Abstract
Background: The emergency department (ED) is often overburdened, due to the high influx of patients and limited availability of attending physicians. This situation highlights the need for improvement in the management of, and assistance provided in the ED. A key point for this purpose is the identification of patients with the highest risk, which can be achieved using machine learning predictive models. The objective of this study is to conduct a systematic review of predictive models used to detect ward admissions from the ED. The main targets of this review are the best predictive algorithms, their predictive capacity, the studies’ quality, and the predictor variables. Methods: This review is based on PRISMA methodology. The information has been searched in PubMed, Scopus and Google Scholar databases. Quality assessment has been performed using the QUIPS tool. Results: Through the advanced search, a total of 367 articles were found, of which 14 were of interest that met the inclusion criteria. Logistic regression is the most used predictive model, achieving AUC values between 0.75–0.92. The two most used variables are the age and ED triage category. Conclusions: artificial intelligence models can contribute to improving the quality of care in the ED and reducing the burden on healthcare systems.
1. Introduction
The emergency department (ED) is a demanding and stressful environment for healthcare workers, due to the large number of patients and limited physicians’ availability. Overcrowding affects overall health and the functioning of the healthcare system [1]. Therefore, early identification of patients at higher risk of admission is necessary to improve outcomes and reduce the burden on healthcare systems.
In the systematic review by Maninchedda et al. [2], the main strategies and control features to reduce ED overcrowding are mentioned. The characteristics were divided into five groups: organization of work, investment in primary care, creation of new dedicated professional figures, labour, and structural modifications and implementation of predictive simulation models using mathematical algorithms. As for mathematical algorithms, in the last few years, the usage of machine learning and deep learning techniques in medicine has increased exponentially [3]. Such predictive models are clinically beneficial for understanding or identifying clinical patterns or potential risk situations in real time [4].
In the context of the ED, it is necessary to detect critical patients more accurately. The most advanced detection can be achieved with the support of artificial-intelligence (AI)-based predictive models at the time of triage. This would help in resources management and forecasting, as well as improving patient care and reducing physician overload. When looking for predictive models for ED, many studies focus on predicting the risk of ED admission. In fact, in 2010, Brabrand et al. presented a systematic review of risk score predictive models for adults admitted to the ED [5]. In 2013, Wallace et al. [6] presented a systematic review of the probability of repeat admission in community-dwelling adults, and in 2014, Wallace et al. [7] presented a systematic review of risk prediction models to predict emergency hospital admission in community-dwelling adults. In the most recent years (2021, 2022 and 2023), several systematic reviews have been presented on prediction models for admissions [8,9,10,11,12]. Hence, there are multiple studies focused on predicting patients’ risk scores when admitted to the ED or hospital.
However, to the best of our knowledge, there is no systematic review to predict ward admissions when a patient is already in the ED to manage best the patients and hospital resources in advance. Therefore, the aim of this study is to perform a systematic review to analyze the existing predictive models of ward admission from the ED. Specific objectives are: (1) to examine the variables included in ward admission prediction models, (2) to summarize the algorithms and performance of these admission predictive models; and (3) to validate the quality of the identified studies.
2. Methods
This review is presented according to PRISMA methodology [13]. This methodology can be summarized in four steps: search strategy, article selection, exclusion and inclusion criteria for data extraction and, if necessary, statistical analysis or quality assessment.
2.1. Search Strategy
To identify the research papers for the conducted systematic review we used PICO methodology [14]. Specifically, we searched the bibliographic databases of Scopus, PubMed, and Google Scholar in January of 2023. The PICO methodology involves defining the patient population (P), the intervention or exposure of interest (I), the comparison group (C), and the outcome of interest (O). By using this methodology, we were able to systematically search for articles that met our predefined criteria.
2.2. Study Selection
Studies were included if they met the following criteria:
- Population: Patients presenting to the emergency department
- Intervention: prediction models for ward admissions in the hospital from emergency department patients
- Comparison: not applicable
- Outcome: patient admission
The criteria are specified in more detail in the following Table 1, where the keywords are summarized.

Table 1.
PICO methodology applied for this study.
After selecting the most significant words, with the aim of providing a complete overview of the available prediction models, the search was limited to 2010 to 2023, in addition to looking for articles written in English or Spanish. The search only focused on the titles, since a more general search of title, abstract, and text provided too many results, so it was decided to narrow the search by focusing on article titles. The titles of the articles did not mention the population of interest, so it was not included in the search but was later considered for the inclusion and exclusion criteria (see Section 2.3. Data Extraction). In addition, a selection of the keywords mentioned in Table 2 was created. For the search, we used the mentioned bibliographic databases with the search strings shown in Table 2.

