Abstract
Introduction: Interventional radiotherapy (brachytherapy, IRT, BT) has evolved with technological advancements, improving dose precision while minimizing exposure to healthy tissues. The integration of 3D-printing technology in IRT has enabled the development of patient-specific devices, optimizing treatment personalization and dosimetric accuracy. Methods: A systematic literature search was conducted in PubMed, Scopus, and Google Scholar to identify studies published between 2020 and 2024 on 3D-printing applications in IRT. The selection process resulted in 74 peer-reviewed articles categorized by radioactive source, brachytherapy technique, endpoint of the 3D-printed product, and study type. Results: The analysis highlights the growing implementation of 3D-printed devices in brachytherapy, particularly in gynecological, prostate, and skin cancers. Most studies focus on technique, including intracavitary, interstitial, and contact applications, with custom applicators and templates emerging as predominant endpoints. The majority of studies involved in vivo clinical applications, followed by in silico computational modeling and in vitro experiments. Conclusions: The upward trend in scientific publications underscores the growing attention on 3D printing for enhancing personalized brachytherapy. The increasing use of 3D-printed templates and applicators highlights their role in optimizing dose delivery and expanding personalized treatment strategies. The current research trend is shifting toward real-world data and in vivo studies to assess clinical applications, ensuring these innovations translate effectively into routine practice. The integration of 3D printing represents a major advancement in radiation oncology, with the potential to enhance treatment efficacy and patient outcomes. Future research should focus on standardizing manufacturing processes and expanding clinical validation to facilitate broader adoption.
1. Introduction
Over time, interventional radiotherapy (brachytherapy, IRT, BT) evolved with the development of safer radioactive sources such as cesium-137, iridium-192, and iodine-125, improving dose control to tumor tissues while minimizing side effects on surrounding healthy tissues. Today, IRT stands as a cornerstone of modern radiation oncology, particularly in the treatment of gynecological, prostate, and skin cancers [1]. A growing body of literature highlights the continuous evolution of IRT, driven by technological advancements and the need for improved treatment personalization. Recent studies demonstrate that the integration of novel materials and advanced imaging techniques has led to superior dosimetric precision and enhanced clinical outcomes in various oncological applications [2].
Today, IRT stands as a cornerstone of modern radiation oncology, particularly using intracavitary, interstitial, and contact techniques, which enable precise and localized dose delivery. Nevertheless, IRT is not yet a universally routine component of clinical practice. While its role is well established—especially in the definitive treatment of gynecological malignancies—it is more selectively applied in specific clinical scenarios, such as irregularly shaped skin tumors or salvage settings, where its dosimetric advantages are particularly valuable. Intracavitary IRT involves placing radioactive sources within natural body cavities, making it a standard approach for treating gynecological malignancies such as cervical and endometrial cancer. Interstitial IRT, on the other hand, involves implanting radioactive sources directly into the tumor or surrounding tissue, providing enhanced dose conformity, and is commonly used for prostate, breast, and soft tissue tumors [3]. Contact IRT delivers radiation through direct contact with the tumor surface, making it particularly effective for treating non-melanoma skin cancers [4].
The adoption of 3D-printing technology in IRT has revolutionized the field by providing unparalleled levels of customization and precision. This approach enables the development of patient-specific devices tailored to individual anatomical and pathological needs, significantly enhancing the efficacy and safety of treatments. This adaptability of 3D-printed devices allows clinicians to address even the most complex anatomical and clinical scenarios, improving therapeutic outcomes and patient comfort. Unlike traditional manufacturing methods, which are often limited in their adaptability to patient-specific anatomical complexities, 3D printing enables the development of personalized devices that optimize dose distribution while reducing radiation exposure to organs at risk (OARs). As highlighted by recent studies, 3D-printed templates and applicators have been shown to improve procedural accuracy, reduce treatment-related complications, and enhance patient comfort compared to conventional approaches [5].
The final product of the 3D-printing process can take various forms, depending on clinical requirements such as applicators, templates, and miscellaneous factors. These applicators can be customized to fit patient-specific anatomical features and are particularly useful in addressing challenges such as unfavorable tumor topographies, narrow anatomical structures, or asymmetrical tumors. By enabling highly conformal dose distributions, 3D-printed solutions enhance tumor control probability and minimize exposure to adjacent OARs.
In gynecological IRT, 3D-printed devices, such as multichannel vaginal cylinders and intrauterine tandems with oblique needle channels, have been instrumental in overcoming the limitations of commercial applicators. These tools facilitate improved dose delivery and ensure better coverage of high-risk clinical target volumes (CTV-HR) [6]. In addition to gynecological applications, 3D printing has been widely adopted in the treatment of superficial malignancies, such as non-melanoma skin cancer (NMSC). Custom contact applicators and molds are fabricated to conform to the patient’s unique skin topography for convex and concave anatomy, reducing air gaps, optimizing dose homogeneity, and ensuring precise positioning. These innovations not only improve treatment accuracy but also enable rapid adjustments to accommodate tumor changes during therapy. Hybrid devices that integrate interstitial and surface techniques further expand the possibilities of personalized IRT.
The use of 3D-printed devices spans a variety of research and clinical contexts. In silico studies leverage computational modeling to evaluate new applicator designs and optimize dosimetry. In vitro studies utilize cell models to test device performance and compatibility. In vivo investigations in animal or human subjects assess the clinical applicability and safety of these innovations. Furthermore, real-life clinical studies have demonstrated the practicality and effectiveness of 3D-printed solutions in routine IRT settings. Whether employed as templates or fully functional applicators, these devices provide the precision and adaptability necessary for modern IRT.
Previous reviews have generally explored the integration of 3D printing into IRT from a broader perspective, focusing on its feasibility and general benefits. In contrast, our review specifically examines the clinical applications of 3D printing in IRT, with a particular emphasis on the final 3D-printed products and the types of studies conducted to validate their use. Over the past decade, numerous investigations have approached this technological advancement using different methodologies, including computational modeling, experimental testing, and clinical validation. These efforts highlight the progressive integration of 3D printing into IRT, demonstrating its ability to address anatomical challenges, improve treatment planning, and enhance the overall quality of care. This review aims to provide a comprehensive overview of these advancements, charting the evolution of 3D printing applications and underscoring its potential to further personalize and optimize treatment strategies in IRT.
