Abstract
Tuberculosis (TB) represents a global public health threat and is a leading cause of morbidity and mortality worldwide. Effective control of TB is complicated with the emergence of multidrug resistance. Yet, there is a fundamental gap in understanding the complex and dynamic interactions between different Mycobacterium tuberculosis strains and the host. In this pilot study, we investigated the host immune response to different M. tuberculosis strains, including drug-sensitive avirulent or virulent, and rifampin-resistant or isoniazid-resistant virulent strains in human THP-1 cells. We identified major differences in the gene expression profiles in response to infection with these strains. The expression of IDO1 and IL-1β in the infected cells was stronger in all virulent M. tuberculosis strains. The most striking result was the overexpression of many interferon-stimulated genes (ISGs) in cells infected with the isoniazid-resistant strain, compared to the rifampin-resistant and the drug-sensitive strains. Our data indicate that infection with the isoniazid-resistant M. tuberculosis strain preferentially resulted in cGAS-STING/STAT1 activation, which induced a characteristic host immune response. These findings reveal complex gene signatures and a dynamic variation in the immune response to infection by different M. tuberculosis strains.
1. Introduction
Tuberculosis (TB), caused by Mycobacterium tuberculosis infection, represents a disease of global public health importance and remains a leading cause of morbidity and mortality. It is the second most common cause of death due to a single infectious agent after COVID-19, surpassing HIV/AIDS [1,2]. About a quarter of the world’s population is currently infected with M. tuberculosis, with more than 10 million new cases of active TB reported globally, resulting in more than 1.5 million deaths annually. The emergence of drug-resistant TB and the increasing incidence of multidrug-resistant (MDR) and, more recently, of extensively drug-resistant (XDR) and totally drug-resistant (TDR) M. tuberculosis strains are an important public health threat and jeopardize current efforts to TB control and prevention [3,4,5,6]. About 450,000 cases of MDR-TB are recorded each year, with a global treatment success rate of 60% [1]. Resistance to rifampin and/or isoniazid is of major concern, since these two drugs represent the cornerstone of the first-line TB treatment, and resistance to both drugs is linked to all multidrug-resistant forms of TB (MDR, XDR, and TDR). Furthermore, monoresistance to isoniazid is noticeably common in contrast to monoresistance to rifampin. Resistance to rifampin typically occurs in strains that are also resistant to isoniazid. While rifampin is unequivocally the most important drug in the global fight against active TB, isoniazid is critical not only for the management of active TB, but it has long been the standard of care for latent TB treatment [7].
The M. tuberculosis cell wall has a complex composition and structure. It is considered to be a major virulence factor and to promote the resistance of M. tuberculosis to antibiotics [8]. Interestingly, the cell wall is significantly thicker in drug-resistant M. tuberculosis strains compared to drug-sensitive strains [9,10]. Cell wall lipids in M. tuberculosis play a significant role in modulating the host immune response, pathogenesis, and virulence [11,12,13,14]. Mycolic acids represent the hallmark of the M. tuberculosis cell wall, and their biosynthesis and regulation are the targets of isoniazid [15,16]. Upon exposure to isoniazid, M. tuberculosis uses different tolerance strategies to overcome the inhibition of mycolic acids biosynthesis induced by isoniazid [17]. As the concentration of mature mycolic acids decreases, the lipid composition becomes altered, which influences M. tuberculosis physiology and host pathogenesis [14,18]. Significant changes in lipid metabolism (β-oxidation of fatty acids) after the acquisition of isoniazid resistance have also been documented [19,20]. While isoniazid blocks the synthesis of the cell-wall mycolic acids, the mechanism of action of the other major anti-TB drug, rifampin, is to inhibit mycobacterial transcription by targeting DNA-dependent RNA polymerase. Resistance to rifampin has been mainly linked to mutations in the gene encoding the β-subunit of RNA polymerase (rpoB gene) [21].
M. tuberculosis is remarkably successful at evading the host immune response [22]. This pathogen adopts several strategies to avoid clearance and persist in the host [23,24]. Macrophages play a crucial role in host defense against M. tuberculosis by promoting the activation of different signaling pathways [25,26]. In particular, cGAS, TBK1, and NF-κB are known to be strongly involved in the activation of the innate immunity by the release of many cytokines, such as IL-1β, and the expression of many interferon-stimulated genes (ISGs) [27,28]. Nevertheless, our understanding of the host–M. tuberculosis interactions is still limited, and many fundamental gaps in our knowledge remain in how these interactions may differ in response to distinct M. tuberculosis strains [29,30].
Infections with different M. tuberculosis genotypes have major impacts on host–pathogen interaction, which can lead to substantial differences in the host immune responses [31,32,33]. The emergence of some mycobacterial lineages, such as the Beijing genotype family, has even been linked to an evolutionary adaptive response to drug resistance [34]. Beijing strains have shown specific properties in their interaction with the host immune system, suggesting a possible human–pathogen co-evolution. The immune response of infected macrophages also showed a wide variation in the response to different M. tuberculosis strains [35]. All of these studies contributed with others to substantial advances in our understanding of TB pathogenesis. However, further work is needed to explore the host immune response to different M. tuberculosis strains and how these differences in immune responses could affect TB pathogenesis. In this pilot study, we tackled this question and investigated the host immune response to different reference M. tuberculosis strains, including drug-sensitive avirulent or virulent, and rifampin-resistant or isoniazid-resistant virulent strains in THP-1 cells. Shifting the focus to the specific impact on differential host interaction with M. tuberculosis strains has the potential to improve our understanding of TB pathogenesis and initiate efforts for a roadmap towards better TB control and prevention strategies.
2. Materials and Methods
2.1. Cell Line and M. tuberculosis Strains
For this study, we used human monocytic THP-1 cells (American Type Culture Collection; Catalog No. TIB-202). The cells were maintained in RPMI 1640 medium supplemented with 10% heat-inactivated fetal bovine serum (FBS) at 37 °C and 5% CO2 in a humidified incubator. THP-1 cells were subsequently differentiated for 48 h with 10 ng/mL phorbol 12-myristate 13-acetate (PMA). The cells were then infected with four different reference mycobacterial strains (H37Ra, H37Rv, H37Rv-INH-R, and H37Rv-RIF-R) at an MOI of 10, as commonly used in other studies [36,37,38]. Both H37Ra (avirulent strain; American Type Culture Collection; Product No. 25177) and H37Rv (virulent strain; American Type Culture Collection; Product No. 27294) are drug-sensitive. H37Rv-INH-R (American Type Culture Collection; Product No. 35822) and H37Rv-RIF-R (American Type Culture Collection; Product No. 35838), are both derivatives of H37Rv, and they are resistant to isoniazid and rifampin, respectively. We used two time points for infection (4 and 24 h) in order to monitor differences in gene expression patterns for differentially expressed genes. In addition to the infected THP-1 samples, we also used uninfected control cells (mock-infected with PBS) as negative controls.
2.2. RNA Isolation and Processing
Total RNA was extracted from controls and infected cells, using TRIzol (Invitrogen, Carlsbad, CA, USA) according to the manufacturer’s protocol. Ten samples were used in total, with 5 samples (negative control, H37Ra, H37Rv, H37Rv-INH-R, and H37Rv-RIF-R) at 4 h and 24 h, representing early infection and late infection, respectively [39]. RNA was then suspended in RNase-free water and stored at −80 °C until further use. RNA quality was assessed to verify its integrity using an Agilent 2100 Bioanalyzer (Agilent Technologies, Santa Clara, CA, USA), and RNA quantity was evaluated by spectrophotometry using NanoDrop 2000 (NanoDrop Technologies, Wilmington, DE, USA). All RNA samples showed a good RNA yield and no RNA degradation. Total RNA was then reverse transcribed to cDNA, amplified, labeled, and hybridized to separate arrays using the GeneChip Human Exon 1.0 ST Array (Affymetrix, Santa Clara, CA, USA), according to the manufacturer’s instructions. For transcriptional profiling, we used triplicate hybridization assays in our microarray experiments in order to assess variability among independent labeling reactions and hybridizations, as well as variation for gene expression in the infected cells [40]. Quality control of the hybridized arrays was also performed for each sample. A visual inspection of the scanned images was conducted, looking for any defects, areas of high background, or areas of low signal. The spike-in controls were checked as well to examine for hybridization uniformity.
