Abstract
Patients with inborn errors of immunity (IEI) are prone to develop infections, either due to a broad spectrum of pathogens or to only one microbe. Since skin is a major barrier tissue, cutaneous infections are among the most prevalent in patients with IEI due to high exposures to many microbes. In the general population, human papillomaviruses (HPVs) cause asymptomatic or self-healing infections, but, in patients with IEI, unusual clinical expression of HPV infection is observed ranging from epidermodysplasia verruciformis (EV) (a rare disease due to β-HPVs) to profuse, persistent, and recalcitrant warts (due to α-, γ-, and μ-HPVs) or even tree man syndrome (due to HPV2). Mutations in EVER1, EVER2, and CIB1 are associated with EV phenotype; GATA2, CXCR4, and DOCK8 mutations are typically associated with extensive HPV infections, but there are several other IEI that are less frequently associated with severe HPV lesions. In this review, we describe clinical, immunological, and genetic patterns of IEI related to severe HPV cutaneous infections and propose an algorithm for diagnosis of IEI with severe warts associated, or not, with lymphopenia.
1. Introduction
Human papillomaviruses (HPVs) are DNA viruses with a specific tropism to keratinocytes, which are the main component of stratified epithelia, including skin, genital, and laryngeal mucosa. There are more than 200 different genotypes of HPVs classified in five (α-, β-, γ-, μ-, and ν-) genera. HPV subtypes of all genera infect the skin, and only some HPVs of α-genus infect the mucosal epithelia. Some α- and β-HPV types are oncogenic and are associated with benign genital condyloma, cervical and anogenital cancers, and non-melanoma skin cancers, respectively [1,2].
In the general population, HPVs cause asymptomatic or self-healing infections, with spontaneous clearances reported: 23% at 2 months and 66% by 2 years [3,4]. The transmission is from skin-to-skin or mucous-to-mucous contact. Seroprevalence is variable, depending on the HPV genus, age, and screening policy of each country. However, it is estimated to be <40% and 20–65% for oncogenic α-HPV and β-HPVs, respectively. Cervical cancer is the main clinical concern following HPV infection, as it is the fourth most frequent female cancer, with a death rate around 7.5%. In addition, more than 85% of deaths due to cervical cancer are in developing countries. The incidence of cutaneous warts varies with age, with a range from 1 to 12% in the adult general population, but could be over 24% in school age children [5].
Inborn errors of immunity (IEI) are characterized by an impaired immune response, affecting tissue-intrinsic immunity that is either, innate, adaptive, or both. IEI could be associated with higher susceptibility to infections, auto-inflammation, and/or autoimmunity. Unusual clinical expression of HPV infection is frequently observed in patients with IEI. The spectrum of the clinical phenotype is large from epidermodysplasis verruciformis (EV) (a rare disease due to β-HPV) to profuse, persistent and recalcitrant warts (due to α-, γ-, and μ-genera) [6]. Very rare individuals develop tree man syndrome (TMS) due to HPV2 [7].
There are some published reviews and case reports that describe clinical, immunological, and genetic patterns of IEI related to severe HPV cutaneous infections, but there are too many aspects of these issues that are still unknown and are being discovered continuously. Here, we present an up-to-date review of the major clinical, immunological, and genetic patterns of IEI related to severe HPV cutaneous infections, and we propose an algorithm for diagnosis of IEI with severe warts in order to help clinicians who may encounter patients with recurrent and recalcitrant warts due to an underlying inherited immunodeficiency.
2. Clinical Phenotypes
Depending on the HPV genera, there are different characteristics of HPV skin lesions. Macroscopy and histology analyses could help with an appropriate diagnosis.
