Abstract
Neck pain is defined as perceived pain, originating in an area bounded above by the nuchal line, below by an imaginary line passing through the spinous process of T1 and laterally by the sagittal plane tangent to the lateral edges of the neck. Our purpose is to investigate the effectiveness of transcutaneous electrical nerve stimulation (TENS) in patients suffering from both acute and chronic cervical pain syndromes. The literature research was conducted by consulting the following databases: PubMed, PEDro, Cochrane, and Google Scholar. To formulate the scientific question correctly, the PICO model was used. This umbrella review includes all systematic reviews with or without meta-analysis, in English, which analyze the use of TENS in subjects suffering from acute or chronic cervical pain. To evaluate the methodological quality of the studies, the AMSTAR model. A total of eleven systematic reviews with or without meta-analyses were included. The results of the study show how TENS seems to have an effect in reducing the intensity of acute and chronic cervical pain, especially in the short term. However, it was not possible to provide precise recommendations in this regard. Based on our result, it is desirable to carry out further studies that support the effectiveness of using TENS in patients suffering from acute and chronic neck pain.
1. Introduction
Neck pain is defined as “perceived pain, originating in an area bounded above by the nuchal line, below by an imaginary line passing through the spinous process of T1 and laterally by the sagittal planes tangent to the lateral edges of the neck” [,,]. It affects approximately 30–50% of the general population each year, constituting the 4% of causes of patients referring to Italian Physical Medicine and Rehabilitation (PRM) outpatients []. The course is generally benign and acute episodes tend to resolve spontaneously within a few weeks. Relapses are frequent but in 10% of cases the symptoms tend to become chronic []. This pathology has a strong impact in the workplace as 11–14% of workers encounter a limitation of work activities [,]. The multifactorial etiology includes non-modifiable factors (age, sex, familiarity, general health conditions, previous traumatic outcomes) and modifiable (postural, behavioral, psychosocial) factors. Often the cause is not identifiable, and we tend to attribute a dysfunctional origin to the onset of pain (“non-specific” or “common” neck pain), which includes inflammatory, muscular, biomechanical, postural, and neurological components [,]. Joint facets are a potential source of axial and peripheral pain. Facet joint pain has a prevalence of 54% to 67% in patients treated for neck pain. Furthermore, facet spondylosis has been associated with cervical radiculopathy and facet joint osteoarthritis accounts for up to 45% of chronic low back pain cases [,,]. The main symptoms are pain, stiffness, reflex contracture of the cervical muscles, limitation of the cervical range of motion (ROM), irradiation to the upper limbs, increased fatigue, dizziness, and headache. Symptoms are often accompanied by visual and auditory disturbances, sleep disturbances, cognitive, and emotional problems (anxiety and depression) []. Several treatments have been proposed for cervical pain, including pharmacological therapies (e.g., nonsteroidal anti-inflammatory drugs, paracetamol, steroids, opioids, tramadol, muscle relaxants, psychotropics, anxiolytics, and hypnotics) and other conservative approaches, as the oxygen–ozone therapy []. In the rehabilitation process, physiotherapy treatment and instrumental physical therapies are commonly used. Among the latter, the transcutaneous electrical nerve stimulation (TENS) has the greatest evidence of efficacy in the treatment of neck pain (chemical effect, vasodilation, analgesic effect, and thermal effect) and it is the most widely used analgesic electrotherapy (symmetrical or asymmetrical rectangular waves, spike, continuous, or packet-burst). The TENS impulses, due to their short duration, are able to selectively activate the A beta fibers and block nociceptive impulses through the Gate-Control mechanism [].
The aim of our article was to investigate the effectiveness of TENS in patients suffering from both acute and chronic cervical pain syndromes.
2. Materials and Methods
2.1. Research Strategy
The literature search for articles published in the last 20 years was conducted by consulting the following databases: PubMed, PEDro, Cochrane, and Google Scholar. The keywords used were “TENS”, “electrotherapy”, “neck pain”, “myofascial pain syndrome”, “upper trapezius myalgia”, and “mechanical neck dis-orders”. The following mesh terms were used for the research: TENS AND/OR neck pain AND/OR myofascial pain syndrome, electrotherapy AND/OR mechanical neck disorders AND/OR upper trapezius myalgia. The titles and abstracts of the initially identified studies were selected, and then the full text of the potential articles eligible for the study.