2.3. Microarray Analysis for Differential Gene Expression
Data from all 10 samples were preprocessed and then summarized at the transcript-cluster (gene) level, and RMA was normalized using Affymetrix Power Tools. Prior to differential expression analysis, low-variability genes were filtered out, leaving 13,460 genes. Differentially expressed genes (DEGs) were identified using the R/Bioconductor package limma [41]. Significant differential expression was defined by a false discovery rate (FDR)-adjusted p-value of less than 0.05, which is calculated by the Benjamini–Hochberg procedure [42]. The visualization of the DEGs in the volcano plots was performed using base R graphics. The R statistical software (version 3.3.3) was also used to produce a heatmap based on the top 100 most significant DEGs in THP-1 cells infected with H37Rv-INH-R relative to mock-infected cells at 24 h post-infection. In order to identify the overlapping DEGs in our data, we generated Venn diagrams, as well using VennDiagram package in R [43,44]. The complete dataset for the microarray analysis of all 10 samples was deposited in the NCBI Gene Expression Omnibus database (GEO; https://www.ncbi.nlm.nih.gov/geo/; accessed on 22 October 2024) and can be publicly accessed through GEO Series accession number GSE246736.
2.4. Functional Enrichment Analysis
To categorize the biological functions of the DEGs in our dataset, we used the DAVID database (https://david.ncifcrf.gov, accessed on 22 October 2024) to perform a Gene Ontology (GO) term enrichment analysis of biological processes, cellular components, and molecular functions; and a Kyoto Encyclopedia of Genes and Genome (KEGG) pathway enrichment analysis [45,46]. A p-value < 0.05 was used as the cut-off value for screening significantly enriched DEGs.
3. Results
3.1. Identification of Differentially Expressed Genes
In this pilot study, we generated gene expression profiles of THP-1 cell lines infected with the following M. tuberculosis reference strains: H37Ra, H37Rv, H37Rv-INH-R, and H37Rv-RIF-R. We chose to use THP-1 cells because they have been shown to display comparable mycobacterial uptake, cellular viability, and cytokine/chemokine induction profiles as human monocyte-derived macrophages [47,48]. Previous studies have shown different transcriptomic profiles comparing THP-1 cells infected with H37Rv, H37Ra, and BCG vaccine [49,50]. These cells can also be reliably grown in the lab and allow us to avoid the putative confounding effects that might arise from genetic differences within macrophages isolated from different donors. The multidimensional scaling (MDS) plot for the microarray expression data showed well-separated grouping according to infections vs. mock infections, and time points of infections (Figure 1).
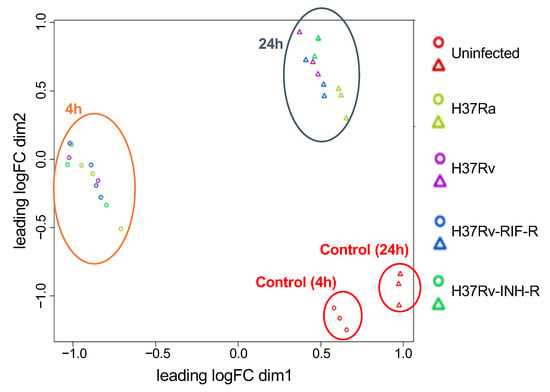
Figure 1.
Multidimensional scaling (MDS) plot based on the expression of all microarray genes between M. tuberculosis-infected and mock-infected THP-1 cells at two time points of infection. Circles represent data based on 4 h post-infection, and triangles depict data based on 24 h post-infection. Each specifically colored circle or triangle represents a replicate of each sample.
A large number of DEGs were detected between infected and mock-infected cells, with the virulent M. tuberculosis strains (H37Rv, H37Rv-INH-R, and H37Rv-RIF-R) showing more DEGs than the non-virulent strain (H37Ra) at 24 h post-infection (Figure 2A). Pairwise comparisons between cells infected with the different strains showed only a few DEGs at 4 h post-infection, but higher numbers after 24 h of infection, with most DEGs detected when avirulent and virulent strains were compared (Figure 2B). Our comparison of H37Rv- with H37Rv-INH-R- and H37Rv-RIF-R-infected cells revealed 55 and 201 DEGs 24 h post-infection, respectively. Based on these findings, the subsequent analyses were therefore focused on the 24-h time point.
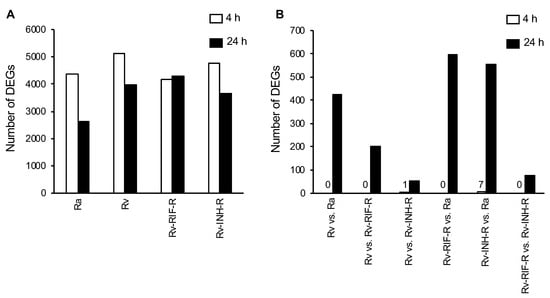
Figure 2.
Number of differentially expressed genes (DEGs) in THP-1 cells at 4 h and 24 h post-infection (p < 0.05). (A) M. tuberculosis-infected cells relative to mock-infected cells. (B) Pairwise comparisons of M. tuberculosis-infected cells.
We next generated Venn diagrams to identify overlapping DEGs. We first analyzed the DEGs by comparing infected and non-infected THP-1 cells. A total of 2608 DEGs were shared between all comparison groups (Figure 3A). In total, 1043 DEGs were shared in the comparison with cells infected with the virulent strains (H37Rv, H37Rv-INH-R, and H37Rv-RIF-R), but not in the group with H37Ra-infected cells. Of note, 319 DEGs stood for a unique profile associated with H37Rv-RIF-R-infected cells. The pairwise comparisons between infected cells showed a total of 55 common DEGs, which represent the overall number of DEGs significant in all four comparisons, with 226 unique genes which were only significant in the pairwise-comparison group H37Rv- vs. H37Ra-infected THP-1 cells (Figure 3B).
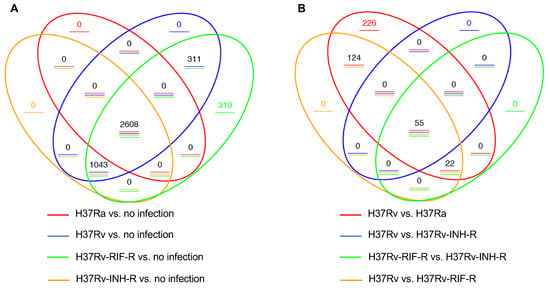
Figure 3.
Venn diagrams of DEGs in THP-1 cells at 24 h post-infection (p < 0.05). The overlapping genes represent the overall number of DEGs between the different comparison groups, while the non-overlapping numbers designate the unique genes to each group. (A) Pairwise comparisons between M. tuberculosis-infected and mock-infected cells. (B) Pairwise comparisons between M. tuberculosis-infected cells.
3.2. Differential Gene Expression in Isoniazid-Resistant M. tuberculosis Infection
Comparison of relative expression of DEGs at 24 h post-infection revealed distinct expression patterns. Whereas some DEGs were up-regulated to comparable levels in all infections (e.g., TNFAIP6), some DEGs, such as IDO1 and IL-1β, were up-regulated to comparable levels in all infections with the virulent reference strains but expressed less in cells infected with the avirulent strain H37Ra (Figure 4A). Strikingly, a subset of DEGs was most strongly induced in H37Rv-INH-R-infected cells, including many interferon-stimulated genes (ISGs), such as CXCL10, MX1, OAS2, IFIT1, DDX58, eIF2aK2 (PKR), RSAD2, and TRIM22 (Figure 4A–C). Relative gene expression differences between infections with H37Rv-INH-R vs. the other strains are also shown in the volcano plots (Figure 5). As a result of this striking differential expression in cells infected with H37Rv-INH-R at 24 h compared to the other infections, we selected the top 100 highly expressed DEGs in H37Rv-INH-R-infected cells vs. mock-infected cells at 24 h and generated a heatmap based on these genes, with all comparison groups, at 4 h and 24 h (Figure 6). This analysis showed that the gene expression patterns varied between infections with the four M. tuberculosis strains. Among the DEGs shown in the heatmap, we observed a stronger expression of ISGs associated with H37Rv-INH-R infection (Figure 6).
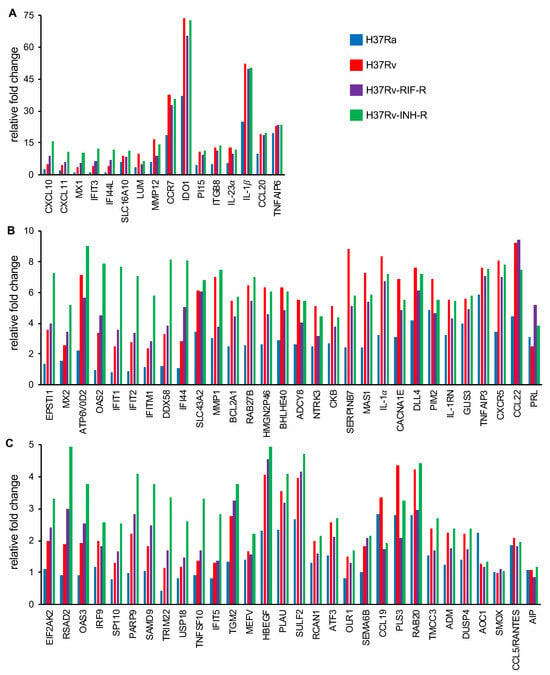
Figure 4.
