Abstract
During the gestation period, pregnant women experience physical and psychological changes, which represent vulnerability factors that can boost the development of mental health conditions. The COVID-19 pandemic is producing new changes in the routines of the whole society, especially on lifestyle habits. The psychological impact associated with the COVID-19 pandemic and pregnant women remains unclear. A scoping review regarding the psychological impact of the COVID-19 pandemic on pregnant women was conducted. Searchers were conducted using the PubMed, Web of Science and CINAHL databases. Articles in Spanish, English and French were included. The search was conducted between November 2020 and September 2021. We identified 31 studies that evaluated 30,049 expectant mothers during the COVID-19 pandemic. Pregnant women showed high levels of anxiety and depression symptomatology. Fear of contagion and concerns regarding the health of the fetus were identified as the main variables related to psychological distress. An increase of the levels of depression, anxiety and stress during the COVID-19 pandemic amongst pregnant women has been observed. Moreover, an increased vulnerability of the fetus due to placental metabolic alterations is discussed. This review suggests that the COVID-19 pandemic is associated with a negative psychological impact on pregnant women. Thus, high levels of anxiety and depression symptoms suggest the need for a systematic approach.
1. Introduction
The first human cases of COVID-19 appeared back in 2019 [1]. As a result, the World Health Organization (WHO) declared a pandemic state in March 2020 [2,3,4]. Governments imposed a series of measures to reduce the risk of contagion, the spread of the SARS-CoV-2 virus and the increasing number of deaths. These measures included social distancing, quarantine and strict hygienic measures [5].
Countries around the world had to adapt to the rapid changes emerging in order to protect public health. Fear of contagion, the potential death of a relative and the possibility of being unemployed during this unprecedented times have affected mental health wellbeing [6].
In particular, psychological impairment was found to be more prevalent among vulnerable groups, including pregnant women [7]. During pregnancy, women may experience a series of physical and psychological changes, which directly affect their mental health [8]. Being multiparous, having a low level of education, being a teenager or having an unwanted pregnancy are among the factors that may affect pregnant women’s psychological state. Thus, a high risk pregnancy and having been diagnosed with a psychopathological disease before pregnancy are risk factors associated with a mental-health disorder during pregnancy [8,9]. In this respect, psychopathological symptoms such as anxiety and depression are the most frequently diagnosed. Moreover, adjustment disorders, substance abuse, eating and mood disorders can also appear during this period [10,11]. This symptomatology may affect both the fetus and the mother’s health: it boosts the risk of prematurity and low-birth weight, and increases the risk medical diseases during pregnancy such as gestational diabetes or pre-eclampsia [10,12,13,14]. Moreover, high levels of anxiety and depression during pregnancy have been associated with an excessive alcohol consumption [11,13].
Apart from the vulnerability factors associated with the expected changes of pregnancy [15], women may also experience increased psychological symptoms associated with the pandemic [16]. Uncertainty about the new virus, anxiety and fear have significantly affected the wellbeing of pregnant woman [17,18,19]. The main causes of anxiety, depression and stress were associated with fear of being infected while in public places, using public transport, during delivery at hospital, along with fear of vertical transmission of SARS-CoV-2 [20,21]. These variables have led women to avoid contacting hospitals/health units, withdrawing scheduled prenatal appointments, which ultimately led to reduced medical control during pregnancy [7,17]. Furthermore, fake information communicated through social media has increased pessimistic thoughts in pregnant women [7,22,23].
Additionally, certain social factors such as economic income and education level have also influenced coping strategies during the COVID-19 pandemic [24,25].
The aim of this study was to assess the psychological impact of the COVID-19 pandemic on pregnant women and to estimate the prevalence of mental symptoms in this population.
2. Materials and Methods
In order to perform an initial mapping of the literature, the methodology referring to a scoping review was used [26]. The characteristics of a scoping review are that it is systematic and rigorous. It allows the possibility of generating hypotheses, as well as proposing which areas of study are partially developed. This scoping review adheres to the PRISMA extension for scoping reviews [27]. The research question guiding this scoping review was to analyze the presence of mental symptoms in pregnant women associated with the COVID-19 pandemic.
2.1. Literature Search and Selection of Studies
Searches were conducted between November 2020 and September 2021 on PubMed, Web of Science and CINAHL databases. The search strategy included keywords related to psychological symptoms, pregnancy, postpartum, depression, trauma and coronavirus. MESH terms (e.g., “Pregnancy” [Mesh] AND “Coronavirus” [Mesh] AND (“Depression” [Mesh] OR “Depressive Disorder” [Mesh] OR “Anxiety” [Mesh] OR “Stress Disorders” OR “Traumatic” OR “Acute” [Mesh]) OR “Disorder” [Mesh]) and text word search terms (“pregnancy” AND “coronavirus” AND (“mental health” OR “depression” OR “anxiety” OR “stress”) were used.
2.2. Inclusion and Exclusion Criteria
The inclusion and exclusion criteria is showed in Table 1.

Table 1.
Inclusion and Exclusion Criteria.
2.3. Data Collection and Analysis
Eligible studies were selected through a multistep approach (elimination of duplicates, title reading, abstract, and full-text assessment). Two researchers (B.R-G.B. and C.C-G) independently examined titles and abstracts, evaluating afterwards full texts according to the inclusion criteria described above. Any disagreement between the reviewers was solved by means of a consensus session with a third reviewer (R.A.C-G). In case of ambiguity in reporting or lack of data, primary authors were contacted for clarification.
Searches yielded 87 unique articles. Forty-three were potentially eligible for inclusion based on title and abstract. After full-text review, thirty-one articles met the inclusion criteria. The PRISMA flow chart summarizes the study selection process (Figure 1).
