Abstract
In the United States, Chronic Kidney Disease (CKD) affects approximately 1 in 7 adults. Despite its significant impact, CKD awareness, education, and screening are often lacking among underserved Latine populations, leading to poorer health outcomes and higher mortality rates. Various studies highlight the crucial role of Community Health Workers (CHWs) in improving health outcomes within minority communities both domestically and globally. However, there remains a gap in research on the acceptance and effectiveness of CHW-led interventions targeting CKD. This prospective intervention study employed a pre-post quasi-experimental design to evaluate a CHW-led educational program aimed at enhancing CKD knowledge, screening, and monitoring among Latines with low health literacy and English proficiency. CHWs utilized a culturally tailored CKD Flipchart, and 100 underserved patients received the intervention. Feedback from 85 participants who completed post-intervention surveys indicated high satisfaction with the program’s relevance and the professionalism of the CHWs. Importantly, 85% expressed a positive intention to seek kidney care following the intervention. Preliminary analysis of medical records before and after the intervention showed improvements in glycemic control (median change = −18.0, p = 0.014) and triglyceride levels (median change = −29.0, p = 0.035), suggesting the program’s effectiveness in managing CKD risk factors. These findings highlight the potential of CHW-led interventions to reduce kidney health disparities among underserved communities.
1. Introduction
In the United States (U.S.), Chronic Kidney Disease (CKD) affects approximately 37 million adults—1 in every 7 adults—and an additional 20 million have risk factors for its development [1,2]. Despite patient awareness and education being recognized as essential components and priorities of CKD prevention and management, supported by international guidelines and organizations [3,4], approximately 90% of patients with CKD are unaware of their condition [1,5,6]. Medically underserved and vulnerable populations bear a disproportionate burden of CKD and experience worse outcomes, including higher mortality [7,8].
Latine individuals represent the U.S.’s largest ethnic/racial minority group, with approximately 14% of Latine adults having CKD at rates paralleling those found in the general population [9,10,11]. Compounding this risk is the fact that Latine individuals have a faster progression to kidney failure—they are 1.3 times more likely to develop kidney failure compared to non-Latine White individuals [9,11]. This disparity is likely attributable to socioeconomic factors, including education, language, and a lack of health insurance [12,13,14,15,16]. The lack of recognition and education about CKD leaves Latine patients, families, and the healthcare system unaware of a substantial future risk of poor outcomes, including cardiovascular events, the need for urgent dialysis, and decreased quality of life [17,18,19,20,21,22,23].
Therefore, education is a necessary component of a comprehensive strategy to improve kidney health outcomes in Latine communities, aiming to increase awareness, enhance prevention, and promote the control of known risk factors [24,25,26,27,28,29]. Ensuring that Latine patients receive culturally and linguistically appropriate educational support is crucial for establishing greater social equity in CKD [30,31,32,33]. Additionally, it is important to note that Latine individuals are a complex and heterogeneous ethnic group, comprising individuals from various cultures, racial/genetic backgrounds, socioeconomic levels, and countries of origin.
In the United States, the National Kidney Foundation and numerous authors have acknowledged the crucial role of Community Health Workers (CHWs) in identifying, preventing, and managing the risks associated with CKD and ultimately improving outcomes for all affected individuals [34]. For instance, initiatives such as “Promotoras de Salud” have demonstrated effectiveness in improving blood pressure and fostering adherence to healthcare [35]. Studies investigating CHW-led interventions targeting diabetes management have reported reductions in depressive symptoms, enhancements in diabetes social support, and improvements in understanding diabetes self-management [36]. Furthermore, these interventions have been associated with increased engagement in type 2 diabetes self-care activities and reductions in hemoglobin A1C levels [37]. Another noteworthy intervention, the “Familias Sanas, in Spanish” program, involves health promoters educating Latino families about CKD, focusing on prevention and the management of risk factors such as diabetes and hypertension [38]. Moreover, among Latinos with poorly controlled diabetes, a 1-year community health worker intervention was associated with improvements in self-reported access to care [39].
Likewise, in Indigenous communities in Australia, a similar model of CHWs, known as Indigenous Health Workers (IHWs), has been implemented. These workers have played a crucial role in managing CKD by educating communities about the disease and facilitating access to tests and treatments [40]. CHWs have been instrumental in reducing the prevalence of CKD in these communities by improving education and prevention [41,42]. In India, community health workers have been used to combat the high incidence of CKD related to diabetes and hypertension. Programs like “The Jan Arogya Abhiyan” have integrated these workers into primary healthcare to provide education and support in managing CKD [41]. This approach to increasing awareness and disease monitoring has improved adherence to treatment regimens and reduced complications associated with CKD [42].
Despite the growing body of evidence supporting the use of CHW programs in CKD and diabetes [43,44,45,46,47,48], there remains a dearth of research investigating the acceptability and effectiveness of CHW-led interventions in addressing CKD unawareness and lack of screening for CKD [49,50,51], particularly in underserved Latine communities. To bridge this gap, this study assessed the acceptability and effectiveness of a CHW-led education intervention targeting underserved Latine individuals aimed at increasing (a) CKD knowledge and (b) CKD screening/monitoring. The intervention utilized a culturally and linguistically appropriate flipchart co-created by patients and CHWs. This research provides a window into how CHW-led interventions are perceived and experienced by Latine CKD patients.
2. Materials and Methods
2.1. Study Design
This prospective intervention study, employing a pre-post quasi-experimental design, evaluates the acceptability and early impact of a CHW-led educational intervention. We recruited 100 Latine patients diagnosed with type 2 diabetes (T2D) and hypertension who are at risk of or have Chronic Kidney Disease (CKD) and who received care at the largest free healthcare clinic in Florida. The clinic offers comprehensive services—including free medical, vision, dental, social, nutrition, and mental healthcare—to uninsured individuals living in poverty in Palm Beach County. It also features a specialized CKD clinic with volunteer nephrologists, hypertension specialists, nurse practitioners, renal dietitians, social workers, and trained CHWs. Additionally, the health education department provides periodic one-on-one and group workshops for patients with diabetes, hypertension, cardiovascular disease, and CKD.
2.2. Intervention Development
In the first phase of our study (CARE 1.0), we effectively integrated Community-Engaged Research principles with a Human-Centered Design approach to co-create CKD-patient education materials in Spanish [43]. This partnership involved the participation of Latine patients and community health workers (CHWs) from different Latine subgroups and resulted in the development of various CKD education prototypes, including a flipchart intended for use in one-on-one education delivered by CHWs. In the second phase (CARE 2.0), we conducted a pilot education intervention aimed at increasing CKD knowledge, screening, and monitoring among Latine patients with low health literacy and English proficiency and living in under-resourced communities using this culturally tailored CKD flipchart and evaluated the patients’ perspectives on the acceptability and effectiveness of this intervention. The co-created flipchart addressed CKD topics such as definition, diagnosis, lab interpretation, prevention, management, lifestyle modifications, medication adherence, and navigating the healthcare system in the community-based free clinic. Participants also received a CKD handout summarizing the educational content, including a graphic of CKD stages, disease progression risks based on eGFR and urine albuminuria, and therapeutic targets for diabetes and blood pressure control to prevent or delay CKD progression.
