Abstract
Current neuroanatomical evidence showed the anatomical relationship between the temporomandibular joint innervation with the vestibular system. However, there is no clear evidence regarding if temporomandibular disorders are associated with balance impairments. Therefore, the aims of this study were to assess the clinical relevance of stabilometric features in populations with temporomandibular disorders and to analyze the influence of the mandibular position and visual afference in the balance scores in both healthy and clinical populations. This observational study was conducted in one sample of healthy controls and one sample with temporomandibular disorders. Sociodemographic data (age, gender, height, weight, body mass index, and foot size), clinical data (presence or absence of temporomandibular disorders) and stabilometric data under six different conditions were collected. Sixty-nine subjects (43.5% male; 36.2% patients) were assessed. No differences between Temporomandibular disorders and healthy groups were found in any stabilometric outcomes, unlike oscillation area with closed eyes and medium interscuspidal position (p < 0.01). Although visual feedback showed to be relevant (p < 0.0001), mandibular position produced no differences in any stabilometric measurement (p > 0.05). This study found that healthy subjects and patients with temporomandibular disorders showed no balance differences in the stabilometric outcomes assessed. Although visual input played an important role in the balance, mandibular position seems to be irrelevant.
1. Introduction
Temporomandibular disorders (TMD) are one of the most common orofacial impairment and the second musculoskeletal condition most prevalent (just after chronic low back pain) involving high economic costs [1]. Although several signs have been described in TMD populations including limited range of movement, adventitious sounds (e.g., clicking, crepitus, grating, and popping) and signs of bruxism and craniofacial pain with articular and/or myofascial etiology [2], current evidence is controversial regarding balance and posture alterations [3,4].
Balance could be defined as the result of postural adjustments regulated by a complex system of mechanisms involving several multisensory inputs (e.g., visual, vestibular, auditive, and somatosensory) [5]. Although neuroanatomical evidence is available demonstrating anatomical relationship between trigeminal neurons (receiving afferences from masticatory muscle receptors such as the neuromuscular spindle, Golgi tendon organs, periodontal ligament receptors, and the TMJ free nerve endings) with the vestibular nuclei and trigeminocerebellar links, the importance of these afferences still unclear [6,7]. In fact, recent studies showed that induced changes in the dental occlusion had a positive effect on the neuromuscular coordination and balance [8,9]. The stomatognathic system (characterized by the maxilla and mandible, dental arches, soft tissues, temporomandibular joint—TMJ, masticatory muscles, and orofacial nerves) is a functional unit that shows muscular and ligamentous connections to the cervical region [5,10]. In fact, associated TMD comorbidities including neck pain and headache [11] showed altered balance compared with healthy populations since cervical spine have important connections to the vestibular and visual systems [12,13]. Therefore, the trigeminal afferences to the vestibular system could be regulated by the tonic motricity of the mandible muscles and infer on the fine regulation of orthostatic posture [14].
Although potential associations between balance and temporomandibular joint (TMJ) have been assessed in several studies [14,15,16,17], most of the studies were conducted in healthy populations. Up to our knowledge, specific evidence regarding the clinical relevance of different standing balance parameters in TMD populations is lacking.
Several clinical tests have been proposed to evaluate postural control, including the Romberg test, the Timed Up and Go, the Berg Balance Score, the Tinetti Scale, the Functional Reach Test, or the BESTest (Balance Evaluation Systems Test) [18]. However, since these tests are based on qualitative and subjective aspects of the evaluation and the current opinion of clinicians is to focus on those clinical instruments with acceptable utility (e.g., validity, reliability, specificity, and sensitivity) [19], alternative methods providing objective, valid and reliable data are needed.
Stabilometry is an objective, reliable, and one of the most widely instrument used in clinical practice for studying several balance features associated with functional disorders of the vestibular system [20]. This device is sensitive to the forces applied by the subject to the ground and, assessing the center of pressure and its trajectory, it provides information about the postural response expressed as distances, locations, and velocities.
Therefore, the main objective of this study was to assess the clinical relevance of stabilometric features (e.g., oscillation surface area, oscillation length in both lateral and anteroposterior axes, total oscillation length, comparison of length of movement and covered area, relation between the gravity center speed movement and the average movement on the anteroposterior axis, average of speed variation, and mean speed) in TMD populations. As secondary objective, we aim to analyze the influence of different measurement procedures (mandibular position and visual afference) in the balance scores in both healthy and clinical populations.
