Featured Application
This systematic review summarizes the available literature about integration of CBCT scans, digital casts, and facial scans.
Abstract
Background: This systematic review summarizes the current knowledge on the superimposition of three-dimensional (3D) diagnostic records to realize an orthodontic virtual patient. The aim of this study is to analyze the accuracy of the state-of-the-art digital workflow. Methods: The research was carried out by an electronic and manual query effectuated from ISS (Istituto Superiore di Sanità in Rome) on three different databases (MEDLINE, Cochrane Library and ISI WEB OF SCIENCE) up to 31st January 2020. The search focused on studies that superimposed at least two different 3D records to build up a 3D virtual patient—information about the devices used to acquire 3D data, the software used to match data and the superimposition method applied have been summarized. Results: 1374 titles were retrieved from the electronic search. After title-abstract screening, 65 studies were selected. After full-text analysis, 21 studies were included in the review. Different 3D datasets were used: facial skeleton (FS), extraoral soft tissues (ST) and dentition (DENT). The information provided by the 3D data was superimposed in four different combinations: FS + DENT (13 papers), FS + ST (5 papers), ST + DENT (2 papers) and all the types (FS + ST + DENT) (1 paper). Conclusions: The surface-based method was most frequently used for 3D objects superimposition (11 papers), followed by the point-based method (6 papers), with or without fiducial markers, and the voxel-based method (1 paper). Most of the papers analyzed the accuracy of the superimposition procedure (15 papers), while the remaining were proof-of-principles (10 papers) or compared different methods (3 papers). Further studies should focus on the definition of a gold standard. The patient is going to have a huge advantage from complete digital planning when more information about the spatial relationship of anatomical structures are needed: ectopic, impacted and supernumerary teeth, root resorption and angulations, cleft lip and palate (CL/P), alveolar boundary conditions, periodontally compromised patients, temporary anchorage devices (TADs), maxillary transverse deficiency, airway analyses, obstructive sleep apnea (OSAS), TMJ disorders and orthognathic and cranio-facial surgery.
1. Introduction
The use of three-dimensional (3D) data is leading to broader possibilities for daily clinical practice: digital planning may enhance diagnostic accuracy and treatment customization [1,2]. Even if 2D radiographic records such as lateral cephalograms and photographs have been routinely used in orthodontic practice, they present some limitations, as they cannot represent the depth of anatomical structures [3,4]. In orthodontics, 3D imaging can help to plan tooth movement with respect to the thickness and morphology of the alveolar bone envelop, to the roots of the contiguous teeth and their periodontal status [5]. The use of cone-beam computed tomography (CBCT) is justified in every clinical situation where more information about the spatial relationship of anatomical structures is needed: ectopic [6], impacted and supernumerary teeth [7,8], root resorption [9], cleft lip and palate [10,11,12], alveolar boundary conditions, placement of temporary anchorage devices [13], maxillary transverse deficiency [14], airway analyses [15], temporomandibular disorders [16] and orthognathic and cranio-facial surgery [17]. Thanks to the intraoral scanners (IOS), it is possible to have an immediate and accurate digital model of the dental arches. The advantages of a digital impression involve the absence of dimensional changes of the impression material, the efficiency of manipulation, sharing and storage as well as the possibility to realize customized virtual set-ups and CAD-CAM appliances or surgical splints for orthognathic surgery patients. As a limitation, some studies have shown that trueness and precision of intraoral scans may be controversial for full-arch digital impressions, as some imprecision may occur in not spatially defined areas. On the other hand, dental laboratory scanners (DLS) are used to digitize impressions or casts; however, any dimensional change of the impression material or plaster cast will be reproduced on three-dimensional dataset [18]. Recently, facial scanners have been introduced in the market with the purpose of acquiring the 3D image of the patients’ face—this can be useful in aesthetic dentistry for planning the patient’s smile [19]. The integration of 3D data from different anatomical structures (skeleton, dentition and facial soft tissues) allows to obtain a 3D virtual simulation of a patient, as well as to simulate the treatment outcome into the patients’ faces, thus leading to a better communication with colleagues, technicians and patients [1,20] (Figure 1).
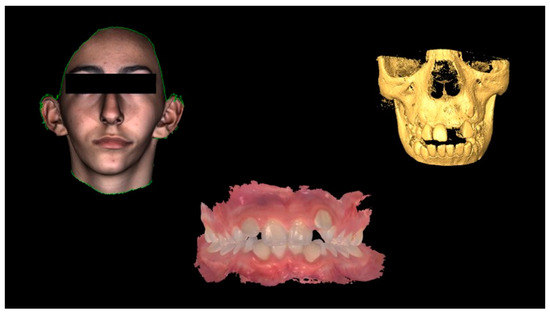
Figure 1.
The three-dimensional workflow (from left to right): 3D image of the face, intraoral impression of the dentition and cone-beam computed tomography (CBCT) scan of the skeleton.
Although 3D data from skeleton, dentition and facial soft tissues are currently available, it is still difficult to merge different data formats in a single planning program—the DICOM (digital imaging and communications in medicine) format for skeletal scaffold, the .STL (standard tessellation language) format or .PLY (polygon file) format for dentition and .OBJ (object code) format for facial soft tissues [21]. The clinicians who approach virtual planning require an accurate, reliable and easy-to-use method for the integration of 3D datasets available in different formats [4]. Despite many procedures that have been described in the recent years, there is still a lack of consensus about a gold standard protocol.