This review is structured as follows: Section 2 describes the methodology used to select and classify the studies. Section 3 presents the results, including a quantitative and qualitative analysis of the selected papers. Section 4 discusses the key trends and implications, and Section 5 outlines the conclusions and directions for future research.
2. Methods
This review was conducted by searching the scientific databases PubMed, Scopus, and Google Scholar for studies related to the application of 3D printing in IRT. The keywords “brachytherapy” and “3D-printing” were used to identify relevant publications published between 2020 and 2024. Figure 1 provides a detailed overview of the article selection process.
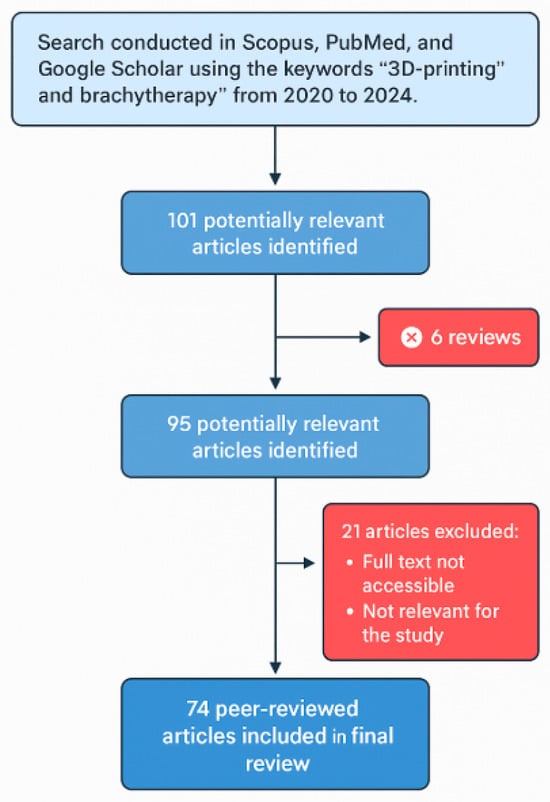
Figure 1.
Flowchart of the article selection process for the review on 3D printing in IRT (2020–2024).
The initial search yielded 101 potentially relevant articles. Exclusion criteria were then applied to ensure the quality and focus of the review. Specifically, six scientific articles were not considered for the analysis because they were reviews themselves, leaving 95 articles for further evaluation. Subsequently, 21 additional articles were excluded because their full text was inaccessible or deemed irrelevant to the study. This process resulted in 74 peer-reviewed articles that were included in the final analysis.
For each study, information was extracted and categorized based on specific assumptions. Publications where multiple techniques, radioactive sources, or endpoints were reported were considered as distinct entries for each category to allow a detailed evaluation of the various implementations. Endpoints were classified as applicators if the 3D-printed device remains in place during irradiation, containing the catheters or sources within its structure. Templates were defined as devices used solely to geometrically configure the placement of catheters or sources, which are removed before irradiation. Miscellaneous endpoints included other uses, such as devices for quality assurance, immobilization systems, and spacers.
The type of study was categorized based on the methodology used. In vitro studies involved cell cultures, while in vivo studies involved animals or patients. In silico studies included simulations or theoretical investigations. The IRT technique was identified as interstitial, intracavitary, or contact, depending on the specific application.
This structured approach ensured a comprehensive evaluation of advancements in the use of 3D printing within IRT.
3. Results
The analysis presented in Table 1 summarizes the characteristics and trends in the application of 3D printing technology in IRT across the 74 included studies. These studies were categorized based on publication year, radioactive source, IRT technique, endpoint of the 3D-printed product, diseases, and type of study. A variety of radioactive sources were identified, including 192Ir, 125I, 60Co, 90Y, and 103Pd, reflecting the range of isotopes commonly used in clinical and experimental settings. The IRT techniques analyzed included interstitial, intracavitary, and contact applications, highlighting the different approaches where 3D printing has been integrated. Endpoints were classified into three main categories: applicators, which remain in place during irradiation; templates, which are used to guide catheter or source positioning and then removed; and miscellaneous applications, encompassing devices for quality assurance, immobilization, or dose modulation. The studies were also categorized by study type, including in vitro experiments on cell cultures, in silico computational simulations, and in vivo investigations involving animal models or patients.

Table 1.
Publication year, radioactive source, IRT technique, endpoint of 3D-printing application, study type, and disease for each analyzed publication.
The radar chart (upper panel, Figure 2) shows the yearly distribution of studies, with the highest number of studies observed in 2024 (24.3%), followed by 2021 (21.6%) and 2023 (21.6%), and 2022 (17.6%). The lowest proportion was observed in 2020 (13.5%).
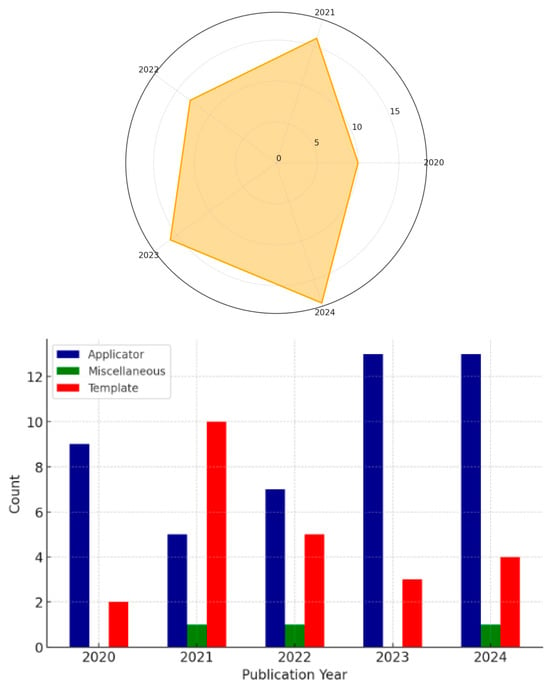
Figure 2.
The upper panel presents a radar chart illustrating the distribution of studies across the years from 2020 to 2024, categorized by the total number of studies analyzed. The lower panel displays a bar chart showing the distribution of endpoints (applicator, template, and miscellaneous) per year.