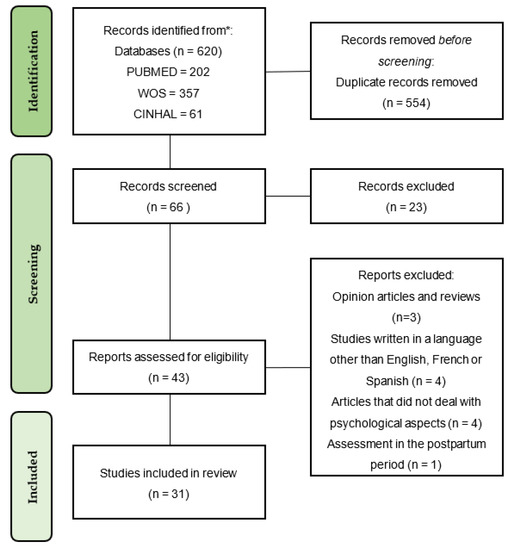
Figure 1.
PRISMA 2020 Flow Diagram.
2.4. Data Extraction and Management
Data were independently extracted by two researchers (B.R-G.B. and C.C-G), and the following information was considered for each article: (1) first author and year of publication; (2) study design; (3) the assessment instrument used in every study; (4) number of participants; (5) the average age of the study population; (6) the gestational age of pregnant women; (7) the percentage that was married when the study was conducted; (8) main results obtained and (9) the most important findings of each study.
2.5. Quality Assessment Tool
The methodological quality of each study was assessed using the score in the Newcastle-Ottawa Quality Assessment Scale (NOQAS) [28] and the adapted version for cross-sectional studies. The criteria included 3 categories with a maximum score of 9 and 10 points for cohort and cross-sectional studies respectively. The first is the “selection”category, which accounts for a maximum of 4 points (5 points for cross-sectional studies), the second is the “comparability”category, which accounts for a maximum of 2 points, and the third is “outcome,” which accounts for a maximum of 3 points. Information regarding the quality of each study was included in Table 2.

Table 2.
Characteristics of included studies.
3. Results
3.1. Study Characteristics
A total of 31 articles written in English were included in this review (Table 2). The countries where they were published were China (n = 5), Turkey (n = 4), United States (n = 2), Canada (n = 4), Iran (n = 1), Ethiopia (n = 1), Singapore (n = 1), Israel (n = 2), Spain (n = 3), Italy (n = 3), Japan (n = 1) Argentina (n = 1) and Qatar (n = 1). Twenty-six studies were cross sectional and three cohort study. A total of 30,049 women participated in the studies (n = 26,846 were pregnant women; n = 290 couples and n = 3,203 non-pregnant women who were controls). The mean age of the participants was 31.03 years old (SD = 4.93). The mean gestational age was 23.85 weeks of gestation (SD = 10.58). In addition, the psychological assessment of the participants was carried out through self-report measures during the COVID-19 pandemic.
3.2. Symptoms of Depression
Most of the selected studies reported depressive symptomatology among pregnant women related to the consequences of the COVID-19 pandemic [29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45]. The psychological tools included in these studies were: the Depression, Anxiety and Stress Scale-21 (DASS-21), the Edinburg Perinatal Depression Scale (EPDS), the Hospital Anxiety, Depression, Stress scale (HADS), The patient Health questionnaire (PHQ-9), Positive and Negative Affect Schedule (PANAS), Beck anxiety inventory (BAI), Inventory of Depression and Anxiety Symptoms II (IDAS-II), Mental Health Inventory (MHI-5), Depression, Anxiety and Stress Scale-21 (DASS-21), Edinburg depression scale (EDS), State-Trait Anxiety Inventory (STAI-State), Cambridge Worry Scale (CWS), Centre for Epidemiologic Studies Depression Scale (CES-D), Multidimensional Scale of Perceived Social Support (MSPSS), Impact of Event Scale-Revised (IES-R), Prenatal Distress Questionnaire (PDQ), Perceived Stress Scale (PSS), Connor-Davidson Resilience Scale (CD-RISC), Athens Insomnia Scale (AIS). Most of them were self-report questionnaires. The prevalence of depressive symptomatology was highly heterogeneous. Some studies reported a prevalence below 20% [40] while others reported a prevalence above 50% [46]. Maintaining a high partner satisfaction, having a high level of education, a high social support, staying physically active and a high income level appeared as variables that could decrease the levels of depression [29,38]. The use of informative tools provided by the hospital could also help to reduce the risk of depression [30,33,46]. When comparing the prevalence of depressive symptoms in pregnant and non-pregnant women, a variety of findings were reported. Thus, the prevalence was higher in non-pregnant women in two studies developed in Israel and China respectively [37,41]. Depressive symptoms were higher among pregnant women in a study in Argentina [45].
3.3. Symptoms of Anxiety
A total of 21 reports estimated the prevalence of anxiety in pregnant women during this pandemic [29,30,31,32,33,35,36,37,38,39,40,41,42,43,44,47,48,49,50,51,52,53,54,55,56]. Depression, Anxiety and Stress Scale-21 (DASS-21), the Edinburg Perinatal Depression Scale (EPDS), the Hospital Anxiety, Depression, Stress Scale (HADS), The Patient Health Questionnaire (PHQ-9), the General Anxiety Disorder-7 (GAD-7), the item 3 of the Oslo Social Support Scale (OSSS-3), the Self-Rating Anxiety Scale (SAS), the Trait Subscale of the Spielberg State-Trait anxiety Inventory (STAI-T), Beck Anxiety Inventory (BAI), the Inventory of Depression and Anxiety Symptoms II (IDAS-II), the Kessler Psychological Distress Scale (K10), the Mental Health Inventory—Short Form (MHI-5), the Patient-Reported Outcomes Measurement Information System (PROMIS), a modified version of the Pregnancy-related Anxiety Scale (PrAS), the Perceived Stress Scale (PSS), the Post-traumatic Stress Disorder Checklist 5 (PCL-5) and the Pandemic-related Pregnancy Stress Scale (PREPS) questionnaires were used to assess symptoms of anxiety, the majority self-report.
