A Low-Cost, Integrated Immunization, Health, and Nutrition Intervention in Conflict Settings in Pakistan—The Impact on Zero-Dose Children and Polio Coverage
Abstract
1. Introduction
2. Materials and Methods
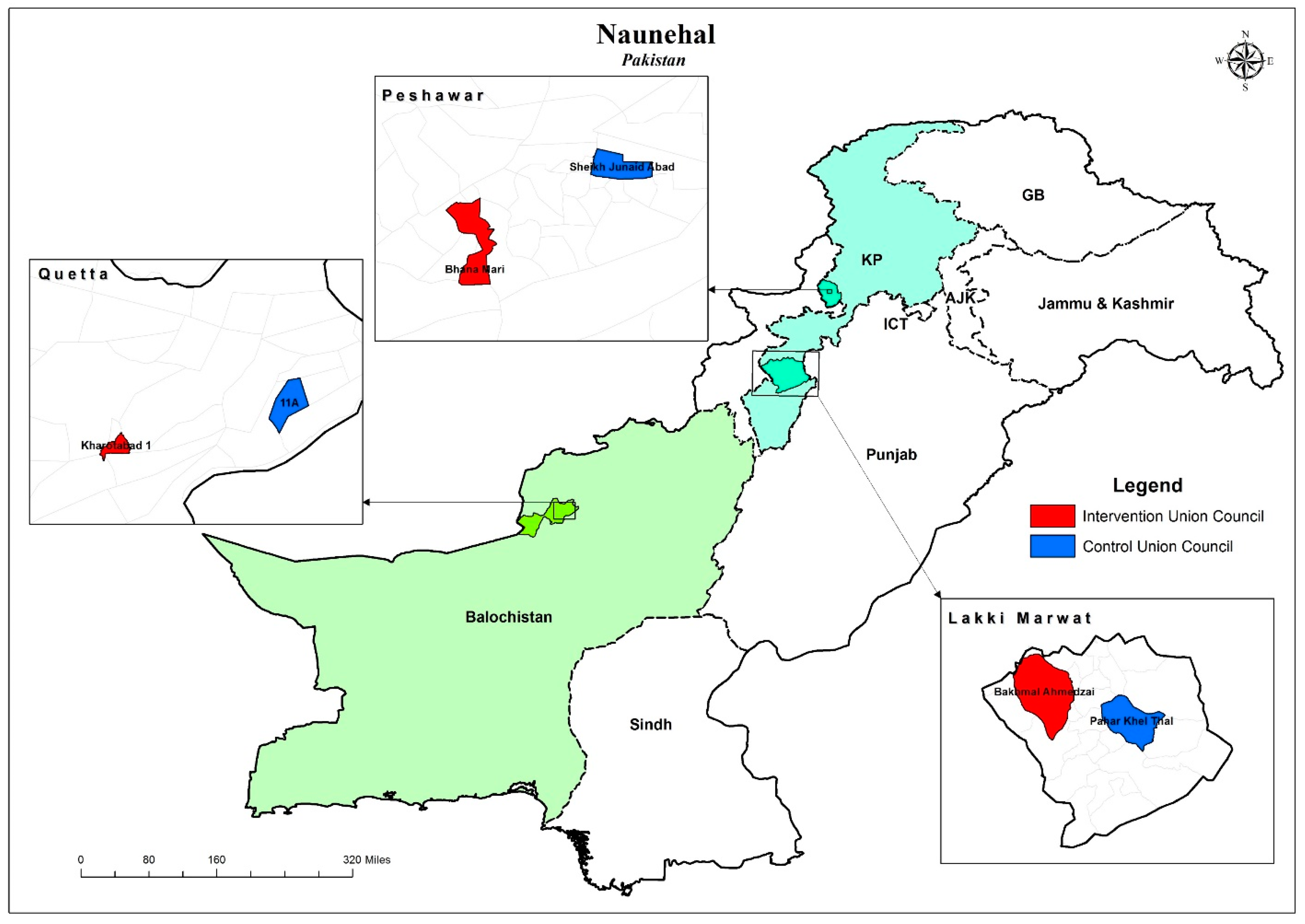
2.1. Study Setting
2.2. Study Design
2.3. Statistical Analysis
2.4. Outcomes
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mbaeyi, C.; Baig, S.; Safdar, R.M.; Khan, Z.; Young, H.; Jorba, J.; Wadood, Z.; Jafari, H.; Alam, M.M.; Franka, R. Progress toward Poliomyelitis Eradication—Pakistan, January 2022–June 2023. Morb. Mortal. Wkly. Rep. 2023, 72, 880–885. [Google Scholar] [CrossRef] [PubMed]
- Centre of Excellence in Women and Child Health—Aga Khan University & Federal Expanded Program on Immunization (EPI). Third-Party Verification Immunization Coverage Survey (TPVICS)—Survey Report; Aga Khan University: Karachi, Pakistan, 2022.
