Diagnostic Accuracy of Electrodiagnostic Comparative Latency Studies of Carpal Tunnel Syndrome: Single Test and Concordance Between Multiple Tests
Abstract
1. Introduction
2. Methods
2.1. Study Design and Participants
2.2. Definitions of Variables
2.3. Electrodiagnostic Data Collection
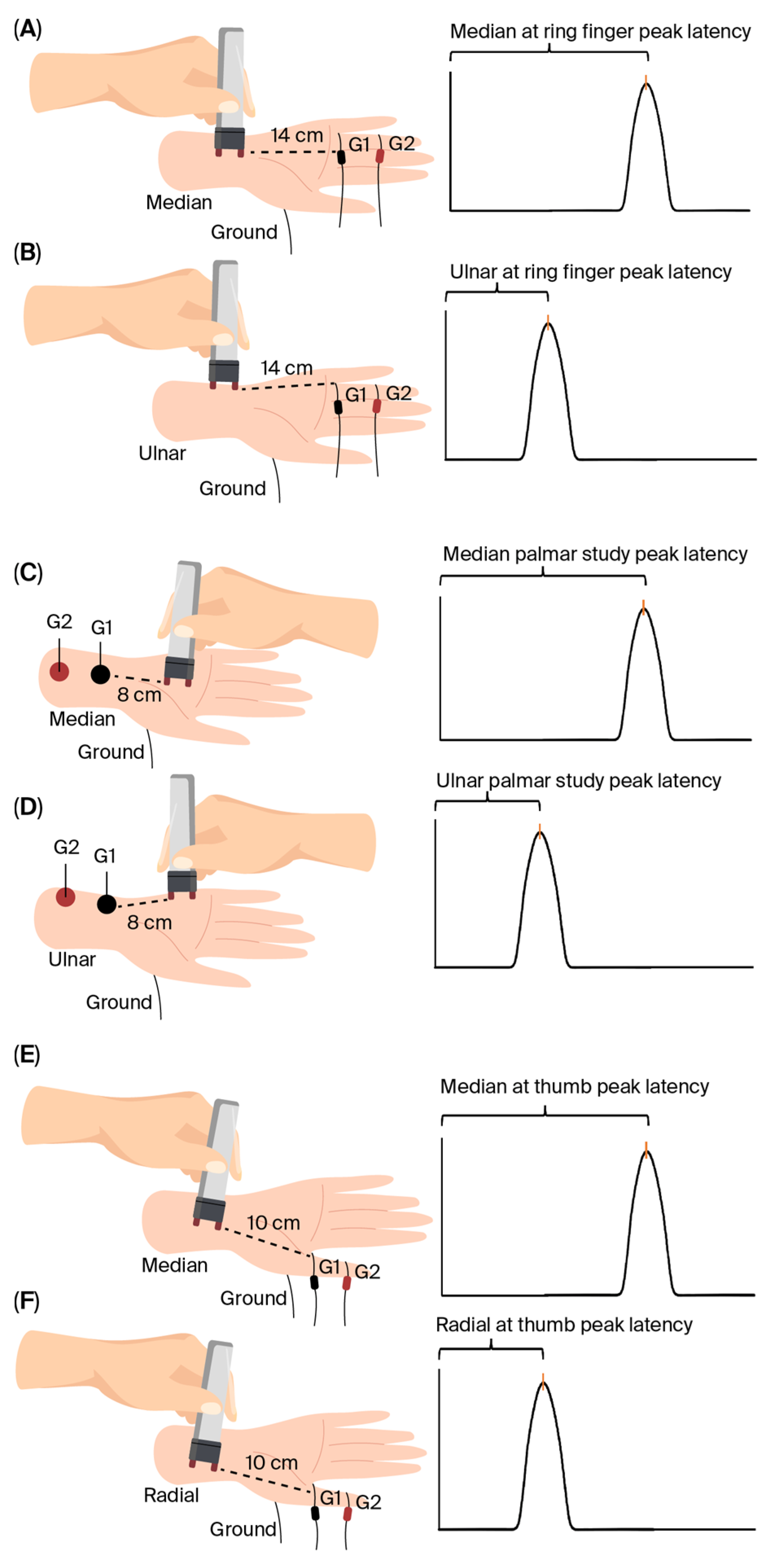
- (A)
- Median sensory latency measured at digit II (digit II latency).