The scores obtained showed an increased mean score of anxiety in pregnant women as a result of the pandemic, (values; pre-COVID-19: 39.34 (SD = 6.39), COVID-19: 44.57 (SD = 9.55)) [54], (values; pre-COVID-19: -0.39 (SD = 0.04), COVID-19: 0,15 (SD = 0.03)) [51], values; pre-COVID-19: 184.78 (SD = 49.67), COVID-19: 202.57 (SD = 52.90) [47](values; pre-COVID-19: 20.6, COVID-19: 23.9) [39]. Most of these studies showed that more than one quarter of pregnant women were experiencing anxiety (17.2%; 18.1%; 32.2%; 32.7%; 35.8%) [29,30,40,52,57,58,59,60] and Sut et al., (2020) and Lebel et al., (2020) showed that more than half of the pregnant women presented this pathology (57%; 64.5% respectively) [38,46]. In contrast, one study comparing pregnant with non-pregnant women showed that the presence of anxiety symptoms was reduced during pregnancy (6.8% pregnant, 17.5% non-pregnant) [41]. The results from a prospective study reported that a great majority had believed that pregnant women have a higher risk for COVID-19 infection than general population. This cohort showed mean HADS-A score of 7.94 (SD = 4.03). Anxiety was associated with a high HADS-D score and concern about the inability to reach obstetrician, and being in advanced age [42]. A study carried out in 450 pregnant women and 274 after delivery reported a prevalence of anxiety symptoms above 50% [55]. Results from a study that evaluated anxiety from pre- to during-pandemic showed that 72% of women reported an indicative of moderate to high anxiety [40]. Another study reported a lower prevalence of clinically relevant anxiety levels in pregnant women in Italy (32.6%), but still significant [53]. Finally, a study from Spain showed higher levels of phobic anxiety in pregnant women than previous of the pandemic [35].
The main causes of anxiety reported in pregnant women during the pandemic were using a public transport (87.5%), COVID-19 infection of a family member (71.1%), being in public places (70%), concern for pregnancy complications and fetus health (70%), attending gynecological appointments (68.7%), becoming infected by COVID-19 (59.2%) and birth time (55.4%) [50]. The results reported from a cohort showed that most patients (82.5%) had concerns about infecting their babies during delivery [42].
3.4. Stress Levels
The assessment of stress in pregnant women was reported in nine studies (Berthelot [29,30,35,40,41,51,53,61]. The studies used Anxiety and Stress Scale-21 (DASS-21) [29,35,37,40,53], Perceived stress scale (PSS) [30], Post- traumatic stress disorder check list 5 (PCL-5) [41,51], the Pandemic-Related Pregnancy Stress scale (PREPS) [61], the Kessler Psychological Distress Scale (K10), [51], Hospital Anxiety, Depression and Stress scale (HADS) [42,46], Prenatal Distress Questionnaire (PDQ), Perceived Stress Scale (PSS) [35,36], Depression, Anxiety and Stress Scale-21 (DASS-21) [29]. One of those studies provided results on post-traumatic stress, comparing prevalence in pregnant and non-pregnant women (0.9% and 5.7%, respectively) [41]. Three studies showed distinctive prevalence rates of stress in pregnant women during the pandemic (11.1% in Singapore; 43.9% in Iran and 89.1% in China) [29,30,40]. The scale used by Heidi Preis (PREPS) indicated that pregnant women suffered stress related to prenatal preparation (27.2%) and the risk of prenatal infection (29.1%) [61]. Perceived stress was shown to increase with feelings of loneliness and fear of contagion and it appeared as a predictor in most anxious and depressive symptoms related to COVID-19 [35,53].
3.5. Mood and Psychopathological Symptoms
Social support was evaluated through two questionnaires: the social support effectiveness questionnaire (SSEQ) and the interpersonal support evaluation list (ISEL) (results obtained: 55.8, SD = 14.9 and 34.1, SD = 6.3 respectively) [38]. Insomnia measured though Insomnia severity index (ISI), was present in 2.6% of pregnant women and somatization problems were reported by 2.4% of pregnant women during the pandemic according to the “Somatization subscale of the symptom checklist 90 (SCL-90)” [41]. Results from another study showed that almost 20% of women interviewed suffered clinical insomnia (ISI > 15) (see cross-national study of factors associated with women’s perinatal mental health and wellbeing during the COVID-19 pandemic.) and another study revealed that insomnia was a predictor variable in most anxious and depressive symptoms related to COVID-19 [35]. In order to know the impact of physical activity on anxiety levels and depression of the pregnant women during the pandemic, the Godin Shephard Leisure-Time Exercise Questionnaire was used, the results obtained were 33.1 (SD = 21.2) [38]. Depersonalization problems were measured using two scales: Dissociative Experiences Scale (DES-II) (results obtained: dissociation/depersonalization: pre-pandemic: B = −0.17 (SD = 0.05), pandemic: 0.07 (SD = 0.03); Positive and Negative Affect Schedule (PANAS) (results obtained: negative affectivity: pre-pandemic: −0.64 (SD = 0.04), pandemic: 0.25 (SD = 0.03); low positive affectivity: pre-pandemic: −0.64 (SD = 0.04), pandemic: 0.25 (SD = 0.03) (Berthelot et al., 2020) and PANAS Positive: 28.71 (SD = 6.81); PANAS Negative: 22.61 (SD = 7.18) (Chaves et al., 2021). Finally, the results of Colli et al., 2021., reported that 11.2% was positive for obsessive-compulsive symptoms [53].
4. Discussion
The aim of this study was to describe the psychological impact of the COVID-19 pandemic on pregnant women and to identify the risk factors associated. To date, there are very few longitudinal studies comparing groups of pregnant women with other populations. The findings of this review indicate an increased prevalence of mental health symptomatology during pregnancy during the COVID-19 pandemic. The most prevalence psychological symptoms affecting pregnant women were depression, anxiety, stress and insomnia during the COVID-19 pandemic.
The main variables concerning expectant mothers were fear of using a public transport, staying in public places, the potential contagion of a relative, fear of infection, possible vertical transmission (from mother to the fetus), prematurity or miscarriage associated with the SARS-CoV-2 virus [21]. In turn, an adequate coping strategy is a key point for pregnant women. Variables such as having a good economic situation, an adequate level of education and sufficient social support [57,58] are protective factors against psychological problems. Social isolation and imposed quarantines tend to change the routines of pregnant women, leading to some of them not attending prenatal appointments [7,17]. This fact may increase the risk of adverse effects during pregnancy. Moreover, the exposure to biased information from the media and social networks has also caused pessimistic thoughts in expectant mothers and their relatives [23,58]. Nevertheless, one study indicated that pregnant women showed an advantage of facing mental problems caused by COVID-19, showing fewer depression, anxiety, insomnia, and PTSD symptoms than non-pregnant women [60]. This may be due, on the one hand, to the better previous situation in terms of mental health and socioeconomic status of women who decide to become pregnant, since there were significant differences between characteristics of participants such as age, marital status and occupation.
