Abstract
The analysis aims at assessing the current trends in orthognathic surgery. The retrospective study covered a group of 124 patients with skeletal malocclusion treated by one team of maxillofacial surgeons at the University Hospital in Zielona Góra, Poland. Various variables were analysed, including demographic characteristics of the group, type of deformity, type of osteotomy used, order in which osteotomy was performed and duration of types of surgery. The mean age of the patients was 28 (ranging from 17 to 48, SD = 7). The group included a slightly bigger number of females (59.7%), with the dominant skeletal Class III (64.5%), and asymmetries were found in 21.8% of cases. Types of osteotomy performed during surgeries were divided as follows: LeFort I, segmental LeFort I, BSSO, BSSO with genioplasty, LeFort I with BSSO, LeFort I with BSSO and genioplasty, segmental LeFort I with BSSO, isolated genioplasty. Bimaxillary surgeries with and without genioplasty constituted the largest group of orthognathic surgeries (49.1%), and a slightly smaller percentage were one jaw surgeries (46.7%). A statistically significant correlation was found between the type of surgery and the skeletal class. In patients with skeletal Class III, bimaxillary surgeries were performed significantly more often than in patients with skeletal Class II (57.5% vs. 20.0%; p = 0.0002). The most common type of osteotomy in all surgeries was bilateral osteotomy of the mandible modo Obwegeser–Epker in combination with Le Fort I maxillary osteotomy (42.7%). The order of osteotomies in bimaxillary surgeries was mandible first in 61.3% of cases. The longest surgery was bimaxillary osteotomy with genioplasty (mean = 265 min), and the shortest surgery was isolated genioplasty (mean = 96 min). The results of the analysis show a significant differentiation between the needs of orthognathic surgery and the types of corrective osteotomy applied to the facial skeleton.
1. Introduction
Attempts to define the appearance of an ideal face have been made by scientists since ancient times. The canons of the beauty of the human face changed over time, but what is symmetrical, proportional and harmonious has always been considered attractive [1,2].
For many people, the pursuit of perfection in the physical appearance has now become a goal in itself.
The growing awareness of the society about possibilities of the orthodontic and surgical treatment and the potential of orthognathic surgery means that the requirements imposed on doctors are more demanding and that the needs for such treatment have increased significantly over the last 20 years [3,4]. The necessity to treat skeletal malocclusion provided a reason for distinguishing a specific medical discipline which is orthognathic surgery [5].
The term “orthognathic surgery” denotes operations in the field of maxillofacial surgery aimed at correcting deformities in the structure of the facial skeleton [6,7]. Treatment of skeletal deformities leads to an improvement in the function of the stomatognathic system and the appearance of the patient’s face as a result of actions of orthognathic surgery combined with elements of plastic surgery. The word “orthognathic” comes from Greek, and literally means “straight bones” (orthos—to straighten, gnathos—bone) [8]. The basis for orthognathic treatment is activation of the craniofacial regions that require correction by osteotomy, and their stabilization in a new position with a selected anastomosis [9,10].
1.1. Historical Development of Orthognathic Surgery
There are not too many reports on the treatment of skeletal deformities in the 19th century. The first operation on a deformed mandible is attributed to Hullihen, who, in 1848, moved back a segment of the alveolar part of the mandible.
The first correction of the ramus of the mandible was reported by Berger of Lyon in 1897. The author reported on the treatment of mandibular prognathism through osteotomies of the condyle [5].
The first half of the twentieth century marked the development and work on horizontal osteotomies of the ramus of the mandible in two major centres in the world—Europe and the USA. Complications of the method, such as recurrence of the deformity, pseudoarthrosis, irreversible damage to a branch of the fifth cranial nerve and the seventh cranial nerve, as well as salivary fistulae and unsightly skin scars, among other things, prompted a search for new solutions [5,7,10].
Bearing in mind the difficulties and complications, it was necessary to find a method that would ensure that bone fragments contacted over a larger region compared to horizontal ramus mandibular osteotomy.
In 1955, Hugo Obwegeser [5,7] proposed the method of intraoral sagittal split ramus mandibular osteotomy (Figure 1), which opened a new chapter in corrective surgery of the mandible—mainly as a result of a significantly smaller number of complications.
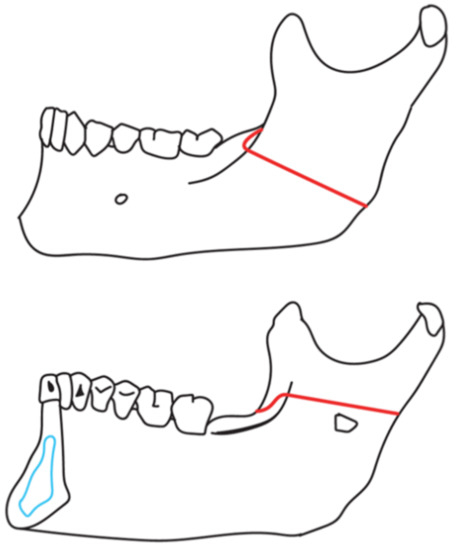
Figure 1.
Schematic view of sagittal mandibular osteotomy modo Obwegeser.
An important modification of Obwegeser’s osteotomy was made in 1958 by Dal Pont—a surgeon from Italy—by extending the sagittal cleft towards the body of the mandible, which significantly increased the adhesion surface for osteotomy fragments (Figure 2). An interesting fact is that Dal Pont never used his method in clinical work after he had returned from his internship in Zurich [10]. To date the Dal-Pont modification has been used successfully by numerous surgical centres in the world.
