Abstract
Smoking is well known to be correlated with cardiovascular abnormalities, in particular atherosclerosis and heart diseases. This article investigates the effect and relationship of smoking tobacco on the thickness of the intima–media (IMT) belonging to the common carotid arteries (CCAs), and also blood concentration of the lipid profile (LP), mainly the total cholesterol, High Density Lipoprotein (HDL), Low Density Lipoprotein (LDL) and also triglycerides. Nineteen male tobacco smokers and thirty-five healthy male non-smoking Saudi participants were involved in this study after obtaining their informed consent. An ultrasound and a spectrophotometer were used to determine the IMTs and lipid parameters, respectively. The thicknesses of the smokers’ right (RCA) and left carotid (LCA) arteries (0.72 and 0.7 mm, respectively) were significantly greater than the thicknesses of the arteries of the non-smokers (0.58 and 0.62 mm, respectively) (p-value = 0.005 and 0.04). Insignificant differences between the means of the other parameters in the two groups were studied. Smoking is a risk factor for stroke, because it significantly increases the IMTs of both the right and left carotid arteries.
1. Introduction
Carotid artery stenosis (CAS), or increased thickness of the carotid arteries, is a cardiovascular disease (CVD) and is one of the major factors associated with strokes worldwide. Of the incidences of stroke, 25–40% can be attributed to two types of CAS, namely, extracranial and intracranial. Strokes are also the third leading cause of disability and mortality globally [].
CAS is caused by atherosclerosis, which is the result of hyperlipidemia and lipid oxidation. Atherosclerosis is characterized by the deposition of fats in the inner layer (intima) of the arteries and is referred to as plaque, which results in obstruction of the supply of blood to the brain, various strokes and sudden death. The main risk factors for CVD include smoking cigarettes, obesity, diabetes, hypertension and unhealthy lifestyles [].
The incidence of strokes in the Gulf countries ranged from 27.6 to 57 per 100,000 people. In Saudi Arabia, the number of stroke survivors was 186 per 100,000 people []. In terms of mortality, 37% of the deaths in Saudi Arabia in 2016 could be attributed to CVD, including strokes [].
Previous studies have generally reported a positive correlation between smoking and the thickening of the carotid arteries [,]. Many prior studies have provided evidence for the variable effects of smoking on the concentration of total blood cholesterol (TC), HDL cholesterol (HDL-C), LDL cholesterol (LDL-C), and also triglycerides (TG) [,,].
This research investigated the consequences of smoking on the common carotid artery (CCA) thickness and also on the lipid profile (LP). The LP included the TC, TG, HDL-C and LDL-C.
2. Materials and Methods
2.1. Study Design
This research can be described as a descriptive, cross-sectional and case–control study. However, the major weaknesses of cross-sectional and case–control studies are the difficulty of determining causal effects and risk factors and the difficulty of generalizing their conclusions []. Still, the cross-sectional and case–control study designs are useful in the description of variables and the pattern of their distribution, and they open a window for surveillance and longitudinal studies.
2.2. Community and Sampling Procedure
Thirty-five healthy male non-smokers and nineteen male tobacco smokers living in the Asir region in the southwest region of the Kingdom of Saudi Arabia were involved in this research after signing a written informed consent form. None of the subjects were suffering from any disease symptoms, and none were using any medication.
The subjects were divided into two major groups: smokers and non-smokers. The smoker and non-smoker groups were age and body mass index (BMI) matched, and they were divided into three groups (20–30, 31–40 and 41–50 years and normal 18.9–25, overweight 25–29.9 and obese ≥ 30), respectively.
Five milliliters of intravenous blood samples were taken from each participant randomly, and transferred to an EDTA tube for analyses of the lipid profiles.
2.3. Ethics Approval
This research was ethically certified by the Research Ethics Committee of the College of Medicine, King Khalid University (REC# 2018-06-36). Investigations were carried out following the rules of the Declaration of Helsinki of 1975, revised in 2013.
2.4. Analysis Procedure
Determination of the LP was by utilizing a spectrophotometer and analysis kits from HUMAN of Germany. The kit code numbers for the TC, TG and HDL-C were 10,017, 10720P and 10,084, respectively. The LDL-C concentration was calculated using the online calculator according to the Friedewald equation available at: https://www.mdcalc.com/ldl-calculated (accessed on 20 February 2021).
