Morphology of Macular Neovascularization in Age-Related Macular Degeneration Influences Treatment Requirement and Visual Outcome After 1 Year
Abstract
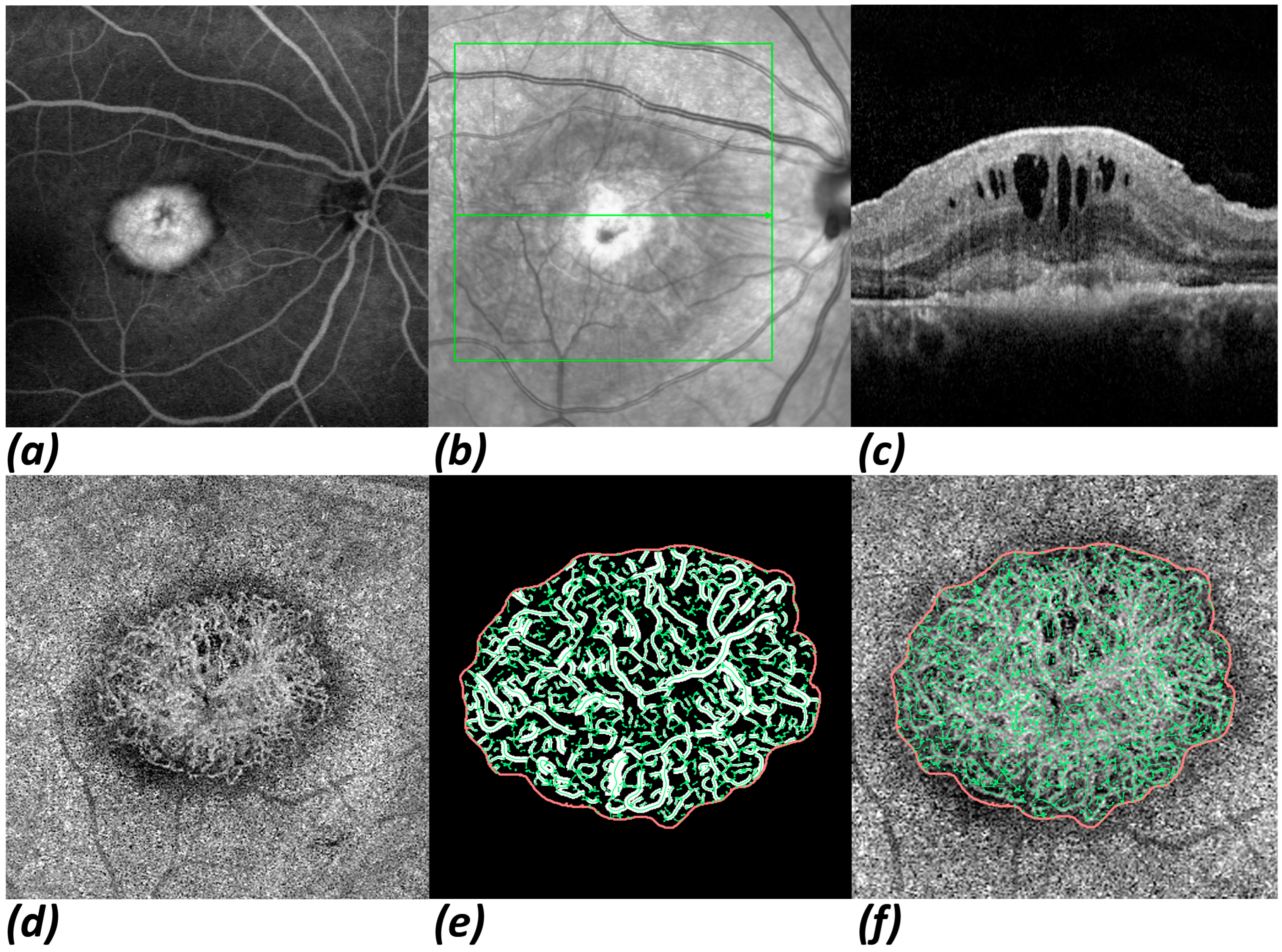
1. Introduction
2. Materials and Methods
2.1. Study Protocol
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| OCT | Optical coherence tomography |
| OCTA | Optical coherence tomography angiography |
| nAMD | Neovascular age-related macular degeneration |
| IVI | Intravitreal injection |
| VEGF | Vascular endothelial growth factor |
| IRF | Intraretinal fluid |
| SRF | Subretinal fluid |
| PED | Pigment epithelium detachment |
| MNV | Macular neovascularization |
| BCVA | Best corrected visual acuity |
| CRT | Central retinal thickness |
| FA | Fluorescence angiography |
| FD | Fractal dimension |
| sumL | Total vessel length |
| IV | Independent variable |
| DV | Dependent variable |
| CT | Choroidal thickness |
| CVI | Choroidal vascularity index |
References
- Li, J.Q.; Welchowski, T.; Schmid, M.; Mauschitz, M.M.; Holz, F.G.; Finger, R.P. Prevalence and incidence of age-related macular degeneration in Europe: A systematic review and meta-analysis. Br. J. Ophthalmol. 2020, 104, 1077. [Google Scholar] [CrossRef] [PubMed]
- Schmidt-Erfurth, U.; Chong, V.; Loewenstein, A.; Michael, L.; Souied, E.; Schlingemann, R.; Eldem, B.; Mones, J.; Richard, G.; Bandello, F.; et al. Guidelines for the management of neovascular age-related macular degeneration by the European Society of Retina Specialists (EURETINA). Br. J. Ophthalmol. 2014, 98, 1144. [Google Scholar] [CrossRef] [PubMed]
- Ketkar, M.; Dave, V.P.; de Ribot, F.M.; Sallam, A.B.; Shettigar, M.P.; Hsieh, Y.-T.; Lai, T.-T.; Soedarman, S.; Liu, L.; Wu, L.; et al. Vitreomacular traction—A review. Eye 2025, 39, 710–717. [Google Scholar] [CrossRef] [PubMed]
- Kal, M.; Winiarczyk, M.; Głuszek, S.; Mackiewicz, J. Choroidal thickness in lamellar macular holes. Graefe’s Arch. Clin. Exp. Ophthalmol. 2021, 259, 653–659. [Google Scholar] [CrossRef]
- Rizzo, C.; Savastano, M.C.; Kilian, R.; Marchini, G.; Rizzo, S. Structural en face optical coherence tomography in neovascular and nonneovascularage-related macular degeneration: Use and utility in clinical practice. Surv. Ophthalmol. 2025, 70, 725–733. [Google Scholar] [CrossRef]
- Limoli, C.; Khalid, H.; Wagner, S.K.; Huemer, J. Retinal Ischemic Perivascular Lesions (RIPLs) as Potential Biomarkers for Systemic Vascular Diseases: A Narrative Review of the Literature. Ophthalmol. Ther. 2025, 14, 1183–1197. [Google Scholar] [CrossRef]
- Bi, Z.; Li, J.; Liu, Q.; Fang, Z. Deep learning-based optical coherence tomography and retinal images for detection of diabetic retinopathy: A systematic and meta analysis. Front. Endocrinol. 2025, 16, 1485311. [Google Scholar] [CrossRef]
