Abstract
Introduction: Fraser syndrome (FS) is a rare autosomal recessive disorder. However, the clinical presentation remains variable. Diagnosis is based on a series of major and minor clinical criteria that can be supported by genetic tests. Prenatal diagnosis remains challenging. Methods: Herein, we reported a case of Fraser syndrome that was missed by ultrasound and diagnosed late at birth. The newborn presented with cryptophthalmos–syndactyly syndrome and absence of the right kidney. Based on a literature review of articles from the past 20 years, the authors found 40 cases, including indexed cases on PUBMED, Scopus, Web of Science, and Scholar using keywords related to “Fraser syndrome”. Through this report, we discuss the polymalformative syndrome, the clinical and paraclinical aspects of this syndrome, its clinical management, and highlight the importance of prenatal diagnosis in the light of research. Results: Our study found that consanguine parents (41.0%) were increasing risk factors for FS and poor socio-economic status delayed the early detection of FS. Among the 40 cases, 27 cases were detected postnatally. More than half of the cases resulted in poor perinatal outcomes. The common findings were cryptophthalmos (87.5%), syndactyly (87.5%), renal abnormalities (55.5%), and genital abnormalities (42.5%). Conclusions: A prenatal diagnosis of Fraser syndrome is still difficult. Thus, a counseled ultrasound scan at a specialized center should be recommended in suspected cases with indirect signs and risk factors of consanguinity.
1. Introduction
Fraser syndrome (FS; cryptophthalmos–syndactyly syndrome; OMIM #219000), also known as Meyer-Schwickerath syndrome, Fraser–François syndrome, or Ullrich–Feichtiger syndrome, is a rare autosomal recessive multiple malformation syndrome characterized by cryptophthalmos, syndactyly, and respiratory and urogenital tract anomalies [1,2]. The prevalence of FS is 0.43 per 100,000 among newborns worldwide. Since the first description of the syndrome by George Fraser in 1962 and later by Thomas et al. in 1986, over 280 cases have been documented to date [3,4].
Fraser syndrome is caused by mutations in the FRAS1 (4q21.21), FREM2 (Fras1-related extracellular matrix gene 2) (13q13.3), and GRIP1 (glutamate-receptor-interacting protein 1) (12q14.3) genes, coding for extracellular matrix proteins essential for the adhesion between the basement membrane of the epidermis and connective tissues of the dermic layer during embryological development. Mutations in these genes are suggested to be responsible for failure in apoptosis [5,6].
Risk factors include consanguine marriage and familial factors [7]. Consanguineous marriage can increase the risk of autosomal recessive conditions in general. Van Healst et al. reported 59 affected individuals from 40 families. Among them, 25 cases were consanguineous [8]. According to Slavotinek et al., FS was present in more girls (57/117) than boys and consanguinity was present in 29/119 (24.8%) of the cases [8]. Cryptophthalmos and syndactyly seem to be the most constant features of this disorder, with cryptophthalmos being the most defining feature but not an obligatory feature of Fraser syndrome [2,9,10]. Other anomalies include CHAOS (congenital obstructive syndrome of the upper airways). A wide variability of expression has been observed, making its clinical diagnosis sometimes challenging [11]. Many cases were detected postnatally [12,13,14,15,16,17].
Through this report, the team emphasizes the characteristics of Fraser syndrome. In addition, we searched English keywords relating to Fraser syndrome, including “Fraser syndrome”, or “Meyer-Schwickerath’s syndrome” or “Fraser-François syndrome”, or “Ullrich-Feichtiger syndrome” and “case report” on databases such as Medline, PubMed, Scopus, and Google Scholar to review the literature from the past 20 years.
2. Case Presentation
A 29-year-old Vietnamese pregnant woman (gravida: 0, parity: 0) with a non-consanguineous Vietnamese partner was hospitalized for induction of labor at 38 weeks and 4 days due to fetal growth restriction (FGR). There was no reported history of toxoplasma, cytomegalovirus (CMV), or rubella infections. Additionally, there was no history of radiation exposure, drug use, and no reported maternal history of fever or genitourinary infections during the pregnancy. There was also no history of cryptophthalmos or other significant abnormalities in their immediate or distant families. The maternal blood group was A with a positive rhesus factor. Both the mother and father were non-smokers. The mother did not consume alcohol.
During the first trimester screening, the nuchal translucency measurement was normal. A non-invasive prenatal test (NIPT) showed a normal karyotype. Trisomy 13, 18, 21, and sexual chromosomal aneuploidy (monoX, XXY, XXX, XYY, XXXY) were low-risk. The screening test for nine common recessive genetic diseases in maternal plasma, including genetic mutations of HBA1 and HBA2 (Alpha thalassemia), HBB (Beta thalassemia), GALT (metabolic disorder of galactose), PAH (urine phenylketone), G6PD (glucose-6-phosphate dehydrogenase deficiency), SLC25A13 (solute carrier family 25 member 13), SRD5A2 (lack of 5-alpha reductase), GAA (metabolic disease of glycogen type 2, Pompe disease), and ATP7B (metabolic disorder of Cu, Wilson disease), were absent.
A four-dimensional morphologic ultrasound at 21 weeks and 5 days was performed without abnormal detection, except for a fetal growth restriction (FGR) with an estimated fetal weight (EFW) below the third percentile. The head circumference measured at 174 mm, abdominal circumference measured at 151 mm, and femoral length measured at 32 mm. The fetal heart rate and fetal movement were normal. The amniotic fluid volume was measured at 6–7 cm. The patient was counseled for amniocentesis; however, she refused.
At 36 weeks of gestational age (GA), the ultrasound showed a small gestational-age fetus with an EFW of 2270 g (5.7% following Hadlock, corresponding to 33 weeks and 4 days of gestational age). The biometric parameters included a biparietal diameter (BPD) of 81 mm (3%), head circumference (HC) of 306 (1%), abdominal circumference (AC) of 297 mm (5%), and femoral length (FL) of 65 mm (2%). The amniotic fluid index (AFI) measured at 10 cm. During pregnancy, the patient was followed up at a different hospital.
During hospitalization, the patient’s cardiotocography was normal. Since the induction of labor failed after using both a balloon and prostaglandin E2, the patient underwent cesarean delivery. The cesarean section was performed uneventfully with a female newborn weighing at 2700 g. The Apgar score was evaluated at 6/1 min and 8/5 min.
However, the neonate was observed to have abnormal morphology. Unilateral cryptophthalmos and cleft palate were noted postnatally. In addition, the neonate presented with abnormalities of the extremities, consisting of partial III-IV-V finger membranous syndactyly on the right hand, partial II-III-IV finger membranous syndactyly on the left hand, and complete II-III-IV-V foot membranous syndactyly on the right side, and complete IV-V membranous syndactyly on the left side. The face was dysmorphic, with marked hypertelorism, a depressed nasal bridge, dysplastic ears, and low-set ears (Figure 1A–G). The rest of the systemic examination was unremarkable.


Figure 1.
The photos of the newborn on postnatal day 1 show the face was dysmorphic with marked hypertelorism, a depressed nasal bridge, right unilateral cryptophthalmos (A), low-set ears and dysplasia (B), a cleft palate (C), partial III-IV-V finger membranous syndactyly on the right hand (D), partial II-III-IV finger membranous syndactyly on the left hand (E), complete II-III-IV-V foot membranous syndactyly on the right side (F), and complete IV-V membranous syndactyly on the left side (G).
Based on the clinical aspect, the neonate was suspected of Fraser syndrome according clinical criteria of Thomas and Van Healst (Table 1).

Table 1.
Criteria for diagnosis of Fraser syndrome.
After birth, the baby was strictly monitored at the neonatal unit for 5 days. Both mother and neonate were discharged on day 5 after birth. The postnatal ultrasound scan demonstrated right renal agenesis. Meanwhile, anterior to the right iliopsoas muscle, a cystic structure measuring 9.5 × 7.3 mm was suspected to be right renal ectopic dysplasia. The infant gained 3300 g by the 28th day of life. The neonate was monitored for one month with the same malformation at birth and without other complications of the digestive tract and cardio-pulmonary system (Figure 2A–G) and Supplemental Video S1.