The educational intervention aimed to raise awareness about Chronic Kidney Disease (CKD) among patients with diabetes and hypertension and to promote regular CKD screening and monitoring to prevent disease progression. This intervention was built upon findings from the CARE 1.0 study [43], which identified barriers such as fear, low-risk perception, and poor understanding of CKD. To address these issues, the intervention sought to improve CKD knowledge in a culturally relevant manner, helping patients understand CKD stages, interpret lab results, and access appropriate medical and nutritional care. Additionally, it connected uninsured patients with free medical, social, nutritional, and educational services provided by the clinic’s CKD program. Delivered by trained CHWs using the CKD-Flipchart, the sessions lasted 45 min to 1 h, depending on individual needs, and were conducted in Spanish to ensure accessibility.
2.3. Training of CHWs
Twelve Latine CHWs from diverse communities (Mexico, Colombia, Peru, Puerto Rico, Cuba, Venezuela, and Uruguay) underwent 20 h of training.
The curriculum included CKD flipchart content, effective communication strategies using motivational interviewing techniques [52], cultural competence, and navigation of free CKD clinic services and community resources. The training also covered how to assist patients with arranging medical appointments, laboratory tests, transportation, accessing CKD educational resources, food and nutrition services, and navigating free clinic services in. general. Additionally, CHWs were instructed in basic research methodology, including survey administration for post-intervention assessment. They collaborated with the research team to develop and iteratively review surveys, aiming to evaluate CKD knowledge and the acceptability of the intervention.
2.4. Recruitment of Patients
Recruitment approaches included various methods to reach potential participants. Initially, the Electronic Medical Record (EMR) of the community health center site of the research study was queried to identify individuals who meet the following criteria: (a) Latine, (b) aged 18 years or older, (c) diagnosed with Type 2 Diabetes (T2D) or displaying laboratory results consistent with T2D (HbA1C > 7%), (d) medical diagnosis of hypertension, (e) eligible to receive free medical and social services, and (f) not having received any previous CKD education. Also, collaboration with community partners was utilized to target patients with T2D and hypertension. This outreach strategy was conducted by project staff, who set up tables at prominent community locations to promote the study. All participants were eligible to receive services at this community-based clinic. Eligibility requirements include being uninsured, living at or below 200% of the federal poverty level [53], and residing in Palm Beach County, Florida.
2.5. Assessment and Measurements of Acceptability and Effectiveness
We utilized a comprehensive approach to assess acceptability and effectiveness. Acceptability was evaluated based on a framework [54], employing self-report measures in surveys co-developed by the research team, which included members of the community and trained CHWs. For acceptability measurements, we co-developed a questionnaire comprising 9 questions based on the framework [54]. These questions included inquiries such as the perceived usefulness of the education on kidney disease, satisfaction with the support received by CHWs, and intentions to recommend the education to others, among others. Responses were rated on a scale from 1 to 5, with varying degrees of agreement or usefulness.
To gauge effectiveness, we compared baseline and post-intervention CKD self-reported knowledge and participants’ behavioral intention [55] toward kidney healthcare, specifically the likelihood of attending medical appointments with primary doctors or kidney specialists for CKD screening and disease monitoring after receiving the CHW-led education. CKD knowledge was assessed indirectly; instead of a formal test using scores, we asked participants if they felt their knowledge had increased due to the intervention. This approach provided insights into the perceived impact of the educational materials and the CHW-led education, though it did not quantify actual CKD knowledge score changes. We used a scale where participants rated their knowledge from 1 (“I do not know anything”) to 4 (“I know a lot”) for both the pre- and post-intervention assessments. This methodology is commonly used when direct measurement of knowledge change is not feasible, and subjective perceptions of learning and impact are valued in such evaluations [55,56,57,58,59,60].
Additionally, we implemented a questionnaire to indicate participants’ behavioral intention [55] toward kidney healthcare, specifically the likelihood of seeking medical appointments with primary doctors or kidney specialists for CKD screening and disease monitoring after receiving CHW-led education. Responses ranged from “extremely unlikely” to “extremely likely” on a scale from 1 to 5.
All surveys for acceptability and effectiveness (indirect CKD knowledge assessment, behavioral intention) were co-developed in collaboration with the community and underwent iterative reviews until the final version was refined. Given the low health and numeracy literacy of the patient population, the research team leveraged previous experiences with community-engaged methodologies, including insights from the CARE 1.0 study and the formation of a CKD advisory board [43]. Phone surveys were administered within three weeks post-intervention by a CHW who was not involved in delivering the intervention. For exploratory purposes, we collected preliminary data from electronic medical records (EMR) to assess the early impact of the intervention on biochemical parameters. These data included blood pressure, glycemic control, estimated Glomerular Filtration Rate (eGFR), and urinary albumin-to-creatinine ratio (uACR), which were compared before and after the intervention. All EMR data were collected within the three-month window both before and after the intervention.
2.6. Statistical Analysis
The statistical analysis encompassed several methods to comprehensively assess the data. The Kolmogorov–Smirnov test was initially utilized to ascertain the normality of the quantitative data distribution, while Levene’s test was employed to ensure the equality of variances. Quantitative variables with a normal distribution were presented as the mean ± standard deviation. For non-normally distributed quantitative data or ordinal data, such as Likert-type scales, the median and interquartile range (25th–75th percentile, Q1–Q3) were employed. Categorical variables were analyzed using odds ratios (OR) with 95% confidence intervals and the Fisher’s exact test. Intragroup data (before vs. after) were compared using the Wilcoxon signed-rank test, while the Mann–Whitney U test was utilized for intergroup comparisons of quantitative data with a non-normal distribution. Changes in biochemical parameter values were calculated by subtracting the post-intervention value from the pre-intervention value. Additionally, to assess the predictive capacity of various variables for a patient’s refusal to visit the doctor and undergo renal function tests, the areas under the ROC curve (AUCs) were calculated along with their 95% confidence intervals and corresponding p-values. All statistical analyses were conducted using SPSS software, version 20 (IBM Corp., Armonk, NY, USA) [61].
3. Results
Figure 1 presents a flow diagram illustrating the total number of charts reviewed, participants invited and enrolled, and the number of participants who completed the study or were lost to follow-up. This diagram provides a visual summary of the participant flow. Table 1 provides a comprehensive overview of the demographic, clinical, and socioeconomic characteristics of the sample (n = 100). The average age of participants was 55.6 years, with a standard deviation of 10.5 years. Notably, the majority of participants identified as female (68%) and hail from various Latin American countries, including Mexico, Guatemala, Honduras, El Salvador, Nicaragua, and Colombia. Among the sample, 82% had T2D, 75% had hypertension, and 13% had CKD, ranging from stages 1 to 4. Among the CHWs, 11 were female and 1 was male, with an average age of 52 years and a range of experience from 0 to 15 years (with a median experience of 9 years). Following the intervention, 85 out of 100 patients completed the post-intervention evaluation. Of these, 51 had laboratory work and medical visits documented in the EMR during the 3-month study period.