- Servillo, A.; Scandale, P.; Oldoni, G.; Begar, P.G.; Bandello, F.; Miserocchi, E.; Cicinelli, M.V. Inflammatory choroidal neovascularization: An evidence-based update. Surv. Ophthalmol. 2025, 70, 451–466. [Google Scholar] [CrossRef]
- Georgiou, M.; Fujinami, K.; Michaelides, M. Retinal imaging in inherited retinal diseases. Ann. Eye Sci. 2020, 5, 25. [Google Scholar] [CrossRef]
- Palmer, L.D.; Thompson, A.C.; Asrani, S. Diagnosing glaucoma progression with optical coherence tomography. Curr. Opin. Ophthalmol. 2025, 36, 130–134. [Google Scholar] [CrossRef]
- Lally, D.R.; Heier, J.S.; Baumal, C.; Witkin, A.J.; Maler, S.; Shah, C.P.; Reichel, E.; Waheed, N.K.; Bussel, I.; Rogers, A.; et al. Expanded spectral domain-OCT findings in the early detection of hydroxychloroquine retinopathy and changes following drug cessation. Int. J. Retina Vitreous 2016, 2, 18. [Google Scholar] [CrossRef] [PubMed]
- Song, A.; Johnson, N.; Ayala, A.; Thompson, A. Optical Coherence Tomography in Patients with Alzheimer’s Disease: What Can It Tell Us? Eye Brain 2021, 13, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Mirmosayyeb, O.; Yazdan Panah, M.; Mokary, Y.; Ghaffary, E.M.; Ghoshouni, H.; Zivadinov, R.; Weinstock-Guttman, B.; Jakimovski, D. Optical coherence tomography (OCT) measurements and disability in multiple sclerosis (MS): A systematic review and meta-analysis. J. Neurol. Sci. 2023, 454, 120847. [Google Scholar] [CrossRef] [PubMed]
- Shahidatul-Adha, M.; Zunaina, E.; Aini-Amalina, M.N. Evaluation of vascular endothelial growth factor (VEGF) level in the tears and serum of age-related macular degeneration patients. Sci. Rep. 2022, 12, 4423. [Google Scholar] [CrossRef]
- Moshtaghion, S.M.M.; Locri, F.; Reyes, A.P.; Plastino, F.; Kvanta, A.; Morillo-Sanchez, M.J.; Rodríguez-de-la-Rúa, E.; Gutierrez-Sanchez, E.; Montero-Sánchez, A.; Lucena-Padros, H.; et al. VEGF in Tears as a Biomarker for Exudative Age-Related Macular Degeneration: Molecular Dynamics in a Mouse Model and Human Samples. Int. J. Mol. Sci. 2025, 26, 3855. [Google Scholar] [CrossRef]
- Coscas, G.; Lupidi, M.; Coscas, F. Image Analysis of Optical Coherence Tomography Angiography. In OCT Angiography in Retinal and Macular Diseases; S.Karger AG: Basel, Switzerland, 2016; pp. 30–36. [Google Scholar]
- Spaide, R.F.; Fujimoto, J.G.; Waheed, N.K.; Sadda, S.R.; Staurenghi, G. Optical coherence tomography angiography. Prog. Retin. Eye Res. 2018, 64, 1–55. [Google Scholar] [CrossRef]
- Laiginhas, R.; Yang, J.; Rosenfeld, P.J.; Falcao, M. Nonexudative Macular Neovascularization—A Systematic Review of Prevalence, Natural History, and Recent Insights from OCT Angiography. Ophthalmol. Retina 2020, 4, 651–661. [Google Scholar] [CrossRef]
- Wang, Y.; Sun, J.; Wu, J.; Jia, H.; Feng, J.; Chen, J.; Yan, Q.; Huang, P.; Wang, F.; Bo, Q.; et al. Growth of nonexudative macular neovascularization in age-related macular degeneration: An indicator of biological lesion activity. Eye 2023, 37, 2048–2054. [Google Scholar] [CrossRef]