Table 2.
Search strings.
2.3. Data Extraction
After automatic article selection, duplicate articles were eliminated. Next, the titles and abstracts of each of the non-duplicate articles were analyzed. Studies that did not meet the established criteria were discarded. Then we proceeded to read the selected articles, analyzing them again with the same criteria mentioned above.
Studies that met any of these criteria were excluded:
- Predictive models for hospital readmission.
- Primary population of interest focused on specific conditions (e.g., asthma or bronchiolitis).
- The model predicts whether a patient will be admitted in the future or requires post-triage data.
- Only provided risk factors evaluation and did not build a prediction model.
- Models that do not answer the specific question, i.e.,do not predict ward admission from the emergency department.
- Published in languages other than English and Spanish.
- Full article not available.
After selecting the studies of interest, a PRISMA diagram was built to summarize the whole process and to describe in a visual way the selection or exclusion of the studies step by step, keeping the articles of interest (see Figure 1).
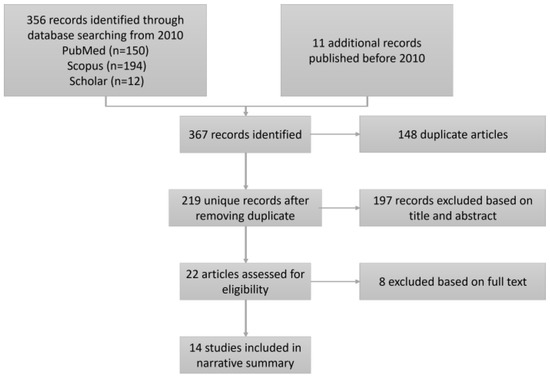
Figure 1.
PRISMA Flow Diagram of Included Hospital Admission Prediction Models from the Emergency Department.
2.4. Methodological Quality Assessment
A methodological quality assessment of the included studies was independently performed using the QUIPS tool [15] to assess the risk of bias in systematic reviews. QUIPS consists of summarizing the risks of the studies in six different domains: study participation, study attrition, prognostic factor measurement, outcome measurement, study confounding, and statistical analysis and reporting.
As a result of each of these criteria, QUIPS has a final score, named overall risk, risk of bias, or quality of evidence. It refers to the degree to which the results of a study may be reliable or generalizable to the target population. It is determined by assessing the risk of various types of biases or limitations in study design and execution. A study with a high overall risk suggests that the study results may not accurately reflect the truth, whereas a study with a low overall risk suggests that the study results are more reliable and trustworthy.
3. Results
In this section all the results will be presented using the methodology mentioned in the previous section.
3.1. Study Identification
This systematic review found a total of 367 possible articles, reducing them to 14 studies at the end of the process (Figure 1). The total of 367 articles was obtained from PubMed (n = 150), Scopus (n = 194), Google Scholar (n = 12), and other search sites other than the above (n = 11).
As seen in Figure 1, after the automatic search, the reviewer eliminated the duplicate articles, leaving 219 articles. Next, after analyzing the titles and abstracts of each of the unduplicated articles, 197 studies were discarded, and 22 studies were obtained for further analysis.
Following the same exclusion criteria, the full texts of the remaining 22 studies were analyzed and six of the 22 articles were discarded, resulting in a final 14 relevant studies. These 14 studies were examined one by one. Table 3 summarizes the most relevant data for each of them.

Table 3.
Hospital Admission Prediction Models from the Emergency Department.
3.2. Description of Included Studies
Of the 14 final articles, three were developed in Spain [17,22,23], three in the Netherlands [18,24,27], two in Greece [19,26], two in the U.K. [21,28], two in the USA [16,20], one in France [29], and 1 in Singapore [25]. Eleven of the 14 articles included as a patient any person attending the emergency department. The remaining articles (n = 3) have some restriction on the population of the study: one excludes ED patients older than 70 years old [24]; one considers only patients older than 18 years and creates two groups of patients with the threshold of 70 years (younger and older than 70 years) [27]; and the third article [17] includes adult patients who were stable on arrival at the ED. Sample sizes ranged from 2476 [17] to 3,189,204 [22] emergency department visits. The percentage of ward admissions from the total instances ranged from 4.6% [17] to 39% [18].