Fold change in the expression of DEGs in THP-1 cell lines infected with reference M. tuberculosis strains relative to mock-infected cells (24 h post-infection; p < 0.05). Representatives of different degrees of variation in gene expression are depicted in this figure. (A) Relative fold changes in gene expression above 10 are shown. (B) Relative fold changes in gene expression between 5 and 10 are shown. (C) Relative fold changes in gene expression between 1 and 5 are shown.
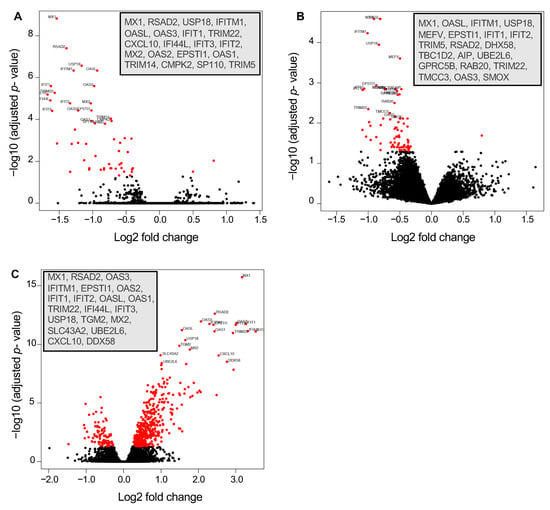
Figure 5.
Volcano plots displaying differentially expressed genes in THP-1 cells in three different comparison groups (24 h post-infection; p < 0.05). The 20 most highly significant DEGs in each plot are indicated in the insets. These genes all indicate higher expression in H37Rv-INH-R-infected cells, relative to H37Rv- and H37Rv-RIF-R-infected cells. (A) H37Rv vs. H37Rv-INH-R. (B) H37Rv-RIF-R vs. H37Rv-INH-R. (C) H37Rv-INH-R vs. H37Ra.
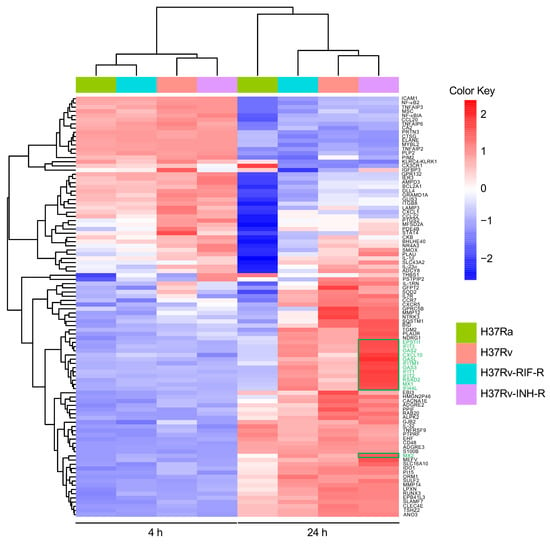
Figure 6.
Heatmap and clustering across M. tuberculosis-infected THP-1 cells relative to mock-infected cells at 4 h and 24 h post-infection, using the top 100 most significant DEGs in cells infected with isoniazid-resistant H37Rv strain at 24 h post-infection. Samples with a relatively high expression of a given gene are shown in red, and samples with a relatively low expression are shown in blue. Lighter color shades and white indicate genes with intermediate expression levels. Some of the interferon-stimulated genes (ISGs) are marked in green, and their overexpression in cells infected with the isoniazid-resistant H37Rv strain is indicated with a green box in the plot.
To determine the key transcription factors that potentially regulate the most significantly expressed DEGs in infected THP-1 cells, we used the interactive web-based program PathwayNet, publicly available at http://pathwaynet.princeton.edu/ (accessed on 22 October 2024) [51]. We examined the interaction predictions for each DEG query in the transcription regulation analysis, and we found the highest relationship confidence in two major transcription factors: signal transducer and activator of transcription 1 (STAT1) and nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB). Differentially expressed ISGs in H37Rv-INH-R were associated with STAT1 signaling, while the expression of many cytokines, such IL-1β, was associated with NF-κB signaling.
3.3. GO and KEGG Enrichment of DEGs in Immune System-Related Pathways
In order to analyze whether DEGs are associated with specific signaling pathways, we performed GO and KEGG enrichment analyses, and we compared two infection groups: drug-sensitive H37Rv vs. H37Rv-INH-R (55 DEGs) and H37Rv-RIF-R vs. H37Rv-INH-R (77 DEGs). Only up-regulated DEGs were considered in these analyses, since only one DEG was down-regulated in the comparison groups.
For the GO enrichment analysis, the 10 most significant biological processes, cellular components, and molecular functions identified are shown in Figure 7A,B and in Table 1 and Table 2. For biological processes, the up-regulated DEGs mainly correlated with innate immune response, defense response to virus, and negative regulation of viral genome replication. The up-regulated DEGs were involved in cellular-component terms, mainly including cytoplasm, cytosol, and nucleoplasm. For molecular functions, the up-regulated DEGs were significantly enriched in terms of protein binding, ubiquitin-protein activity, double-stranded RNA binding, and 2′-5′-oligoadenylate synthetase activity.
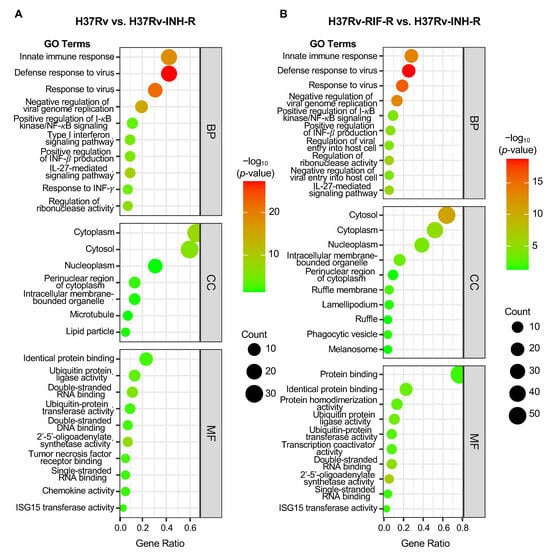
Figure 7.
Bubble plot of GO enrichment analysis of up-regulated DEGs in cells infected with the isoniazid-resistant H37Rv strain (24 h post-infection; p < 0.05). All GO terms are grouped into three categories: biological process (BP), cellular component (CC), and molecular function (MF). (A) Comparison group: drug-sensitive H37Rv vs. isoniazid-resistant H37Rv. (B) Comparison group: rifampin-resistant H37Rv vs. isoniazid-resistant H37Rv.

Table 1.
Top 10 enriched GO terms of DEGs (H37Rv vs. H37Rv-INH-R).

Table 2.
Top 10 enriched GO terms of DEGs (H37Rv-RIF-R vs. H37Rv-INH-R).
The top 10 KEGG enrichments correlated with virus and immune system-related pathways, including influenza A, hepatitis C, NOD-like receptor signaling, DNA and RNA sensing, cytokine–cytokine receptor interaction, and FoxO signaling (Figure 8A,B; Table 3 and Table 4).
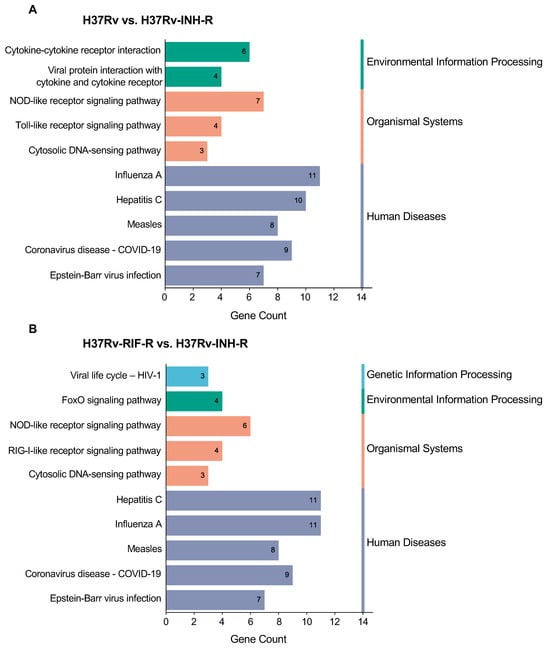
Figure 8.
KEGG analysis of up-regulated DEGs in cells infected with the isoniazid-resistant H37Rv strain. The first ten enriched pathways at 24 h post-infection are shown (p < 0.05). The KEGG pathways were subsequently divided into three or four categories: environmental information processing, organismal systems, genetic information processing and human diseases. (A) Comparison group drug-sensitive H37Rv vs. isoniazid-resistant H37Rv. (B) Comparison group rifampin-resistant H37Rv vs. isoniazid-resistant H37Rv.