2.5. Intima–Media Thickness (IMT) Measurement of the Common Carotid Arteries
Measurement of IMT of both carotid arteries, i.e., right (RCA) and left (LCA), was done utilizing a real-time, gray-scale ultrasound (US) using a logic 3, LSD 30269WS5. A high-frequency (10 MHZ) linear transducer was utilized, which provided a suitable image quality. Performance of the US was done with the participants in the supine position. IMTs of both the carotid arteries were then measured. The posterior wall of the carotid arteries was taken as the beginning point after due magnification of the image for better visualization.
2.6. Statistical Analysis
The Statistical Package for Social Sciences (SPSS) version 20 was used for the analysis of the obtained results. The tests used were the t-test percent, the independent t-test, and the Fisher’s least significance difference (LSD) of Analysis of Variance (ANOVA)test. The t-test percent from the online resource MedCalc was used to assess the effect of the CVD risk factors on the two study groups. The independent t-test was used to investigate the effect of smoking, whereas the ANOVA test was carried out for the investigation of the effect of age and BMI on the studied parameters.
3. Results
3.1. The Cardiovascular Disease Risk Factors of the Study Groups
Some modifiable risk factors for CVD (hypertension, diabetes, abdominal obesity, cigarette smoking and dyslipidemia) and two non-modifiable risk factors (aging and male gender) were assessed before investigating the effect of smoking (Table 1).

Table 1.
Risk factors of CVD in the study groups.
3.2. Smoking with RCA and LCA IMT
The means of blood HDL and LDL cholesterol were lower in the blood of smokers than in non-smokers, whereas the TC, TG, the TC/HDL-C ratio and IMTs of the two corresponding carotid arteries were increased (Table 2). Significant increases in the RCA and LCA’s thickness were noted, whereas the other variations were insignificant (see Table 2 and corresponding Figure 1).

Table 2.
Mean values of the investigated parameters in the study groups.
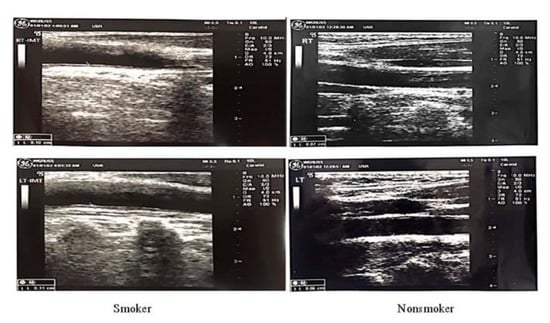
Figure 1.
Increase in the thickness of the RCA and LCA.
3.3. Effect of the Duration and Frequency of Smoking
The duration of smoking decreased the ratio of TC/HDL-C insignificantly, whereas the other parameters increased insignificantly (Table 3). The duration of smoking was correlated insignificantly and inversely to the TC/HDL ratio (Pearson’s correlation = −0.252) and to the frequency of smoking (Pearson’s correlation = −0.088).

Table 3.
The effect of the duration and frequency of smoking on the mean values of the studied parameters.
The duration of smoking had an insignificant increase effect on all of the parameters studied except for the TC/HDL-C ratio, which decreased, whereas the frequency of smoking decreased all the studied parameters insignificantly, except for the HDL-C concentration, which increased.
The frequency of smoking decreased all the studied parameters insignificantly, except for the HDL, which experienced an insignificant increase (Table 3). The frequency of smoking was correlated inversely with total cholesterol (Pearson’s correlation = −0.271), triglycerides (Pearson’s correlation = −0.005), the HDL-C (Pearson’s correlation = −0.005), LDL-C (Pearson’s correlation = −0.64), the cholesterol/HDL ratio (Pearson’s correlation = −0.139), the IMT of the RCA (Pearson’s correlation = −0.226) and the IMT of the LCA (Pearson’s correlation = −0.454). The inverse correlation of the frequency of smoking and the LDL-C and the IMT of the left carotid artery was significant (p-value= 0.034 and p-value= 0.045, respectively).
3.4. Effect of Age
With regard to the smokers, age had insignificant effects on all the studied analytes (Table 3). The ages of the non-smokers had a significant effect on the TC, TC/HDL ratio and the IMTs of the RCA and LCA (Table 4).