The bar chart (lower panel, Figure 2) illustrates the frequency of endpoints per year. Applicators were the most frequently reported endpoint across all years, with percentages of 81.8% in 2020, 31.3% in 2021, 53.8% in 2022, 81.3% in 2023, and 72.2% in 2024. Templates were the second most reported endpoint, with proportions of 18.2% in 2020, 62.5% in 2021, 38.5% in 2022, 18.8% in 2023, and 22.2% in 2024. Miscellaneous endpoints were rarely reported, with percentages of 0.0% in 2020, 6.3% in 2021, 7.7% in 2022, and 0.0% in 2023 and 5.6% 2024.
The alluvial plot (Figure 3) shows that the most frequently used radioactive source is 192Ir, followed by 125I. Interstitial techniques are the most commonly employed, with a significant proportion of studies also using intracavitary and contact techniques. The majority of studies are categorized as in vivo, followed by in silico and in vitro. The plot highlights the connections between sources, techniques, and study types, with 192Ir predominantly associated with interstitial and intracavitary techniques, while 125I is mainly linked to interstitial applications.

Figure 3.
Alluvial plot illustrates the relationships between the radioactive source, technique, and study type in the analyzed articles. The plot highlights the flow of studies from radioactive sources to techniques including contact, interstitial, and intracavitary and subsequently to study types such as in silico, in vitro, and in vivo. The thickness of the flows represents the frequency of occurrences within the dataset.
The bar chart (Figure 4) shows that interstitial templates and interstitial applicators are the most frequently reported, each exceeding 20 studies. Intracavitary applicators follow with 13 studies, while contact applicators have 10 studies. Miscellaneous is reported with a lower frequency, at 2 studies, while interstitial miscellaneous has the lowest representation, with only 1 study.
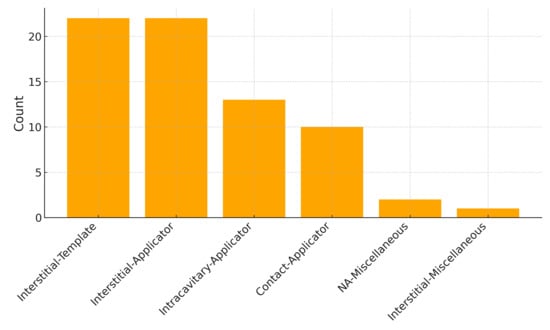
Figure 4.
Bar chart presents the distribution of studies categorized by technique and endpoint.
4. Discussion
The results highlight the significant role of 3D printing in IRT, with key trends emerging across sources, techniques, endpoints, and study types.
The yearly distribution of articles shows a positive trend overall, with an increase in the number of publications over time. However, there is a noticeable decline in articles published between 2021 and 2022. This deflection might be attributed to challenges in conducting research during the COVID-19 pandemic, which likely impacted the availability of resources and the pace of experimental and clinical studies.
The analysis revealed that 192Ir and 125I are the most frequently used radioactive sources, reflecting their established roles in clinical and experimental settings. 192Ir is the most used source in after-loaders, which further emphasizes its prevalence and versatility in IRT applications. The predominance of 192Ir, particularly in interstitial and intracavitary techniques, underscores its effectiveness for precise dose delivery. In contrast, 125I is primarily linked to interstitial applications, likely due to its low-energy emission characteristics suitable for localized treatments.
Among the techniques, interstitial approaches dominated the dataset, followed by intracavitary and contact techniques. The dominance of interstitial techniques can be attributed to the ability of 3D printing to conform implants more effectively in complex anatomical scenarios where interstitial approaches are preferred. This capability makes interstitial techniques particularly valuable in cases involving irregularly shaped tumors or challenging anatomical regions. Intracavitary techniques, frequently associated with gynecological cancers, also showed strong representation, while contact techniques were more focused on superficial tumors, such as non-melanoma skin cancers.
In terms of endpoints, applicators emerged as the most reported category across all years, highlighting their role as fully functional devices that are ready for use directly in clinical settings. Templates, on the other hand, are closely tied to interstitial techniques in most publications, as they are primarily used to guide catheter or source positioning. This distinction between endpoints reflects the versatility of 3D printing in addressing different clinical needs, with applicators offering a complete solution and templates providing precise guidance for interstitial treatments.
The bar chart further illustrates this distribution, with interstitial applicators and templates being the most frequently reported combinations, exceeding 20 occurrences each. The high frequency of interstitial templates highlights their utility in procedures requiring precise catheter placement in anatomically complex regions. Intracavitary and contact applicators follow, with counts between 10 and 15, reflecting their relevance in specific clinical scenarios, such as gynecological and superficial tumors. Less frequent categories, such as interstitial miscellaneous and intracavitary templates, were reported in fewer than five studies, likely representing specialized or emerging applications of 3D printing in IRT.
Finally, the analysis of study types showed a majority of in vivo investigations. This trend reflects the focus on obtaining results in real-world clinical settings, which often rely on feedback and insights from prior in silico simulations and in vitro experiments using cell cultures. The progression from computational and laboratory-based studies to in vivo applications underscores the strong translational aspect of 3D-printed IRT devices, highlighting their ability to move from experimental development to practical implementation. This translational approach ensures that these technologies are not only innovative but also relevant and impactful in clinical practice.
A major limitation in the current body of evidence is the lack of randomized controlled trials directly comparing 3D-printed moulds with standard devices. As a result, most claims regarding the superiority of 3D-printed solutions are based on theoretical dose distributions or non-randomized feasibility studies. While the preliminary data are promising, these potential advantages require rigorous clinical validation before they can be translated into standardized patient care protocols.
5. Conclusions
The integration of advanced technologies, such as 3D printing, is increasingly important in IRT, enabling greater treatment precision, customization, and efficiency. The growing trend in research reflects its expanding role in clinical practice. 3D printing has demonstrated versatility across various radioactive sources, techniques, and endpoints, with interstitial techniques particularly benefiting from its ability to adapt implants to complex anatomical structures. The focus on in vivo studies highlights the translational impact of these technologies, bridging the gap between research and real-world clinical applications. This progression underscores the value of innovative approaches in optimizing and personalizing IRT, paving the way for improved standards of care.