Figure 2.
The photos of the newborn at one month and eight days showed the dysmorphic face, with marked hypertelorism, a depressed nasal bridge, right unilateral cryptophthalmos (A), low-set ears and dysplasia (B), a cleft palate (C), partial III-IV-V finger membranous syndactyly on the right hand (D), partial II-III-IV finger membranous syndactyly on the left hand (E), complete II-III-IV-V foot membranous syndactyly on the right side (F), and complete IV-V membranous syndactyly on the left side (G).
The patient displayed total cryptophthalmos of the right eye and an absent eyebrow but the ocular globe was felt underneath the skin. The diagnosis was confirmed by genetic analysis, which showed novel compound heterozygous variants of FRAS1 gene on chromosome 4 was found. Concisely, 03 heterozygous variants not reported in ClinVar (classified as likely pathogenic (c.4426-1G>A, location 78418948) and uncertain significance (c.4426G>C, location 78418949 và c.11411A>G, location 78539406) according to the American College of Medical Genetics and Genomics (ACMG) criteria) in the FRAS1 gene (Figure 3). Thus, pathogenic/likely pathogenic homozygous or in-trans compound heterozygous variants in this gene may be associated with Fraser syndrome 1; probably linking to clinical diagnosis. The parental genetic analysis revealed a heterozygous variant of the FRAS1 gene on chromosome 4, location 78418948, relating to a variation of NM_025074.7:c.4426-1G>A (Father) and a heterozygous variant of the FRAS1 gene on chromosome 4, location 78539406, relating to a variation of NM_025074.7:c.11411A>G (Mother) (Supplemental Figure S1A,B).
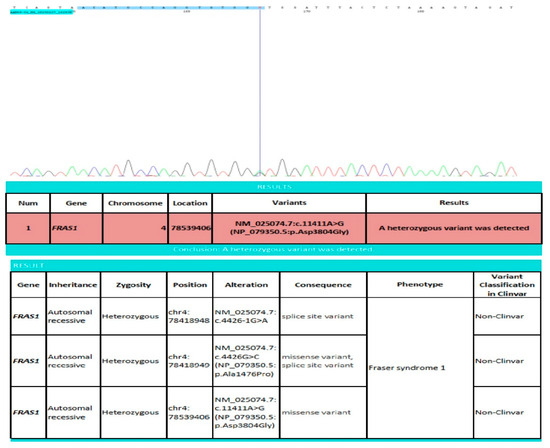
Figure 3.
Findings showing the heterozygous variation of the FRAS1 gene of the newborn. FRAS1: Fraser extracellular matrix complex subunit 1; chr: chromosome.
Until today, the baby was monitored for a systematic approach of surgical management in the future.
3. Discussion
Fraser syndrome (MIM#219000) is an autosomal recessive disorder characterized by the association of cryptophthalmos, syndactyly of the four extremities, urinary tract abnormalities, and laryngo-tracheal anomalies. This condition is due to homozygous or compound heterozygous mutations in the FRAS/FREM complex genes: FRAS1, FREM2, and GRIP1. Severe malformations have not been reported in association with the type of gene mutation. However, GRIP1 gene mutation was documented in severe forms and the fetus died early [6]. Consanguinity is a risk factor for autosomal recessive disorders. Parents with a low socioeconomic background and limited access to medical facilities are contributing factors for delayed detection of FS. Due to genetic counseling or fear of repeated FS, almost all cases were primipara. Previously, one case was recorded during the ninth pregnancy. Additionally, in one case, FS was reported during the second pregnancy and the fourth pregnancy; the third pregnancy was normal (Table 2).
The diagnosis of FS is based on clinical findings, imaging, and genetic tests for causative mutations [1]. Karyotype and imaging of the urogenital tract may be required in case of ambiguous genitalia. The diagnostic criteria for FS are divided into six major criteria (syndactyly, cryptophthalmos spectrum, urinary tract abnormalities, ambiguous genitalia, laryngeal and tracheal anomalies, and positive family history) and five minor criteria (anorectal defects, dysplastic ears, skull ossification defects, umbilical abnormalities, nasal anomalies) [8]. However, major manifestations such as cryptophthalmos and syndactyly are difficult to detect through prenatal ultrasonography, especially in the presence of oligohydramnios. Similarly, a prenatal ultrasound did not reveal or raise any suspicions for Fraser Syndrome in the present case. Only a few prenatal cases have been reported. The earliest diagnosis in our findings was between 18–19 weeks of GA. Almost all cases were diagnosed late after birth. The latest case was diagnosed 9 months postnatally. The diagnosis is usually made at birth from the obvious malformations, although it can also be diagnosed during prenatal ultrasounds. Therefore, the patient should be counseled at a consultant center when detecting one of the anomalies on ultrasound, such as ophthalmic abnormality or renal agenesis. Additionally, some indirect signs could help to investigate the malformation. For example, severe oligohydramnios may be caused by renal agenesis or hyperechoic lung and ascites in congenital obstructive syndrome of the upper airways (CHAOS) (Table 3 and Table 4). In addition, magnetic resonance imaging (MRI) could be indicated where necessary.
Generally, Fraser syndrome is highly variable, its malformations ranging from minor signs to lethal anomalies. Mostly, FS is usually characterized by eye (unilateral or bilateral cryptophthalmos, microphthalmos/anophthalmos), urinary tract (renal agenesis, bladder atresia/hypoplasia), and genital anomalies (ambiguous genitalia, cryptorchidism, underdevelopment of male genitalia). Cutaneous syndactyly occurs in both hands and feet. Patients may also present craniofacial (dysplastic ears, bifid nose, cleft lip/palate, microglossia), respiratory (laryngeal stenosis/hypoplasia), cardiac (atrial and ventricular septal defect), digestive tract (anal agenesis/imperforation, diaphragmatic hernia, large bowel obstruction), and skeletal anomalies (skull/spine malformations, clubfoot) [18,19]. In the case of severe manifestations, the disease may be fatal for the fetus; the major causes of early death after birth include laryngeal and/or kidney anomalies. According to Slavotinek et al., cryptophthalmos was present in 103/117 (88%), syndactyly in 72/117 (61.5%), and ambiguous genitalia in 20/117 (17.1%) of the cases. Ear malformations were recorded in 69/117 (59%) and renal agenesis in 53/117 (45.3%) of the cases [1]. The results were similar to our findings in the literature review of the past 20 years (Supplemental Table S1). Other abnormalities include umbilical hernias, a single umbilical artery, hydrometrocolpos secondary to vaginal atresia, and imperforate hymens [20].
Clinically, cryptophthalmos is defined as the continuous passage of skin from the forehead to the cheek and the absence of a palpebral fissure. It may be related to microphthalmia and anophthalmia [21]. Cryptophthalmos may be unilateral or bilateral and may be found in isolation or as one component of a syndrome. Upon high-resolution ultrasound examination, skin was seen to be continuous over the eyeballs on both sides and the palpebral fissure could not be identified. Echoes from the lens and ciliary apparatus could not be seen within the eyeballs, which revealed a single cavity [22]. Possible differential diagnoses should be made, which include ankyloblepharon (partial or complete adhesion of the ciliary edges of superior and inferior eyelids), blepharophimosis (narrowing of the eye opening), and symblepharon (partial or complete adhesion of the palpebral conjunctiva of the eyelid to the bulbar conjunctiva of the eyeball) [23]. Syndactyly is defined as the fusion of two or more digits (bone or soft tissue). It can be present in other syndromes, such as Apert syndrome, Carpenter syndrome, Manitoba oculotrichonal syndrome, and Lenz microphthalmia syndrome [24,25]. Relating to this abnormality, the patient is usually diagnosed after birth at an ophthalmology department or plastic surgery outpatient clinic [2,26,27,28].