Table 4.
Effect of age (years) on the calculated parameters’ mean and standard deviation for smokers and non-smokers.
3.5. The Effect of BMI
BMI had different effects on smokers’ and non-smokers’ studied parameters. In the non-smoking group, BMI had an insignificant effect on all of the parameters studied (Table 5).

Table 5.
Effect of BMI on calculated parameters’ mean values for smokers and non-smokers.
The smokers’ BMIs increased TC, TG, HDL-cholesterol and the TC/HDL ratio insignificantly. The RCA and LCA IMTs increased significantly as the smokers’ BMIs increased (Table 5). In summary, BMI was shown to have a regulatory effect on smokers’ lipid profiles.
Regarding the effect of smoking irrespective of the BMI effect, it significantly affected the LCA (p-value = 0.005) and the RCA (p-value = 0.04) (Table 2), while the BMI exerted significant effects on the LCA (p-value = 0.016) and the RCA (p-value = 0.05). The conclusion of this comparison is that the smoking effect on carotid artery thickness is higher than the effect of BMI.
3.6. Carotid Artery IMTs and Corresponding Lipid Profile
Non-smokers’ carotid artery IMTs were associated insignificantly with increased TC, TG and the TC/HDL-C ratio, and were also associated with insignificant decreases in HDL-C and LDL-C (Table 6).

Table 6.
Mean values of studied parameters in smokers and non-smokers, according to carotid artery thicknesses.
With regard to the smokers, the carotid artery IMTs were associated with an insignificant increase in the concentration of TG and HDL-C, LDL-C and the TC/HDL-C ratio. The cholesterol increased significantly as the IMTs increased (Table 5).
From the above-mentioned results, it is apparent that carotid artery IMT is associated with abnormal lipid profile.
4. Discussion
Compared to previous findings, the smokers in this study exhibited a significant increase in the IMTs of both the RCA and the LCA. The IMTs of the two carotid arteries increased insignificantly as the duration of smoking increased, and decreased as the frequency of smoking increased. The studied parameters of both smokers and non-smokers were affected variably by both age and BMI. Carotid artery IMTs play a crucial role in determining the LP, specifically the plasma HDL-C, blood cholesterol and cholesterol ratio.
A significant, positive effect of smoking on TC, TG and LDL-C was reported in most of the previous studies [,,,]. Venkatesan et al. (2006) found that the TC, LDL-C and non-HDL-C were elevated notably in the blood of smokers, compared to non-smokers []. With regard to the effect of smoking on the concentration of HDL-C in the blood, most previous studies demonstrated that smoking significantly decreased the level of HDL-C in the blood [,,]. To some extent, the findings of this study are similar to those of previous research, as this work reported that smoking was associated with insignificant increases in the TC, TG and the blood cholesterol ratio, and with an insignificant decrease in HDL-C.
It is well known that smoking is strongly correlated with high TC/HDL and also LDL/HDL ratios. Elevated cholesterol ratios are risk factors for CVD, strokes and sudden death [,,]. However, the cholesterol ratios in this study increased insignificantly in the blood of smokers compared to non-smokers. All of the previous studies found that smoking was accompanied by high TC, elevated LDL-C and depleted HDL-C, and therefore with high cholesterol ratios [,,,,,,].
Similar to our findings, previous research has demonstrated that smoking is associated with increased thickness of the carotid arteries [,,,,].
With regard to the effect of the frequency of smoking, we concluded that it was associated insignificantly with decreased TC, TG, the TC/HDL-C ratio and RCA and LCA IMTs; this frequency was also associated with an insignificant increase in HDL-C. Alharbi (2011) reported that smoking one to five cigarettes per day was correlated with significantly increased triglycerides, and that smoking six to fifteen cigarettes per day resulted in significantly increased HDL-C and TG []. The HDL-C increase due to smoking cigarettes more frequently may play a role in removing cholesterol from blood vessel walls, because HDL-C reverses the transport of cholesterol from the extrahepatic tissues to the liver (thus acting as a scavenging molecule) []. In contrast to our study and that of Alharbi (2011), a Japanese study found that heavy smoking was associated with a high concentration of triglycerides and a low concentration of HDL []. An Iraqi study mentioned that heavy smoking might be associated with increased total cholesterol and LDL [].