Table 3.
Top 10 enriched KEGG pathway terms of DEGs (H37Rv vs. H37Rv-INH-R).

Table 4.
Top 10 enriched KEGG pathway terms of DEGs (H37Rv-RIF-R vs. H37Rv-INH-R).
4. Discussion
Our pilot study revealed considerable differences in the host response to infection with different reference M. tuberculosis strains. The analysis of overlapping genes indicated distinct profiles in infected cells. While 319 DEGs had a unique profile associated with H37Rv-RIF-R-infected cells, no DEG was found to be unique to the cells infected with the other strains. Moreover, the pairwise comparison between the different M. tuberculosis-infected cells indicated 226 unique genes within the cells infected with the drug-sensitive strains (H37Rv vs. H37Ra) but not with the drug-resistant strains. Only a small number of DEGs (55 genes) were also common between all four strains, even though they are all derivatives from the same strain, H37 [52]. This finding emphasizes the complexity of the host immune response to M. tuberculosis infection and warrants further investigations that will lead to a better understanding of the mycobacterial strain- and isolate-specific interactions with their host cells.
We observed major differences in host gene expression when comparing infections with the avirulent H37Ra strain and all virulent H37Rv strains. The expression of IDO1 and IL-1β in the infected cells was stronger with all virulent M. tuberculosis strains, compared to infections with the avirulent strain. Previous work has shown an up-regulation of IDO1 expression in human and murine macrophages upon infection with reference M. tuberculosis strains (e.g., H37Rv), and this finding correlated with higher bacterial burden [53,54]. IL-1β was also shown to be essential in the host resistance to M. tuberculosis infection in mouse models [55,56,57]. A comparison of THP-1 cells infected with H37Rv and the non-virulent H37Ra or BCG previously revealed a significant increase in IL-1β and other pro-inflammatory cytokines in H37Rv-infected cells [50]. Differences in macrophage response between clinical latent TB and active TB cases also correlated with variations in IL-1β expression levels [58]. Furthermore, another study suggested a mechanism driven by IL-1β, in which modern M. tuberculosis lineages induce more IL-1β expression in comparison with ancient lineages, which might contribute to a higher replication rate of the intracellular bacilli [59]. Clinical isolates of M. tuberculosis were also shown to differentially induce IL-1β secretion from macrophages in vitro [60]. In agreement with these findings, our data confirmed differences in the IDO1 and IL-1β expression between four different reference M. tuberculosis strains, with the virulent strains showing the highest expression in these genes. Given the role of IDO1 and IL-1β in TB pathogenesis, this suggests therefore that both of these genes could be considered potential biomarkers for TB infection and could lead to an exciting possibility for the development of novel host-directed TB interventions.
The most striking result of our study is that the infection with H37Rv-INH-R generated a much higher induction of ISGs in comparison to cells infected with H37Rv and H37Rv-RIF-R. Our data indicate that STAT1 was a major transcription factor associated with the DEGs in response to H37Rv-INH-R infection. Multiple recognition and signaling pathways for the host innate immune responses to M. tuberculosis have been documented and characterized, with TLR2-MyD88 and cGAS-STING playing major roles [61]. Our observation that H37Rv-INH-R infection caused the highest ISG expression levels suggests a stronger induction of STAT1 as a result of cGAS-STING activation, rather than TLR2-MyD88 activation. Different signaling pathways may induce changes in the host response to M. tuberculosis infection [28]. Based on our findings, we propose a model for the host signaling response to the different reference M. tuberculosis strains (Figure 9). In addition to the overexpression of ISGs in the cells infected with the isoniazid-resistant M. tuberculosis strain, we also found a higher induction of PKR (eIF2aK2) in those cells. PKR plays a key role in controlling virus infection and has been shown to modulate cytokine expression in response to BCG infection [62] and potentially restrict intracellular replication of the H37Rv-derived strain mc26206 [63]. PKR is also involved in NF-κB activation by more strongly affecting proteins with shorter half-lives, such as the NF-κB inhibitor IκBα [64,65,66]. This links PKR to the observation that NF-κB dynamics play an important role in TB pathogenesis [67,68]. In agreement, we identified NF-κB as the other major transcription factor associated with the DEGs. GO and KEGG pathway enrichment analyses also demonstrated that the up-regulated DEGs in isoniazid-resistant infected cells were significantly enriched in various pathways, especially innate immune response, defense response to viruses, cytoplasm, and protein binding. We found an unexpected up-regulation of many ISGs (e.g., OAS and DDX58) in cells infected with H37Rv-INH-R, and both KEGG and GO analyses indicated an enrichment in the NOD-like receptor signaling pathway, double-stranded RNA binding, and 2′-5′-oligoadenylate synthetase activity. Both PKR and OAS-RNase L pathways have been shown to play an important role in host immune defense and in inducing an increased secretion of IL-1β [69,70,71]. Therefore, it would be interesting to determine how host immunity could be differentially triggered in infections with different M. tuberculosis strains through the activation of some of the pathways identified in this pilot study and the overexpression of IL-1β. Our understanding of the differential gene expression in cells infected with different M. tuberculosis strains still remains very limited. The M. tuberculosis cell wall plays a critical role in modulating the host immune response [22,72]. However, little is known about how its complex structural variations between mycobacterial strains (e.g., drug-sensitive vs. drug-resistant) can influence infection and disease outcome [73,74]. It is therefore important to elucidate how different signaling pathways triggered by the infection with a given M. tuberculosis strain, as proposed in our model, could induce ISG and PKR expression after infection with clinical strains, thus improving our understanding of TB pathogenesis and the host immune response to M. tuberculosis infection.
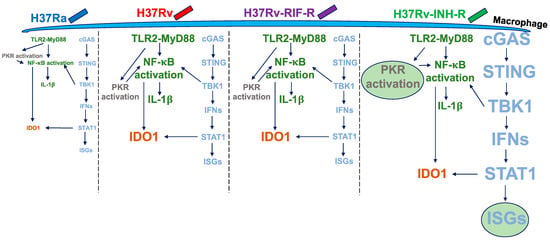
Figure 9.
Model for host signaling response to reference M. tuberculosis strains. Different font size is used to illustrate the changes in host response to the different reference M. tuberculosis strains. Higher gene expression is shown in a big font size, and lower gene expression is shown in small font size. H37Rv-INH-R induced the highest expression of ISGs and PKR compared to the other strains, as indicated by the circles and the big font size.
The mechanism of INH resistance is complex and has been thoroughly studied in an attempt to improve early diagnosis of INH-resistant M. tuberculosis strains [75,76,77,78,79,80,81,82,83]. It is mainly mediated by mutations in the katG gene or in the inhA regulatory regions [84]. INH is activated by the catalase–peroxidase encoded by katG, and this activation interferes with the biosynthesis of mycolic acids by inhibiting NADH-dependent enoyl-ACP reductase encoded by inhA. Mutations in other genes have been also associated with INH resistance; however, they are not as common as the ones in katG (42 to 95%) and inhA (6 to 43%) in M. tuberculosis clinical strains, and their mode of action in INH resistance has not been fully elucidated [85]. Nevertheless, not all INH-resistant strains harbor defined genetic mutations or a defined mechanism associated with resistance to this drug, thus complicating efforts to identify those strains [86]. In addition, some studies indicated that some M. tuberculosis strains acquire drug resistance at higher rates, suggesting a higher mutation rate in these strains and a higher probability that these strains will develop multidrug resistance [87,88]. Resistance to INH is linked to all multidrug-resistant forms of TB (MDR, XDR, and TDR). Several studies have shown that INH resistance is acquired first, followed by resistance to rifampin and the other anti-TB drugs [81,83,89,90,91], thus highlighting the significant impact of INH on the success of treatment in active and latent TB and warranting further efforts to understand the global burden of INH-resistant TB [92].
Our data showed an overexpression of ISGs in THP-1 cells infected with the INH-resistant strain, H37Rv-INH-R, in which the katG gene is deleted. However, it is still unknown how the disruption of katG and inhA, by mutation or deletion, impacts the host response to INH resistance. It is therefore important to define the role of mutations in these genes in regulating the host immune response to INH-resistant M. tuberculosis infection. Such findings will provide a strong foundation for the impact of INH resistance-conferring mutations on the differential host response, which might open up new research avenues to further explore the biological function of these genes and to clarify the underlying molecular mechanisms involved in TB pathogenesis. Nevertheless, further studies are needed to confirm the identified DEGs and pathways in human infections with clinical M. tuberculosis strains.