2. Materials and Methods
2.1. Study Design
An observational study to assess the association between TMD and stabilometric features including oscillation surface area, oscillation length in both lateral and anteroposterior axes, total oscillation length, comparison of length of movement and covered area, relation between the gravity center speed movement and the average movement on the anteroposterior axis, average of speed variation, and mean speed. This study followed the Strengthening the Reporting of Observational studies in Epidemiology (STROBE) guidelines and checklist [21]. Furthermore, this study was conducted according to the Declaration of Helsinki and approved by the Institutional Ethics Committee of Clinical Research of Camilo José Cela University (UCJC 30-12-2019).
2.2. Participants
Two consecutive samples of patients with TMD and healthy participants were screened for eligibility criteria by using local announcements from September 2020 to December 2020 from a private university located in Spain (Camilo José Cela University).
To be eligible, participants had to be aged between 18 to 65 years (since the peak TMD prevalence occurs in 45-to-64 years old subjects [4]). Exclusion criteria included presence of neurological diseases, lack of dental pieces, prior oral surgery, being under pharmacological or physiotherapy treatment 2 months prior to their participation, being under orthodontic treatment; pregnancy, any underlying medical condition (e.g., trauma, tumor, fractures, etc.), or any other condition affecting the balance or the vestibular system.
In addition to these criteria, specific criteria were applied for both healthy and TMD populations. Participants were excluded from the healthy sample if they presented any orofacial pain episode 6 months prior to their participation in the study. Participants were included in the TMD population following the Axis I physical diagnosis from the new Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) [22] by one experienced examiner and excluded if they presented orofacial pain non-related with TMD. Based on a prior study conducted by Perinetti [6] assessing stabilometric outcomes under different occlusal and visual conditions, this study required at least 26 subjects. Prior to their participation in the study, all participants read and signed the written informed consent.
2.3. Assessments
Sociodemographic data included age, gender, height, weight, body mass index (BMI), and foot size. The clinical assessment included: (a) presence or absence of TMD; and (b) a stabilometric assessment under 6 different conditions combining the visual input (eyes opened and closed) and the occlusal input (inoclussion, medium intercuspidation, and maximum intercuspidation).
As recommended in a recent review conducted by Yamamoto et al. [23], we considered consistent instruments settings, standing posture, position of the feet, recording time, and environmental conditions for all the assessments. All the procedures were conducted in the same room located in Camilo José Cela University (Madrid, Spain) by two experienced raters blinded to the participant allocation (TMD or healthy) with a Fusyo stabilometric platform (Medicapteurs trademark, Toulouse, France). This room was checked to be silent (<40 dB) to avoid acoustic spatial orientation and a normal illumination (40 lx). The recording time for each measurement was set to 60 s with 40 Hz frame rate. Final analyzed scores were calculated as the mean average of 3 trials for all the 6 assessed conditions). Feet position was set in a 30° angle with no heels contact. For recording stabilometric outcomes with opened eyes, a circular visual target with 5 cm diameter was placed 1 m in front of the subject eyes (Figure 1a).
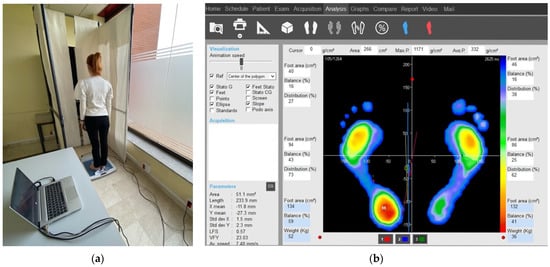
Figure 1.
Participants stabilometric assessment: (a) environmental conditions and (b) software used for measuring balance outcomes.
Stabilometric outcomes assessed included oscillation surface area (Surface), oscillation length in both lateral (ML-Length) and anteroposterior (AP-Length) axes, total oscillation length, comparison of length of movement and covered area (length as a function of the surface or LFS), relation between the gravity center speed movement and the average movement on the anteroposterior axis (Speed variation as a function of AP or SVFAP), average of speed variation (ASV) and mean speed (Figure 1b).