Accordingly, treatment is dependent on which malformations are present, and genetic counseling is indicated. Emergency surgery is required in the case of respiratory distress [29]. Following functional stability, esthetics are considered. Management requires many step-by-step surgeries [2]. The surgical repair of FS requires a multidisciplinary team (including a maxillofacial surgeon, ear–nose–throat (ENT) specialist, nephrologist, ophthalmologist, and other specialists) [30,31]. The prognosis is dependent on the severity of the renal and laryngeal malformations. Noticeably, CHAOS is a severe abnormality [32].
To date, survival rates of FS depend on the severity of the associated anomalies, with laryngeal and/or kidney malformations as the major causes of fatality [33]. Development could be delayed or normal with the survival rate varying from 2 to 32 years. Previously, there were some reports of people surviving beyond the age of 20 years [3,31]. Some other defects could be present in the adolescent along with other abnormalities, such as craniosynostosis, hearing loss, and generalized tonic–clonic seizures [34].

Table 2.
Pregnancy characteristics of Fraser syndrome in the literature of the past 20 years.
Table 2.
Pregnancy characteristics of Fraser syndrome in the literature of the past 20 years.
| Reports (Authors, Published Year, Country) | GA at Detection | Age of Parent | Pregnancy Characteristics | History | Risk Factors | Newborn’s Gene Mutation | Parent Gene Mutation | Outcomes | |
|---|---|---|---|---|---|---|---|---|---|
| Vijayaraghavan et al. (2005), India [22] | Antenatal at 26 weeks | 24 yo | G2P1 | First baby died on 2nd day due to congenital heart disease | - | - | - | Termination of pregnancy | |
| Allali et al. (2006), Casablanca [35] | Postnatal | 24 yo | G2P2 | First newborn died after birth | Consanguineous marriage | - | - | - SVD - Term - Alive | |
| Slavotinek et al. (2006), USA [33] | Case 1 | Postnatal | - | - | - | - | c.5446delTCTTTC in exon 40 and c.6992insGG in exon 49 | - | Survival of 2 years |
| Case 2 | Postnatal | 14 yo | - | - | Unknown history of consanguinity or exposures during the pregnancy. | c.G3095A, predicting p.G1032E in heterozygous form in exon 24 | - | - SVD at 42 weeks of GA - Survival at 13 years | |
| Kumari et al. (2008), India [32] | Postnatal | - | First child | - | Second-degree consanguineous parents | - | - | - CS at full-term - Death | |
| Eskander et al. (2008), USA [12] | Postnatal | 28 yo | Primipara | - | - | - | - | IOL for postdate CS due to failed IOL Died after birth due to ARI. | |
| Dilli et al. (2010), Turkey [18] | Postnatal | 27 yo | G5P4 | - | - | - | - | Male 2420 g 46 cm Poor outcome | |
| Yassin et al. (2010), Sudan [7] | Postnatal | 25 yo | Second child | Healthy | Consanguineous parents paternal cousins had FS No regular antenatal US | - | - | SVD at term | |
| Pasu et al. (2011), England [14] | Postnatal day 1 | - | Primipara | - | Non-consanguineous parents of Southeast Asian origin. | - | - | - Vaginal ventouse delivery at 39 + 2 weeks - Male, 2.8 kg - Alive | |
| Vogel et al. (2012), Netherlands [6] | Case 1 | Prenatal | - | Third pregnancy | - | - | - Mutation analysis of GRIP1 revealed that Chr12 (GRCh37):g.66786456C/G, NM_021150.3:c.2113 + 1G/C substitution - Homozygous for the mutation | the parents and two unaffected siblings were heterozygous. | Stillborn 20 weeks |
| Case 2 | Prenatal | - | - | - | Consanguineous | - | - | Stillborn boy after 30 weeks | |
| Case 3 | Prenatal | - | - | - | Consanguineous | - | Heterozygous for a 4-bp deletion in exon 10 of GRIP1 (NM_021150.3:c.1181_1184del) (p.Lys394ThrfsX8) | Pregnancy termination at 30 weeks | |
| Hoefele et al. (2013), Germany [36] | Prenatal at 11 weeks | - | G2P0 | Stillborn at 29 weeks, suspicion of FS | Healthy | Mutation of FRAS1 gene | Both parents are heterozygous for a FRAS1 mutation. | Abortion at 13 weeks | |
| Lorena et al. (2014), Brazil [26] | Postnatal at 9 months | - | - | - | Consanguineous | - | - | Female child Alive | |
| De Bernardo et al. (2015), Italy [29] | Postnatal | - | - | - | - | Mutations c.[5752dup]; [8544 + 1G>T] p.[(Cy51918fs)], in the gene FREM2 | - | - Natural birth at 40 weeks, 3 d - Female - 3220 g - 46 cm - Apgar score 4/6 - Tracheostomy | |
| Saleem et al. (2015), Pakistan [37] | Postnatal at 3 months | - | Sixth pregnancy | Healthy | Consanguineous | Genetic analysis was not done due to financial constraints | - | -SVD at home - 2 kg | |
| Sangtani et al. (2015), India [2] | Postnatal | - | Second child | Healthy | Consanguineous | - | - | SVD Term Male | |
| Abdalla et al. (2016), Egypt [11] | Case 1 | Postnatal at 6 months | Second child | Healthy | Consanguineous | - | - | Female | |
| Case 2 | Postnatal | - | First child | Healthy | Consanguineous | - | - | Term Death after birth | |
| Case 3 | Antenatal at 28 weeks | 30 yo | Second child | Healthy | Consanguineous | - | Normal karyotype | Termination Male | |
| Case 4 | Postnatal | - | Pregnancy after 7 first trimester abortions | - | Non-consanguineous | - | - | Full term Stillborn Male | |
| Case 5 | Antenatal at 24 weeks | - | Pregnancy after 7 first trimester abortions and full-term with FS | - | Non-consanguineous | - | - | Termination | |
| Case 6 | Antenatal at 24 weeks | 21 yo | Primigravida | Healthy | - | - | - | Termination | |
| Selvaraj et al. (2016), India [38] | Antenatal at 22 weeks | 22 yo | G4P4 | - First pregnancy was terminated at 24 weeks due to suspicion of bladder outlet obstruction and ascites. - Second pregnancy was diagnosed with FS | - Consanguineous marriage - History of pregnancy with FS | - | - | Termination of pregnancy | |
| Dumitru et al. (2016), Romania [13] | Postnatal | - | G2P2 | Healthy parents | Non-consanguineous marriage | - | - | - CS - Female -1480 g - 38 cm - Death due to ARI | |
| Dar Parvez Mohi Ud Din et al. (2017), India [39] | Postnatal at 6 months | - | Second child | - | Non-consanguineous marriage | Mutation of the FRAM2 | - | - CS at 40 weeks - 2.8 kg | |
| Mbonda et al. (2019), Cameroon [24] | Postnatal at 6 months | 29 yo | Primipara | - HIV - Psychiatric disorders - Bilateral club foot. | - No antenatal care - No consanguinity - Separated parents | - | - | - SVD at term of 9 months - Female - Severe illness at age of 6 months due to pneumonia. | |
| Alsaman et al. (2020), Syria [25] | Postnal | 19 yo | G2P1 | - | Non-consanguineous marriage | - | - | - CS at 39 weeks due to cephalopelvic disproportion - 3600 g - Death due to respiratory insufficiency | |
| Ikeda et al. (2020), Japan [4] | Antenatal | 38 yo | G2P0 | - | Non-consanguineous marriage | - | - | - Terminated pregnancy at 21 weeks - Male - 520 g - 29.5 cm | |
| Waseem et al. (2021), Pakistan [28] | Posnatal at 2 months | - | Primipara | - | - Consanguineous - Low socioeconomic background | - | - | SVD Term Male 3 kg | |
| Shrestha et al. (2022), Nepal [40] | Posnatal | 24 yo | - | - | - Low socioeconomic condition - Non-consanguineous | - | - | - SVD - 1400 g - 45 cm - Apgar score of 3 pts at 1 min and 4 pts at 5 min. - Death after 3 h of birth. | |
| Golshahi et al. (2022), Iran [41] | Antenatal at 18 weeks and 3 days | 26 yo | Primipara | - | - Consanguineous marriage - No pregnancy follow-up | Absent due to high expenses | - Heterozygous mutations in the FRAS1 gene - Some other genes, including NBAS, MYL3, PKD1L1, and NUP160 | - Abortion with PGE1 - Death 600 g | |