The differential host immune response to different M. tuberculosis strains (e.g., overexpression of ISGs in the cells infected with H37Rv-INH-R) provides opportunities to define a new facet of host–pathogen interactions that differentially regulates signaling pathways in response to INH-resistant and other M. tuberculosis strains. A recent study investigating a broad profiling of both host and pathogen traits following M. tuberculosis infection with H37Rv strain in a genetically diverse mouse panel indicated distinct immune states and variable inter-species genetic interactions that affect TB pathogenesis [93]. A few studies have already suggested the power of gene expression signatures to detect active TB, differentiate between latent and active TB, and even predict TB disease risk and monitor treatment response [94,95,96,97]. Each of these studies has identified a set of gene signatures for TB; however, our study focused, for the first time, on investigating possible gene signatures associated with different M. tuberculosis strains. The overexpression of ISGs was found to be unique to cells infected with an isoniazid-resistant M. tuberculosis strain, thus warranting further investigation of such a signature in clinical strains or prospective cohort studies. A recent study identified host blood transcriptional signature genes in rifampin-resistant TB infection in comparison with drug-sensitive TB infection [98]. Some DEGs have been identified and were suggested as possible biomarkers to differentiate MDR rifampin-resistant TB patients from drug-sensitive or mono-resistant patients. The characterization of such differential host response has therefore the potential to improve our understanding of the complex and dynamic interactions between M. tuberculosis strains and the host.
While we found compelling differences in the host response to different M. tuberculosis strains, it is important to acknowledge some limitations that need to be addressed in future studies. Even though THP-1 cells represent a good model to study M. tuberculosis interaction with macrophages, the use of other cell lines and ex vivo monocyte-derived macrophages would generate a more thorough analysis of the host immune response to different M. tuberculosis strains. Other important follow-up studies can include infection with different clinical M. tuberculosis strains, for which the host response can be analyzed by RNA sequencing; quantitative RT-PCR; and the analyses of differential protein expression of differentially regulated gene products such as ISGs, IDO1, and IL-1β.
5. Conclusions
Our data showed that each mycobacterial strain was able to induce unique host immune responses in the same cell line, which could have clinical and pathological relevance and lays the groundwork for future studies to investigate strain-specific host–pathogen interactions with clinical M. tuberculosis strains and human monocyte-derived macrophages, and ultimately to develop potential new models for host-directed TB therapies. These findings also provide opportunities for new efforts to develop potential biomarkers and/or therapeutic targets for INH resistance and other TB phenotypes.
Author Contributions
Conceptualization, L.T.; methodology, D.M., L.Y.A. and L.T.; formal analysis, D.M. and L.T.; writing—original draft preparation, L.T.; writing—review and editing, D.M., L.Y.A. and L.T.; supervision, L.T.; funding acquisition, L.T. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the Doris Duke Charitable Foundation COVID-19 Fund to Retain Clinical Scientists awarded to UC Davis School of Medicine by the Burroughs Wellcome Fund, grant number: 2021273-OF (L.T.).
Data Availability Statement
The complete dataset for this study is available from the NCBI Gene Expression Omnibus database (GEO; https://www.ncbi.nlm.nih.gov/geo/; accessed on 22 October 2024) and is publicly accessed through GEO Series accession number GSE246736.
Acknowledgments
The authors acknowledge Ping Wang for her technical support and Blythe Durbin-Johnson at the UC Davis Bioinformatics Core for her assistance in analyzing the microarray data. We also thank Myriam Fornage and Stefan Rothenburg for their insightful discussions and comments on this manuscript.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- World Health Organization (WHO). Global Tuberculosis Report 2022. Available online: https://www.who.int/teams/global-tuberculosis-programme/tb-reports/global-tuberculosis-report-2022 (accessed on 22 June 2023).
- Chakaya, J.; Petersen, E.; Nantanda, R.; Mungai, B.N.; Migliori, G.B.; Amanullah, F.; Lungu, P.; Ntoumi, F.; Kumarasamy, N.; Maeurer, M.; et al. The WHO global tuberculosis 2021 report—Not so good news and turning the tide back to end TB. Int. J. Infect. Dis. 2022, 124, S26–S29. [Google Scholar] [CrossRef] [PubMed]
- Velayati, A.A.; Farnia, P.; Masjedi, M.R. The totally drug resistant tuberculosis (TDR-TB). Int. J. Clin. Exp. Med. 2013, 6, 307–309. [Google Scholar] [PubMed]
- Klopper, M.; Warren, R.M.; Hayes, C.; van Pittius, N.C.G.; Streicher, E.M.; Müller, B.; Sirgel, F.A.; Chabula-Nxiweni, M.; Hoosain, E.; Coetzee, G.; et al. Emergence and spread of extensively and totally drug-resistant tuberculosis, South Africa. Emerg. Infect. Dis. 2013, 19, 449–455. [Google Scholar] [CrossRef] [PubMed]
- Zhan, L.; Wang, J.; Wang, L.; Qin, C. The correlation of drug resistance and virulence in Mycobacterium tuberculosis. Biosaf. Health 2020, 2, 18–24. [Google Scholar] [CrossRef]
- Dean, A.S.; Tosas Auguet, O.; Glaziou, P.; Zignol, M.; Ismail, N.; Kasaeva, T.; Floyd, K. 25 years of surveillance of drug-resistant tuberculosis: Achievements, challenges, and way forward. Lancet Infect. Dis. 2022, 22, e191–e196. [Google Scholar] [CrossRef]
- Getahun, H.; Matteelli, A.; Abubakar, I.; Aziz, M.A.; Baddeley, A.; Barreira, D.; Den Boon, S.; Borroto Gutierrez, S.M.; Bruchfeld, J.; Burhan, E.; et al. Management of latent Mycobacterium tuberculosis infection: WHO guidelines for low tuberculosis burden countries. Eur. Respir. J. 2015, 46, 1563–1576. [Google Scholar] [CrossRef]
- Niederweis, M.; Danilchanka, O.; Huff, J.; Hoffmann, C.; Engelhardt, H. Mycobacterial outer membranes: In search of proteins. Trends Microbiol. 2010, 18, 109–116. [Google Scholar] [CrossRef]
- Velayati, A.A.; Farnia, P.; Ibrahim, T.A.; Haroun, R.Z.; Kuan, H.O.; Ghanavi, J.; Farnia, P.; Kabarei, A.N.; Tabarsi, P.; Omar, A.R.; et al. Differences in cell wall thickness between resistant and nonresistant strains of Mycobacterium tuberculosis: Using transmission electron microscopy. Chemotherapy 2009, 55, 303–307. [Google Scholar] [CrossRef]
- Velayati, A.A.; Farnia, P.; Masjedi, M.R.; Ibrahim, T.A.; Tabarsi, P.; Haroun, R.Z.; Kuan, H.O.; Ghanavi, J.; Varahram, M. Totally drug-resistant tuberculosis strains: Evidence of adaptation at the cellular level. Eur. Respir. J. 2009, 34, 1202–1203. [Google Scholar] [CrossRef]
- Cox, J.S.; Chen, B.; McNeil, M.; Jacobs, W.R. Complex lipid determines tissue-specific replication of Mycobacterium tuberculosis in mice. Nature 1999, 402, 79–83. [Google Scholar] [CrossRef]
- Barry, C.E. Interpreting cell wall ‘virulence factors’ of Mycobacterium tuberculosis. Trends Microbiol. 2001, 9, 237–241. [Google Scholar] [CrossRef] [PubMed]
