Abstract
The treatment of non-small cell lung cancer has dramatically changed over the last decade through the use of targeted therapies and immunotherapies. Implementation of these treatment regimens relies on detailed knowledge regarding each tumor’s specific genomic profile, underscoring the necessity of obtaining superior diagnostic tissue specimens. While these treatment approaches are commonly utilized in the metastatic setting, approval among earlier-stage disease will continue to rise, highlighting the importance of early and comprehensive biomarker testing at the time of diagnosis for all patients. Pulmonologists play an integral role in the diagnosis and staging of non-small cell lung cancer via sophisticated tissue sampling techniques. This multifaceted review will highlight current indications for the use of targeted therapies and immunotherapies in non-small cell lung cancer and will outline the quality of various diagnostic approaches and subsequent success of tissue biomarker testing. Pulmonologist-specific methods, including endobronchial ultrasound and guided bronchoscopy, will be examined as well as other modalities such as CT-guided transthoracic biopsy and more.
1. Introduction
Despite a consistent decline in incidence and mortality over the past two decades, lung cancer remains the leading cause of cancer-related mortality for both men and women in the United States (US) and worldwide [1,2]. Non-small cell lung cancer (NSCLC) accounts for approximately 82% of all lung cancer diagnoses [3]. Unfortunately, a dismal 26% five-year overall survival (OS) rate continues to plague this disease [4]. Consequently, efforts to improve diagnosis and treatment remain at the forefront of cancer research. Precision medicine has recently revolutionized the NSCLC treatment landscape, offering benefits including improved progression-free survival (PFS) and OS through the use of targeted therapies and immunotherapies.
Per National Comprehensive Cancer Network (NCCN) guidelines, targeted therapies are now the preferred, first-line agents for metastatic NSCLC among tumors harboring associated oncogenic driver mutations [5]. Despite limited approval in earlier stage disease, ongoing research will continue to transform this space [6]. NCCN guidelines highlight immunotherapy indications for metastatic and locally advanced NSCLC along with resectable disease in the adjuvant and neoadjuvant settings [7]. Ensuring all patients have access to appropriate, individualized therapies requires comprehensive testing at the time of diagnosis. A united multidisciplinary approach among all involved physicians is imperative to achieve this goal.
Pulmonologists are at the forefront of lung cancer diagnoses and play an important role when obtaining the initial biopsy and determining disease staging. Without early and adequate tissue specimens acceptable for histopathologic analysis, immunohistochemistry (IHC), and genomic sequencing, providing appropriate treatment recommendations is impaired. This multifaceted review will highlight current indications for targeted therapies and immunotherapies in NSCLC and the important role of biomarkers and IHC analysis. Additionally, various diagnostic modalities will be explored, outlining the quality of each individual approach.
2. Indications for Targeted Therapy
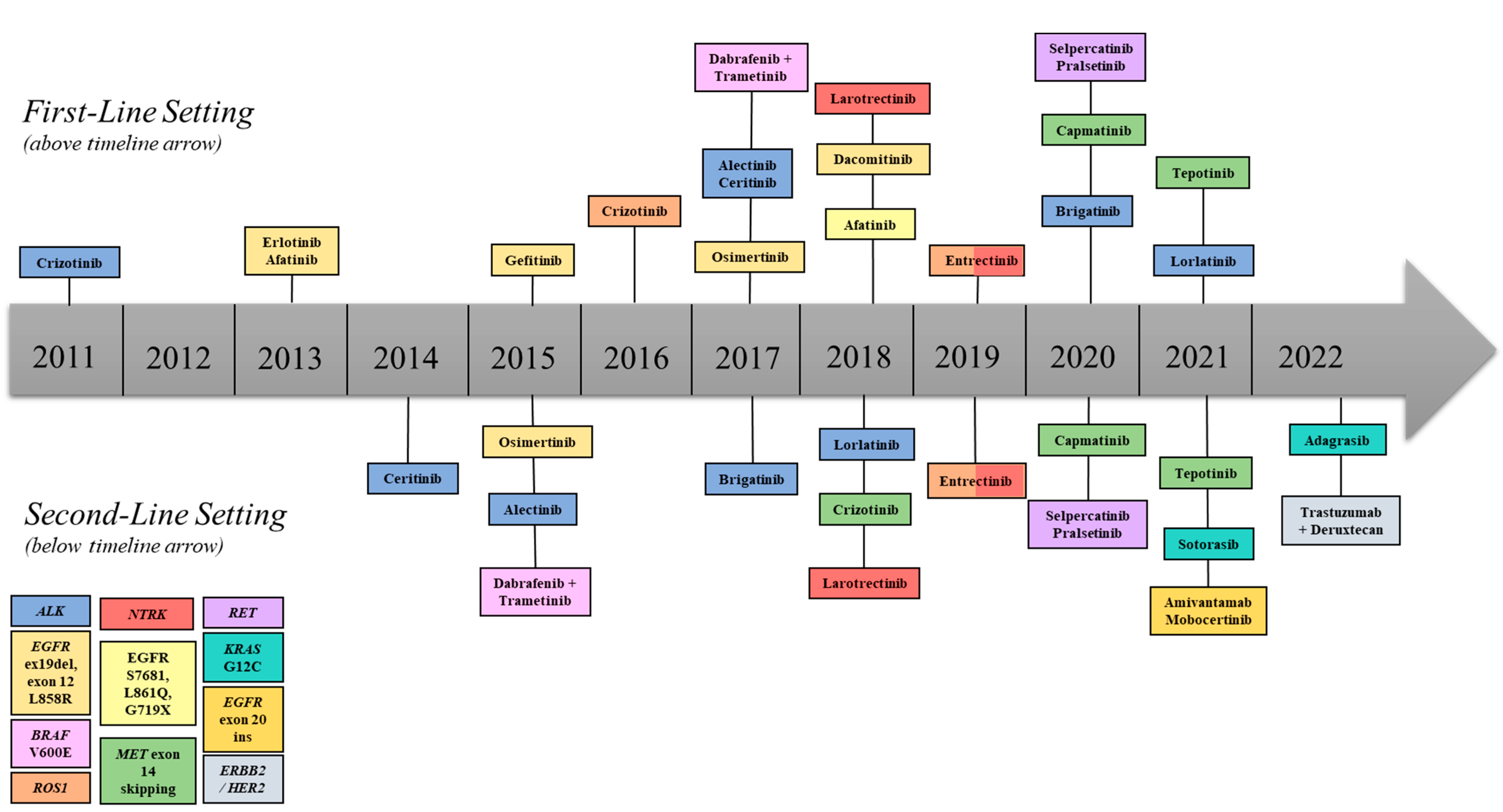
Evolution of targeted therapies is a direct result of improved knowledge regarding the biologic basis of tumor-specific genomic alterations and development of sophisticated means for detecting such abnormalities. Currently, many NSCLC oncogenic driver mutations are recognized with respective targeted drug therapies. These biomarkers include EGFR (epidermal growth factor receptor) mutations, ALK (anaplastic lymphoma kinase) rearrangements, ROS1 (c-ros oncogene 1) rearrangements, BRAF (v-raf murine sarcoma viral oncogene homolog B1 mutations, NTRK (neurotrophic tyrosine receptor kinase) gene fusions, MET (mesenchymal-epithelial transition factor) mutations/amplifications, RET (rearranged during transfection) rearrangements, ERBB2/HER2 (erythroblastic oncogene B/human epidermal growth factor 2 mutations/amplifications, and KRAS (kirsten rat sarcoma viral oncogene homolog) mutations. Not only are associated targeted therapies highly effective, with impressive response rates, but they also possess favorable side effect profiles compared to cytotoxic chemotherapy. Those targeting EGFR and ALK alterations are the most notable and widely studied. Other oncogenic driver mutations and associated therapies are outlined in Table 1/Figure 1.

Table 1.
Oncogenic driver mutations and respective first- and subsequent-line targeted therapies recommended by the NCCN [7,8,9]. * NCCN preferred agent.
Figure 1.
Timeline of FDA-approved targeted therapies for NSCLC. First-line therapies depicted above, and second-line therapies depicted below the central arrow.
