Abstract
Objective: The aim of this study was to describe the prevalence of anatomical variants in the bifid mandibular condyle (BMC) and report its association with temporomandibular joint (TMJ) pathology. Methods: We searched the Medline, Scopus, Web of Science, Google Scholar, CINAHL, and LILACS databases from their inception up to September 2023. Two authors independently performed the search, study selection, and data extraction, and they also assessed the methodological quality with an assurance tool for anatomical studies (AQUA). Finally, the pooled prevalence was estimated using a random effects model. Results: A total of 50 studies met the eligibility criteria. Twenty studies, with a total of 88,625 subjects, were included in the meta-analysis. The overall prevalence of the bifid mandibular condyle (BMC) variant was 1% (95% CI = 1% to 2%). Conclusions: The correlation between the BMC and TMJ pathologies has a relatively low prevalence in studies that present a considerable number of subjects. From a clinical point of view, a direct association cannot be made between the presence of the BMC and TMJ pathologies or symptoms.
1. Introduction
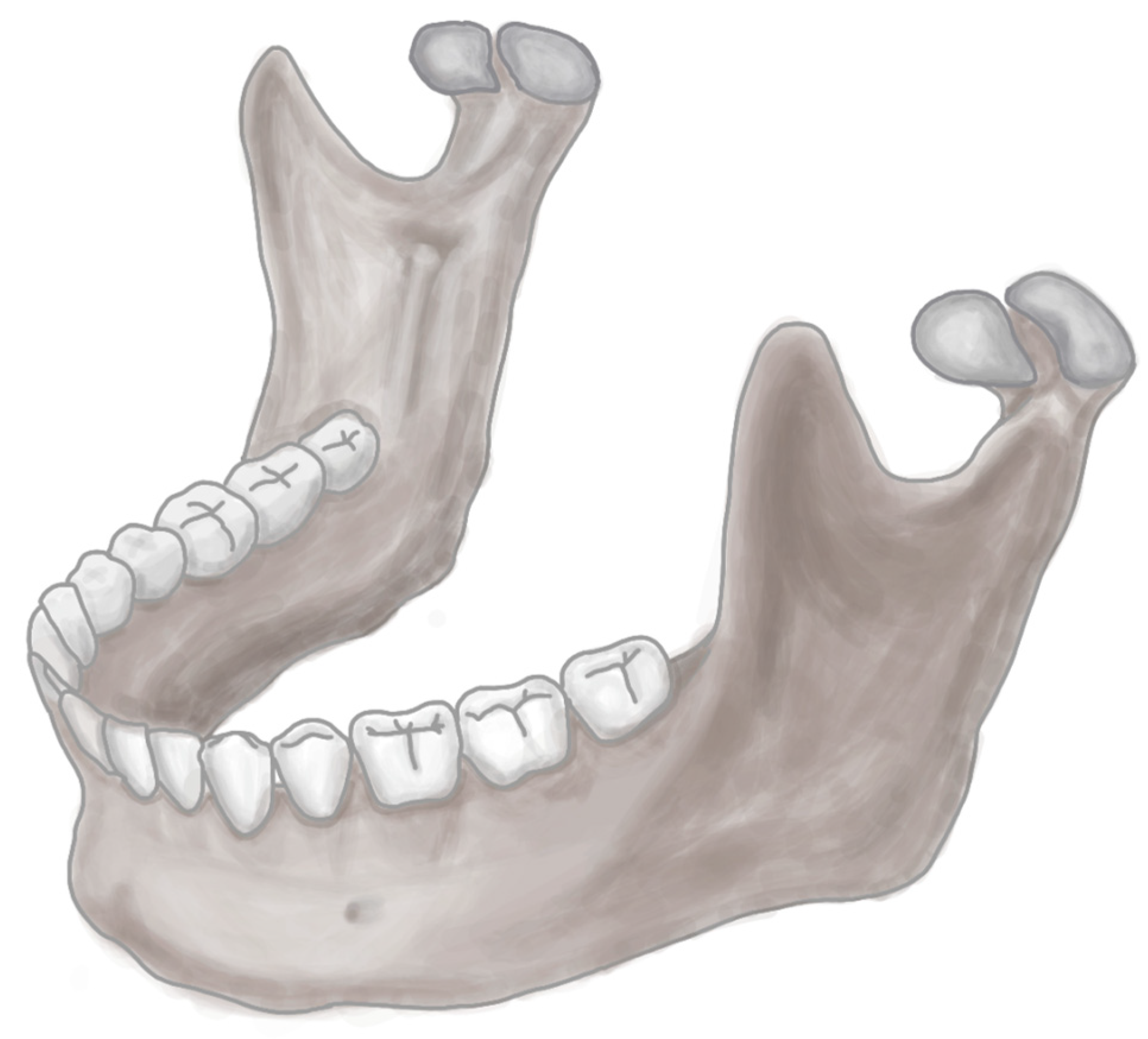
The mandible is a bone belonging to the viscerocranium, the only mobile bone of the skull. Structurally, it is made up of two components: the mandibular body and the mandibular ramus, each with different anatomical characteristics and repairs that fulfill fundamental roles, such as providing articulation to the lower teeth, in addition to allowing the passage of neurovascular structures of importance for the oral and dental region [1,2,3]. In the branch of the mandible are the coronoid and condylar processes; the latter acts as an articular component within the mandible, which allows it to articulate with the mandibular fossa of the temporal bone, thus forming the temporomandibular