- United Nations Inter-Agency Group for Child Mortality Estimation (UN IGME). Levels & Trends in Child Mortality Report—Estimates Developed by the United Nations Inter-Agency Group for Child Mortality Estimation; United Nations Children’s Fund (UNICEF): New York, NY, USA, 2023; Available online: https://data.unicef.org/resources/levels-and-trends-in-child-mortality/ (accessed on 5 November 2023).
- United Nations Children’s Fund (UNICEF); World Health Organization (WHO); International Bank for Reconstruction and Development/The World Bank. Levels and Trends in Child Malnutrition: UNICEF/WHO/World Bank Group Joint Child Malnutrition Estimates: Key Findings of the 2023 Edition; UNICEF: New York, NY, USA; WHO: Geneva, Switzerland, 2023; Available online: https://www.who.int/publications/i/item/9789240073791 (accessed on 5 November 2023).
- Owais, A.; Rizvi, A.; Jawwad, M.; Horton, S.; Das, J.K.; Merritt, C.E.; Moreno, R.; Asfaw, A.G.; Rutter, P.; Nguyen, P.H.; et al. Assessing the hidden burden and costs of COVID-19 pandemic in South Asia: Implications for health and well-being of women, children and adolescents. PLoS Glob. Public Health 2023, 3, e0001567. [Google Scholar] [CrossRef] [PubMed]
- Habib, A.; Tabassum, F.; Hussain, I.; Khan, T.; Syed, N.; Shaheen, F.; Soofi, S.B.; Bhutta, Z.A. Exploring knowledge and perceptions of polio disease and its immunization in Polio High-Risk areas of Pakistan. Vaccines 2023, 11, 1206. [Google Scholar] [CrossRef] [PubMed]
- Ataullahjan, A.; Ahsan, H.; Soofi, S.B.; Habib, A.; Bhutta, Z.A. Eradicating polio in Pakistan: A systematic review of programs and policies. Expert Rev. Vaccines 2021, 20, 661–678. [Google Scholar] [CrossRef] [PubMed]
- Gul, A. WHO: Afghanistan, Pakistan Close to Eradicating Polio; Voice of America: New York, NY, USA, 2023; Available online: https://www.voanews.com/a/who-afghanistan-pakistan-close-to-eradicating-polio-/7205201.html (accessed on 7 December 2023).
- Global Polio Eradication Initiative; World Health Organization. Polio Endgame Strategy 2019–2023: Eradication, Integration, Certification, and Containment; Global Polio Eradication Initiative; World Health Organization: Geneva, Switzerland, 2017; Available online: https://reliefweb.int/report/world/polio-endgame-strategy-2019-2023-eradication-integration-certification-and-containment?gad_source=1&gclid=CjwKCAiAqY6tBhAtEiwAHeRopbRO0PX7b7WgKR48I2VosT4pv7jhPVmzdXZXCGM7rnZBnXdQylhBJhoCGowQAvD_BwE (accessed on 10 November 2023).
- Closser, S.; Jooma, R.; Varley, E.; Qayyum, N.; De Sousa Ferreira Guedes Rodrigues, S.; Sarwar, A.; Omidian, P.A. Polio eradication and health systems in Karachi: Vaccine refusals in context. Glob. Health Commun. 2015, 1, 32–40. [Google Scholar] [CrossRef]
- Das, J.K.; Khan, A.; Tabassum, F.; Padhani, Z.A.; Habib, A.; Mirani, M.; Rahman, A.R.; Khan, Z.; Rizvi, A.; Ahmed, I.; et al. The Last Mile—Community Engagement and conditional Incentives to Accelerate polio eradication in Pakistan: Study Protocol for a Quasi-Experimental Trial. Methods Protoc. 2023, 6, 83. [Google Scholar] [CrossRef]
- Kirmani, S.; Saleem, A.F. Impact of COVID-19 pandemic on paediatric services at a referral centre in Pakistan: Lessons from a low-income and middle-income country setting. Arch. Dis. Child. 2020, 106, 627–628. [Google Scholar] [CrossRef]
- Chandir, S.; Siddiqi, D.A.; Setayesh, H.; Khan, A. Impact of COVID-19 lockdown on routine immunisation in Karachi, Pakistan. Lancet Glob. Health 2020, 8, e1118–e1120. [Google Scholar] [CrossRef] [PubMed]
- Rahman, S.U.; Haq, F.U.; Imran, M.; Shah, A.; Bibi, N.; Khurshid, R.; Romman, M.; Gaffar, F.; Khan, M.I. Impact of the COVID-19 lockdown on routine vaccination in Pakistan: A hospital-based study. Hum. Vaccines Immunother. 2021, 17, 4934–4940. [Google Scholar] [CrossRef]
- Habib, A.; Soofi, S.B.; Cousens, S.; Anwar, S.; Haque, N.U.; Ahmed, I.; Ali, N.; Tahir, R.; Bhutta, Z.A. Community engagement and integrated health and polio immunisation campaigns in conflict-affected areas of Pakistan: A cluster randomised controlled trial. Lancet Glob. Health 2017, 5, e593–e603. [Google Scholar] [CrossRef] [PubMed]
- Habib, A.; Soofi, S.; Suhag, Z.; Ahmed, I.; Tahir, R.; Anwar, S.; Nauman, A.A.; Sharif, M.; Islam, M.; Cousens, S.; et al. A holistic strategy of Mother and Child Health Care to improve the coverage of Routine and Polio Immunization in Pakistan, Results from a Large Demonstration Project. Vaccines 2024, 12, 89. [Google Scholar] [CrossRef] [PubMed]
- Ataullahjan, A.; Khan, N.A.; Islam, M.B.; Tahir, R.; Anwar, S.; Ahmed, I.; Nauman, A.; Bhutta, Z.A. NAUNEHAL; Integrated immunization and MNCH interventions: A quasi-experimental study–Protocol. PLoS ONE 2023, 18, e0287722. [Google Scholar] [CrossRef] [PubMed]
- GPEI. GPEI-2023—Zero-Dose Children in Seven Subnational Consequential Geographies Hold Key to Success; Global Polio Eradication Initiative; World Health Organization: Geneva, Switzerland, 2023; Available online: https://polioeradication.org/news-post/2023-zero-dose-children-in-seven-subnational-most-consequential-geographies-hold-key-to-success (accessed on 22 December 2023).