The findings obtained from the 31 selected studies are in agreement with previous studies. A survey of pregnant women and postpartum women during the pandemic, showed that 40% of participants suffered from post-traumatic stress disorder and around 70% suffered from depression and/or anxiety following the onset of the new virus [62]. It is also in line with the results found in a systematic review that summarized the increase of mental disorders in pregnant women caused by this pandemic [63]. In contrast, previous studies have shown a prevalence of depression lower than 60% [43,45,55]. Nonetheless, these findings point out the importance of providing reliable information since one cause of these problems is the references that pregnant women receive [64]. A longitudinal study showed that the stress generated by COVID-19 is related to fear of contagion and its adverse effects [64]. Furthermore, previous studies pointed out that the stress generated during pregnancy, along with the risk of loneliness, increases the prevalence of depressive symptomatology [15]. Finally, another study points out that women concerns about being infected leads to use of disinfectant products in large quantities, which poses a danger of poisoning [64].
However, the COVID-19 pandemic has not been the first pandemic. The Spanish flu in the beginning of the XX Century and the H1N1 influenza pandemic in 2009 also affected pregnant women. Their levels of anxiety, stress and depression increased as a result of the situation they were exposed to. The measures imposed were similar, so that uncertainty about how the disease would affect the fetus and mother, social distance, the need to be alone at the time of delivery and reducing hospital stay were also responsible for mental problems in the peripartum period [65,66].
4.1. Limitations
The main limitation of this study is the small number of databases consulted and the lack of a meta-analytic perspective. Another issue that should be addressed in future investigations is the point of the pandemic at which the measurement was taken, since recent studies show a significant decrease in anxiety and depression symptoms after one year of its duration [67]. Moreover, the studies included in this review do not discriminate between the main stress factors according to Lancet’s COVID-19 Commission Mental Health Task Force recommendations: contracting the infection, close relation having the infection, safety of others in your care and stress of living in a pandemic [68]. Moreover, most of the included studies were cross-sectional self-report surveys, which could overestimate the real prevalence of this type of psychological disorders. In addition, geographical coverage of the articles selected was focused on high-income countries, which invites to infer that this outcome is a problem exclusive of those countries, which is far from the reality. Another limitation is the variation of the characteristics of the included studies: the sample sizes, the different types of the surveys implemented, the moment of the measurements and their reliability and validity. Finally, the selection bias hinders the ability to make a quantitative summary of the studies.
4.2. Strengths
The main strength is that we have conducted a scoping review following up the PRISMA extension for scoping reviews guidelines. Our search was exhaustive, collecting all kind of psychological symptoms. Finally, the point at which the measurement was taken must be taken into account, since the evolution of the pandemic and the restrictions adopted have been different in each region. For instance, the results of Aknin et al., 2021 showed a significant increase in anxiety and depression symptoms at the beginning of the pandemic and a significant decrease in these symptoms after one year of its duration. Nonetheless, the unexpectedly high rates of current mental health issues warrant an urgent call to action.
4.3. Implications for Practice and Future Research
These data could be helpful to guide future interventions or the adjustment of the pathways of care such as providing accurate information and encouraging pregnant women to engage in healthy behaviors during pregnancy [55,69]. Likewise, communication and reassurance about their routine prenatal care may be a priority to avoid increased levels of depression and anxiety. On the other hand, screening tests for psychological problems (e.g., EPDS, PHQ-9, GAD-7) and intimate partner violence should be implemented. It is essential to promote protective factors and positive coping strategies such as via internet-based mindfulness programs, daily routine, self-care, mindfulness, prenatal or postnatal groups. Another strategy is to provide online mental health resources and tele-psychotherapy to treat psychological problems in the perinatal period.
In order to enhance social support, health care providers may focus on the opportunity that families have, within subsystems and across the family, to buffer pregnant women against the risks of social disruption due to COVID-19 [70]. Clinicians may assess whether pregnant women have adequate social support and encourage them to have regular contact with relative and friends (via telephone, social networks, video calls or face-to-face when possible). Involving the partner during the perinatal period can also be of help. During the COVID-19 pandemic, certain psychological strategies have been reported to have some positive results at reducing anxiety, depression and stress among pregnant women [71]. More precisely, through an online cognitive-behavioral therapy during the COVID-19 pandemic, a group of psychologists managed to reduce a range of psychopathological symptoms in pregnant women. Reducing stress and psychopathological symptoms during pregnancy can also promote the health of the fetus [46]. This fact is associated with the Fetal Programming Hypothesis by which the environment the fetus is exposed to during pregnancy can shape his/her future health and disease after birth [72]. Another activity to promote is prolonged skin-to-skin contact with the infant and early and exclusive breastfeeding, whenever possible.
The women exposed to previous pandemics (e.g., 1918 Spanish Flu) had a higher risk of having children that would prematurely die of a heart attack when adults [73]. A previous study based on more than 65 millions of women found that higher levels of stress during pregnancy is associated with obesity, infantile colic and autism spectrum disorder in the offspring [74].
Finally, this review helps to understand the mental health situation that pregnant women are facing as a result of the current pandemic.
5. Conclusions
The results of this scoping review appear to suggest that levels of anxiety, stress and depression in pregnant women have increased as a result of the COVID-19 pandemic. Nonetheless, these conclusions are drawn from observational studies conducted over a short period of time. Longitudinal studies with a more robust methodology are needed to confirm these results. The characteristics of the included studies also presented characteristics with wide methodological differences. Economic situation, education level and social support have a considerable impact on mental health in pregnant women. All pregnant women should have their psychosocial and mental health status assessed throughout pregnancy and postpartum. In turn, health-care providers may provide relevant and evidence-based information intended for both pregnant woman and their relatives, as well as promoting protective factors such as social support.