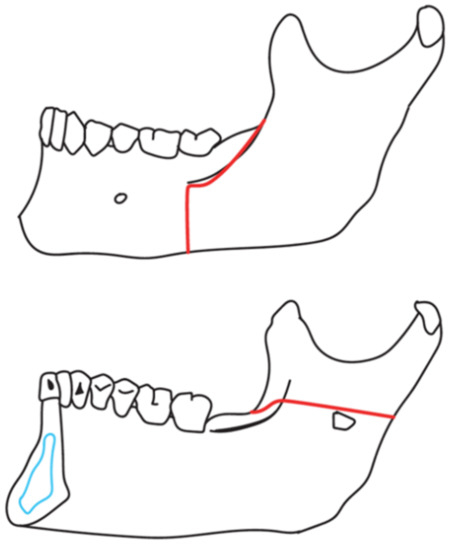
Figure 2.
Schematic view of sagittal mandibular osteotomy modo Obwegeser–Dal-Pont.
The scope of mandibular osteotomy with regard to the lingual side was also subject to modification. Hunsuk and Epker saw no need to extend it towards the posterior edge of the mandibular ramus (Figure 3), but to end osteotomy internally, right behind the mandibular foramen, and their concept also finds its supporters today [11,12].
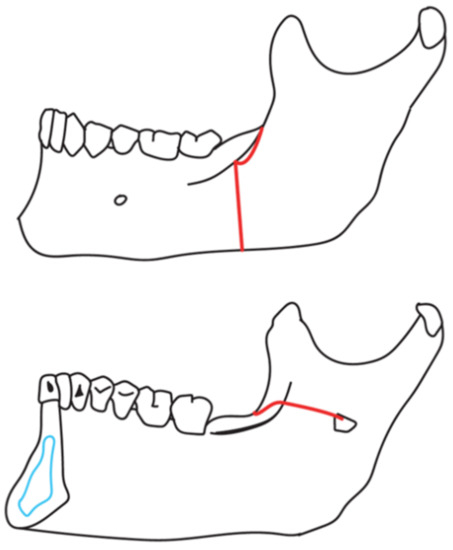
Figure 3.
Schematic view of oblique mandibular osteotomy modo Obwegeser–Epker (Hunsuck).
At the same time, observations and modifications regarding the possibility of maxillary osteotomy were carried out [5,7]. The first maxillary osteotomy—a means to access the nasopharyngeal tumour—was performed by Von Langebeck in 1859. In the 1920s, Wassmund practised osteotomies on the anterior segment of the maxilla and made attempts to perform osteotomy with regard to the entire maxilla along the Le Fort I fracture line. Schuchardt, on the other hand, preferred segmental osteotomies within the maxilla, which, however, failed to become established in orthognathic surgery [5,7].
However, it was only in the 1950s when significant progress in this regard was made, and thanks to Kole, Trauner and Obwegeser, Le Fort I maxillary osteotomies became permanently established in clinical practice (Figure 4).
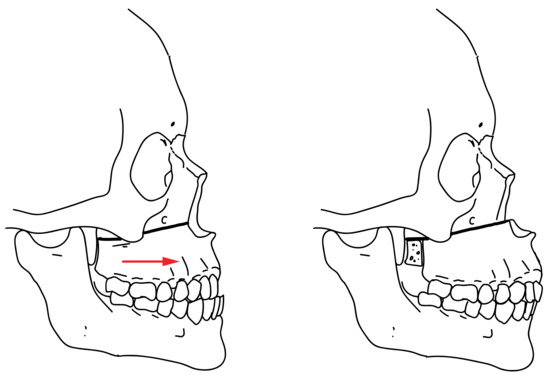
Figure 4.
Schematic view of Le Fort I osteotomy.
Almost 15 years after starting the treatment of mandibular deformities, Obwegeser [9] presented the use of Le Fort I maxillary corrective osteotomies, as well as the combination of maxillary and mandibular osteotomies during one surgery, which marks the beginning of the bimaxillary era [10].
However, Hoffer—who, in 1936, proposed the correction of the mandibular body accessed extraorally—is considered to be the originator of genioplasty [7]. Today, after modifications, this surgery has become a permanent part of the canon of orthognathic surgery (Figure 5).
Figure 5.
Schematic view of genioplasty.
1.2. Contemporary Aspects of Orthognathic Surgery
Nowadays, orthognathic surgery is actually an independent surgical specialty closely related to orthodontics [13]. Corrective osteotomies of the mandible in various modifications, Le Fort I maxillary osteotomies, jaw segmentation or genioplasty are routine surgeries aimed at correcting skeletal deformities of the face [14].
Recent years have seen the development of diagnostics and 3D planning in orthognathic surgeries, as well as attempts to use digital technologies supporting surgical treatment [15]. The improvement of surgical techniques and access to new technologies significantly reduce the risk of complications, improve safety of surgery and its availability to patients [16,17,18].
1.3. Aim of the Study
The study aimed at analysing a group of patients in regard to the incidence of skeletal malocclusions with the breakdown into skeletal Classes I, II and III and skeletal open bite, assessment of the demographic profile of the group, type of osteotomy used, order in which osteotomy was performed, duration of a specific type of surgery, adjunctive procedures used during surgery and the distribution depending on the season of the year when surgery was performed.
The second element of the analysis was to find statistically significant correlations between the above-mentioned variables.
2. Materials and Methods
The present complies with the World Medical Association Declaration of Helsinki on medical research protocols and ethics.
Our retrospective study covered a group of 124 patients, including 74 females—59.7%, aged 17–48 (Mean = 28, SD = 7) with a skeletal deformity, treated surgically by one team of maxillofacial surgeons from January 2015 to December 2020, at the University Hospital in Zielona Góra, Poland. All the patients were operated by two experienced maxillofacial surgeons.
Patients with a history of trauma in the facial skeleton, craniofacial syndromes and patients treated with distraction osteogenesis (DO) were excluded from the study.