Future research should aim to standardize the design and manufacturing workflows of 3D-printed devices for brachytherapy to ensure reproducibility and quality assurance across institutions. In addition, large-scale prospective clinical trials are needed to validate the clinical efficacy and safety of these technologies. Cost-effectiveness analyses will be critical to assess their sustainability in routine practice. Finally, integrating 3D printing with artificial intelligence-driven planning tools may offer new frontiers in precision oncology and personalized radiotherapy.
Author Contributions
Conceptualization, E.R. and S.R.; methodology, E.R.; software, M.V.; validation, P.C., V.L. and L.B.; formal analysis, B.F.; investigation, B.F. and S.R.; data curation, E.P.; writing—original draft preparation, E.R.; writing—review and editing, E.P. and M.D.S.; visualization, M.D.S., L.T. and G.C.; supervision, G.C. and A.N.; project administration, M.D.S. and L.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| 3D | Three-dimensional |
| BT | Brachytherapy |
| CT | Computed Tomography |
| CTV-HR | High-risk Clinical Target Volume |
| Gyn | Gynecology |
| HDR | High Dose Rate |
| IRT | Interventional Radiotherapy |
| MRI | Magnetic Resonance Imaging |
| NA | Not Available |
| OAR | Organ at Risk |
| QA | Quality Assurance |
References
- Pötter, R.; Tanderup, K.; Kirisits, C.; De Leeuw, A.; Kirchheiner, K.; Nout, R.; Tan, L.T.; Haie-Meder, C.; Mahantshetty, U.; Segedin, B.; et al. The EMBRACE II study: The outcome and prospect of two decades of evolution within the GEC-ESTRO GYN working group and the EMBRACE studies. Clin. Transl. Radiat. Oncol. 2018, 9, 48–60. [Google Scholar] [CrossRef] [PubMed]
- Bellis, R.; Rembielak, A.; Barnes, E.A.; Paudel, M.; Ravi, A. Additive manufacturing (3D printing) in superficial brachytherapy. J. Contemp. Brachytherapy 2021, 13, 468–482. [Google Scholar] [CrossRef]
- Tanderup, K.; Viswanathan, A.N.; Kirisits, C.; Frank, S.J. Magnetic Resonance Image Guided Brachytherapy. Semin. Radiat. Oncol. 2014, 24, 181–191. [Google Scholar] [CrossRef] [PubMed]
- Poltorak, M.; Banatkiewicz, P.; Poltorak, L.; Sobolewski, P.; Zimon, D.; Szwast, M.; Walecka, I. Brachytherapy and 3D printing for skin cancer: A review paper. J. Contemp. Brachytherapy 2024, 16, 156–169. [Google Scholar] [CrossRef] [PubMed]
- Chen, E.; Zhang, Y.; Zhang, H.; Jia, C.; Liang, Y.; Wang, J. Dosimetry study of three-dimensional print template for 125I implantation therapy. Radiat. Oncol. 2021, 16, 115. [Google Scholar] [CrossRef]
- Segedin, B.; Kobav, M.; Zobec Logar, H.B. The Use of 3D Printing Technology in Gynaecological Brachytherapy—A Narrative Review. Cancers 2023, 15, 4165. [Google Scholar] [CrossRef]
- Biltekin, F.; Akyol, H.; Gültekin, M.; Yildiz, F. 3D printer-based novel intensity-modulated vaginal brachytherapy applicator: Feasibility study. J. Contemp. Brachytherapy 2020, 12, 17–26. [Google Scholar] [CrossRef]
- Subashi, E.; Jacobs, C.; Hood, R.; Kirsch, D.G.; Craciunescu, O. A design process for a 3D printed patient-specific applicator for HDR brachytherapy of the orbit. 3D Print. Med. 2020, 6, 15. [Google Scholar] [CrossRef]
- Pashazadeh, A.; Robatjazi, M.; Castro, N.J.; Friebe, M. A multiwell applicator for conformal brachytherapy of superficial skin tumors: A simulation study. Ski. Res. Technol. 2020, 26, 537–541. [Google Scholar] [CrossRef]
- He, X.; Liu, M.; Zhang, M.; Sequeiros, R.B.; Xu, Y.; Wang, L.; Liu, C.; Wang, Q.; Zhang, K.; Li, C. A novel three-dimensional template combined with MR-guided 125I brachytherapy for recurrent glioblastoma. Radiat. Oncol. 2020, 15, 146. [Google Scholar] [CrossRef]
- Kunogi, H.; Yamaguchi, N.; Sasai, K. Evaluation of a new bi-valve vaginal speculum applicator design for gynecologic interstitial brachytherapy. J. Contemp. Brachytherapy 2020, 12, 27–34. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.; Yang, Z.; Jiang, S.; Zhou, L.; Zhou, Z.; Wang, W. Individualized and inverse optimized needle configuration for combined intracavitary-interstitial brachytherapy in locally advanced cervical cancer. J. Cancer Res. Ther. 2019, 15, 1589. [Google Scholar] [CrossRef] [PubMed]
- Is 3D printing-gided three-dimensional brachytherapy suitable for cervical cancer: From one single research institute? Eur. J. Gynaecol. Oncol. 2020, 41, 591. [CrossRef]
- Jiang, W.; Jiang, P.; Wei, S.; Jiang, Y.; Ji, Z.; Sun, H.; Fan, J.; Li, W.; Shao, Y.; Wang, J. The accuracy and safety of CT-guided iodine-125 seed implantation assisted by 3D non-coplanar template for retroperitoneal recurrent carcinoma. World J. Surg. Oncol. 2020, 18, 307. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Wang, H.; Jiang, Y.; Ji, Z.; Guo, F.; Jiang, P.; Li, X.; Chen, Y.; Sun, H.; Fan, J.; et al. The efficacy and dosimetry analysis of CT-guided 125I seed implantation assisted with 3D-printing non-co-planar template in locally recurrent rectal cancer. Radiat. Oncol. 2020, 15, 179. [Google Scholar] [CrossRef] [PubMed]