Author Contributions
Conceptualization, R.A.C.-G., A.d.l.T.-L. and C.C.-G.; methodology, B.R.-G., R.A.C.-G. and R.A.C.-G.; validation, R.A.C.-G.; formal analysis, R.A.C.-G., B.R.-G. and C.C.-G.; investigation, R.A.C.-G., and C.C.-G.; writing—original draft preparation, R.A.C.-G., B.R.-G. and C.C.-G.; writing—review and editing, B.R.-G., C.C.-G., and A.d.l.T.-L.; visualization, R.A.C.-G. and A.d.l.T.-L.; supervision, B.R.-G. and R.A.C.-G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Alanagreh, L.; Alzoughool, F.; Atoum, M. The Human Coronavirus Disease COVID-19: Its Origin, Characteristics, and Insights into Potential Drugs and Its Mechanisms. Pathogens 2020, 9, 331. [Google Scholar] [CrossRef] [PubMed]
- Umakanthan, S.; Sahu, P.; Ranade, A.V.; Bukelo, M.M.; Rao, J.S.; Abrahao-Machado, L.F.; Dahal, S.; Kumar, H.; Kv, D. Origin, transmission, diagnosis and management of coronavirus disease 2019 (COVID-19). Postgrad Med. J. 2020, 96, 753–758. [Google Scholar] [PubMed]
- Ministerio de Sanidad, Consumo y Bienestar Social—Profesionales—Situación actual Coronavirus. Available online: https://www.mscbs.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov/situacionActual.htm (accessed on 2 September 2021).
- Coronavirus Disease (COVID-19) Pandemic. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019?adgroupsurvey=%7Badgroupsurvey%7D&gclid=Cj0KCQjw7MGJBhD-ARIsAMZ0eeuXa_sAMir7JGEFInKKfby2BZSNQQiICNxjCOYt-lF_nBdn5wD0lkEaAkKXEALw_wcB (accessed on 2 September 2021).
- Kakodkar, P.; Kaka, N.; Baig, M. A Comprehensive Literature Review on the Clinical Presentation, and Management of the Pandemic Coronavirus Disease 2019 (COVID-19). Cureus 2020, 12, e7560. [Google Scholar] [CrossRef]
- Han, Q.; Zheng, B.; Agostini, M.; Bélanger, J.J.; Gützkow, B.; Kreienkamp, J.; Reitsema, A.M.; van Breen, J.A.; Collaboration, P.; Leander, N.P. Associations of risk perception of COVID-19 with emotion and mental health during the pandemic. J. Affect. Disord. 2021, 284, 247–255. [Google Scholar] [CrossRef]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; McIntyre, R.S.; Choo, F.N.; Tran, B.; Ho, R.; Sharma, V.K.; et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain. Behav. Immun. 2020, 87, 40–48. [Google Scholar] [CrossRef] [PubMed]
- Bjelica, A.; Cetkovic, N.; Trninic-Pjevic, A.; Mladenovic-Segedi, L. The phenomenon of pregnancy—A psychological view. Ginekol. Pol. 2018, 89, 102–106. [Google Scholar] [CrossRef]
- Nagandla, K.; Nalliah, S.; Yin, L.; Majeed, Z.; Ismail, I.; Zubaidah, S.; Ragavan, U.; Krishnan, S. Prevalence and associated risk factors of depression, anxiety and stress in pregnancy. Int. J. Reprod. Contracept. Obstet. Gynecol. 2016, 5, 2380–2388. [Google Scholar] [CrossRef]
- Guimaraes, F.J.; Da Silva Santos, F.J.; Bern Leite, A.F.; De Holanda, V.R.; De Sousa, G.S.; Alburquerque Perrelli, J.G. Preferencias Enfermedad mental en mujeres embarazadas. Enfermería Glob. 2018, 18, 499–534. [Google Scholar] [CrossRef]
- Kassada, D.S.; Waidman, M.A.P.; Miasso, A.I.; Marcon, S.S. Prevalência de transtornos mentais e fatores associados em gestantes. Acta Paul. Enferm. 2015, 28, 495–502. [Google Scholar] [CrossRef][Green Version]
- Biaggi, A.; Conroy, S.; Pawlby, S.; Pariante, C.M. Identifying the women at risk of antenatal anxiety and depression: A systematic review. J. Affect. Disord. 2016, 191, 62–77. [Google Scholar] [CrossRef]
- Auger, N.; Potter, B.J.; Healy-Profitós, J.; He, S.; Schnitzer, M.E.; Paradis, G. Mood disorders in pregnant women and future cardiovascular risk. J. Affect. Disord. 2020, 266, 128–134. [Google Scholar] [CrossRef] [PubMed]
- Accortt, E.E.; Cheadle, A.C.D.; Dunkel Schetter, C. Prenatal depression and adverse birth outcomes: An updated systematic review. Matern. Child Health J. 2015, 19, 1306–1337. [Google Scholar] [CrossRef]
- Caparros-Gonzalez, R.A.; Perra, O.; Alderdice, F.; Lynn, F.; Lobel, M.; García-García, I.; Peralta-Ramírez, M.I. Psychometric validation of the Prenatal Distress Questionnaire (PDQ) in pregnant women in Spain. Women Health 2019, 59, 937–952. [Google Scholar] [CrossRef] [PubMed]
- Knight, M.; Bunch, K.; Vousden, N.; Morris, E.; Simpson, N.; Gale, C.; O’Brien, P.; Quigley, M.; Brocklehurst, P.; Kurinczuk, J.J.; et al. Characteristics and outcomes of pregnant women admitted to hospital with confirmed SARS-CoV-2 infection in UK: National population based cohort study. BMJ 2020, 369, m2107. [Google Scholar] [CrossRef]
- Sapkota, B.; Mali, N.S.; Singh, R.D. Prenatal Anxiety among Pregnant Women Visiting in Antenatal Care Outpatient Department at Paropakar Maternity and Women’s Hospital. Int. J. Health Sci. Res. 2019, 9, 173–181. [Google Scholar]
- Ravaldi, C.; Ricca, V.; Wilson, A.; Homer, C.; Vannacci, A. Previous psychopathology predicted severe COVID-19 concern, anxiety, and PTSD symptoms in pregnant women during “lockdown” in Italy. Arch. Women’s Ment. Heals 2020, 23, 783–786. [Google Scholar] [CrossRef]