- Mendelson, M.; Walters, S.; Smith, I.; Kaplan, G. Strain-specific mycobacterial lipids and the stimulation of protective immunity to tuberculosis. Tuberculosis 2005, 85, 407–413. [Google Scholar] [CrossRef] [PubMed]
- Rocha-Ramírez, L.M.; Estrada-García, I.; López-Marín, L.M.; Segura-Salinas, E.; Méndez-Aragón, P.; van Soolingen, D.; Torres-González, R.; Chacón-Salinas, R.; Estrada-Parra, S.; Maldonado-Bernal, C.; et al. Mycobacterium tuberculosis lipids regulate cytokines, TLR-2/4 and MHC class II expression in human macrophages. Tuberculosis 2008, 88, 212–220. [Google Scholar] [CrossRef] [PubMed]
- Takayama, K.; Wang, L.; David, H.L. Effect of isoniazid on the in vivo mycolic acid synthesis, cell growth, and viability of Mycobacterium tuberculosis. Antimicrob. Agents Chemother. 1972, 2, 29–35. [Google Scholar] [CrossRef]
- Glickman, M.S.; Cox, J.S.; Jacobs, W.R. A novel mycolic acid cyclopropane synthetase is required for cording, persistence, and virulence of Mycobacterium tuberculosis. Mol. Cell 2000, 5, 717–727. [Google Scholar] [CrossRef]
- Goossens, S.N.; Sampson, S.L.; Van Rie, A. Mechanisms of drug-induced tolerance in Mycobacterium tuberculosis. Clin. Microbiol. Rev. 2020, 34, e00141-20. [Google Scholar] [CrossRef]
- Shui, W.; Gilmore, S.A.; Sheu, L.; Liu, J.; Keasling, J.D.; Bertozzi, C.R. Quantitative proteomic profiling of host−pathogen interactions: The macrophage response to Mycobacterium tuberculosis lipids. J. Proteome Res. 2009, 8, 282–289. [Google Scholar] [CrossRef]
- Nieto R, L.M.; Mehaffy, C.; Dobos, K.M. Comparing isogenic strains of Beijing genotype Mycobacterium tuberculosis after acquisition of isoniazid resistance: A proteomics approach. Proteomics 2016, 16, 1376–1380. [Google Scholar] [CrossRef]
- Nieto R, L.M.; Mehaffy, C.; Islam, M.N.; Fitzgerald, B.; Belisle, J.; Prenni, J.; Dobos, K. Biochemical characterization of isoniazid-resistant Mycobacterium tuberculosis: Can the analysis of clonal strains reveal novel targetable pathways? Mol. Cell. Proteom. 2018, 17, 1685–1701. [Google Scholar] [CrossRef]
- Telenti, A.; Imboden, P.; Marchesi, F.; Lowrie, D.; Cole, S.; Colston, M.J.; Matter, L.; Schopfer, K.; Bodmer, T. Detection of rifampicin-resistance mutations in Mycobacterium tuberculosis. Lancet 1993, 341, 647–650. [Google Scholar] [CrossRef]
- Chandra, P.; Grigsby, S.J.; Philips, J.A. Immune evasion and provocation by Mycobacterium tuberculosis. Nat. Rev. Microbiol. 2022, 20, 750–766. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.H.; Liu, H.; Ge, B. Innate immunity in tuberculosis: Host defense vs pathogen evasion. Cell. Mol. Immunol. 2017, 14, 963–975. [Google Scholar] [CrossRef] [PubMed]
- Zhai, W.; Wu, F.; Zhang, Y.; Fu, Y.; Liu, Z. The immune escape mechanisms of Mycobacterium tuberculosis. Int. J. Mol. Sci. 2019, 20, 340. [Google Scholar] [CrossRef]
- O’Garra, A.; Redford, P.S.; McNab, F.W.; Bloom, C.I.; Wilkinson, R.J.; Berry, M.P.R. The immune response in tuberculosis. Annu. Rev. Immunol. 2013, 31, 475–527. [Google Scholar] [CrossRef]
- BoseDasgupta, S.; Pieters, J. Macrophage-microbe interaction: Lessons learned from the pathogen Mycobacterium tuberculosis. Semin. Immunopathol. 2018, 40, 577–591. [Google Scholar] [CrossRef] [PubMed]
- Wassermann, R.; Gulen, M.F.; Sala, C.; Perin, S.G.; Lou, Y.; Rybniker, J.; Schmid-Burgk, J.L.; Schmidt, T.; Hornung, V.; Cole, S.T.; et al. Mycobacterium tuberculosis differentially activates cGAS- and inflammasome-dependent intracellular immune responses through ESX-1. Cell Host Microbe 2015, 17, 799–810. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.; Yang, J.; Zhang, Z.; Zhang, L.; Zhu, B.; Lie, L.; Huang, Y.; Ma, R.; Zhou, C.; Hu, S.; et al. Different signaling pathways define different interferon-stimulated gene expression during mycobacteria infection in macrophages. Int. J. Mol. Sci. 2019, 20, 663. [Google Scholar] [CrossRef]
- Correa-Macedo, W.; Cambri, G.; Schurr, E. The interplay of human and Mycobacterium tuberculosis genomic variability. Front. Genet. 2019, 10, 865. [Google Scholar] [CrossRef]
- Pattanaik, K.P.; Sengupta, S.; Jit, B.P.; Kotak, R.; Sonawane, A. Host-mycobacteria conflict: Immune responses of the host vs. the mycobacteria TLR2 and TLR4 ligands and concomitant host-directed therapy. Microbiol. Res. 2022, 264, 127153. [Google Scholar] [CrossRef]
- López, B.; Aguilar, D.; Orozco, H.; Burger, M.; Espitia, C.; Ritacco, V.; Barrera, L.; Kremer, K.; Hernandez-Pando, R.; Huygen, K.; et al. A marked difference in pathogenesis and immune response induced by different Mycobacterium tuberculosis genotypes. Clin. Exp. Immunol. 2003, 133, 30–37. [Google Scholar] [CrossRef]
- Caws, M.; Thwaites, G.; Dunstan, S.; Hawn, T.R.; Lan, N.T.N.; Thuong, N.T.T.; Stepniewska, K.; Huyen, M.N.T.; Bang, N.D.; Loc, T.H.; et al. The influence of host and bacterial genotype on the development of disseminated disease with Mycobacterium tuberculosis. PLoS Pathog. 2008, 4, e1000034. [Google Scholar] [CrossRef] [PubMed]
- Krishnan, N.; Malaga, W.; Constant, P.; Caws, M.; Tran, T.H.C.; Salmons, J.; Nguyen, T.N.L.; Nguyen, D.B.; Daffé, M.; Young, D.B.; et al. Mycobacterium tuberculosis lineage influences innate immune response and virulence and is associated with distinct cell envelope lipid profiles. PLoS ONE 2011, 6, e23870. [Google Scholar] [CrossRef] [PubMed]
- Parwati, I.; van Crevel, R.; van Soolingen, D. Possible underlying mechanisms for successful emergence of the Mycobacterium tuberculosis Beijing genotype strains. Lancet Infect. Dis. 2010, 10, 103–111. [Google Scholar] [CrossRef] [PubMed]
- Portevin, D.; Gagneux, S.; Comas, I.; Young, D. Human macrophage responses to clinical isolates from the Mycobacterium tuberculosis complex discriminate between ancient and modern lineages. PLoS Pathog. 2011, 7, e1001307. [Google Scholar] [CrossRef]
- Pandey, A.K.; Yang, Y.; Jiang, Z.; Fortune, S.M.; Coulombe, F.; Behr, M.A.; Fitzgerald, K.A.; Sassetti, C.M.; Kelliher, M.A. NOD2, RIP2 and IRF5 play a critical role in the type I interferon response to Mycobacterium tuberculosis. PLoS Pathog. 2009, 5, e1000500. [Google Scholar] [CrossRef]
- Watson, R.O.; Bell, S.L.; MacDuff, D.A.; Kimmey, J.M.; Diner, E.J.; Olivas, J.; Vance, R.E.; Stallings, C.L.; Virgin, H.W.; Cox, J.S. The cytosolic sensor cGAS detects Mycobacterium tuberculosis DNA to induce type I interferons and activate autophagy. Cell Host Microbe 2015, 17, 811–819. [Google Scholar] [CrossRef]
- Weindel, C.G.; Bell, S.L.; Vail, K.J.; West, K.O.; Patrick, K.L.; Watson, R.O. LRRK2 maintains mitochondrial homeostasis and regulates innate immune responses to Mycobacterium tuberculosis. eLife 2020, 9, e51071. [Google Scholar] [CrossRef]
- Vrieling, F.; Kostidis, S.; Spaink, H.P.; Haks, M.C.; Mayboroda, O.A.; Ottenhoff, T.H.M.; Joosten, S.A. Analyzing the impact of Mycobacterium tuberculosis infection on primary human macrophages by combined exploratory and targeted metabolomics. Sci. Rep. 2020, 10, 7085. [Google Scholar] [CrossRef]
- Lee, M.L.; Kuo, F.C.; Whitmore, G.A.; Sklar, J. Importance of replication in microarray gene expression studies: Statistical methods and evidence from repetitive cDNA hybridizations. Proc. Natl. Acad. Sci. USA 2000, 97, 9834–9839. [Google Scholar] [CrossRef]