- Jiang, P.; Qu, A.; Wei, S.; Sun, H.; Zhang, X.; Li, X.; Wang, J. The Preliminary Results of 3-Dimensional Printed Individual Template Assisted 192Ir High-Dose Rate Interstitial Brachytherapy for Central Recurrent Gynecologic Cancer. Technol. Cancer Res. Treat. 2020, 19, 1533033820971607. [Google Scholar] [CrossRef]
- Pashazadeh, A.; Friebe, M. Transverse dose profile simulation of extruded lines for a 3D printed models for superficial skin cancer therapy. Curr. Dir. Biomed. Eng. 2020, 6, 559–562. [Google Scholar] [CrossRef]
- Simpson-Page, E.; Hamlett, L.; Lew, D.; Stephens, H.; Wilks, R.; Kairn, T.; Crowe, S.B. 3D printed brachytherapy jig for Reference Air Kerma Rate calibration. Phys. Eng. Sci. Med. 2021, 44, 1141–1150. [Google Scholar] [CrossRef]
- Bielęda, G.; Marach, A.; Boehlke, M.; Zwierzchowski, G.; Malicki, J. 3D-printed surface applicators for brachytherapy: A phantom study. J. Contemp. Brachytherapy 2021, 13, 549–562. [Google Scholar] [CrossRef]
- Ji, Z.; Jiang, Y.; Sun, H.; Chen, Y.; Guo, F.; Fan, J.; Wang, J. 3D-printed template and optical needle navigation in CT-guided iodine-125 permanent seed implantation. J. Contemp. Brachytherapy 2021, 13, 410–418. [Google Scholar] [CrossRef]
- Qu, A.; Jiang, P.; Wei, S.; Jiang, Y.; Ji, Z.; Sun, H.; Li, W.; Shao, Y.; Fan, J.; Wang, J. Accuracy and dosimetric parameters comparison of 3D-printed non-coplanar template-assisted computed tomography-guided iodine-125 seed ablative brachytherapy in pelvic lateral recurrence of gynecological carcinomas. J. Contemp. Brachytherapy 2021, 13, 39–45. [Google Scholar] [CrossRef] [PubMed]
- Ji, Z.; Sun, H.; Jiang, Y.; Chen, Y.; Guo, F.; Fan, J.; Wang, J. Analysis on the accuracy of CT-guided radioactive I-125 seed implantation with 3D printing template assistance in the treatment of thoracic malignant tumors. J. Radiat. Res. 2021, 62, 910–917. [Google Scholar] [CrossRef] [PubMed]
- Yan, J.; Qin, X.; Zhang, F.; Hou, X.; Yu, L.; Qiu, J. Comparing multichannel cylinder and 3D-printed applicators for vaginal cuff brachytherapy with preliminary exploration of post-hysterectomy vaginal morphology. J. Contemp. Brachytherapy 2021, 13, 641–648. [Google Scholar] [CrossRef]
- Kang, W.; Zhang, H.; Liang, Y.; Chen, E.; Zhao, J.; Gao, Z.; Wang, J. Comparison of three-dimensional-printed template-guided and traditional implantation of125I seeds for gynecological tumors: A dosimetric and efficacy study. J. Cancer Res. Ther. 2021, 17, 688–694. [Google Scholar] [CrossRef] [PubMed]
- Semeniuk, O.; Cherpak, A.; Robar, J. Design and evaluation of 3D printable patient-specific applicators for gynecologic HDR brachytherapy. Med. Phys. 2021, 48, 4053–4063. [Google Scholar] [CrossRef]
- Wang, L.; Wang, H.; Jiang, Y.; Ji, Z.; Guo, F.; Jiang, P.; Qiu, B.; Sun, H.; Fan, J.; Li, W.; et al. Dosimetric comparison of computed tomography-guided iodine-125 seed implantation assisted with and without three-dimensional printing non-coplanar template in locally recurrent rectal cancer: A propensity score matching study. J. Contemp. Brachytherapy 2021, 13, 18–23. [Google Scholar] [CrossRef]
- Han, X.; Fang, S.; Sheng, R.; Wang, Y.; Zhou, J.; Wang, J. Dosimetry verification of three-dimensional printed polylactic acid template-guided precision125 I seed implantation for lung cancer using a desktop three-dimensional printer. J. Appl. Clin. Med. Phys. 2021, 22, 202–209. [Google Scholar] [CrossRef]
- Deufel, C.L.; Dalvin, L.A.; Qian, J.; Vaishnav, B.; Cutsinger, J.M.; Wittich, M.N.; Petersen, I.A. How to design, fabricate, and validate a customized COMS-style eye plaque: Illustrated with a narrow-slotted plaque example. Brachytherapy 2021, 20, 1235–1244. [Google Scholar] [CrossRef]
- Mohammadi, R.; Siavashpour, Z.; Rashid Hosseini Aghdam, S.; Fazli, S.; Major, T.; Asghar Rohani, A. Manufacturing and evaluation of multi-channel cylinder applicator with 3D printing technology. J. Contemp. Brachytherapy 2021, 13, 80–90. [Google Scholar] [CrossRef]
- Liu, Y.; Jiang, P.; Zhang, H.; Wang, J. Safety and efficacy of 3D-printed templates assisted CT-guided radioactive iodine-125 seed implantation for the treatment of recurrent cervical carcinoma after external beam radiotherapy. J. Gynecol. Oncol. 2021, 32, e15. [Google Scholar] [CrossRef]
- Gong, W.; Chen, Y.; Ji, Z.; Jiang, Y.; Qiu, B.; Sun, H.; Wang, J. The accuracy and dosimetric analysis of 3D-printing non-coplanar template-assisted iodine-125 seed implantation for recurrent chest wall cancer. J. Contemp. Brachytherapy 2021, 13, 273–279. [Google Scholar] [CrossRef] [PubMed]