2.4. Statistical Analysis
All statistical analyses were performed using the Statistical Package for the Social Science (SPSS) Version 21 for Mac OS. First, a Kolmogorov—Smirnoff test was performed to verify the normal distribution of the sample (p > 0.05). Regarding the comparability of groups (by gender and healthy and TMD populations) for all the stabilometric parameters and sociodemographic characteristics, Student t-tests for independent samples were used. Regarding within- and between-healthy and TMD populations stabilometric differences with and without visual input, Student t-tests for independent samples were calculated.
Finally, a one-way analysis of variance (ANOVA) test was used in order to investigate the importance of the mandibular position input (inoclussion, medium intercuspidation, and maximum intercuspidation) within both clinical and healthy populations. In case of significant differences, a Bonferroni post hoc analysis was carried out in order to investigate the specific differences between jaw postures within populations. The effect size was estimated using η2 when significant. An effect size of 0.01 was considered small, 0.06 medium and 0.14 large. p values were assumed to be significant only if < 0.017 (Bonferroni correction: 0.05/3) level [24].
3. Results
From a total of 72 volunteers responding to the announcements, three were excluded because of vertigo non associated with TMD. Finally, 69 subjects (43.5% male and 36.2% TMD) were finally included in the analyses. Table 1 summarizes demographic data of the total sample, by gender and presence/absence of TMD. In general, males showed greater height, weight, BMI, and foot size. Thus, populations with TMD showed lower weight, BMI, and foot size scores compared with healthy controls.

Table 1.
Sociodemographic features of the total sample, by gender and health condition.
Data regarding the importance of visual input in stabilometry for both TMD and healthy populations are stated in Table 2. In both populations, an increased oscillation surface, length and mean speed were found (all, p < 0.0001). In addition, the healthy population decreased both AP-Length and SVFAP in closed-eyes measurements compared with opened-eyes (both, p < 0.01). Finally, we found no differences between healthy and TMD populations in closed-eyes measurements in any stabilometric outcome (all, p > 0.05). However, significant differences were found for oscillation surface (p < 0.01), AP-Length (p < 0.01), SVFAP (p < 0.05), and ASV (p < 0.05).

Table 2.
Importance of Visual input for stabilometric features in subjects with and without TMD.
Data from the TMD population in three different occlusal postures reported in Table 3 showed no differences between postures for the assessed variables (all, p > 0.05). Similarly, no differences between mandibular positions were found in healthy subjects (all, p > 0.05) as shown in Table 4.

Table 3.
Importance of mandibular position in stabilometric features in subjects with TMD.

Table 4.
Importance of mandibular position in stabilometric features in healthy subjects.
Finally, stabilometric differences between TMD and healthy populations for each posture assessed are presented in Table 5. No differences were found between populations for none of the assessed outcomes (p > 0.05), but medium intercuspidation with closed eyes (p < 0.01).

Table 5.
TMD and healthy subjects stabilometric differences.
4. Discussion
Although previous studies assessed the association between dental occlusion and visual input with body balance and posture, up to our knowledge, this is the first study analyzing multiple stabilometric features including two samples (healthy volunteers and patients with TMD) under six different conditions for assessing within and between both populations balance differences.
Our results suggested that (1) in general, there are no balance differences between healthy and this TMD clinical populations; (2) mandibular position is not a relevant factor affecting stabilometric balance scores; and (3) although visual afferences play a relevant role in the balance in both populations, surprisingly healthy subjects showed increased oscillation surface, AP-Length, SVFAP and ASV compared with TMD patients.
The TMD sample analyzed in this study showed several sociodemographic characteristics differences with the healthy sample. We found that healthy controls were heavier and showed greater BMI compared with TMD subjects. These results are consistent with the current literature since patients with TMD are more likely to present decreased BMI and abdominal obesity compared with healthy controls [25]. However, it should be considered that other studies found no association between weight nor BMI with TMD [4,26,27]. In addition, foot size differences were found between healthy and TMD populations. Although foot size was included in the multivariable analysis, it should be considered that foot size is negatively correlated with total oscillation length, LFS, and mean speed and positively correlated with ASV and SVFAP and, therefore, affects the differences observed.