| Laminou et al. (2022), Nigeria [15] | Postnatal day 1 | - | Sixth pregnancy | - | - Consanguineous marriage - Poorly monitored | Refused | - | - SVD - Term - Female - 2800 g - 49 cm | |
| Neri et al. (2023), Colombia [20] | Antenatal at 35 weeks | 19 yo | Primipara | Healthy | Non-consanguineous marriage | - | - | - CS for breech presentation - 36 weeks - Female - 2550 g - Apgar 2/1 min and 0/5 min - Death | |
| Ramadugu et al. (2023), India [23] | Postnatal | 23 yo | Primipara | High blood glucose levels during 6 to 7 months of pregnancy | No history of consanguineous marriage | Lack of resource settings | - | - CS - female - 3416 g - NICU admission for 2 days due to ARI. - Alive | |
| Bouba Traore et al. (2024), Nigeria [19] | Case 1 | Postnatal day 15 | 22 yo | Second child | Healthy | - | - | - | SVD Male Term 3200 g 50 cm Alive |
| Case 2 | Postnatal day 3 | 34 yo | Eighth child | Healthy | Consanguinity | - | - | SVD Female Term 2980 g 51 cm Alive | |
| Mohamed et al. (2024), Sudan [42] | Postnatal | 22 yo 24 yo | - | Malaria and urinary tract infection during pregnancy | - Poorly Monitored - Non-consanguineous marriage | - | - | Female | |
| Sajoura et al. (2024), Morocco [16] | Postnatal day 1 | 34 yo 35 yo | Primiparous | Healthy | - Non-consanguineous marriage - Poor follow-up during pregnancy | - | - | CS at 42 weeks Death at the age of 40 days due to severe ARI + hypovolaemic shock | |
| Mangla et al. (2024), India [10] | Antenatal | 21 yo | Primigravida | - | - | - | - | Pregnancy termination | |
| Present case (2015), Vietnam | Postnatal | 29 yo | Primipara | Healthy | No | Heterozygous variation of FRAS1 gene on chr4, location 78539406, variants NM_025074.7:c.11411A>G (NP_079350.5:p.Asp3804Gly) | Parental gene analysis revealed a heterozygous variant of FRAS1 gene on chromosome 4, location 78418948 and 78539406 | - IOL for SGA - CS due to failed IOL Alive | |
ARI: acute respiratory insufficiency; CS: cesarean section; d: days; G: gravida; g: gram; GRIP1: glutamate receptor interacting protein 1; IOL: induction of labor; kg: kilogram; P: parity; SGA: small gestational age; SVD: spontaneous vaginal delivery; FRAS1: Fraser extracellular matrix complex subunit 1; FREM2: FRAS1 related extracellular matrix protein 2. Sign “-”: not mentioned; weeks: weeks; yo: years old.

Table 3.
Cases of prenatal diagnosis of Fraser syndrome using ultrasound in literature of the past 20 years.
Table 3.
Cases of prenatal diagnosis of Fraser syndrome using ultrasound in literature of the past 20 years.
| Reports (Authors, Published Year, Country) | Time Point | Cryptoph Thalmos | Syndactyly | Urinary Abnormality | Respiratory Abnormality | Ear Malformation | Genital Abnormality | Others | |
|---|---|---|---|---|---|---|---|---|---|
| Vijayaraghavan et al. (2005), India [22] | 26 weeks | + Unilateral microphthalmos Skin over the eyeballs on both sides and unidentified palpebral fissure | + Bilateral cutaneous syndactyly of all fingers | + Agenesis of the right kidney | - | + Small ears and deformed | + Short penis and lacked preputial cover | SGA small omphalocele | |
| Allali et al. (2006), Casablanca [35] | - | - | - | - | - | - | - | - | |
| Slavotinek et al. (2006), USA [1] | Case 1 | - | - | - | - | - | - | - | - |
| Case 2 | - | - | - | - | - | - | - | - | |
| Eskander et al. (2008), USA [12] | - | - | - | - | - | - | - | - | |
| Kumari et al. (2008), India [32] | - | - | - | - | - | - | - | Severe intrauterine growth retardation Oligohydramnios | |
| Dilli et al. (2010), Turkey [18] | - | - | - | - | - | - | - | - | |
| Yassin et al. (2010), Sudan [7] | - | - | - | - | - | - | - | - | |
| Pasu et al. (2011), England [14] | 20 weeks | - | - | + Unilateral right renal agenesis | - | - | - | - | |
| Vogel et al. (2012), Netherlands [6] | Case 1 | - | - | - | - | + Tracheal atresia | - | - | Severely hydropic fetus and ascites. |
| Case 2 | - | + Cryptophthalmos | + Absence of bladder and kidneys | + Hyperechogenic lungs | - | - | - | ||
| Case 3 | - | - | - | + Bilateral renal agenesis | - | - | - | Severe oligohydramnios | |
| Hoefele et al. (2013), Germany [36] | 11 weeks | - | - | - | - | - | - | Bilateral cleft lip and palate. | |
| Lorena et al. (2014), Brazil [26] | - | - | - | - | - | - | - | - | |
| De Bernardo et al. (2015), Japan [29] | - | - | - | - | - | - | - | - | |
| Saleem et al. (2015), Pakistan [37] | - | - | - | - | - | - | - | - | |
| Sangtani et al. (2015), India [2] | - | - | - | - | - | - | - | - | |
| Selvaraj et al. (2016) [38] | Case 1 | 22 weeks | - | - | + Unilateral renal agenesis | + Bilateral hyperechoic enlarged lungs. Diaphragmatic inversion and flattening were seen. Congenital high airway obstruction | - | - | - Fetal heart was seen in midline, appeared compressed - Ascites - Single umbilical artery - Reduced amniotic fluid |
| Case 2 | 13–16 weeks | - | - | + Unilateral renal agenesis | + Bilateral enlarged hyperechoic lungs CHAOS | - | - | - Single umbilical artery - Ascites - Transverse section of kidney | |
| Dumitru et al. (2016), Romania [13] | - | - | - | - | - | - | - | - | |
| Dar Parvez Mohi Ud Din et al. (2017), India [22] | - | - | - | - | - | - | - | - | |
| Mbonda et al. (2019), Cameroon [24] | - | - | - | - | - | - | - | - | |
| Alsaman et al. (2020), Syria [25] | 20 and 25 weeks | - | + Bilateral syndactyly on both hands and feet | - | + Hyperechoic lungs Enlargement of the lungs | - | - | - Ascites - Shortness in upper and lower limbs, nuchal edema, hydrops fetalis - Cardiac compression - Intrahepatic biliary atresia | |
| Ikeda et al. (2020), Japan [4] | 19 weeks | - | - | + Bilateral Renal agenesis, no urinary bladder, | + Distended trachea from the caudal of the carina to the bronchi Enlarged lungs - CHAOS | - | - | Severe oligohydramnios, high volume of ascites Hepatomegaly | |
| Waseem et al. (2021), Pakistan [28] | - | - | - | - | - | - | - | - | |
| Shrestha et al. (2022), Nepal [40] | - | - | - | - | - | - | - | - | |
| Golshahi et al. (2022) [41] | 18 weeks 3 d | + Unilateral microphthalmos | + Bilateral syndactyly | + Renal agenesis (found as a lying down the adrenal sign) | + - Hyper-echogenic lungs - CHAOS | - | - | Single umbilical artery, severe oligohydramnios | |
| Laminou et al. (2022), Nigeria [15] | - | - | - | - | - | - | - | - | |
| Neri et al. (2023), Colombia [20] | 36 weeks | + Microphthalmia | - | - | - | - | - | Hypotelorism | |
| Ramadugu et al. (2023), India [23] | - | - | - | - | - | - | - | Mild oligohydramnios | |
| Bouba Traore et al. (2024), Nigeria [19] | Case 1 | - | - | - | - | - | - | - | - |
| Case 2 | - | - | - | - | - | - | - | - | |
| Mohamed et al. (2024), Sudan [42] | - | - | - | - | - | - | - | - | |
| Sajoura et al. (2024), Morocco [16] | - | - | - | - | - | - | - | - | |
| Mangla et al. (2024), India [10] | Antenatal | + Absence of an eye globe and lens | - | + Renal agenesis (sleeping adrenals sign) - Non-visualization of the urinary bladder, and Doppler of renal arteries. | - | - | - | - Severe oligohydramnios - Non-visualization of the urinary bladder | |
| Present case (2025), Vietnam | - | - | - | - | - | - | - | - FGR - Reduced AFI | |
CHAOS: Congenital high airway obstruction syndrome; weeks: weeks; Sign “-”: not mentioned; Sign “+”: present.