2.1. Epidermodysplasia Verruciformis
With less than 250 cases reported worldwide, epidermodysplasia verruciformis (EV) is a rare disease that appears at young ages: infancy (7.5% of cases), childhood (61.5% of cases), and adolescence (22% of cases). Lesions are characterized by progressive onset hyperpigmented or achromic flat verrucous lesions, irregular patches of a reddish-brown color, keratotic seborrheic lesions, and pityriasis versicolor-like macules. The lesions are found mainly on sun-exposed areas, such as the face, trunk, neck, forearms, hands, and feet (Figure 1). Although various genotypes of β-HPVs are detected in EV lesions, HPV5 and -8 are found in 80% of cases. Histologic features of an EV lesion are characterized by a flat wart and showing mild to moderate hyperkeratosis, hypergranulosis, and acanthosis of the epidermis. The keratinocytes in the upper layer of the epidermis are enlarged and exhibit a vacuolated nucleus and a pale blue-gray color [8].

Figure 1.
Epidermodysplasia verruciformis lesions initially localized on the face, and then generalized to the neck and the trunk in a 12-year-old male patient with STK4 deficiency.
EV can be isolated (typical EV) or syndromic (atypical EV) associated with other clinical manifestations, infectious, or not. [9]. Among 40–50-year-old patients, 30 to 60% of EV patients develop non-melanoma skin cancer, particularly squamous cell carcinoma, occurring in sun-exposed areas. People with black skin have a much lower incidence of skin cancer. Most squamous cell carcinomas remain localized. Metastases are not frequent [8,10].
2.2. Profuse Warts (PWs)
Profuse warts (PWs) are defined as more than 20 lesions in more than one area of the body. If they do not disappear after 6 months of treatment, they are also classified as recalcitrant [11]. PW cauliflower-like papules have a rough, hyperkeratotic surface but they can be flat depending on the HPV involved (Figure 2). PWs are the consequence of an infection with α- or γ-HPV, and less frequently with μ- and ν-HPVs [12]. Histologic analyses of PWs have shown markedly papillomatous epidermis with hypergranulomatosis and overlying tiers of parakeratosis. The upper epidermis may contain large pink inclusions, particularly in cases arising on acral skin. Other lesions have shown smaller basophilic granules. Classically, in the upper epidermis, koilocytes or vacuolated keratinocytes which have a small shrunken nucleus surrounded by a perinuclear halos are observed [13].

Figure 2.
Profuse cauliflower and flat warts in a 26-year-old female patient with GATA2 deficiency (DCML syndrome).
2.3. Tree Man Syndrome
In exceptional cases, the warts can also transform into exophytic cutaneous lesions and giant horns, resulting in tree man syndrome [7]. TMS presents with the most extensive warts developing into cutaneous horns, which can be giant and generalized. These lesions start as cutaneous warts, slowly spreading over the hands and feet before transforming into cutaneous horns, characteristic of the TMS phenotype (Figure 3). This condition is extremely rare, with less than 10 cases reported so far. All cases were sporadic with no family history. Due to the paucity of reported cases, it is unclear whether these lesions in TMS have malignant potential [7].

Figure 3.
Tree man syndrome giant horns from an HPV2-driven multifocal benign epithelial tumor overexpressing viral oncogenes in the epidermis basal layer in a 30-year-old male patient with CD28 deficiency [7].
3. Immunological Phenotypes and Inborn Errors of Immunity
3.1. No immunological Phenotype in Blood (Skin-Intrinsic Immunity Disorder)
Isolated EV is due to autosomal recessive (AR) mutations in TMC6 and TMC8, which encode EVER1 and EVER2, two endoplasmic reticulum plasma membrane proteins, respectively, and in CIB1, which encodes calcium and integrin binding protein [9,14] (Table 1). Patients with isolated EV did not show any major leukocyte abnormalities, neither quantitative nor qualitative, in terms of proliferation or antibodies production. The HPV proteins, E5 and E8, targeted the EVER1–EVER2–CIB1 complex, strongly suggesting that this complex is acting as a restriction factor to HPVs in keratinocytes. In terms of the physiological mechanism, the dominant hypothesis is that isolated EV is the consequence of IEI affecting the keratinocyte-intrinsic immune response [14].

Table 1.
Etiologies and immunological phenotypes of isolated EV.