2.2. P.I.C.O.
To formulate the scientific question correctly, the PICO model was used: Population: Patients with acute or chronic cervical pain syndrome, whether of mechanical, myofascial, or other origin; Intervention: TENS; Comparison: Comparison with conventional therapies or with other methods applied individually or combined with TENS; Outcome: Pain, disability, and function [].
2.3. Inclusion/Exclusion Criteria
This umbrella review includes all systematic reviews with or without meta-analysis, in English, which analyze the use of TENS in subjects suffering from acute or chronic cervical pain, published in the last 20 years. Studies with an AMSTAR score of less than 6 were excluded [].
2.4. Quality of Study Evaluation
To evaluate the methodological quality of the studies, the AMSTAR model (Assessment of Multiple Systematic Review) was used, which is a checklist consisting of 11 items to which you can answer “Yes”, “No”, “You cannot answer”, or “Not applicable”. Each item is assigned a score of 1 if the answer is “Yes”, while the score is null if all the other answers are given. The AMSTAR model characterizes the quality of the systematic review at three levels: Low quality score 0–3, medium quality score 4–7, high quality score 8–11 [].
3. Results
A total of 11 systematic reviews with or without meta-analyzes were included (1 acute neck pain; 6 chronic neck pain; 4 acute and chronic neck pain) (Figure 1) [,,,,,,,,,,].
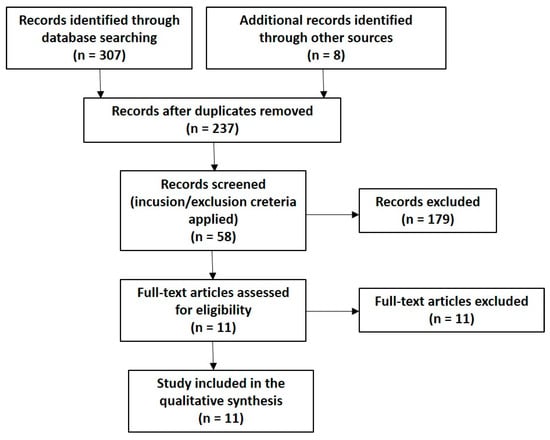
Figure 1.
Flow chart.
Among the systematic reviews (SR) included, there is not a complete homogeneity. Some of them include studies that do not specifically treat TENS in acute or chronic neck pain, but also analyze other rehabilitation approaches in other areas of the body. In these cases, in the discussion of the results, the data relating to the individual RCTs reported in the reference review were extrapolated. It was decided to distinguish the systematic reviews in which TENS is treated not specifically (Table 1) from those in which TENS is always reported in relation to neck pain (Table 2). Table 3 shows the methodological quality of the included reviews, assessed according to the Amstar criteria, while Table 4 shows the main TENS and treatment parameters used in the included articles.

Table 1.
Characteristics of the systematic reviews (SR) included in which few studies speak of transcutaneous electrical nerve stimulation (TENS).

Table 2.
Characteristics of the systematic reviews (SR) included in which few studies speak of TENS.

Table 3.
Methodological quality of the included studies.

Table 4.
Main parameters of TENS and treatment used in included RS.
The systematic review of Vemon et al. [] includes four studies, only one [] dealing with TENS, used as a comparator treatment. The group that received TENS had a significant reduction in pain 3 weeks after the end of the rehabilitation program. In the study by Haines et al. [], the efficacy of TENS is included in a multimodal comparison treatment [], which did not demonstrate significant differences between the experimental and control groups, both as regards pain and general function.
The systematic review by Rickards [] demonstrates that TENS appears to have an immediate effect in reducing the intensity of myofascial pain in the neck and upper back, however, there are insufficient data to determine the efficacy of TENS beyond immediate post treatment.