- Caparros-Gonzalez, R.A.; Luque-Fernández, M.Á. Mental health in the perinatal period and maternal stress during the Covid-19 pandemic: Influence on fetal development. Rev. Esp. Salud Publica 2020, 94, e1–e2. [Google Scholar]
- Caparros-Gonzalez, R.A.; Ganho-Ávila, A.; Torre-Luque, A. de la The COVID-19 Pandemic Can Impact Perinatal Mental Health and the Health of the Offspring. Behav. Sci. 2020, 10, 162. [Google Scholar] [CrossRef] [PubMed]
- Naurin, E.; Markstedt, E.; Stolle, D.; Enström, D.; Wallin, A.; Andreasson, I.; Attebo, B.; Eriksson, O.; Martinsson, K.; Elden, H.; et al. Pregnant under the pressure of a pandemic: A large-scale longitudinal survey before and during the COVID-19 outbreak. Eur. J. Public Health 2021, 31, 7–13. [Google Scholar] [CrossRef]
- Shayganfard, M.; Mahdavi, F.; Haghighi, M.; Sadeghi Bahmani, D.; Brand, S. Health Anxiety Predicts Postponing or Cancelling Routine Medical Health Care Appointments among Women in Perinatal Stage during the Covid-19 Lockdown. Int. J. Environ. Res. Public Health 2020, 17, 8272. [Google Scholar] [CrossRef]
- Pacheco, F.; Sobral, M.; Guiomar, R.; de la Torre-Luque, A.; Caparros-Gonzalez, R.A.; Ganho-ávila, A. Breastfeeding during covid-19: A narrative review of the psychological impact on mothers. Behav. Sci. 2021, 11, 34. [Google Scholar] [CrossRef] [PubMed]
- Brik, M.; Sandonis, M.A.; Fernández, S.; Suy, A.; Parramon-Puig, G.; Maiz, N.; Dip, M.E.; Ramos-Quiroga, J.A.; Carreras, E. Psychological impact and social support in pregnant women during lockdown due to SARS-CoV2 pandemic: A cohort study. Acta obstetricia et gynecologica Scandinavica 2021, 100, 1026–1033. [Google Scholar] [CrossRef] [PubMed]
- He, D.; Ren, J.; Luo, B.; Xiang, J.; Wang, G.; Gu, L.; Chen, P. Women’s Psychological Health, Family Function, and Social Support During Their Third Trimester of Pregnancy Within the COVID-19 Epidemic: A Cross-sectional Survey. Disaster Med. Public Health Prep. 2021, 1–5, Advance online publication. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Munn, Z.; Peters, M.D.J.; Stern, C.; Tufanaru, C.; McArthur, A.; Aromataris, E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med. Res. Methodol. 2018, 18, 143. [Google Scholar] [CrossRef]
- Effati-Daryani, F.; Zarei, S.; Mohammadi, A.; Hemmati, E.; Ghasemi Yngyknd, S.; Mirghafourvand, M. Depression, stress, anxiety and their predictors in Iranian pregnant women during the outbreak of COVID-19. BMC Psychol. 2020, 8, 99. [Google Scholar] [CrossRef]
- Jiang, H.; Jin, L.; Qian, X.; Xiong, X.; La, X.; Chen, W.; Yang, X.; Yang, F.; Zhang, X.; Abudukelimu, N.; et al. Maternal Mental Health Status and Approaches for Accessing Antenatal Care Information During the COVID-19 Epidemic in China: Cross-Sectional Study. J. Med. Internet Res. 2021, 23, e18722. [Google Scholar] [CrossRef] [PubMed]
- Matsushima, M.; Horiguchi, H. The COVID-19 Pandemic and Mental Well-Being of Pregnant Women in Japan: Need for Economic and Social Policy Interventions. Disaster Med. Public Health Prep. 2020, 1–6. [Google Scholar] [CrossRef]
- Shahid, A.; Javed, A.; Rehman, S.; Tariq, R.; Ikram, M.; Suhail, M. Evaluation of psychological impact, depression, and anxiety among pregnant women during the COVID-19 pandemic in Lahore, Pakistan. Int. J. Gynaecol. Obstet. 2020, 151, 462–465. [Google Scholar] [CrossRef]
- Sun, G.; Wang, Q.; Lin, Y.; Li, R.; Yang, L.; Liu, X.; Peng, M.; Wang, H.; Yang, X.; Ren, W.; et al. Perinatal Depression of Exposed Maternal Women in the COVID-19 Pandemic in Wuhan, China. Front. Psychiatry 2020, 11, 551812. [Google Scholar] [CrossRef]
- Wu, Y.; Zhang, C.; Liu, H.; Duan, C.; Li, C.; Fan, J.; Li, H.; Chen, L.; Xu, H.; Li, X.; et al. Perinatal depressive and anxiety symptoms of pregnant women during the coronavirus disease 2019 outbreak in China. Am. J. Obstet. Gynecol. 2020, 223, e1–e240. [Google Scholar] [CrossRef] [PubMed]
- Romero-Gonzalez, B.; Puertas-Gonzalez, J.A.; Mariño-Narvaez, C.; Peralta-Ramirez, M.I. Variables del confinamiento por COVID-19 predictoras de sintomatología ansiosa y depresiva en mujeres embarazadas. Med. Clin. 2021, 156, 172–176. [Google Scholar] [CrossRef]
- Puertas-Gonzalez, J.A.; Mariño-Narvaez, C.; Peralta-Ramirez, M.I.; Romero-Gonzalez, B. The psychological impact of the COVID-19 pandemic on pregnant women. Psychiatry Res. 2021, 301, 113978. [Google Scholar] [CrossRef] [PubMed]
- Yirmiya, K.; Yakirevich-Amir, N.; Preis, H.; Lotan, A.; Atzil, S.; Reuveni, I. Women’s Depressive Symptoms during the COVID-19 Pandemic: The Role of Pregnancy. Int. J. Environ. Res. Public Health 2021, 18, 4298. [Google Scholar] [CrossRef] [PubMed]