- (B)
- Comparative latency studies (COLSs) consisting of the following:
2.4. Outcomes
- (A)
- Single-test strategies were defined by an abnormal result in one parameter:
- Palmdiff;
- Thumbdiff;
- Ringdiff.
- (B)
- Concordance between multiple tests was defined as follows:
- One of three: at least one abnormal result among thumbdiff, palmdiff, and ringdiff;
- Two of three: at least two abnormal results among thumbdiff, palmdiff, and ringdiff;
- One of palm–radial: at least one abnormal result among palmdiff and thumbdiff;
- Two of palm–radial: both palmdiff and thumbdiff are abnormal;
- One of palm–ring: at least one abnormal result among palmdiff and ringdiff;
- Two of palm–ring: both palmdiff and ringdiff are abnormal;
- One of radial–ring: at least one abnormal result among thumbdiff and ringdiff;
- Two of radial–ring: both thumbdiff and ringdiff are abnormal.
2.5. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Diagnostic Accuracy for Patients Without DM
3.3. Diagnostic Accuracy for Patients with DM
3.4. Diagnostic Accuracy for Patients with Symptom Durations Greater than Six Months
4. Discussion
Supplementary Materials
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CTS | Carpal tunnel syndrome |
| EDX | Electrodiagnostic studies |
| COLS | Comparative latency studies |
| Palmdiff | Median–ulnar mixed palmar latency difference test |
| Ringdiff | Median–ulnar ring finger latency difference test |
| Thumbdiff | Median–radial thumb latency difference test |
References
- Werner, R.A.; Andary, M. Electrodiagnostic evaluation of carpal tunnel syndrome. Muscle Nerve 2011, 44, 597–607. [Google Scholar] [CrossRef]
- Shetty, K.D.; Basu, A.R.; Nuckols, T.K. Refining quality measures for electrodiagnostic testing in suspected carpal tunnel syndrome to account for acceptable variations in practice: Expert review process. Muscle Nerve 2024, 70, 316–324. [Google Scholar] [CrossRef] [PubMed]
- Jablecki, C.K.; Andary, M.T.; So, Y.T.; Wilkins, D.E.; Williams, F.H. Literature review of the usefulness of nerve conduction studies and electromyography for the evaluation of patients with carpal tunnel syndrome. AAEM Quality Assurance Committee. Muscle Nerve 1993, 16, 1392–1414. [Google Scholar] [PubMed]
- Chen, X.; Cao, J.; Lao, J.; Liu, A.; Rui, J. Evaluation of electrophysiological examinations for the diagnosis of carpal tunnel syndrome. J. Orthop. Surg. Res. 2025, 20, 680. [Google Scholar] [CrossRef] [PubMed]
- Demino, C.; Fowler, J.R. The Sensitivity and Specificity of Nerve Conduction Studies for Diagnosis of Carpal Tunnel Syndrome: A Systematic Review. Hand 2021, 16, 174–178. [Google Scholar] [CrossRef]