joint (TMJ). A malformation or variant of any articular or bone component of the TMJ will alter the function of the region. One of the variants of the articular bone components is the multi-headed condyle, a term used to define a rare anomaly that affects the condyle [4,5,6]. The mandibular condyle with two heads is called the bifid mandibular condyle (BMC) (Figure 1). This is characterized by the fact that the head of the mandibular condyle is duplicated and can be both articular components or only one of the two bifurcated condyles. On the other hand, the condyle can be divided into three heads, which is known as the trifid mandibular condyle. Some cases have also been discovered with a condyle divided into four heads, called a tetraphid condyle [7]. Demographically, the BMC does not seem to affect individuals of any specific ethnicity, race, sex, or age, but some literature has reported that the majority of cases are between 3 and 67 years of age. The prevalence of the BMC is controversial, since it varies widely between different published studies, with the most common being 0.3% to 1.82% (4–6). The BMC can be asymptomatic or present different signs and symptoms, such as pain, swelling, hypomobility, joint blockage, deviation, joint dislocation, or even TMJ ankylosis. This highlights the importance of understanding this entity to identify its possible causative factors, and to know the types and degrees of joint dysfunction that can arise without clinical intervention and how these could functionally alter the TMJ [8,9,10,11].
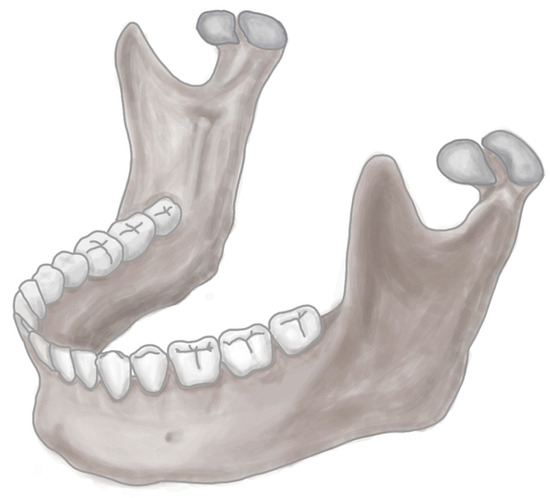
Figure 1.
BMC.
The objective of this review is to understand the prevalence and characteristics of the BMC and its relationship with TMJ pathologies.
2. Methods
2.1. Protocol
This systematic review and meta-analysis were performed and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [12].