Table 4.
Postnatal characteristics among cases of Fraser syndrome in the literature of the past 20 years.
Table 4.
Postnatal characteristics among cases of Fraser syndrome in the literature of the past 20 years.
| Report (Authors, Published Year, Country) | Eyes | Limbs | Urinary Tract | Respiratory Tract | Others | ||
|---|---|---|---|---|---|---|---|
| Vijayaraghavan et al. (2005), India [22] | Bilateral cryptophthalmos | Syndactyly of the fingers | Right kidney was absent | - | - Low frontal hairline - Bilateral low-set ears with abnormal pinna - Broad abnormal nose - Micrognathia - Micropenis - Small omphalocele containing a Meckel’s diverticulum. | ||
| Allali et al. (2006), Casablanca [35] | - Ankyloblepharon on the left side - Cryptophthalmos on the right side - A cornea reduced to an opaque thin plate clinging to the iris without an anterior chamber and a non-individualized eyeball | Syndactyly | Renal abnormalities | Laryngeal stenosis tracheal abnormality | - Anorectal abnormalities - Ambiguous genitalia - Ear malformations - CT scan of the cranium and orbits and the transfontanelle ultrasound were normal | ||
| Slavotinek et al. (2006), USA [33] | Case 1 | Unilateral cryptophthalmos | No syndactyly | Hydronephrosis | Laryngeal stenosis/webs | - Tongue of hair extending from the anterior scalp hairline to the eyebrow - Asymmetry of the nares, stridor with minor webbing of the vocal cords, hearing impairment, hydronephrosis, and a bicornuate uterus - Inner ear dysplasia | |
| Case 2 | Cryptophthalmos with small and fused palpebral fissures bilaterally, bilateral anophthalmia | - | - | - | - Bilateral cleft lip and palate. - An extension of the anterior hairline across the lateral forehead and the nares were hypoplastic with a groove to the left of the midline of the nasal tip and a right preauricular pit - Absence of the corpus callosum with abnormal folding of the gyri, partial fusion of the thalami, dysplasia of the hippocampi and lateral ventricles, and prominent caudate heads | ||
| Eskander et al. (2008), USA [12] | Bilateral cryptophthalmos | Upper and lower extremities demonstrated prominent soft-tissue syndactyly | Left kidney and ureter agenesis | Pulmonary hypoplasia | - A flat forehead - Small nose with depressed nasal bridge - External genitalia were ambiguous and show labial malformation with clitoral enlargement Vagina was atretic and anus was patent Large intestine showed markedly distended rectosigmoid area and left adrenal gland was slightly hemorrhagic | ||
| Kumari et al. (2008), India [32] | Complete cryptophthalmos of the right eye | Complete cutaneous syndactyly of both the hands and feet | Bilateral renal agenesis | Tracheal stenosis | The ears were malformed and low-set. The nose was flat with a wide nasal bridge. The testes were found at the pelvic brim. | ||
| Dilli et al. (2010), Turkey [18] | Bilateral cryptophthalmos | Syndactyly | Bilateral polycystic kidney | Laryngeal stenosis | - Flat nose, hypoplastic nose and ears, mycrostomy, bifid uvula and cleft palate - Perineal fistula and anal atresia - Ambiguous genitalia | ||
| Yassin et al. (2010), Sudan [7] | Bilateral cryptophtalmos | Syndactyly in both hands and feet | Bilateral dysplatic kidney | - Clitoromegaly with hypoplasia of the labia - Low-set umbilicus - Depressed nasal bridge, broad nose with midline nasal groove | |||
| Pasu et al. (2011), England [14] | Right complete cryptophthalmos was noted with a palpable eyeball beneath | Clinodactyly of the right fourth and fifth toes | - | - | - Umbilical hernia, widely spaced fontanelle, bulbous nose | ||
| Vogel et al. (2012), Netherlands [6] | Case 1 | Bilateral cryptophthalmos | The fingers and toes were short with partial bilateral cutaneous syndactyly | There were no kidneys and a severely hypoplastic bladder. | The larynx was malformed and atretic; there was bilateral pulmonary hyperplasia with abnormal lung lobation. | - Low-set simple ears, micrognathia and a beaked nose with notched alae nasi - External genitalia were male with hypoplastic scrotum and malformed hypoplastic penis - Anus was abnormally positioned and appeared stenotic | |
| Case 2 | Bilateral complete cryptophthalmos, | - | - Absence of autopsy | - Absence of autopsy | Abnormal frontal hairline and broad nose | ||
| Case 3 | - | - | Bilateral renal agenesis bilateral ureter agenesis hypoplasia of the bladder | - | Hydrocephaly and dysmorphic features typical for FS | ||
| Hoefele et al. (2013), Germany [36] | - | Syndactyly of the second to the fourth finger on the right hand and between the second and the fifth toe on both feet | Atresia of the epiglottis resulting in an occlusion of the trachea | - | - | ||
| Lorena et al. (2014), Brazil [26] | Total unilateral cryptophthalmos (left side), epiphora (right side) with mucopurulent discharge | Syndactyly of the fingers and toes | - | - | - Depressed nasal bridge, low-set ears, atresia of the external auditory canal, prominent labia majora - Brachycephaly, absent septum pellucidum, prominent lateral ventricles, major skull bone defect, thinning of the brain mantle, small posterior fossa | ||
| De Bernardo et al. (2015), Japan [29] | - Bilateral cryptophthalmos Occipitofrontal circumference 34.5 cm - Left microphthalmos and malformation-like coloboma into right ocular globe with cysts and small calcification parietal anterior | Syndactyly | Right kidney agenesis | - Sub-stenosis laryngeal - Respiratory distress | - Bradycardia - Bilateral microtia - Ambiguous genitalia - Incomplete myelination of the brain | ||
| Saleem et al. (2015), Pakistan [37] | - Bilateral cryptophthalmos - Microphthalmic | Bilaterally complete syndactyly | - | - | - Spaced nipples and an umbilical hernia - Genitalia were ambiguous with phallus, complete labial fusion, and absent testes - Hypertelorism | ||
| Sangtani et al. (2015), India [2] | - | Syndactyly of hands and feet, | Enlarged hydronephrotic left kidney, and dilated left ureter Right renal agenesis | - | Bilateral cleft lip and palate | ||
| Selvaraj et al. (2016) [38] | Case 1 | - | - Partial syndactyly of fingers - Complete syndactyly of toes | - | - | - Abnormal genitalia with imperforate anus - Face was severely dysmorphic with marked hypertelorism, depressed nasal bridge, and low-set ears | |
| Case 2 | - | - Partial syndactyly of 3rd and 4th fingers - Complete syndactyly of toes | - | - | - Abnormal genitalia with imperforate anus - Abortus showing wide open eyes with dysmorphic facies | ||
| Dumitru et al. (2016), Romania [13] | Complete bilateral cryptophthalmos | Complete bilateral syndactyly on both hands and feet | Bilateral renal agenesia with agenesis of the ureters, hypertrophic adrenal glands, hypoplasic bladder. | Hypoplastic lungs | - Severe facial dysmorphism with low-set ears, flat nasal bridge, micrognathia and incomplete ossification of the skull bones. - An umbilical hernia, imperforate anus, and ambiguous genitalia - Patent ductus arteriosus and foramen ovale. | ||
