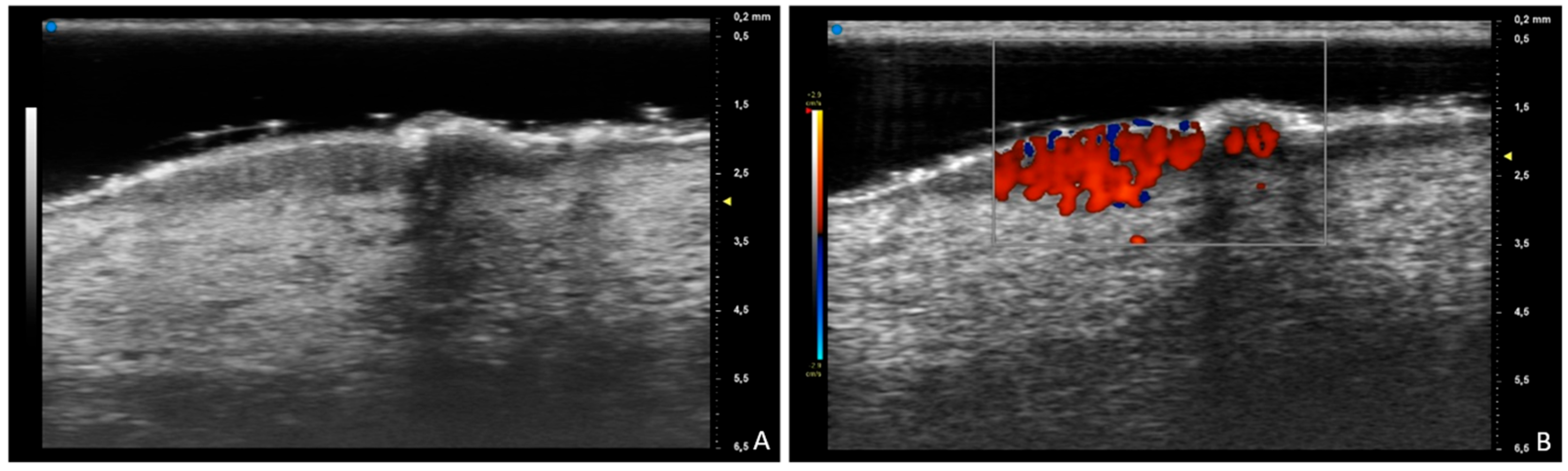
Prurigo Nodularis at Ultra-High-Frequency Ultrasound
Abstract
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Brooks, S.G.; Coscarella, G.; Yosipovitch, G. Prurigo Nodularis: A historic perspective. Clin. Dermatol. 2025; in press. [Google Scholar] [CrossRef] [PubMed]
- Patruno, C.; Pelucchi, C.; Galeone, C.; Emmi, M.; Amerio, P. Epidemiology and Severity of Prurigo Nodularis in Europe: A Literature Review with an Application to Italian Data. Dermatol. Pract. Concept. 2025, 15, 4716. [Google Scholar] [CrossRef] [PubMed]
- Igarashi, A.; Yoshida, T.; Sunaga, Y.; Nawata, H.; Arima, K. Current Status of Prurigo Nodularis in Japan: A Retrospective Study Using a Health Insurance Claims Database. J. Clin. Med. 2025, 14, 1872. [Google Scholar] [CrossRef] [PubMed]
- Errichetti, E.; Piccirillo, A.; Stinco, G. Dermoscopy of prurigo nodularis. J. Dermatol. 2015, 42, 632–634. [Google Scholar] [CrossRef] [PubMed]
- Bianco, M.; D’Oria, F.; Falcidia, C.; Foggi, G.; Matteodo, E.; Di Giulio, S.; Facheris, P.; Ibba, L.; Perugini, C.; Valenti, M.; et al. New and Emerging Biologics and Jak Inhibitors for the Treatment of Prurigo Nodularis: A Narrative Review. Medicina 2025, 61, 631. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, H.; Izumi, K. Dupilumab-Induced Psoriasis in a Patient with Prurigo Nodularis: A Case Report. Cureus 2025, 17, e81636. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Sun, J. High-frequency ultrasound features of pemphigoid nodularis: A case report. Skin. Res. Technol. 2022, 28, 171–172. [Google Scholar] [CrossRef] [PubMed]
- Porriño-Bustamante, M.L.; Alfageme, F.; Suárez, L.; de Domingo, M.A.; Hospital, M.; Roustán, G. High-Frequency Color Doppler Sonography of Bullous Pemphigoid: Correlation With Histologic Findings. J. Ultrasound Med. 2016, 35, 1821–1825. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Michelucci, A.; Tagliati, C.; Manzo Margiotta, F.; Salvia, G.; Fogante, M.; Rizzetto, G.; Corvino, A.; Molinelli, E.; Offidani, A.; Simonetti, O.; et al. Prurigo Nodularis at Ultra-High-Frequency Ultrasound. Diagnostics 2025, 15, 1624. https://doi.org/10.3390/diagnostics15131624
Michelucci A, Tagliati C, Manzo Margiotta F, Salvia G, Fogante M, Rizzetto G, Corvino A, Molinelli E, Offidani A, Simonetti O, et al. Prurigo Nodularis at Ultra-High-Frequency Ultrasound. Diagnostics. 2025; 15(13):1624. https://doi.org/10.3390/diagnostics15131624
Chicago/Turabian StyleMichelucci, Alessandra, Corrado Tagliati, Flavia Manzo Margiotta, Giorgia Salvia, Marco Fogante, Giulio Rizzetto, Antonio Corvino, Elisa Molinelli, Annamaria Offidani, Oriana Simonetti, and et al. 2025. "Prurigo Nodularis at Ultra-High-Frequency Ultrasound" Diagnostics 15, no. 13: 1624. https://doi.org/10.3390/diagnostics15131624
APA StyleMichelucci, A., Tagliati, C., Manzo Margiotta, F., Salvia, G., Fogante, M., Rizzetto, G., Corvino, A., Molinelli, E., Offidani, A., Simonetti, O., Romanelli, M., & Dini, V. (2025). Prurigo Nodularis at Ultra-High-Frequency Ultrasound. Diagnostics, 15(13), 1624. https://doi.org/10.3390/diagnostics15131624