Leaver et al. [] compare two types of TENS (conventional and ENAR TENS) with the “sham TENS” and demonstrate the absence of significant differences between the experimental groups and the control group regarding pain and disability, in each time period reported [short, medium, and long term].
In the study by Alexandre Mauricio Passos Nunes et al. [], only one RCT [] analyzes TENS and demonstrates its greater efficacy in reducing pain symptoms compared to stretching exercises, however, it does not report important clinical differences regarding pain reduction in the short term.
Kroeling et al. [] affirm that the treatment with TENS is lacking and limited conflicting, so no definitive statements can be issued regarding the efficacy of TENS in mechanical disorders of the cervical spine.
In the systematic review by Damgaard et al. [], 42 RCTs were included, involving a total of 3919 subjects. TENS is discussed in one study characterized by low risk of bias [] and in two characterized by high risk of bias [,]. TENS appears to have effects on pain in patients with chronic nonspecific neck pain, however there is no evidence for the application of a specific physiotherapy modality in a specific subgroup of patients.
Of the 9 studies included in the review by Resende et al. [], only one analyzes TENS in relation to chronic neck pain [], the latter compares three types of TENS (H-TEMS, L-TENS, BURST-TENS) with placebo and shows the lack of significant differences between the various treatment groups both as regards pain and secondary outcomes.
In the review by Gross et al. [], 5 RCTs [,,,,] state that in patients suffering from chronic headache of cervicogenic origin, TENS appears to be less effective than cervical manipulation in reducing pain in the short term. In patients suffering from subacute and chronic neck pain, TENS appears to produce the same effects as cervical mobilization with regard to the improvement of pain, function, quality of life, and patient satisfaction up to an intermediate follow-up period. The systematic review by Kroeling et al. [] demonstrates that in patients with acute and chronic neck pain, TENS may be more effective in pain relief than EMS and placebo, but not as effective as therapeutic exercise, infrared radiation, manual therapy, or ultrasound. No additional benefits have been shown when TENS is combined with other therapies such as infrareds, therapeutic exercise, hot packs, or a combination of neck collar, therapeutic exercise, and dressings. In patients with myofascial neck pain, TENS appears to reduce pain better than placebo. However, it is not possible to issue definitive declarations on the efficacy of TENS and its clinical use in cervical pain. Martimbianco et al. [] show that there are no substantial differences between all the types of TENS used in the study and the sham TENS, especially in the short term. When compared with other interventions, the latter appear to be more effective in pain reduction, but without significant differences with respect to all other outcomes.
4. Discussion
Neck pain has a multifactorial etiology. The precise identification of the structure causing the pain is very difficult, not only because the various structures are innervated by several segments, but also because facilitation-convergence and sensitization mechanisms favor the phenomenon of referred pain []. Psycho-social factors are frequently found in subjects with persistent pain and judged responsible for a reduction in the pain threshold, which is why, given the current conception of cervical pain, it is recommended to consider the bio-psycho-social unity of the subject with neck pain, paying attention not only to the clinical aspects (severity and duration), but also to the personal, cultural, and social (environmental) dimensions that characterize the patient, as well as to the impact of the problem on daily life activities [,]. The presence of numerous visceral and nervous structures requires careful collection of information in order to exclude the presence of “red flags”, or signs and symptoms attributable to the presence of other pathologies, which can cause symptoms similar to that of neck pain [,]. In the presence of chronic musculoskeletal pain, both alterations in the processing of information by the central nervous system and an increased reactivity of central neurons were found, all of which predisposes to central pain sensitization; in this condition each new peripheral lesion can become a new source of nociceptive input that maintains or aggravates the painful condition [,]. The pathophysiological mechanisms underlying most conditions associated with chronic pain are still unclear. In 90% of cases, however, the disorder is non-specific; only in 0.4% is it related to serious pathologies and in 3% to fractures derived from trauma. In case of referred pain, distant from the cervical region, the presence of irradiated symptoms must be assumed []. Muscles are also able to cause the onset of pain in areas distant from the cervical region, due to the presence of trigger points. The trigger point is a relatively small, contracted nodular type tissue modification, which is located within a taut band of a muscle fiber, it is quite sensitive to touch and can generate pain locally and in distant areas called target areas. Trigger points can be both active and latent; primary if they concern the muscle directly subjected to overload, or secondary if activated in a distant muscle. The muscles that most frequently develop trigger points are the trapezius, the sternocleido-mastoid, the sub-occipital muscles, the spleni, and the levator scapula []. A further cause of neck pain can be facet joint syndrome, which can affect the cervical or lumbar spine. The articular facets are vertebral bone structures that have the function of connecting the vertebrae to each other allowing the movements of the spine [,]. When joint damage occurs as a result of trauma or arthritic phenomena, pain occurs. The mechanism of onset is due to the cartilage damage that causes a “rubbing” between the two bone surfaces, with consequent inflammation; this in turn can lead to the formation of osteophytes. The same physiological deterioration of cartilage, which occurs with advancing age, can irritate the nerves that innervate the facet joints, thus contributing to the onset of pain [,,].