The most commonly used algorithm was logistic regression, with seven out of 14 articles using it [16,17,24,25,27,28,29]. The second most used model was gradient boosting, in three studies [20,21,22]. Other studies used Random forest [19], Gaussian Naïve Bayes [26], gradient-powered decision tree modelling [18], and an artificial neural network [23]. All models predict ward admission from the ED, either giving a binary or probabilistic response.
3.3. Variables Used to Develop Predictive Models
Continuing with the variables used in the articles, the number of variables used varied from six variables [18] to 21 variables [16]. All the articles used hospital variables, either clinical or triage variables. In three studies, the variables were not exactly specified [18,20,21]. The following Table 4 summarizes the variables in six categories: demographics, triage information, clinical and laboratory findings, medical history, medication, and others.

Table 4.
Variables used in each study.
As presented in Table 4, all studies used a triage data category. One study [21] emphasized that the triage category is one of the most important factors in the prediction of admission. In 11 of the 14 articles [16,17,19,21,22,23,25,26,27,28,29], a demographic category was used, and within this category, the age variable was used in all 11 studies. Four of these articles distinguish age as a good predictor of hospital admission [16,17,21,25]. Clinical and laboratory findings is the third most used category: nine articles out of 14 have used variables from that category [17,18,19,20,21,22,23,24,26,27]. Laboratory data were used extensively, with five out of nine studies using it [18,19,24,26,27]. Vital signs variables have been used in three out of nine [18,24,27] studies. In six studies, variables from the medical history have been used [21,22,23,25,27,28]. One of them determines that previous admission in the last month and previous admission in the last year are good predictors of hospital admission [21]. In one study, medications have been incorporated [17]. Finally, nine studies use other variables that do not correspond to these categories [16,19,21,23,25,26,27,28,29]. Of these unclassified variables, the mode of arrival at the emergency department is the most common one. According to one article, this variable is a good predictor [16].
3.4. Predictiveness of Models
The results of the 14 studies analyzed were presented using the AUC metric, which measures the separability of the classes in a classification problem (Table 5). In most of the articles, the 95% confidence interval (CI) was calculated to provide a range in which the model is estimated to perform with a 95% probability. The larger the range, the greater the uncertainty. The study with the best result was [20], conducted in the USA, which obtained an AUC of 0.92 (95% CI 0.92–0.93). In second place was article [22], conducted in Spain, which obtained an AUC of 0.8938 (95% CI 0.8929–0.8948). In third place was study [28], also conducted in the USA, which obtained an AUC of 0.8774 (95% CI 0.8752–0.8796).

Table 5.
Summarization of the results.
3.5. Methodological Quality Assessment
Using the QUIPS tool, a quality assessment of the 14 studies has been carried out. Table 6 summarizes the risk level for each QUIPS section, where:
 : means low risk of bias
: means low risk of bias : means moderate risk of bias
: means moderate risk of bias : means high risk of bias
: means high risk of bias

Table 6.
Risk of the selected studies using the QUIPS tool.
Table 6.
Risk of the selected studies using the QUIPS tool.
| Reference | Study Participation | Study Attrition | Prognostic Factor | Outcome | Study Confounding | Statistical Analysis and Reporting | Overall Risk of Bias |
|---|---|---|---|---|---|---|---|
| Parker et al. [16] |  |  |  |  |  |  |  |
| Elvira Martínez et al. [17] |  |  |  |  |  |  |  |
| De Hond, Anne et al. [18] |  |  |  |  |  |  |  |
| Feretzakis, Georgios et al. [19] |  |  |  |  |  |  |  |
| Hong, Woo Suk et al. [20] |  |  |  |  |  |  |  |
| Graham, B et al. [21] |  |  |  |  |  |  |  |
| Cusidó, J et al. [22] |  |  |  |  |  |  |  |
| Alexander Zlotnik et al. [23] |  |  |  |  |  |  |  |
| A. Brink et al. [24] |  |  |  |  |  |  |  |
| Sun, Yan et al. [25] |  |  |  |  |  |  |  |
| Feretzakis, Georgios et al. [26] |  |  |  |  |  |  |  |
| Lucke, Jacinta A et al. [27] |  |  |  |  |  |  |  |
| Allan Cameron et al. [28] |  |  |  |  |  |  |  |
| Noel, Guilhem el al. [29] |  |  |  |  |  |  |  |
After analyzing all the articles, the overall risk is low, since the high risk indicator does not appear in any of the articles. Figure 2 presents the risk factor of each domain for the selected articles of the review.