2.1. EGFR-Mutant NSCLC
In 2004, EGFR mutations were first described among NSCLC [10], with exon 19 deletions and exon 21 L858R point mutations promoting tumorigenesis in approximately 20% of all lung cancers of adenocarcinoma histology [8]. In 2013, the US Food and Drug Administration (FDA) approved the first EGFR-tyrosine kinase inhibitor (TKI), erlotinib, in the first-line setting for EGFR-mutant, metastatic NSCLC. The phase III EURTAC trial demonstrated a median PFS benefit of 4.5 months compared to platinum doublet chemotherapy (HR 0.37; 95% CI 0.25–0.54; p < 0.0001) along with improved tolerability [10,11] Second-generation EGFR-TKIs then emerged followed by the third-generation agent, osimertinib. While active against common EGFR-sensitizing mutations, osimertinib is also uniquely selective for the T790M mutation, a common resistance mechanism to the first- and second-generation EGFR-TKIs [12]. In fact, osimertinib was first approved in 2015, in the second-line setting, for patients whose tumors developed T790M-positive resistance to earlier agents [12]. Later, the efficacy of osimertinib in previously untreated, metastatic NSCLC was evaluated against first-generation EGFR-TKIs in the phase III FLAURA trial. Patients treated with osimertinib derived a 54% reduction in the risk of disease progression or death (HR 0.46; 95% CI 0.37–0.57; p < 0.0001), with a median OS of 38.6 months [13,14]. Furthermore, osimertinib displayed superior penetration of the central nervous system (CNS) with significantly greater PFS among this subgroup [13]. This subsequently revolutionized the treatment of such patients, as many with CNS metastases may forego brain radiotherapy until much later in their disease course. Given the impressive results in overall efficacy and tolerability, in 2018, oral osimertinib became, and currently remains, standard of care (SOC) for stage IV, EGFR-mutant (ex19del, L858R) NSCLC.
Recently, EGFR-TKIs have also led the way for implementation of targeted therapies in early-stage, resectable disease. In the phase III ADAURA trial, adjuvant osimertinib was compared to placebo among EGFR-mutant, stage IB-IIIA NSCLC patients following complete resection. Although not required, 60% of patients within each treatment arm received adjuvant chemotherapy, as SOC, prior to enrollment [15]. Osimertinib increased median disease-free survival by 7.2 months for those with stage II-IIIA disease, with 89% of the osimertinib and 59% of the placebo cohorts still alive and disease free at 24 months (HR 0.20; 99.12% CI 0.14–0.30; p < 0.001) [15]. Additionally, osimertinib decreased the risk of CNS disease recurrence or death by 82% at 24 months [15]. Outcomes of this trial led to the FDA approval of adjuvant osimertinib, and since 2021, the NCCN has recommended up to three years of adjuvant osimertinib, with or without adjuvant chemotherapy, for resected stage IIB-IIIA or high risk stage IB-IIA, EGFR-mutant NSCLC [16]. Although treatment with EGFR-TKIs is not yet established in the neoadjuvant or stage IIIB/C settings, the ongoing, respective NeoADAURA and LAURA trials may provide new future direction for this innovative class of targeted therapy [6].
2.2. ALK-Rearranged NSCLC
ALK rearrangements were first described in 2007. Crizotinib, targeting multiple alterations, including ALK, MET, and ROS1, received accelerated FDA approval in 2011 for ALK-rearranged NSCLC due to impressive results from phase I and II trials [17]. Phase III studies followed, including PROFILE 1014, comparing crizotinib to platinum doublet chemotherapy in the first-line setting for metastatic NSCLC harboring ALK rearrangements. Oral crizotinib decreased risk of disease progression or death by 55% compared to standard chemotherapy (HR 0.45; CI 0.35–0.60; p < 0.001) with additional benefits observed for objective response rate, duration of response, one-year survival, and patient-reported global quality of life [18]. Since then, multiple agents have been approved including alectinib, the first next-generation agent compared to crizotinib in the phase III ALEX trial. Alectinib showed a remarkable median PFS advantage of 23.9 months (HR 0.43; CI 0.32–0.58; p < 0.001) [19], as well as superior CNS disease control compared to crizotinib with an 11.8-month median CNS response duration advantage (HR 0.16, CI 0.10–0.28; p < 0.001) [20]. While most recently published OS data remains immature, the five-year OS rate for the alectinib and crizotinib cohorts were 62.5% and 45.5%, respectively [19]. Following this trial, in 2017, the FDA approved first-line alectinib for metastatic, ALK-rearranged NSCLC. While ALK-TKIs have not been approved for early-stage disease, the ongoing, phase III ALCHEMIST-ALK and ALINA trials are evaluating crizotinib and alectinib, respectively, in the adjuvant setting, along with the phase II ALNEO trial that is evaluating alectinib in the neoadjuvant setting [12].
3. Indications for Immunotherapy
Tumors evade detection by the host immune system through immune checkpoint pathways, most notably the programmed cell death protein-1 (PD-1)/programmed death-ligand 1 (PD-L1) axis. Development of highly selective antibodies targeting this pathway has also revolutionized the treatment of NSCLC. Approximately 25% of NSCLC patients have high tumor expression of PD-L1, defined as a tumor proportion score (TPS) greater than 50% [21,22] as measured by IHC. Tumors with high PD-L1 expression have a greater likelihood of response to immune checkpoint inhibitors (ICIs) [21,22].
In 2016, the landmark phase III clinical trial, KEYNOTE-024, established immunotherapy as the first-line treatment for metastatic NSCLC with high PD-L1 expression without concomitant EGFR mutations or ALK rearrangements. Patients treated with pembrolizumab monotherapy had an improved median PFS by 4.3 months compared with the chemotherapy group (HR 0.50; 95% CI 0.37–0.68; p < 0.001) [23]. Likewise, median OS improved by 15.8 months among the pembrolizumab arm (HR 0.63; 95% CI 0.47–0.86) [24]. Adverse events occurred less frequently in those treated with pembrolizumab and the rates of serious treatment-related adverse events were similar between the two groups [23,24].
Since promising results from KEYNOTE-024, immunotherapy has been studied in earlier stage disease. The phase III PACIFIC trial investigated the use of durvalumab, an anti-PD-L1 antibody, as consolidative therapy following definitive chemoradiation compared to placebo in patients with nonoperable stage III NSCLC. Median PFS among the durvalumab arm improved by 11.2 months compared to placebo (HR 0.52; 95% CI 0.42–0.65; p < 0.001) [25]. The most recent predicted five-year OS rate for patients treated with durvalumab and placebo is 42.9% and 33.4%, respectively [26]. Of note, a subgroup analysis of patients with EGFR mutations showed no benefit from durvalumab [25], underscoring the need for comprehensive biomarker testing among patients diagnosed with locally advanced NSCLC.
The next frontier of immunotherapy research in NSCLC is in the perioperative period for early-stage disease. In 2022, initial results from CheckMate816 showed the addition of PD-1 inhibitor, nivolumab, to neoadjuvant platinum-based chemotherapy performed better than neoadjuvant chemotherapy alone for stage IB-IIIA, resectable NSCLC. The primary end-point, median event-free survival for nivolumab plus chemotherapy reached 31.6 months versus 20.8 months for chemotherapy alone (HR 0.63; CI 0.43–0.91; p = 0.005) [27]. Furthermore, pathologic response, correlating with long-term benefits of neoadjuvant therapy, was also evaluated. Impressively, 24% of patients treated with the addition of nivolumab achieved a complete pathologic response upon surgical resection, compared to only 2.2% of patients treated solely with chemotherapy [27]. While long-term outcome data remains to be seen, results from CheckMate816 have led to the approval of nivolumab in the neoadjuvant setting [27]. In the adjuvant, phase III IMpower010 trial, the subsequent addition of PD-L1 inhibitor, atezolizumab, to adjuvant platinum-based chemotherapy demonstrated a 34% disease-free survival advantage for patients with stage II-IIIA, PD-L1-positive NSCLC who underwent surgical resection [28]. Hence, for appropriate patients who do not undergo neoadjuvant chemoimmunotherapy, atezolizumab is approved in the adjuvant setting [7]. Several other phase III trials are currently undergoing accrual to assess chemotherapy plus adjuvant PD-L1 blockade in resectable NSCLC [29].
4. Indications for Biomarker Testing
As evidenced above, appropriate biomarker and PD-L1 testing are imperative to provide optimal treatment regimens for patients with NSCLC. Comprehensive testing should be implemented regardless of tumor histology. Traditionally, testing all nonsquamous histologies was advised; however, squamous cell carcinomas should also be considered. Approximately 5–10% of these tumors will harbor a targetable mutation; furthermore, tumor heterogeneity cannot be ruled out [16]. While individual tumor histology (e.g., adenocarcinoma or squamous cell carcinoma) should not be the factor to preclude or promote biomarker testing, it is particularly helpful to guide systemic therapy in addition to immunotherapy in the absence of genomic alterations, as the effectiveness of different cytotoxic chemotherapy agents may be affected by intrinsic mechanisms of resistance inherent to different subtypes of NSCLC [30]. In patients with metastatic NSCLC with no actionable genomic alterations, low PD-L1 expression and/or high tumor burden cytotoxic chemotherapy remain the cornerstone of systemic therapy. Moreover, FDA-approved regimens containing the anti-angiogenic agent bevacizumab are contraindicated in patients with squamous NSCLC in view of an increased risk of high rates of life-threatening hemoptysis [31].