3.2. Immunological Phenotype with Qualitative or/and Quantitative T Cells Defects Only
In contrast to isolated EV, syndromic EV is related to IEI affecting T cells. Some of these IEI are also associated with PW phenotype. For some of them, warts are a major clinical symptom (Table 2) [6]. For instance, in AR DOCK8 deficiency, warts were reported in >40% of patients that were characterized by T and NK cell lymphopenia, and some patients developed α-HPV-induced malignancies [15]. Furthermore, AR mutations in the serine/threonine kinase 4 (STK4) gene are primarily characterized by a reduced amount and survival of circulating naïve T cells. Progressive CD4 T cell lymphopenia with profoundly low naïve CD4 T cell counts is hallmark, while CD8 T cells and NK cells are within normal range. T cell proliferation responses to both antigens and mitogens are markedly impaired. B cell counts are mildly low with hypergammaglobulinemia of IgG and variable increases in IgA and IgE [16].

Table 2.
Etiologies, clinical phenotypes, and immunological phenotypes of warts associated with IEI with qualitative or/and quantitative T cell defects.
More recently, patients with CARMIL2 and CD28 deficiencies were associated with HPV susceptibility [7,17]. These IEI both affect the CD28 signaling pathway, which is the major costimulatory pathway of TCR. Patients with CARMIL2 deficiency developed disseminated warts among other infectious manifestations, and they also had decreased memory B cells [17], whereas CD28 deficiency was associated with PW only. Interestingly, one of the CD28 patients developed TMS [7].
3.3. Immunological Phenotype with Several Impaired Leukocyte Subsets
This category includes warts, hypogammaglobulinemia, infections, myelokathexis (WHIM) syndrome, and classical CID and SCID syndromes (Table 3). The warts are also due to α-HPV and the immunological phenotypes of these diseases are variable but qualitative or/and quantitative T cell defects are common to all of them [24]. For example, in WHIM syndrome, between 60 and 80% of patients develop warts after α-HPV infection, and about 16% of these patients develop HPV-related cancers. This disease is associated with mutations in the CXCR4 gene, encoding a chemokine receptor. The immunological phenotype is characterized by neutropenia, low counts of dendritic cells (DC), memory B cells, and naïve CD4+ and CD8+ T cells [26]. In GATA2 haploinsufficiency, α-HPV infections occur in more than 50% of the cases, and genital cancers are frequent. Low monocyte, DC, B cell, CD4+ T cell, and NK cell counts are the most common immunological features of the patients [18,24].

Table 3.
Etiologies, clinical phenotypes, and immunological phenotypes of warts associated with several impaired leukocyte subsets.
4. Warts and IEI: Diagnostic Strategy
When an HPV-related clinical manifestation is severe, meaning profuse, chronic or recalcitrant and resistant to treatment, an IEI should be suspected especially if there are other infections, atopy, autoimmunity, or malignancy. Together with familial and patient history and physical examination, a guided differential diagnosis hypothesis should be formulated. Afterwards, focused laboratory testing should be investigated starting with immunoglobulin levels, T cell counts, and T cell subpopulation counts [29]. In Figure 4, we propose an algorithm for laboratory testing orientation for diagnosis of IEI related to HPV susceptibility, with or without impaired leukocyte populations.
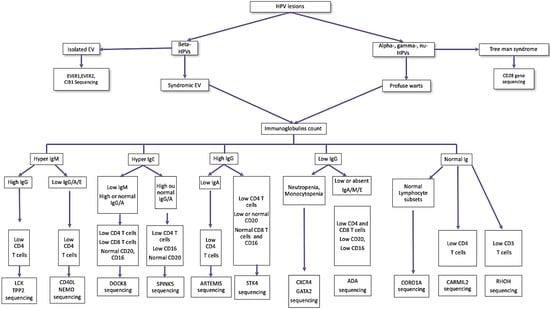
Figure 4.
Algorithm for laboratory testing orientation to diagnosis IEI with severe warts and lymphopenia. DOCK8, dedicator of cytokinesis 8; EV, epidermodysplasia verruciformis; ADA, adenosine desaminase severe combined immunodeficiency; NEMO, nuclear factor κB essential modulator deficiency; TPP2, tripeptidyl peptidase 2; LCK, lymphocyte-specific protein tyrosine kinase; SPINK5, serine peptidase inhibitor Kazal type 5; STK4, serine/threonine kinase 4; CXCR4, C-X-C motif chemokine receptor 4; CORO1A, coronin 1A, CARMIL2, capping protein regulator and myosin 1 linker 2, RHOH, Ras homolog family member H.