The aim of this systematic review is to summarize the current knowledge about the superimposition methods of three-dimensional diagnostic records and to analyze their declared accuracy.
2. Materials and Methods
On the 31st of January 2020, the electronic search was carried out at the ISS (Istituto Superiore di Sanità of Rome) on three different databases (MEDLINE, Cochrane Library and ISI WEB OF SCIENCE). The search strategy was based on the PICO (patient, intervention, comparison, outcome) criteria modified as previously described by Joda et al. [21,22].
The search strategy was assembled from a combination of qualified medical subject headings (MeSH terms) as key words in simple or multiple conjunctions: (((digital OR virtual OR 3-d OR “3 d” OR 3d OR “three dimensional” OR three-dimensional OR threedimensional OR “3 dimensional” OR 3-dimensional OR 3dimensional) AND (patient OR patients)) OR (cbct OR “cone beam” OR cone-beam OR conebeam OR “CT scan” OR CT-scan OR “computed tomography”) OR (((face OR facial OR extraoral OR extra-oral OR “extra oral” OR intraoral OR intra-oral OR “intra oral”) AND (scan OR scans)) OR photogrammetry OR ((“digital dental” OR digital-dental) AND (cast OR set-up OR “set up” OR setup)))) AND (superimposition OR super-imposition OR “super imposition” OR (data AND (fusion OR matching))) AND (orthodontic OR orthodontics OR ((orthognathic OR maxillofacial OR maxillo-facial OR “maxillo facial” OR orofacial OR oro-facial OR “oro facial”) AND surgery) OR dentistry OR (digital AND smile AND design) OR prosthodontics).
A further manual search was performed on the following journals: American Journal of Orthodontics and Dentofacial Orthopedics, British Journal of Oral and Maxillofacial Surgery, Clinical Implant Dentistry and Related Research, Clinical Oral Implants Research, Dentomaxillofacial Radiology, European Journal of Oral Implantology, European Journal of Orthodontics, Facial and Plastic Surgery Clinics of North America, Implant Dentistry, International Journal of Oral and Maxillofacial Implants, International Journal of Oral and Maxillofacial Surgery, International Journal of Prosthodontics, Journal of Craniomaxillofacial Surgery, Journal of Oral and Maxillofacial Surgery, Journal of Oral Implantology, Journal of Prosthetic Dentistry, Journal of Prosthodontics, Oral Surgery Oral Medicine Oral Pathology and Radiology and Orthodontics and Craniofacial Research.
The selection of the abstracts to be included was independently performed by two researchers (F.M. and E.S.) based on the following inclusion criteria:
- Observational studies (case reports, case series, cohort studies) on humans aimed at creating a 3D virtual dental patient
- Information about the 3D imaging devices used, and the superimposition software employed
- Detailed description of the superimposition method applied
- English language
Doubts about the potential inclusion of an abstract were cleared up by discussion with a third researcher (P.G.).
Only the papers whose whole text was retrieved for full-text analysis were included in the review.
3. Results
Through the developed search strategy, 1374 titles were initially retrieved (Cochrane Library: 65 abstracts; Pubmed: 590 abstracts; ISI web of science: 719 abstracts) and seven papers were further included by manual search. After the screening phase, 63 abstracts and, subsequently, 21 full texts were selected for review (18 from electronic search; 3 from manual search). A total of 21 articles were included in the review (Figure 2).
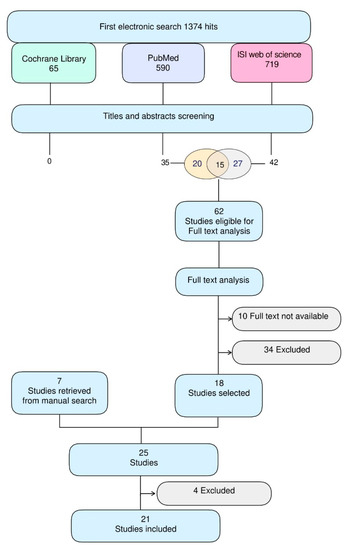
Figure 2.
Flowchart of the review process.
All the included studies were designed as case report, case series or single-cohort clinical investigations; no randomized controlled trials were identified.
To simulate a virtual patient three different 3D datasets were used:
- Facial skeleton (FS): acquired by CBCT or conventional CT scans
- Facial soft tissues (ST): acquired by stereophotogrammetry, laser scanner or 3D photography with a smartphone app.
- Dentition (DENT): acquired by intraoral scanners (IOS) or digitization of plaster casts or dental impression through dental laboratory scanners (DLS).
The 3D data most frequently reported from the selected papers were FS (n = 19), followed by dentition (n = 16) and ST (n = 8).