When considering disease stage, the NCCN recommends reflex PD-L1 IHC analysis for all locally advanced and metastatic disease. Additionally, patients with stage II-IIIA NSCLC who undergo surgical resection and are candidates for adjuvant chemotherapy should also be tested for PD-L1 to determine eligibility for adjuvant atezolizumab. Similarly, genomic testing is recommended for all metastatic disease, and at a minimum, testing for EGFR mutations is recommended among stage I–III disease [7]. Arguably, comprehensive genomic and PD-L1 testing should be implemented, regardless of stage, immediately at the time of diagnosis. Frequently, tissue biopsy is obtained prior to staging confirmation, and automatic reflex testing can expeditiously guide therapy once definitive stage is determined. A pragmatic example is the patient with early-stage disease who may be a candidate for neoadjuvant chemoimmunotherapy, provided the tumor does not harbor EGFR or ALK alterations. Additionally, many patients with early and locally advanced disease will progress, necessitating this tumor-specific information. If previously obtained, this prevents risks associated with additional invasive procedures and saves valuable time, money, and resources at an important treatment juncture. Furthermore, ongoing clinical trials continue to evaluate the efficacy of numerous targeted therapies in the adjuvant and neoadjuvant arenas, which will likely showcase promising results leading to new FDA approvals. Ultimately, understanding a tumor’s genomic profile can expedite the implementation of late-breaking effective therapies.
Finally, not only is comprehensive genomic testing important when utilizing SOC treatments, but it is equally necessary when considering clinical trial participation, with enrollment eligibility often hinging upon these results. Unsurprisingly, trials involving targeted therapies require this information, as do those involving immunotherapies, as certain genomic alterations are known to augment ICI effectiveness. Assuming each patient is a clinical trial candidate at the time of diagnosis will save time and, more importantly, the risk of an additional future procedure.
5. Disparities in Biomarker Testing
While biomarker testing directly informs the selection of treatment options for NSCLC, research shows next generation sequencing (NGS) is underutilized in everyday practice. A review from a real-world electronic health record database showed that NGS-based testing was only observed among 48.7% of all patients with advanced/metastatic NSCLC (n = 14,768) and only 35.5% of patients with nonsquamous NSCLC had NGS-based testing prior to initiation of first-line therapy [32]. Moreover, notable racial disparities were found. For advanced/metastatic NSCLC, black/African-American patients were less likely to undergo biomarker testing at any point during their treatment trajectories (73.6% vs. 76.4%, p = 0.03), especially prior to first-line therapy (25.8% vs. 31.5%; p < 0.0001), compared to their white counterparts [32]. As biomarker testing has become standard, follow-up research is needed to ensure all patients receive equitable care.
6. Tissue Specimen & Diagnostic Testing
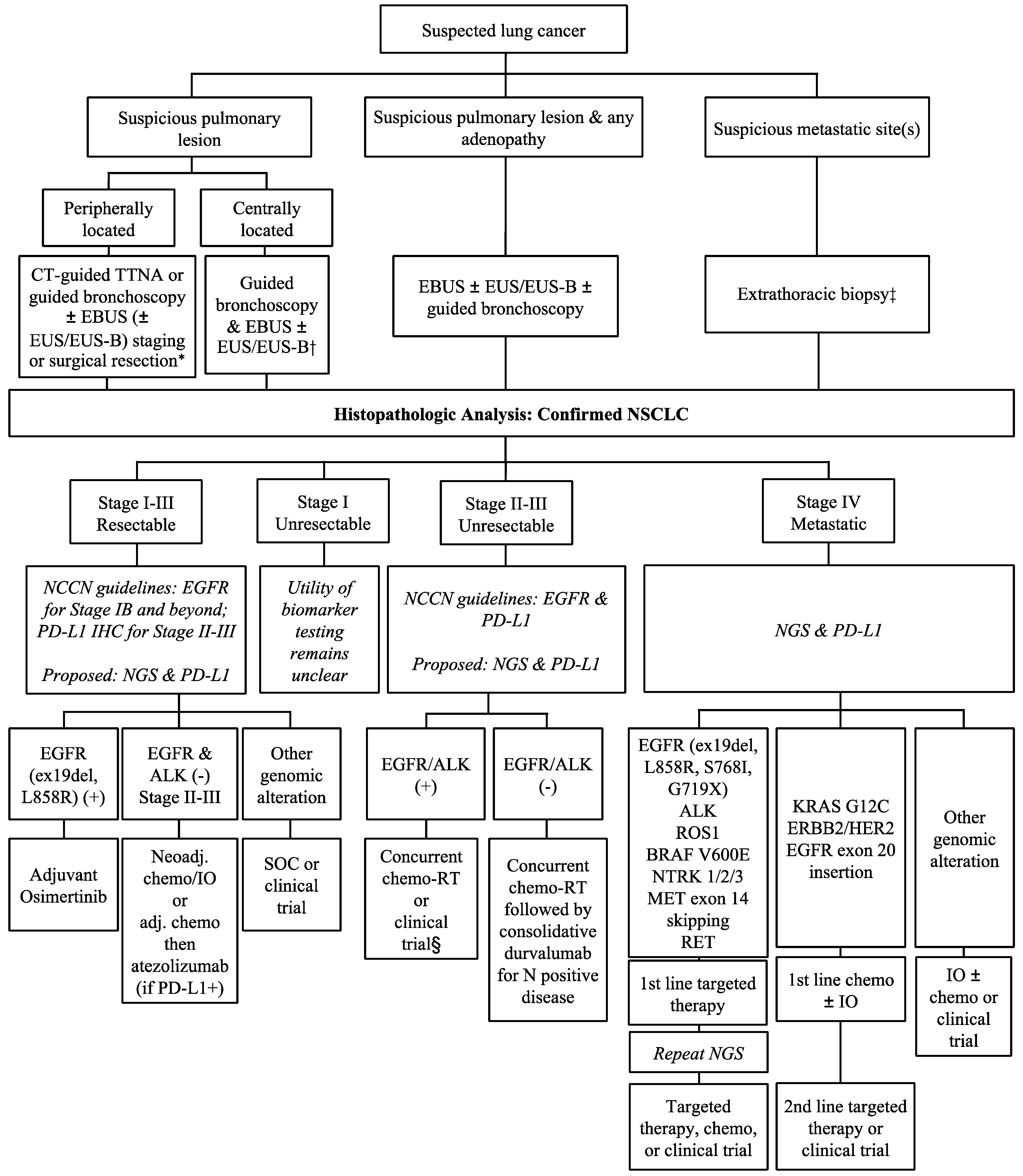
Optimal treatment of lung cancer is determined by biopsy results and staging. If there is clinical evidence of metastasis, sampling from distant sites should be prioritized to confirm stage IV disease. Staging scans can help identify clinical nodal disease, however, it is important to obtain pathologic confirmation, ensuring accurate staging. For example, a retrospective study found a stage shift in nearly 20% of patients who underwent endobronchial ultrasound (EBUS) compared to PET-CT alone [33]. Furthermore, accurate mediastinal staging affects treatment planning for both surgical and nonsurgical patients. It is important to differentiate mediastinal N0/N1 disease from N2/N3 disease, as this influences surgical candidacy. Similarly, nodal involvement may also impact radiation treatment planning. There are many diagnostic approaches available; however, only EBUS-transbronchial needle aspiration (TBNA) and guided bronchoscopies allow concurrent hilar and mediastinal node sampling, making them prime modalities for NSCLC diagnosis and staging. A comprehensive flow chart outlining the suggested tissue diagnosis modalities and subsequent biomarker testing is provided in Figure 2.
Figure 2.
Approach to tissue biopsy and biomarker testing and treatment in NSCLC by disease stage. IO = immunotherapy; SOC = standard of care. * The utility of routine mediastinal and hilar staging for lesions < 1–2 cm is not clear at present. † Many factors need to be considered such as lung function, local expertise, patient’s preference, and probability of disease. ‡ If obvious widely metastatic disease or certainty on single/minimal metastasis on imaging, the easiest/fastest/highest yield site should be biopsied. § The benefit of consolidative durvalumab has not been established in these patients.
6.1. Endobronchial Ultrasound
EBUS utilizes an ultrasound transducer located on the tip of a flexible bronchoscope allowing visualization of structures beyond the airway wall and real-time disease sampling. EBUS-TBNA advantageously provides access to a wide array of lymph node stations (2R, 2L, 3p, 4R, 4L, 7, 10R, 10L, 11s, 11i, 11L, 12R, 12L). A method for nodal identification using EBUS and proper biopsy order has previously been described [34,35]. In some cases, sampling of a centrally located primary parenchymal lesion is also possible [36]. The median diagnostic sensitivity of EBUS-TBNA is reportedly 81–89% [35], with low complication risks.