5. Conclusions
HPV skin lesions are a common symptom during infancy to childhood. Although recalcitrant warts, or even EV, are a rare clinical manifestation, physicians, including dermatologists and pediatricians, should consider IEI for a patient with recurrent or disseminated HPV skin lesions. The diagnosis strategy is crucial for a prompt and appropriate treatment of those patients. Furthermore, investigations of patients with EV or PW will increase our understanding of skin-intrinsic host immunity against HPVs.
Author Contributions
Conceptualization, A.E.K.; writing—original draft preparation, A.E.K.; writing—review and editing, F.A., J.E.B., K.Z., V.B., E.J., J.-L.C. and A.A.B.; supervision, J.-L.C. and A.A.B. All authors have read and agreed to the published version of the manuscript.
Funding
The Laboratory of Human Genetics of Infectious Diseases is supported by the Howard Hughes Medical Institute, the Rockefeller University, the St. Giles Foundation, the National Institutes of Health (NIH) (R01AI143810), the National Center for Advancing Translational Sciences (NCATS), the NIH Clinical and Translational Science Awards (CTSA) program (UL1TR001866), the French National Research Agency (ANR) under the “Investments for the Future” program (ANR-10-IAHU-01), the Integrative Biology of Emerging Infectious Diseases Laboratory of Excellence (ANR-10-LABX-62-IBEID), the French Foundation for Medical Research (FRM) (EQU201903007798), ANR CARMIL2 (ANR-21-CE15-0034), ITMO Cancer of Aviesan and INCa within the framework of the 2021–2030 Cancer Control Strategy (on funds administered by Inserm), the French national reference center for primary immunodeficiencies (CEREDIH), the French Society of Dermatology, the Square Foundation, Grandir-Fonds de solidarité pour l’Enfance, Institut National de la Santé et de la Recherche Médicale (INSERM), and the University of Paris Cité.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors have no conflict of interest to declare.
References
- Bernard, H.-U.; Burk, R.D.; Chen, Z.; van Doorslaer, K.; zur Hausen, H.; de Villiers, E.-M. Classification of Papillomaviruses (PVs) Based on 189 PV Types and Proposal of Taxonomic Amendments. Virology 2010, 401, 70–79. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- PaVE: Papilloma Virus Genome Database. Available online: https://pave.niaid.nih.gov/#home (accessed on 22 October 2021).
- Massing, A.M.; Epstein, W.L. Natural History of Warts. A Two-Year Study. Arch. Dermatol. 1963, 87, 306–310. [Google Scholar] [CrossRef]
- Kainz, J.T.; Kozel, G.; Haidvogl, M.; Smolle, J. Homoeopathic versus Placebo Therapy of Children with Warts on the Hands: A Randomized, Double-Blind Clinical Trial. Dermatology 1996, 193, 318–320. [Google Scholar] [CrossRef]
- Loo, S.K.; Tang, W.Y. Warts (Non-Genital). BMJ Clin. Evid. 2009, 2009, 1710. [Google Scholar] [PubMed]
- Béziat, V. Human genetic dissection of papillomavirus-driven diseases: New insight into their pathogenesis. Hum. Genet. 2020, 139, 919–939. [Google Scholar] [CrossRef] [PubMed]
- Béziat, V.; Rapaport, F.; Hu, J.; Titeux, M.; Bonnet des Claustres, M.; Bourgey, M.; Griffin, H.; Bandet, É.; Ma, C.S.; Sherkat, R.; et al. Humans with Inherited T Cell CD28 Deficiency Are Susceptible to Skin Papillomaviruses but Are Otherwise Healthy. Cell 2021, 184, 3812–3828.e30. [Google Scholar] [CrossRef] [PubMed]
- Zambruno, G. Epidermodysplasie Verruciforme, Orpha.Net. Available online: https://www.orpha.net/consor/cgi-bin/Disease_Search.php?lng=FR&data_id=8531&MISSING%20CONTENT=Epidermodisplasia-verruciforme&search=Disease_Search_Simple&title=Epidermodisplasia-verruciforme (accessed on 11 July 2022).