2.2. Eligibility Criteria
Studies on the presence of variants and their association with any clinical condition were considered eligible for inclusion if the following criteria were met: (1) population: availability of dissection specimens or BMC images; (2) results: prevalence of the BMC, variants, and their correlation with TMJ pathologies or surrounding regions; and (3) studies: inclusion of research articles, research reports, or original research published in English or Spanish in peer-reviewed journals and indexed in the reviewed databases (listed in Section 2.3). On the other hand, the exclusion criteria were as follows: (1) population: animal studies; (2) studies that analyzed variants from other regions, such as the mandibular ramus, coronoid process, or other neighboring structures only; and (3) studies published as letters to the editor or comments.
2.3. Electronic Search
We systematically searched MEDLINE (via PubMed), Web of Science, Google Scholar, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Scopus, and EMBASE from 1990 to September 2023.
The search strategy included a combination of the following terms: “Anatomy mandibular condyle” (No MeSH), “variation mandibular condyle” (No MeSH), “bifid mandibular condyle ” (No MeSH terms), “trifid mandibular condyle” (No MeSH), “variation anatomical” (No MeSH), “clinical anatomy” (No MeSH), and “pathologies temporomandibular joint” (No MeSH), using the Boolean connectors “AND”, “OR”, and “NOT”.
2.4. Study Selection
Two authors (JJV and MO) independently screened the titles and abstracts of the references retrieved from the search. We obtained the full texts of the references that either author considered potentially relevant. A third reviewer (MR) was included if a consensus could not be reached.
2.5. Data Collection Process
Two authors (PU and JJV) independently extracted data on the outcomes of each study. The following data were extracted from the original reports: (1) authors and year of publication; (2) country; (3) type of study; (4) sample characteristics (sample size, age, distribution, and sex); (5) prevalence and morphological characteristics of the BMC; (6) statistical data reported by each study; and (7) laterality of the variant.
2.6. Assessment of the Methodological Quality of the Included Studies
Quality assessment of the retrospective and prospective observational studies was performed using the methodological quality assurance for anatomical studies (AQUA) tool proposed by the International Evidence-Based Anatomy Working Group [13]. Two reviewers (JJV and PN) independently performed the data extraction and quality assessment. A third reviewer (KK) was involved if a consensus could not be reached. For case study bias, two authors (JS and MR) separately assessed the risk of bias. To bias the case studies, the Joanna Briggs Institute assessment tool for case reports was used [14].This questionnaire has eight items, with answers such as “yes”, “unclear”, “no”, or “not applicable”, with the following criteria to be evaluated: (1) low risk of bias: more than 70% score of “yes”, (2) moderate risk of bias: 50–69% score of “yes”, and (3) high risk of bias: less than 49% score of “yes”.
2.7. Statistical Methods
The data extracted from the meta-analysis were interpreted by calculating the prevalence of BMC variants using the JAMOVI software 2.4.8 version [14]. For the appropriate statistical model for the analysis of the data obtained, we used the DerSimonian–Laird model. Additionally, a random effects model was used because BMC prevalence data were heterogeneous. To calculate heterogeneity, we use the chi-square test (I2). For the chi-square test, the p-value proposed by the Cochrane Collaboration was considered significant when it was <0.10. The values of the I2 statistic were interpreted with a 95% confidence interval [CI] as follows: 0–40% might not be important, 30–60% might indicate moderate heterogeneity, 50–90% might represent substantial heterogeneity, and 75–100% could represent a significant amount of heterogeneity [15].