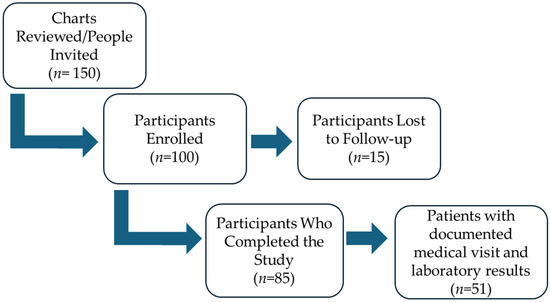
Figure 1.
Flow chart of study participation.

Table 1.
Characteristics of patient participants.
3.1. CKD Knowledge Assessment
Table 2 presents a comparison of patients’ perceptions of their knowledge levels about kidney disease topics before and after the educational intervention. Of all participants who received the education and answered post-intervention questionnaires (n = 85), only 7 patients were aware they had CKD.

Table 2.
Patient’s perception of their knowledge level regarding kidney disease topics before and after the educational intervention.
3.2. Gender Differences in the Impact of Educational Intervention and Risk Perception in Kidney Disease Knowledge
Regarding the perception of “knowing quite a lot/a lot” about the 9 analyzed topics of kidney disease, it was observed that before the educational intervention, women exhibited a lower number of mastered topics (median 0, Q1–Q3 = 0–2) compared to men (median 1, Q1–Q3 = 0–3) (p = 0.022, Mann–Whitney U test). However, after the intervention, both women (median 9, Q1–Q3 = 7–9) and men (median 9, Q1–Q3 = 8–9) did not display differences in the number of topics they reported “knowing quite a lot/a lot” (p = 0.330, Mann–Whitney U test). Moreover, individuals classified as having “high risk” to “extremely high risk of kidney disease progression” or not did not demonstrate differences in the number of mastered topics, both before (median 1, Q1–Q3 = 0–2 vs. median 0, Q1–Q3 = 0–3, respectively, p = 0.878) and after the intervention (median 9, Q1–Q3 = 7.5–9 vs. median 9, Q1–Q3 = 7–9, p = 0.713).
3.3. Patients’ Perspectives on the Acceptability of the CHW-Led Education
Participants provided insights into the acceptability of the education intervention, focusing on various aspects such as content, perception of its usefulness, satisfaction, the CHW, and recommendations for program enhancement (Table 3). Among all participants who completed the post-survey (n = 85), 100% reported satisfaction with the program, with positive feedback on the usefulness and appropriateness of the covered topics, as well as the program’s structure and flow. All respondents expressed satisfaction with the CHW’s professionalism, resourcefulness, knowledge, and level of engagement, and they will recommend the education to others.

Table 3.
Acceptability of the education intervention.
In response to an open-ended question about further education interests regarding CKD, most patients (59%) expressed a desire for additional information on topics such as (a) kidney-friendly diets, (b) self-management strategies, and (c) medications for prevention. Moreover, 20% expressed interest in understanding the interconnection between diabetes, kidney disease, and cardiovascular health. Regarding any issues, they felt were missing or could be improved on the flipchart or patient handout, more than half of the feedback highlighted the need for more detailed information on specific kidney-friendly diets and preserving kidney health. Patients also suggested adding more content to diets that can protect kidneys, such as a low-protein and a low-sodium diet, as well as providing information on preferred foods to have and foods to avoid, how much protein and carbohydrates, and recommendable cooking techniques to preserve kidney function. Additionally, 20% of patients suggested incorporating more visuals or illustrations to enhance understanding, particularly regarding the process of dialysis and kidney transplants.
3.4. Predictive Capacity of Various Variables for a Patient’s Behavioral Intention to Seek Kidney-HealthCare
After receiving the CHW-led intervention, 85% of the surveyed participants expressed that it is likely or extremely likely that they will visit their doctor and undergo kidney function testing, monitoring, and medical management as prescribed. To understand the factors associated with the 15% of patients who did not express intent to seek kidney healthcare, we conducted a Receiver Operating Characteristic (ROC) analysis. The analysis examined various variables, including age, annual income, education level, household size, and the number of topics perceived to be mastered after the intervention. Surprisingly, none of these variables were found to predict the likelihood of patients denying visiting their doctor and undergoing CKD screening/monitoring. Specifically, age (AUC: 0.520, 95% CI 0.353–0.803, p = 0.687), annual income (AUC: 0.569, 95% CI = 0.394–0.744, p = 0.393), education level (AUC: 0.503, 95% CI 0.349–0.657, p = 0.969), household size (AUC: 0.404, 95% CI 0.261–0.547, p = 0.238), and the number of topics perceived to be mastered after the intervention (AUC: 0.551, 95% CI 0.401–0.701, p = 0.529) did not serve as predictors for this behavior intent. This finding underscores the need for further research to identify the specific variables influencing patients’ unwillingness to visit their doctor post-intervention, particularly among those who felt “unlikely” or “extremely unlikely” to do so. Understanding these factors is crucial for developing targeted interventions to address barriers to healthcare access and improve patient outcomes.
In examining the relationship between patients’ negative behavior intent (“unlikely” and “extremely unlikely” to visit their doctor) post-intervention, we focused on their perception of knowledge. Interestingly, among patients who expressed no behavioral intent to undergo CKD screening and monitoring tests (15 out of 15, 100%), all reported knowing “quite a bit” or “a lot” about two specific topics: (1) goals for blood pressure and glycemia, and (2) tests to verify kidney function. In contrast, among patients who expressed a likelihood of visiting their doctor post-intervention, only 72.9% (62 out of 85 patients) reported knowing “a lot” or “quite a bit” about these topics, with a statistically significant difference (p = 0.014). This suggests that the absence of beneficial behavior intent may not stem from a lack of information or understanding but rather from an excessive confidence in one’s knowledge of the subject. The presence of a high-risk disease progression (eGFR between 15–29 mL/min/1.73 m2 and/or proteinuria > 500 mg/g creatinine) did not influence the number of topics mastered, both before (median 1, Q1–Q3 = 0–2 vs. median 0, Q1–Q3 = 0–3, respectively, p = 0.878) and after the intervention (median 9, Q1–Q3 = 7.5–9 vs. median 9, Q1–Q3 = 7–9, respectively, p = 0.713).
Furthermore, the patient’s level of education significantly influenced the number of topics perceived to be mastered by patients. Before the intervention, those with a high school education or more reported mastering a higher number of topics (median 3, Q1–Q3 = 0–7) compared to those with lower education levels (median 0, Q1–Q3 = 0–1) (p = 0.001). However, after the intervention, no significant differences were observed between the two groups (median 9, Q1–Q3 = 8–9 vs. median 9, Q1–Q3 = 7–9, respectively, p = 0.135).