The 11 systematic reviews included in the umbrella review show that TENS is able to reduce pain but does not appear to be more effective than other routinely used therapies. Some studies shown that TENS is effective in managing neck pain, but only in the short term. TENS showed no lasting effects over time. One review [] provides inconclusive evidence of the benefit of TENS in patients suffering from chronic neck pain due to the low quality of the studies and the heterogeneity of the same.
The studies show that no type of TENS application prevails over the others, moreover, when administered together with other therapies, it does not bring further benefits. Furthermore, when the administration of TENS is administered together with another intervention, it does not seem to show substantial differences with the comparison group in all the outcomes considered, both in the short and in the medium term.
All patients who underwent TENS were suffering from acute or chronic neck pain with mechanical, myofascial, and traumatic (whiplash’s syndrome) etiology. TENS is one of the possible therapeutic strategies that can be proposed to the patient with acute or chronic cervical pain, although it is not the therapy that allows us to achieve the best results.
Eight systematic reviews analyze the frequency parameter, and most of them use values included in the range from 2 to 100 Hz [,,,,,]. The two extremes of this range represent the frequencies, respectively, used in the endorphinic TENS (1–5 Hz) and in the conventional TENS (60–100 Hz), that is the two most used modalities of application in clinical practice.
The data reported regarding the current intensity are lacking and inaccurate, and none of the revisions reports specific intensity values, thus limiting the search for the most suitable current intensity value for the treatment of patients with acute or chronic neck pain.
The duration of the pulse was in the range 40 µs–250 µs [,,,,]. The extremes of this range represent, again, the pulse duration values usually used, respectively, in the endorphinic TENS (<60 µs) and in the conventional TENS (>60 µs).
The duration of the single session, in most of the studies, varies from 10 to 30 min, while the duration of the entire treatment program is usually between 2 and 6 weeks. Further studies are needed to define more precisely the duration of the treatment.
Some studies carry out the follow-up evaluation up to 6 months later [,,,], others at 3 months [,], others still carry out it immediately after treatment [] or up to 12 months after the end of the therapeutic program [].
The positioning of the electrodes represents therapeutic information often neglected in the various reviews; despite this it is good practice that they are placed on the painful region. There is very low-quality evidence that demonstrates the efficacy of TENS in chronic pain in the trapezius muscle.
The heterogeneity of the rehabilitation protocols used during the development of the studies remains a fundamental problem to standardize and protocol the rehabilitation treatment.
Implications for Future Research and Clinical Practice
It is important to seek clear scientific evidence and high-level recommendations due to their relevance in clinical practice. The main limitation of the study is due to the excessive heterogeneity of the studies, especially in relation to the different methods and rehabilitation protocols in patients suffering from acute and chronic neck pain.
5. Conclusions
Taken together, results of this umbrella review of systematic reviews show how TENS seems to have an effect in reducing the intensity of acute and chronic cervical pain, especially in the short term. However, it was not possible to provide precise recommendations in this regard. Based on our result, it is desirable to carry out further studies that support the effectiveness of using TENS in patients suffering from acute and chronic neck pain.
