
3.2. Vastus Medialis and Vastus Lateralis
The activity of VM and VL was significantly affected by Cwall and CGR, and by the interaction between d and Cwall (Table 2). VL activity was also significantly influenced by the interaction between Cwall and CGR. Post hoc comparison (Table 3) highlighted that the shift in CGR from forefoot to rearfoot increased significantly the VM and VL activity, independently of the conditions imposed on d and Cwall (p < 10−3). VM and VL activity also significantly increased shifting Cwall from the scapular to the pelvic zone when (with CGR either at rearfoot or forefoot). Among the different exercise conditions, VM and VL reached a maximum activity of 23% and 27% MVIC, respectively (Figure 2, Table 4).
3.3. Semitendinosus and Bicep Femoris
The mean ST activity was significantly affected by all exercise variables and interactions between pairs of variables (Table 2). Post hoc comparison (Table 3) highlighted that the ST activity increased significantly by (1) shifting CGR from rearfoot to forefoot when (with Cwall at either the scapular or pelvic zone) and when with Cwall at the scapular zone; (2) increasing d with CGR at the forefoot (with Cwall either at the scapular or pelvic zone); (3) shifting Cwall from the pelvic to scapular the zone when (with CGR at either at rearfoot or forefoot), and when with CGR at the forefoot. The ST activity reached an activation level higher than 10% MVIC only at the exercise condition (, Cwall at scapular zone, and CGR at forefoot) that maximised the ES activity (Figure 2, Table 4).
The EMG activity of BF was significantly affected by all exercise variables and by the interaction between d and CGR. However, in all exercise conditions, the level of BF activity was lower than 10% MVIC.
3.4. Tibialis Anterior and Gastrocnemius Lateralis
The activities of the TB and GL were significantly affected by d and CGR and by the interaction between these two factors (Table 2). Post hoc comparison (Table 3) indicated that shifting CGR from forefoot to rearfoot increased the TA activity (p < 10−3) while decreasing the GL activity (p ≤ 0.01) in all exercise conditions (for all the four combinations of the d and Cwall variables). The effect of changing d was significant only with CGR at the rearfoot for the TA, and with CGR at the forefoot for the GL (independently of the shift in Cwall between the pelvic and scapular zone). The TA muscle reached the highest level of EMG activity, compared with all other muscles (Figure 2, Table 4). This maximum level (44% MVIC) was achieved for , Cwall at the scapular zone and CGR at rearfoot. The maximum EMG level reached by the GL was less than half (17% MVIC) of that of the TA, and it was reached for , Cwall at the scapular zone, and CGR at the forefoot.
4. Discussion
We recorded and analysed the electromyographic activity of lower limb and lumbar muscles during static body-weight wall-squat exercises executed with knees flexed at 45°. The results highlight that muscle activity can be finely modulated by manipulating three different exercise variables: the distance (d) of the ankles from the wall; the voluntary shift between the scapular and pelvic zone of the centre of pressure (Cwall) of the force exerted by the wall on the back; the voluntary shift between the rearfoot and forefoot of the centre of pressure (CGR) of the ground reaction force.
This study highlights that the VM and VL activity can be considerably increased (up to nearly 100%) by the shift in CGR from forefoot to rearfoot, independently of the values of the other variables. The effect size of the CGR variable on the quadriceps () is at least two times higher than that of the other variables and the variables tested by Blanpied during the dynamic wall-squat exercise [7]. The VM and VL reach levels of activation up to about 25% MVIC, which can be considered effective in the initial phase of a quadriceps strengthening intervention for knee rehabilitating patients. In the following phase, the demand of knee-extensor muscle torque and the quadriceps activity can be progressively enhanced by gradually increasing the knee flexion angle from the value (45°) selected in this study [14]. However, a parallel increase in the tibiofemoral and patellofemoral compressive forces also occurs. Actually, a knee flexion angle of 45° allows the minimisation of the tibiofemoral and patellofemoral compressive forces in absence of ACL-loading tibiofemoral shear forces, which may occur in the final 40–45° range of knee extension [9,14,22,23,24,25]. Ultimately, for patients with quadriceps weakness and inhibition secondary to a knee injury, we suggest the use of the SBWS executed with and CGR shifted at the rearfoot because it can lead to enough quadriceps muscle activation for muscle strengthening purposes while minimising the mechanical loading on the knee joint structures. It is worth noting that, given its joint-safety attributes, this exercise can be used in the early stage of rehabilitation programmes as soon as the patient can tolerate partial weight-bearing.