The clinical data collected from the medical records and subjected to the analysis included:
1—sex, 2—age at the time of surgery, 3—diagnosis of skeletal malocclusion, 4—occurrence of asymmetry, 5—type of osteotomy performed during surgery, 6—one jaw or two jaw surgery, 7—maxilla or mandible first, 8—duration of surgery in minutes, 9—adjunctive surgical procedures, 10—time of the year when surgery was performed. The detailed variables subjected to the analysis are presented in Table 1.

Table 1.
The detailed variables subjected to the analysis.
The diagnosis of skeletal malocclusion which determined the surgical treatment plan was based on the patient’s clinical examination, and the use of diagnostic instruments such as facial photographs, cone beam computed tomography (CBCT) examinations of the skull, dental arch scans, and soft tissue cephalometric analysis (STCA) using NemoFab software (NEMOTEC, Spain).
Complex deformities were classified according to the diagnosis of the dominant deformity.
Statistical Methods
The statistical analysis of the results was performed using STATISTICA v. 13.3 (TIBCO Software Inc., Tulsa, OK, USA) and an EXCEL spreadsheet.
- For all quantitative parameters (age, duration of surgery, etc.), the conformity of their distribution with the normal distribution was tested. The conformity was assessed with the Shapiro–Wilk test for normality. The assumed critical level of significance was p < 0.05.
- For quantitative parameters, mean values (M), standard deviations (SD) and extreme values, the lowest (Min) and the highest (Max) values were calculated.
- The significance of differences in mean values of parameters with a distribution close to the normal one was tested using the analysis of variance (ANOVA) and post-hoc Tukey tests.
- For nominal qualitative (e.g., sex) and ordinal (e.g., skeletal class) variables, frequencies (n) and percentages (%) were calculated and collected in multivariate contingency tables.
- The hypotheses that no correlations between qualitative traits existed were tested using the Pearson Chi-square test. When the test result was p < 0.05, it was assumed that a significant correlation between the variables existed.
3. Results
On the basis of the cephalometric analysis, four patterns of skeletal deformities of the face were determined in the study group (skeletal Classes I, II and III, and skeletal open bite).
A detailed distribution of sex in relation to the age groups at the time of surgery is presented in Table 2.

Table 2.
A detailed age distribution at the time of surgery in the study group of patients.
A detailed distribution of sex in relation to skeletal malocclusion at the time of surgery is presented in Table 3.

Table 3.
Demographic characteristic of the variables according to skeletal groups and other skeletal malocclusion.
Asymmetry occurred in 21.8% of the patients who had undergone surgery, and for skeletal Class III it was significantly more frequent than for Class II (26.2% vs. 10.0%—a significant difference at a level of p = 0.046 < 0.05). A detailed distribution of the incidence of asymmetry is presented in Table 4 and Figure 6.

Table 4.
Incidence of asymmetry according to skeletal groups and other skeletal malocclusion.
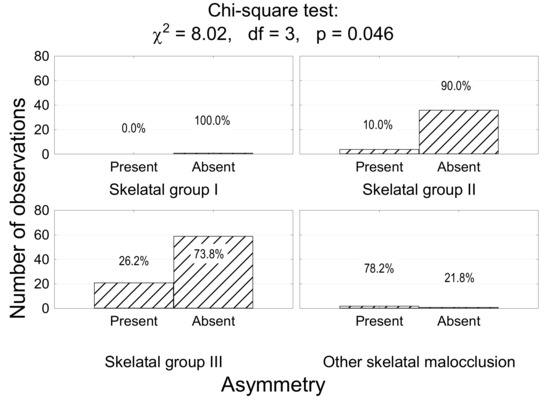
Figure 6.
The number (percentage) of patients in the groups with different skeletal classes and incidences of asymmetry, and the result of the Chi-squared test.
The most common surgery in the study group was one jaw surgery without genioplasty (45.2%, n = 56). A similar number accounted for bimaxillary surgeries without genioplasty (44.4%, n = 55). Bimaxillary surgeries with genioplasty (4.8%, n = 6) held the third place, followed by isolated genioplasty in 4.0% (n = 5) and one jaw surgery with genioplasty in two patients (1.6%).
However, all bimaxillary operations—with and without genioplasty—accounted for the largest group of patients, i.e., 49.2% (n = 61).
Statistical differences in the surgical treatment of skeletal Class II and III were found in correlation with one jaw and two jaw surgeries (<0.001). For skeletal Class II, one jaw surgeries were significantly more frequent than in the treatment of skeletal Class III (67.5% vs. 36.2%; p = 0.0023). For skeletal Class III, two jaw surgeries were performed significantly more often than in the group of patients with skeletal Class II (57.5% vs. 20.0%; p = 0.0002).
A detailed distribution of the type of surgery depending on the skeletal class is presented in Table 5 and Figure 7.

Table 5.
Incidence type of surgical treatment according to skeletal groups and other skeletal maloclusion.
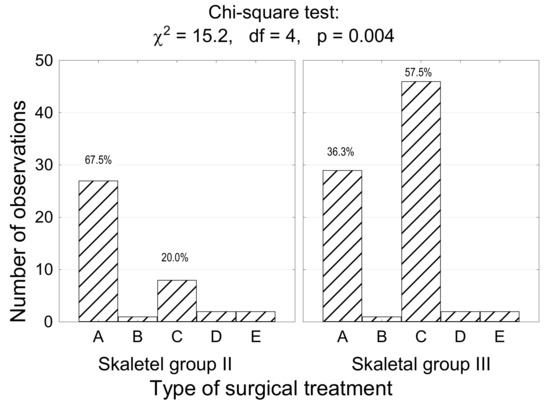
Figure 7.