The 3D data were superimposed according to four different combinations (Figure 3):
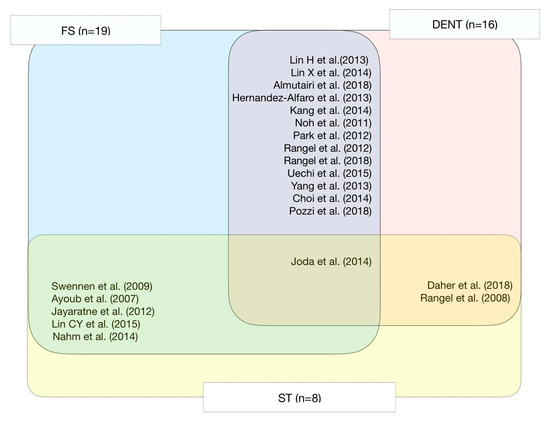
Figure 3.
Summary of the included studies.
- 13 papers merged skeleton with dentition (FS + DENT = 13)
- 5 papers merged skeleton with facial soft tissues (FS + ST = 5)
- 2 paper merged facial soft tissues with dentition (ST + DENT = 2)
- 1 paper integrated all the 3D datasets (FS + ST + DENT = 1)
The included studies performed different superimposition protocols:
- 11 studies used the surface-based method
- 6 studies used the point-based method
- 2 studies compared the surface-based method and point-based method
- 1 article used the voxel-based method
- 1 article compared the voxel-based and surface-based method
Most of the studies retrieved declared as a primary outcome the assessment of the accuracy of the chosen superimposition procedure (n = 15); moreover, the feasibility to simulate a digital patient was analyzed (n = 10) and the accuracy of two different superimposition methods (n = 3) were also analyzed.
The results of the research are summarized in Table 1.

Table 1.
Information on the included studies.
The included studies which declared to analyze of the accuracy of a superimposition procedure or the agreement between the results of different methods were further analyzed [Table 2].

Table 2.
Information on the studies that analyzed the reliability of the registration.
3.1. Descriptive Analysis
3.1.1. Facial Skeleton + Soft Tissue + Dentition
A virtual patient simulation based on three datasets matching technique (FS + ST + DENT) was performed in two studies both reported as a proof-of-principle on a single case. Joda and Gallucci merged intraoral scans of the dentition, CBCT and stereophotogrammetric facial scans to build a 3D virtual patient by means of a surface-based method [18].
3.1.2. Facial Skeleton + Soft Tissue
Ayoub et al. merged stereophotogrammetry and conventional CT data of human faces by a point-based method [23,24]: DICOM and Di3D software (Di3D, Dimensional Imaging, Hillington Park, Glasgow, UK) files were converted into a VRML (virtual reality modelling language) common language by Amira (Thermo Fisher Scientific, Berlin, Germany) and superimposed with a two-step procedure: firstly, Procrustes registration was applied in order to normalize information of size, shape and space, then face and skeleton were matched by means of 10 corresponding landmarks distributed on the entire face area of the human head. Finally, iterative closest point algorithm (ICP) was applied. The registration error was calculated to be ±1.5 mm using the closest point distance from the transformed Di3D skin surface to the transformed CT skin surface. In 2009 Swennen et al. introduced a new approach to acquire a three-dimensional virtual skull model appropriate for orthognathic surgery planning without the use of plaster dental models and without deformation of the facial soft tissue mask named “triple cone-beam computed tomography scan procedure” [25]. This technique, validated on 10 orthognathic patients, required the acquisition of three CBCT scans: a CBCT of the patient with a wax bite wafer in place, a second, low dose, CBCT of the patient with a triple Tray AlgiNot impression in place and third high resolution scan of the impression previously done. The three DICOM files were pre-aligned manually and then overlapped by a triple voxel-base registration (N-1). In order to investigate the accuracy of the procedure, a synthetic skull was used; a supplementary CBCT scan in extended field modus was performed on the synthetic skull with the triple tray in position. The superimposition between this and the scan of the impression has been assumed as a gold standard (N-2); the mean distance between the registered impression scan N-1 and registered impression scan N-2 was 0.08 ± 0.03 mm. Jayaratne et al. evaluated the feasibility of integrating 3D pictures and CBCT images on 29 orthognathic patients [26]. DICOM files of CBCT were converted into the .stl binary format; 3D images of bone and skin were segmented from CBCT scans. Then, 3D data were superimposed using a surface-based method with 3dMDpatient software (3dMD LLC, Atlanta, USA). The root mean square (RMS) between the measured distances was applied to calculate the error of the procedure (0.74 mm for the whole face). Areas surrounding lips and eyes resulted to be the most variable regions in the face during registration, as shown by the color maps. Lin et al. tried to establish how much the CBCT’s field of view (FOV) can influence the superimposition accuracy between scans and full-face stereophotogrammetric images [27]. For 30 patients, 3D facial images and CBCT scans were acquired; the 13 cm FOV (small FOV) scans were simulated from 22 cm FOV (large FOV) ones by deleting the excess files. For each patient, the large FOV scan and the corresponding 3dMD image were imported into VRMesh software and then merged; the same procedure was performed with the small FOV. The study showed the absence of any clinically significant difference in terms of accuracy of superimposition between a large or small FOV.
Nahm et al. introduced a new 3D facial scanner that is combined with a CBCT apparatus to minimize the time lapse between the two registration; consequently, this technique may reduce any bias due to facial mimics or postural changes [28]. An extraoral scan and CBCT were initially superimposed, considering face skin as a reference; hence, the 3D facial image was voxelized, face skin files were extracted from the CBCT by a thresholding process and the two data sets were merged together using Morpheus 3D Software (Morpheus, Gyoung-gi Korea). The registration accuracy of 0.60 ± 0.12 mm was established by the average surface distance of soft tissue surfaces of the CBCT and 3D facial images.