3.5. Biochemical Parameters Analysis
For exploratory purposes, we compared preliminary biochemical and clinical data from patients’ electronic medical records (EMR) within 3 months before and after the intervention for those participants who expressed a positive intent to seek kidney healthcare as a result of the intervention. Of 72 patients who reported a positive intent to seek kidney healthcare, only 51 had documented a medical visit and laboratory results within the period analyzed. Table 4 presents the median values and corresponding quartiles (Q1 and Q3) for various biochemical parameters before and after the intervention, along with the statistical significance of the observed changes. Our analysis suggests a decrease in glycemia levels after the intervention (median change = −18.0, p = 0.014). Additionally, there was a notable decrease in triglyceride levels (median change = −29.0, p = 0.035), indicating that the intervention may have had a positive influence on specific biochemical parameters related to metabolic control and CKD risk factors, particularly glycemia and triglycerides. However, various external factors (unrelated to the intervention), such as concurrent treatments, medication adjustments, or other health-related activities, may have contributed to the observed improvement. Therefore, future studies should aim to account for these potential confounding factors to assess the specific impact of the intervention more accurately on glycemic control and other biochemical parameters. On the other hand, the intervention did not significantly impact other parameters such as HbA1c, cholesterol, eGFR, and uACR. These findings indicate that while the intervention may have contributed to improvements in specific CKD risk factors, its effects on broader kidney health and metabolic outcomes require further analysis and longer-term follow-up to fully elucidate.

Table 4.
Comparison of biochemical parameters three months before and after CKD education intervention for those participants that reported positive behavior intent to seek kidney healthcare **.
4. Discussion
Our findings provide valuable insights into the perspectives of underserved Latine patients regarding the acceptability and impact of a CHW-led education intervention on CKD knowledge and behavioral intent toward kidney healthcare. CHW programs are recognized for their role in improving medication adherence, self-management skills, and access to healthcare services, particularly within underserved populations with chronic conditions [30,44,45]. This study’s findings highlight the positive relationship between CHWs and the communities they serve [47,48,49,50,51], emphasizing their critical role in increasing access to culturally tailored CKD education and kidney care, consistent with prior research [34,43,44,45,46,47,48,49,50,51]. Moreover, the positive impact of CHWs on enhancing CKD knowledge and fostering a positive attitude toward kidney care underscores the promise of leveraging CHWs’ roles and integrating them into future healthcare models and community health strategies.
Regarding the perception of knowledge about CKD topics, a significant improvement was observed post-intervention. Before the intervention, most participants (over 80%) had limited knowledge about kidney functions, CKD risks, and renal function tests. However, after the intervention, this outcome reversed, with over 80% of participants reporting knowing “quite a bit” or “a lot” about these topics. These results underscore the effectiveness of the co-created educational material and its implementation by CHWs in improving CKD knowledge in this vulnerable population. This improvement in knowledge is crucial, as CKD is a disease often overlooked in its early stages due to the lack of obvious symptoms, making education and awareness vital for early detection and management [62,63].
The intervention not only enhanced self-reported CKD knowledge but also fostered a positive intent to seek kidney healthcare. In the post-intervention evaluation, 85% of participants indicated that they were likely or extremely likely to visit their doctor and undergo renal function tests and CKD monitoring, and 60% of participants had CKD tests post-intervention. This positive behavioral intent addresses a critical barrier in CKD management: the lack of awareness, low perceived susceptibility to CKD, and the need for periodic screening and monitoring [3,4,64].
Our analyses also revealed that certain factors, such as age, income level, education level, and household size, did not predict the likelihood of participants visiting the doctor for renal function tests. This suggests that other barriers, possibly related to confidence in acquired knowledge or psychosocial factors, could influence this behavior intent [12,15,17,22,65]. These findings underscore the complexity of the behavioral change process and the challenges in healthcare decision-making within vulnerable communities. Education and awareness alone may not be sufficient to overcome all barriers to medical care [60].
While the intervention appears to positively influence specific biochemical parameters related to metabolic control and CKD risk factors, such as glycemia and triglycerides, it did not significantly impact other indicators of kidney and metabolic health, including HbA1c, cholesterol, eGFR, and uACR. These results should be interpreted with caution. First, the biochemical parameters were measured within a three-month post-intervention window, which may be too short to draw definitive conclusions about the intervention’s impact on clinical outcomes. Second, the absence of a control group limits our ability to account for other factors, such as lifestyle changes, access and adherence to medications, and comorbidities, that may explain the variability in response [11]. These limitations highlight the need for additional studies with long-term follow-up to fully evaluate the intervention’s effects on overall kidney health and risk factors.
Participant feedback emphasized the importance of ongoing education and the need for additional information, particularly on diet and other aspects of kidney disease self-management. Patients suggested that the program could benefit from more detailed dietary recommendations tailored to different stages of kidney disease and practical strategies for preserving kidney health. This feedback is critical for continuously adapting and improving educational interventions, ensuring they remain relevant and beneficial for patients [35,54,64,66].
The high level of acceptance and satisfaction reported by participants suggests that CHWs are valued in CKD education and community support. While this study did not include a control group to make direct comparisons, the positive feedback indicates that CHWs were likely effective in engaging the underserved community on kidney health topics. This is consistent with other research showing that CHW programs can be effective in improving community health outcomes [67,68,69,70]. For example, similar programs have been successful in areas such as reducing emergency department visits [62], increasing cancer screening referrals [63], and managing chronic conditions like diabetes and hypertension [64,65]. Expanding CHW-led initiatives to other vulnerable populations might similarly enhance CKD recognition and management while reducing health disparities [35,44,48,49,50]. CHWs are particularly effective in bridging gaps between healthcare services and patients, addressing cultural and linguistic barriers that could otherwise impede access to care [24,30].
Our findings align with studies showing that CHWs can enhance disease-specific knowledge, positively impact chronic disease management, and improve access to care [35,40,41,42,49,60]. CHWs can also be integrated with other approaches, such as telemedicine, which faces challenges like technology access and acceptance [67]. For example, the combination of CHWs and telemedicine in Canada for diabetes management [68] highlights how CHWs can complement other methods to improve healthcare accessibility [69].
While our intervention did not aim to assess direct changes in CKD-related clinical outcomes as primary outcomes, the exploratory analysis of improved specific biochemical parameters—interpreted with caution—along with high participant satisfaction, increased self-reported CKD knowledge, and positive intent to seek care suggests that CHWs can effectively engage communities with low CKD awareness and serve as agents of change. Additionally, the positive feedback on culturally tailored educational materials co-created by CHWs highlights their effectiveness in addressing CKD knowledge gaps. Replicating such CHW-led programs in other vulnerable communities could further enhance CKD awareness, improve access to effective education, and facilitate CKD screening and monitoring, particularly for individuals with low health literacy and limited English proficiency living in under-resourced areas.
This study has several limitations due to its quasi-experimental design, which lacks a control group and restricts our ability to definitively attribute observed changes solely to the intervention. Although significant changes in biochemical parameters were noted, these results should be interpreted with caution due to potential influences from comorbidities, medication adherence, and lifestyle changes. Future studies should include a control group and additional sham training to better isolate the effects of CHW education and account for other variables that may impact the results [53,54]. Another limitation of this study is the absence of data on whether participants had a primary care doctor or health insurance, factors that could significantly influence their willingness and ability to seek medical care. Additionally, while most participants were recruited from a free clinic, our broader recruitment did not adequately account for varying levels of healthcare access among participants. Another limitation is the lack of information regarding the documentation status of participants, which could have provided critical insights into the role of immigration status in healthcare-seeking behavior. Finally, while immigration fears were indirectly addressed, a more direct assessment of how these fears impact the willingness to engage in medical care would have strengthened our analysis.