- de Jong, S.J.; Imahorn, E.; Itin, P.; Uitto, J.; Orth, G.; Jouanguy, E.; Casanova, J.-L.; Burger, B. Epidermodysplasia Verruciformis: Inborn Errors of Immunity to Human Beta-Papillomaviruses. Front. Microbiol. 2018, 9, 1222. [Google Scholar] [CrossRef]
- Orth, G. Génétique et Sensibilité Aux Papillomavirus: Le Modèle de l’épidermodysplasie Verruciforme. Bull. Acad. Natl. Méd. 2010, 194, 923–941. [Google Scholar] [CrossRef]
- Leung, L. Recalcitrant Nongenital Warts. Aust. Fam. Physician 2011, 40, 40–42. [Google Scholar] [PubMed]
- Uitto, J.; Saeidian, A.H.; Youssefian, L.; Saffarian, Z.; Casanova, J.-L.; Béziat, V.; Jouanguy, E.; Vahidnezhad, H. Recalcitrant Warts, Epidermodysplasia Verruciformis, and the Tree-Man Syndrome: Phenotypic Spectrum of Cutaneous Human Papillomavirus Infections at the Intersection of Genetic Variability of Viral and Human Genomes. J. Invest. Dermatol. 2022, 142, 1265–1269. [Google Scholar] [CrossRef]
- Emanuel, P. Verruca Vulgaris Pathology. Available online: https://dermnetnz.org/topics/verruca-vulgaris-pathology (accessed on 11 June 2022).
- de Jong, S.J.; Créquer, A.; Matos, I.; Hum, D.; Gunasekharan, V.; Lorenzo, L.; Jabot-Hanin, F.; Imahorn, E.; Arias, A.A.; Vahidnezhad, H.; et al. The Human CIB1–EVER1–EVER2 Complex Governs Keratinocyte-Intrinsic Immunity to β-Papillomaviruses. J. Exp. Med. 2018, 215, 2289–2310. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aydin, S.E.; Kilic, S.S.; Aytekin, C.; Kumar, A.; Porras, O.; Kainulainen, L.; Kostyuchenko, L.; Genel, F.; Kütükcüler, N.; Karaca, N.; et al. DOCK8 Deficiency: Clinical and Immunological Phenotype and Treatment Options—A Review of 136 Patients. J. Clin. Immunol. 2015, 35, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Abdollahpour, H.; Appaswamy, G.; Kotlarz, D.; Diestelhorst, J.; Beier, R.; Schäffer, A.A.; Gertz, E.M.; Schambach, A.; Kreipe, H.H.; Pfeifer, D.; et al. The phenotype of human STK4 deficiency. Blood 2012, 119, 3450–3457. [Google Scholar] [CrossRef] [PubMed]
- Alazami, A.M.; Al-Helale, M.; Alhissi, S.; Al-Saud, B.; Alajlan, H.; Monies, D.; Shah, Z.; Abouelhoda, M.; Arnaout, R.; Al-Dhekri, H.; et al. Novel CARMIL2 Mutations in Patients with Variable Clinical Dermatitis, Infections, and Combined Immunodeficiency. Front. Immunol. 2018, 9, 203. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bousfiha, A.; Jeddane, L.; Picard, C.; Al-Herz, W.; Ailal, F.; Chatila, T.; Cunningham-Rundles, C.; Etzioni, A.; Franco, J.L.; Holland, S.M.; et al. Human Inborn Errors of Immunity: 2019 Update of the IUIS Phenotypical Classification. J. Clin. Immunol. 2020, 40, 66–81. [Google Scholar] [CrossRef] [Green Version]
- Crequer, A.; Troeger, A.; Patin, E.; Ma, C.S.; Picard, C.; Pedergnana, V.; Fieschi, C.; Lim, A.; Abhyankar, A.; Gineau, L.; et al. Human RHOH Deficiency Causes T Cell Defects and Susceptibility to EV-HPV Infections. J. Clin. Invest. 2012, 122, 3239–3247. [Google Scholar] [CrossRef]
- OMIM—Online Mendelian Inheritance in Man. Available online: https://www.omim.org/ (accessed on 20 October 2021).