- Ritchie, M.E.; Phipson, B.; Wu, D.; Hu, Y.; Law, C.W.; Shi, W.; Smyth, G.K. limma powers differential expression analyses for RNA-sequencing and microarray studies. Nucleic Acids Res. 2015, 43, e47. [Google Scholar] [CrossRef]
- Benjamini, Y.; Hochberg, Y. Controlling the false discovery rate: A practical and powerful approach to multiple testing. J. R. Stat. Soc. Ser. B Stat. Methodol. 1995, 57, 289–300. [Google Scholar] [CrossRef]
- Chen, H.; Boutros, P.C. VennDiagram: A package for the generation of highly-customizable Venn and Euler diagrams in R. BMC Bioinformatics 2011, 12, 35. [Google Scholar] [CrossRef] [PubMed]
- Shade, A.; Handelsman, J. Beyond the Venn diagram: The hunt for a core microbiome. Environ. Microbiol. 2012, 14, 4–12. [Google Scholar] [CrossRef] [PubMed]
- Huang, D.W.; Sherman, B.T.; Lempicki, R.A. Systematic and integrative analysis of large gene lists using DAVID bioinformatics resources. Nat. Protoc. 2009, 4, 44–57. [Google Scholar] [CrossRef]
- Sherman, B.T.; Hao, M.; Qiu, J.; Jiao, X.; Baseler, M.W.; Lane, H.C.; Imamichi, T.; Chang, W. DAVID: A web server for functional enrichment analysis and functional annotation of gene lists (2021 update). Nucleic Acids Res. 2022, 50, W216–W221. [Google Scholar] [CrossRef]
- Madhvi, A.; Mishra, H.; Leisching, G.R.; Mahlobo, P.Z.; Baker, B. Comparison of human monocyte derived macrophages and THP1-like macrophages as in vitro models for M. tuberculosis infection. Comp. Immunol. Microbiol. Infect. Dis. 2019, 67, 101355. [Google Scholar] [CrossRef]
- Shah, P.T.; Tufail, M.; Wu, C.; Xing, L. THP-1 cell line model for tuberculosis: A platform for in vitro macrophage manipulation. Tuberculosis 2022, 136, 102243. [Google Scholar] [CrossRef]
- Fontán, P.; Aris, V.; Ghanny, S.; Soteropoulos, P.; Smith, I. Global transcriptional profile of Mycobacterium tuberculosis during THP-1 human macrophage infection. Infect. Immun. 2008, 76, 717–725. [Google Scholar] [CrossRef]
- Pu, W.; Zhao, C.; Wazir, J.; Su, Z.; Niu, M.; Song, S.; Wei, L.; Li, L.; Zhang, X.; Shi, X.; et al. Comparative transcriptomic analysis of THP-1-derived macrophages infected with Mycobacterium tuberculosis H37Rv, H37Ra and BCG. J. Cell. Mol. Med. 2021, 25, 10504–10520. [Google Scholar] [CrossRef]
- Park, C.Y.; Krishnan, A.; Zhu, Q.; Wong, A.K.; Lee, Y.-S.; Troyanskaya, O.G. Tissue-aware data integration approach for the inference of pathway interactions in metazoan organisms. Bioinformatics 2015, 31, 1093–1101. [Google Scholar] [CrossRef]
- Steenken, W., Jr.; Gardner, L.U. History of H37 strain of tubercle bacillus. Am. Rev. Tuberc. 1946, 54, 62–66. [Google Scholar] [PubMed]
- Gautam, U.S.; Mehra, S.; Kaushal, D. In-Vivo gene signatures of Mycobacterium tuberculosis in C3HeB/FeJ mice. PLoS ONE 2015, 10, e0135208. [Google Scholar] [CrossRef] [PubMed]
- Simper, J.D.; Perez, E.; Schlesinger, L.S.; Azad, A.K. Resistance and susceptibility immune factors at play during Mycobacterium tuberculosis infection of macrophages. Pathogens 2022, 11, 1153. [Google Scholar] [CrossRef] [PubMed]
- Juffermans, N.P.; Florquin, S.; Camoglio, L.; Verbon, A.; Kolk, A.H.; Speelman, P.; van Deventer, S.J.; van Der Poll, T. Interleukin-1 signaling is essential for host defense during murine pulmonary tuberculosis. J. Infect. Dis. 2000, 182, 902–908. [Google Scholar] [CrossRef]
- Sugawara, I.; Yamada, H.; Hua, S.; Mizuno, S. Role of interleukin (IL)-1 type 1 receptor in mycobacterial infection. Microbiol. Immunol. 2001, 45, 743–750. [Google Scholar] [CrossRef]
- Fremond, C.M.; Togbe, D.; Doz, E.; Rose, S.; Vasseur, V.; Maillet, I.; Jacobs, M.; Ryffel, B.; Quesniaux, V.F.J. IL-1 receptor-mediated signal is an essential component of MyD88-dependent innate response to Mycobacterium tuberculosis infection. J. Immunol. 2007, 179, 1178–1189. [Google Scholar] [CrossRef]
- Lee, M.-R.; Chang, L.-Y.; Chang, C.-H.; Yan, B.-S.; Wang, J.-Y.; Lin, W.-H. Differed IL-1 beta response between active TB and LTBI cases by ex vivo stimulation of human monocyte-derived macrophage with TB-specific antigen. Dis. Markers 2019, 2019, 7869576. [Google Scholar] [CrossRef]
- Romagnoli, A.; Petruccioli, E.; Palucci, I.; Camassa, S.; Carata, E.; Petrone, L.; Mariano, S.; Sali, M.; Dini, L.; Girardi, E.; et al. Clinical isolates of the modern Mycobacterium tuberculosis lineage 4 evade host defense in human macrophages through eluding IL-1β-induced autophagy. Cell Death Dis. 2018, 9, 624. [Google Scholar] [CrossRef]
- Novikov, A.; Cardone, M.; Thompson, R.; Shenderov, K.; Kirschman, K.D.; Mayer-Barber, K.D.; Myers, T.G.; Rabin, R.L.; Trinchieri, G.; Sher, A.; et al. Mycobacterium tuberculosis triggers host type I IFN signaling to regulate IL-1β production in human macrophages. J. Immunol. 2011, 187, 2540–2547. [Google Scholar] [CrossRef]
- Mishra, A.; Akhtar, S.; Jagannath, C.; Khan, A. Pattern recognition receptors and coordinated cellular pathways involved in tuberculosis immunopathogenesis: Emerging concepts and perspectives. Mol. Immunol. 2017, 87, 240–248. [Google Scholar] [CrossRef]
- Cheung, B.K.W.; Lee, D.C.W.; Li, J.C.B.; Lau, Y.-L.; Lau, A.S.Y. A role for double-stranded RNA-activated protein kinase PKR in Mycobacterium-induced cytokine expression. J. Immunol. 2005, 175, 7218–7225. [Google Scholar] [CrossRef] [PubMed]
- Smyth, R.; Berton, S.; Rajabalee, N.; Chan, T.; Sun, J. Protein kinase R restricts the intracellular survival of Mycobacterium tuberculosis by promoting selective autophagy. Front. Microbiol. 2021, 11, 613963. [Google Scholar] [CrossRef] [PubMed]
- Deb, A.; Haque, S.J.; Mogensen, T.; Silverman, R.H.; Williams, B.R. RNA-dependent protein kinase PKR is required for activation of NF-kappa B by IFN-gamma in a STAT1-independent pathway. J. Immunol. 2001, 166, 6170–6180. [Google Scholar] [CrossRef] [PubMed]
- Deng, J.; Lu, P.D.; Zhang, Y.; Scheuner, D.; Kaufman, R.J.; Sonenberg, N.; Harding, H.P.; Ron, D. Translational repression mediates activation of nuclear factor kappa B by phosphorylated translation initiation factor 2. Mol. Cell. Biol. 2004, 24, 10161–10168. [Google Scholar] [CrossRef]
- Yu, H.; Peng, C.; Zhang, C.; Stoian, A.M.M.; Tazi, L.; Brennan, G.; Rothenburg, S. Maladaptation after a virus host switch leads to increased activation of the pro-inflammatory NF-κB pathway. Proc. Natl. Acad. Sci. USA 2022, 119, e2115354119. [Google Scholar] [CrossRef]
- Fallahi-Sichani, M.; Kirschner, D.E.; Linderman, J.J. NF-κB signaling dynamics play a key role in infection control in tuberculosis. Front. Physiol. 2012, 3, 170. [Google Scholar] [CrossRef]
- Bai, X.; Feldman, N.E.; Chmura, K.; Ovrutsky, A.R.; Su, W.-L.; Griffin, L.; Pyeon, D.; McGibney, M.T.; Strand, M.J.; Numata, M.; et al. Inhibition of nuclear factor-kappa B activation decreases survival of Mycobacterium tuberculosis in human macrophages. PLoS ONE 2013, 8, e61925. [Google Scholar] [CrossRef]
- Chakrabarti, A.; Banerjee, S.; Franchi, L.; Loo, Y.-M.; Gale, M.; Núñez, G.; Silverman, R.H. RNase L activates the NLRP3 inflammasome during viral infections. Cell Host Microbe 2015, 17, 466–477. [Google Scholar] [CrossRef]
- Banerjee, S. RNase L and the NLRP3-inflammasome: An old merchant in a new trade. Cytokine Growth Factor Rev. 2016, 29, 63–70. [Google Scholar] [CrossRef]
- Gusho, E.; Baskar, D.; Banerjee, S. New advances in our understanding of the “unique” RNase L in host pathogen interaction and immune signaling. Cytokine 2020, 133, 153847. [Google Scholar] [CrossRef]