- UNICEF. The State of the World’s Children 2023; UNICEF: New York, NY, USA, 2023; Available online: https://www.unicef.org/reports/state-worlds-children-2023#SOWC (accessed on 19 December 2023).
- Edmond, K.; Yousufi, K.; Naziri, M.; Higgins-Steele, A.; Qadir, A.; Sadat, S.M.; Bellows, A.L.; Smith, E.R. Mobile outreach health services for mothers and children in conflict-affected and remote areas: A population-based study from Afghanistan. Arch. Dis. Child. 2019, 105, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Hussain, R.; McGarvey, S.T.; Shahab, T.; Fruzzetti, L. Fatigue and Fear with Shifting Polio Eradication Strategies in India: A Study of Social Resistance to Vaccination. PLoS ONE 2012, 7, e46274. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Reducing Missed Opportunities for Vaccination (MOV). 2023. Available online: https://www.who.int/teams/immunization-vaccines-and-biologicals/essential-programme-on-immunization/implementation/reducing-missed-opportunities-for-vaccination (accessed on 29 November 2023).
- Centre of Excellence in Women and Child Health—The Aga Khan University & Biostat Global Consulting. 2022 Supplementary Immunization Coverage Survey in Super High Risk Union Councils of Pakistan (TPVICS-SHRUCs Round 2)—Survey Report; Aga Khan University: Karachi, Pakistan, 2023. [Google Scholar]
- Carrera, C.; Azrack, A.; Begkoyian, G.; Pfaffmann, J.; Ribaira, E.; O’Connell, T.; Doughty, P.; Aung, K.; Prieto, L.; Rasanathan, K.; et al. The comparative cost-effectiveness of an equity-focused approach to child survival, health, and nutrition: A modelling approach. Lancet 2012, 380, 1341–1351. [Google Scholar] [CrossRef] [PubMed]
- Crocker-Buqué, T.; Edelstein, M.; Mounier-Jack, S. Interventions to reduce inequalities in vaccine uptake in children and adolescents aged <19 years: A systematic review. J. Epidemiol. Community Health 2016, 71, 87–97. [Google Scholar] [CrossRef] [PubMed]
- Amsalu, R.; Firoz, T.; Lange, I.; Tappis, H. Editorial: Maternal Health in Conflict Settings. Front. Glob. Women’s Health 2022, 3, 807257. [Google Scholar] [CrossRef] [PubMed]
- Munyuzangabo, M.; Gaffey, M.F.; Khalifa, D.; Als, D.; Ataullahjan, A.; Kamali, M.; Jain, R.; Meteke, S.; Radhakrishnan, A.; Shah, S.; et al. Delivering maternal and neonatal health interventions in conflict settings: A systematic review. BMJ Glob. Health 2021, 5 (Suppl. 1), e003750. [Google Scholar] [CrossRef] [PubMed]
| Overall | Peshawar | Quetta | Lakki Marwat | |||||
|---|---|---|---|---|---|---|---|---|
| Control | Intervention | Control | Intervention | Control | Intervention | Control | Intervention | |
| Household Characteristics | N = 1277 | N = 1286 | N = 411 | N = 401 | N = 433 | N = 446 | N = 433 | N = 439 |
| Finished floor | 773 (69.4) | 696 (59.3) | 404 (97.6) | 390 (96.2) | 344 (79.0) | 253 (56.2) | 25 (5.9) | 53 (12.0) |
| Finished roof | 1139 (87.9) | 998 (76.2) | 411 (100.0) | 403 (99.2) | 373 (84.5) | 298 (63.0) | 355 (82.3) | 297 (65.7) |