| Dar Parvez Mohi Ud Din et al. (2017), India [39] | - Normal anterior and posterior segment of the right eye with coloboma of the right upper eyelid - Left complete cryptophthalmos with a palpable eyeball beneath | Syndactyly of all fingers of bilateral hands and all toes of bilateral feet | Left renal agenesis | - | - Nasal deformity - Absence of bilateral testes in the scrotum | ||
| Mbonda et al. (2019), Cameroon [24] | Bilateral cryptophthalmos | Syndactyly | - | - | - Nasal malformation - Anal imperforation with a nearby anal fistula - External genitalia anomaly | ||
| Alsaman et al. (2020), Syria [25] | Bilateral anophthalmia | Bilateral syndactyly on hands and feet | Right renal agenesis | -Lung enlargement -Autopsy: Dilated pleural lymphatic vessels, interstitial fibroblast hypertrophy and vascular wall thickening in the lung. | - Pseudo-hypertelorism - Low-set ears, flat nasal bridge - Cutaneous and subcutaneous edema, large-volume ascites - Ambiguous genitalia - Gonad and Mullerian structures were found on the left posterior pelvic wall - Autopsy: Congestion of red pulp with hemosiderin accumulation and immature white pulp of the spleen | ||
| Ikeda et al. (2020), Japan [4] | Bilateral cryptophthalmos | Syndactyly of both hands (I–IV) | Autopsy: Agenesis of the kidneys, ureters, and bladder. | Autopsy: Pleural effusion and ascites, atresia of the epiglottis with a dilated trachea, hyperinflated and heavy lungs. | Low-set, malformed ears | ||
| Waseem et al. (2021), Pakistan [28] | - Complete cryptophthalmos in the right eye with partially formed eyebrow and absence of eyelids and eyelashes - Conjunctivitis in the left eye | Cutaneous syndactyly of hands | - | - | - Hypertelorism - Low-set ears - High-arched palate with ankyloglossia - Cryptorchidism and hypospadias | ||
| Shrestha et al. (2022), Nepal [40] | Absent eyelashes | Syndactyly of toes of both feet | - | - | - Wide anterior fontanelle - Ambiguous genitalia with phallus and complete labial fusion - Abnormal face bones, flat nasal bridge, prominent occiput, hypertelorism, and dysplastic low-set ears - Single umbilical artery - Sacral dimpling with tuft of hair and protrusion of tail-like appendages at back in sacrum; likely lipomeningocele - Widely spaced nipples and low hair line - Congenital cardiac defect - Club foot | ||
| Golshahi et al. (2022) [41] | Unilateral cryptophthalmos | Cutaneous syndactyly of the four limbs | - | - | Low-set umbilicus containing a single umbilical artery | ||
| Laminou et al. (2022), Nigeria [15] | Complete bilateral cryptophthalmia | Polydactyly | - | - | Nasal depression Umbilical hernia | ||
| Neri et al. (2023), Colombia [20] | Bilateral anophthalmia | Syndactyly in upper and lower limbs | - | - | - Low-set ears - Micrognathia, broad nasal bridge - Ballooning abdomen - External female genitalia with imperforate hymen - Vaginal atresia - Uterus and vagina had cystic appearance | ||
| Ramadugu et al. (2023), India [23] | Unilateral cryptophthalmos | - | - Mild hydronephrosis in the right kidney - Irregular urinary bladder walls | - | - | ||
| Bouba Traore et al. (2024), Nigeria [19] | Case 1 | Bilateral cryptophthalmos | Syndactyly | - | - | - Elongated skull with part of the forehead invaded by hair - Nasal depression - Shape anomaly of the thorax | |
| Case 2 | Bilateral cryptophthalmos | Syndactyly | - | - | - Pseudo-bald, low-set ears - Depressed nasal root - Shape anomaly of the thorax - Anal imperforation with genital anomaly | ||
| Mohamed et al. (2024), Sudan [42] | Bilateral partial cryptophthalmos | Syndactyly Overlapping fingers Rocker-bottom feet | - | - | Multiple small atrial septal defects and ventricular septal defects. | ||
| Sajoura et al. (2024), Morocco [16] | Bilateral anophthalmia | Syndactyly | - | - | - Cleft palate - Dysmorphic facies with domed forehead, hypertelorism, micrognathia, low-set ears, and short neck. - Bilateral cryptorchidism. - Triventricular hydrocephalus. - Malformative tri-ventricular hydrocephalus, hypoplasia of brainstem and cerebellum, and poly-microgyria | ||
| Mangla et al. (2024), India [10] | Cryptophthalmos | - | Renal agenesis | - | - | ||
| Present case (2025), Vietnam | Bilateral cryptophthalmos | Syndactyly on hands and feet | Absence of the right kidney | - | - Nasal depression - Low-setears and dysplasia - Cleft palate - Tracheal stenosis, glottic web - Smaller eyeball of the right eye without crystalline lens. | ||
Autopsy was refused due to cultural constraints; Sign “-”: not mentioned. CT: computed tomography; FS: Fraser syndrome.
Since Fraser syndrome is an autosomal recessive disease, genetic counseling should be proposed for at-risk families. If both parents are carriers of a disease-causing mutation, it is recommended to inform them of the 25% risk of having an affected child for each pregnancy. A prenatal genetic diagnosis is possible if the pathogenic mutations responsible for the disease have been identified in the family. We also advise prenatal genetic screening and testing for future pregnancies for our patients. Assisted reproductive technologies could help in selecting embryos which do not carry genetic and chromosomal abnormalities [43,44]. In the case of assisted reproductive technology using in vitro fertility, a pre-implantation genetic diagnosis should be assessed. However, the long-term outcomes of offspring are a cause for concern [45,46,47]. Additionally, the risk of invasive procedures should be made known to the patient [48]. Further studies are necessary to elucidate these points.
4. Conclusions
In summary, Fraser syndrome is a rare autosomal recessive disorder characterized by syndactyly, cryptophthalmos, and variable abnormalities. Prenatal diagnosis by ultrasound remains challenging. Therefore, counseled ultrasound scans should be performed in cases of aroused suspicion.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/diagnostics15131606/s1, Supplementary Figure S1. The gene analysis of parent shows heterozygous variation relating to FRAS1 of father (A) and mother (B); Supplemental Video S1. The right unilateral cryptophthalmos with movement of the eyeball was followed-up at 1 month age. Supplemental Table S1. Summarized characteristics of Fraser syndrome in the past-20-year literature.
Author Contributions
Conceptualization, X.T.T.P., P.N.N. and X.S.H.; methodology, P.N.N.; software, P.N.N.; validation, X.T.T.P., P.N.N. and X.S.H.; formal analysis, P.N.N.; investigation, X.T.T.P., P.N.N. and X.S.H.; resources, X.S.H.; data curation, X.T.T.P. and X.S.H.; writing—original draft preparation, P.N.N.; writing—review and editing, P.N.N.; visualization, X.T.T.P. and X.S.H.; supervision, X.T.T.P. and P.N.N.; project administration, X.T.T.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This report was naturally waived by the institutional ethics committee of Tu Du Hospital for the report of clinical cases.
Informed Consent Statement
Written informed consent was obtained from the parents of patients prior to publication of this report and the use of accompanying images.
Data Availability Statement
No new data were created or analyzed in this study.
Acknowledgments
We thank the family who agreed to allow us to publish the clinical data. The authors are also grateful for all colleagues working at Tu Du Hospital. All of them contributed to taking care of this patient.