- Nakano, Y.; Kataoka, K.; Takeuchi, J.; Fujita, A.; Kaneko, H.; Shimizu, H.; Ito, Y.; Terasaki, H. Vascular maturity of type 1 and type 2 choroidal neovascularization evaluated by optical coherence tomography angiography. PLoS ONE 2019, 14, e0216304. [Google Scholar] [CrossRef]
- Told, R.; Reiter, G.S.; Mittermüller, T.J.; Schranz, M.; Reumueller, A.; Schlanitz, F.G.; Weigert, G.; Pollreisz, A.; Sacu, S.; Schmidt-Erfurth, U. Profiling neovascular age-related macular degeneration choroidal neovascularization lesion response to anti-vascular endothelial growth factor therapy using SSOCTA. Acta Ophthalmol. 2021, 99, e240–e246. [Google Scholar] [CrossRef]
- Leveziel, N.; Joubert, M.; Hermans, M.; Moser, E.; Picard, S.L.; Maurel, F. Quality of Life of Patients Suffering from Exudative Age-Related Macular Degeneration and Treated by Intravitreal Injections and Its Predictors: The Equade Study. Value Health 2013, 16, A509–A510. [Google Scholar] [CrossRef]
- Montero Moreno, J.A.; Arnaiz, C.; Martinez-Perez, L.; de la Fuente, A.; Gonzalez Uruena, C. Impact of intravitreous bevacizumab injections on perceived quality of life in a cohort of patients with exudative age related macular degeneration: Real life results at 4 years. Acta Ophthalmol. 2016, 94. [Google Scholar] [CrossRef]
- Zhang, Q.; Zhang, A.; Lee, C.; Lee, A.Y.; Rezaei, K.A.; Roisman, L.; Miller, A.; Zheng, F.; Gregori, G.; Durbin, M.K.; et al. Projection Artifact Removal Improves Visualization and Quantitation of Macular Neovascularization Imaged by Optical Coherence Tomography Angiography. Ophthalmol. Retina 2016, 1, 124–136. [Google Scholar] [CrossRef] [PubMed]
- Siggel, R.; Spital, C.; Lentzsch, A.; Liakopoulos, S. Comparison of Automated versus Manually Modified OCT Angiography En Face Slabs for Detection of Choroidal Neovascularization. Ophthalmol. Retina 2020, 4, 471–480. [Google Scholar] [CrossRef]
- Parravano, M.; Borrelli, E.; Sacconi, R.; Costanzo, E.; Marchese, A.; Manca, D.; Varano, M.; Bandello, F.; Querques, G. A Comparison Among Different Automatically Segmented Slabs to Assess Neovascular AMD using Swept Source OCT Angiography. Transl. Vis. Sci. Technol. 2019, 8, 8. [Google Scholar] [CrossRef]
- Rothaus, K.; Jiang, X. Multi-scale Midline Extraction Using Creaseness. In Pattern Recognition and Image Analysis; Singh, S., Singh, M., Apte, C., Perner, P., Eds.; Springer: Berlin/Heidelberg, Germany, 2005; pp. 502–511. [Google Scholar]
- Al-Sheikh, M.; Iafe, N.A.; Phasukkijwatana, N.; Sadda, S.R.; Sarraf, D. Biomarkers of neovascular activity in age-related macular degeneration using optical coherence tomography angiography. Retina 2018, 38, 220–230. [Google Scholar] [CrossRef]
- Schmidt-Erfurth, U.; Waldstein, S.M. A paradigm shift in imaging biomarkers in neovascular age-related macular degeneration. Prog. Retin. Eye Res. 2016, 50, 1–24. [Google Scholar] [CrossRef]