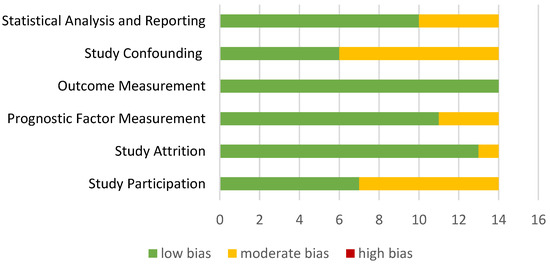
Figure 2.
Summary of methodogical analysis.
Most studies were able to report all QUIPS checklist items, except for the “Study Confounding” and “Study Participation” domains. This suggests that the studies included in this review had a low risk of bias, but it is important to consider the potential impact of “confounding variables” and “Study Participation”.
4. Discussion
This systematic review identified 14 studies that developed machine learning models for predicting hospital admissions from the ED. The number of variables used is very varied, since there are studies that use a small number of variables and others that use more than 20 variables. Most of the articles analyzed (n = 11) used data from all patients in the ED to develop their models, while a few had restrictions on the population studied. Specifically, three articles had such restrictions: one excluded patients over 70 years old [24], one focused only on patients over 18 years and created two groups based on the threshold of 70 years [27], and the third one included stable adult patients upon arrival to the ED [17]. In terms of variables, the review identified several factors that consistently predicted patient admission, such as age, mode of arrival, and the triage category. It was found that the most used models for this type of prediction are logistic regression and gradient boosting, since 10 out of 14 articles used either one of these two, although the most widely used is logistic regression, with seven out of 14 articles using it. Overall, the findings suggest that these models can be effective in accurately predicting patient ward admission, with many studies reporting good relationships between sensitivity and specificity. The article with the best result presented an AUC of 0.92 [95% CI 0.92–0.93] [20], and the article with the worst result presented an AUC of 0.766 (95% CI 0.759–0.781) [24].
Five out of the 14 articles have been published in the last three years, which shows that artificial intelligence is increasingly used in health services, more specifically in the ED.
No other systematic reviews of models predicting ward admission from the ED have been found. Therefore, this study cannot be compared with any other systematic review.
5. Conclusions
To date, the logistic regression algorithm is the most widely used to predict hospital ward admission from the emergency department. Although the predictive models found by this systematic review do not use environmental variables, Diaz et al. [30] observed that some environmental variables have a good relationship with ED admission. Hence, non-clinical variables should be considered when developing such models. None of the studies described implementation, and to our knowledge, none of the models are currently implemented in the ED as a prediction tool for hospital ward admission.
These predictive models improve the quality of the emergency department, including better internal management, since, by predicting the number of admissions, better resources management can be carried out.
Author Contributions
Conceptualization, L.A. and N.L.; methodology, L.A. and N.L.; formal analysis, L.A.; investigation, L.A.; resources, L.A. and N.L.; data curation, L.A.; writing—original draft preparation, L.A.; writing—review and editing, L.A., N.L. and J.K.; visualization, L.A., N.L. and J.K.; supervision, N.L.; project administration, N.L.; funding acquisition, N.L. All authors have read and agreed to the published version of the manuscript.
Funding
This work has been partially funded by the research project INURGE (ZL-2022/00571) of the Basque Government’s HAZITEK programme from the public agency SPRI.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Research Ethics Committee of the Gipuzkoa Health Area (protocol code SAMURG-2022-01, 6 February 2023).