Author Contributions
Conceptualization, T.P. and R.S.; methodology, F.A. and A.d.S.; software, M.M.; validation, M.P. (Marco Paoloni), M.P. (Mirko Pesce) and A.B.; formal analysis, L.R.; investigation, S.V.; resources, T.P.; data curation, M.M.; writing—original draft preparation, F.A.; writing—review and editing, S.V., F.A., and L.R., A.d.S.; visualization, T.P.; supervision, R.S.; project administration, M.M.; funding acquisition, none. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not Applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No data are reported.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Cohen, S.P. Epidemiology, Diagnosis, and Treatment of Neck Pain. Mayo Clin. Proc. 2015, 90, 284–299. [Google Scholar] [CrossRef] [PubMed]
- Mangone, M.; Paoloni, M.; Procopio, S.; Venditto, T.; Zucchi, B.; Santilli, V.; Paolucci, T.; Agostini, F.; Bernetti, A. Sagittal spinal alignment in patients with ankylosing spondylitis by rasterstereographic back shape analysis: An observational retrospective study. Eur. J. Phys. Rehabil. Med. 2020, 56, 191–196. [Google Scholar] [CrossRef]
- Mangone, M.; Bernetti, A.; Agostini, F.; Paoloni, M.; De Cicco, F.A.; Capobianco, S.V.; Bai, A.V.; Bonifacino, A.; Santilli, V.; Paolucci, T. Changes in Spine Alignment and Postural Balance After Breast Cancer Surgery: A Rehabilitative Point of View. Biores Open Access 2019, 8, 121–128. [Google Scholar] [CrossRef] [PubMed]
- Gimigliano, F.; De Sire, A.; Gastaldo, M.; Maghini, I.; Paoletta, M.; Pasquini, A.; Boldrini, P.; Selb, M.; Prodinger, B.; SIMFER Residents Section Group. Use of the International Classification of Functioning, Disability and Health Generic-30 Set for the characterization of outpatients: Italian Society of Physical and Rehabilitative Medicine Residents Section Project. Eur. J. Phys. Rehabil. Med. 2019, 55, 258–264. [Google Scholar] [CrossRef] [PubMed]
- Bernetti, A.; Agostini, F.; De Sire, A.; Mangone, M.; Tognolo, L.; Di Cesare, A.; Ruiu, P.; Paolucci, T.; Invernizzi, M.; Paoloni, M. Neuropathic Pain and Rehabilitation: A Systematic Review of International Guidelines. Diagnostics 2021, 11, 74. [Google Scholar] [CrossRef] [PubMed]
- Côté, P.; Cassidy, D.J.; Carroll, L.J.; Kristman, V. The annual incidence and course of neck pain in the general population: A population-based cohort study. Pain 2004, 112, 267–273. [Google Scholar] [CrossRef] [PubMed]
- Damiani, C.; Mangone, M.; Paoloni, M.; Goffredo, M.; Franceschini, M.; Servidio, M.; Pournajaf, S.; Santilli, V.; Agostini, F.; Bernetti, A. Trade-Offs with rehabilitation Effectiveness (REs) and Efficiency (REy) in a sample of Italian disabled persons in a in post-acuity rehabilitation unit. Ann. Ig. 2020, 32, 327–335. [Google Scholar] [PubMed]
- Liu, R.; Kurihara, C.; Tsai, H.T.; Silvestri, P.J.; Bennett, M.I.; Pasquina, P.F.; Cohen, S.P. Classification and Treatment of Chronic Neck Pain: A Longitudinal Cohort Study. Reg. Anesth. Pain Med. 2017, 42, 52–61. [Google Scholar] [CrossRef] [PubMed]
- Seccia, R.; Boresta, M.; Fusco, F.; Tronci, E.; Di Gemma, E.; Palagi, L.; Mangone, M.; Agostini, F.; Bernetti, A.; Santilli, V.; et al. Data of patients undergoing rehabilitation programs. Data Brief. 2020, 30, 105419. [Google Scholar] [CrossRef]