The number (percentage) of patients in the groups with different skeletal classes and types of surgical treatment, and the result of the chi-squared test. A—one jaw surgery, B—one jaw + genioplasty, C—bimaxillary surgery, D—bimaxillary surgery + genioplasty, E—no jaw (genioplasty).
The most common corrective osteotomy performed during surgery was the combination of Le Fort I maxillary osteotomy with sagittal split osteotomy of the mandible modo Obwegeser–Epker (42.7%). Le Fort I isolated osteotomy with segmentation was the least frequently performed surgery (0.8%). A detailed distribution of osteotomies performed is presented in Table 6.

Table 6.
Distribution of osteotomy applied during surgery in the study group of patients.
The correlation between skeletal Class II and III and the type of osteotomy used during surgery (A to I) was analysed. A statistically significant relationship was found between skeletal Classes II and III and Types A, D and F of osteotomy (p < 0.001). The result is shown in Figure 8.
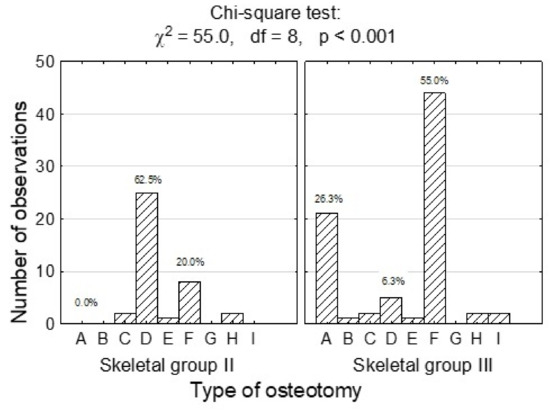
Figure 8.
The number (percentage) of patients in the groups with different skeletal classes and types of osteotomy, and the result of the Chi-squared test. A—Le Fort I, B—Le Fort I + segmentation, C—BSSO—Obwegeser–Dal Pont, D—BSSO—Obwegeser–Epker, E—BSSO—Obwegeser–Epker + genioplasty, F—Le Fort I + BSSO (Obwegeser–Epker), G—Le Fort I + BSSO (Obwegeser–Epker) + genioplasty, H—Le Fort I + segmentation + BSSO (Obwegeser–Epker), I—Genioplasty.
The order of osteotomy performed in bimaxillary surgeries in the study group of patients (n = 61) was determined. In most cases, osteotomy was started with a surgery on the mandible (61.3%). No statistically significant correlation between skeletal Classes II and III and the order in which osteotomy was performed in bimaxillary surgeries was found (p = 0.727 > 0.05).
The detailed results of the analysis are presented in Table 7.

Table 7.
The frequency of the order in which a particular osteotomy was performed in bimaxillary surgeries broken down into skeletal classes and skeletal open bite.
In the substantial majority of orthognathic surgeries, no adjunctive surgical procedures were performed (72.6%, n = 90). The most frequently performed adjunctive procedure was septoplasty (13.7%), and the smallest number of cases was recorded for skeletal anchorage assembly (0.8%).
A detailed breakdown of adjunctive procedures in the study group is presented in Table 8.

Table 8.
Distribution of adjunctive procedures performed during surgery in the study group of patients.
The relationship between performing adjunctive surgical procedures depending on the skeletal class and skeletal open bite was determined. The probability of performing adjunctive procedures for skeletal Classes II and III is very small (<0.001). The absence of adjunctive surgical procedures is significantly more frequent for skeletal Class II than skeletal Class III (92.5% vs. 65.0%; p = 0.0025). A detailed breakdown of these correlations is presented in Table 9.

Table 9.
The frequency of adjunctive procedures used during surgery (broken down into skeletal groups and skeletal open bite).
The duration of a particular type of surgical treatment was determined in minutes. The longest orthognathic surgery was bimaxillary osteotomy with genioplasty (mean = 265 min). The shortest surgery was isolated genioplasty (mean = 96 min). A detailed breakdown of the correlation between the duration of surgery and the type of surgery is presented in Table 10 and Figure 9.

Table 10.
A detailed breakdown of the correlation between the duration of surgery and the type of surgical treatment in the study group of patients (min.).
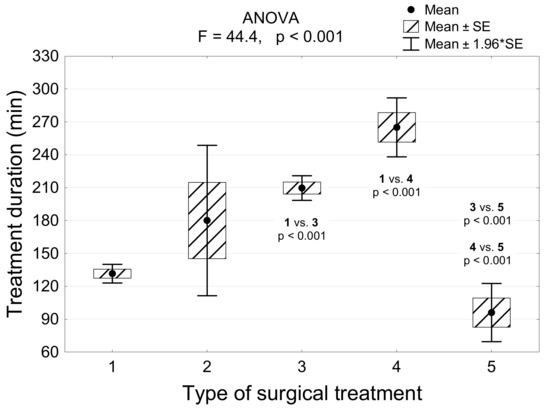
Figure 9.
The duration of treatment in the groups of patients differing in the type of treatment and the results of the analysis of variance (ANOVA) and post-hoc Tukey tests.
No seasonal distribution in the orthognathic procedures was found in the study group. Most surgery were performed in summer (31.5%), slightly less in winter (29.0%), then in spring (20.2%) and the least in the fall season (19.4%).
4. Discussion
Aesthetics and harmony of the human face is a very broad and complex issue. Attention to external appearance is an integral part of everyone’s life. The psychological aspects of the society’s positive reception of a person with a pretty face and good figure—and therefore self-confidence and success in interpersonal relationships—are important. Epidemiologically, dentofacial deformities (DFD) affect about 20% of the population—according to various sources [19,20]. In the classic breakdown of malocclusion, Class I accounts for the highest percentage of 50–55%, Class II accounts for 15–20% and Class III accounts for roughly 1%, which constitutes a small percentage of malocclusion [20,21].