However, important challenges remain, such as the lack of early detection and the need to strengthen the doctor–patient relationship. Improving communication and providing clear instructions from primary care are essential not only for patients with chronic kidney disease but also for vulnerable groups more broadly. The findings highlight the effectiveness of using community health workers (CHWs) as a strategy that not only facilitates interventions but also stands out for its ability to build trust and establish long-term relationships with patients. Compared to other strategies, such as chronic disease management programs utilizing telemedicine or technology-based interventions, CHWs offer a particular advantage by focusing on personal relationships, a critical element for the success of community health interventions. Further research is needed to optimize this approach, particularly in populations with significant barriers to healthcare access.
One limitation of this study is the absence of data on whether participants had a primary care doctor or health insurance, factors that could significantly influence their willingness and ability to seek medical care. Additionally, while most participants were recruited from a free clinic, our broader recruitment did not adequately account for varying levels of healthcare access among participants. Another key limitation is the lack of information regarding participants’ documentation status, which could have provided critical insights into the role of immigration status in healthcare-seeking behavior. Although immigration fears were indirectly addressed, a more direct assessment of how these concerns impact the willingness to engage in medical care would have strengthened our analysis. The decision not to collect data on participants’ documentation status was influenced by ethical considerations. While this information is rarely gathered in health research due to concerns about privacy breaches, discomfort, and the potential for a “chilling effect” on participant trust [71,72,73,74], it is important to understand the barriers faced by immigrants. While our educational approach, which involved co-creating CKD materials with CHWs and patients and having a CHW conduct the intervention, indirectly addressed CKD care-related fears and trust issues with the educational content, a more direct assessment of these factors would have strengthened our analysis. Future research should address these gaps to better understand the barriers and facilitators to healthcare for vulnerable Latine populations.
5. Conclusions
Our study underscores the high acceptability of CHW-led interventions and culturally tailored educational materials, highlighting their positive impact on enhancing CKD knowledge and fostering positive behavioral intent toward kidney healthcare among the Latine population with or at risk for CKD. Integrating CHWs into clinical care teams is a promising strategy for delivering culturally appropriate CKD education and improving kidney health outcomes. Additionally, establishing sustainable funding mechanisms is crucial for scaling and maintaining CHW programs in safety-net settings.
Author Contributions
Conceptualization, J.D.-M., I.D.-E., C.D., L.K. and A.J.-P.; data curation, J.D.-M., C.D., A.J.-P., B.L. and J.M.; formal analysis, J.D.-M., I.D.-E., B.L., Y.M., W.K., O.D.-E. and E.W.; funding acquisition, J.D.-M. and M.H.; investigation, J.D.-M., A.J.-P. and G.A.H.-F.; methodology, J.D.-M., I.D.-E., C.D., L.K., A.J.-P., J.M., Y.M., G.A.H.-F., W.K., O.D.-E., E.W. and M.H.; project administration, J.D.-M. and M.H.; resources, J.D.-M.; software, J.D.-M., I.D.-E., L.K., J.M., Y.M., G.A.H.-F., W.K., O.D.-E., E.W. and M.H.; supervision, J.D.-M. and M.H.; validation, J.D.-M., J.M., Y.M., W.K., O.D.-E. and E.W.; visualization, J.D.-M.; writing—original draft preparation, J.D.-M., C.D., L.K. and B.L.; writing—review and editing, J.D.-M. and M.H. All authors added comments to the manuscript and made in-text suggestions for improvement. After consent from all authors above, the final manuscript was submitted by J.D.-M. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the National Kidney Foundation (2022-24 Kidney Health Equity Community Engagement Award). The funders had no role in the study design, in the collection, analysis, or interpretation of data, in the writing of the manuscript, or in the decision to publish the results.
Institutional Review Board Statement
This study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board (or Ethics Committee) of Florida International University (Protocol Approval #: IRB-23-0449, 30 August 2023).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available, as we only asked for informed consent from the participants to share data with other researchers on request.
Acknowledgments
We express our gratitude to all participants and the Caridad Center. The contributions of patients, CHWs, clinicians, and other community stakeholders to the CARE study. Additionally, we thank the Caridad research advisory board for their critical reflections at different steps of the study protocol. Diaz-Martinez, Hospital, and Wagner’s efforts were supported in part by the National Institute on Minority Health and Health Disparities of the National Institutes of Health under Award Number NIMHD (U54MD012393), Florida International University Research Center in Minority Institutions.
Conflicts of Interest
The authors declare no conflict of interest. The authors, Carlos Duran and Wayne Kotzker, are from Florida Kidney Physicians (Boca Raton, FL 33431, USA). However, the experimental data and results of the study have nothing to do with that institution. Laura Kallus, Aydeivis Jean-Pierre, Brenda Lopez, Jessica Mancilla, and Yoel Madruga are from Caridad Center (Boynton Beach, FL 33472, USA), which is a nonprofit organization, and were not involved in the decision to publish the study results.
References
- Centers for Disease Control and Prevention Centers for Disease Control and Prevention. In Chronic Kidney Disease Surveillance System—United States. Available online: https://www.cdc.gov/kidney-disease/php/data-research/index.html (accessed on 10 June 2023).
- Murphy, D.; McCulloch, C.E.; Lin, F.; Banerjee, T.; Bragg-Gresham, J.L.; Eberhardt, M.S.; Morgenstern, H.; Pavkov, M.E.; Saran, R.; Powe, N.R.; et al. Trends in Prevalence of Chronic Kidney Disease in the United States. Ann. Intern. Med. 2016, 165, 473. [Google Scholar] [CrossRef]
- Chu, C.D.; McCulloch, C.E.; Banerjee, T.; Pavkov, M.E.; Burrows, N.R.; Gillespie, B.W.; Saran, R.; Shlipak, M.G.; Powe, N.R.; Tuot, D.S.; et al. CKD Awareness among US Adults by Future Risk of Kidney Failure. Am. J. Kidney Dis. 2020, 76, 174–183. [Google Scholar] [CrossRef] [PubMed]
- Shlipak, M.G.; Tummalapalli, S.L.; Boulware, L.E.; Grams, M.E.; Ix, J.H.; Jha, V.; Kengne, A.-P.; Madero, M.; Mihaylova, B.; Tangri, N.; et al. The Case for Early Identification and Intervention of Chronic Kidney Disease: Conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Kidney Int. 2021, 99, 34–47. [Google Scholar] [CrossRef] [PubMed]
- National Kidney Foundation Inc. Facts about Chronic Kidney Disease. Available online: https://www.kidney.org/atoz/content/about-chronic-kidney-disease (accessed on 23 May 2024).