- Montemurro, N.; Perrini, P.; Mangini, V.; Galli, M.; Papini, A. The Y-shaped trabecular bone structure in the odontoid process of the axis: A CT scan study in 54 healthy subjects and biomechanical considerations. J. Neurosurg. Spine 2019, 30, 585–592. [Google Scholar] [CrossRef] [PubMed]
- Jaumard, N.V.; Udupa, J.K.; Welch, W.C.; Winkelstein, B.A. Kinematic magnetic resonance imaging to define the cervical facet joint space for the spine in neutral and torsion. Spine 2014, 39, 664–672. [Google Scholar] [CrossRef] [PubMed]
- Cavanaugh, J.M.; Lu, Y.; Chen, C.; Kallakuri, S. Pain generation in lumbar and cervical facet joints. J. Bone Joint. Surg Am. 2006, 88 (Suppl. 2), 63–67. [Google Scholar] [PubMed]
- Masiero, S.; Litwocenko, S.; Agostini, F.; On behalf section of Rehabilitation in Environ-mental Thermal for Italian Society of Physical Medicine and Rehabilitation. Rehabilitation in an Italian thermal setting: A new therapeutic strategy for patients with musculoskeletal disability-the results of an Italian survey. Int. J. Biometeorol. 2020, 64, 951–954. [Google Scholar] [CrossRef] [PubMed]
- de Sire, A.; Agostini, F.; Lippi, L.; Mangone, M.; Marchese, S.; Cisari, C.; Bernetti, A.; Invernizzi, M. Oxygen-Ozone Therapy in the Rehabilitation Field: State of the Art on Mechanisms of Action, Safety and Effectiveness in Patients with Musculoskeletal Disorders. Biomolecules 2021, 11, 356. [Google Scholar] [CrossRef] [PubMed]
- Paolucci, T.; Cardarola, A.; Colonnelli, P.; Ferracuti, G.; Gonnella, R.; Murgia, M.; Santilli, V.; Paoloni, M.; Bernetti, A.; Agostini, F.; et al. Give me a kiss! An integrative rehabilitative training program with motor imagery and mirror therapy for recovery of facial palsy. Eur. J. Phys. Rehabil. Med. 2020, 56, 58–67. [Google Scholar] [CrossRef] [PubMed]
- Methley, A.M.; Campbell, S.; Chew-Graham, C.; McNally, R.; Cheraghi-Sohi, S. PICO, PICOS and SPIDER: A comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv. Res. 2014, 14, 57. [Google Scholar] [CrossRef] [PubMed]
- Shea, B.J.; Reeves, B.C.; Wells, G.; Thuku, M.; Hamel, C.; Moran, J.; Moher, D.; Tugwell, P.; Welch, V.; Kristjansson, E.; et al. AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 2017, 358, j4008. [Google Scholar] [CrossRef]
- Vernon, H.T.; Humphreys, B.K.; Hagino, C.A. A systematic review of conservative treatments for acute neck pain not due to whiplash. J. Manip. Physiol. Ther. 2005, 28, 443–448. [Google Scholar] [CrossRef]
- Haines, T.; Gross, A.R.; Burnie, S.; Goldsmith, C.H.; Perry, L.; Graham, N. Cervical Overview Group (COG). A Cochrane review of patient education for neck pain. Spine J. 2009, 9, 859–871. [Google Scholar] [CrossRef]
- Rickards, L.D. The effectiveness of non-invasive treatments for active myofascial trig-ger point pain: A systematic review of the literature. Int. J. Osteopath. Med. 2006, 9, 120–136. [Google Scholar] [CrossRef]
- Leaver, A.M.; Refshauge, K.M.; Maher, C.G.; McAuley, J.H. Conservative interventions provide short-term relief for non-specific neck pain: A systematic review. J. Physiother. 2010, 56, 73–85. [Google Scholar] [CrossRef]
- Passos Nunes, A.M.; Azinheira Martins Moita, J.P. Effectiveness of physical and rehabilitation techniques in reducing pain in chronic trapezius myalgia: A systematic review and meta-analysis. Int. J. Osteopath. Med. 2015, 18, 189–206. [Google Scholar] [CrossRef]