Several studies have demonstrated the adequacy of validated techniques for the use of smears in IHC, NGS, and liquid-based cytology preparations [37,38,39,40]. A meta-analysis of 33 studies reported a pooled probability of adequate material for molecular analysis from EBUS-TBNA sampling in almost 95% of cases [41]. Rapid on-site evaluation (ROSE) offers immediate feedback regarding diagnosis and quality of obtained specimens during EBUS-TBNA. The diagnostic yield with ROSE has an absolute percentage increase of 2.9–8% [37]. Studies also suggest that the use of ROSE can minimize molecular analysis failure [37]. In one study, successful molecular profiling was 10% higher in the cohort diagnosed with the addition of ROSE compared to its absence, although not statistically significant [42]. While the College of American Pathologists makes no recommendation for or against the use of one collection medium, fixative, or stain over another, it is worth noting that ethanol fixed samples with “negative” PD-L1 expression should be interpreted with caution due to a considerable rate of false negative results [37,43].
6.2. Endoscopic Ultrasound
Endoscopic ultrasound (EUS) fine-needle aspiration (FNA) employs the same concepts of EBUS-TBNA while using an EUS scope to obtain ultrasound-guided FNA samples via the esophagus, while EUS-B utilizes an EBUS scope. EUS-FNA/EUS-B allow access to mediastinal lymph nodes (4L, 7, 8, 9), celiac lymph nodes, the left adrenal gland, and portions of the liver, along with parenchymal lesions located close to the esophagus. The main advantages of this method, compared to EBUS-TBNA, include access to subdiaphragmatic sites. While EUS-FNA offers similar diagnostic sensitivity of 83–89%, routine use is limited only to augment EBUS-TBNA in select cases [35].
6.3. CT-Guided Lung Biopsy
CT-guided lung biopsy has been an important diagnostic mechanism for pulmonary nodules, most notably peripherally based lesions. Studies evaluating its diagnostic yield estimate an 82–95% accuracy [44]. Samples are obtained via FNA and/or core needle biopsy (CNB) [45,46]. CNB is preferred over FNA due to superior diagnostic and genomic analysis ability. While FNA comparatively underperforms, CNB has an impressive sensitivity and specificity for malignancy [44,45,46], with one study reporting 92% and 98.6%, respectively [47]. Compared to FNA, CNB specimens are more likely to have remaining unexhausted tissue available for genomic analysis [47,48]. While CT-guided biopsy often obtains larger samples compared to transbronchial approaches, a recently published study reveals similar overall success rates for NGS analysis between the two modalities, with CT-guided biopsy performing inferiorly to transbronchial biopsy for RNA-based NGS testing [49]. Similarly, success of PD-L1 TPS analysis was comparable between CT-guided CNB, EBUS-TBNA, and endobronchial biopsy [50].
Despite relatively high diagnostic and molecular-testing yields, CT-guided lung biopsy possesses greater complication risks compared to bronchoscopic approaches. Pneumothorax occurs in approximately 9–43% of patients; at onset, each case has a 0–15% chance of subsequent chest-tube insertion [44]. Though reportedly less common, intrapulmonary hemorrhage may occur in up to 26% of cases, with CNB representing an increased risk [44]. These tangible adverse events create motivation to develop safer diagnostic approaches with equivalent or greater yield.
6.4. Guided Bronchoscopy
Guided bronchoscopy allows pulmonologists access to pulmonary lesions unreachable via traditional bronchoscopy, offering an improved safety profile compared to the alternative CT-guided samplings. Brushes, forceps, and aspiration needles are all used for sampling under radial probe endobronchial ultrasound (rEBUS), electromagnetic navigational bronchoscopy (ENB), and robotic-assisted bronchoscopy (RAB) guidance. Many studies have examined the clinical efficacy of these approaches. A large meta-analysis reported a weighted diagnostic yield of 70.6% for rEBUS [51]. NAVIGATE, a large multi-institutional prospective cohort study evaluated ENB finding a 72.9% diagnostic yield for malignancy [52]. Pooled meta-analyses corroborate these results with a suggested diagnostic yield of 65–70% [53]. However, these studies did not include digital tomosynthesis-corrected (DT)-ENB. The combination of ENB and rEBUS has revealed varied outcomes for enhancing diagnostic success [52,54,55]. RAB currently operates under two platforms in the US, the Monarch system or Ion Endoluminal system. The Monarch platform employs ENB technology and was evaluated via the BENEFIT trial [56]. Here, rEBUS was used to confirm lesion localization with a 96.2% accuracy and a subsequent diagnostic yield of 74.1%; lesions with concentric view per rEBUS were associated with improved diagnostic accuracy [56]. The Ion Endoluminal system incorporates shape sensing (ss) technology, and a recent study found a 98.7% target localization rate and an overall diagnostic yield of 81.7% [57]. A retrospective investigation comparing ss-RAB and DT-ENB demonstrated comparable diagnostic yields at 77% and 80%, respectively [58]. Finally, a retrospective study comparing the diagnostic yields of RAB versus CT-guided transthoracic biopsy were 87.6% and 88.4%, respectively [59]. Respective sensitivities and specificities for malignancy were 82.1% and 100% for RAB and 88.5% and 100% for CT-guided transthoracic biopsy [59]. Advantages of guided bronchoscopy approaches include minimal complication rates, between 2–4%, with a smaller risk of serious events requiring invasive intervention or hospitalization [51,52,56,60,61]. Additionally, concurrent mediastinal staging is commonplace, along with placement of fiducial markers or pleural dye to assist in surgical and/or radiation therapy [52]. Combined, these results reveal a promising new era for pulmonary biopsy.
Equally important to diagnostic efficacy is the ability to obtain adequate tissue for comprehensive biomarker and IHC testing. An early retrospective study evaluating ENB found that 94.1% (n = 17) of specimens were viable for EGFR and ALK alteration analyses and 100% (n = 22) were acceptable for IHC analysis [62]. Most cases utilized transbronchial forceps biopsy samples for biomarker testing [62]. A more recent study reported similar results in the setting of ENB, revealing 91.7% (n = 13) of NSCLC samples were adequate for EGFR, ALK, and PD-L1 testing [63]. Transbronchial forceps instrument was also the most common sampling device used [63]. Comparing rEBUS and transbronchial biopsy to subsequent surgical specimens revealed a 3% (n = 56) false negative rate among transbronchial biopsies for EGFR mutational analysis, a direct result of low tumor cell quantity in the associated specimens [64]. Another recent study demonstrated tremendous success rates on genomic alteration testing with specimens obtained with transbronchial brushing under rEBUS guidance [65]. Samples were adequate in 99.1% and 85.1% with DNA and RNA sequencing, respectively [65]. While these previous studies produced promising results for limited biomarker analysis, comprehensive genomic testing has escalated along with the rapid rise in available targeted agents. One report evaluated feasibility of NGS and PD-L1 testing from samples obtained via rEBUS and ENB procedures. PD-L1 testing was successfully performed on 94% (n = 232) of cases [66]. A smaller cohort underwent subsequent surgical resection with perfect concordance among the 50% threshold (n = 15), whereas the >1% threshold identified three false negative cases (n = 8) from bronchoscopy specimens [66]. Unfortunately, exhausted tissue, leading to unacceptable NGS analysis, affected 30.9% (n = 188) of cases, disproportionately impacting early-stage disease [66]. These results suggest the importance of procuring larger tissue samples while maintaining a minimally invasive approach. A recent analysis of RAB with different sampling methods including needle aspiration, transbronchial forceps, and cryobiopsy were evaluated. Cryobiopsy produced less crush artifact and obtained a median amount of diagnostic tissue, approximately 11-fold higher, than needle aspiration and 2-fold higher than transbronchial forceps [67]. Forty-nine cases of NSCLC were analyzed via IHC, fluoresence in situ hybridization (FISH), and NGS. One hundred percent (n = 29) of cryobiopsy, 83% (n = 18) of forceps biopsy, and 50% (n = 2) of needle aspiration specimens were acceptable for such extensive analysis [67]. This study provides important insight into promising new biopsy approaches to improve concurrent diagnosis and molecular analysis.
6.5. Surgical Approaches
Mediastinoscopy is performed via mediastinoscope insertion through a base of neck incision. This method provides access to ipsilateral and contralateral pretracheal, paratracheal, and anterior subcarinal lymph nodes. Independently, it is generally reserved for circumstances when EBUS-TBNA/EUS-FNA fail to confirm disease in highly suspected cases [35]. A meta-analysis found the addition of mediastinoscopy following EBUS/EUS resulted in improved diagnostic sensitivity for N2/N3 disease with increased likelihood of upstaging [68]. As such, thoracic surgeons may perform mediastinoscopy prior to surgical resection.
Video-assisted thorascopic surgery (VATS) is the most common operative method used for lung cancer resection, providing access to the full tumor specimen along with a wide range of ipsilateral nodes; however, contralateral nodes are generally inaccessible [35]. Given ample attainable tissue, VATS has a 99% diagnostic sensitivity with improved ability for subsequent molecular analysis [35,69]. It can also provide information regarding pleural tumor involvement. Despite superior diagnostic abilities, VATS, as an isolated diagnostic tool, is generally reserved for select cases.