| Finished walls | 831 (69.0) | 730 (59.7) | 409 (98.9) | 389 (96.1) | 325 (71.8) | 244 (52.1) | 97 (23.2) | 97 (20.9) |
| Solid fuel | 443 (20.6) | 464 (26.2) | 5 (1.9) | 14 (2.6) | 6 (1.6) | 11 (2.6) | 432 (99.7) | 439 (100.0) |
| Single room for sleeping | 231 (12.3) | 221 (13.9) | 47 (14.6) | 44 (10.0) | 9 (2.3) | 22 (5.3) | 175 (38.8) | 155 (33.9) |
| Improved source of drinking water | 1053 (69.6) | 972 (71.1) | 410 (99.8) | 406 (99.8) | 210 (46.1) | 141 (31.9) | 433 (100.0) | 425 (96.7) |
| Improved source of sanitation | 1208 (95.7) | 1147 (89.7) | 410 (99.8) | 406 (99.8) | 423 (96.9) | 392 (87.5) | 375 (87.4) | 349 (78.9) |
| Father’s Education | ||||||||
| No formal schooling | 350 (33.3) | 317 (28.8) | 106 (26.3) | 79 (24.2) | 179 (42.1) | 145 (35.5) | 65 (16.2) | 93 (24.0) |
| Primary | 306 (23.5) | 310 (24.0) | 16 (6.0) | 28 (5.9) | 107 (24.6) | 166 (37.2) | 183 (42.2) | 116 (27.6) |
| Secondary | 387 (27.5) | 389 (27.5) | 142 (35.0) | 158 (36.2) | 99 (22.4) | 96 (19.6) | 146 (33.0) | 135 (28.5) |
| Intermediate or above | 237 (15.8) | 278 (19.7) | 147 (32.7) | 142 (33.6) | 51 (10.9) | 41 (7.8) | 39 (8.6) | 95 (19.9) |
| Mother’s Education | ||||||||
| No formal schooling | 1091 (86.1) | 1109 (85.1) | 271 (65.1) | 285 (71.0) | 396 (91.0) | 406 (90.8) | 424 (98.3) | 418 (95.7) |
| Primary | 35 (3.9) | 58 (5.0) | 10 (2.8) | 17 (4.6) | 23 (5.6) | 29 (6.6) | 2 (0.4) | 12 (2.7) |
| Secondary | 71 (5.2) | 69 (5.5) | 55 (14.5) | 56 (13.0) | 14 (2.9) | 9 (1.9) | 2 (0.3) | 4 (0.8) |
| Intermediate or above | 83 (4.8) | 58 (4.4) | 75 (17.6) | 49 (11.4) | 3 (0.6) | 4 (0.7) | 5 (1.0) | 5 (0.8) |
| Wealth Index (Quintiles) | ||||||||
| Poorest | 223 (10.1) | 292 (16.8) | 0 (0.0) | 6 (1.1) | 1 (0.2) | 7 (1.6) | 222 (51.9) | 279 (64.8) |
| Poor | 253 (16.3) | 262 (19.5) | 6 (2.1) | 14 (2.6) | 58 (13.3) | 121 (28.8) | 189 (43.0) | 127 (27.8) |
| Middle | 218 (27.1) | 297 (26.1) | 17 (5.4) | 52 (14.5) | 181 (44.1) | 212 (46.8) | 20 (4.7) | 33 (7.4) |
| Rich | 260 (25.2) | 255 (22.4) | 120 (32.7) | 174 (44.1) | 139 (30.5) | 81 (17.4) | 1 (0.2) | 0 (0.0) |
| Richest | 326 (21.2) | 188 (15.2) | 268 (59.8) | 161 (37.6) | 57 (11.8) | 27 (5.4) | 1 (0.2) | 0 (0.0) |
| Children Under Five Years Old | N = 2175 | N = 2212 | N = 542 | N = 574 | N = 992 | N = 946 | N = 641 | N = 692 |
| Gender | ||||||||
| Male | 1133 (51.5) | 1124 (50.9) | 288 (52.4) | 273 (48.1) | 502 (50.9) | 498 (52.3) | 343 (53.4) | 353 (51.0) |
| Female | 1042 (48.5) | 1088 (49.1) | 254 (47.6) | 301 (51.9) | 490 (49.1) | 448 (47.7) | 298 (46.6) | 339 (49.0) |
| Age (Months) | ||||||||
| 0–5 | 178 (7.9) | 193 (8.2) | 52 (9.3) | 52 (8.3) | 76 (7.6) | 70 (7.2) | 50 (7.8) | 71 (10.2) |
| 6–11 | 187 (8.9) | 204 (10.0) | 61 (12.5) | 77 (14.1) | 80 (8.4) | 85 (9.5) | 46 (7.4) | 42 (5.8) |
| 12–23 | 405 (18.7) | 380 (17.2) | 115 (20.6) | 126 (21.0) | 181 (18.6) | 156 (16.6) | 109 (17.0) | 98 (13.7) |