- Lebel, C.; MacKinnon, A.; Bagshawe, M.; Tomfohr-Madsen, L.; Giesbrecht, G. Elevated depression and anxiety symptoms among pregnant individuals during the COVID-19 pandemic. J. Affect. Disord. 2020, 277, 5–13. [Google Scholar] [CrossRef]
- Moyer, C.A.; Compton, S.D.; Kaselitz, E.; Muzik, M. Pregnancy-related anxiety during COVID-19: A nationwide survey of 2740 pregnant women. Arch. Womens. Ment. Health 2020, 23, 757–765. [Google Scholar] [CrossRef]
- Ng, Q.J.; Koh, K.M.; Tagore, S.; Mathur, M. Perception and Feelings of Antenatal Women during COVID-19 Pandemic: A Cross-Sectional Survey. Ann. Acad. Med. Singapore 2020, 49, 543–552. [Google Scholar] [CrossRef]
- Zhou, Y.; Shi, H.; Liu, Z.; Peng, S.; Wang, R.; Qi, L.; Li, Z.; Yang, J.; Ren, Y.; Song, X.; et al. The prevalence of psychiatric symptoms of pregnant and non-pregnant women during the COVID-19 epidemic. Transl. Psychiatry 2020, 10, 319. [Google Scholar] [CrossRef]
- Akgor, U.; Fadıloglu, E.; Soyak, B.; Unal, C.; Cagan, M.; Temiz, B.E.; Erzenoglu, B.E.; Ak, S.; Gultekin, M.; Ozyuncu, O. Anxiety, depression and concerns of pregnant women during the COVID-19 pandemic. Arch. Gynecol. Obstet. 2021, 304, 125–130. [Google Scholar] [CrossRef]
- Farrell, T.; Reagu, S.; Mohan, S.; Elmidany, R.; Qaddoura, F.; Ahmed, E.E.; Corbett, G.; Lindow, S.; Abuyaqoub, S.M.; Alabdulla, M.A. The impact of the COVID-19 pandemic on the perinatal mental health of women. J. Perinat. Med. 2020, 48, 971–976. [Google Scholar] [CrossRef]
- Khoury, J.E.; Atkinson, L.; Bennett, T.; Jack, S.M.; Gonzalez, A. COVID-19 and mental health during pregnancy: The importance of cognitive appraisal and social support. J. Affect. Disord. 2021, 282, 1161–1169. [Google Scholar] [CrossRef]
- López-Morales, H.; Del Valle, M.V.; Canet-Juric, L.; Andrés, M.L.; Galli, J.I.; Poó, F.; Urquijo, S. Mental health of pregnant women during the COVID-19 pandemic: A longitudinal study. Psychiatry Res. 2021, 295, 113567. [Google Scholar] [CrossRef]
- Kahyaoglu Sut, H.; Kucukkaya, B. Anxiety, depression, and related factors in pregnant women during the COVID-19 pandemic in Turkey: A web-based cross-sectional study. Perspect. Psychiatr. Care 2021, 57, 860–868. [Google Scholar] [CrossRef] [PubMed]
- Ayaz, R.; Hocaoğlu, M.; Günay, T.; Yardımcı, O.D.; Turgut, A.; Karateke, A. Anxiety and depression symptoms in the same pregnant women before and during the COVID-19 pandemic. J. Périnat. Med. 2020, 48, 965–970. [Google Scholar] [CrossRef] [PubMed]
- Taubman-Ben-Ari, O.; Chasson, M.; Abu Sharkia, S.; Weiss, E. Distress and anxiety associated with COVID-19 among Jewish and Arab pregnant women in Israel. J. Reprod. Infant Psychol. 2020, 38, 340–348. [Google Scholar] [CrossRef] [PubMed]
- Berthelot, N.; Lemieux, R.; Garon-Bissonnette, J.; Drouin-Maziade, C.; Martel, É.; Maziade, M. Uptrend in distress and psychiatric symptomatology in pregnant women during the coronavirus disease 2019 pandemic. Acta Obstet. Gynecol. Scand. 2020, 99, 848–855. [Google Scholar] [CrossRef]
- Kassaw, C.; Pandey, D. The prevalence of general anxiety disorder and its associated factors among women’s attending at the perinatal service of Dilla University referral hospital, Dilla town, Ethiopia, April, 2020 in Covid pandemic. Heliyon 2020, 6, e05593. [Google Scholar] [CrossRef]
- Liu, X.; Chen, M.; Wang, Y.; Sun, L.; Zhang, J.; Shi, Y.; Wang, J.; Zhang, H.; Sun, G.; Baker, P.; et al. Prenatal anxiety and obstetric decisions among pregnant women in Wuhan and Chongqing during the COVID-19 outbreak: A cross-sectional study. BJOG An. Int. J. Obstet. Gynaecol. 2020, 127, 1229–1240. [Google Scholar] [CrossRef]
- Sinaci, S.; Ozden Tokalioglu, E.; Ocal, D.; Atalay, A.; Yilmaz, G.; Keskin, H.L.; Erdinc, S.O.; Sahin, D.; Moraloglu Tekin, O. Does having a high-risk pregnancy influence anxiety level during the COVID-19 pandemic? Eur. J. Obstet. Gynecol. Reprod. Biol. 2020, 255, 190–196. [Google Scholar] [CrossRef]
- Colli, C.; Penengo, C.; Garzitto, M.; Driul, L.; Sala, A.; Degano, M.; Preis, H.; Lobel, M.; Balestrieri, M. Prenatal Stress and Psychiatric Symptoms During Early Phases of the COVID-19 Pandemic in Italy. Int. J. Womens. Health 2021, 13, 653–662. [Google Scholar] [CrossRef]
- Preis, H.; Mahaffey, B.; Heiselman, C.; Lobel, M. Vulnerability and resilience to pandemic-related stress among U.S. women pregnant at the start of the COVID-19 pandemic. Soc. Sci. Med. 2020, 266, 113348. [Google Scholar] [CrossRef]
- Chaves, C.; Marchena, C.; Palacios, B.; Salgado, A.; Duque, A. Effects of the COVID-19 pandemic on perinatal mental health in Spain: Positive and negative outcomes. Women Birth 2021, in press. [Google Scholar] [CrossRef]
- Davenport, M.H.; Meyer, S.; Meah, V.L.; Strynadka, M.C.; Khurana, R. Moms Are Not OK: COVID-19 and Maternal Mental Health. Front. Glob. Women’s Health 2020, 1. [Google Scholar] [CrossRef]