Regarding the clinical relevance of balance differences between patients with TMD and healthy subjects, evidence is controversial. Since trigeminal proprioceptive afferences to the vestibular systems are reported, it is suggested that stabilometry could be used for finding relevant balance differences during the clinical practice or research [3]. Although there is evidence supporting balance difference between myogenous TMD and healthy populations (in particular, sway area and mean speed) [28], several evidence did not show a clear association between TMD and postural instability [29,30]. In fact, a previous study found greater sway index, ML-Length, and medial-lateral symmetry scores in healthy populations [31]. Other study conducted in elderly subjects with and without TMD, also found that the presence and severity of TMD, in addition to the presence of pain to palpation of TMJ and masticatory and cervical muscles did not alter the variables related to postural balance in this population [32]. Our results showed no differences between healthy subjects and patients with TMD, but sway area with closed eyes. Therefore, based on our results, we cannot confirm the clinical relevance of stabilometric balance assessment to determine TMD.
We conducted this study assessing the balance under six different conditions. There is an agreement between the lack of changes between mandibular positions (inoclussion, medium intercuspidation, and maximum intercuspidation) and stabilometric outcomes found in this study with prior evidence [3,6]. Manfredini et al. [3] reported in a critical review that stabilometric devices failed to detect changes based on mandibular position and dental occlusion. Thus, Perinetti found no differences between mandibular rest position and dental intercuspidation measurements [6]. In addition, our results are consistent with the literature regarding the visual input importance in balance [6].
Finally, although this study demonstrated that stabilometry showed a poor clinical relevance, it should be considered that several factors could potentially compensate or mask the trigeminal proprioceptive afferences from different types of afferences (e.g., auditive or visual conditions, sociodemographic characteristics, lower limb strength, or somatosensitive afferences) since body balance is regulated by a complex system with a high intrasubject variability.
Limitations
There are some limitations that should be recognized in this study. First, our sample size estimation was based on a previous study which did not reported the sample size calculation. Therefore, this sample and our results could not be representative. Second, although we considered a large number of internal and external variables that could bias the measurements, further studies should consider features which were not considered for this study (e.g., homogeneous weight, BMI, and foot size) and other important covariates in the maintenance of balance and postural control (e.g., lower limb strength and fat mass/lean mass percentage).
5. Conclusions
This study found that healthy subjects and TMD patients showed no balance differences assessed with stabilometry under six different conditions (Eyes: open/closed; Mandibular position: inoclussion/medium intercuspidation/maximum intercuspidation) including oscillation surface, oscillation ML-axis, AP-axis and total length, length as a function of the surface, the speed variation as a function of Y, the average of speed variation, and mean speed in none of the assessed postures, but sway area with closed eyes and medium intercuspidation. Mandibular position showed no influence in stabilometric scores. However, the lack of visual afferences involved greater surface, total oscillation length, and mean speed in both populations.
Author Contributions
Conceptualization, R.D.-D., G.M.G.-S., and M.B.C.-C.; methodology, R.D.-D. and A.E.G.; software, S.O.C.-M.; formal analysis, J.A.V.-C.; investigation, R.D.-D., A.E.G., and S.O.C.-M.; resources, S.O.C.-M.; data curation, J.A.V.-C.; writing—original draft preparation, J.A.V.-C.; writing—review and editing, J.A.V.-C.; supervision, J.A.V.-C.; project administration, R.D.-D. and J.A.V.-C. All authors have read and agreed to the published version of the manuscript.
Funding
The APC was funded by Camilo Jose Cela University (ID: UEMDTT).
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Ethics Committee of Camilo José Cela University (UCJC-30-12-2019).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data that support the findings of this study are available from the first author (R Delgado-Delgado) or the corresponding author (JA Valera-Calero), upon reasonable request.