3.1.3. Soft Tissues + Dentition
The possibility to match 3D face scans and intraoral scans was considered by two articles. Rangel et al. published a technical paper showing the integration of a digital dental cast into 3D facial photographs [29]. To superimpose the digital dental casts and the 3D facial images, the anterior teeth and the forehead were used as registration areas; an iterative closest point algorithm was applied to match the 3D data sets in the correct anatomical position. The average surface distance for the anterior teeth was 0.35 ± 0.32 mm. Daher et al. introduced a method to elaborate a 3D digital smile design in a cheap way using an IOS, a smartphone and a designated app [30]; the 3D images were superimposed through a point-based superimposition method using an open-source software (Blender, blender.org).
3.1.4. Facial skeleton + Dentition
Thirteen articles focused on the integration of digital model into CBCT scan. Pozzi et al. introduced the “smiling scan technique” to create a virtual dental patient showing a broad smile under static conditions; this technique is based on the superimposition of two different digital data sets, the DICOM files generated by the cone beam computed tomography (CBCT) scan recorded while the patient displayed a broad smile for the duration of the scan and the STL files obtained by the intraoral optical surface scanning (IOS) or extraoral optical surface scanning (EOS) of the patient’s intraoral anatomy [23]. Noh et al. analyzed the accuracy of the registration between laser-scanned digital models and CBCT scans with a surface-based algorithm [31]. The aim of the study was to compare the accuracy of the registration with three different approaches: the selection of only the buccal side of the teeth, only the lingual side and both sides. The accuracy of the registration was quantified by comparing the mean Euclidean discrepancy between the digital model and the CBCT scan; moreover, color maps were used to visualize the distribution of the 3D displacements. The results showed that the mean 3D deviation was 0.27–0.33 mm. Park et al. proposed the selection of basal bone structure of the mandible as regional registration method to superimpose pre- and post-treatment CBCT scan [32]. They analyzed the accuracy and reliability of the proposed surface-registration by comparing it with a plane registration: the results showed that surface-registration showed higher reliability. Rangel et al. proposed the integration of digital models into CBCT reconstruction by means of external fiducial titanium markers glued to the gingiva [29]. Lin et al. analyzed the influence of image artifacts due to metallic restorations/orthodontic brackets on the surface-based registration of digital models onto CBCT reconstruction; the aim of the study was to compare the accuracy and reliability of the registration of the 3D dataset in two experimental groups (CBCT scan with and without streaking artifacts) [33]. The accuracy of the registration was quantified by comparing the mean Euclidean and root-mean-squared (RMS) discrepancies between digital model and CBCT scan; moreover, color maps were used to visualize the distribution of the 3D displacements. The results showed that the mean deviation between the two groups was 0.13–0.43 mm, while RMS deviation was 0.13–0.53 mm. Yang et al. proposed the integration of digital models into CBCT reconstruction by means of external fiducial titanium markers glued to a palatal plate [34]. The accuracy of the registration was quantified by comparing the mean Euclidean and root-mean-squared (RMS) discrepancies between digital model and CBCT scan. The results showed that the mean deviation between the two groups was less than 0.28 mm, while RMS deviation was 0.13 mm. Hernandez-Alfaro proposed the superimposition of digital models obtained through intraoral scanner onto CBCT scan in order to realize a CAD-CAM splint for orthognathic surgery [35]. Lin X et al. analyzed the accuracy of a five-points-registration between laser-scanned digital model and CBCT reconstruction of a skull model with orthodontic braces (producing artifacts on the CBCT scan) [36]. The accuracy of the registration was quantified by comparing 11 bone-to-tooth linear measurements between the experimental group (digital model + CBCT) and control group (CBCT). The results showed a good reliability since the possibility of a registration error > 0.5 mm was 5%. Kang et al. analyzed the accuracy of a two-step (landmarks- and surface-based) registration of optical-scanned digital models onto CBCT reconstruction of a typodont model with orthodontic braces (producing artifacts on the CBCT scan); the aim of the study was to assess the accuracy of the registration with three different 3D images (optical scan of the digital model, occlusal bite and bite tray impression) [37]. The accuracy of the registration was quantified by comparing the mean Euclidean discrepancy between the digital model and the CBCT scan; moreover, color maps were used to visualize the distribution of the 3D displacements. The results showed that the mean deviations between the digital model and CBCT scan were 0.01 ± 0.11, 0.17 ± 0.18, and 0.47 ± 0.28 for the optical image of the digital dental cast, the occlusal bite and the bite tray impression, respectively. Choi et al. analyzed a model to replace the dental arches into the CBCT reconstruction; the aim of the study was to compare the accuracy of the landmarks- and surface-based registration, and to assess if the number of landmarks (three, five, seven, nine and fourteen) could influence the registration accuracy [38]. The accuracy of the registration was quantified by comparing the mean Euclidean discrepancies between digital models and CBCT scans. The results showed that the mean deviations between the digital model and CBCT scan were 0.12 ± 0.17, 0.18 ± 0.17, 0.20 ± 0.41, 0.16 ± 0.18, 0.18 ± 0.23, 0.20 ± 0.19, 0.17 ± 0.18, and 0.47 ± 0.28 for the surface-based and for the three-, five-, seven-, nine- and fourteen-landmarks-based registration, respectively. Surface-based registration showed the highest accuracy, the number of reference points did not significantly affect the accuracy of landmarks-based registration, however the lowest error was for a seven-points superimposition. Uechi et