- Kroeling, P.; Gross, A.R.; Goldsmith, C.H. Cervical Overview Group. A Cochrane review of electrotherapy for mechanical neck disorders. Spine 2005, 30, E641–E648. [Google Scholar] [CrossRef] [PubMed]
- Damgaard, P.; Bartels, E.M.; Ris, I.; Christensen, R.; Juul-Kristensen, B. Evidence of Physiotherapy Interventions for Patients with Chronic Neck Pain: A Systematic Review of Randomised Controlled Trials. ISRN Pain 2013, 2013, 567175. [Google Scholar] [CrossRef]
- Resende, L.; Merriwether, E.; Rampazo, É.P.; Dailey, D.; Embree, J.; Deberg, J.; Liebano, R.E.; Sluka, K.A. Meta-analysis of transcutaneous electrical nerve stimulation for relief of spinal pain. Eur. J. Pain 2018, 22, 663–678. [Google Scholar] [CrossRef]
- Gross, A.; Langevin, P.; Burnie, S.J.; Bédard-Brochu, M.S.; Empey, B.; Dugas, E.; Faber-Dobrescu, M.; Andres, C.; Graham, N.; Goldsmith, C.H.; et al. Manipulation and mobilisation for neck pain contrasted against an inactive control or another active treatment. Cochrane Database Syst. Rev. 2015, 9, CD004249. [Google Scholar] [CrossRef] [PubMed]
- Kroeling, P.; Gross, A.; Graham, N.; Burnie, S.J.; Szeto, G.; Goldsmith, C.H.; Haines, T.; Forget, M. Electrotherapy for neck pain. Cochrane Database Syst. Rev. 2013, 8, CD004251. [Google Scholar]
- Martimbianco, A.L.C.; Porfírio, G.J.; Pacheco, R.L.; Torloni, M.R.; Riera, R. Transcutaneous electrical nerve stimulation (TENS) for chronic neck pain. Cochrane Database Syst. Rev. 2019, 12, CD011927. [Google Scholar] [CrossRef]
- Nordemar, R.; Thörner, C. Treatment of acute cervical pain-a comparative group study. Pain 1981, 10, 93–101. [Google Scholar] [CrossRef]
- Söderlund, A.; Lindberg, P. Cognitive behavioural components in physiotherapy management of chronic whiplash associated disorders (WAD)—A randomised group study. G Ital. Med. Lav. Ergon. 2007, 29 (Suppl. A), A5–A11. [Google Scholar] [CrossRef]
- Vitiello, A.L.; Bonello, R.; Pollard, H. The effectiveness of ENAR for the treatment of chronic neck pain in Australian adults: A preliminary single-blind, randomised controlled trial. Chiropr. Osteopat. 2007, 15, 9. [Google Scholar] [CrossRef] [PubMed]
- Ardiç, F.; Sarhus, M.; Topuz, O. Comparison of two different techniques of electrotherapy on myofascial pain. J. Back Musculoskelet Rehabil. 2002, 16, 11–16. [Google Scholar] [CrossRef] [PubMed]
- Chiu, T.T.; Hui-Chan, C.W.; Chein, G. A randomized clinical trial of TENS and exercise for patients with chronic neck pain. Clin. Rehabil. 2005, 19, 850–860. [Google Scholar] [CrossRef]
- Smania, N.; Corato, E.; Fiaschi, A.; Pietropoli, P.; Aglioti, S.M.; Tinazzi, M. Repetitive magnetic stimulation: A novel therapeutic approach for myofascial pain syndrome. J. Neurol. 2005, 252, 307–314. [Google Scholar] [CrossRef] [PubMed]
- Sahin, N.; Albayrak, I.; Ugurlu, H. Effect of different transcutaneous electrical stimulation modalities on cervical myofascial pain syndrome. J. Musculoskelet Pain 2011, 19, 18–23. [Google Scholar] [CrossRef]
- Li, C.; Zhang, X.L.; Ding, H.; Tao, Y.Q.; Zhan, H.S. Comparative study on effects of manipulation treatment and transcutaneous electrical nerve stimulation on patients with cervi-cogenic headache. Zhong Xi Yi Jie He Xue Bao 2007, 5, 403–406. (In Chinese) [Google Scholar] [PubMed]