- Mappa, I.; Distefano, F.A.; Rizzo, G. Effects of coronavirus 19 pandemic on maternal anxiety during pregnancy: A prospectic observational study. J. Perinat. Med. 2020, 48, 545–550. [Google Scholar] [CrossRef]
- Saccone, G.; Florio, A.; Aiello, F.; Venturella, R.; De Angelis, M.C.; Locci, M.; Bifulco, G.; Zullo, F.; Di Spiezio Sardo, A. Psychological impact of coronavirus disease 2019 in pregnant women. Am. J. Obstet. Gynecol. 2020, 223, 293–295. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Wu, W.; Zhao, X.; Zhang, W. Recommended psychological crisis intervention response to the 2019 novel coronavirus pneumonia outbreak in China: A model of West China Hospital. Precis. Clin. Med. 2020, 3, 3–8. [Google Scholar] [CrossRef]
- O’Connor, C.; Murphy, M. Going viral: Doctors must tackle fake news in the covid-19 pandemic. BMJ 2020, 369, m1587. [Google Scholar] [CrossRef] [PubMed]
- Lemieux, R.; Garon-Bissonnette, J.; Loiselle, M.; Martel, É.; Drouin-Maziade, C.; Berthelot, N. Association entre la fréquence de consultation des médias d’information et la détresse psychologique chez les femmes enceintes durant la pandémie de COVID-19: Association between news media consulting frequency and psychological distress in pregnant women. Can. J. Psychiatry 2021, 66, 34–42. [Google Scholar] [CrossRef] [PubMed]
- Shao, B.; Mo, M.; Xin, X.; Jiang, W.; Wu, J.; Huang, M.; Wang, S.; Muyiduli, X.; Si, S.; Shen, Y.; et al. The interaction between prepregnancy BMI and gestational vitamin D deficiency on the risk of gestational diabetes mellitus subtypes with elevated fasting blood glucose. Clin. Nutr. 2020, 39, 2265–2273. [Google Scholar] [CrossRef]
- Basu, A.; Kim, H.H.; Basaldua, R.; Choi, K.W.; Charron, L.; Kelsall, N.; Hernandez-Diaz, S.; Wyszynski, D.F.; Koenen, K.C. A cross-national study of factors associated with women’s perinatal mental health and wellbeing during the COVID-19 pandemic. PLoS ONE 2021, 16, e0249780. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.K.; Weston, D.; Greenberg, N. Psychological impact of infectious disease outbreaks on pregnant women: Rapid evidence review. Public Health 2020, 189, 26–36. [Google Scholar] [CrossRef] [PubMed]
- Rogozińska, E.; Marlin, N.; Jackson, L.; Rayanagoudar, G.; Ruifrok, A.E.; Dodds, J.; Molyneaux, E.; van Poppel, M.N.M.; Poston, L.; Vinter, C.A.; et al. Effects of antenatal diet and physical activity on maternal and fetal outcomes: Individual patient data meta-analysis and health economic evaluation. Health Technol. Assess. 2017, 21, 1–158. [Google Scholar] [CrossRef]
- Dubey, S.; Biswas, P.; Ghosh, R.; Chatterjee, S.; Dubey, M.J.; Chatterjee, S.; Lahiri, D.; Lavie, C.J. Psychosocial impact of COVID-19. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 779–788. [Google Scholar] [CrossRef]
- Braunack-Mayer, A.; Tooher, R.; Collins, J.E.; Street, J.M.; Marshall, H. Understanding the school community’s response to school closures during the H1N1 2009 influenza pandemic. BMC Public Heals 2013, 13, 344. [Google Scholar] [CrossRef]
- Aknin, L.; De Neve, J.-E.; Dunn, E.; Fancourt, D.; Goldberg, E.; Helliwell, J.; Jones, S.P.; Karam, E.; Layard, R.; Lyubomirsky, S.; et al. Mental Health During the First Year of the COVID-19 Pandemic: A Review and Recommendations for Moving Forward. PsyArXiv 2021. [Google Scholar] [CrossRef]
- Cannella, D.; Lobel, M.; Monheit, A. Knowing is believing: Information and attitudes towards physical activity during pregnancy. J. Psychosom. Obstet. Gynecol. 2010, 31, 236–242. [Google Scholar] [CrossRef]
- Sun, S.; Goldberg, S.B.; Lin, D.; Qiao, S.; Operario, D. Psychiatric symptoms, risk, and protective factors among university students in quarantine during the COVID-19 pandemic in China. Global. Health 2021, 17, 15. [Google Scholar] [CrossRef]
- Puertas-Gonzalez, J.A.; Mariño-Narvaez, C.; Romero-Gonzalez, B.; Peralta-Ramirez, M.I. Stress and Psychopathology Reduction in Pregnant Women through Online Cognitive Behavioural Therapy during COVID-19: A Feasibility Study. Behav. Sci. 2021, 11, 100. [Google Scholar] [CrossRef] [PubMed]
- Barker, D.J.P. Fetal programming of coronary heart disease. Trends Endocrinol. Metab. 2002, 13, 364–368. [Google Scholar] [CrossRef]
- Helgertz, J.; Bengtsson, T. The Long-Lasting Influenza: The Impact of Fetal Stress During the 1918 Influenza Pandemic on Socioeconomic Attainment and Health in Sweden, 1968–2012. Demography 2019, 56, 1389–1425. [Google Scholar] [CrossRef] [PubMed]
- Caparros-Gonzalez, R.A.; de la Torre-Luque, A.; Romero-Gonzalez, B.; Quesada-Soto, J.M.; Alderdice, F.; Peralta-Ramírez, M.I. Stress During Pregnancy and the Development of Diseases in the offspring: A Systematic-Review and Meta-Analysis. Midwifery 2021, 97, 102939. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).