- Jacobo-Delgado, Y.M.; Rodríguez-Carlos, A.; Serrano, C.J.; Rivas-Santiago, B. Mycobacterium tuberculosis cell-wall and antimicrobial peptides: A mission impossible? Front. Immunol. 2023, 14, 1194923. [Google Scholar] [CrossRef] [PubMed]
- Allué-Guardia, A.; García, J.I.; Torrelles, J.B. Evolution of drug-resistant Mycobacterium tuberculosis strains and their adaptation to the human lung environment. Front. Microbiol. 2021, 12, 612675. [Google Scholar] [CrossRef] [PubMed]
- Schami, A.; Islam, M.N.; Belisle, J.T.; Torrelles, J.B. Drug-resistant strains of Mycobacterium tuberculosis: Cell envelope profiles and interactions with the host. Front. Cell. Infect. Microbiol. 2023, 13, 1274175. [Google Scholar] [CrossRef] [PubMed]
- Ramaswamy, S.V.; Reich, R.; Dou, S.-J.; Jasperse, L.; Pan, X.; Wanger, A.; Quitugua, T.; Graviss, E.A. Single nucleotide polymorphisms in genes associated with isoniazid resistance in Mycobacterium tuberculosis. Antimicrob. Agents Chemother. 2003, 47, 1241–1250. [Google Scholar] [CrossRef]
- Hazbón, M.H.; Brimacombe, M.; del Valle, M.B.; Cavatore, M.; Guerrero, M.I.; Varma-Basil, M.; Billman-Jacobe, H.; Lavender, C.; Fyfe, J.; García-García, L.; et al. Population genetics study of isoniazid resistance mutations and evolution of multidrug-resistant Mycobacterium tuberculosis. Antimicrob. Agents Chemother. 2006, 50, 2640–2649. [Google Scholar] [CrossRef]
- Vilchèze, C.; Jacobs, W.R. The mechanism of isoniazid killing: Clarity through the scope of genetics. Annu. Rev. Microbiol. 2007, 61, 35–50. [Google Scholar] [CrossRef]
- Da Silva, P.E.A.; Palomino, J.C. Molecular basis and mechanisms of drug resistance in Mycobacterium tuberculosis: Classical and new drugs. J. Antimicrob. Chemother. 2011, 66, 1417–1430. [Google Scholar] [CrossRef]
- Sun, G.; Luo, T.; Yang, C.; Dong, X.; Li, J.; Zhu, Y.; Zheng, H.; Tian, W.; Wang, S.; Barry, C.E.; et al. Dynamic population changes in Mycobacterium tuberculosis during acquisition and fixation of drug resistance in patients. J. Infect. Dis. 2012, 206, 1724–1733. [Google Scholar] [CrossRef]
- Palomino, J.C.; Martin, A. Drug resistance mechanisms in Mycobacterium tuberculosis. Antibiotics 2014, 3, 317–340. [Google Scholar] [CrossRef]
- Cohen, K.A.; Abeel, T.; Manson McGuire, A.; Desjardins, C.A.; Munsamy, V.; Shea, T.P.; Walker, B.J.; Bantubani, N.; Almeida, D.V.; Alvarado, L.; et al. Evolution of extensively drug-resistant tuberculosis over four decades: Whole genome sequencing and dating analysis of Mycobacterium tuberculosis isolates from KwaZulu-Natal. PLoS Med. 2015, 12, e1001880. [Google Scholar] [CrossRef]
- Unissa, A.N.; Subbian, S.; Hanna, L.E.; Selvakumar, N. Overview on mechanisms of isoniazid action and resistance in Mycobacterium tuberculosis. Infect. Genet. Evol. 2016, 45, 474–492. [Google Scholar] [CrossRef] [PubMed]
- Dookie, N.; Rambaran, S.; Padayatchi, N.; Mahomed, S.; Naidoo, K. Evolution of drug resistance in Mycobacterium tuberculosis: A review on the molecular determinants of resistance and implications for personalized care. J. Antimicrob. Chemother. 2018, 73, 1138–1151. [Google Scholar] [CrossRef]
- Cohen, T.; Becerra, M.C.; Murray, M.B. Isoniazid resistance and the future of drug-resistant tuberculosis. Microb. Drug Resist. 2004, 10, 280–285. [Google Scholar] [CrossRef] [PubMed]
- Seifert, M.; Catanzaro, D.; Catanzaro, A.; Rodwell, T.C. Genetic mutations associated with isoniazid resistance in Mycobacterium tuberculosis: A systematic review. PLoS ONE 2015, 10, e0119628. [Google Scholar] [CrossRef] [PubMed]
- Valafar, S.J. Systematic review of mutations associated with isoniazid resistance points to continuing evolution and subsequent evasion of molecular detection, and potential for emergence of multidrug resistance in clinical strains of Mycobacterium tuberculosis. Antimicrob. Agents Chemother. 2021, 65, e02091-20. [Google Scholar] [CrossRef] [PubMed]
- Borrell, S.; Gagneux, S. Infectiousness, reproductive fitness and evolution of drug-resistant Mycobacterium tuberculosis. Int. J. Tuberc. Lung Dis. 2009, 13, 1456–1466. [Google Scholar] [PubMed]
- Ford, C.B.; Shah, R.R.; Maeda, M.K.; Gagneux, S.; Murray, M.B.; Cohen, T.; Johnston, J.C.; Gardy, J.; Lipsitch, M.; Fortune, S.M. Mycobacterium tuberculosis mutation rate estimates from different lineages predict substantial differences in the emergence of drug-resistant tuberculosis. Nat. Genet. 2013, 45, 784–790. [Google Scholar] [CrossRef]
- Izu, A.; Cohen, T.; Degruttola, V. Bayesian estimation of mixture models with prespecified elements to compare drug resistance in treatment-naïve and experienced tuberculosis cases. PLoS Comput. Biol. 2013, 9, e1002973. [Google Scholar] [CrossRef]
- Eldholm, V.; Monteserin, J.; Rieux, A.; Lopez, B.; Sobkowiak, B.; Ritacco, V.; Balloux, F. Four decades of transmission of a multidrug-resistant Mycobacterium tuberculosis outbreak strain. Nat. Commun. 2015, 6, 7119. [Google Scholar] [CrossRef]
- Manson, A.L.; Cohen, K.A.; Abeel, T.; Desjardins, C.A.; Armstrong, D.T.; Barry, C.E.; Brand, J.; TBResist Global Genome Consortium; Chapman, S.B.; Cho, S.-N.; et al. Genomic analysis of globally diverse Mycobacterium tuberculosis strains provides insights into the emergence and spread of multidrug resistance. Nat. Genet. 2017, 49, 395–402. [Google Scholar] [CrossRef]
- Stagg, H.R.; Lipman, M.C.; McHugh, T.D.; Jenkins, H.E. Isoniazid-resistant tuberculosis: A cause for concern? Int. J. Tuberc. Lung Dis. 2017, 21, 129–139. [Google Scholar] [CrossRef] [PubMed]
- Smith, C.M.; Baker, R.E.; Proulx, M.K.; Mishra, B.B.; Long, J.E.; Park, S.W.; Lee, H.-N.; Kiritsy, M.C.; Bellerose, M.M.; Olive, A.J.; et al. Host-pathogen genetic interactions underlie tuberculosis susceptibility in genetically diverse mice. eLife 2022, 11, e74419. [Google Scholar] [CrossRef] [PubMed]
- Zak, D.E.; Penn-Nicholson, A.; Scriba, T.J.; Thompson, E.; Suliman, S.; Amon, L.M.; Mahomed, H.; Erasmus, M.; Whatney, W.; Hussey, G.D.; et al. A blood RNA signature for tuberculosis disease risk: A prospective cohort study. Lancet 2016, 387, 2312–2322. [Google Scholar] [CrossRef] [PubMed]
- Warsinske, H.; Vashisht, R.; Khatri, P. Host-response-based gene signatures for tuberculosis diagnosis: A systematic comparison of 16 signatures. PLoS Med. 2019, 16, e1002786. [Google Scholar] [CrossRef]
- Mulenga, H.; Zauchenberger, C.-Z.; Bunyasi, E.W.; Mbandi, S.K.; Mendelsohn, S.C.; Kagina, B.; Penn-Nicholson, A.; Scriba, T.J.; Hatherill, M. Performance of diagnostic and predictive host blood transcriptomic signatures for tuberculosis disease: A systematic review and meta-analysis. PLoS ONE 2020, 15, e0237574. [Google Scholar] [CrossRef]
- Vargas, R.; Abbott, L.; Bower, D.; Frahm, N.; Shaffer, M.; Yu, W.-H. Gene signature discovery and systematic validation across diverse clinical cohorts for TB prognosis and response to treatment. PLoS Comput. Biol. 2023, 19, e1010770. [Google Scholar] [CrossRef]
- Madamarandawala, P.; Rajapakse, S.; Gunasena, B.; Madegedara, D.; Magana-Arachchi, D. A host blood transcriptional signature differentiates multi-drug/rifampin-resistant tuberculosis (MDR/RR-TB) from drug susceptible tuberculosis: A pilot study. Mol. Biol. Rep. 2023, 50, 3935–3943. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).