- Sagong, M.; Kim, J.H.; Woo, S.J.; Kim, Y.C.; Cho, H.; Lee, Y.H.; Byon, I.; Jo, Y.J.; Chin, H.S.; Kin, J.; et al. Predictors of Disease Activity After Anti-VEGF Treatment for Neovascular Age-Related Macular Degeneration Using Real-World Data from the PROOF Study. Ophthalmol. Ther. 2024, 13, 2839–2853. [Google Scholar] [CrossRef]
- Bogunović, H.; Waldstein, S.M.; Schlegl, T.; Langs, G.; Sadeghipour, A.; Liu, X.; Gerendas, B.S.; Osborne, A.; Schmidt-Erfurth, U. Prediction of Anti-VEGF Treatment Requirements in Neovascular AMD Using a Machine Learning Approach. Investig. Ophthalmol. Vis. Sci. 2017, 58, 3240–3248. [Google Scholar] [CrossRef]
- Simader, C.; Ritter, M.; Bolz, M.; Deak, G.G.; Mayr-Sponer, U.; Golbaz, I.; Kundi, M.; Schmidt-Erfurth, U.M. Morphologic Parameters Relevant for Visual Outcome During Anti-Angiogenic Therapy of Neovascular Age-Related Macular Degeneration. Ophthalmology 2014, 121, 1237–1245. [Google Scholar] [CrossRef]
- Costa, I.; Andrade, H.; Pereira, B.; Camacho, P. Neurodegeneration and choroidal vascular features on OCT in the progression to advanced age-related macular degeneration. Int. J. Ophthalmol. 2025, 18, 103–110. [Google Scholar] [CrossRef] [PubMed]
- Sadeghi, E.; Valsecchi, N.; Rahmanipour, E.; Ejlalidiz, M.; Hasan, N.; Vupparaboina, K.K.; Ibrahim, M.N.; Rasheed, M.A.; Baek, J.; Iannetta, D.; et al. Choroidal biomarkers in age-related macular degeneration. Surv. Ophthalmol. 2025, 70, 167–183. [Google Scholar] [CrossRef]
- Koizumi, H.; Kano, M.; Yamamoto, A.; Saito, M.; Maruko, I.; Kawasaki, R.; Sekiryu, T.; Okada, A.A.; Iida, T. Short-Term Changes in Choroidal Thickness After Aflibercept Therapy for Neovascular Age-Related Macular Degeneration. Am. J. Ophthalmol. 2015, 159, 627–633.e1. [Google Scholar] [CrossRef]
- Lee, J.Y.; Folgar, F.A.; Maguire, M.G.; Ying, G.; Toth, C.A.; Martin, D.F.; Jaffe, G.J. Outer Retinal Tubulation in the Comparison of Age-Related Macular Degeneration Treatments Trials (CATT). Ophthalmology 2014, 121, 2423–2431. [Google Scholar] [CrossRef]
- Tao, L.W.; Wu, Z.; Guymer, R.H.; Luu, C.D. Ellipsoid zone on optical coherence tomography: A review. Clin. Exp. Ophthalmol. 2016, 44, 422–430. [Google Scholar] [CrossRef]
- Sacconi, R.; Sarraf, D.; Garrity, S.; Freund, K.B.; Yannuzzi, L.A.; Gal-Or, L.; Souied, E.; Sieiro, A.; Corbellli, E.; Carnevali, A.; et al. Nascent Type 3 Neovascularization in Age-Related Macular Degeneration. Ophthalmol. Retina 2018, 2, 1097–1106. [Google Scholar] [CrossRef]
- Monge, M.; Araya, A.; Wu, L. Subretinal drusenoid deposits: An update. Taiwan J. Ophthalmol. 2022, 12, 138–146. [Google Scholar] [CrossRef]
- El Ameen, A.; Cohen, S.Y.; Semoun, O.; Miere, A.; Srour, M.; Maftouh, M.Q.; Oubraham, H.; Blanco-Garavito, R.; Querques, G.; Souied, E.H. Type 2 neovascularization secondary to age-related macular degeneration imaged by optical coherence tomography angiography. Retina 2015, 35, 2212–2218. [Google Scholar] [CrossRef]