- Drăghici, N.C.; Tămaș, M.M.; Leucuța, D.C.; Lupescu, T.D.; Strilciuc, Ș.; Rednic, S.; Mureșanu, D.F. Diagnosis Accuracy of Carpal Tunnel Syndrome in Diabetic Neuropathy. Medicina 2020, 56, 279. [Google Scholar] [CrossRef]
- Chen, J.; Fowler, J.R. Comparison of Diagnostic Accuracy of Electrodiagnostic Testing and Ultrasonography for Carpal Tunnel Syndrome. Hand 2023, 18, 407–412. [Google Scholar] [CrossRef]
- Claes, F.; Kasius, K.M.; Meulstee, J.; Verhagen, W.I. Comparing a new ultrasound approach with electrodiagnostic studies to confirm clinically defined carpal tunnel syndrome: A prospective, blinded study. Am. J. Phys. Med. Rehabil. 2013, 92, 1005–1011. [Google Scholar] [CrossRef]
- Robinson, L.R.; Micklesen, P.J.; Wang, L. Optimizing the number of tests for carpal tunnel syndrome. Muscle Nerve 2000, 23, 1880–1882. [Google Scholar] [CrossRef]
- Padua, L.; Coraci, D.; Erra, C.; Pazzaglia, C.; Paolasso, I.; Loreti, C.; Caliandro, P.; Hobson-Webb, L.D. Carpal tunnel syndrome: Clinical features, diagnosis, and management. Lancet Neurol. 2016, 15, 1273–1284. [Google Scholar] [CrossRef]
- Jablecki, C.K.; Andary, M.T.; Floeter, M.K.; Miller, R.G.; Quartly, C.A.; Vennix, M.J.; Wilson, J.R. Practice parameter: Electrodiagnostic studies in carpal tunnel syndrome. Report of the American Association of Electrodiagnostic Medicine, American Academy of Neurology, and the American Academy of Physical Medicine and Rehabilitation. Neurology 2002, 58, 1589–1592. [Google Scholar] [CrossRef] [PubMed]
- Preston, D.C.; Shapiro, B.E. Electromyography and Neuromuscular Disorders: Basic Statistic for Electrodiagnostic Studies, 2nd ed.; Butterworth-Heinemann: Philadelphia, PA, USA, 2005; pp. 107–113. [Google Scholar]
- De Kleermaeker, F.; Meulstee, J.; Claes, F.; Kasius, K.M.; Verhagen, W.I.M. Treatment outcome in patients with clinically defined carpal tunnel syndrome but normal electrodiagnostic test results: A randomized controlled trial. J. Neurol. 2017, 264, 2394–2400. [Google Scholar] [CrossRef] [PubMed]
- Witt, J.C.; Hentz, J.G.; Stevens, J.C. Carpal tunnel syndrome with normal nerve conduction studies. Muscle Nerve 2004, 29, 515–522. [Google Scholar] [CrossRef] [PubMed]
- Fowler, J.R.; Gaughan, J.P.; Ilyas, A.M. The sensitivity and specificity of ultrasound for the diagnosis of carpal tunnel syndrome: A meta-analysis. Clin. Orthop. Relat. Res. 2011, 469, 1089–1094. [Google Scholar] [CrossRef]
- Nora, D.B.; Becker, J.; Ehlers, J.A.; Gomes, I. What symptoms are truly caused by median nerve compression in carpal tunnel syndrome? Clin. Neurophysiol. 2005, 116, 275–283. [Google Scholar] [CrossRef]