- Qiu, B.; Jiang, Y.; Ji, Z.; Sun, H.; Fan, J.; Li, W.; Shao, Y.; Jiang, P.; Wang, J. The Accuracy of Individualized 3D-Printing Template-Assisted I125 Radioactive Seed Implantation for Recurrent/Metastatic Head and Neck Cancer. Front. Oncol. 2021, 11, 664996. [Google Scholar] [CrossRef]
- Wang, H.; Peng, R.; Li, X.; Wang, Y.; Jiang, Y.; Ji, Z.; Guo, F.; Tian, S.; Sun, H.; Fan, J.; et al. The dosimetry evaluation of 3D printing non-coplanar template-assisted CT-guided 125I seed stereotactic ablation brachytherapy for pelvic recurrent rectal cancer after external beam radiotherapy. J. Radiat. Res. 2021, 62, 473–482. [Google Scholar] [CrossRef]
- Bielęda, G.; Chicheł, A.; Boehlke, M.; Zwierzchowski, G.; Chyrek, A.; Burchardt, W.; Stefaniak, P.; Wiśniewska, N.; Czereba, K.; Malicki, J. 3D printing of individual skin brachytherapy applicator: Design, manufacturing, and early clinical results. J. Contemp. Brachytherapy 2022, 14, 205–214. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Shen, Z.; Qu, A.; Jiang, P.; Jiang, Y.; Wang, J. A comparative study of dosimetric parameters of 3D-printed non-coplanar template-assisted CT-guided iodine-125 seed implantation brachytherapy in patients with inguinal lymph node metastatic carcinomas. J. Contemp. Brachytherapy 2022, 14, 452–461. [Google Scholar] [CrossRef]
- Sohn, J.J.; Polizzi, M.; Richeson, D.; Gholami, S.; Das, I.J.; Song, W.Y. A Novel Workflow with a Customizable 3D Printed Vaginal Template and a Direction Modulated Brachytherapy (DMBT) Tandem Applicator for Adaptive Interstitial Brachytherapy of the Cervix. J. Clin. Med. 2022, 11, 6989. [Google Scholar] [CrossRef]
- Di, X.; Zhang, H.; Liu, X.; Zhao, J.; Gao, Z.; Yu, H.; Su, X.; Liang, Y.; Wang, J. A new technique for trans-perirectal iodine-125 seed implantation in prostatic cancer guided by CT and 3D printed template: Two case reports. Front. Oncol. 2022, 12, 1031970. [Google Scholar] [CrossRef] [PubMed]
- Marar, M.; Simiele, E.; Niedermayr, T.; Kidd, E.A. Applying 3D-Printed Templates in High-Dose-Rate Brachytherapy for Cervix Cancer: Simplified Needle Insertion for Optimized Dosimetry. Int. J. Radiat. Oncol. 2022, 114, 111–119. [Google Scholar] [CrossRef]
- Hagan, C.T.; Bloomquist, C.; Kim, I.; Knape, N.M.; Byrne, J.D.; Tu, L.; Wagner, K.; Mecham, S.; DeSimone, J.; Wang, A.Z. Continuous liquid interface production of 3D printed drug-loaded spacers to improve prostate cancer brachytherapy treatment. Acta Biomater. 2022, 148, 163–170. [Google Scholar] [CrossRef]
- Chatzikonstantinou, G.; Diefenhardt, M.; Fleischmann, M.; Meissner, M.; Scherf, C.; Trommel, M.; Ramm, U.; Rödel, C.; Tselis, N.; Licher, J. Customized 3D-printed molds for high dose-rate brachytherapy in facial skin cancer: First clinical experience. JDDG J. Dtsch. Dermatol. Ges. 2023, 21, 35–41. [Google Scholar] [CrossRef]
- Wang, B.; Qiu, B.; Wu, L.; Liu, Y.; Zhang, J.; Wang, R.; Zhang, K.; Wang, J. Efficacy and safety of 3D printing coplanar template-assisted iodine-125 seed implantation as palliative treatment for inoperable pancreatic cancer. J. Contemp. Brachytherapy 2022, 14, 140–147. [Google Scholar] [CrossRef]
- Qin, X.; Zhang, F.; Hou, X.; Yu, L.; Yu, L.; Yan, J.; Qiu, J. Efficacy and safety of a 3D-printed applicator for vaginal brachytherapy in patients with central pelvic-recurrent cervical cancer after primary hysterectomy. Brachytherapy 2022, 21, 193–201. [Google Scholar] [CrossRef] [PubMed]
- Sohn, J.J.; Polizzi, M.; Kang, S.-W.; Ko, W.-H.; Cho, Y.-H.; Eom, K.-Y.; Chung, J.-B. Intensity Modulated High Dose Rate (HDR) Brachytherapy Using Patient Specific 3D Metal Printed Applicators: Proof of Concept. Front. Oncol. 2022, 12, 829529. [Google Scholar] [CrossRef]
- Li, P.; Fan, J.; Zhang, K.; Wang, J.; Hu, M.; Yang, S.; Xing, C.; Yuan, Q. Interstitial125 I Brachytherapy as a Salvage Treatment for Refractory Cervical Lymph Node Metastasis of Thoracic Esophageal Squamous Cell Carcinoma After External Irradiation With a CT-Guided Coplanar Template-Assisted Technique: A Retrospective Study. Technol. Cancer Res. Treat. 2022, 21, 15330338221103102. [Google Scholar] [CrossRef] [PubMed]
- Zwierzchowski, G.; Bielęda, G.; Szymbor, A.; Boehlke, M. Personalized Superficial HDR Brachytherapy—Dosimetric Verification of Dose Distribution with Lead Shielding of Critical Organs in the Head and Neck Region. J. Pers. Med. 2022, 12, 1432. [Google Scholar] [CrossRef]
- Morcos, M.; Vogel, J.; Garcia, J.R.; Gomez-Lobo, V.; Bartolac, S. Treatment of pediatric vaginal rhabdomyosarcoma with the use of a real-time tracked custom applicator. Brachytherapy 2022, 21, 291–299. [Google Scholar] [CrossRef] [PubMed]
- Mao, Z.; Zhao, H. 3D-printed vaginal cylindrical template with curved needle channels in MRI-guided vaginal cuff brachytherapy. J. Contemp. Brachytherapy 2023, 15, 422–431. [Google Scholar] [CrossRef]