However, we observe significant racial differences in the incidence of specific types of skeletal malocclusion. Class III deformities are more widespread in South-East Asian populations, affecting 15–23% of the people. It mainly results from the genetic determinants of the condition.
It is estimated that in Caucasian populations, skeletal Class III is significantly less frequent and accounts for 1–5% of the total population [22,23].
In the study group, skeletal Class III accounted for the largest percentage (64.0%), followed by skeletal Class II (32.3%). Skeletal open bite (2.4%) held the third place, and the last one was skeletal Class I (0.8%). Many authors report the incidence of skeletal Class III as the largest group undergoing surgery due to skeletal malocclusion, which corresponds with our results [14,22,24,25]. It may result from the most noticeable deformities in the profile and aesthetics of the face in those patients, which is the main determinant of entering orthognathic treatment [22,26]. The argument for such a large number of patients with skeletal Class III treated surgically is the fact that a Class II deformity is mainly treated orthodontically. Studies of the Asian population show that the convex facial profile disfigures someone’s appearance less than the concave profile does [24].
In the present study, females constituted a larger group of patients (59.7%, n = 74). The results correspond with the data that may be found in the literature where the number of females is slightly bigger. Sato et al. report that females accounted for 60.93% of the patients treated surgically for a skeletal deformity [14]. In a study by Dedong et al., the group of females accounts for 59.0%, which closely corresponds with our analysis. The authors report that the primary motivation for surgical treatment is improvement of the appearance of the face in both females (83.87%) and males (83.33%). Increased self-confidence (43.55%) comes second. The third is the patients’ improvement of occlusion (41.94%) as a determinant of surgical treatment of a skeletal deformity [26]. A study by Takatsui et al.—in which psychological aspects after orthognathic surgery were assessed—reveals a much larger group of females (68.0%) undergoing surgical treatment [27]. Improvement of facial aesthetics—and not a functional disorder associated with a skeletal deformation—is the main factor in undergoing treatment in the study group.
No statistically significant relationship between sex and the skeletal class was found in our study group—p > 0.05. A slight dominance of females may result from greater determination to improve their facial features and aesthetics [20,24,26,27].
The mean age of surgically treated patients in our study was 28 (ranging from 17 to 48, SD = 7) and did not differ statistically significantly for skeletal Classes II and III. The results correspond with the studies by Sato et al. in which the mean age of orthognathic patients was 29 years and 4 months (SD = 9), but the age amplitude was much greater (14–63) [14]. Venguoplan et al. indicate an average age of 26.7 years for orthognathically operated patients in the United States in a large population of 10,345 patients under study [28]. Furthermore, the results of our study correspond with the reports of Boeck et al. who found no statistically significant difference between the mean age of the patients and the type of malocclusion [21,24].
In conclusion, amongst patients who seek surgical treatment, the group aged 20–30 is in the majority—a result of their complete bone growth. Therefore, it is possible for them to undertake surgical treatment with no consequence of inhibiting bone growth of the facial skeleton. Additionally, it is the optimum age for an orthodontist to refer the patient for complex orthodontic and surgical treatment—also as a result of the patient’s emotional maturity, and when decisions result from his or her needs and not external motivation (doctor, parents) [29]. In our analysis, patients aged 21–30 also accounted for the largest percentage in the group, totaling 43.55% (n = 54), which is consistent with the reports by other authors [22,29].
The term “asymmetry” is used to describe differences between homologous elements. The perfect two-sided symmetry of the face is practically non-existent. However, it usually remains subclinical and unnoticeable. The pursuit of almost perfect symmetry poses a lot of difficulties and remains the main goal of treatments for correcting deformities of the facial skeleton. The aetiology of asymmetry is frequently divided into three groups of factors: congenital, developmental, and acquired. This aetiology, however, is not always known. The asymmetry component is related to all types of skeletal malocclusion, but most frequently it coexists with skeletal Class III [24,30]. The incidence of asymmetry in orthodontic patients ranges from 12% to 37% in the United States. It is 23% in Belgium, and 21% in Hong Kong [31]. Our analysis showed the presence of asymmetry in 21.8% of the patients undergoing surgery. In the group of patients with skeletal Class III, it was reported significantly more often (26.2% vs. 10.0%; p = 0.046 < 0.05). Our results correspond with the authors’ reports on the incidence of asymmetry in the European population, and the correlation between the incidence of a deformity and skeletal Class III was statistically confirmed.
The most frequently performed type of surgery in our analysis was bimaxillary surgery in all modifications—with genioplasty and segmentation of the jaw—which was performed in 49.2% of cases.
A slightly smaller percentage accounted for one jaw surgeries, on both the mandible and the maxilla, which were performed in 46.5% of cases. In our sample the proportions of one jaw to bimaxillary surgeries are similar. Chew et al. report bimaxillary surgeries (Le Fort I osteotomy + BSSO) as the most frequently performed orthognathic surgeries (73.1%) in the group of patients with dentofacial deformities. One jaw surgeries accounted for 24.1% of all surgeries (including Le Fort I osteotomy which accounted for 13.2% vs. BSSO which accounted for 10.4%). Genioplasty was performed as a secondary procedure to one jaw and bimaxillary procedures [24]. Therefore, the results of our analysis partially correspond with the reports of Chew et al.
Numerous retrospective analyses show the dominance of bimaxillary surgeries [21,24,31]. It may result from the significant progress in diagnostic instruments as well as the development of awareness of the impact of orthognathic treatment on both occlusion and aesthetics of the face as well as properties of the respiratory tract, and the continuous improvement of surgical techniques, including shortening the duration of surgery [15,16,25,32].