- D’Arcy, C.A.; McGee, S. The rational clinical examination. Does this patient have carpal tunnel syndrome? JAMA 2000, 283, 3110–3117. [Google Scholar] [CrossRef]
- Padua, L.; LoMonaco, M.; Gregori, B.; Valente, E.M.; Padua, R.; Tonali, P. Neurophysiological classification and sensitivity in 500 carpal tunnel syndrome hands. Acta Neurol. Scand. 1997, 96, 211–217. [Google Scholar] [CrossRef]
- Bland, J.D. A neurophysiological grading scale for carpal tunnel syndrome. Muscle Nerve 2000, 23, 1280–1283. [Google Scholar] [CrossRef]
- Abuzinadah, A.R. Values and Diagnostic Accuracy of Electrodiagnostic Findings in Carpal Tunnel Syndrome Based on Age, Gender, and Diabetes. Diagnostics 2024, 14, 1381. [Google Scholar] [CrossRef]
- Wang, Q.; Chu, H.; Wang, H.; Jin, Y.; Zhao, X.; Weng, C.; Lu, Z. Ring finger sensory latency difference in the diagnosis and treatment of carpal tunnel syndrome. BMC Neurol. 2021, 21, 432. [Google Scholar] [CrossRef]
- Rempel, D.; Evanoff, B.; Amadio, P.C.; de Krom, M.; Franklin, G.; Franzblau, A.; Gray, R.; Gerr, F.; Hagberg, M.; Hales, T.; et al. Consensus criteria for the classification of carpal tunnel syndrome in epidemiologic studies. Am. J. Public Health 1998, 88, 1447–1451. [Google Scholar] [CrossRef]
- Robinson, L.R.; Micklesen, P.J.; Wang, L. Strategies for analyzing nerve conduction data: Superiority of a summary index over single tests. Muscle Nerve 1998, 21, 1166–1171. [Google Scholar] [CrossRef]
- Sonoo, M.; Menkes, D.L.; Bland, J.D.P.; Burke, D. Nerve conduction studies and EMG in carpal tunnel syndrome: Do they add value? Clin. Neurophysiol. Pract. 2018, 3, 78–88. [Google Scholar] [CrossRef] [PubMed]
- Albers, J.W.; Brown, M.B.; Sima, A.A.; Greene, D.A. Frequency of median mononeuropathy in patients with mild diabetic neuropathy in the early diabetes intervention trial (EDIT). Tolrestat Study Group For Edit (Early Diabetes Intervention Trial). Muscle Nerve 1996, 19, 140–146. [Google Scholar] [CrossRef]
- Gazioglu, S.; Boz, C.; Cakmak, V.A. Electrodiagnosis of carpal tunnel syndrome in patients with diabetic polyneuropathy. Clin. Neurophysiol. 2011, 122, 1463–1469. [Google Scholar] [CrossRef] [PubMed]
- Mi, J.; Liu, Z. Obesity, Type 2 Diabetes, and the Risk of Carpal Tunnel Syndrome: A Two-Sample Mendelian Randomization Study. Front. Genet. 2021, 12, 688849. [Google Scholar] [CrossRef]
- Werner, R.A.; Franzblau, A.; D’Arcy, H.J.; Evanoff, B.A.; Tong, H.C. Differential aging of median and ulnar sensory nerve parameters. Muscle Nerve 2012, 45, 60–64. [Google Scholar] [CrossRef]