| 24–59 | 1405 (64.4) | 1435 (64.7) | 314 (57.7) | 319 (56.5) | 655 (65.3) | 635 (66.8) | 436 (67.9) | 481 (70.3) |
| Overall | Bhana Mari | Bakhmal Ahmedzai | Kharotabad | |
|---|---|---|---|---|
| Mobile health camp days | 829 | 252 | 258 | 319 |
| Total beneficiaries | 30,768 | 7524 | 7225 | 16,019 |
| Women of a Reproductive Age (WRA) in camps | 10,572 (34.4%) | 1851 (24.6%) | 3039 (42.1%) | 5682 (35.5%) |
| Pregnant women in camps | 4416 (41.8%) | 661 (35.7%) | 824 (27.1%) | 2931 (51.6%) |
| Children under five years old at camps | 13,931 (45.3%) | 5550 (73.8%) | 4157 (57.5%) | 4224 (26.4%) |
| Children under 5 years old provided with routine immunization | 5193 (37.3%) | 962 (17.3%) | 3082 (74.1%) | 1149 (27.2%) |
| Children under 5 years old provided with an OPV | 7684 (55.2%) | 4310 (77.7%) | 1402 (33.7%) | 1972 (46.7%) |
| Total number of immunization doses administered | ||||
| BCG | 890 (6.4%) | 74 (1.3%) | 648 (15.6%) | 168 (4.0%) |
| OPV | 3721 (26.7%) | 532 (9.6%) | 2739 (65.9%) | 450 (10.7%) |
| Penta | 3541 (25.4%) | 471 (8.5%) | 2654 (63.8%) | 416 (9.8%) |
| PCV | 3526 (25.3%) | 466 (8.4%) | 2645 (63.6%) | 415 (9.8%) |
| IPV | 1344 (9.6%) | 211 (3.8%) | 1031 (24.8%) | 102 (2.4%) |
| Rota | 2554 (18.3%) | 293 (5.3%) | 1941 (46.7%) | 320 (7.6%) |
| Measles | 2501 (18.0%) | 421 (7.6%) | 1313 (31.6%) | 767 (18.2%) |
| Vaccine Refusals | ||||
| Routine immunization | 3 (0.0%) | 2 (0.0%) | 0 (0.0%) | 1 (0.0%) |
| OPV | 70 (0.5%) | 7 (0.1%) | 7 (0.2%) | 56 (1.3%) |
| Baseline | Endline | Control—% Diff (95% CI) | Intervention—% Diff (95% CI) | DID Estimate—% Diff (95% CI) | DID Estimate—p-Value | |||
|---|---|---|---|---|---|---|---|---|
| Control | Intervention | Control | Intervention | |||||
| N = 1122 | N = 1160 | N = 961 | N = 1000 | |||||
| Immunization Status | ||||||||
| Fully immunized | 210 (15.9) | 305 (27.5) | 282 (25.8) | 478 (51.0) | 9.9 (3.2, 16.6) | 23.6 (17.2, 29.9) | 13.6 (4.5, 22.8) | 0.0038 |
| Partially immunized | 463 (42.5) | 430 (40.6) | 393 (40.7) | 473 (45.6) | −1.8 (−9.2, 5.6) | 5.0 (−2.6, 12.6) | 6.8 (−3.7, 17.3) | 0.2039 |
| Non-recipients of routine immunizations | 449 (41.6) | 425 (31.9) | 286 (33.5) | 49 (3.4) | −8.1 (−18.3, 2.1) | −28.6 (−34.9, −22.2) | −20.4 (−32.4, −8.5) | 0.0009 |
| Zero dose | 447 (41.3) | 422 (31.6) | 47 (5.0) | 13 (0.9) | −36.3 (−43.6, −29.0) | −30.8 (−37.4, −24.1) | 5.5 (−4.3, 15.4) | 0.2676 |
| Ever had a vaccination card | 537 (44.5) | 640 (60.6) | 616 (57.3) | 912 (93.2) | 12.8 (2.2, 23.4) | 32.6 (25.6, 39.6) | 19.8 (7.2, 32.4) | 0.0022 |
| At Birth | ||||||||
| N = 1122 | N = 1160 | N = 961 | N = 1000 | |||||
| BCG | 665 (57.8) | 722 (66.9) | 664 (65.4) | 919 (92.9) | 7.6 (−2.8, 18.0) | 26.0 (19.4, 32.5) | 18.3 (6.1, 30.6) | 0.0034 |
| OPV0 | 631 (53.8) | 708 (65.6) | 576 (53.5) | 873 (89.0) | −0.4 (−11.2, 10.4) | 23.4 (16.7, 30.0) | 23.8 (11.1, 36.4) | 0.0003 |
| At 6 Weeks | ||||||||