6.6. Thoracentesis
Patients presenting with a pleural effusion and presumed, or previously diagnosed, lung cancer should undergo a thoracentesis for at least diagnostic purposes. Malignant pleural effusions may alter disease staging and treatment recommendations. Pleural fluid has a reported 72% diagnostic yield for malignancy with 49–91% sensitivity following submission of two specimens [70]. Factors impacting diagnostic yield include sample preparation and tumor type, highly favoring adenocarcinoma histology [70,71]. Like standard tissue, biomarker testing can be performed on pleural fluid samples. High tumor cellularity, as opposed to sample amount, improves success of molecular analysis; a goal tumor cellularity of >10% is often sought [72]. Comparisons of NGS and PD-L1 testing performed on standard tissue biopsy and pleural fluid samples reveal highly congruent results of greater than 80% in multiple analyses [72]. Thoracentesis provides a minimally invasive diagnostic approach with easily attainable specimen.
6.7. Extra-Thoracic Disease Sampling
Lung cancer may also be diagnosed from biopsies or surgical specimens obtained from metastatic sites. Additionally, confirmatory biopsies of extrathoracic areas may be warranted to solidify metastatic disease. A 2014 study evaluated NSCLC biopsy specimens from various sites and their respective success rates for EGFR, ALK, and KRAS molecular/FISH analyses. While intrathoracic disease specimens comprised the majority, overall success rates reached 90–94% with small biopsies/cytologic specimens reaching 85–88% [73]. Extrathoracic site-based failure rates for EGFR, ALK, and KRAS were 17.4% (n = 23), 22.2% (n = 18), and 14.3% (n = 14) for bone; 0% (n = 23), 0% (n = 21), and 0% (n = 17) for brain; and 14.3% (n = 14), 12.5% (n = 8), and 50% (n = 4) for liver, respectively [73]. Increased failure rates were seen from nonsurgical specimens and cytologic cell block specimens from bone. Surgical specimens revealed a 0% failure rate for all mutational analyses representing the presence of ample tumor cells to undergo diagnostic and molecular testing [73]. Osseous failure relates to tissue processing and acid decalcification, which damages nucleic acids interfering with molecular analysis [73]. A more recent study assessing the role of CT-guided percutaneous osteolytic biopsy found a 100% diagnostic rate with a subsequent molecular analysis yield of 94.6% (n = 37) in the absence of tissue decalcification [74]. This underscores the importance of expert tissue handling among pathologists to maximize molecular testing.
Additionally, the adrenal glands are frequently subject to CT-guided percutaneous biopsy for diagnostic means. A large retrospective review identified the diagnostic sensitivity and specificity for lung cancer to be 97% and 100%, respectively [75]. Additionally, the procedure was remarkably safe, with only a 1.1% rate of minor, and no major, complications reported [75].
6.8. Liquid Biopsy
Liquid biopsy is an emerging diagnostic tool in the field of NSCLC. This noninvasive test is typically performed on plasma to identify circulating tumor cells, cell-free DNA (cfDNA), and exosomes. While tissue biopsy remains the gold standard, liquid biopsy can provide information reflecting tumor heterogeneity or metastatic disease. A major limitation of liquid biopsy is its variable sensitivity, depending on the testing platform and extent of tumor burden. Patients with extrathoracic disease have a higher likelihood of successfully detecting EGFR mutations on liquid biopsy compared to patients with intrathoracic metastasis [76]. Real-world studies have shown sensitivity of NGS-based cfDNA assays ranging from 75–90% [77].
As a tool for monitoring treatment response, cfDNA is emerging as a marker of minimal residual disease and prognostic information. The presence of cfDNA after curative treatment can predict disease recurrence [78,79] and may also provide valuable information to guide treatment. In one study, patients with the presence of cfDNA showed benefit from consolidation immunotherapy while patients without presence of cfDNA showed no benefit [77]. While such tests are not yet endorsed by the NCCN, it is possible that they will eventually be incorporated into SOC management of such patients.
7. Conclusions
Timely and accurate biomarker testing is crucial to determine optimal treatment for all stages of NSCLC. This review provides evidence regarding the utility and clinical impact of common targeted therapies and ICIs currently in use. Identification of targetable mutations and PD-L1 status not only carries direct implications for SOC treatments but can also provide important opportunities for clinical trial participation. Reflex testing to obtain all biomarker data at the time of initial diagnosis can expedite patient care, especially given high recurrence rates seen among NSCLC. At the core, pulmonologists play a central role in the diagnosis of NSCLC and ensuring all appropriate data is obtained prior to treatment planning. EBUS-TBNA and guided bronchoscopy methods are safe, effective, and minimally invasive modalities to obtain adequate specimens for diagnosis, staging, and biomarker analysis in one comprehensive procedure. As precision medicine continues to advance, it is crucial that clinicians prioritize a multidisciplinary approach in the diagnosis and treatment of NSCLC.
Author Contributions
Conceptualization, D.S.B. and F.A.A.; investigation, C.L.M., A.L.Z., D.S.B. and F.A.A.; resources, C.L.M., A.L.Z., D.S.B. and F.A.A.; writing—original draft preparation, C.L.M. and A.L.Z.; writing—review and editing, C.L.M., A.L.Z., D.S.B. and F.A.A.; supervision, D.S.B. and F.A.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- National Cancer Institute. SEER Cancer Stat Facts: Lung and Bronchus Cancer Bethesda, MD. 2022. Available online: https://seer.cancer.gov/statfacts/html/lungb.html (accessed on 27 December 2022).
- Lung Cancer Research Foundation. Lung Cancer Facts 2022. 2022. Available online: https://www.lungcancerresearchfoundation.org/lung-cancer-facts/#:~:text=LUNG%20CANCER%20is%20the%20leading%20cause%20of%20cancer%20death%20worldwide.&text=AN%20ESTIMATED%20236%2C740%20PEOPLE%20will,in%202022%20in%20the%20U.S.&text=1%20IN%2016%20PEOPLE%20will,and%201%20in%2017%20women.&text=Approximately%20130%2C180%20AMERICAN%20LIVES%20are%20lost%20annually (accessed on 28 December 2022).
- American Cancer Society. Cancer Facts & Figures 2022; American Cancer Society: Atlanta, GA, USA, 2022. [Google Scholar]
- Ganti, A.K.; Klein, A.B.; Cotarla, I.; Seal, B.; Chou, E. Update of Incidence, Prevalence, Survival, and Initial Treatment in Patients with Non–Small Cell Lung Cancer in the US. JAMA Oncol. 2021, 7, 1824. [Google Scholar] [CrossRef] [PubMed]
- Ettinger, D.S.; Wood, D.E.; Aisner, D.L.; Akerley, W.; Bauman, J.R.; Bharat, A.; Bruno, D.S.; Chang, J.Y.; Chirieac, L.R.; D’Amico, T.A.; et al. Non–Small Cell Lung Cancer, Version 3.2022, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. 2022, 20, 497–530. [Google Scholar] [CrossRef]
- Aggarwal, C.; Bubendorf, L.; Cooper, W.A.; Illei, P.; Nunes, P.B.; Ong, B.-H.; Tsao, M.-S.; Yatabe, Y.; Kerr, K.M. Molecular testing in stage I–III non-small cell lung cancer: Approaches and challenges. Lung Cancer 2021, 162, 42–53. [Google Scholar] [CrossRef]
- National Comprehensive Cancer Network. Non-Small Cell Lung Cancer (Version 6. 2022). 2022. Available online: https://www.nccn.org/professionals/physician_gls/pdf/nscl.pdf (accessed on 30 December 2022).