- Tong, H.C.; Werner, R.A.; Franzblau, A. Effect of aging on sensory nerve conduction study parameters. Muscle Nerve 2004, 29, 716–720. [Google Scholar] [CrossRef]
- Zhang, Y.; Liu, X.; Jia, J.; Zhang, Q.; Lin, Y.; Zhang, L.; Lu, Q.; Lv, H.; Zheng, X. Diabetic polyneuropathy and carpal tunnel syndrome together affect hand strength, tactile sensation and dexterity in diabetes patients. J. Diabetes Investig. 2021, 12, 2010–2018. [Google Scholar] [CrossRef]
- Papanas, N.; Stamatiou, I.; Papachristou, S. Carpal Tunnel Syndrome in Diabetes Mellitus. Curr. Diabetes Rev. 2022, 18, e010921196025. [Google Scholar] [CrossRef]
- Abuzinadah, A.R.; Alzabidi, Z.H.; Abuzaid, A.E.; Kattan, K.W.; Alsubaie, B.S.; Altunisi, A.M.; AlKutbi, A.M.; Bamaga, A.K.; AlShareef, A.A. Carpal Tunnel Decompression Surgery Outcome and Effect of Diabetes. Eur. Neurol. 2020, 83, 189–194. [Google Scholar] [CrossRef]
- Yagci, I.; Gunduz, O.H.; Sancak, S.; Agirman, M.; Mesci, E.; Akyuz, G. Comparative electrophysiological techniques in the diagnosis of carpal tunnel syndrome in patients with diabetic polyneuropathy. Diabetes Res. Clin. Pract. 2010, 88, 157–163. [Google Scholar] [CrossRef]
- Padua, L.; Cuccagna, C.; Giovannini, S.; Coraci, D.; Pelosi, L.; Loreti, C.; Bernabei, R.; Hobson-Webb, L.D. Carpal tunnel syndrome: Updated evidence and new questions. Lancet Neurol. 2023, 22, 255–267. [Google Scholar] [CrossRef]
- Zivkovic, S.; Gruener, G.; Arnold, M.; Winter, C.; Nuckols, T.; Narayanaswami, P. Quality measures in electrodiagnosis: Carpal tunnel syndrome-An AANEM Quality Measure Set. Muscle Nerve 2020, 61, 460–465. [Google Scholar] [CrossRef]
| Without DM | With DM | |
|---|---|---|
| Palmdiff | ≥0.5 ms | ≥0.5 ms (<50 years) ≥1.2 ms (≥50 years) |
| Ringdiff | ≥0.6 ms | ≥0.5 ms (<50 years) ≥1.6 ms (≥50 years) |
| Thumbdiff | ≥1 ms | ≥1 ms (<60 years) ≥1.8 ms (≥60 years) |
| Variable | Patients Without CTS n = 233 | Patients with CTS n = 305 |
|---|---|---|
| Age (years), median (IQR) | 45 (35–57) | 49 (40–56) |
| Male, n (%) | 113 (48.50%) | 53 (17.38%) |
| Diabetes Mellitus, n (%) | 48 (20.60%) | 61 (20.00%) |
| Hypothyroidism, n (%) | 19 (9.55%) | 57 (19.39%) |
| Disease duration (months), median (IQR) | 6 (2–24) | 12 (5–36) |
| Burning feet | 48 (22.64%) | 106 (37.46%) |
| Right-hand dominant, n (%) | 144 (92.31%) | 190 (92.23%) |
| Age < 30 years, n (%) | 35 (15.02%) | 22 (7.21%) |
| Age 30–39 years, n (%) | 46 (19.74%) | 54 (17.70%) |
| Age 40–49 years, n (%) | 52 (22.32%) | 77 (25.25%) |
| Age 50–59 years, n (%) | 50 (21.46%) | 104 (34.10%) |
| Age≥ >60 years, n (%) | 50 (21.46%) | 48 (15.74%) |