Notably, within the different exercise configurations, the TA reached the highest level of activation (about 44% MVIC) among the eight selected muscles. This level was achieved with Cwall shifted at the scapular zone, CGR at the rearfoot, and the foot placed near the wall (). This result is in line with our previous study [14], which, based on biomechanical modelling and force plate measurements, highlighted that the SBWS can impose high torque demand on the ankle dorsiflexor muscles. The present study definitively confirms that the SBWS may enable effective strengthening of the TA, using body weight as the sole resistance while imposing low stability and balance demand due to the wall support.
The activity of the muscles of the rear part of the body (ES, GM, BF, ST, and GL) was maximised in the same exercise condition: feet placed far from the wall (), Cwall shifted at the scapular zone, and CGR shifted at the forefoot. However, even in this favourable condition, the GM, BF, and ST reached limited levels of activity given by 6%, 6%, and 10%, respectively. For this reason, the SBWS exercise with the knee at 45° of flexion cannot be considered effective for hamstring and glute strengthening. In contrast, the GL and ES activity reached levels of 17% and 23% MVIC, respectively. Thus, the SBWS exercise can potentially be used as a safe initial intervention in patients with limited muscle endurance in low back muscles, prior to the execution of more challenging exercises, such as the body-weight supine bridge exercise [26,27,28,29,30,31].
The shift in the centre of pressure CGR of the ground reaction force between rearfoot and forefoot significantly affected the activity of all selected muscles. Overall, this variable had a dominant impact over the muscle activity, compared with the other two variables (Figure 2, Table 2 and Table 3). The effect of the CGR shift was particularly important for muscles (VM, VL, TA, ES, and GL) that reached considerable levels of activity, which may be identified as the target muscles of the exercise. Ultimately, this study highlights that the shift in CGR between rearfoot and forefoot constitutes a relevant variant of the SBWS exercise.
Interestingly, post hoc analysis revealed that the shift in Cwall between the scapular and the pelvic zone did not significantly change the activity of any muscle when the feet were placed near the wall and CGR was shifted to the rearfoot (Table 3). In this condition, CGR is located near the wall and the horizontal distance between the body’s centre of mass, and CGR is minimised. This, in turn, minimises the tendency of gravity to rotate the entire body backward and, consequently, the magnitude of the equilibrating force the wall should exert on the back. Ultimately, this limits the effects of the Cwall shift. On the contrary, this shift induces its greatest effects when the distance of CGR from the wall is maximised, that is, when and CGR shifted at the forefoot.
The main limitation of the study is related to the limited number of conditions imposed on the exercise variables. In fact, only two conditions were selected for each variable ( or ; CGR shifted at rearfoot or forefoot, Cwall shifted at the pelvic or scapular zone). However, for each variable, the two selected conditions constitute appropriate boundaries that enclose the natural range of the variable variation. For example, a d distance slightly lower than with the knee flexed at 45° was not accessible to all participants due to the lack of necessary ankle dorsiflexion mobility. Likewise, a distance d slightly greater than caused limited stability between the foot and the ground (with a marked tendency of the foot to slide forward) in some participants. The boundary values of the variables are also the most appropriate in order to identify the conditions that maximise muscle activity and to determine these maximum levels.
Another limitation is related to the postural position maintained during the exercise. All participants reported a clear self-perception of their ability to shift Cwall between the scapular and the gluteal zone and CGR between the rearfoot and forefoot while maintaining a static wall-squat position with neutral spine alignment [32], vertical trunk orientation, and the whole foot plant on the ground. The posture that participants assumed during the exercise was carefully controlled by the investigators, even though the forward tilt angle of the pelvis was not precisely determined. Critically, this angle can influence the degree of lumbar lordosis and muscle activity in the lower back and lower limbs. Further research is, therefore, needed to investigate the effect of this variable.
A further limitation stems from the fact that the exact position of Cwall and CGR during the trials was not measured experimentally. This would have required the use of force platforms placed under each foot and on the wall supporting the back. Shifts in Cwall and CGR were voluntarily performed and freely controlled by the participants without the use of any feedback signal. Aside from the lack of this information in the present study, our experimental setup may be useful to therapists working in rehabilitation environments that are not equipped with technologically advanced devices.
5. Conclusions
We analysed the electromyographic activity of lower limb and lumbar muscles during the SBWS with knees flexed at 45° by manipulating three different variables: horizontal distance of the ankles from the wall; scapular or pelvic location of the centre of pressure of the force exerted by the wall on the back; rearfoot or forefoot location of the centre of pressure of the ground reaction force. The exercise configurations that maximise the activity of each muscle were identified, together with the corresponding level of maximum muscle activity. The study results highlight that the SBWS leads to quadriceps, tibialis anterior, and lumbar muscles activation levels that can improve muscle strength in the early phase of rehabilitation interventions as soon as the patient can tolerate partial weight-bearing. Therefore, we suggest that the exercise could be suitable for patients having low back pain, with limited lumbar muscle endurance or quadriceps weakness and inhibition secondary to a knee injury.