Furthermore, our study revealed a statistically significant correlation between the type of surgery and the skeletal class. In patients with skeletal Class III, bimaxillary surgeries were performed significantly more often than in patients with skeletal Class II (57.5% vs. 20.0%; p = 0.0002). For skeletal Class II, one jaw surgeries were significantly more frequent than in the treatment of skeletal Class III (67.5% vs. 36.2%; p = 0.0023). The results correspond with the reports of numerous authors, where the correction of skeletal Class III is treated by two jaw corrective osteotomy. It may result from the greater patients’ awareness of the safety of bimaxillary surgery, better aesthetic results and the most important effect, which is stable treatment results after using BIMAX surgery [32,33]. Surgeons also use treatment of skeletal Class II based on one jaw BSSO surgery as a popular therapeutic option [14,32,33]. In our study, we broke down the type of sagittal split ramus mandibular osteotomy into two of its modifications (Obwegeser–Dal Pont vs. Obwegeser–Epker). We find no such a breakdown in the literature, where sagittal and split osteotomies as a whole are referred to as BSSO (bilateral sagittal split osteotomy) procedures. Therefore, this topic is not referred to in the discussion.
The sequence of osteotomy performed in bimaxillary surgery is still the subject of debate [34,35]. Classically, the first orthognathic surgeries started with maxillary osteotomy—because of not a very stable connection between osteotomy fragments and greater stability of the jaw after its fixation. Currently, as a result of the enormous progress and the use of miniplate osteosynthesis for stabilizing the fragments, the decision on the order of osteotomies depends solely on the surgeon’s preferences. The sequence of surgery is usually determined by an anticipated movement of the maxillomandibular complex, and, as a result, stability of the location of the osteotomy fragments [35,36,37].
Our study showed that in 61.3% of cases of bimaxillary surgeries surgery was started with osteotomy of the mandible. No statistically significant correlation between skeletal Classes II and III and the order in which osteotomy was performed in bimaxillary surgeries was found (p = 0.727 > 0.05).
Adjunctive procedures during orthognathic surgery may be an important part of the treatment [25]. A study of a large group of 101,692 orthognathic patients in the United States showed that for 19.6% of cases adjunctive procedures were performed during surgery. The authors mentioned genioplasty, septoplasty and rhinoplasty as adjunctive procedures [38]. Our analysis revealed that adjunctive procedures were performed in 27.4% of all surgeries. However, genioplasty was excluded from adjunctive procedures, since it was classified as a separate surgery. Septoplasty was the most common adjunctive procedure in 13.7% of cases.
No statistically significant adjunctive procedures were performed for skeletal Classes II and III (<0.001) in our study.
The longest surgery in our study was bimaxillary osteotomy with genioplasty (mean = 265 min, SD = 34). The mean duration of bimaxillary osteotomy is 210 min (SD = 34), and for one jaw surgery it is 132 min (SD = 33). The shortest procedure turned out to be isolated genioplasty (mean = 96 min, SD = 30). The results correspond with the studies carried out by other researchers [39,40]. Andersen et al. report bimaxillary surgery performed within 223 min (SD = 42). The duration of Le Fort I one jaw osteotomy is 133 min (SD = 39), and for BSSO it is 103 min (SD = 33). In another study, Bowe et al. reported that the mean time for bimaxillary osteotomy (n = 107) was 139.3 min, for Le Fort I osteotomy (n = 42) it was 82.2 min, and for BSSO (n = 102) it was 80.3 min [41]. In this case, our analysis does not correspond with the results of the study in which the duration of all orthognathic procedures was shorter.
No seasonal nature of the duration of surgery was found in our analysis. No seasonal distribution in the procedures was found in the study group, which does not correspond with the study carried out by Chang-Hoon and Hyun-Hee [33]. They revealed a clear seasonal variation, that demonstrated peaks every winter and summer during summer and winter breaks at schools in Korea. Our results may indicate strong determination to make a decision to undertake surgical treatment and awareness of the advantages of orthognathic treatment.
Orthognathic surgery has been developed as a successful technique with low complication rate. Despite the variety of complications reported, their frequency seems to be low. Orthognathic surgery appears to be a safe procedure [17]. In our study, the intraoperative complications were identified in 10 patients (8%), of which three patients with a bad split in the sagittal split osteotomy, two patients with inferior alveolar nerve laceration, two patients with increased bleeding during the surgery, two patients with dental injuries, and one patient with rupture of the hard palate mucosa during segmentation.
Because of the ethnically homogeneous population in Poland, our study—a retrospective analysis—covers only a group of Polish nationality. The patients were treated in one academic centre by the same team of maxillofacial surgeons, and since there are few facilities for treating deformities of the facial skeleton in Poland, the study may be a representative analysis of the current trends in orthognathic surgery in Poland.
5. Conclusions
This study documents that patients with skeletal Class III accounted for the largest percentage (64%) in the study group. The bimaxillary surgery was the most frequently performed surgery (49.2%) and there was statistically more frequent for skeletal Class III, and one jaw surgeries for skeletal Class II. The patients aged 20–30 were the most numerous group amongst those who sought treatment.