| Padua CTS severity classification | ||
| Padua 0, n (%) | 71 (30.47%) | 35 (11.48%) |
| Padua 1, n (%) | 28 (12.02%) | 25 (8.20%) |
| Padua 2, n (%) | 112 (48.07%) | 114 (37.38%) |
| Padua 3, n (%) | 22 (9.44%) | 131 (42.95%) |
| Bland CTS severity classification | ||
| Bland 0, n (%) | 147 (63.09%) | 100 (32.79%) |
| Bland 1, n (%) | 36 (15.45%) | 44 (14.43%) |
| Bland 2, n (%) | 46 (19.74%) | 96 (31.48%) |
| Bland 3, n (%) | 4 (1.72%) | 65 (21.31%) |
| Distribution of CTS and non-CTS diagnoses | ||
| CTS, n (%) | 0 (0.00%) | 305 (100.00%) |
| Ulnar neuropathy, n (%) | 43 (18.45%) | 0 (0.00%) |
| Radiculopathy, n (%) | 34 (14.59%) | 0 (0.00%) |
| Rotator cuff, n (%) | 6 (2.58%) | 0 (0.00%) |
| De Quervain’s tenosynovitis, n (%) | 5 (2.15%) | 0 (0.00%) |
| Carpometacarpal arthritis, n (%) | 6 (2.58%) | 0 (0.00%) |
| Fibromyalgia, n (%) | 12 (5.15%) | 0 (0.00%) |
| Epicondylitis, n (%) | 7 (3.00%) | 0 (0.00%) |
| Musculoskeletal disorders, n (%) | 120 (51.5%) | 0 (0.00%) |
| COLS | ROC (95% CI) | Sensitivity (95% CI) | Specificity (95% CI) | PPV (95% CI) | NPV (95% CI) |
|---|---|---|---|---|---|
| Whole cohort (n = 429) | |||||
| Thumbdiff | 0.683 (0.65–0.72) | 43% (36.7–49.5) | 93.5% (88.9–96.6) | 89.7% (82.8–94.6) | 55.4% (49.7–61) |
| Palmdiff | 0.753 (0.72–0.79) | 56.6% (50.1–62.9) | 94.1% (89.6–97) | 92.6% (87.2–96.3) | 62.1% (56.2–67.8) |
| Ringdiff | 0.73 (0.69–0.77) | 52.5% (46–58.9) | 93.5% (88.9–96.6) | 91.4% (85.5–95.5) | 59.9% (54–65.6) |
| One of three COLSs | 0.758 (0.72–0.79) | 63.5% (57.1–69.6) | 88.1% (82.6–92.4) | 87.6% (81.8–92) | 64.7% (58.4–70.6) |
| Two of three COLSs | 0.741 (0.71–0.78) | 52.5% (46–58.9) | 95.7% (91.7–98.1) | 94.1% (88.7–97.4) | 60.4% (54.6–66) |
| One of palmdiff–thumbdiff | 0.753 (0.72–0.79) | 59.8% (53.4–66) | 90.8% (85.7–94.6) | 89.6% (83.8–93.8) | 63.2% (57.1–69) |
| Two of palmdiff–thumbdiff | 0.683 (0.65–0.72) | 39.8% (33.6–46.2) | 96.8% (93.1–98.8) | 94.2% (87.8–97.8) | 54.9% (49.3–60.4) |
| One of palmdiff–ringdiff | 0.766 (0.73–0.80) | 61.9% (55.5–68) | 91.4% (86.3–95) | 90.4% (84.9–94.4) | 64.5% (58.4–70.3) |
| Two of palmdiff–ringdiff | 0.717 (0.68–0.75) | 47.1% (40.7–53.6) | 96.2% (92.4–98.5) | 94.3% (88.5–97.7) | 58% (52.2–63.6) |
| One of thumbdiff–ringdiff | 0.738 (0.70–0.78) | 57.8% (51.3–64.1) | 89.7% (84.4–93.7) | 88.1% (82.1–92.7) | 61.7% (55.6–67.5) |
| Two of thumbdiff–ringdiff | 0.675 (0.64–0.71) | 37.7% (31.6–44.1) | 97.3% (93.8–99.1) | 94.8% (88.4–98.3) | 54.2% (48.7–59.7) |
| Patients with symptom duration > 6 months (n = 269) | |||||
| Thumbdiff | 0.669 (0.63–0.71) | 37.6% (30.2–45.4) | 96.2% (90.4–98.9) | 93.9% (85.2–98.3) | 49.3% (42.2–56.4) |