In our study, the duration of smoking increased the total cholesterol, triglycerides, HDL-C and carotid artery IMTs insignificantly, and decreased total cholesterol/HDL-C ratio insignificantly. In contrast to our findings, Hassan et al. (2013) stated that the duration of smoking was associated with decreased HDL-C [], while we found that the HDL-C increased insignificantly as the duration of smoking increased.
With regard to the consequence of age on the LP parameters studied, this study found that the non-smokers’ ages had significant effects on the total cholesterol, the total blood cholesterol/HDL-C ratio and the RCA and LCA IMTs. The smokers’ ages had an insignificant effect on the lipid profile. Rizvi and Nagra (2014) found that age and gender had significant effects on the lipid profile [].
In this study, we found that the BMI of the non-smokers insignificantly influenced all the said parameters while the BMI of the smokers significantly influenced the IMT of the CA. A previous study conducted in Florida, USA concluded that high BMI is correlated with elevated triglycerides and depleted HDL-C [].
We found that the carotid artery IMTs were associated with an insignificant decrease in HDL-C in the non-smoking group and an insignificant increase in HDL-C in the group of smokers. Yang et al. (2014) reported that human subjects with carotid plaques had significantly lower HDL-C and significantly increased LDL, TC/HDL-C ratios and LDL/HDL ratios than did healthy human subjects without carotid plaques [].
This research is descriptive in nature, and its findings cannot be generalized due to the small number of samples and subgroups.
5. Conclusions
The conclusions of this study are as follows:
- (1)
- Smoking is a risk factor for strokes because of the significant increase in carotid artery IMTs;
- (2)
- TC, TG, HDLC, LDL-C and the TC/HDL ratio of the smokers differed insignificantly from those of the non-smokers; and
- (3)
- Due to the small number of participants in the subgroups, it is not statistically valid to draw a conclusion about the effects of age, BMI, smoking duration and smoking frequency.
Author Contributions
Conceptualization: M.A. (Magbool Alelyani), I.H. and M.E.A.M.; data curation: M.A. (Magbool Alelyani), G.S.Z., I.H., M.J.M., M.A. (Mohammed Adam) and M.E.A.M.; formal analysis: G.S.Z., M.A. (Mohammed Adam) and M.E.A.M.; funding acquisition: M.E.A.M.; investigation: S.A.S.A.-S.A., M.J.M., M.A. (Mohammed Adam) and M.E.A.M.; methodology: M.A. (Magbool Alelyani) and G.S.Z.; project administration: M.E.A.M.; resources: S.A.S.A.-S.A., G.S.Z., I.H., M.J.M. and M.A. (Mohammed Adam); software: M.E.A.M.; supervision: S.A.S.A.-S.A., G.S.Z. and I.H.; validation: M.E.A.M.; visualization: M.A. (Magbool Alelyani) and S.A.S.A.-S.A.; writing—original draft: G.S.Z., M.A. (Mohammed Adam) and M.E.A.M.; writing—review and editing: M.A. (Magbool Alelyani), G.S.Z. and M.E.A.M. All authors have read and agreed to the published version of the manuscript.
Funding
The authors extend their appreciation to the deanship of scientific research of King Khalid University for financially supporting this project under grant number R.G.P1.\92\40.
Institutional Review Board Statement
This research was ethically certified by the Research Ethics Committee of the College of Medicine, King Khalid University (REC# 2018-06-36).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data can be accessed from the author upon request.
Acknowledgments
The authors extend their appreciation to the deanship of scientific research of King Khalid University for financially supporting this project.
Conflicts of Interest
All the authors declare there is no conflict of interest.
References
- Prasad, K. Pathophysiology and Medical Treatment of Carotid Artery Stenosis. Int. J. Angiol. 2015, 24, 158–172. [Google Scholar] [CrossRef]
- Rafieian-Kopaei, M.; Setorki, M.; Doudi, M.; Baradaran, A.; Nasri, H. Atherosclerosis: Process, Indicators, Risk Factors and New Hopes. Int. J. Prev. Med. 2014, 5, 927–946. [Google Scholar] [PubMed]
- Aljefree, N.; Ahmed, F. Prevalence of Cardiovascular Disease and Associated Risk Factors among Adult Population in the Gulf Region: A Systematic Review. Adv. Public Health 2015, 2015, 1–23. [Google Scholar] [CrossRef]
- WHO. Risk of Premature Death Due to NCDs (Saudi Arabia). Available online: https://www.who.int/nmh/countries/sau_en.pdf (accessed on 23 February 2021).