- Crequer, A.; Picard, C.; Patin, E.; D’Amico, A.; Abhyankar, A.; Munzer, M.; Debré, M.; Zhang, S.-Y.; de Saint-Basile, G.; Fischer, A.; et al. Inherited MST1 Deficiency Underlies Susceptibility to EV-HPV Infections. PLoS ONE 2012, 7, e44010. [Google Scholar] [CrossRef] [PubMed]
- Guerouaz, N.; Ismaili, N.; Bousfiha, M.A.; Ailal, F.; Picard, C.; Hassam, B.; Senouci, K. Le déficit en DOCK8 (dedicator of cytokinesis 8 gene): À propos d’un nouveau cas. Ann Dermatol Venerol. Ann. Dermatol. Vénéreol. 2014, 141, S502–S503. Available online: https://www.sciencedirect.com/science/article/pii/B9780123742797140238 (accessed on 20 October 2021). [CrossRef]
- Yee, C.S.; Massaad, M.J.; Bainter, W.; Ohsumi, T.K.; Föger, N.; Chan, A.C.; Akarsu, N.A.; Aytekin, C.; Ayvaz, D.Ç.; Tezcan, I.; et al. Recurrent Viral Infections Associated with a Homozygous CORO1A Mutation That Disrupts Oligomerization and Cytoskeletal Association. J. Allergy Clin. Immunol. 2016, 137, 879–888.e2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Béziat, V.; Jouanguy, E. Human inborn errors of immunity to oncogenic viruses. Curr. Opin. Immunol. 2021, 72, 277–285. [Google Scholar] [CrossRef]
- Wang, Y.; Ma, C.S.; Ling, Y.; Bousfiha, A.; Camcioglu, Y.; Jacquot, S.; Payne, K.; Crestani, E.; Roncagalli, R.; Belkadi, A.; et al. Dual T Cell- and B Cell-Intrinsic Deficiency in Humans with Biallelic RLTPR Mutations. J. Exp. Med. 2016, 213, 2413–2435. [Google Scholar] [CrossRef] [PubMed]
- Dotta, L.; Notarangelo, L.D.; Moratto, D.; Kumar, R.; Porta, F.; Soresina, A.; Lougaris, V.; Plebani, A.; Smith, C.E.; Norlin, A.C.; et al. Long-Term Outcome of WHIM Syndrome in 18 Patients: High Risk of Lung Disease and HPV-Related Malignancies. J. Allergy Clin. Immunol. Pract. 2019, 7, 1568–1577. [Google Scholar] [CrossRef] [Green Version]
- Volk, T.; Pannicke, U.; Reisli, I.; Bulashevska, A.; Ritter, J.; Björkman, A.; Schäffer, A.A.; Fliegauf, M.; Sayar, E.H.; Salzer, U.; et al. DCLRE1C (ARTEMIS) Mutations Causing Phenotypes Ranging from Atypical Severe Combined Immunodeficiency to Mere Antibody Deficiency. Hum. Mol. Genet. 2015, 24, 7361–7372. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eränkö, E.; Ilander, M.; Tuomiranta, M.; Mäkitie, A.; Lassila, T.; Kreutzman, A.; Klemetti, P.; Mustjoki, S.; Hannula-Jouppi, K.; Ranki, A. Immune Cell Phenotype and Functional Defects in Netherton Syndrome. Orphanet J. Rare Dis. 2018, 13, 213. [Google Scholar] [CrossRef] [PubMed]
- Leiding, J.W.; Holland, S.M. Warts and All: HPV in Primary Immunodeficiencies. J. Allergy Clin. Immunol. 2012, 130, 1030–1048. [Google Scholar] [CrossRef] [PubMed] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).