Author Contributions
Conceptualisation, A.B., C.V.D., R.P. and S.C.; methodology, A.B., R.L. and S.C.; software, A.B. and R.L.; validation, A.B., C.V.D., R.P. and S.C.; formal analysis, A.B., R.P. and S.C.; investigation, A.B. and R.L.; resources, A.B.; data curation, A.B. and R.L.; writing—original draft preparation, A.B.; writing—review and editing, C.V.D., R.P. and S.C.; visualisation, A.B.; supervision, A.B., C.V.D., R.P. and S.C.; project administration, A.B. and R.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of the University of Perugia (Protocol Code n.3/2022, 15 February 2022).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kisner, C.; Colby, L. Therapeutic Exercise: Foundations and Techniques, 6th ed.; F.A. Davis Company: Philadelphia, PA, USA, 2012; p. 836. [Google Scholar]
- Heckmann, T.P.; Barber-Westin, S.D.; Noyes, F.R. Meniscal repair and transplantation: Indications, techniques, rehabilitation, and clinical outcome. J. Orthop. Sports Phys. Ther. 2006, 36, 795–814. [Google Scholar] [CrossRef] [PubMed]
- Cho, M. The effects of modified wall squat exercises on average adults’ deep abdominal muscle thickness and lumbar stability. J. Phys. Ther. Sci. 2013, 25, 689–692. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, Y. The influence of unstable modified wall squat exercises on the posture of female university students. J. Phys. Ther. Sci. 2015, 27, 2477–2480. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morrow, J.; Disch, J.; Jackson, A.; Mood, D. Measurement and Evaluation in Human Performance, 4th ed.; Human Kinetics: Champaign, IL, USA, 2011. [Google Scholar]
- Lubans, R.D.; Morgan, P.; Callister, R.; Plotnikoff, R.C.; Eather, N.; Riley, N.; Smith, C.J. Test-retest reliability of a battery of field-based health-related fitness measures for adolescents. J. Sports Sci. 2011, 29, 685–693. [Google Scholar] [CrossRef] [PubMed]
- Blanpied, P. Changes in Muscle Activation During Wall Slides and Squat-Machine Exercise. J. Sport Rehabil. 1999, 8, 123–134. [Google Scholar] [CrossRef]
- Shelburne, K.B.; Pandy, M.G. A musculoskeletal model of the knee for evaluating ligament forces during isometric contractions. J. Biomech. 1997, 30, 163–176. [Google Scholar] [CrossRef]
- Pandy, M.G.; Shelburne, K.B. Dependence of cruciate-ligament loading on muscle forces and external load. J. Biomech. 1997, 30, 1015–1024. [Google Scholar] [CrossRef]
- Shelburne, K.B.; Pandy, M.G. Determinants of cruciate-ligament loading during rehabilitation exercise. Clin. Biomech. 1998, 13, 403–413. [Google Scholar] [CrossRef]
- Zheng, N.; Fleisig, G.S.; Escamilla, R.F.; Barrentine, S.W. An analytical model of the knee for estimation of internal forces during exercise. J. Biomech. 1998, 31, 963–967. [Google Scholar] [CrossRef]
- Escamilla, R.F.; Macleod, T.D.; Wilk, K.E.; Paulos, L.; Andrews, J.R. Cruciate ligament loading during common knee rehabilitation exercises. Proc. Inst. Mech. Eng. Part H 2012, 226, 670–680. [Google Scholar] [CrossRef]
- Biscarini, A.; Contemori, S.; Busti, D.; Botti, F.M.; Pettorossi, V.E. Knee flexion with quadriceps cocontraction: A new therapeutic exercise for the early stage of ACL rehabilitation. J. Biomech. 2016, 49, 3855–3860. [Google Scholar] [CrossRef] [PubMed]
- Biscarini, A.; Contemori, S.; Dieni, C.V.; Panichi, R. Joint Torques and Tibiofemoral Joint Reaction Force in the Bodyweight “Wall Squat” Therapeutic Exercise. Appl. Sci. 2020, 10, 3019. [Google Scholar] [CrossRef]
- Escamilla, R.F.; Zheng, N.; Macleod, T.D.; Edwards, W.B.; Imamura, R.; Hreljac, A.; Fleisig, G.S.; Wilk, K.E.; Moorman, C.T.; Andrews, J.R. Patellofemoral joint force and stress during the wall squat and one-leg squat. Med. Sci. Sports Exerc. 2009, 41, 879–888. [Google Scholar] [CrossRef] [PubMed]