- Faatz, H.; Gunnemann, M.-L.; Rothaus, K.; Book, M.; Gutfleisch, M.; Lommatzsch, A.; Pauleikhoff, D. Einfluss der CNV-Gefäßmorphologie bei exsudativer altersabhängiger Makuladegeneration auf die Visusentwicklung und den Anti-VEGF-Therapiebedarf nach 1 Jahr. Ophthalmologe 2021, 118, 154–161. [Google Scholar] [CrossRef]
- Faghihi, S.; Faghihi, H.; Bazvand, F.; Bahar, M.M.; Torkashvand, A.; Ahmed, A.H.; Rahimi, M.; Akbarzadeh, A.; Khameneh, E.A.; Pour, E.K.; et al. Baseline optical coherence tomography angiography biomarkers predict visual outcomes in treatment-naïve neovascular age-related macular degeneration patients. Sci. Rep. 2024, 14, 24528. [Google Scholar] [CrossRef]
- Faatz, H.; Rothaus, K.; Ziegler, M.; Book, M.; Lommatzsch, C.; Spital, G.; Gutfleisch, M.; Pauleikhoff, D.; Lommatzsch, A. Quantitative Comparison of the Vascular Structure of Macular Neovascularizations Between Swept-Source and Spectral-Domain Optical Coherence Tomography Angiography. Clin. Ophthalmol. 2020, 14, 3179–3186. [Google Scholar] [CrossRef] [PubMed]
- Coscas, F.; Cabral, D.; Pereira, T.; Geraldes, C.; Narotamo, H.; Miere, A.; Lupidi, M.; Sellam, A.; Papoila, A.; Coscas, G.; et al. Quantitative optical coherence tomography angiography biomarkers for neovascular age-related macular degeneration in remission. PLoS ONE 2018, 13, e0205513. [Google Scholar] [CrossRef] [PubMed]
- Choi, W.; Moult, E.M.; Waheed, N.K.; Adhi, M.; Lee, B.; Lu, C.D.; de Carlo, T.E.; Jayaraman, V.; Rosenfeld, P.J.; Duker, J.S.; et al. Ultrahigh-Speed, Swept-Source Optical Coherence Tomography Angiography in Nonexudative Age-Related Macular Degeneration with Geographic Atrophy. Ophthalmology 2015, 122, 2532–2544. [Google Scholar] [CrossRef] [PubMed]
| Age | 77.9 ± 7.1 Years (n = 96) |
| Gender | Male 33.3% (n = 32), Female 66.7% (n = 64) |
| Laterality | Right eye 55.2% (n = 53), left eye 44.8% (n = 43) |
| MNV type | Type 1 49.0% (n = 47), type 2 30.2% (n = 29), type 3 20.8% (n = 20) |
| BCVA (logMAR) Baseline At 1 year | 0.58 ± 0.33 (n = 96) 0.54 ± 0.40 (n = 96) |
| Number of IVIs at 1 year | 8.26 ± 2.92 (n = 96) |
| Unit | n | Beta | 95% CI | p Value | |
|---|---|---|---|---|---|
| OCT parameters | |||||
| CRT | |||||
| baseline | 200 µm | 96 | 0.110 | [0.021; 0.198] | <0.05 |
| after upload | 200 µm | 94 | 0.165 | [0.043; 0.287] | <0.01 |
| decrease during upload | 10% | 94 | −0.035 | [−0.064; −0.005] | <0.05 |
| PED | |||||
| presence at baseline | present | 96 | 0.116 | [−0.052; 0.283] | 0.179 |
| height at baseline | 200 µm | 96 | 0.072 | [−0.007; 0.150] | 0.078 |
| presence after upload | present | 94 | 0.001 | [−0.159; 0.161] | 0.988 |
| height after upload | 200 µm | 94 | 0.079 | [−0.027; 0.185] | 0.148 |
| height decrease during upload | 10% | 61 | −0.001 | [−0.021; 0.020] | 0.937 |
| IRF after upload | present | 93 | 0.125 | [−0.132; 0.383] | 0.343 |