- Vassalotti, J.; Diamantidis, C.J.; Cook, D.J. Shared Viewpoint—Developing the Future of Kidney Care. J. Gen. Intern. Med. 2022, 37, 947–948. [Google Scholar] [CrossRef] [PubMed]
- Yan, G.; Shen, J.I.; Harford, R.; Yu, W.; Nee, R.; Clark, M.J.; Flaque, J.; Colon, J.; Torre, F.; Rodriguez, Y.; et al. Racial and Ethnic Variations in Mortality Rates for Patients Undergoing Maintenance Dialysis Treated in US Territories Compared with the US 50 States. Clin. J. Am. Soc. Nephrol. 2020, 15, 101–108. [Google Scholar] [CrossRef] [PubMed]
- Bikbov, B.; Purcell, C.A.; Levey, A.S.; Smith, M.; Abdoli, A.; Abebe, M.; Adebayo, O.M.; Afarideh, M.; Agarwal, S.K.; Agudelo-Botero, M.; et al. Global, Regional, and National Burden of Chronic Kidney Disease, 1990–2017: A Systematic Analysis for the Global Burden of Disease Study 2017. Lancet 2020, 395, 709–733. [Google Scholar] [CrossRef]
- Fischer, M.J.; Go, A.S.; Lora, C.M.; Ackerson, L.; Cohan, J.; Kusek, J.W.; Mercado, A.; Ojo, A.; Ricardo, A.C.; Rosen, L.K.; et al. CKD in Hispanics: Baseline Characteristics From the CRIC (Chronic Renal Insufficiency Cohort) and Hispanic-CRIC Studies. Am. J. Kidney Dis. 2011, 58, 214–227. [Google Scholar] [CrossRef]
- United States Renal Data System. 2022 USRDS Annual Data Report: Epidemiology of Kidney Disease in the United States; National Institute of Diabetes and Digestive and Kidney Diseases: Bethesda, MD, USA, 2022. [Google Scholar]
- Desai, N.; Lora, C.M.; Lash, J.P.; Ricardo, A.C. CKD and ESRD in US Hispanics. Am. J. Kidney Dis. 2019, 73, 102–111. [Google Scholar] [CrossRef]
- Norton, J.M.; Moxey-Mims, M.M.; Eggers, P.W.; Narva, A.S.; Star, R.A.; Kimmel, P.L.; Rodgers, G.P. Social Determinants of Racial Disparities in CKD. J. Am. Soc. Nephrol. 2016, 27, 2576–2595. [Google Scholar] [CrossRef]
- Nicholas, S.B.; Kalantar-Zadeh, K.; Norris, K.C. Socioeconomic Disparities in Chronic Kidney Disease. Adv. Chronic Kidney Dis. 2015, 22, 6–15. [Google Scholar] [CrossRef]
- Ortega, A.N.; McKenna, R.M.; Kemmick Pintor, J.; Langellier, B.A.; Roby, D.H.; Pourat, N.; Vargas Bustamante, A.; Wallace, S.P. Health Care Access and Physical and Behavioral Health Among Undocumented Latinos in California. Med. Care 2018, 56, 919–926. [Google Scholar] [CrossRef] [PubMed]
- Ornelas, I.J.; Yamanis, T.J.; Ruiz, R.A. The Health of Undocumented Latinx Immigrants: What We Know and Future Directions. Annu. Rev. Public Health 2020, 41, 289–308. [Google Scholar] [CrossRef]
- Mitchell, T. Unauthorized Immigrant Population Trends for States, Birth Countries and Regions. Available online: https://www.pewresearch.org/race-and-ethnicity/feature/unauthorized-trends/ (accessed on 10 June 2024).
- Estrella, M.L.; Allen-Meares, P.; Ricardo, A.C.; Fischer, M.J.; Gordon, E.J.; Carmona-Powell, E.; Sondheimer, J.; Chen, J.; Horwitz, E.; Wang, X.; et al. Prospective Associations of Health Literacy with Clinical Outcomes in Adults with CKD: Findings from the CRIC Study. Nephrol. Dial. Transplant. 2023, 38, 904–912. [Google Scholar] [CrossRef] [PubMed]
- Lora, C.M.; Gordon, E.J.; Sharp, L.K.; Fischer, M.J.; Gerber, B.S.; Lash, J.P. Progression of CKD in Hispanics: Potential Roles of Health Literacy, Acculturation, and Social Support. Am. J. Kidney Dis. 2011, 58, 282–290. [Google Scholar] [CrossRef] [PubMed]
- Lora, C.M.; Ricardo, A.C.; Chen, J.; Cai, J.; Flessner, M.; Moncrieft, A.; Peralta, C.; Raij, L.; Rosas, S.E.; Talavera, G.A.; et al. Acculturation and Chronic Kidney Disease in the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Prev. Med. Rep. 2018, 10, 285–291. [Google Scholar] [CrossRef]
- Crews, D.C.; Kuczmarski, M.F.; Grubbs, V.; Hedgeman, E.; Shahinian, V.B.; Evans, M.K.; Zonderman, A.B.; Burrows, N.R.; Williams, D.E.; Saran, R.; et al. Effect of Food Insecurity on Chronic Kidney Disease in Lower-Income Americans. Am. J. Nephrol. 2014, 39, 27–35. [Google Scholar] [CrossRef]
- Billany, R.E.; Thopte, A.; Adenwalla, S.F.; March, D.S.; Burton, J.O.; Graham-Brown, M.P.M. Associations of Health Literacy with Self-Management Behaviours and Health Outcomes in Chronic Kidney Disease: A Systematic Review. J. Nephrol. 2023, 36, 1267–1281. [Google Scholar] [CrossRef]
- Boulware, L.E.; Carson, K.A.; Troll, M.U.; Powe, N.R.; Cooper, L.A. Perceived Susceptibility to Chronic Kidney Disease among High-Risk Patients Seen in Primary Care Practices. J. Gen. Intern. Med. 2009, 24, 1123–1129. [Google Scholar] [CrossRef]
- Cervantes, L.; Rizzolo, K.; Carr, A.L.; Steiner, J.F.; Chonchol, M.; Powe, N.; Cukor, D.; Hasnain-Wynia, R. Social and Cultural Challenges in Caring for Latinx Individuals With Kidney Failure in Urban Settings. JAMA Netw. Open 2021, 4, e2125838. [Google Scholar] [CrossRef]
- Narva, A.S.; Norton, J.M.; Boulware, L.E. Educating Patients about CKD. Clin. J. Am. Soc. Nephrol. 2016, 11, 694–703. [Google Scholar] [CrossRef]
- Stevens, P.E. Evaluation and Management of Chronic Kidney Disease: Synopsis of the Kidney Disease: Improving Global Outcomes 2012 Clinical Practice Guideline. Ann. Intern Med. 2013, 158, 825. [Google Scholar] [CrossRef] [PubMed]
- Ikizler, T.A.; Burrowes, J.D.; Byham-Gray, L.D.; Campbell, K.L.; Carrero, J.-J.; Chan, W.; Fouque, D.; Friedman, A.N.; Ghaddar, S.; Goldstein-Fuchs, D.J.; et al. KDOQI Clinical Practice Guideline for Nutrition in CKD: 2020 Update. Am. J. Kidney Dis. 2020, 76, S1–S107. [Google Scholar] [CrossRef]
- Kwong, Y.D.; Tuot, D.S. Optimizing Self-Management Programs in Kidney Disease: Implementation of Sick-Day Protocols. Kidney Med. 2022, 4, 100530. [Google Scholar] [CrossRef]
- Kidney Disease Outcomes Quality Initiative. KDOQI Clinical Practice Guidelines and Clinical Practice Recommendations for Diabetes and Chronic Kidney Disease. Am. J. Kidney Dis. 2007, 49, S12–S154. [Google Scholar] [CrossRef] [PubMed]
- Langham, R.G.; Kalantar-Zadeh, K.; Bonner, A.; Balducci, A.; Hsiao, L.L.; Kumaraswami, L.A.; Laffin, P.; Liakopoulos, V.; Saadi, G.; Tantisattamo, E.; et al. Kidney Health for All: Bridging the Gap in Kidney Health Education and Literacy. Clin. Kidney J. 2022, 55, 603–610. [Google Scholar] [CrossRef]
- Cervantes, L.; Robinson, B.M.; Steiner, J.F.; Myaskovsky, L. Culturally Concordant Community-Health Workers: Building Sustainable Community-Based Interventions That Eliminate Kidney Health Disparities. J. Am. Soc. Nephrol. 2022, 33, 1252–1254. [Google Scholar] [CrossRef] [PubMed]
- Kimmel, P.L.; Jefferson, N.; Norton, J.M.; Star, R.A. How Community Engagement Is Enhancing NIDDK Research. Clin. J. Am. Soc. Nephrol. 2019, 14, 768–770. [Google Scholar] [CrossRef]
- Payán, D.; Zawadzki, M.; Song, A. Advancing Community-Engaged Research to Promote Health Equity: Considerations to Improve the Field. Perspect. Public Health 2022, 142, 139–141. [Google Scholar] [CrossRef]
- O’Mara-Eves, A.; Brunton, G.; McDaid, D.; Oliver, S.; Kavanagh, J.; Jamal, F.; Matosevic, T.; Harden, A.; Thomas, J. Community Engagement to Reduce Inequalities in Health: A Systematic Review, Meta-Analysis and Economic Analysis. Public Health Res. 2013, 1, 1–526. [Google Scholar] [CrossRef]
- National Kidney Foundation Community Health Workers. Available online: https://www.kidney.org/NKF-Community-Health-Workers (accessed on 10 June 2024).