Conflicts of Interest
The authors declare that they have no competing interests.
Abbreviations
| AC | Abdominal circumference |
| AFI | Amniotic fluid index |
| ARI | Acute respiratory insufficiency |
| BPD | Biparietal diameter |
| CMV | Cytomegalovirus |
| CHAOS | Congenital high airway obstruction syndrome |
| CT | Computed tomography |
| CS | Cesarean section |
| ENT | Ear-nose throat |
| MRI | Magnetic resonance imaging |
| G6PD | Glucose-6-phosphate dehydrogenase deficiency |
| GA | Gestational age |
| HC | Head circumference |
| NIPT | Non-invasive prenatal test |
| IOL | Induction of labor |
| FL | Femoral length |
| FGR | Fetal growth restriction |
| FS | Fraser syndrome |
| FRAS1 | Fraser extracellular matrix complex subunit 1 |
| FREM2 | FRAS1 related extracellular matrix protein 2 |
| GRIP1 | Glutamate receptor interacting protein 1 |
| SLC25A13 | Solute carrier family 25 member 13 |
| SGA | Small gestational age |
| SVD | Spontaneous vaginal delivery |
References
- Slavotinek, A.M.; Tifft, C.J. Fraser syndrome and cryptophthalmos: Review of the diagnostic criteria and evidence for phenotypic modules in complex malformation syndromes. J. Med. Genet. 2002, 39, 623. [Google Scholar] [CrossRef] [PubMed]
- Sangtani, J.K.; Kamble, R.H.; Shrivastav, S.; Sharma, N. Fraser syndrome without cryptophthalmos: A rare case report. J. Cleft Lip Palate Craniofacial Anom. 2015, 2, 139–142. [Google Scholar] [CrossRef]
- Bouaoud, J.; Olivetto, M.; Testelin, S.; Dakpe, S.; Bettoni, J.; Devauchelle, B. Fraser syndrome: Review of the literature illustrated by a historical adult case. Int. J. Oral. Maxillofac. Surg. 2020, 49, 1245–1253. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, S.; Akamatsu, C.; Ijuin, A.; Nagashima, A.; Sasaki, M.; Mochizuki, A.; Nagase, H.; Enomoto, Y.; Kuroda, Y.; Kurosawa, K.; et al. Prenatal diagnosis of Fraser syndrome caused by novel variants of FREM2. Hum. Genome Var. 2020, 7, 32. [Google Scholar] [CrossRef] [PubMed]
- Smyth, I.; Du, X.; Taylor, M.S.; Justice, M.J.; Beutler, B.; Jackson, I.J. The extracellular matrix gene Frem1 is essential for the normal adhesion of the embryonic epidermis. Proc. Natl. Acad. Sci. USA 2004, 101, 13560–13565. [Google Scholar] [CrossRef] [PubMed]
- Vogel, M.J.; van Zon, P.; Brueton, L.; Gijzen, M.; van Tuil, M.C.; Cox, P.; Schanze, D.; Kariminejad, A.; Ghaderi-Sohi, S.; Blair, E.; et al. Mutations in GRIP1 cause Fraser syndrome. J. Med. Genet. 2012, 49, 303. [Google Scholar] [CrossRef]
- Yassin, A.; Abdulmonim, S.; Al-asad, S.; Hashim, A.; Hassan, A. Sudanese infant with Fraser syndrome. Sudan J. Med. Sci. 2010, 5, 303–305. [Google Scholar] [CrossRef][Green Version]
- van Haelst, M.M.; Scambler, P.J.; Fraser Syndrome Collaboration Group Hennekam, R.C.M. Fraser syndrome: A clinical study of 59 cases and evaluation of diagnostic criteria. Am. J. Med. Genet. Part A 2007, 143A, 3194–3203. [Google Scholar] [CrossRef]
- Berg, C.; Geipel, A.; Germer, U.; Pertersen-Hansen, A.; Koch-Dörfler, M.; Gembruch, U. Prenatal detection of Fraser syndrome without cryptophthalmos: Case report and review of the literature. Ultrasound Obstet. Gynecol. 2001, 18, 76–80. [Google Scholar] [CrossRef]
- Mangla, M.; Kaliappan, A.; Srirambhatla, A.; Chandrupatla, M.; Motwani, R.; Kumar, N. Fraser syndrome with limb reduction defect: A rare and unique anatomic variation. Surg. Radiol. Anat. 2024, 46, 501–506. [Google Scholar] [CrossRef]
- Abdalla, E.M.; Zayed, L.H.; Issa, N.M.; Amin, A.K. Fraser syndrome: Phenotypic variability and unusual findings in four Egyptian families. Egypt. J. Med. Hum. Genet. 2016, 17, 233–238. [Google Scholar] [CrossRef][Green Version]
- Eskander, B.S.; Shehata, B.M. Fraser syndrome: A new case report with review of the literature. Fetal Pediatr. Pathol. 2008, 27, 99–104. [Google Scholar] [CrossRef] [PubMed]
- Dumitru, A.; Costache, M.; Lazaroiu, A.M.; Simion, G.; Secara, D.; Cirstoiu, M.; Emanoil, A.; Georgescu, T.A.; Sajin, M. Fraser Syndrome—A Case Report and Review of Literature. Maedica 2016, 11, 80–83. [Google Scholar]
- Pasu, S.; Dhir, L.; Mackenzie, S.; Thompson, G. Fraser Syndrome: Case Report with Review of Literature. J. Surg. Res. 2011, 1, 1–3. [Google Scholar] [CrossRef]
- Laminou, L.; Habou, O.; Amadou, M.; Hadjia, A.K.Y.; Abdou, A. Fraser syndrome: About a Case and Review of the Literature. J. Surg. Res. 2022, 5, 585–587. [Google Scholar] [CrossRef]
- Sajoura, C.; Ech-Chebab, M.; Ayyad, A.; Messaoudi, S.; Amrani, R. Fraser Syndrome: A Case Report. Open J. Pediatr. 2024, 14, 476–481. [Google Scholar] [CrossRef]
- Bustillo-Sierra, C.M.; Alvarenga-Calidonio, R.H. Fraser syndrome: A case report. Rev. Mex. Pediatr. 2019, 86, 155–158. [Google Scholar]
- Dilli, D.; Kanmaz, H.; Oğuz, Ş.; Dilmen, U. A Case Report of Fraser Syndrome. J. Child 2010, 10, 144–148. [Google Scholar] [CrossRef]
- Traore, H.A.B.; Issiaka, M.; Laouali, L.; Yakoura, A.K.; Amza, A. Differential Contribution of Fraser Syndrome and Anophthalmos: 4 Cases and Review of the Literature. Adv. Clin. Med. Res. 2024, 5, 1–11. [Google Scholar] [CrossRef]
- Dávila Neri, I.; Farias Vela, A.P.; Aragón Mendoza, R.L.; Gallo Roa, R.; Russo Vizcaino, G.C. Prenatal hydrometrocolpos as an unusual finding in Fraser syndrome. Case Rep. 2023, 12, 20220038. [Google Scholar] [CrossRef]
- Searle, A.; Shetty, P.; Melov, S.J.; Alahakoon, T.I. Prenatal diagnosis and implications of microphthalmia and anophthalmia with a review of current ultrasound guidelines: Two case reports. J. Med. Case Rep. 2018, 12, 250. [Google Scholar] [CrossRef] [PubMed]
- Vijayaraghavan, S.B.; Suma, N.; Lata, S.; Kamakshi, K. Prenatal sonographic appearance of cryptophthalmos in Fraser syndrome. Ultrasound Obstet. Gynecol. 2005, 25, 629–630. [Google Scholar] [CrossRef] [PubMed]
- Ramadugu, R.; Kuppili, S.; Suvvari, T.K.; Lella, V.V.; Thomas, V. A Rare Case of Complete Cryptophthalmos and Suspected Fraser’s Syndrome in a Female Neonate. Clin. Med. Insights Case Rep. 2023, 16, 11795476231189042. [Google Scholar] [CrossRef]