- Majeed, U.; Manochakian, R.; Zhao, Y.; Lou, Y. Targeted therapy in advanced non-small cell lung cancer: Current advances and future trends. J. Hematol. Oncol. 2021, 14, 108. [Google Scholar] [CrossRef]
- Harrison, P.T.; Vyse, S.; Huang, P.H. Rare epidermal growth factor receptor (EGFR) mutations in non-small cell lung cancer. Semin. Cancer Biol. 2020, 61, 167–179. [Google Scholar] [CrossRef]
- Karachaliou, N.; Fernandez-Bruno, M.; Bracht, J.W.P.; Rosell, R. EGFR first- and second-generation TKIs—There is still place for them in EGFR-mutant NSCLC patients. Transl. Cancer Res. 2018, 8, S23–S47. [Google Scholar] [CrossRef] [PubMed]
- Rosell, R.; Carcereny, E.; Gervais, R.; Vergnenegre, A.; Massuti, B.; Felip, E.; Palmero, R.; Garcia-Gomez, R.; Pallares, C.; Sanchez, J.M.; et al. Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): A multicentre, open-label, randomised phase 3 trial. Lancet Oncol. 2012, 13, 239–246. [Google Scholar] [CrossRef]
- Tan, A.C.; Tan, D.S.W. Targeted Therapies for Lung Cancer Patients with Oncogenic Driver Molecular Alterations. J. Clin. Oncol. 2022, 40, 611–625. [Google Scholar] [CrossRef] [PubMed]
- Soria, J.-C.; Ohe, Y.; Vansteenkiste, J.; Reungwetwattana, T.; Chewaskulyong, B.; Lee, K.H.; Dechaphunkul, A.; Imamura, F.; Nogami, N.; Kurata, T.; et al. Osimertinib in Untreated EGFR-Mutated Advanced Non–Small-Cell Lung Cancer. N. Engl. J. Med. 2018, 378, 113–125. [Google Scholar] [CrossRef]
- Ramalingam, S.S.; Vansteenkiste, J.; Planchard, D.; Cho, B.C.; Gray, J.E.; Ohe, Y.; Zhou, C.; Reungwetwattana, T.; Cheng, Y.; Chewaskulyong, B.; et al. Overall Survival with Osimertinib in Untreated, EGFR-Mutated Advanced NSCLC. N. Engl. J. Med. 2020, 382, 41–50. [Google Scholar] [CrossRef]
- Wu, Y.-L.; Tsuboi, M.; He, J.; John, T.; Grohe, C.; Majem, M.; Goldman, J.W.; Laktionov, K.; Kim, S.-W.; Kato, T.; et al. Osimertinib in Resected EGFR-Mutated Non–Small-Cell Lung Cancer. N. Engl. J. Med. 2020, 383, 1711–1723. [Google Scholar] [CrossRef]
- Aisner, D.L.; Riely, G.J. Non–Small Cell Lung Cancer: Recommendations for Biomarker Testing and Treatment. J. Natl. Compr. Cancer Netw. 2021, 19, 610–613. [Google Scholar] [CrossRef]
- Blackhall, F.; Cappuzzo, F. Crizotinib: From discovery to accelerated development to front-line treatment. Ann. Oncol. 2016, 27, iii35–iii41. [Google Scholar] [CrossRef]
- Solomon, B.J.; Mok, T.; Kim, D.-W.; Wu, Y.-L.; Nakagawa, K.; Mekhail, T.; Felip, E.; Cappuzzo, F.; Paolini, J.; Usari, T.; et al. First-Line Crizotinib versus Chemotherapy in ALK-Positive Lung Cancer. N. Engl. J. Med. 2014, 371, 2167–2177. [Google Scholar] [CrossRef]
- Mok, T.; Camidge, D.R.; Gadgeel, S.M.; Rosell, R.; Dziadziuszko, R.; Kim, D.W.; Pérol, M.; Ou, S.-H.; Ahn, J.; Shaw, A.; et al. Updated overall survival and final progression-free survival data for patients with treatment-naive advanced ALK-positive non-small-cell lung cancer in the ALEX study. Ann. Oncol. 2020, 31, 1056–1064. [Google Scholar] [CrossRef]
- Peters, S.; Camidge, D.R.; Shaw, A.T.; Gadgeel, S.; Ahn, J.S.; Kim, D.W.; Ou, S.H.I.; Pérol, M.; Dziadziuszko, R.; Rosell, R.; et al. Alectinib versus Crizotinib in Untreated ALK-Positive Non–Small-Cell Lung Cancer. N. Engl. J. Med. 2017, 377, 829–838. [Google Scholar] [CrossRef] [PubMed]
- Garon, E.B.; Rizvi, N.A.; Hui, R.; Leighl, N.; Balmanoukian, A.S.; Eder, J.P.; Patnaik, A.; Aggarwal, C.; Gubens, M.; Horn, L.; et al. Pembrolizumab for the Treatment of Non–Small-Cell Lung Cancer. N. Engl. J. Med. 2015, 372, 2018–2028. [Google Scholar] [CrossRef]
- Herbst, R.S.; Baas, P.; Kim, D.-W.; Felip, E.; Pérez-Gracia, J.L.; Han, J.-Y.; Molina, J.; Kim, J.-H.; Arvis, C.D.; Ahn, M.-J.; et al. Pembrolizumab versus docetaxel for previously treated, PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010): A randomised controlled trial. Lancet 2015, 387, 1540–1550. [Google Scholar] [CrossRef]
- Reck, M.; Rodríguez-Abreu, D.; Robinson, A.G.; Hui, R.; Csőszi, T.; Fülöp, A.; Gottfried, M.; Peled, N.; Tafreshi, A.; Cuffe, S.; et al. Pembrolizumab versus Chemotherapy for PD-L1–Positive Non–Small-Cell Lung Cancer. N. Engl. J. Med. 2016, 375, 1823–1833. [Google Scholar] [CrossRef] [PubMed]
- Reck, M.; Rodríguez–Abreu, D.; Robinson, A.G.; Hui, R.; Csőszi, T.; Fülöp, A.; Gottfried, M.; Peled, N.; Tafreshi, A.; Cuffe, S.; et al. Updated Analysis of KEYNOTE-024: Pembrolizumab Versus Platinum-Based Chemotherapy for Advanced Non–Small-Cell Lung Cancer With PD-L1 Tumor Proportion Score of 50% or Greater. J. Clin. Oncol. 2019, 37, 537–546. [Google Scholar] [CrossRef]
- Antonia, S.J.; Villegas, A.; Daniel, D.; Vicente, D.; Murakami, S.; Hui, R.; Yokoi, T.; Chiappori, A.; Lee, K.H.; De Wit, M.; et al. Durvalumab after Chemoradiotherapy in Stage III Non-Small-Cell Lung Cancer. N. Engl. J. Med. 2017, 377, 1919–1929. [Google Scholar] [CrossRef] [PubMed]
- Spigel, D.R.; Faivre-Finn, C.; Gray, J.E.; Vicente, D.; Planchard, D.; Paz-Ares, L.; Vansteenkiste, J.F.; Garassino, M.C.; Hui, R.; Quantin, X.; et al. Five-Year Survival Outcomes from the PACIFIC Trial: Durvalumab After Chemoradiotherapy in Stage III Non–Small-Cell Lung Cancer. J. Clin. Oncol. 2022, 40, 1301–1311. [Google Scholar] [CrossRef] [PubMed]
- Forde, P.M.; Spicer, J.; Lu, S.; Provencio, M.; Mitsudomi, T.; Awad, M.M.; Felip, E.; Broderick, S.R.; Brahmer, J.R.; Swanson, S.J.; et al. Neoadjuvant Nivolumab plus Chemotherapy in Resectable Lung Cancer. N. Engl. J. Med. 2022, 386, 1973–1985. [Google Scholar] [CrossRef] [PubMed]
- Felip, E.; Altorki, N.; Zhou, C.; Csőszi, T.; Vynnychenko, I.; Goloborodko, O.; Luft, A.; Akopov, A.; Martinez-Marti, A.; Kenmotsu, H.; et al. Adjuvant atezolizumab after adjuvant chemotherapy in resected stage IB–IIIA non-small-cell lung cancer (IMpower010): A randomised, multicentre, open-label, phase 3 trial. Lancet 2021, 398, 1344–1357. [Google Scholar] [CrossRef]
- Chaft, J.E.; Shyr, Y.; Sepesi, B.; Forde, P.M. Preoperative and Postoperative Systemic Therapy for Operable Non–Small-Cell Lung Cancer. J. Clin. Oncol. 2022, 40, 546–555. [Google Scholar] [CrossRef]
- Scagliotti, G.V.; Parikh, P.; Von Pawel, J.; Biesma, B.; Vansteenkiste, J.; Serwatowski, C.M.; Serwatowski, P.; Gatzemeier, U.; Digumarti, R.; Zukin, M.; et al. Phase III Study Comparing Cisplatin Plus Gemcitabine with Cisplatin Plus Pemetrexed in Chemotherapy-Naive Patients With Advanced-Stage Non–Small-Cell Lung Cancer. J. Clin. Oncol. 2008, 26, 3543–3551. [Google Scholar] [CrossRef]
- Sandler, A.; Gray, R.; Perry, M.C.; Brahmer, J.; Schiller, J.H.; Dowlati, A.; Lilenbaum, R.; Johnson, D.H. Paclitaxel–Carboplatin Alone or with Bevacizumab for Non–Small-Cell Lung Cancer. N. Engl. J. Med. 2006, 355, 2542–2550. [Google Scholar] [CrossRef]
- Bruno, D.S.; Hess, L.M.; Li, X.; Su, E.W.; Patel, M. Disparities in Biomarker Testing and Clinical Trial Enrollment Among Patients with Lung, Breast, or Colorectal Cancers in the United States. JCO Precis. Oncol. 2022, 6, e2100427. [Google Scholar] [CrossRef]