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
The authors would like to thank INVIZA-Asunción Klinika and STT Systems for their support in the project.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Savioli, G.; Ceresa, I.F.; Gri, N.; Bavestrello Piccini, G.; Longhitano, Y.; Zanza, C.; Piccioni, A.; Esposito, C.; Ricevuti, G.; Bressan, M.A. Emergency Department Overcrowding: Understanding the Factors to Find Corresponding Solutions. J. Pers. Med. 2022, 12, 279. [Google Scholar] [CrossRef] [PubMed]
- Maninchedda, M.; Proia, A.S.; Bianco, L.; Aromatario, M.; Orsi, G.B.; Napoli, C. Main Features and Control Strategies to Reduce Overcrowding in Emergency Departments: A Systematic Review of the Literature. Risk Manag. Healthc. Policy 2023, 16, 255–266. [Google Scholar] [CrossRef] [PubMed]
- Mueller, B.; Kinoshita, T.; Peebles, A.; Graber, M.A.; Lee, S. Artificial intelligence and machine learning in emergency medicine: A narrative review. Acute Med. Surg. 2022, 9, e740. [Google Scholar] [CrossRef] [PubMed]
- Briganti, G.; Le Moine, O. Artificial Intelligence in Medicine: Today and Tomorrow. Front. Med. 2020, 7, 27. [Google Scholar] [CrossRef]
- Brabrand, M.; Folkestad, L.; Clausen, N.G.; Knudsen, T.; Hallas, J. Risk scoring systems for adults admitted to the emergency department: A systematic review. Scand. J. Trauma Resusc. Emerg. Med. 2010, 18, 8. [Google Scholar] [CrossRef]
- Wallace, E.; Hinchey, T.; Dimitrov, B.D.; Bennett, K.; Fahey, T.; Smith, S.M. A Systematic Review of the Probability of Repeated Admission Score in Community-Dwelling Adults. J. Am. Geriatr. Soc. 2013, 61, 357–364. [Google Scholar] [CrossRef]
- Wallace, E.; Stuart, E.; Vaughan, N.; Bennett, K.; Fahey, T.; Smith, S.M. Risk Prediction Models to Predict Emergency Hospital Admission in Community-dwelling Adults. Med. Care 2014, 52, 751–765. [Google Scholar] [CrossRef]
- Jiang, S.; Liu, Q.; Ding, B. A systematic review of the modelling of patient arrivals in emergency departments. Quant. Imaging Med. Surg. 2023, 13, 1957–1971. [Google Scholar] [CrossRef]
- Monahan, A.C.; Feldman, S.S. Models predicting hospital admission of adult patients utilizing prehospital data: Systematic review using PROBAST and CHARMS. JMIR Med. Inform. 2021, 9, e30022. [Google Scholar] [CrossRef]
- Silva, E.; Pereira, M.F.; Vieira, J.T.; Ferreira-Coimbra, J.; Henriques, M.; Rodrigues, N.F. Predicting hospital emergency department visits accurately: A systematic review. Int. J. Health Plann. Manag. 2023, 1–14. [Google Scholar] [CrossRef]
- Brink, A.; Alsma, J.; van Attekum, L.A.; Bramer, W.M.; Zietse, R.; Lingsma, H.; Schuit, S.C. Predicting inhospital admission at the emergency department: A systematic review. Emerg. Med. J. 2022, 39, 191–198. [Google Scholar] [CrossRef]
- Sánchez-Salmerón, R.; Gómez-Urquiza, J.L.; Albendín-García, L.; Correa-Rodríguez, M.; Martos-Cabrera, M.B.; Velando-Soriano, A.; Suleiman-Martos, N. Machine learning methods applied to triage in emergency services: A systematic review. Int. Emerg. Nurs. 2022, 60, 101109. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. Ann. Intern. Med. 2009, 151, 264–269. Available online: https://www.acpjournals.org/doi/10.7326/0003-4819-151-4-200908180-00135 (accessed on 14 April 2023). [CrossRef] [PubMed]
- Santos, C.M.d.C.; Pimenta, C.A.d.M.; Nobre, M.R.C. The PICO strategy for the research question construction and evidence search. Rev. Lat. Am. Enferm. 2007, 15, 508–511. [Google Scholar] [CrossRef] [PubMed]
- Hayden, J.A.; van der Windt, D.A.; Cartwright, J.L.; Côté, P.; Bombardier, C. Assessing Bias in Studies of Prognostic Factors. Ann. Intern. Med. 2013, 158, 280–286. [Google Scholar] [CrossRef]