- Wilks, R.; Crowe, S.B.; Chan, P.; Cheuk, R.; Kairn, T. A 3D printed patient-specific vaginal mould for brachytherapy. J. Phys. Conf. Ser. 2023, 2630, 012026. [Google Scholar] [CrossRef]
- Rane, S.; Hanania, A.; Arango, E.; Kumar, K.; Payne, L.; Dittmar, S.; Gomber, G.; Ugarte, V.; Ludwig, M. A 3D-Printable, Low-Cost Obturator for Less Invasive Gynecologic Brachytherapy. Cureus 2023, 15, e41162. [Google Scholar] [CrossRef]
- Quiñones Rodríguez, L.Á.; Pavón, J.P.; Ramírez, I.C.; Bayard, L.G.; Oquendo, M.A.I. Clinical implementation of 3D printed plesiotherapy moulds using free open source software. Ann. 3D Print. Med. 2023, 12, 100124. [Google Scholar] [CrossRef]
- Cobussen, A.; Petric, P.; Wulff, C.N.; Buus, S.; Spejlborg, H.; Nielsen, S.K.; Traberg, A.; Meisner, B.; Hokland, S.; Lindegaard, J.C. Clinical outcomes using a 3D printed tandem-needle-template and the EMBRACE-II planning aims for image guided adaptive brachytherapy in locally advanced cervical cancer. Acta Oncol. 2023, 62, 1470–1478. [Google Scholar] [CrossRef] [PubMed]
- Marar, M.; Niedermayr, T.; Kidd, E.A. Developing Next-Generation 3-Dimensional Printing for Cervical Cancer Hybrid Brachytherapy: A Guided Interstitial Technique Enabling Improved Flexibility, Dosimetry, and Efficiency. Int. J. Radiat. Oncol. 2023, 117, 312–320. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Cheng, Y.; Song, Y.; Lei, J.; Li, Y.; Li, X.; Shi, H. Dosimetric parameters and safety analysis of 3D-printing non-coplanar template-assisted interstitial brachytherapy for non-centrally recurrent cervical cancer. Front. Oncol. 2023, 13, 1174470. [Google Scholar] [CrossRef] [PubMed]
- Liu, B.; Wu, Y.; Sun, L.; Guo, C.; Wang, Q.; Mu, Z. Dosimetry and plan parameters study of three-dimensional-printed template-based intra-cavitary/interstitial interpolation technology using computed tomography-guided high-dose-rate brachytherapy in locally advanced cervical cancer. J. Contemp. Brachytherapy 2023, 15, 325–333. [Google Scholar] [CrossRef]
- Lee, V.W.Y.; Yip, W.W.L.; Tang, S.Y.K.; Leung, M.P.H.; Kwan, K.K.K.; Liu, A.C.H.; Chan, V.N.Y.; Wu, J.W.S.; Cheng, J.N.S.; Chiang, C.-L.; et al. Efficacy and feasibility of 3D printed redesigned VeneziaTM applicator for treating advanced cervix and recurrent endometrial cancer. Phys. Med. 2023, 114, 103150. [Google Scholar] [CrossRef]
- Kiseleva, M.; Lescot, T.; Selivanova, S.V.; Fortin, M. Gold-Enhanced Brachytherapy by a Nanoparticle-Releasing Hydrogel and 3D-Printed Subcutaneous Radioactive Implant Approach. Adv. Healthc. Mater. 2023, 12, 2300305. [Google Scholar] [CrossRef]
- Zeng, Z.; Lu, Y.; Zhang, F.; Zhang, J.; Zhang, W.; Luo, C.; Guo, Y.; Yan, J.; Yu, L. Personalized Brachytherapy for a Herlyn-Werner-Wunderlich Syndrome Patient with Endometrial Cancer: A Case Report. Cancer Manag. Res. 2023, 15, 691–697. [Google Scholar] [CrossRef]
- Chen, Y.; Ji, Z.; He, C.; Dai, J.; Zhang, K.; Li, C.; Song, Y.; Yan, L.; Ma, Y.; Jiang, Y.; et al. Stereotactic ablative brachytherapy with or without assistance of 3D-printing templates for inoperable locally recurrent or oligometastatic soft-tissue sarcoma: A multicenter real-world study. Am. J. Cancer Res. 2023, 13, 6226. [Google Scholar]
- Bienvenido, R.; Quiñones, L.Á.; Pérez, J.; Castro, I.; Gutiérrez, L.; López, J.D.D.; Botana, J.; Iborra, M.A. Study of dose dependence on density in planar 3D-printed applicators for HDR Ir192 surface brachytherapy. Brachytherapy 2023, 22, 250–259. [Google Scholar] [CrossRef]
- Kamio, Y.; Roy, M.-È.; Morgan, L.-A.; Barkati, M.; Beauchemin, M.-C.; DeBlois, F.; Basaric, B.; Carrier, J.-F.; Bedwani, S. The Montreal split ring applicator: Towards highly adaptive gynecological brachytherapy using 3D-printed biocompatible patient-specific interstitial caps. J. Contemp. Brachytherapy 2023, 15, 453–464. [Google Scholar] [CrossRef]
- He, X.; Xu, Y.; Liu, M.; Fang, J.; Zhang, K.; Guo, X.; Yan, X.; Li, C. Three-dimensional template combined with MR-guided iodine-125 brachytherapy for recurrent brain metastases. J. Contemp. Brachytherapy 2023, 15, 174–183. [Google Scholar] [CrossRef] [PubMed]
- Lescot, T.; Lebel-Cormier, M.; Seniwal, B.; Gros-Louis, P.; Bellerive, C.; Landreville, S.; Beaulieu, L.; Fortin, M. Tumor Shape-Specific Brachytherapy Implants by 3D-Printing, Precision Radioactivity Painting, and Biomedical Imaging. Adv. Healthc. Mater. 2023, 12, 2300528. [Google Scholar] [CrossRef] [PubMed]
- Straathof, R.; Van Vliet-Pérez, S.M.; Kolkman-Deurloo, I.-K.K.; Wauben, L.S.G.L.; Nout, R.A.; Heijmen, B.J.M.; Rossi, L.; Dankelman, J.; Van De Berg, N.J. Automated planning of curved needle channels in 3D printed patient-tailored applicators for cervical cancer brachytherapy. Phys. Med. Biol. 2024, 69, 235007. [Google Scholar] [CrossRef]