3. Results
3.1. Included Articles
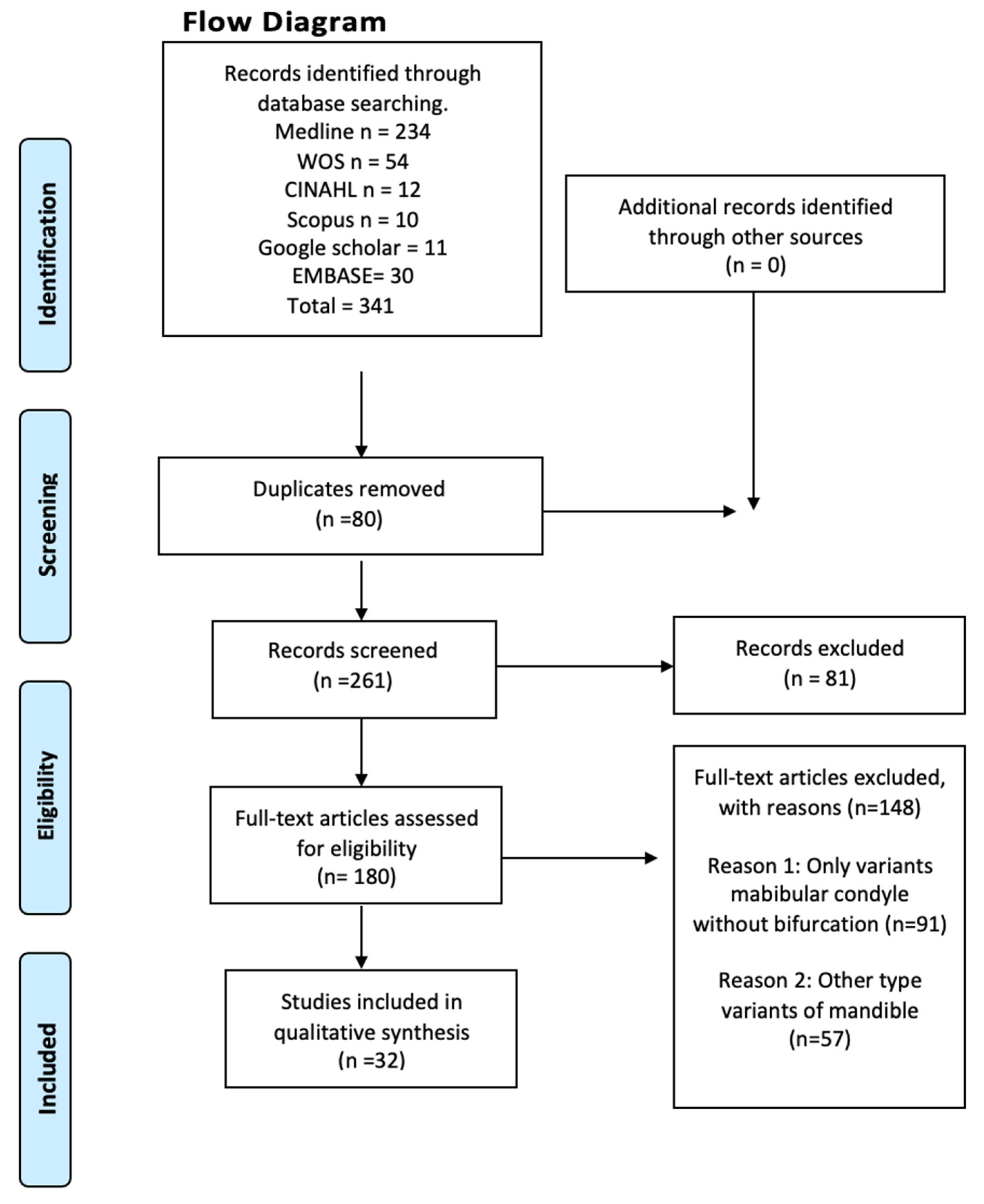
The search resulted in a total of 1097 articles from different databases that met the criteria and search terms established by the research team. The filter was applied to the titles and/or abstracts of the articles in the consulted databases, and the primary criterion of elimination of duplicates was used. In total, 180 full-text articles were evaluated for eligibility for inclusion in this meta-analysis and systematic review. Next, 148 studies were excluded because their primary and secondary results did not match those of this review or because they did not meet the established criteria for good data extraction, resulting in 32 articles being included for analysis (n = 88,625 patients, images, and cadavers) (Figure 2).