| N = 1093 | N = 1134 | N = 942 | N = 980 | |||||
| OPV1 | 335 (26.6) | 456 (41.8) | 544 (50.9) | 799 (81.4) | 24.4 (14.5, 34.3) | 39.6 (32.4, 46.8) | 15.2 (3.1, 27.4) | 0.0141 |
| Penta 1 | 559 (47.2) | 557 (51.8) | 562 (52.1) | 850 (86.4) | 4.8 (−5.4, 15.0) | 34.6 (26.9, 42.4) | 29.8 (17.1, 42.5) | <0.0001 |
| PCV 1 | 538 (45.2) | 545 (50.5) | 563 (52.2) | 845 (85.9) | 7.0 (−3.2, 17.2) | 35.4 (27.5, 43.3) | 28.4 (15.6, 41.3) | <0.0001 |
| Rota Virus 1 | 531 (43.9) | 566 (52.8) | 558 (51.8) | 827 (83.7) | 7.8 (−2.3, 18.0) | 30.9 (23.0, 38.8) | 23.0 (10.3, 35.8) | 0.0005 |
| At 10 Weeks | ||||||||
| N = 1056 | N = 1111 | N = 909 | N = 956 | |||||
| OPV 2 | 259 (21.6) | 403 (38.7) | 378 (36.3) | 642 (69.2) | 14.7 (6.2, 23.2) | 30.5 (23.5, 37.6) | 15.9 (5.0, 26.8) | 0.0046 |
| Penta 2 | 295 (23.8) | 430 (40.8) | 491 (47.4) | 710 (74.7) | 23.6 (14.4, 32.8) | 33.9 (26.2, 41.7) | 10.3 (−1.6, 22.3) | 0.0891 |
| PCV 2 | 292 (23.6) | 425 (40.4) | 488 (47.2) | 703 (73.9) | 23.6 (14.5, 32.8) | 33.5 (25.7, 41.3) | 9.8 (−2.1, 21.8) | 0.1056 |
| Rota Virus 2 | 288 (23.3) | 412 (39.2) | 483 (46.6) | 700 (73.3) | 23.3 (14.2, 32.3) | 34.1 (26.5, 41.7) | 10.9 (−0.9, 22.6) | 0.0695 |
| At 14 Weeks | ||||||||
| N = 1024 | N = 1080 | N = 882 | N = 921 | |||||
| OPV 3 | 229 (19.7) | 343 (34.0) | 315 (30.3) | 563 (63.7) | 10.6 (2.6, 18.7) | 29.7 (22.8, 36.6) | 19.1 (8.5, 29.6) | 0.0004 |
| Penta 3 | 209 (18.1) | 338 (33.4) | 309 (30.3) | 530 (60.6) | 12.2 (4.0, 20.4) | 27.2 (19.9, 34.6) | 15.0 (4.1, 25.9) | 0.0071 |
| PCV 3 | 209 (18.1) | 330 (32.5) | 298 (29.3) | 527 (60.4) | 11.2 (3.2, 19.2) | 27.9 (20.8, 35.0) | 16.7 (6.1, 27.3) | 0.0022 |
| IPV 1 | 432 (36.3) | 460 (44.5) | 448 (44.4) | 654 (71.6) | 8.1 (−1.3, 17.5) | 27.1 (19.2, 34.9) | 19.0 (6.8, 31.2) | 0.0024 |
| At 9 Months | ||||||||
| N = 853 | N = 875 | N = 763 | N = 767 | |||||
| Measles 1 | 331 (32.4) | 397 (47.7) | 420 (47.5) | 591 (76.0) | 15.1 (5.9, 24.3) | 28.4 (20.9, 35.8) | 13.3 (1.5, 25.1) | 0.0269 |
| At 15 Months | ||||||||
| N = 639 | N = 662 | N = 598 | N = 565 | |||||
| Measles 2 | 164 (19.8) | 230 (35.1) | 247 (37.7) | 307 (54.6) | 17.9 (9.1, 26.7) | 19.5 (11.3, 27.6) | 1.6 (−10.3, 13.4) | 0.7963 |
| Baseline | Endline | Control—% Diff (95% CI) | Intervention—% Diff (95% CI) | DID Estimate—% Diff (95% CI) | DID Estimate—p-Value | |||
|---|---|---|---|---|---|---|---|---|
| Control | Intervention | Control | Intervention | |||||
| N = 789 | N = 810 | N = 597 | N = 700 | |||||
| Immunization Status | ||||||||
| Fully immunized | 74 (9.6) | 144 (20.2) | 60 (7.4) | 270 (43.2) | −2.1 (−6.0, 1.8) | 23.0 (15.8, 30.2) | 25.2 (17.1, 33.3) | <0.0001 |
| Partially immunized | 275 (38.7) | 250 (33.7) | 257 (42.7) | 384 (52.6) | 4.0 (−5.6, 13.6) | 18.9 (10.3, 27.4) | 14.8 (2.1, 27.5) | 0.0225 |
| Non-recipients of routine immunizations | 440 (51.8) | 416 (46.0) | 280 (49.9) | 46 (4.2) | −1.9 (−13.6, 9.8) | −41.9 (−49.8, −34.0) | −40.0 (−54.0, −26.0) | <0.0001 |