al. proposed the integration of digital models into CBCT reconstruction by means of external fiducial ceramic markers glued to an occlusal splint; the aim of the study was to assess the accuracy of the surface-based registration of digital models in open-mouth position, inter-cuspal position and centric relation [39]. The accuracy of each registration was quantified by comparing the total root-mean-squared (RMS) Euclidean discrepancy between each pair of fiducial markers on digital model and CBCT scan, while the overall accuracy was quantified by the sum of RMS of the Euclidean distances of three registration procedures. The results showed that the deviations between the digital model and CBCT scan were 0.08 ± 0.05, 0.03 ± 0.02, 0.03 ± 0.02, and 0.12 ± 0.02 for the optical image of the dental cast registration, for the simulation of the inter-cuspal position and the centric relation, and for the overall accuracy, respectively. Almutairi et al. analyzed the accuracy of a three-step (manual-, landmarks- and surface-based) registration of optical-scanned digital models onto CBCT reconstruction of six dried skulls with orthodontic braces (producing artifacts on the CBCT scan) by means of external fiducial dental stone markers tied to the brackets [40]; the aim of the study was to compare the accuracy of the registration of the 3D dataset (experimental group) with a 3D model of the skull obtained using an industrial 3D laser scanner considered as the gold standard (control group). Then, the two groups were merged by both intraoral markers and skull surfaces. The accuracy of the registration was quantified by comparing the 3D discrepancies between the experimental group and the control group dentitions; moreover, color maps were used to visualize the distribution of the 3D displacements. The results showed that the deviations between the experimental group and the control group dentitions were 0.13–0.19 mm and 0.11–0.20 mm when registered on intraoral markers and on skull surfaces, respectively. Rangel et al. proposed a marker-based integration of digital models into CBCT reconstruction by means of five external fiducial titanium markers glued to the gingiva in each jaw; the reference points were extrapolated from the centroid of the external fiducial markers [41]. The aim of the study was to compare the accuracy of the testing protocol (experimental group) with the triple scan procedure proposed by Swennen et al. (control group) [25]. The accuracy of the procedure was quantified by comparing the mean surface-to-surface distances between the experimental group and the control group; moreover, color maps were used to visualize the distribution of the 3D displacements. The results showed that the mean surface-to-surface distances between the experimental group and the control group dentitions were 0.39–0.46 mm and 0.30–0.42 mm for the upper and lower jaw, respectively.
4. Discussion
The innovations in digital technologies have encouraged the research on the simulation of a 3D virtual patient [42]. This progress was evident in this systematic review: 90% of the selected papers have been published in the last decade and 52% within the last five years. Concerning data integration, three methods have been described in literature: voxel-based, point-based and surface-based with or without fiducial markers. Marker-based registration protocols use easily identifiable reference markers that can be clearly identified on anatomical structures [38]. Surface-based registration is an automatic procedure that involves the selection of the surfaces to be matched then, iterative closest point (ICP) algorithm matches the 3D objects to minimize the distance between the selected areas. Two studies compared surface-related and point-related registration: both concluded that the surface-related one has a lower error, as the identification of landmarks is biased from the human perception [32]. Point-based registration is a direct and semi-automatic procedure based on the manual selection of at least three corresponding landmarks on two 3D objects; then, the “least squares” moves the 3D objects to find the best fit for the point pairs. Choi et al. showed that the accuracy does not increase when increasing the number of reference landmarks, and the minimum registration error is when seven corresponding points are considered [38]. Based on the results of that study, a surface-based registration is more accurate than the point-based one; however, a point-based registration is a good option when streaking artifacts impede to identify homologous areas on the CBCT. Voxel-based registration requires to overlap voxels belonging to different CBCT files. Even if this procedure has the lowest registration error declared, it has the inconvenience of necessitating a double radiographic examination, which is associated with an increase of radiation exposure [25]. To keep the radiation dose as low as reasonably achievable (ALARA principles), a 13-cm FOV CBCT scan can be performed with good registration results [36].
Limitations and Strengths
The main limitation of this study was the absence of a gold standard approach; since the studies were heterogeneous in the selection of the patient sample, in the choice of reference points or areas, a statistical comparative analysis of the results achieved was not possible. Furthermore, only two studies indicated a “gold standard” as a reference; [25,40] however, both the articles did not assess sensitivity, specificity and reliability of the methods [43]. Even though the methods currently present in literature cannot be compared in accuracy, we evaluated the level of agreement among different studies through a descriptive analysis.
5. Conclusions
The possibility to simulate a virtual patient represents an important step towards a personalized diagnostic and therapeutic approach [44,45,46]. Future investigations would focus on the analysis of the effective clinical advantages that the patient can get from a simplified digital planning. A comparison between patients’ digital and conventional planning would allow to understand the effectiveness of the digital technology in the short- (short chair-side time, fewer controls, less patient’s discomfort) and long-term (stability of the results, incidence of relapse) treatment outcomes.