- Escortell-Mayor, E.; Riesgo-Fuertes, R.; Garrido-Elustondo, S.; Asúnsolo-Del Barco, A.; Díaz-Pulido, B.; Blanco-Díaz, M.; Bejerano-Álvarez, E. TEMA-TENS Group. Primary care randomized clinical trial: Manual therapy effectiveness in comparison with TENS in patients with neck pain. Man. Ther. 2011, 16, 66–73. [Google Scholar] [CrossRef]
- Fernández-De-Las-Peñas, C.; Cleland, J.A.; Huijbregts, P.; Palomeque-Del-Cerro, L.; González-Iglesias, J. Repeated Applications of Thoracic Spine Thrust Manipulation do not Lead to Tolerance in Patients Presenting with Acute Mechanical Neck Pain: A Secondary Analysis. J. Man. Manip. Ther. 2009, 17, 154–162. [Google Scholar] [CrossRef]
- González-Iglesias, J.; Fernández-de-las-Peñas, C.; Cleland, J.A.; Gutiérrez-Vega Mdel, R. Thoracic spine manipulation for the management of patients with neck pain: A randomized clinical trial. J. Orthop. Sports Phys. Ther. 2009, 39, 20–27. [Google Scholar] [CrossRef]
- González-Iglesias, J.; Fernández-de-las-Peñas, C.; Cleland, J.A.; Alburquerque-Sendín, F.; Palomeque-del-Cerro, L.; Méndez-Sánchez, R. Inclusion of thoracic spine thrust manipula-tion into an electro-therapy/thermal program for the management of patients with acute mechanical neck pain: A randomized clinical trial. Man. Ther. 2009, 14, 306–313. [Google Scholar] [CrossRef]
- Curatolo, M.; Petersen-Felix, S.; Arendt-Nielsen, L.; Giani, C.; Zbinden, A.M.; Radanov, B.P. Central hypersensitivity in chronic pain after whiplash injury. Clin. J. Pain. 2001, 17, 306–315. [Google Scholar] [CrossRef] [PubMed]
- Haldeman, S.; Carroll, L.; Cassidy, J.D.; Schubert, J.; Nygren, Å. The Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders. Eur. Spine J. 2008, 17 (Suppl. 1), 5–7. [Google Scholar] [CrossRef]
- Guzman, J.; Hurwitz, E.L.; Carroll, L.J.; Haldeman, S.; Côté, P.; Carragee, E.J.; Peloso, P.M.; van der Velde, G.; Holm, L.W.; Hogg-Johnson, S.; et al. Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders. A new conceptual model of neck pain: Linking onset, course, and care: The Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders. Spine 2008, 33 (Suppl. 4), S14–S23. [Google Scholar] [CrossRef] [PubMed]
- Rubinstein, S.M.; van Tulder, M. A best-evidence review of diagnostic procedures for neck and low-back pain. Best Pract. Res. Clin. Rheumatol. 2008, 22, 471–482. [Google Scholar] [CrossRef] [PubMed]
- Carroll, L.J.; Hogg-Johnson, S.; van der Velde, G.; Haldeman, S.; Holm, L.W.; Carragee, E.J.; Hurwitz, E.L.; Côté, P.; Nordin, M.; Peloso, P.M.; et al. Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders. Course and prognostic factors for neck pain in the general population: Results of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders. Spine 2008, 33 (Suppl. 4), S75–S82. [Google Scholar] [CrossRef] [PubMed]
- Giamberardino, M.A.; Costantini, R.; Affaitati, G.; Fabrizio, A.; Lapenna, D.; Tafuri, E.; Mezzetti, A. Viscero-visceral hyperalgesia: Characterization in different clinical models. Pain 2010, 151, 307–322. [Google Scholar] [CrossRef]
- Gelhorn, H.L.; Sexton, C.C.; Classi, P.M. Patient preferences for treatment of major depressive disorder and the impact on health outcomes: A systematic review. Prim. Care Companion CNS Disord. 2011, 13, PCC.11r01161. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).