Conflicts of Interest
The authors declare no conflict of interest and the funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- Valesan, L.F.; Da-Cas, C.D.; Réus, J.C.; Denardin, A.C.S.; Garanhani, R.R.; Bonotto, D.; Januzzi, E.; de Souza, B.D.M. Prevalence of temporomandibular joint disorders: A systematic review and meta-analysis. Clin Oral Investig. 2021, 25, 441–453. [Google Scholar] [CrossRef] [PubMed]
- Ohrbach, R.; Dworkin, S.F. The evolution of TMD diagnosis: Past, present, future. J. Dent. Res. 2016, 95, 1093–1101. [Google Scholar] [CrossRef] [PubMed]
- Manfredini, D.; Castroflorio, T.; Perinetti, G.; Guarda-Nardini, L. Dental occlusion, body posture and temporomandibular disorders: Where we are now and where we are heading for. J. Oral Rehabil. 2012, 39, 463–471. [Google Scholar] [CrossRef]
- Delgado-Delgado, R.; Martínez-Conesa, A.; Valera-Calero, J.A.; Calvo-Moreno, S.O.; Gallego-Sendarrubias, G.M.; Centene-ra-Centenera, M.B. Association between Temporomandibular Disorders with Head and Neck Posture: A Systematic Review. Int. J. Dent. Oral Sci. 2021, 8, 1024–1029. [Google Scholar]
- Cuccia, A.; Caradonna, C. The relationship between the stomatognathic system and body posture. Clinics (Sao Paulo) 2009, 64, 61–66. [Google Scholar] [CrossRef]
- Perinetti, G. Dental occlusion and body posture: No detectable correlation. Gait Posture 2006, 24, 165–168. [Google Scholar] [CrossRef]
- Amaral, A.P.; Politti, F.; Hage, Y.E.; Arruda, E.E.; Amorin, C.F.; Biasotto-Gonzalez, D.A. Immediate effect of nonspecific mandibular mobilization on postural control in subjects with temporomandibular disorder: A single-blind, randomized, controlled clinical trial. Braz. J. Phys. 2013, 17, 121–127. [Google Scholar] [CrossRef]
- Oliveira, S.S.I.; Pannuti, C.M.; Paranhos, K.S.; Tanganeli, J.P.C.; Laganá, D.C.; Sesma, N.; Duarte, M.; Frigerio, M.L.M.A.; Cho, S.C. Effect of occlusal splint and therapeutic exercises on postural balance of patients with signs and symptoms of temporoman-dibular disorder. Clin. Exp. Dent. Res. 2019, 12, 109–115. [Google Scholar] [CrossRef] [PubMed]
- Didier, H.; Assandri, F.; Gaffuri, F.; Cavagnetto, D.; Abate, A.; Villanova, M.; Maiorana, C. The Role of Dental Occlusion and Neuromuscular Behavior in Professional Ballet Dancers’ Performance: A Pilot Study. Healthcare 2021, 9, 251. [Google Scholar] [CrossRef]
- Nitecka-Buchta, A.; Proba, T.; Proba, P.; Stefański, K.; Baron, S. Functional Assessment of the Stomatognathic System, after the Treatment of Edentulous Patients, with Different Methods of Establishing the Centric Relation. Pain Res. Manag. 2018, 2018, 1572037. [Google Scholar] [CrossRef]
- Walczyńska-Dragon, K.; Baron, S.; Nitecka-Buchta, A.; Tkacz, E. Correlation between TMD and cervical spine pain and mobility: Is the whole body balance TMJ related? Biomed. Res. Int. 2014, 2014, 582414. [Google Scholar] [CrossRef] [PubMed]
- Treleaven, J. Sensorimotor disturbances in neck disorders affecting postural stability, head and eye movement control. Man. Ther. 2008, 13, 2–11. [Google Scholar] [CrossRef] [PubMed]
- Hiengkaew, V.; Panichaporn, W.; Thanungkul, S. Postural balance, visual verticality perception, and its association in individuals with and without neck pain. J. Med. Assoc. Thai. 2014, 97 (Suppl. 7), S70–S74. [Google Scholar]
- Gangloff, P.; Perrin, P.P. Unilateral anaesthesia modifies postural control in human subjects. Neurosci. Lett. 2002, 330, 179–182. [Google Scholar] [CrossRef]
- Bracco, P.; Deregibus, A.; Piscetta, R. Effects of different jaw relations on postural stability in human subjects. Neurosci. Lett. 2004, 356, 228–230. [Google Scholar] [CrossRef] [PubMed]
- Gangloff, P.; Louis, J.-P.; Perrin, P.P. Dental occlusion modifies gaze and posture stabilization in human subjects. Neurosci. Lett. 2000, 293, 203–206. [Google Scholar] [CrossRef]