Author Contributions
Conceptualization, F.M. and E.S.; methodology, P.G.; software, E.S.; validation, F.M., P.G. and E.S.; formal analysis, F.M. and E.S.; investigation, F.M., E.S. and M.A.Z.; resources, P.G.; data curation, F.M., E.S. and M.A.Z.; writing—original draft preparation, F.M. and E.S.; writing—review and editing, E.S.; visualization, A.R.; supervision, C.G.; project administration, P.G.; funding acquisition, P.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Acknowledgments
We are pleased to thank Bruno Oliva and Nicola Vanacore for the methodological validation of the present study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Mangano, F.; Shibli, J.A.; Fortin, T. Digital Dentistry: New Materials and Techniques. Int. J. Dent. 2016, 2016, 5261247. [Google Scholar] [CrossRef] [PubMed]
- Van Noort, R. The future of dental devices is digital. Dent. Mater. 2012, 28, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Botticelli, S.; Verna, C.; Cattaneo, P.M.; Heidmann, J.; Melsen, B. Two- versus three-dimensional imaging in subjects with unerupted maxillary canines. Eur. J. Orthodont. 2011, 33, 344–349. [Google Scholar] [CrossRef] [PubMed]
- Staderini, E.; Guglielmi, F.; Cornelis, M.A.; Cattaneo, P.M. Three-dimensional prediction of roots position through cone-beam computed tomography scans-digital model superimposition: A novel method. Orthodo. Craniofac. Res. 2019, 22, 16–23. [Google Scholar] [CrossRef] [PubMed]
- Tepedino, M.; Franchi, L.; Fabbro, O.; Chimenti, C. Post-orthodontic lower incisor inclination and gingival recession-a systematic review. Prog. Orthod. 2018, 19, 17. [Google Scholar] [CrossRef]
- Tepedino, M.; Chimenti, C.; Masedu, F.; Iancu Potrubacz, M. Predictable method to deliver physiologic force for extrusion of palatally impacted maxillary canines. Am. J. Orthod. Dentofac. Orthop. 2018, 153, 195–203. [Google Scholar] [CrossRef]
- Laurenziello, M.; Montaruli, G.; Gallo, C.; Tepedino, M.; Guida, L.; Perillo, L.; Troiano, G.; Lo Muzio, L.; Ciavarella, D. Determinants of maxillary canine impaction: Retrospective clinical and radiographic study. J. Clin. Exp. Dent. 2017, 9, e1304–e1309. [Google Scholar] [CrossRef]
- Lai, C.S.; Bornstein, M.M.; Mock, L.; Heuberger, B.M.; Dietrich, T.; Katsaros, C. Impacted maxillary canines and root resorptions of neighbouring teeth: A radiographic analysis using cone-beam computed tomography. Eur. J. Orthodont. 2013, 35, 529–538. [Google Scholar] [CrossRef]
- Bouwens, D.G.; Cevidanes, L.; Ludlow, J.B.; Phillips, C. Comparison of mesiodistal root angulation with posttreatment panoramic radiographs and cone-beam computed tomography. Am. J. Orthod. Dentofac. Orthop. 2011, 139, 126–132. [Google Scholar] [CrossRef]
- Rizzo, M.I.; Zadeh, R.; Bucci, D.; Palmieri, A.; Monarca, C.; Staderini, E.; Oliva, G.; Candida, E.; Gallenzi, P.; Cordaro, M.; et al. Volumetric analysis of cleft lip deformity using 3D stereophotogrammetry. Annali Italiani Di Chirurgia 2019, 90, 281–286. [Google Scholar]
- Staderini, E.; De Luca, M.; Candida, E.; Rizzo, M.I.; Rajabtork Zadeh, O.; Bucci, D.; Zama, M.; Lajolo, C.; Cordaro, M.; Gallenzi, P. Lay People Esthetic Evaluation of Primary Surgical Repair on Three-Dimensional Images of Cleft Lip and Palate Patients. Medicina (Kaunas, Lithuania) 2019, 55, 576. [Google Scholar] [CrossRef] [PubMed]
- Staderini, E.; Patini, R.; Camodeca, A.; Guglielmi, F.; Gallenzi, P. Three-Dimensional Assessment of Morphological Changes Following Nasoalveolar Molding Therapy in Cleft Lip and Palate Patients: A Case Report. Dent. J. 2019, 7, 27. [Google Scholar] [CrossRef] [PubMed]
- Cornelis, M.A.; Tepedino, M.; Cattaneo, P.M.; Nyssen-Behets, C. Root repair after damage due to screw insertion for orthodontic miniplate placement. J. Clin. Exp. Dent. 2019, 11, e1133–e1138. [Google Scholar] [CrossRef] [PubMed]
- Staderini, E.; Patini, R.; De Luca, M.; Gallenzi, P. Three-dimensional stereophotogrammetric analysis of nasolabial soft tissue effects of rapid maxillary expansion: A systematic review of clinical trials. Acta Otorhinolaryngol. Ital. Organo Uff. Della Soc. Ital. di Otorinolaringol. e Chirurgia Cervico-Facciale 2018, 38, 399–408. [Google Scholar] [CrossRef]