- Han, P.; Li, F.; Zhang, Y.; Gao, L.; Zhang, G.; Guo, Q.; Zhu, Y.; Su, Q. B-ultrasound or CT-guided 3D-printing individualized non-coplanar template brachytherapy for the treatment of locally uncontrolled recurrent head and neck squamous cell carcinoma. Adv. Dermatol. Allergol. 2024, 41, 41–48. [Google Scholar] [CrossRef] [PubMed]
- Di, X.; Gao, Z.; Yu, H.; Liu, X.; Zhao, J.; Wang, J.; Zhang, H. 125I seed brachytherapy for non-central pelvic recurrence of cervical cancer after external beam radiotherapy. Radiat. Oncol. 2024, 19, 70. [Google Scholar] [CrossRef]
- Lu, Z.; Zhu, G.; Qiu, Z.; Guo, H.; Li, J.; Zheng, L.; Chen, C.; Che, J.; Xiang, Y.; Wang, Y. 3D-printed brachytherapy in patients with cervical cancer: Improving efficacy and safety outcomes. Radiat. Oncol. 2024, 19, 152. [Google Scholar] [CrossRef]
- Feng, C.; Wen, X.; Li, S.; Hua, L.; Chen, S. Comparison of 3D-printed multichannel non–co-planar vaginal applicators and single-channel vaginal applicators for brachytherapy with positive or close surgical margins in cervical cancer. Brachytherapy 2024, 23, 641–647. [Google Scholar] [CrossRef]
- AK, S.N.; Saxena, K.; Puzhakkal, N.; Makuny, D.; Mathew, J.; Lawrence, K.D. Design and development of additivemanufactured multi-channel brachytherapy applicators for cancer treatment. J. Micromanufacturing 2024, 6, 25165984231215888. [Google Scholar] [CrossRef]
- Ewongwo, A.; Niedermayr, T.; Kidd, E.A. Design approach and benefits of the 3D-printed vaginal individualized applicator (VIA). Brachytherapy 2024, 23, 282–289. [Google Scholar] [CrossRef]
- Wang, K.; Qu, A.; Deng, X.; Jiang, W.; Sun, H.; Wang, J.; Jiang, P. Efficacy and safety of 3-dimensional printing noncoplanar template (3D-PNCT)-assisted high-dose-rate interstitial brachytherapy (HDR-ISBT) for reirradiation of recurrent cervical cancer: A prospective cohort. J. Gynecol. Oncol. 2025, 36, e20. [Google Scholar] [CrossRef]
- Shen, J.; Chen, M.; Qiu, H.; Yang, C.; Liu, H.; Chen, J.; Wang, D.; Zhao, H.; Sun, S.; Mei, Z.; et al. Evaluation and improvement of the safety of 3D-printed template assisted intracavitary/interstitial brachytherapy for cervical cancer using repeat FMEA. Brachytherapy 2024, 23, 580–589. [Google Scholar] [CrossRef]
- Mobit, P.; Yang, C.C.; Nittala, M.R.; He, R.; Ahmed, H.Z.; Shultz, G.; Lin, A.; Vijayakumar, S. Eye Plaque Brachytherapy for Choroidal Malignant Melanoma: A Case Report on the Use of Innovative Technology to Expand Access, Improve Practice, and Enhance Outcomes. Cureus 2024, 16, e54572. [Google Scholar] [CrossRef]
- Poltorak, M.; Banatkiewicz, P.; Poltorak, L.; Sobolewski, P.; Zimon, D.; Szwast, M.; Walecka, I. Individualized 3D printing for skin cancer brachytherapy: Development, implementation, clinical applications, and treatment assessment. J. Contemp. Brachytherapy 2024, 16, 173–183. [Google Scholar] [CrossRef]
- De Ridder, M.; Smolic, M.; Kastelijns, M.; Kloosterman, S.; Van Der Vegt, S.; Rijken, J.A.; Jürgenliemk-Schulz, I.M.; Dehnad, H.; Kroon, P.S.; Moerland, M.A. Individualized 3D-printed applicators for magnetic resonance imaging-guided brachytherapy in nasal vestibule cancer. Phys. Imaging Radiat. Oncol. 2024, 31, 100629. [Google Scholar] [CrossRef] [PubMed]
- Jin, N.; Meng, F.; Zhu, L.; Xing, L.; Lin, Q.; Zhang, H. Multimodal image-guided surgical robot versus 3D-printed template for brachytherapy of malignant tumours in the skull base and deep facial region: A clinical comparative study. Int. J. Oral Maxillofac. Surg. 2025, 54, 217–224. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Emrich, J.; Mourtada, F. Novel 3D printed universal conical holder for eye plaque quality assurance. J. Appl. Clin. Med. Phys. 2024, 25, e14395. [Google Scholar] [CrossRef] [PubMed]
- Friebe, M.; Boese, A.; Nathan, J.C.; Hutmacher, D.W.; Pashazadeh, A. Personalized 3D Printed Patches for Fast and Safe Radiation Therapy of Non Melanoma Skin Cancer. Phys. Sci. 2024, 9, 0097. [Google Scholar] [CrossRef]
- Poltorak, M.; Banatkiewicz, P.; Poltorak, L.; Sobolewski, P.; Zimon, D.; Szwast, M.; Walecka, I. Reproducibility and air gap pockets of 3D-printed brachytherapy applicator placement in high-dose-rate skin cancer. Phys. Med. 2024, 123, 103401. [Google Scholar] [CrossRef]
- Sekii, S.; Morita, K.; Yada, R.; Tsujino, K. Semi-automatic design concept of 3D-printed individualized template for interstitial brachytherapy of vaginal tumors. Ann. 3D Print. Med. 2024, 14, 100147. [Google Scholar] [CrossRef]
- Ji, Z.; Jiang, Y.L.; Sun, H.T.; Qiu, B.; Li, M.; Fan, J.H.; Wang, J.J. Three-Dimensional-Printed Template-Guided Radioactive Seed Brachytherapy via a Submental Approach for Recurrent Base of Tongue and Floor of Mouth Cancer. World J. Oncol. 2024, 15, 414–422. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).