Author Contributions
Conceptualization: E.Z., R.N., H.G. and P.G.; methodology: E.Z., R.N., S.P. and A.O.; software: S.P., P.G. and E.Z.; validation: E.Z. and R.N.; formal analysis: H.G., R.N. and E.Z.; investigation: P.G., S.P. and A.O.; resources: R.N. and E.Z.; data curation R.N., E.Z. and A.O; writing—original draft preparation: E.Z., S.P. and A.O. writing—review and editing: E.Z., A.O., H.G. and R.N.; visualization: E.Z., P.G. and R.N.; supervision: R.N., E.Z., H.G. and A.O.; project administration: E.Z., R.N., S.P. and P.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived for this study, due to the retrospective analysis of datasets, where the data are properly anonymized and informed consent was obtained at the time of original data collection.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Naini, F.B.; Moss, J.P.; Gill, D.S. The enigma of facial beauty: Esthetics, proportions, deformity, and controversy. Am. J. Orthod. Dentofacial Orthop. 2006, 130, 277–282. [Google Scholar] [CrossRef]
- Little, A.C.; Jones, B.C.; DeBruine, L.M. Facial attractiveness: Evolutionary based research. Philos. Trans. R. Soc. B Biol. Sci. 2011, 366, 1638–1659. [Google Scholar] [CrossRef] [Green Version]
- Hönn, M.; Göz, G. The ideal of facial beauty: A review. J. Orofac. Orthop. 2007, 68, 6–16. [Google Scholar] [CrossRef]
- Harrar, H.; Myers, S.; Ghanem, A.M. Art or Science? An Evidence-Based Approach to Human Facial Beauty a Quantitative Analysis Towards an Informed Clinical Aesthetic Practice. Aesthetic Plast. Surg. 2018, 42, 137–146. [Google Scholar] [CrossRef] [Green Version]
- Steinhäuser, E.W. Historical development of orthognatic surgery. J. Craniomaxillofac. Surg. 1996, 24, 195–204. [Google Scholar] [CrossRef]
- Proffit, W.R.; Turvey, T.A.; Phillips, C. Orthognathic surgery: A hierarchy of stability. Int. J. Adult Orthod. Orthognath. Surg. 1996, 3, 191–204. [Google Scholar]
- Nowak, R.M. Historical outline of orthognathic surgery Dent. Med. Probl. 2014, 51, 131–135. [Google Scholar]
- Panula, K. Correction of Dentofacial Deformities with Orthognatic Surgery. In Outcome of Treatment with Special Reference to Costs, Benefits and Risks; Department of Oral and Maxillofacial Surgery, Institute of Dentistry, University of Oulu: Oulu, Finland, 2003. [Google Scholar]
- Obwegeser, H.L. Surgical correction of small or retrodisplaced maxillae. Dish-Face Deform. Plast. Reconstr. Surg. 1969, 43, 351–365. [Google Scholar] [CrossRef]
- Obwegeser, H.L. Orthognathic Surgery and a Tale of How Three Procedures Came to Be: A Letter to the Next Generations of Surgeons. Clin. Plast. Surg. 2007, 34, 331–355. [Google Scholar] [CrossRef] [PubMed]
- Hunsuck, E.E. A modified intraoral sagittal splitting technique for correction of mandibular prognathism. J. Oral Surg. Anaesth. 1968, 2, 249–252. [Google Scholar]
- Epker, B.N. Modifications in the sagittal osteotomy of the mandible. J. Oral Surg. 1977, 35, 157–159. [Google Scholar]
- Klein, K.P.; Kaban, L.B.; Masoud, M.I. Orthognathic Surgery and Orthodontics: Inadequate Planning Leading to Complications or Unfavorable Results. Oral Maxillofac. Surg. Clin. N. Am. 2020, 32, 71–82. [Google Scholar] [CrossRef]
- Sato, F.R.; Mannarino, F.S.; Asprino, L.; de Moraes, M. Prevalence and treatment of dentofacial deformities on a multiethnic population: A retrospective study. Oral Maxillofac. Surg. 2014, 18, 173–179. [Google Scholar] [CrossRef]
- Efanov, J.I.; Roy, A.A.; Huang, K.N.; Borsuk, D.E. Virtual Surgical Planning: The Pearls and Pitfalls. Plast. Reconstr. Surg. Glob. Open 2018, 17, e1443. [Google Scholar] [CrossRef]
- Steinhuber, T.; Brunold, S.; Gärtner, C.; Offermanns, V.; Ulmer, H.; Ploder, O. Is Virtual Surgical Planning in Orthognathic Surgery Faster Than Conventional Planning? A Time and Workflow Analysis of an Office-Based Workflow for Single- and Double-Jaw Surgery. J. Oral Maxillofac. Surg. 2018, 76, 397–407. [Google Scholar] [CrossRef] [PubMed]
- Posnick, J.C.; Choi, E.; Chavda, A. Surgical Site Infections Following Bimaxillary Orthognathic, Osseous Genioplasty, and Intranasal Surgery: A Retrospective Cohort Study. J. Oral Maxillofac. Surg. 2017, 75, 584–595. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cosola, S.; Marconcini, S.; Giammarinaro, E.; Poli, G.L.; Covani, U.; Barone, A. Oral health-related quality of life and clinical outcomes of immediately or delayed loaded implants in the rehabilitation of edentulous jaws: A retrospective comparative study. Minerva Stomatol. 2018, 67, 189–195. [Google Scholar] [CrossRef]
- Eslamipour, F.; Najimi, A.; Tadayonfard, A.; Azamian, Z. Impact of Orthognatic Surgery of Life in Patients with Dentofacial Deformities. Hindawi Int. J. Dent. 2017, 6, 4103905. [Google Scholar] [CrossRef]