- Feng, X.; Li, G.; Qu, Z.Y.; Liu, L.; Nasstrom, K.; Shi, X.Q. Comparative analysis of upper airway volume with lateral cephalograms and cone-beam computed tomography. Am. J. Orthod. Dentofac. Orthop. 2015, 147, 197–204. [Google Scholar] [CrossRef]
- Huang, X.; Cen, X.; Liu, J. Effect of protraction facemask on the temporomandibular joint: A systematic review. BMC Oral Health 2018, 18, 38. [Google Scholar] [CrossRef]
- Saponaro, G.; Doneddu, P.; Gasparini, G.; Staderini, E.; Boniello, R.; Todaro, M.; D’Amato, G.; Pelo, S.; Moro, A. Custom made onlay implants in peek in maxillofacial surgery: A volumetric study. Childs Nerv. Syst. 2020, 36, 385–391. [Google Scholar] [CrossRef]
- Winkler, J.; Gkantidis, N. Trueness and precision of intraoral scanners in the maxillary dental arch: An in vivo analysis. Sci. Rep. 2020, 10, 1172. [Google Scholar] [CrossRef]
- Joda, T.; Gallucci, G.O. The virtual patient in dental medicine. Clin. Oral Implants Res. 2015, 26, 725–726. [Google Scholar] [CrossRef]
- Mangano, C.; Luongo, F.; Migliario, M.; Mortellaro, C.; Mangano, F.G. Combining Intraoral Scans, Cone Beam Computed Tomography and Face Scans: The Virtual Patient. J. Craniofac. Surg. 2018, 29, 2241–2246. [Google Scholar] [CrossRef]
- Joda, T.; Bragger, U.; Gallucci, G. Systematic Literature Review of Digital Three-Dimensional Superimposition Techniques to Create Virtual Dental Patients. Int. J. Oral Maxillofac. Implants 2015, 30, 330–337. [Google Scholar] [CrossRef] [PubMed]
- Efstratiadis, S.; Baumrind, S.; Shofer, F.; Jacobsson-Hunt, U.; Laster, L.; Ghafari, J. Evaluation of Class II treatment by cephalometric regional superpositions versus conventional measurements. Am. J. Orthod. Dentofac. Orthop. 2005, 128, 607–618. [Google Scholar] [CrossRef] [PubMed]
- Pozzi, A.; Arcuri, L.; Moy, P.K. The smiling scan technique: Facially driven guided surgery and prosthetics. J. Prosthodont. Res. 2018, 62, 514–517. [Google Scholar] [CrossRef] [PubMed]
- Ayoub, A.F.; Xiao, Y.; Khambay, B.; Siebert, J.P.; Hadley, D. Towards building a photo-realistic virtual human face for craniomaxillofacial diagnosis and treatment planning. Int. J. Oral Maxillofac. Surg. 2007, 36, 423–428. [Google Scholar] [CrossRef]
- Swennen, G.R.J.; Mollemans, W.; De Clercq, C.; Abeloos, J.; Lamoral, P.; Lippens, F.; Neyl, N.; Casselman, J.; Schutyser, F. A Cone-Beam Computed Tomography Triple Scan Procedure to Obtain a Three-Dimensional Augmented Virtual Skull Model Appropriate for Orthognathic Surgery Planning. J. Craniofac. Surg. 2009, 20, 297–307. [Google Scholar] [CrossRef] [PubMed]
- Jayaratne, Y.S.N.; McGrath, C.P.J.; Zwahlen, R.A. How Accurate Are the Fusion of Cone-Beam CT and 3-D Stereophotographic Images? PLoS ONE 2012, 7, e49585. [Google Scholar] [CrossRef]
- Lin, C.Y.; Hsung, T.C.; Khambay, B. Reducing cone beam CT scan height as a method of radiation reduction for photorealistic three-dimensional orthognathic planning. J. Cranio-Maxillofac.Surg. 2015, 43, 907–912. [Google Scholar] [CrossRef]
- Nahm, K.Y.; Kim, Y.; Choi, Y.S.; Lee, J.; Kim, S.H.; Nelson, G. Accurate registration of cone-beam computed tomography scans to 3-dimensional facial photographs. Am. J. Orthod. Dentofac. Orthop. 2014, 145, 256–264. [Google Scholar] [CrossRef]
- Rangel, F.A.; Maal, T.J.J.; Berge, S.J.; van Vlijmen, O.J.C.; Plooij, J.M.; Schutyser, F.; Kuijpers-Jagtman, A.M. Integration of digital dental casts in 3-dimensional facial photographs. Am. J. Orthod. Dentofac. Orthop. 2008, 134, 820–826. [Google Scholar] [CrossRef]
- Daher, R.; Ardu, S.; Vjero, O.; Krejci, I. 3D Digital Smile Design With a Mobile Phone and Intraoral Optical Scanner. Compend. Contin. Educ. Dent. 2018, 39, e5–e8. [Google Scholar]
- Noh, H.; Nabha, W.; Cho, J.H.; Hwang, H.S. Registration accuracy in the integration of laser-scanned dental images into maxillofacial cone-beam computed tomography images. Am. J. Orthod. Dentofac. Orthop. 2011, 140, 585–591. [Google Scholar] [CrossRef] [PubMed]