- Escamilla, R.F.; Fleisig, G.S.; Zheng, N.; Barrentine, S.W.; Wilk, K.E.; Andrews, J.R. Biomechanics of the knee during closed kinetic chain and open kinetic chain exercises. Med. Sci. Sports Exerc. 1998, 30, 556–569. [Google Scholar] [CrossRef]
- Biscarini, A.; Benvenuti, P.; Botti, F.M.; Mastrandrea, F.; Zanuso, S. Modelling the joint torques and loadings during squatting at the Smith machine. J. Sports Sci. 2011, 29, 457–469. [Google Scholar] [CrossRef]
- Biscarini, A.; Botti, F.M.; Pettorossi, V.E. Selective contribution of each hamstring muscle to anterior cruciate ligament protection and tibiofemoral joint stability in leg-extension exercise: A simulation study. Eur. J. Appl. Physiol. 2013, 113, 2263–2273. [Google Scholar] [CrossRef]
- Neumann, D.A. Kinesiology of the Musculoskeletal System, 2nd ed.; Mosby: St. Louis, MO, USA, 2010. [Google Scholar]
- Konrad, P. The ABC of EMG. A Practical Introduction to Kinesiological Electromyography; Noraxon Inc.: Scottsdale, AZ, USA, 2006. [Google Scholar]
- Biscarini, A.; Benvenuti, P.; Botti, F.M.; Brunetti, A.; Brunetti, O.; Pettorossi, V.E. Voluntary enhanced cocontraction of hamstring muscles during open kinetic chain leg extension exercise: Its potential unloading effect on the anterior cruciate ligament. Am. J. Sports Med. 2014, 42, 2103–2112. [Google Scholar] [CrossRef]
- Butler, D.L.; Noyes, F.R.; Grood, E.S. Ligamentous restraints to anterior-posterior drawer in the human knee: A biomechanical study. J. Bone Jt. Surg. 1980, 62, 259–270. [Google Scholar] [CrossRef]
- Smidt, G.L. Biomechanical analysis of knee flexion and extension. J. Biomech. 1973, 6, 79–92. [Google Scholar] [CrossRef]
- Wilk, K.E.; Escamilla, R.F.; Fleisig, G.S.; Barrentine, S.W.; Andrews, J.R.; Boyd, M.L. A comparison of tibiofemoral joint forces and electromyographic activity during open and closed kinetic chain exercises. Am. J. Sports Med. 1996, 24, 518–527. [Google Scholar] [CrossRef]
- Kaufman, K.R.; An, K.N.; Litchy, W.J.; Morrey, B.F.; Chao, E.Y. Dynamic joint forces during knee isokinetic exercise. Am. J. Sports Med. 1991, 19, 305–316. [Google Scholar] [CrossRef] [PubMed]
- McGill, S.M. Low back exercises: Evidence for improving exercise regimens. Phys. Ther. 1998, 78, 754–765. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ekstrom, R.A.; Donatelli, R.A.; Carp, K.C. Electromyographic analysis of core trunk, hip, and thigh muscles during 9 rehabilitation exercises. J. Orthop. Sports Phys. Ther. 2007, 37, 754–762. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schellenberg, K.L.; Lang, J.M.; Chan, K.M.; Burnham, R.S. A clinical tool for office assessment of lumbar spine stabilization endurance: Prone and supine bridge maneuvers. Am. J. Phys. Med. Rehabil. 2007, 86, 380–386. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Okubo, Y.; Kaneoka, K.; Imai, A.; Shiina, I.; Tatsumura, M.; Izumi, S.; Miyakawa, S. Electromyographic analysis of transversus abdominis and lumbar multifidus using wire electrodes during lumbar stabilization exercises. J. Orthop. Sports Phys. Ther. 2010, 40, 743–750. [Google Scholar] [CrossRef] [Green Version]
- Hadała, M.; Gryckiewicz, S. The effectiveness of lumbar extensor training: Local stabilization or dynamic strengthening exercises. A review of literature. Ortop. Traumatol. Rehabil. 2014, 16, 561–572. [Google Scholar] [CrossRef]
- Biscarini, A.; Busti, D.; Calandra, A.; Contemori, S. The “supine bridge” therapeutic exercise: Determination of joint torques by means of biomechanical modelling and technologies. J. Mech. Med. Biol. 2017, 17, 1750104-1–1750104-16. [Google Scholar] [CrossRef]
- Panjabi, M.M. The stabilizing system of the spine. Part II. Neutral zone and instability hypothesis. J. Spinal Disord. 1992, 5, 390–396. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).