| Zero dose | 438 (51.4) | 416 (46.0) | 42 (6.8) | 12 (1.1) | −44.6 (−52.6, −36.5) | −45.0 (−53.3, −36.7) | −0.4 (−11.8, 11.0) | 0.9432 |
| Ever had a vaccination card | 258 (35.7) | 335 (47.1) | 265 (37.3) | 632 (93.2) | 1.6 (−9.4, 12.6) | 46.1 (37.8, 54.4) | 44.5 (30.9, 58.1) | <0.0001 |
| At Birth | ||||||||
| N = 789 | N = 810 | N = 597 | N = 700 | |||||
| BCG | 342 (47.6) | 390 (53.7) | 309 (48.9) | 622 (90.5) | 1.2 (−10.6, 13.1) | 36.8 (28.5, 45.2) | 35.6 (21.3, 49.9) | <0.0001 |
| OPV0 | 312 (42.8) | 369 (50.6) | 231 (32.0) | 590 (87.1) | −10.8 (−21.6, 0.0) | 36.5 (28.4, 44.5) | 47.2 (34.0, 60.5) | <0.0001 |
| At 6 Weeks | ||||||||
| N = 766 | N = 786 | N = 589 | N = 683 | |||||
| OPV1 | 152 (18.3) | 253 (34.8) | 226 (31.3) | 528 (77.8) | 13.0 (3.4, 22.7) | 43.0 (34.2, 51.7) | 29.9 (17.1, 42.8) | <0.0001 |
| Penta 1 | 258 (35.5) | 288 (40.1) | 243 (32.9) | 580 (85.1) | −2.6 (−13.1, 7.8) | 45.0 (35.4, 54.6) | 47.6 (33.6, 61.6) | <0.0001 |
| PCV 1 | 242 (33.2) | 281 (39.1) | 243 (32.9) | 578 (84.7) | −0.3 (−10.6, 10.0) | 45.6 (36.0, 55.3) | 45.9 (31.9, 59.9) | <0.0001 |
| Rota Virus 1 | 228 (31.2) | 277 (38.6) | 243 (32.9) | 565 (82.1) | 1.7 (−8.5, 11.9) | 43.5 (33.5, 53.5) | 41.8 (27.7, 55.9) | <0.0001 |
| At 10 Weeks | ||||||||
| N = 744 | N = 768 | N = 572 | N = 663 | |||||
| OPV 2 | 100 (13.8) | 218 (32.2) | 106 (14.4) | 393 (62.2) | 0.5 (−5.5, 6.5) | 30.0 (21.5, 38.5) | 29.5 (19.2, 39.8) | <0.0001 |
| Penta 2 | 129 (15.8) | 233 (33.8) | 210 (29.9) | 456 (69.6) | 14.1 (4.7, 23.5) | 35.8 (26.3, 45.3) | 21.7 (8.4, 35.0) | 0.0015 |
| PCV 2 | 126 (15.5) | 229 (33.4) | 208 (29.7) | 453 (69.0) | 14.2 (4.8, 23.6) | 35.6 (26.0, 45.1) | 21.4 (8.1, 34.6) | 0.0017 |
| Rota Virus 2 | 125 (15.5) | 225 (32.8) | 209 (29.8) | 449 (68.0) | 14.3 (4.9, 23.8) | 35.2 (25.6, 44.7) | 20.8 (7.6, 34.1) | 0.0023 |
| At 14 Weeks | ||||||||
| N = 723 | N = 743 | N = 559 | N = 637 | |||||
| OPV 3 | 84 (12.2) | 174 (27.1) | 80 (9.8) | 328 (55.1) | −2.3 (−7.4, 2.7) | 27.9 (19.3, 36.5) | 30.2 (20.4, 40.1) | <0.0001 |
| Penta 3 | 83 (12.1) | 174 (27.1) | 65 (8.6) | 298 (51.6) | −3.6 (−8.3, 1.2) | 24.4 (15.5, 33.4) | 28.0 (18.0, 38.0) | <0.0001 |
| PCV 3 | 83 (12.1) | 166 (25.8) | 65 (8.6) | 296 (51.4) | −3.5 (−8.3, 1.3) | 25.6 (17.0, 34.2) | 29.1 (19.4, 38.8) | <0.0001 |
| IPV 1 | 167 (22.8) | 223 (32.9) | 208 (30.0) | 440 (70.2) | 7.2 (−2.2, 16.7) | 37.3 (28.5, 46.1) | 30.0 (17.3, 42.8) | <0.0001 |
| At 9 Months | ||||||||
| N = 605 | N = 619 | N = 504 | N = 534 | |||||
| Measles 1 | 132 (20.7) | 206 (36.8) | 215 (34.0) | 408 (75.0) | 13.3 (3.9, 22.8) | 38.2 (29.7, 46.7) | 24.9 (12.2, 37.5) | 0.0001 |
| At 15 Months | ||||||||
| N = 437 | N = 458 | N = 403 | N = 388 | |||||
| Measles 2 | 51 (10.6) | 105 (25.1) | 108 (24.6) | 184 (47.9) | 14.0 (4.8, 23.2) | 22.8 (13.3, 32.3) | 8.8 (−4.3, 21.9) | 0.1862 |
| Overall | ||||
|---|---|---|---|---|
| Baseline | Endline | % Diff (95% CI) | p-Value | |
