Abstract
Here, we describe the case of a 48-year-old female patient with prurigo nodularis, where B-mode and color-Doppler ultrasound of one nodule was performed; this revealed hypoechoic dermal and hyperechoic epidermal thickening with lesion hypervascularity. To the best of our knowledge, no previous published articles have reported ultra-high-frequency ultrasound images of this disease, so this case can encourage prurigo nodularis studies in order to better assess ultrasound features and their usefulness in supporting clinical diagnosis and in distinguishing prurigo nodularis from other diseases.
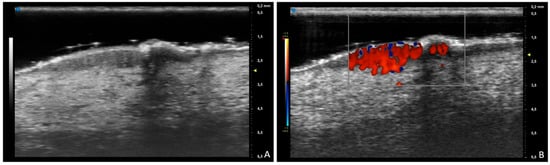
Figure 1.
A 48-year-old female patient with chronic pruritus and persistent itching nodules. (A) B-mode ultrasound of one nodule shows hypoechoic dermal and hyperechoic epidermal thickening at 70 MHz; (B) color-Doppler ultrasound reveals hypervascularity of the lesion. Prurigo nodularis is a chronic inflammatory skin condition characterized by itchy hyperkeratotic crusted or eroded light-to-bright-red papules or nodules from a few millimeters to 2–3 cm in size, with hyperpigmented borders, usually bilaterally and symmetrically located in the dorsal part of the extremities, back and buttocks [1]. The median estimated prevalence of prurigo nodularis is 32.7 cases per 100,000 [2,3]. Dermatological examination is essential to try to identify associated diseases and underlying dermatoses that can be masked by prurigo nodularis. Dermoscopic white starburst pattern surrounding brown-reddish/brown-yellowish crusts, erosions and/or hyperkeratosis/scales can support the clinical diagnosis of prurigo nodularis [4]. Skin biopsy is necessary in prurigo nodularis of unclear origin. The aim of the treatment is to try to interrupt the itch–scratch cycle. First-line therapy for prurigo nodularis includes topical corticosteroids, antihistamines, calcineurin inhibitors and intralesional steroid injection. Second-line treatment is characterized by ultraviolet light therapy and/or systemic treatments such as immunosuppressants, gabapentinoids, antidepressants and mu-opioid receptor antagonists. Adult refractory patients can be treated with dupilumab, which is the first FDA- and EMA-approved drug for this disease [5,6]. To the best of our knowledge, no previous published articles have reported ultra-high-frequency ultrasound images about this disease, so this case can encourage prurigo nodularis studies in order to better assess ultrasound features and their usefulness in supporting clinical diagnosis and in distinguishing prurigo nodularis from other diseases, such as inconspicuous blister in pemphigoid nodularis or the common bullous pemphigoid in early stages, which would show anechoic subepidermal cystic structures with a hypoechoic subjacent upper dermis and no vascularization pattern [7,8].
Author Contributions
Conceptualization, A.M. and C.T.; methodology, A.M., C.T., F.M.M., G.S., M.F., G.R., A.C., E.M., A.O., O.S., M.R. and V.D.; data curation, A.M., C.T., F.M.M., G.S., M.F., G.R., A.C. and E.M.; writing—original draft preparation, A.M., C.T., F.M.M., G.S., M.F., G.R., A.C., E.M., A.O., O.S., M.R. and V.D.; writing—review and editing, A.M., C.T., F.M.M., G.S., M.F., G.R., A.C., E.M., A.O., O.S., M.R. and V.D.; supervision, A.C., E.M., A.O., O.S., M.R. and V.D. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Written informed consent has been obtained from the patient.
Data Availability Statement
Data are contained within the article.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Brooks, S.G.; Coscarella, G.; Yosipovitch, G. Prurigo Nodularis: A historic perspective. Clin. Dermatol. 2025; in press. [Google Scholar] [CrossRef] [PubMed]
- Patruno, C.; Pelucchi, C.; Galeone, C.; Emmi, M.; Amerio, P. Epidemiology and Severity of Prurigo Nodularis in Europe: A Literature Review with an Application to Italian Data. Dermatol. Pract. Concept. 2025, 15, 4716. [Google Scholar] [CrossRef] [PubMed]
- Igarashi, A.; Yoshida, T.; Sunaga, Y.; Nawata, H.; Arima, K. Current Status of Prurigo Nodularis in Japan: A Retrospective Study Using a Health Insurance Claims Database. J. Clin. Med. 2025, 14, 1872. [Google Scholar] [CrossRef] [PubMed]
- Errichetti, E.; Piccirillo, A.; Stinco, G. Dermoscopy of prurigo nodularis. J. Dermatol. 2015, 42, 632–634. [Google Scholar] [CrossRef] [PubMed]
- Bianco, M.; D’Oria, F.; Falcidia, C.; Foggi, G.; Matteodo, E.; Di Giulio, S.; Facheris, P.; Ibba, L.; Perugini, C.; Valenti, M.; et al. New and Emerging Biologics and Jak Inhibitors for the Treatment of Prurigo Nodularis: A Narrative Review. Medicina 2025, 61, 631. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, H.; Izumi, K. Dupilumab-Induced Psoriasis in a Patient with Prurigo Nodularis: A Case Report. Cureus 2025, 17, e81636. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Sun, J. High-frequency ultrasound features of pemphigoid nodularis: A case report. Skin. Res. Technol. 2022, 28, 171–172. [Google Scholar] [CrossRef] [PubMed]
- Porriño-Bustamante, M.L.; Alfageme, F.; Suárez, L.; de Domingo, M.A.; Hospital, M.; Roustán, G. High-Frequency Color Doppler Sonography of Bullous Pemphigoid: Correlation With Histologic Findings. J. Ultrasound Med. 2016, 35, 1821–1825. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).