- Boeck, E.M.; Lunardi, N.; Pinto Ados, S.; Pizzol, K.E.; Boeck, N.R.J. Occurrence of skeletal malocclusions in Brazilian patients with dentofacial deformities. Braz. Dent. J. 2011, 22, 340–345. [Google Scholar] [CrossRef]
- Nowak, R.; Rzepecka-Skupień, M.; Zawiślak, E. Complex orthodontic and surgical management of an adult patient with transverse maxillary deficiency and skeletal class III malocclusion: A case report. Dent. Med. Probl. 2020, 57, 103–109. [Google Scholar] [CrossRef]
- Ruslin, M.; Forouzanfar, T.; Astuti, I.A.; Soemantri, E.S.; Tuinzing, D.B. The epidemiology, treatment, and complication of dentofacial deformities in an Indonesian population: A 21-year analysis. J. Oral Maxillofac. Surg. Med. Pathol. 2015, 27, 601–607. [Google Scholar] [CrossRef]
- Watanabe, M.; Suda, N.; Ohyama, K. Mandibular prognathism in Japanese families ascertained through orthognathically treated patients. Am. J. Orthod. Dentofac. Orthop. 2005, 128, 466–470. [Google Scholar] [CrossRef] [PubMed]
- Chew, M.T. Spectrum and management of dentofacial deformities in a multiethnic Asian population. Angle Orthod. 2006, 76, 806–809. [Google Scholar] [CrossRef] [PubMed]
- Olkun, H.K.; Borzabadi-Farahani, A.; Uçkan, S. Orthognathic Surgery Treatment Need in a Turkish Adult Population: A Retrospective Study. Int. J. Environ. Res. Public Health 2019, 28, 1881. [Google Scholar] [CrossRef] [Green Version]
- Yu, D.; Wang, F.; Wang, X.; Fang, B.; Shen, S.G. Presurgical Motivations, Self-Esteem, and Oral Health of Orthognathic Surgery Patients. J. Craniofacial Surg. 2013, 24, 743–747. [Google Scholar] [CrossRef]
- Takatsuji, H.; Kobayashi, T.; Kojima, T.; Hasebe, D.; Izumi, N.; Saito, I.; Saito, C. Effects of orthognathic surgery on psychological status of patients with jaw deformities. Int. J. Oral Maxillofac. Surg. 2015, 44, 1125–1130. [Google Scholar] [CrossRef]
- Venugoplan, S.R.; Nanda, V.; Turkistani, K.; Desai, S.; Allareddy, V. Discharge patterns of orthognathic surgeries in the United States. J. Oral Maxillofac. Surg. 2012, 70, e77–e86. [Google Scholar] [CrossRef]
- Nancy, W.N.; Glover, K.; Major, P.; Varnhagen, C.; Grace, M. Age limitation on provision of orthopedic therapy and orthognathic surgery. Am. J. Orthod. Dentofac. Orthop. 1998, 113, 156–164. [Google Scholar] [CrossRef]
- Agrawal, M.; Agrawal, J.A.; Nanjannawar, L.; Fulari, S.; Kagi, V. Dentofacial Asymmetries: Challenging Diagnosis and Treatment Planning. J. Int. Oral Health 2015, 7, 128–131. [Google Scholar]
- Thiesen, G.; Gribel, B.F.; Freitas, M.P.M. Facial asymmetry: A current review. Dent. Press J. Orthod. 2015, 20, 110–125. [Google Scholar] [CrossRef]
- Eslamipour, F.; Borzabadi-Farahani, A.; Le, B.T.; Shahmoradi, M. A Retrospective Analysis of Dentofacial Deformities and Orthognathic Surgeries. Ann. Maxillofac. Surg. 2017, 7, 73–77. [Google Scholar] [CrossRef]
- Lee, C.H.; Park, H.H.; Seo, B.M.; Lee, S.J. Modern trends in Class III orthognathic treatment: A time series analysis. Angle Orthod. 2017, 87, 269–278. [Google Scholar] [CrossRef]
- Perez, D. Edward Ellis III: Sequencing Bimaxillary Surgery: Mandible First. J. Oral Maxillofac. Surg. 2011, 69, 2217–2224. [Google Scholar] [CrossRef]
- Turvey, T. Sequencing of Two-Jaw Surgery: The Case for Operating on the Maxilla First. J. Oral Maxillofac. Surg. 2011, 69, 2225. [Google Scholar] [CrossRef]
- Borba, A.M.; Borges, A.H.; Cé, P.S.; Venturi, B.A.; Naclério-Homem, M.G.; Miloro, M. Mandible-first sequence in bimaxillary orthognathic surgery: A systematic review. Int. J. Oral Maxillofac. Surg. 2016, 45, 472–475. [Google Scholar] [CrossRef]
- Liebregts, J.; Baan, F.; de Koning, M.; Ongkosuwito, E.; Bergé, S.; Maal, T.; Xi, T. Achievability of 3D planned bimaxillary osteotomies: Maxilla-first versus mandible-first surgery. Sci. Rep. 2017, 24, 9314. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Berlin, N.L.; Tuggle, C.T.; Steinbacher, D.M. Improved Short-Term Outcomes following Orthognathic Surgery Are Associated with High-Volume Centers. Plast. Reconstr. Surg. 2016, 138, 273e–281e. [Google Scholar] [CrossRef] [PubMed]
- Garg, M.; Cascarini, L.; Coombes, D.M.; Walsh, S.; Tsarouchi, D.; Bentley, R.; Brennan, P.A.; Dhariwal, D.K. Multicentre study of operating time and inpatient stay for orthognathic surgery. Br. J. Oral Maxillofac. Surg. 2010, 48, 363. [Google Scholar] [CrossRef]
- Andersen, K.; Thastum, M.; Nørholt, S.E.; Blomlöf, J. Relative blood loss and operative time can predict length of stay following orthognathic surgery. Int. J. Oral Maxillofac. Surg. 2016, 45, 1209–1212. [Google Scholar] [CrossRef] [PubMed]
- Bowe, C.M.; Gurney, B.; Sloane, J.; Johnson, P.; Newlands, C. Operative time, length of stay and reoperation rates for orthognatic surgery. Br. J. Oral Maxillofac. Surg. 2021, 59, 163–167. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).