- Mbonda, A.; Endomba, F.T.; Kanmounye, U.S.; Nkeck, J.R.; Tochie, J.N. Diagnosis of Fraser syndrome missed out until the age of six months old in a low-resource setting: A case report. BMC Pediatr. 2019, 19, 292. [Google Scholar] [CrossRef] [PubMed]
- Alsaman, M.Z.B.; Agha, S.; Sallah, H.; Badawi, R.; Kitaz, M.N.; Assani, A.; Nawfal, H. Bilateral anophthalmia and intrahepatic biliary atresia, two unusual components of Fraser syndrome: A case report. BMC Pregnancy Childbirth 2020, 20, 358. [Google Scholar] [CrossRef]
- Lorena, S.H.T.; Gonçalves, E.D.; Machado, M.A.C.; Jablinski, C.E.C.; Briceño, C.A.; Silva, J.A.F. Fraser Syndrome: Case report in lacrimal system. Rev. Bras. Oftalmol. 2014, 73, 123–125. [Google Scholar] [CrossRef][Green Version]
- Das, D.; Modaboyina, S.; Raj, S.; Agrawal, S.; Bajaj, M.S. Clinical features and orbital anomalies in Fraser syndrome and a review of management options. Indian J. Ophthalmol. 2022, 70, 2559–2563. Available online: https://journals.lww.com/ijo/fulltext/2022/07000/clinical_features_and_orbital_anomalies_in_fraser.63.aspx (accessed on 12 May 2025). [CrossRef]
- Waseem, M.; Waseem, H.; Khani, M.N. Fraser syndrome: A case report. KHYBER Med. Univ. J. 2021, 13, 47–48. [Google Scholar]
- De Bernardo, G.; Giordano, M.; Di Toro, A.; Sordino, D.; De Brasi, D. Prenatal diagnosis of Fraser syndrome: A matter of life or death? Ital. J. Pediatr. 2015, 41, 86. [Google Scholar] [CrossRef]
- Saleh, G.M.; Hussain, B.; Verity, D.H.; Collin, J.R.O. A Surgical Strategy for the Correction of Fraser Syndrome Cryptophthalmos. Ophthalmology 2009, 116, 1707–1712.e1. [Google Scholar] [CrossRef]
- Falls, M.E.; Rabinowitz, M.P.; Carrasco, J.R.; Rabinowitz, M.R. Endoscopic Management of Lacrimal System Dysgenesis and Dacryocystoceles in Fraser Syndrome: A Case Report and Literature Review. Allergy Rhinol. 2018, 9, 2152656718804905. [Google Scholar] [CrossRef] [PubMed]
- Cavoretto, P.; Molina, F.; Poggi, S.; Davenport, M.; Nicolaides, K.H. Prenatal diagnosis and outcome of echogenic fetal lung lesions. Ultrasound Obstet. Gynecol. 2008, 32, 769–783. [Google Scholar] [CrossRef] [PubMed]
- Kalpana Kumari, M.K.; Kamath, S.; Mysorekar, V.V.; Nandini, G. Fraser syndrome. Indian J Pathol Microbiol. 2008, 51, 228–229. [Google Scholar] [CrossRef] [PubMed]
- Slavotinek, A.; Li, C.; Sherr, E.H.; Chudley, A.E. Mutation analysis of the FRAS1 gene demonstrates new mutations in a propositus with Fraser syndrome. Am J Med Genet. A 2006, 140A, 1909–1914. [Google Scholar] [CrossRef]
- Allali, B.; Hamdani, M.; Lamari, H.; Rais, L.; Benhaddou, M.; Kettani, A.; Lahbil, D.; Amraoui, A.; Zaghloul, K. Syndrome de Fraser: À propos d′un cas. J. Fr. Ophtalmol. 2006, 29, 184–187. [Google Scholar] [CrossRef]
- Hoefele, J.; Wilhelm, C.; Schiesser, M.; Mack, R.; Heinrich, U.; Weber, L.T.; Biskup, S.; Daumer-Haas, C.; Klein, H.G.; Rost, I. Expanding the mutation spectrum for Fraser syndrome: Identification of a novel heterozygous deletion in FRAS1. Gene 2013, 520, 194–197. [Google Scholar] [CrossRef] [PubMed]
- Saleem, A.A.; Siddiqui, S.N. Fraser Syndrome. J. Coll. Physicians Surg. Pak. 2015, 25 (Suppl. 2), S124–S126. [Google Scholar]
- Shahid, S.L.R. Fraser Syndrome: Prenatal Detection at 16 Weeks of Gestation. J. Fetal Med. 2016, 3, 97–100. [Google Scholar]
- Din, D.P.M.U.; Ahmad, M.L.; Anjum, W.A.; Ali, L.F.; Ahmad, B.B.; Yasir, M.; Gulshan, W.N. Fraser syndrome: Case report with review of literature. Int. J. Adv. Res. 2016, 5, 588–591. [Google Scholar] [CrossRef]
- Shrestha, S.; Thani, K.P.; Keshari, M.; Shrestha, A. Fraser Syndrome: A Rare Case Report. J. Karnali Acad. Health Sci. 2022, 5, 3. [Google Scholar] [CrossRef]
- Golshahi, F.; Moradi, B.; Jabbari, F.; Ahmadi, M. A case of Fraser Syndrome Diagnosed by Ultrasound as a Single Modality; Necessity of Genetic Confirmation? J. Obstet. Gynecol. Cancer Res. 2022, 7, 574–577. [Google Scholar] [CrossRef]
- Altayeb, M.A.M.; Kheir, A.E.M.; Abbadi, N.S.; Elkhazin, A.A.S. Fraser Syndrome; Case report and Literature Review. Sudan. J. Health Sci. 2024, 2, 85–92. [Google Scholar]
- Trinh, N.B.; Vuong, A.D.B.; Nguyen, P.N. Successful Management by Selective Embryo in the Carnitine-Acylcarnitine Translocase Deficiency with SLC25A20 C. 199-10T> G Variation: The First Case Report from Vietnam and Literature. Oman Med. J. 2023, 27, 6809–6823. [Google Scholar] [PubMed]
- Bich Trinh, N.; Dinh Bao Vuong, A.; Nhon Nguyen, P. Successful management of pregnancy in Turner syndrome (Monosomy X): A rare condition-based learning experience from Vietnam. Int. J. Reprod. Biomed. 2024, 22, 411–416. [Google Scholar] [CrossRef] [PubMed]
- Gullo, G.; Scaglione, M.; Cucinella, G.; Perino, A.; Chiantera, V.; D’Anna, R.; Laganà, A.S.; Buzzaccarini, G. Impact of assisted reproduction techniques on the neuro-psycho-motor outcome of newborns: A critical appraisal. J. Obstet. Gynaecol. 2022, 42, 2583–2587. [Google Scholar] [CrossRef] [PubMed]
- Gullo, G.; Basile, G.; Cucinella, G.; Greco, M.E.; Perino, A.; Chiantera, V. Marinelli S. Fresh vs. frozen embryo transfer in assisted reproductive techniques: A single center retrospective cohort study and ethical-legal implications. Eur. Rev. Med. Pharmacol. Sci. 2023, 27, 6809–6823. [Google Scholar] [CrossRef] [PubMed]
- Gullo, G.; Scaglione, M.; Laganà, A.S.; Perino, A.; Andrisani, A.; Chiantera, V.; Cucinella, G.; Gitas, G.; Barra, F.; Riemma, G. Assisted Reproductive Techniques and Risk of Congenital Heart Diseases in Children: A Systematic Review and Meta-analysis. Reprod. Sci. 2023, 30, 2896–2906. [Google Scholar] [CrossRef]
- Alteri, A.; Cermisoni, G.C.; Pozzoni, M.; Gaeta, G.; Cavoretto, P.I.; Viganò, P. Obstetric, neonatal, and child health outcomes following embryo biopsy for preimplantation genetic testing. Hum. Reprod. Update 2023, 29, 291–306. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).