- Parker, C.A.; Liu, N.; Wu, S.X.; Shen, Y.; Lam, S.S.W.; Ong, M.E.H. Predicting hospital admission at the emergency department triage: A novel prediction model. Am. J. Emerg. Med. 2019, 37, 1498–1504. [Google Scholar] [CrossRef]
- Martínez, C.M.E.; Fernández, C.; Del Castillo, J.G.; Armengol, J.J.G.; Villarroel, P.; Sánchez, F.J.M. Prediction model for in-hospital admission in patients arriving in the emergency department. An. Sist. Sanit. Navar. 2012, 35, 207–217. [Google Scholar] [CrossRef]
- De Hond, A.; Raven, W.; Schinkelshoek, L.; Gaakeer, M.; Ter Avest, E.; Sir, O.; Lameijer, H.; Hessels, R.A.; Reijnen, R.; De Jonge, E.; et al. Machine learning for developing a prediction model of hospital admission of emergency department patients: Hype or hope? Int. J. Med. Inform. 2021, 152, 104496. [Google Scholar] [CrossRef]
- Feretzakis, G.; Karlis, G.; Loupelis, E.; Kalles, D.; Chatzikyriakou, R.; Trakas, N.; Karakou, E.; Sakagianni, A.; Tzelves, L.; Petropoulou, S.; et al. Using Machine Learning Techniques to Predict Hospital Admission at the Emergency Department. J. Crit. Care Med. 2022, 8, 107–116. [Google Scholar] [CrossRef]
- Hong, W.S.; Haimovich, A.D.; Taylor, R.A. Predicting hospital admission at emergency department triage using machine learning. PLoS ONE 2018, 13, e0201016. [Google Scholar] [CrossRef]
- Graham, B.; Bond, R.; Quinn, M.; Mulvenna, M. Using Data Mining to Predict Hospital Admissions From the Emergency Department. IEEE Access 2018, 6, 10458–10469. [Google Scholar] [CrossRef]
- Cusidó, J.; Comalrena, J.; Alavi, H.; Llunas, L. Predicting Hospital Admissions to Reduce Crowding in the Emergency Departments. Appl. Sci. 2022, 12, 10764. [Google Scholar] [CrossRef]
- Zlotnik, A.; Alfaro, M.C.; Pérez, M.C.P.; Gallardo-Antolín, A.; Martínez, J.M.M. Building a Decision Support System for Inpatient Admission Prediction With the Manchester Triage System and Administrative Check-in Variables. CIN Comput. Inform. Nurs. 2016, 34, 224. [Google Scholar] [CrossRef] [PubMed]
- Brink, A.; Alsma, J.; Brink, H.S.; De Gelder, J.; Lucke, J.A.; Mooijaart, S.P.; Zietse, R.; Schuit, S.C.E.; Lingsma, H.F. Prediction admission in the older population in the Emergency Department: The CLEARED tool. Neth. J. Med. 2020, 78, 357–367. [Google Scholar]
- Sun, Y.; Heng, B.H.; Tay, S.Y.; Seow, E. Predicting hospital admissions at emergency department triage using routine administrative data. Acad. Emerg. Med. Off. J. Soc. Acad. Emerg. Med. 2011, 18, 844–850. [Google Scholar] [CrossRef] [PubMed]
- Feretzakis, G.; Sakagianni, A.; Loupelis, E.; Karlis, G.; Kalles, D.; Tzelves, L.; Chatzikyriakou, R.; Trakas, N.; Petropoulou, S.; Tika, A.; et al. Predicting Hospital Admission for Emergency Department Patients: A Machine Learning Approach. Stud. Health Technol. Inform. 2022, 289, 297–300. [Google Scholar] [CrossRef]
- Lucke, J.A.; de Gelder, J.; Clarijs, F.; Heringhaus, C.; de Craen, A.J.M.; Fogteloo, A.J.; Blauw, G.J.; de Groot, B.; Mooijaart, S.P. Early prediction of hospital admission for emergency department patients: A comparison between patients younger or older than 70 years. Emerg. Med. J. 2017, 35, 18–27. [Google Scholar] [CrossRef]
- Cameron, A.; Rodgers, K.; Ireland, A.; Jamdar, R.; McKay, G.A. A simple tool to predict admission at the time of triage. Emerg. Med. J. 2015, 32, 174–179. [Google Scholar] [CrossRef]
- Noel, G.; Bonte, N.; Persico, N.; Bar, C.; Luigi, S.; Roch, A.; Michelet, P.; Gentile, S.; Viudesa, G. Real-time estimation of inpatient beds required in emergency departments. Eur. J. Emerg. Med. 2019, 26, 440–445. [Google Scholar] [CrossRef] [PubMed]
- Díaz, J.; Alberdi, J.C.; Pajares, M.S.; López, C.; López, R.; Lage, M.B.; Otero, A. A model for forecasting emergency hospital admissions: Effect of environmental variables. J. Environ. Health 2001, 64, 9–15. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).