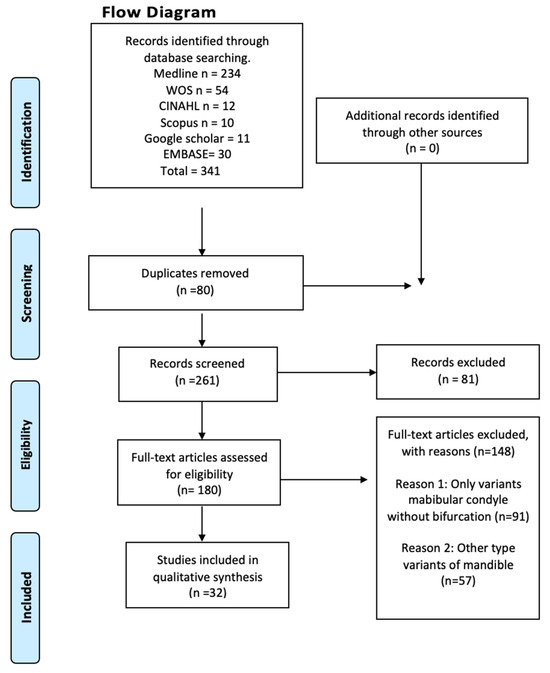
Figure 2.
Search diagram.
3.2. Characteristics of the Studies and the Study Population
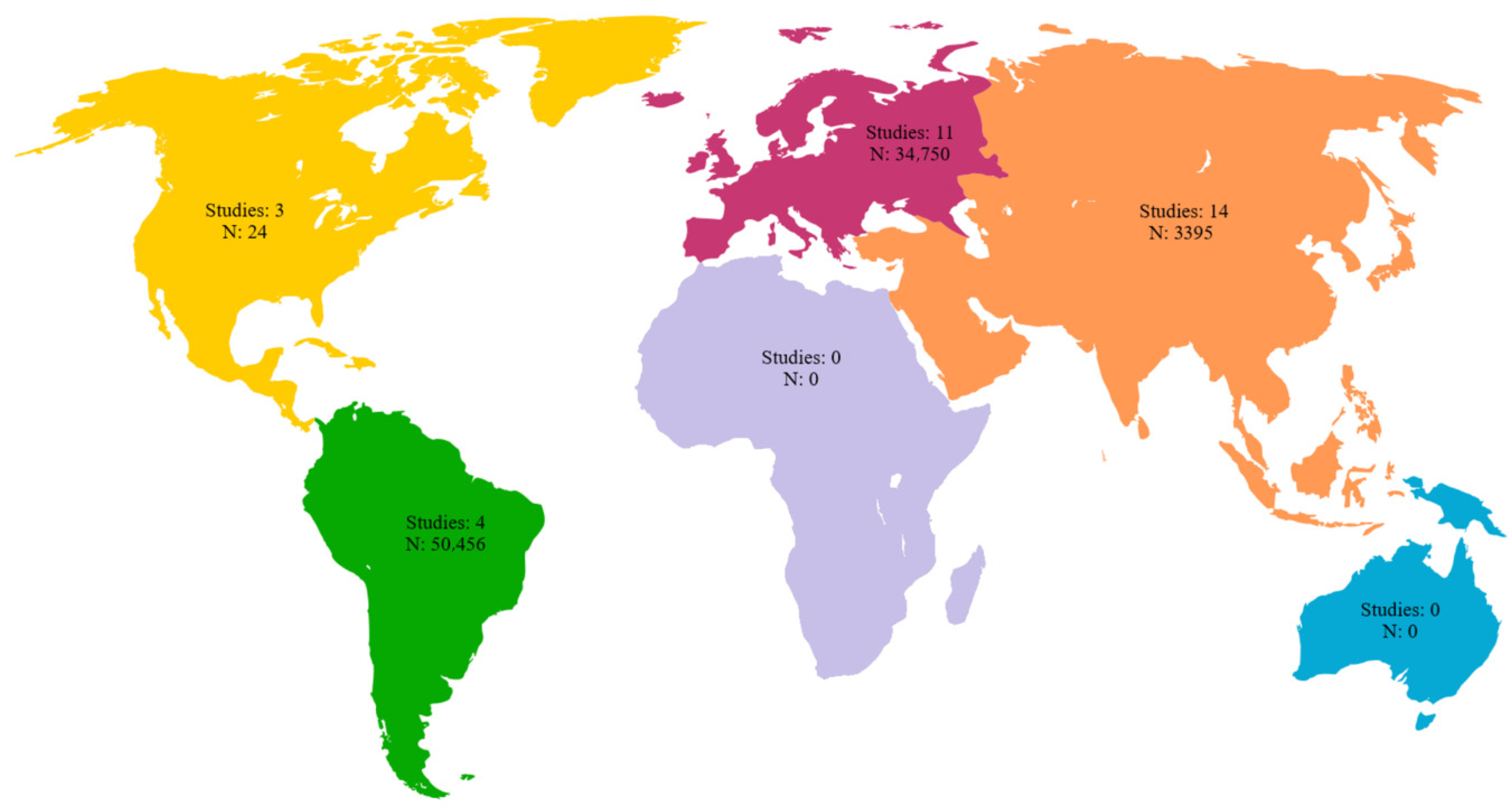
Among the 32 included studies, 11 were case reports, 21 were retrospective studies and none were prospective studies. The samples included in the reviewed studies were geographically distributed across all continents except Africa and Oceania. A total of 11 studies were conducted in Europe which is equivalent to 34.37%. The cumulative number of patients in these studies was 34,750, accounting for 39.21% of the reviewed samples. Among the reviewed studies, 14 were conducted in Asia, which was equivalent to 43.75% of the studies included in this review; the cumulative number of patients in these studies was 3395, which is equivalent to 3.83% of samples included in our analysis. Three studies were conducted in North America, which is equivalent to 9.37% of the studies included in this review. It should be noted that the cumulative number of patients in these three studies was 24, which accounts for 0.03% of the sample size included in our analysis. Four studies were conducted in South America, accounting for 12.5% of the studies included in this review, and the cumulative number of patients in these studies was 50,456, or 56.93% of the analyzed samples (Table 1 and Figure 3).

Table 1.
Characteristics of the included studies.
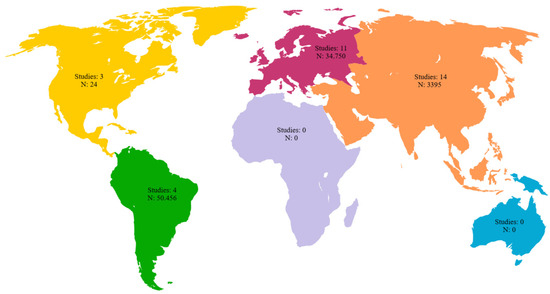
Figure 3.
Geographic distribution of the included studies with number of subjects per continent.
Regarding the 32 studies that included the characteristics of laterality of the jaws with the BMC, only the jaws with the variant were included in this analysis, since we believe that including all jaws that were analyzed would overestimate the results and would not be representative of the characteristics of the BMC. Six of the thirty-two included studies did not report the laterality of jaws with anatomical variants; for the studies that showed the laterality of the anatomical variants, 66 jaws presented bilaterality of the BMC, while 248 jaws presented the BMC unilaterally.
For the sex characteristics in the 32 studies included in this review, we will show the sex of the subjects who presented the variant. Sex was not reported in 10,309 jaws with the BMC variant, which is equivalent to 11.63% of all included subjects. In this review, for the studies that presented the sex of the sample with the BMC, 144 were male, equivalent to 0.16%, while 168 were female, equivalent to 0.18%. It should be noted that the results are only expressed for the variant and not for the total sample, since if we included the entire sample of studies, the results could be overestimated. Regarding the detection methods of BMC in the included studies, 13 studies identified BMC through panoramic radiography, 6 studies through CT scan. On the other hand, the largest number of subjects was detected through panoramic radiography (81,086 subjects), then through cone beam computerized tomography (3110 subjects), and finally through macroscopic evaluation (corpse) (2525 subjects) (Table 2).