- Park, T.J.; Lee, S.H.; Lee, K.S. A method for mandibular dental arch superimposition using 3D cone beam CT and orthodontic 3D digital model. Korean J. Orthod. 2012, 42, 169–181. [Google Scholar] [CrossRef] [PubMed]
- Lin, H.H.; Chiang, W.C.; Lo, L.J.; Hsu, S.S.P.; Wang, C.H.; Wan, S.Y. Artifact-Resistant Superimposition of Digital Dental Models and Cone-Beam Computed Tomography Images. J. Oral Maxillofac. Surg. 2013, 71, 1933–1947. [Google Scholar] [CrossRef] [PubMed]
- Yang, W.M.; Ho, C.T.; Lo, L.J. Automatic Superimposition of Palatal Fiducial Markers for Accurate Integration of Digital Dental Model and Cone Beam Computed Tomography. J. Oral Maxillofac. Surg. 2015, 73. [Google Scholar] [CrossRef]
- Hernandez-Alfaro, F.; Guijarro-Martinez, R. New protocol for three-dimensional surgical planning and CAD/CAM splint generation in orthognathic surgery: An in vitro and in vivo study. Int. J. Oral Maxillofac. Surg. 2013, 42, 1547–1556. [Google Scholar] [CrossRef]
- Lin, X.; Chen, T.; Liu, J.; Jiang, T.; Yu, D.; Shen, S.G. Point-based superimposition of a digital dental model on to a three-dimensional computed tomographic skull: An accuracy study in vitro. Br. J. Oral Maxillofac. Surg. 2015, 53, 28–33. [Google Scholar] [CrossRef]
- Kang, S.H.; Lee, J.W.; Lim, S.H.; Kim, Y.H.; Kim, M.K. Dental image replacement on cone beam computed tomography with three-dimensional optical scanning of a dental cast, occlusal bite, or bite tray impression. Int. J. Oral Maxillofac. Surg. 2014, 43, 1293–1301. [Google Scholar] [CrossRef]
- Choi, Y.S.; Kim, M.K.; Lee, J.W.; Kang, S.H. Impact of the number of registration points for replacement of three-dimensional computed tomography images in dental areas using three-dimensional light-scanned images of dental models. Oral Radiol. 2014, 30, 32–37. [Google Scholar] [CrossRef]
- Uechi, J.; Tsuji, Y.; Konno, M.; Hayashi, K.; Shibata, T.; Nakayama, E.; Mizoguchi, I. Generation of virtual models for planning orthognathic surgery using a modified multimodal image fusion technique. Int. J. Oral Maxillofac. Surg. 2015, 44, 462–469. [Google Scholar] [CrossRef]
- Almutairi, T.; Naudi, K.; Nairn, N.; Ju, X.Y.; Whitters, J.; Ayoub, A. Replacement of the Distorted Dentition of the Cone-Beam Computed Tomography Scans for Orthognathic Surgery Planning. Int. J. Oral Maxillofac. Surg. 2018, 76, 1561.e1–1561.e8. [Google Scholar] [CrossRef]
- Rangel, F.A.; Maal, T.J.J.; de Koning, M.J.J.; Bronkhorst, E.M.; Berge, S.J.; Kuijpers-Jagtman, A.M. Integration of digital dental casts in cone beam computed tomography scans-a clinical validation study. Clin. Oral Invest. 2018, 22, 1215–1222. [Google Scholar] [CrossRef] [PubMed]
- Staderini, E.; Patini, R.; Guglielmi, F.; Camodeca, A.; Gallenzi, P. How to Manage Impacted Third Molars: Germectomy or Delayed Removal? A Systematic Literature Review. Medicina (Kaunas) 2019, 55, 79. [Google Scholar] [CrossRef] [PubMed]
- Patini, R.; Staderini, E.; Camodeca, A.; Guglielmi, F.; Gallenzi, P. Case Reports in Pediatric Dentistry Journals: A Systematic Review about Their Effect on Impact Factor and Future Investigations. Dent. J. 2019, 7, 103. [Google Scholar] [CrossRef] [PubMed]
- Farronato, M.; Maspero, C.; Abate, A.; Grippaudo, C.; Connelly, S.T.; Tartaglia, G.M. 3D cephalometry on reduced FOV CBCT: Skeletal class assessment through AF-BF on Frankfurt plane-validity and reliability through comparison with 2D measurements. Eur. Radiol. 2020. [Google Scholar] [CrossRef]
- Lo Giudice, A.; Ronsivalle, V.; Grippaudo, C.; Lucchese, A.; Muraglie, S.; Lagravere, M.O.; Isola, G. One Step before 3D Printing-Evaluation of Imaging Software Accuracy for 3-Dimensional Analysis of the Mandible: A Comparative Study Using a Surface-to-Surface Matching Technique. Materials (Basel) 2020, 13, 2798. [Google Scholar] [CrossRef]
- Muraglie, S.; Leonardi, R.; Aboulazm, K.; Stumpo, C.; Loreto, C.; Grippaudo, C. Evaluation of structural skeletal asymmetry of the glenoid fossa in adult patients with unilateral posterior crossbite using surface-to-surface matching on CBCT images. Angle Orthod 2020, 90, 376–382. [Google Scholar] [CrossRef]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).