| N = 869 | N = 60 | |||
| Gender | ||||
| Male | 440 (49.4) | 29 (47.7) | −1.7 (−13.2, 9.7) | 0.7675 |
| Female | 429 (50.6) | 31 (52.3) | 1.7 (−9.7, 13.2) | 0.7675 |
| Maternal Education | ||||
| No formal schooling | 790 (88.5) | 58 (97.4) | 8.9 (3.5, 14.3) | 0.0015 |
| Primary | 55 (9.3) | 1 (0.7) | −8.6 (−12.1, −5.0) | <0.0001 |
| Secondary | 14 (1.4) | 0 (0.0) | ||
| Intermediate or above | 10 (0.8) | 1 (2.0) | 1.2 (−2.9, 5.2) | 0.5729 |
| Wealth Quintile | ||||
| Poorest | 285 (20.8) | 20 (23.5) | 2.7 (−14.2, 19.6) | 0.7508 |
| Poor | 256 (25.6) | 26 (44.0) | 18.4 (3.1, 33.6) | 0.0186 |
| Middle | 202 (33.1) | 8 (21.1) | −12.0 (−29.0, 5.0) | 0.1662 |
| Rich | 95 (15.9) | 4 (7.8) | −8.1 (−19.0, 2.8) | 0.1435 |
| Richest | 31 (4.6) | 2 (3.6) | −1.0 (−8.5, 6.5) | 0.7930 |
| Reason for Not Receiving Immunization | ||||
| Place of immunization too far | 95 (15.7) | 4 (7.1) | −8.5 (−16.9, −0.1) | 0.0462 |
| Inconvenient/unknown timing/long wait | 47 (6.0) | 4 (3.5) | −2.5 (−6.7, 1.8) | 0.2492 |
| Parent/caretaker busy | 58 (6.2) | 4 (8.2) | 2.0 (−9.1, 13.1) | 0.7231 |
| Child not well | 54 (7.1) | 2 (2.3) | −4.9 (−9.3, −0.5) | 0.0305 |
| Rumors | 127 (12.3) | 6 (9.2) | −3.1 (−13.3, 7.1) | 0.5452 |
| No faith in immunization | 141 (17.4) | 18 (31.2) | 13.9 (−3.9, 31.7) | 0.1256 |
| Fear of side effects | 205 (19.0) | 0 (0.0) | ||
| Vaccinator/vaccine not available | 69 (5.6) | 1 (3.4) | −2.2 (−9.5, 5.1) | 0.5477 |
| Others | 5 (0.9) | |||
| Do not know | 39 (6.7) | 4 (5.9) | −0.8 (−8.0, 6.3) | 0.8221 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khan, A.M.; Ahmed, I.; Jawwad, M.; Islam, M.; Tahir, R.; Anwar, S.; Nauman, A.A.; Bhutta, Z.A. A Low-Cost, Integrated Immunization, Health, and Nutrition Intervention in Conflict Settings in Pakistan—The Impact on Zero-Dose Children and Polio Coverage. Pathogens 2024, 13, 185. https://doi.org/10.3390/pathogens13030185
Khan AM, Ahmed I, Jawwad M, Islam M, Tahir R, Anwar S, Nauman AA, Bhutta ZA. A Low-Cost, Integrated Immunization, Health, and Nutrition Intervention in Conflict Settings in Pakistan—The Impact on Zero-Dose Children and Polio Coverage. Pathogens. 2024; 13(3):185. https://doi.org/10.3390/pathogens13030185
Chicago/Turabian StyleKhan, Amira M., Imran Ahmed, Muhammad Jawwad, Muhammad Islam, Rehman Tahir, Saeed Anwar, Ahmed Ali Nauman, and Zulfiqar A. Bhutta. 2024. "A Low-Cost, Integrated Immunization, Health, and Nutrition Intervention in Conflict Settings in Pakistan—The Impact on Zero-Dose Children and Polio Coverage" Pathogens 13, no. 3: 185. https://doi.org/10.3390/pathogens13030185
APA StyleKhan, A. M., Ahmed, I., Jawwad, M., Islam, M., Tahir, R., Anwar, S., Nauman, A. A., & Bhutta, Z. A. (2024). A Low-Cost, Integrated Immunization, Health, and Nutrition Intervention in Conflict Settings in Pakistan—The Impact on Zero-Dose Children and Polio Coverage. Pathogens, 13(3), 185. https://doi.org/10.3390/pathogens13030185