- Vial, M.R.; Khan, K.A.; O’Connell, O.; Peng, S.A.; Gomez, D.R.; Chang, J.Y.; Rice, D.C.; Mehran, R.; Jimenez, C.J.; Grosu, H.B.; et al. Endobronchial Ultrasound-Guided Transbronchial Needle Aspiration in the Nodal Staging of Stereotactic Ablative Body Radiotherapy Patients. Ann. Thorac. Surg. 2016, 103, 1600–1605. [Google Scholar] [CrossRef]
- Avasarala, S.K.; Aravena, C.; Almeida, F.A. Convex probe endobronchial ultrasound: Historical, contemporary, and cutting-edge applications. J. Thorac. Dis. 2020, 12, 1085–1099. [Google Scholar] [CrossRef]
- Marshall, T.; Kalanjeri, S.; Almeida, F.A. Lung cancer staging, the established role of bronchoscopy. Curr. Opin. Pulm. Med. 2021, 28, 17–30. [Google Scholar] [CrossRef] [PubMed]
- Almeida, F.A.; Salam, S.; Mehta, A.C.; Yuhico, L.; Sarda, Y.; Choi, H.; Cicenia, J.C.; Gildea, T.; Machuzak, M.; Mazzone, P.; et al. Sampling Utility of the Convex Probe Endobronchial Ultrasound Visible Intrapulmonary Lesion. J. Bronchol. Interv. Pulmonol. 2018, 25, 290–299. [Google Scholar] [CrossRef] [PubMed]
- Roy-Chowdhuri, S.; Dacic, S.; Ghofrani, M.; Illei, P.B.; Layfield, L.J.; Lee, C.; Michael, C.W.; Miller, R.A.; Mitchell, J.W.; Nikolic, B.; et al. Collection and Handling of Thoracic Small Biopsy and Cytology Specimens for Ancillary Studies: Guideline From the College of American Pathologists in Collaboration With the American College of Chest Physicians, Association for Molecular Pathology, American Society of Cytopathology, American Thoracic Society, Pulmonary Pathology Society, Papanicolaou Society of Cytopathology, Society of Interventional Radiology, and Society of Thoracic Radiology. Arch. Pathol. Lab. Med. 2020, 144, 933–958. [Google Scholar] [CrossRef]
- Stoy, S.P.; Segal, J.P.; Mueller, J.; Furtado, L.V.; Vokes, E.E.; Patel, J.D.; Murgu, S. Feasibility of Endobronchial Ultrasound-guided Transbronchial Needle Aspiration Cytology Specimens for Next Generation Sequencing in Non–small-cell Lung Cancer. Clin. Lung Cancer 2018, 19, 230–238.e2. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, J.P.; Zhou, Y.; Jakubowski, M.A.; Wang, Z.; Brainard, J.A.; Klein, R.D.; Farver, C.F.; Almeida, F.A.; Cheng, Y.-W. Next-generation sequencing of liquid-based cytology non-small cell lung cancer samples. Cancer Cytopathol. 2017, 125, 178–187. [Google Scholar] [CrossRef]
- Rooper, L.M.; Nikolskaia, O.; Carter, J.; Ning, Y.; Lin, M.-T.; Maleki, Z. A single EBUS-TBNA procedure can support a large panel of immunohistochemical stains, specific diagnostic subtyping, and multiple gene analyses in the majority of non–small cell lung cancer cases. Hum. Pathol. 2016, 51, 139–145. [Google Scholar] [CrossRef]
- Labarca, G.; Folch, E.; Jantz, M.; Mehta, H.J.; Majid, A.; Fernandez-Bussy, S. Adequacy of Samples Obtained by Endobronchial Ultrasound with Transbronchial Needle Aspiration for Molecular Analysis in Patients with Non–Small Cell Lung Cancer. Systematic Review and Meta-Analysis. Ann. Am. Thorac. Soc. 2018, 15, 1205–1216. [Google Scholar] [CrossRef]
- Trisolini, R.; Cancellieri, A.; Tinelli, C.; de Biase, D.; Valentini, I.; Casadei, G.; Paioli, D.; Ferrari, F.; Gordini, G.; Patelli, M.; et al. Randomized Trial of Endobronchial Ultrasound-Guided Transbronchial Needle Aspiration with and Without Rapid On-site Evaluation for Lung Cancer Genotyping. Chest 2015, 148, 1430–1437. [Google Scholar] [CrossRef]
- Koomen, B.M.; Vreuls, W.; de Boer, M.; de Ruiter, E.J.; Hoelters, J.; Vink, A.; Willems, S.M. False-negative programmed death-ligand 1 immunostaining in ethanol-fixed endobronchial ultrasound-guided transbronchial needle aspiration specimens of non-small-cell lung cancer patients. Histopathology 2021, 79, 480–490. [Google Scholar] [CrossRef]
- Nakamura, K.; Matsumoto, K.; Inoue, C.; Matsusue, E.; Fujii, S. Computed Tomography-guided Lung Biopsy: A Review of Techniques for Reducing the Incidence of Complications. Interv. Radiol. 2021, 6, 83–92. [Google Scholar] [CrossRef]
- Anzidei, M.; Porfiri, A.; Andrani, F.; Di Martino, M.; Saba, L.; Catalano, C.; Bezzi, M. Imaging-guided chest biopsies: Techniques and clinical results. Insights into Imaging 2017, 8, 419–428. [Google Scholar] [CrossRef] [PubMed]
- Sangha, B.S.; Hague, C.J.; Jessup, J.; O’Connor, R.; Mayo, J.R. Transthoracic Computed Tomography–Guided Lung Nodule Biopsy: Comparison of Core Needle and Fine Needle Aspiration Techniques. Can. Assoc. Radiol. J. 2016, 67, 284–289. [Google Scholar] [CrossRef] [PubMed]
- Tian, P.; Wang, Y.; Li, L.; Zhou, Y.; Luo, W.; Li, W. CT-guided transthoracic core needle biopsy for small pulmonary lesions: Diagnostic performance and adequacy for molecular testing. J. Thorac. Dis. 2017, 9, 333–343. [Google Scholar] [CrossRef] [PubMed]
- Schneider, F.; Smith, M.A.; Lane, M.C.; Pantanowitz, L.; Dacic, S.; Ohori, N.P. Adequacy of Core Needle Biopsy Specimens and Fine-Needle Aspirates for Molecular Testing of Lung Adenocarcinomas. Am. J. Clin. Pathol. 2015, 143, 193–200. [Google Scholar] [CrossRef]
- Kunimasa, K.; Matsumoto, S.; Nishino, K.; Honma, K.; Maeda, N.; Kuhara, H.; Tamiya, M.; Inoue, T.; Kawamura, T.; Kimura, T.; et al. Comparison of sampling methods for next generation sequencing for patients with lung cancer. Cancer Med. 2022, 11, 2744–2754. [Google Scholar] [CrossRef]
- Chen, M.; Xu, Y.; Zhao, J.; Li, J.; Liu, X.; Zhong, W.; Wang, M. Feasibility and reliability of evaluate PD-L1 expression determination using small biopsy specimens in non-small cell lung cancer. Thorac. Cancer 2021, 12, 2339–2344. [Google Scholar] [CrossRef] [PubMed]
- Ali, M.S.; Trick, W.; Mba, B.I.; Mohananey, D.; Sethi, J.; Musani, A.I. Radial endobronchial ultrasound for the diagnosis of peripheral pulmonary lesions: A systematic review and meta-analysis. Respirology 2017, 22, 443–453. [Google Scholar] [CrossRef] [PubMed]
- Folch, E.E.; Pritchett, M.A.; Nead, M.A.; Bowling, M.R.; Murgu, S.D.; Krimsky, W.S.; Murillo, B.A.; LeMense, G.P.; Minnich, D.J.; Bansal, S.; et al. Electromagnetic Navigation Bronchoscopy for Peripheral Pulmonary Lesions: One-Year Results of the Prospective, Multicenter NAVIGATE Study. J. Thorac. Oncol. 2018, 14, 445–458. [Google Scholar] [CrossRef]
- Wagh, A.; Ho, E.; Murgu, S.; Hogarth, D.K. Improving diagnostic yield of navigational bronchoscopy for peripheral pulmonary lesions: A review of advancing technology. J. Thorac. Dis. 2020, 12, 7683–7690. [Google Scholar] [CrossRef]
- Eberhardt, R.; Anantham, D.; Ernst, A.; Feller-Kopman, D.; Herth, F. Multimodality Bronchoscopic Diagnosis of Peripheral Lung Lesions. Am. J. Respir. Crit. Care Med. 2007, 176, 36–41. [Google Scholar] [CrossRef]
- Ozgul, G.; Cetinkaya, E.; Ozgul, M.A.; Abul, Y.; Gencoglu, A.; Kamiloglu, E.; Gul, S. Efficacy and safety of electromagnetic navigation bronchoscopy with or without radial endobronchial ultrasound for peripheral lung lesions. Endosc. Ultrasound 2016, 5, 189–195. [Google Scholar] [CrossRef] [PubMed]