- Brownstein, J.N.; Chowdhury, F.M.; Norris, S.L.; Horsley, T.; Jack, L.; Zhang, X.; Satterfield, D. Effectiveness of Community Health Workers in the Care of People with Hypertension. Am. J. Prev. Med. 2007, 32, 435–447. [Google Scholar] [CrossRef]
- Spencer, M.S.; Kieffer, E.C.; Sinco, B.; Piatt, G.; Palmisano, G.; Hawkins, J.; Lebron, A.; Espitia, N.; Tang, T.; Funnell, M.; et al. Outcomes at 18 Months From a Community Health Worker and Peer Leader Diabetes Self-Management Program for Latino Adults. Diabetes Care 2018, 41, 1414–1422. [Google Scholar] [CrossRef] [PubMed]
- Reininger, B.M.; Lopez, J.; Zolezzi, M.; Lee, M.; Mitchell-Bennett, L.A.; Xu, T.; Park, S.K.; Saldana, M.V.; Perez, L.; Payne, L.Y.; et al. Participant Engagement in a Community Health Worker-Delivered Intervention and Type 2 Diabetes Clinical Outcomes: A Quasiexperimental Study in MexicanAmericans. BMJ Open 2022, 12, e063521. [Google Scholar] [CrossRef] [PubMed]
- Fisher, T.L.; Burnet, D.L.; Huang, E.S.; Chin, M.H.; Cagney, K.A. Cultural Leverage. Med. Care Res. Rev. 2007, 64, 243S–282S. [Google Scholar] [CrossRef]
- Chang, A.; Patberg, E.; Cueto, V.; Li, H.; Singh, B.; Kenya, S.; Alonzo, Y.; Carrasquillo, O. Community Health Workers, Access to Care, and Service Utilization Among Florida Latinos: A Randomized Controlled Trial. Am. J. Public Health 2018, 108, 1249–1251. [Google Scholar] [CrossRef]
- Cass, A.; Cunningham, J.; Wang, Z.; Hoy, W. Regional Variation in the Incidence of End-stage Renal Disease in Indigenous Australians. Med. J. Aust. 2001, 175, 24–27. [Google Scholar] [CrossRef] [PubMed]
- Kumar, V.; Yadav, A.K.; Sethi, J.; Ghosh, A.; Sahay, M.; Prasad, N.; Varughese, S.; Parameswaran, S.; Gopalakrishnan, N.; Kaur, P.; et al. The Indian Chronic Kidney Disease (ICKD) Study: Baseline Characteristics. Clin. Kidney J. 2022, 15, 60–69. [Google Scholar] [CrossRef] [PubMed]
- Jha, V.; Garcia-Garcia, G.; Iseki, K.; Li, Z.; Naicker, S.; Plattner, B.; Saran, R.; Wang, A.Y.-M.; Yang, C.-W. Chronic Kidney Disease: Global Dimension and Perspectives. Lancet 2013, 382, 260–272. [Google Scholar] [CrossRef]
- Diaz-Martinez, J.; Kallus, L.; Levine, H.M.; Lavernia, F.; Pierre, A.J.; Mancilla, J.; Barthe, A.; Duran, C.; Kotzker, W.; Wagner, E.; et al. Community-Engaged Research (CEnR) to Address Gaps in Chronic Kidney Disease Education among Underserved Latines—The CARE Study. Int. J. Environ. Res. Public Health 2023, 20, 7026. [Google Scholar] [CrossRef]
- Cervantes, L.; Hasnain-Wynia, R.; Steiner, J.F.; Chonchol, M.; Fischer, S. Patient Navigation: Addressing Social Challenges in Dialysis Patients. Am. J. Kidney Dis. 2020, 76, 121–129. [Google Scholar] [CrossRef]
- Aponte, J.; Jackson, T.D.; Wyka, K.; Ikechi, C. Health Effectiveness of Community Health Workers as a Diabetes Self-Management Intervention. Diabetes Vasc. Dis. Res. 2017, 14, 316–326. [Google Scholar] [CrossRef]
- Haboush-Deloye, A.; Marquez, E.; Dunne, R.; Pharr, J.R. The Importance of Community Voice: Using Community-Based Participatory Research to Understand the Experiences of African American, Native American, and Latinx People during a Pandemic. Prev. Chronic Dis. 2023, 20, 220152. [Google Scholar] [CrossRef] [PubMed]
- Nelson, R.G.; Pankratz, V.S.; Ghahate, D.M.; Bobelu, J.; Faber, T.; Shah, V.O. Home-Based Kidney Care, Patient Activation, and Risk Factors for CKD Progression in Zuni Indians. Clin. J. Am. Soc. Nephrol. 2018, 13, 1801–1809. [Google Scholar] [CrossRef] [PubMed]
- Walton, J.W.; Snead, C.A.; Collinsworth, A.W.; Schmidt, K.L. Reducing Diabetes Disparities Through the Implementation of a Community Health Worker–Led Diabetes Self-Management Education Program. Fam. Community Health 2012, 35, 161–171. [Google Scholar] [CrossRef] [PubMed]
- Chang, W.; Oo, M.; Rojas, A.; Damian, A.J. Patients’ Perspectives on the Feasibility, Acceptability, and Impact of a Community Health Worker Program: A Qualitative Study. Health Equity 2021, 5, 160–168. [Google Scholar] [CrossRef]
- Sherman, M.; Covert, H.; Fox, L.; Lichtveld, M. Successes and Lessons Learned From Implementing Community Health Worker Programs in Community-Based and Clinical Settings: Insights From the Gulf Coast. J. Public Health Manag. Pract. 2017, 23, 85–93. [Google Scholar] [CrossRef]
- Lopez, P.M.; Islam, N.; Feinberg, A.; Myers, C.; Seidl, L.; Drackett, E.; Riley, L.; Mata, A.; Pinzon, J.; Benjamin, E.; et al. A Place-Based Community Health Worker Program: Feasibility and Early Outcomes, New York City, 2015. Am. J. Prev. Med. 2017, 52, S284–S289. [Google Scholar] [CrossRef]
- Emery, R.L.; Wimmer, M. Motivational Interviewing. In StatPearls; StatPearls Publishing LLC: Rockville, MD, USA, 2019; Volume 35, p. 21. [Google Scholar]
- Department of Health and Human Services (HHS). Federal Poverty Level (FPL); Department of Health and Human Services (HHS): Washington, DC, USA, 2024. [Google Scholar]