- Cortese, S.; Mondello, A.; Galarza, R.; Biondi, A. Postural alterations as a risk factor for temporomandibular disorders. Acta Odontol. Latinoam. 2017, 30, 57–61. [Google Scholar] [PubMed]
- Leirós-Rodríguez, R.; Romo-Pérez, V.; García-Soidán, J.L.; Soto-Rodríguez, A. Identification of Body Balance Deterioration of Gait in Women Using Accelerometers. Sustainability 2020, 12, 1222. [Google Scholar] [CrossRef]
- Valera-Calero, J.A.; Guodemar-Pérez, J.; Cleland, J.A.; Ojedo-Martín, C.; Gallego-Sendarrubias, G.M. Physical therapist attitude and opinion about cervical spine examination: A national Spanish survey. Int. J. Clin. Pract. 2020, 22, e13781. [Google Scholar] [CrossRef]
- Rodríguez-Rubio, P.R.; Bagur-Calafat, C.; López-de-Celis, C.; Bueno-Gracía, E.; Cabanas-Valdés, R.; Herrera-Pedroviejo, E.; Girabent-Farrés, M. Validity and Reliability of the Satel 40 Hz Stabilometric Force Platform for Measuring Quiet Stance and Dynamic Standing Balance in Healthy Subjects. Int. J. Env. Res. Public Health 2020, 17, 7733. [Google Scholar] [CrossRef]
- Cuschieri, S. The STROBE guidelines. Saudi J. Anaesth. 2019, 13, S31–S34. [Google Scholar] [CrossRef]
- Schiffman, E.; Ohrbach, R.; Truelove, E.; Look, J.; Anderson, G.; Goulet, J.P.; List, T.; Svensson, P.; Gonzalez, Y.; Lobbezoo, F.; et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: Recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group. J. Oral Facial Pain Headache 2014, 28, 6–27. [Google Scholar] [CrossRef]
- Yamamoto, M.; Ishikawa, K.; Aoki, M.; Mizuta, K.; Ito, Y.; Asai, M.; Shojaku, H.; Yamanaka, T.; Fujimoto, C.; Murofushi, T.; et al. Japanese standard for clinical stabilometry assessment: Current status and future directions. Auris Nasus Larynx 2018, 45, 201–206. [Google Scholar] [CrossRef] [PubMed]
- Valera-Calero, A.; Lluch Girbés, E.; Gallego-Izquierdo, T.; Malfliet, A.; Pecos-Martín, D. Endocrine response after cervical manipulation and mobilization in people with chronic mechanical neck pain: A randomized controlled trial. Eur. J. Phys. Rehabil. Med. 2019, 55, 792–805. [Google Scholar] [CrossRef] [PubMed]
- Rhim, E.; Han, K.; Yun, K.I. Association between temporomandibular disorders and obesity. J. Craniomaxillofac. Surg. 2016, 44, 1003–1007. [Google Scholar] [CrossRef] [PubMed]
- Jordani, P.C.; Campi, L.B.; Braido, G.V.V.; Fernandes, G.; Visscher, C.M.; Gonçalves, D.A.G. Obesity, sedentarism and TMD-pain in adolescents. J. Oral Rehabil. 2019, 46, 460–467. [Google Scholar] [CrossRef]
- Jordani, P.C.; Campi, L.B.; Circeli, G.Z.; Visscher, C.M.; Bigal, M.E.; Gonçalves, D.A. Obesity as a risk factor for temporomandibular disorders. J. Oral Rehabil. 2017, 44, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Nota, A.; Tecco, S.; Ehsani, S.; Padulo, J.; Baldini, A. Postural stability in subjects with temporomandibular disorders and healthy controls: A comparative assessment. J. Electromyogr. Kinesiol. 2017, 37, 21–24. [Google Scholar] [CrossRef]
- Ferrario, V.F.; Sforza, C.; Schmitz, J.H.; Taroni, A. Occlusion and center of foot pressure variation: Is there a relationship? J. Prosthet. Dent. 1996, 76, 302–308. [Google Scholar] [CrossRef]
- Delgado-Delgado, R.; Iriarte-Álvarez, N.; Valera-Calero, J.A.; Centenera-Centenera, M.B.; Garnacho-Garnacho, V.E.; Gallego-Sendarrubias, G.M. Association between temporomandibular disorders with clinical and sociodemographic features: An observational study. Int. J. Clin. Pract. 2021, 75, e13961. [Google Scholar] [CrossRef]
- Ries, L.G.; Bérzin, F. Analysis of the postural stability in individuals with or without signs and symptoms of temporomandibular disorder. Braz. Oral Res. 2008, 22, 378–383. [Google Scholar] [CrossRef] [PubMed]
- Oltramari-Navarro, P.V.; Yoshie, M.T.; Silva, R.A.; Conti, A.C.; Navarro, R.L.; Marchiori, L.L.; Fernandes, K.B. Influence of the presence of Temporomandibular Disorders on postural balance in the elderly. Coda 2017, 9, e20160070. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).