- Tell, G.S.; Polak, J.F.; Ward, B.J.; Kittner, S.J.; Savage, P.J.; Robbins, J. Relation of smoking with carotid artery wall thickness and stenosis in older adults. The Cardiovascular Health Study. The Cardiovascular Health Study (CHS) Collaborative Research Group. Circulation 1994, 90, 2905–2908. [Google Scholar] [CrossRef]
- Fan, A.Z.; Paul-Labrador, M.; Merz, C.N.B.; Iribarren, C.; Dwyer, J.H. Smoking status and common carotid artery intima-medial thickness among middle-aged men and women based on ultrasound measurement: A cohort study. BMC Cardiovasc. Disord. 2006, 6, 42. [Google Scholar] [CrossRef][Green Version]
- Jain, R.B.; Ducatman, A. Associations between smoking and lipid/lipoprotein concentrations among US adults aged ≥20 years. J. Circ. Biomark. 2018, 7, 1–10. [Google Scholar] [CrossRef]
- Khurana, M.; Sharma, D.; Khandelwal, P.D. Lipid profile in smokers and tobacco chewers--a comparative study. J. Assoc. Phys. India 2000, 48, 895–897. [Google Scholar]
- Chwyeed, S. A comparison between the effect of shisha and cigarette smoking on serum lipid profile of males in Nasiriyah City. Med. J. Babylon 2018, 15, 39. [Google Scholar] [CrossRef]
- Koh, E.T.; Owen, W.L. Descriptive Research and Qualitative Research. In Introduction to Nutrition and Health Research; Koh, E.T., Owen, W.L., Eds.; Springer: Boston, MA, USA, 2000; pp. 219–248. [Google Scholar]
- Singh, D. Effect of Cigarette Smoking on Serum Lipid Profile in Male Population of Udaipur. Biochem. Anal. Biochem. 2016, 5, 283. [Google Scholar] [CrossRef]
- Rashan, M.A.A.; Omar, T.D.; Razzaq, H.A.A.; Hassali, M.A. The Impact of Cigarette Smoking on Lipid Profile among Iraqi Smokers. Int. J. Collab. Res. Intern. Med. Public Health 2016, 8, 491–500. [Google Scholar]
- Hassan, E.E.; Gabra, H.M.; Abdalla, Z.A.; Ali, A.E. Effect of Cigarette Smoking on Lipid Profile in Male at Collage of Police and Low Khartoum, Sudan. Asian J. Biomed. Pharm. Sci. 2013, 3, 8–31. [Google Scholar]
- Venkatesan, A.; Hemalatha, A.; Bobby, Z.; Selvaraj, N.; Sathiyapriya, V. Effect of smoking on lipid profile and lipid peroxidation in normal subjects. Indian J. Physiol. Pharmacol. 2006, 50, 73–278. [Google Scholar]
- Batic-Mujanovic, O.; Zildzic, M.; Beganlic, A.; Kusljugić, Z. The effect of cigarette smoking on HDL-cholesterol level [Abstract]. Med. Arh. 2006, 60 (Suppl. 2), 90–92. [Google Scholar]
- He, B.-M.; Zhao, S.-P.; Peng, Z.-Y. Effects of cigarette smoking on HDL quantity and function: Implications for atherosclerosis. J. Cell. Biochem. 2013, 114, 2431–2436. [Google Scholar] [CrossRef]
- Devaranavadgi, B.B.; Aski, B.S.; Kashinath, R.T.; Hundekari, I.A. Effect of Cigarette Smoking on Blood Lipids—A Study in Belgaum, Northern Karnataka, India. Glob. J. Med. Res. 2012, 12, 56–61. [Google Scholar]
- Alharbi, W.D.M. Influence of cigarette smoking on lipid profile in male university students. Pak. J. Pharmacol. 2011, 28, 45–49. [Google Scholar]