- Sekhon, M.; Cartwright, M.; Francis, J.J. Acceptability of Healthcare Interventions: An Overview of Reviews and Development of a Theoretical Framework. BMC Health Serv. Res. 2017, 17, 88. [Google Scholar] [CrossRef]
- Ajzen, I. The Theory of Planned Behavior. Organ. Behav. Hum. Decis. Process. 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Sanci, L.A.; Coffey, C.M.; Veit, F.C.; Carr-Gregg, M.; Patton, G.C.; Day, N.; Bowes, G. Evaluation of the Effectiveness of an Educational Intervention for General Practitioners in Adolescent Health Care: Randomised Controlled Trial. BMJ 2000, 320, 224–230. [Google Scholar] [CrossRef]
- Johnson, A.M.; Brimhall, A.S.; Johnson, E.T.; Hodgson, J.; Didericksen, K.; Pye, J.; Harmon, G.J.C.; Sewell, K.B. A Systematic Review of the Effectiveness of Patient Education through Patient Portals. JAMIA Open 2023, 6, ooac085. [Google Scholar] [CrossRef]
- Rosenthal, G.E.; Shannon, S.E. The Use of Patient Perceptions in the Evaluation of Health-Care Delivery Systems. Med. Care 1997, 35, NS58–NS68. [Google Scholar] [CrossRef]
- Edmonston, D.; Lydon, E.; Mulder, H.; Chiswell, K.; Lampron, Z.; Marsolo, K.; Goss, A.; Ayoub, I.; Shah, R.C.; Chang, A.R.; et al. Concordance With Screening and Treatment Guidelines for Chronic Kidney Disease in Type 2 Diabetes. JAMA Netw. Open 2024, 7, e2418808. [Google Scholar] [CrossRef]
- Schrauben, S.J.; Cavanaugh, K.L.; Fagerlin, A.; Ikizler, T.A.; Ricardo, A.C.; Eneanya, N.D.; Nunes, J.W. The Relationship of Disease-Specific Knowledge and Health Literacy With the Uptake of Self-Care Behaviors in CKD. Kidney Int. Rep. 2020, 5, 48–57. [Google Scholar] [CrossRef]
- Dudley, W.N.; Benuzillo, J.G.; Carrico, M.S. SPSS and SAS Programming for the Testing of Mediation Models. Nurs. Res. 2004, 53, 59–62. [Google Scholar] [CrossRef] [PubMed]
- Rust, G.; Baltrus, P.; Ye, J.; Daniels, E.; Quarshie, A.; Boumbulian, P.; Strothers, H. Presence of a Community Health Center and Uninsured Emergency Department Visit Rates in Rural Counties. J. Rural. Health 2009, 25, 8–16. [Google Scholar] [CrossRef]
- United States Renal Data System. 2020 USRDS Annual Data Report; National Institute of Diabetes and Digestive and Kidney Diseases: Bethesda, MD, USA, 2020. [Google Scholar]
- Szczech, L.A.; Stewart, R.C.; Su, H.-L.; DeLoskey, R.J.; Astor, B.C.; Fox, C.H.; McCullough, P.A.; Vassalotti, J.A. Primary Care Detection of Chronic Kidney Disease in Adults with Type-2 Diabetes: The ADD-CKD Study (Awareness, Detection and Drug Therapy in Type 2 Diabetes and Chronic Kidney Disease). PLoS ONE 2014, 9, e110535. [Google Scholar] [CrossRef] [PubMed]
- Afkarian, M.; Zelnick, L.R.; Hall, Y.N.; Heagerty, P.J.; Tuttle, K.; Weiss, N.S.; de Boer, I.H. Clinical Manifestations of Kidney Disease Among US Adults with Diabetes, 1988–2014. JAMA 2016, 316, 602–610. [Google Scholar] [CrossRef]
- Zheng, Y.; Ley, S.H.; Hu, F.B. Global Aetiology and Epidemiology of Type 2 Diabetes Mellitus and Its Complications. Nat. Rev. Endocrinol. 2018, 14, 88–98. [Google Scholar] [CrossRef]
- Blewett, L.A.; Owen, R.A. Accountable Care for the Poor and Underserved: Minnesota’s Hennepin Health Model. Am. J. Public Health 2015, 105, 622–624. [Google Scholar] [CrossRef]
- Brown, L.D.; Vasquez, D.; Salinas, J.J.; Tang, X.; Balcázar, H. Evaluation of Healthy Fit: A Community Health Worker Model to Address Hispanic Health Disparities. Prev. Chronic Dis. 2018, 15, 170347. [Google Scholar] [CrossRef]
- Turner, B.J.; Liang, Y.; Ramachandran, A.; Poursani, R. Telephone or Visit-Based Community Health Worker Care Management for Uncontrolled Diabetes Mellitus: A Longitudinal Study. J. Community Health 2020, 45, 1123–1131. [Google Scholar] [CrossRef]
- Krantz, M.J.; Coronel, S.M.; Whitley, E.M.; Dale, R.; Yost, J.; Estacio, R.O. Effectiveness of a Community Health Worker Cardiovascular Risk Reduction Program in Public Health and Health Care Settings. Am. J. Public Health 2013, 103, e19–e27. [Google Scholar] [CrossRef]
- Lahman, M.; Mendoza, B.; Rodriguez, K.; Schwartz, J. Undocumented Research Participants: Ethics and Protection in a Time of Fear. Hisp. J. Behav. Sci. 2011, 33, 304–322. [Google Scholar] [CrossRef]
- Hernández, M.G.; Nguyen, J.; Casanova, S.; Suárez-Orozco, C.; Saetermoe, C.L. Doing No Harm and Getting It Right: Guidelines for Ethical Research with Immigrant Communities. New Dir. Child Adolesc. Dev. 2013, 2013, 43–60. [Google Scholar] [CrossRef]
- Bachmeier, J.D.; Van Hook, J.; Bean, F.D. Can We Measure Immigrants’ Legal Status? Lessons from Two U.S. Surveys. Int. Migr. Rev. 2014, 48, 538–566. [Google Scholar] [CrossRef]
- Lekas, H.-M.; Pahl, K.; Fuller Lewis, C. Rethinking Cultural Competence: Shifting to Cultural Humility. Health Serv. Insights 2020, 13, 1178632920970580. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).