| Palmdiff | 0.668 (0.63–0.71) | 34.5% (27.3–42.3) | 99.0% (94.8–100) | 98.3% (90.8–100) | 48.8% (41.9–55.8) |
| Ringdiff | 0.684 (0.64–0.73) | 40.6% (33.0–48.5) | 96.2% (90.4–98.9) | 94.4% (86.2–98.4) | 50.5% (43.3–57.7) |
| One of three COLSs | 0.717 (0.67–0.76) | 52.1% (44.2–59.9) | 91.3% (84.2–96.0) | 90.5% (82.8–95.6) | 54.6% (46.9–62.1) |
| Two of three COLSs | 0.685 (0.65–0.72) | 37.0% (29.6–44.8) | 100% (96.5–100) | 100% (94.1–100) | 50.0% (43.0–57.0) |
| One of palmdiff–thumbdiff | 0.709 (0.67–0.75) | 46.7% (38.9–54.6) | 95.2% (89.1–98.4) | 93.9% (86.3–98.0) | 52.9% (45.5–60.3) |
| Two of palmdiff–thumbdiff | 0.627 (0.59–0.66) | 25.5% (19.0–32.8) | 100% (96.5–100) | 100% (91.6–100) | 45.8% (39.2–52.5) |
| One of palmdiff–ringdiff | 0.700 (0.66–0.74) | 44.8% (37.1–52.8) | 95.2% (89.1–98.4) | 93.7% (85.8–97.9) | 52.1% (44.8–59.4) |
| Two of palmdiff–ringdiff | 0.652 (0.62–0.69) | 30.3% (23.4–37.9) | 100% (96.5–100) | 100% (92.9–100) | 47.5% (40.7–54.3) |
| One of thumbdiff–ringdiff | 0.710 (0.66–0.76) | 49.7% (41.8–57.6) | 92.3% (85.4–96.6) | 91.1% (83.2–96.1) | 53.6% (46.0–61.1) |
| Two of thumbdiff–ringdiff | 0.642 (0.61–0.68) | 28.5% (21.7–36.0) | 100% (96.5–100) | 100% (92.5–100) | 46.8% (40.1–53.6) |
| COLS | ROC (95% CI) | Sensitivity (95% CI) | Specificity (95% CI) | PPV (95% CI) | NPV (95% CI) |
|---|---|---|---|---|---|
| Age < 60 years (n = 57) | |||||
| Thumbdiff | 0.750 (0.64–0.86) | 65.8% (48.6–80.4) | 84.2% (60.4–96.6) | 89.3% (71.8–97.7) | 55.2% (35.7–73.6) |
| Palmdiff | 0.776 (0.68–0.87) | 60.5% (43.4–76.0) | 94.7% (74.0–99.9) | 95.8% (78.9–99.9) | 54.5% (36.4–71.9) |
| Ringdiff | 0.724 (0.63–0.82) | 50.0% (33.4–66.6) | 94.7% (74.0–99.9) | 95.0% (75.1–99.9) | 48.6% (31.9–65.6) |
| One of three COLSs | 0.816 (0.71–0.92) | 78.9% (62.7–90.4) | 84.2% (60.4–96.6) | 90.9% (75.7–98.1) | 66.7% (44.8–84.4) |
| Two of three COLSs | 0.750 (0.66–0.85) | 55.3% (38.3–71.4) | 94.7% (74.0–99.9) | 95.5% (77.2–99.9) | 51.4% (34.0–68.6) |
| One of palmdiff–thumbdiff | 0.803 (0.69–0.91) | 76.3% (59.8–88.6) | 84.2% (60.4–96.6) | 90.6% (75.8–98.0) | 64.0% (42.5–82.0) |
| Two of palmdiff–thumbdiff | 0.724 (0.63–0.82) | 50.0% (33.4–66.6) | 94.7% (74.0–99.9) | 95.0% (75.1–99.9) | 48.6% (31.9–65.6) |
| One of palmdiff–ringdiff | 0.789 (0.69–0.88) | 63.2% (46.0–78.2) | 94.7% (74.0–99.9) | 96.0% (79.6–99.8) | 56.3% (37.7–73.6) |
| Two of palmdiff–ringdiff | 0.711 (0.62–0.81) | 47.4% (31.0–64.2) | 94.7% (74.0–99.9) | 94.7% (74.0–99.9) | 47.4% (31.0–64.2) |
| One of thumbdiff–ringdiff | 0.789 (0.68–0.90) | 73.7% (56.9–86.6) | 84.2% (60.4–96.6) | 90.3% (74.2–98.0) | 61.5% (40.6–79.8) |