- Kunutsor, S.K.; Zaccardi, F.; Karppi, J.; Kurl, S.; Laukkanen, J.A. Is High Serum LDL/HDL Cholesterol Ratio an Emerging Risk Factor for Sudden Cardiac Death? Findings from the KIHD Study. J. Atheroscler. Thromb. 2017, 24, 600–608. [Google Scholar] [CrossRef]
- Lemieux, I.; Lamarche, B.; Couillard, C.; Pascot, A.; Cantin, B.; Bergeron, J.; Dagenais, G.R.; Després, J.-P. Total Cholesterol/HDL Cholesterol Ratio vs LDL Cholesterol/HDL Cholesterol Ratio as Indices of Ischemic Heart Disease Risk in Men. Arch. Intern. Med. 2001, 161, 2685–2692. [Google Scholar] [CrossRef]
- Nam, B.H.; Kannel, W.B.; D’Agostino, R.B. Search for an Optimal Atherogenic Lipid Risk Profile: From the Framingham Study. Am. J. Cardiol. 2006, 97, 372–375. [Google Scholar] [CrossRef]
- Kim, D.; Sung, H.; Cho, E.; Lee, J. Relationship of Thickness of Carotid Artery according to Smoking and Drinking in University Students. Korean J. Clin. Lab. Sci. 2018, 50, 345–353 . [Google Scholar] [CrossRef][Green Version]
- Mahmoud, M.Z. Effects of cigarettes smoking on common carotid arteries intima media thickness in current smokers. Ozean J. Appl. Sci. 2012, 5, 259–269. [Google Scholar]
- Babiker, M.S. The Effects of Smoking on Carotid Artery Hemodynamics. J. Diagn. Med. Sonogr. 2016, 32, 149–152. [Google Scholar] [CrossRef]
- Hansen, K.; Östling, G.; Persson, M.; Nilsson, P.M.; Melander, O.; Engström, G.; Hedblad, B.; Rosvall, M. The effect of smoking on carotid intima–media thickness progression rate and rate of lumen diameter reduction. Eur. J. Intern. Med. 2016, 28, 74–79. [Google Scholar] [CrossRef]
- Simão, D.M.B.; Ribeiro, P.P.; Abrantes, A.F.; Pinheiro, J.P.; Almeida, R.P.P.; Brito, A.Q.L.C.; Rodrigues, S. Effects of smoking on carotid artery structures and haemodynamics. Health Manag. 2018, 18, 314–317. [Google Scholar]
- Feingold, K.R. Introduction to Lipids and Lipoproteins; Feingold, K.R., Anawalt, B., Boyce, A., Chrousos, G., de Herder, W.W., Dungan, K., Grossman, A., Hershman, J.A., Hofland, J., Kaltsas, G., et al., Eds.; Endotext: South Dartmouth, MA, USA, 2000; pp. 1–25. [Google Scholar]
- Chun, W.; Sano, A.; Nishida, H.; Urano, S.; Sakagami, K. Effect of cigarette smoking on lipid profile: Analysis of mass screening of 29 519 middle-aged Japanese men. In Tobacco: The Growing Epidemic; Lu, R., Mackay, J., Niu, S., Peto, R., Eds.; Springer: London, UK, 2000. [Google Scholar]
- Rizvi, N.B.; Nagra, S.A. Summary: Lipid Profile. In Minerals and Lipids Profiles in Cardiovascular Disorders in South Asia; Springer: Berlin/Heidelberg, Germany, 2014; pp. 143–145. [Google Scholar]
- Shamai, L.; Lurix, E.; Shen, M.; Novaro, G.M.; Szomstein, S.; Rosenthal, R.; Hernandez, A.V.; Asher, C.R. Association of Body Mass Index and Lipid Profiles: Evaluation of a Broad Spectrum of Body Mass Index Patients Including the Morbidly Obese. Obes. Surg. 2010, 21, 42–47. [Google Scholar] [CrossRef]
- Yang, C.; Sun, Z.; Li, Y.; Ai, J.; Sun, Q.; Tian, Y. The correlation between serum lipid profile with carotid intima-media thickness and plaque. BMC Cardiovasc. Disord. 2014, 14, 1–7. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).