| SRF after upload | present | 93 | 0.111 | [−0.101; 0.322] | 0.309 |
| IRF and SRF after upload | present | 93 | 0.104 | [−0.192; 0.399] | 0.493 |
| OCTA parameters | |||||
| MNV area | 1 mm | 80 | 0.096 | [0.050; 0.142] | <0.01 |
| MNV total vessel length | 20 mm | 80 | 0.153 | [0.074; 0.232] | <0.01 |
| MNV flow density | 10% | 80 | −0.098 | [−0.275; 0.078] | 0.279 |
| MNV fractal dimension | 80 | 1.017 | [0.403; 1.631] | <0.01 |
| Unit | n | Beta | 95% CI | p Value | |
|---|---|---|---|---|---|
| OCT parameters | |||||
| CRT | |||||
| baseline | 200 µm | 96 | 0.493 | [−0.166; 1.152] | 0.145 |
| after upload | 200 µm | 94 | 1.741 | [0.864; 2.619] | <0.01 |
| decrease during upload | 10% | 94 | −0.346 | [−0.562; −0.130] | <0.01 |
| PED | |||||
| presence at baseline | present | 96 | 1.413 | [0.211; 2.614] | <0.05 |
| height at baseline | 200 µm | 96 | 0.833 | [0.275; 1.391] | <0.01 |
| presence after upload | present | 94 | 2.502 | [1.419; 3.584] | <0.01 |
| height after upload | 200 µm | 94 | 1.851 | [1.143; 2.559] | <0.01 |
| height decrease during upload | 10% | 61 | −0.295 | [−0.435; −0.154] | <0.01 |
| IRF after upload | present | 93 | 3.028 | [1.614; 4.441] | 0.175 |
| SRF after upload | present | 93 | 1.205 | [−0.516; 2.925] | <0.01 |
| IRF and SRF after upload | present | 93 | 3.375 | [1.403; 5.347] | <0.01 |
| OCTA parameters | |||||
| MNV area | 1 mm | 80 | 0.193 | [−0.162; 0.549] | 0.290 |
| MNV total vessel length | 20 mm | 80 | 0.397 | [−0.204; 0.998] | 0.199 |
| MNV flow density | 10% | 80 | −0.819 | [−2.067; 0.430] | 0.202 |
| MNV fractal dimension | 80 | 5.037 | [0.540; 9.534] | <0.05 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grün, M.; Rothaus, K.; Ziegler, M.; Lommatzsch, A.; Lange, C.; Faatz, H. Morphology of Macular Neovascularization in Age-Related Macular Degeneration Influences Treatment Requirement and Visual Outcome After 1 Year. J. Pers. Med. 2025, 15, 246. https://doi.org/10.3390/jpm15060246
Grün M, Rothaus K, Ziegler M, Lommatzsch A, Lange C, Faatz H. Morphology of Macular Neovascularization in Age-Related Macular Degeneration Influences Treatment Requirement and Visual Outcome After 1 Year. Journal of Personalized Medicine. 2025; 15(6):246. https://doi.org/10.3390/jpm15060246
Chicago/Turabian StyleGrün, Michael, Kai Rothaus, Martin Ziegler, Albrecht Lommatzsch, Clemens Lange, and Henrik Faatz. 2025. "Morphology of Macular Neovascularization in Age-Related Macular Degeneration Influences Treatment Requirement and Visual Outcome After 1 Year" Journal of Personalized Medicine 15, no. 6: 246. https://doi.org/10.3390/jpm15060246
APA StyleGrün, M., Rothaus, K., Ziegler, M., Lommatzsch, A., Lange, C., & Faatz, H. (2025). Morphology of Macular Neovascularization in Age-Related Macular Degeneration Influences Treatment Requirement and Visual Outcome After 1 Year. Journal of Personalized Medicine, 15(6), 246. https://doi.org/10.3390/jpm15060246