- Chen, A.C.; Pastis, N.J.; Mahajan, A.K.; Khandhar, S.J.; Simoff, M.J.; Machuzak, M.S.; Cicenia, J.; Gildea, T.R.; Silvestri, G.A. Robotic Bronchoscopy for Peripheral Pulmonary Lesions: A Multicenter Pilot and Feasibility Study (BENEFIT). Chest 2020, 159, 845–852. [Google Scholar] [CrossRef] [PubMed]
- Kalchiem-Dekel, O.; Connolly, J.G.; Lin, I.-H.; Husta, B.C.; Adusumilli, P.S.; Beattie, J.A.; Buonocore, D.J.; Dycoco, J.; Fuentes, P.; Jones, D.R.; et al. Shape-Sensing Robotic-Assisted Bronchoscopy in the Diagnosis of Pulmonary Parenchymal Lesions. Chest 2022, 161, 572–582. [Google Scholar] [CrossRef] [PubMed]
- Low, S.-W.; Lentz, R.J.; Chen, H.; Katsis, J.; Aboudara, M.C.; Whatley, S.; Paez, R.; Rickman, O.B.; Maldonado, F. Shape-Sensing Robotic-Assisted Bronchoscopy vs Digital Tomosynthesis-Corrected Electromagnetic Navigation Bronchoscopy: A Comparative Cohort Study of Diagnostic Performance. Chest 2022. [Google Scholar] [CrossRef]
- Lee-Mateus, A.Y.; Reisenauer, J.; Garcia-Saucedo, J.C.; Abia-Trujillo, D.; Buckarma, E.H.; Edell, E.S.; Grage, R.A.; Bowman, A.W.; Labarca, G.; Johnson, M.M.; et al. Robotic-assisted bronchoscopy versus CT -guided transthoracic biopsy for diagnosis of pulmonary nodules. Respirology 2023, 28, 66–73. [Google Scholar] [CrossRef]
- Seijo, L.M. Electromagnetic navigation bronchoscopy: Clinical utility in the diagnosis of lung cancer. Lung Cancer Targets Ther. 2016, 7, 111–118. [Google Scholar] [CrossRef]
- Chaddha, U.; Kovacs, S.P.; Manley, C.; Hogarth, D.K.; Cumbo-Nacheli, G.; Bhavani, S.V.; Kumar, R.; Shende, M.; Egan, J.P.; Murgu, S. Robot-assisted bronchoscopy for pulmonary lesion diagnosis: Results from the initial multicenter experience. BMC Pulm. Med. 2019, 19, 243. [Google Scholar] [CrossRef]
- Ha, D.; Choi, H.; Almeida, F.A.; Arrossi, A.; Brainard, J.; Cicenia, J.; Farver, C.; Gildea, T.; Machuzak, M.S.; Mazzone, P. Histologic and Molecular Characterization of Lung Cancer with Tissue Obtained by Electromagnetic Navigation Bronchoscopy. J. Bronchol. Interv. Pulmonol. 2013, 20, 10–15. [Google Scholar] [CrossRef]
- Oh, J.H.; Choi, C.-M.; Kim, S.; Jang, S.J.; Oh, S.Y.; Kim, M.Y.; Hwang, H.; Ji, W. Diagnostic Performance of Electromagnetic Navigation Bronchoscopy-Guided Biopsy for Lung Nodules in the Era of Molecular Testing. Diagnostics 2021, 11, 1432. [Google Scholar] [CrossRef]
- Kim, I.; Eom, J.S.; Kim, A.R.; Lee, C.H.; Lee, G.; Jo, E.J.; Kim, M.-H.; Mok, J.H.; Lee, K.; Kim, K.U.; et al. Molecular analysis of small tissue samples obtained via transbronchial lung biopsy using radial probe endobronchial ultrasound. PLoS ONE 2019, 14, e0212672. [Google Scholar] [CrossRef]
- Furuya, N.; Matsumoto, S.; Kakinuma, K.; Morikawa, K.; Inoue, T.; Saji, H.; Goto, K.; Mineshita, M. Suitability of transbronchial brushing cytology specimens for next-generation sequencing in peripheral lung cancer. Cancer Sci. 2021, 112, 380–387. [Google Scholar] [CrossRef]
- Robin, M.; Mhanna, L.; Chaltiel, L.; Plat, G.; Héluain, V.; Basset, C.; Meilleroux, J.; Filleron, T.; Mazières, J.; Hermant, C.; et al. Feasibility of comprehensive genotyping specimens from radial endobronchial ultrasonography and electromagnetic navigation bronchoscopy. ERJ Open Res. 2021, 7, 00942–2020. [Google Scholar] [CrossRef] [PubMed]
- Oberg, C.L.; Lau, R.P.; Folch, E.E.; He, T.; Ronaghi, R.; Susanto, I.; Channick, C.; Tome, R.G.; Oh, S. Novel Robotic-Assisted Cryobiopsy for Peripheral Pulmonary Lesions. Lung 2022, 200, 737–745. [Google Scholar] [CrossRef] [PubMed]
- Gunawan, A.; Manuel, L.; Fong, L.S.; Bassin, L. In patients with lung cancer is combined endobronchial ultrasound and endoscopic ultrasound superior to conventional mediastinoscopy in staging the mediastinum? Ann. Med. Surg. 2021, 71, 102953. [Google Scholar] [CrossRef] [PubMed]
- Cooke, D.T.; Gandara, D.R.; Goodwin, N.C.; Calhoun, R.F.; Lara, P.N., Jr.; Mack, P.C.; David, E.A. Outcomes and efficacy of thoracic surgery biopsy for tumor molecular profiling in patients with advanced lung cancer. J. Thorac. Cardiovasc. Surg. 2014, 148, 36–40. [Google Scholar] [CrossRef]
- Rivera, M.P.; Mehta, A.C.; Wahidi, M.M. Establishing the Diagnosis of Lung Cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013, 143, e142S–e165S. [Google Scholar] [CrossRef] [PubMed]
- Dorry, M.; Davidson, K.; Dash, R.; Jug, R.; Clarke, J.M.; Nixon, A.B.; Mahmood, K. Pleural effusions associated with squamous cell lung carcinoma have a low diagnostic yield and a poor prognosis. Transl. Lung Cancer Res. 2021, 10, 2500–2508. [Google Scholar] [CrossRef]
- Grigoriadou, G.I.; Esagian, S.M.; Ryu, H.S.; Nikas, I.P. Molecular Profiling of Malignant Pleural Effusions with Next Generation Sequencing (NGS): Evidence that Supports Its Role in Cancer Management. J. Pers. Med. 2020, 10, 206. [Google Scholar] [CrossRef]
- VanderLaan, P.A.; Yamaguchi, N.; Folch, E.; Boucher, D.H.; Kent, M.S.; Gangadharan, S.P.; Majid, A.; Goldstein, M.A.; Huberman, M.S.; Kocher, O.N.; et al. Success and failure rates of tumor genotyping techniques in routine pathological samples with non-small-cell lung cancer. Lung Cancer 2014, 84, 39–44. [Google Scholar] [CrossRef]
- Toffart, A.-C.; Asfari, S.; Mc Leer, A.; Reymond, E.; Jankowski, A.; Moro-Sibilot, D.; Stephanov, O.; Ghelfi, J.; Lantuejoul, S.; Ferretti, G.R. Percutaneous CT-guided biopsy of lytic bone lesions in patients clinically suspected of lung cancer: Diagnostic performances for pathological diagnosis and molecular testing. Lung Cancer 2020, 140, 93–98. [Google Scholar] [CrossRef]
- McDermott, E.; Kilcoyne, A.; O’Shea, A.; Cahalane, A.M.; McDermott, S. The role of percutaneous CT-guided biopsy of an adrenal lesion in patients with known or suspected lung cancer. Abdom. Imaging 2021, 46, 1171–1178. [Google Scholar] [CrossRef] [PubMed]
- Smolle, E.; Taucher, V.; Lindenmann, J.; Pichler, M.; Smolle-Juettner, F.-M. Liquid biopsy in non-small cell lung cancer—Current status and future outlook—A narrative review. Transl. Lung Cancer Res. 2021, 10, 2237–2251. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.-R.; Schultheis, A.M.; Yu, H.; Mandelker, D.; Ladanyi, M.; Büttner, R. Precision medicine in non-small cell lung cancer: Current applications and future directions. Semin. Cancer Biol. 2022, 84, 184–198. [Google Scholar] [CrossRef]
- Newman, A.M.; Bratman, S.V.; To, J.; Wynne, J.F.; Eclov, N.C.W.; Modlin, L.A.; Liu, C.L.; Neal, J.W.; Wakelee, H.A.; Merritt, R.E.; et al. An ultrasensitive method for quantitating circulating tumor DNA with broad patient coverage. Nat. Med. 2014, 20, 548–554. [Google Scholar] [CrossRef] [PubMed]
- Chae, Y.K.; Oh, M.S. Detection of Minimal Residual Disease Using ctDNA in Lung Cancer: Current Evidence and Future Directions. J. Thorac. Oncol. 2019, 14, 16–24. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).