| Two of thumbdiff–ringdiff | 0.684 (0.59–0.78) | 42.1% (26.3–59.2) | 94.7% (74.0–99.9) | 94.1% (71.3–99.9) | 45.8% (29.3–61.5) |
| Age ≥ 60 years (n = 52) | |||||
| Thumbdiff | 0.591 (0.49–0.68) | 21.7% (7.46–43.7) | 96.6% (82.2–99.9) | 83.3% (35.9–99.6) | 60.9% (45.4–74.9) |
| Palmdiff | 0.579 (0.47–0.69) | 26.1% (10.2–48.4) | 89.7% (72.6–97.8) | 66.7% (29.9–92.5) | 60.6% (44.4–75.8) |
| Ringdiff | 0.639 (0.53–0.75) | 34.8% (16.4–57.3) | 93.1% (77.2–99.2) | 80.0% (44.8–97.5) | 64.4% (48.8–78.5) |
| One of three COLSs | 0.666 (0.55–0.78) | 43.5% (23.2–65.5) | 89.7% (72.6–97.8) | 76.9% (46.2–95.0) | 66.7% (49.8–80.9) |
| Two of three COLSs | 0.618 (0.51–0.73) | 30.4% (13.2–52.9) | 93.1% (77.2–99.2) | 77.8% (40.8–97.2) | 62.9% (46.7–77.8) |
| One of palmdiff–thumbdiff | 0.622 (0.51–0.74) | 34.8% (16.4–57.3) | 89.7% (72.6–97.8) | 72.7% (39.0–94.0) | 63.4% (46.9–77.9) |
| Two of palmdiff–thumbdiff | 0.548 (0.47–0.63) | 13% (2.78–33.6) | 96.6% (82.2–99.9) | 75% (19.4–99.4) | 58.3% (43.2–72.5) |
| One of palmdiff–ringdiff | 0.644 (0.53–0.76) | 39.1% (19.7–61.6) | 89.7% (72.6–97.8) | 75% (42.8–94.5) | 65% (48.3–79.4) |
| Two of palmdiff–ringdiff | 0.574 (0.48–0.67) | 21.7% (7.46–43.7) | 93.1% (77.2–99.2) | 71.4% (29.8–96.3) | 60% (44.4–74.3) |
| One of thumbdiff–ringdiff | 0.683 (0.57–0.79) | 43.5% (23.2–65.5) | 93.1% (77.2–99.2) | 83.3% (51.6–97.9) | 67.5% (50.9–81.4) |
| Two of thumbdiff–ringdiff | 0.548 (0.47–0.63) | 13% (2.78–33.6) | 96.6% (82.2–99.9) | 75% (19.4–99.4) | 58.3% (43.2–72.5) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abuzinadah, A.R. Diagnostic Accuracy of Electrodiagnostic Comparative Latency Studies of Carpal Tunnel Syndrome: Single Test and Concordance Between Multiple Tests. Diagnostics 2025, 15, 2888. https://doi.org/10.3390/diagnostics15222888
Abuzinadah AR. Diagnostic Accuracy of Electrodiagnostic Comparative Latency Studies of Carpal Tunnel Syndrome: Single Test and Concordance Between Multiple Tests. Diagnostics. 2025; 15(22):2888. https://doi.org/10.3390/diagnostics15222888
Chicago/Turabian StyleAbuzinadah, Ahmad R. 2025. "Diagnostic Accuracy of Electrodiagnostic Comparative Latency Studies of Carpal Tunnel Syndrome: Single Test and Concordance Between Multiple Tests" Diagnostics 15, no. 22: 2888. https://doi.org/10.3390/diagnostics15222888
APA StyleAbuzinadah, A. R. (2025). Diagnostic Accuracy of Electrodiagnostic Comparative Latency Studies of Carpal Tunnel Syndrome: Single Test and Concordance Between Multiple Tests. Diagnostics, 15(22), 2888. https://doi.org/10.3390/diagnostics15222888