Table 2.
Methods for identifying the BMC in the subjects included in this study.
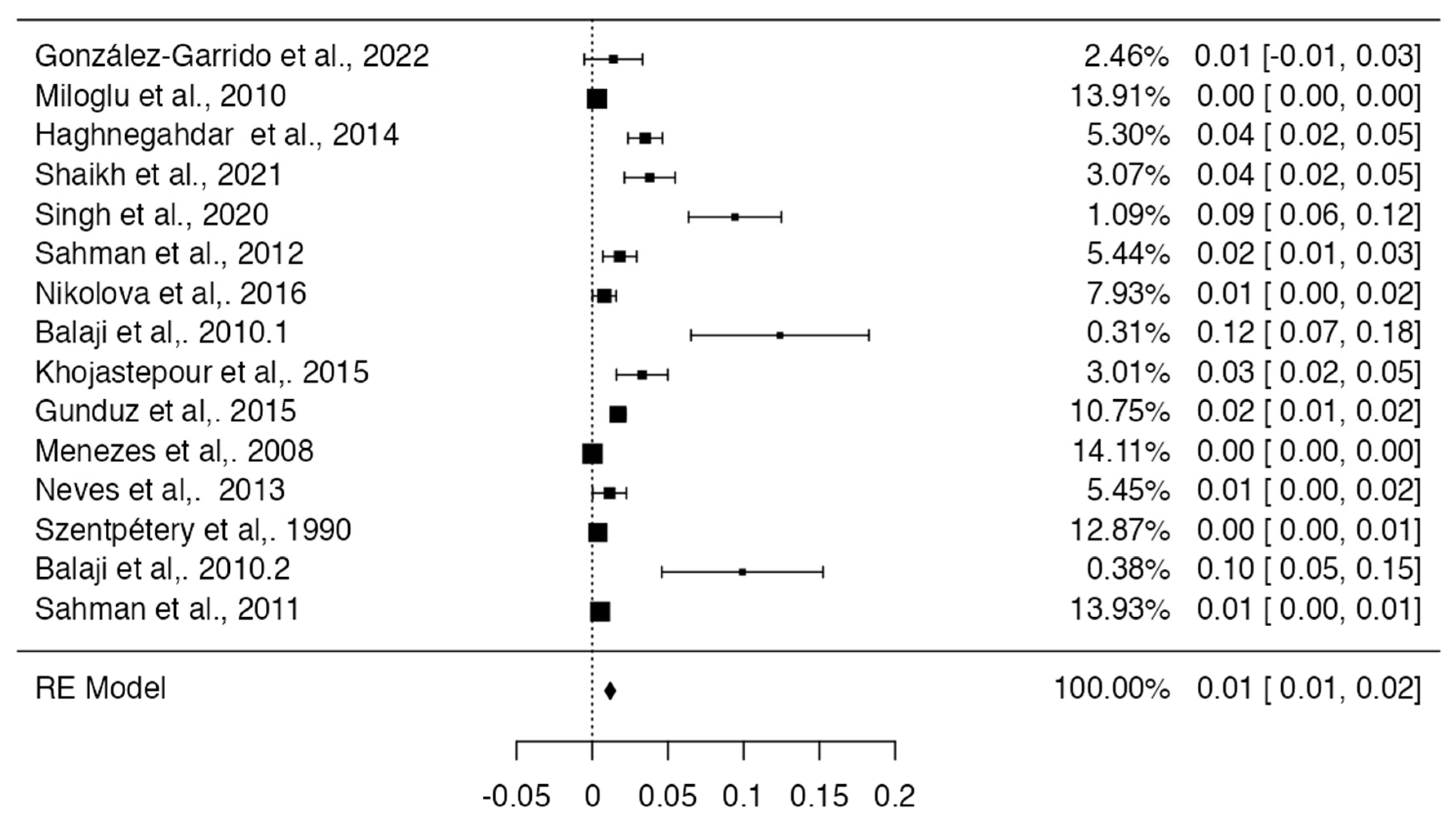
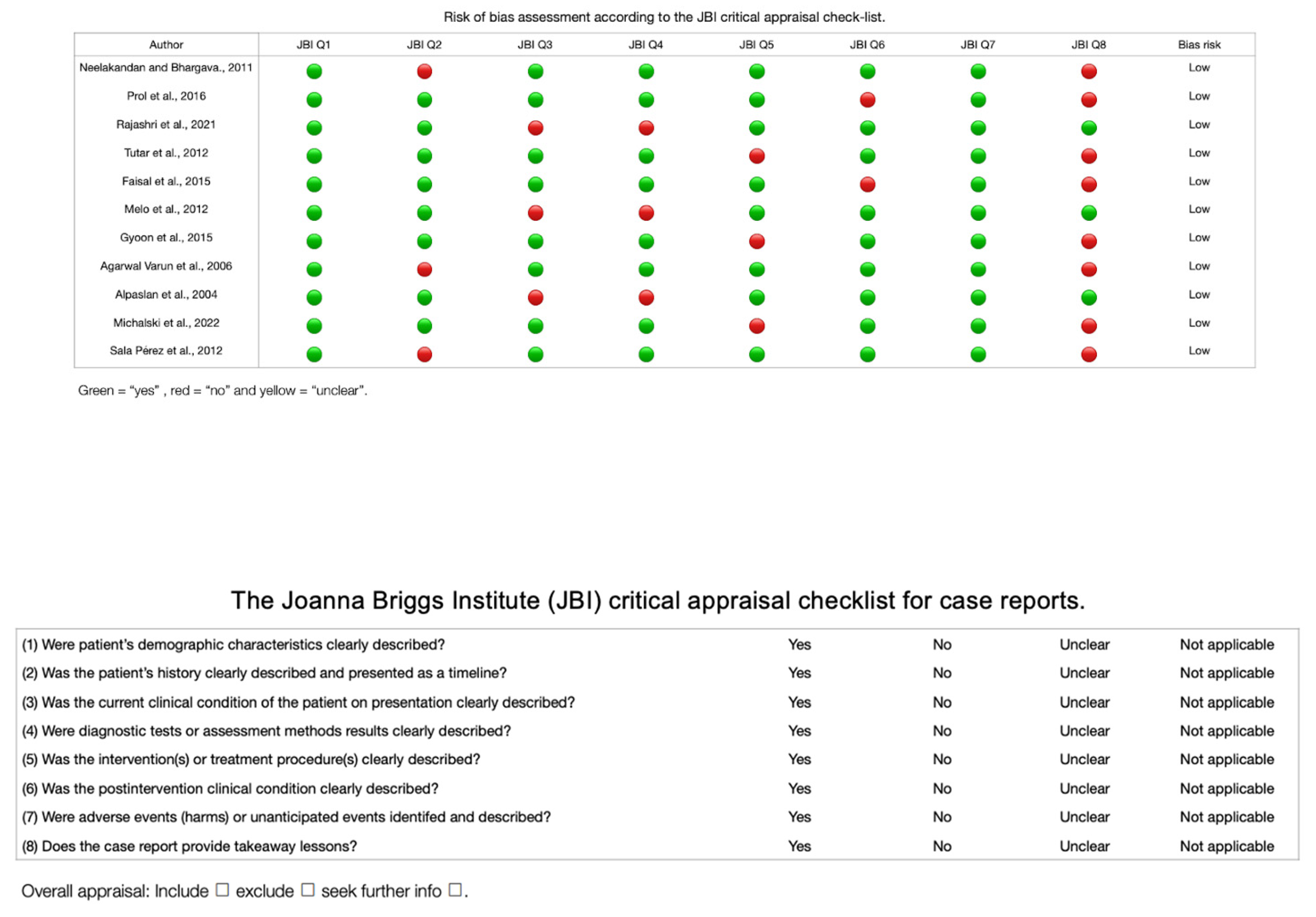
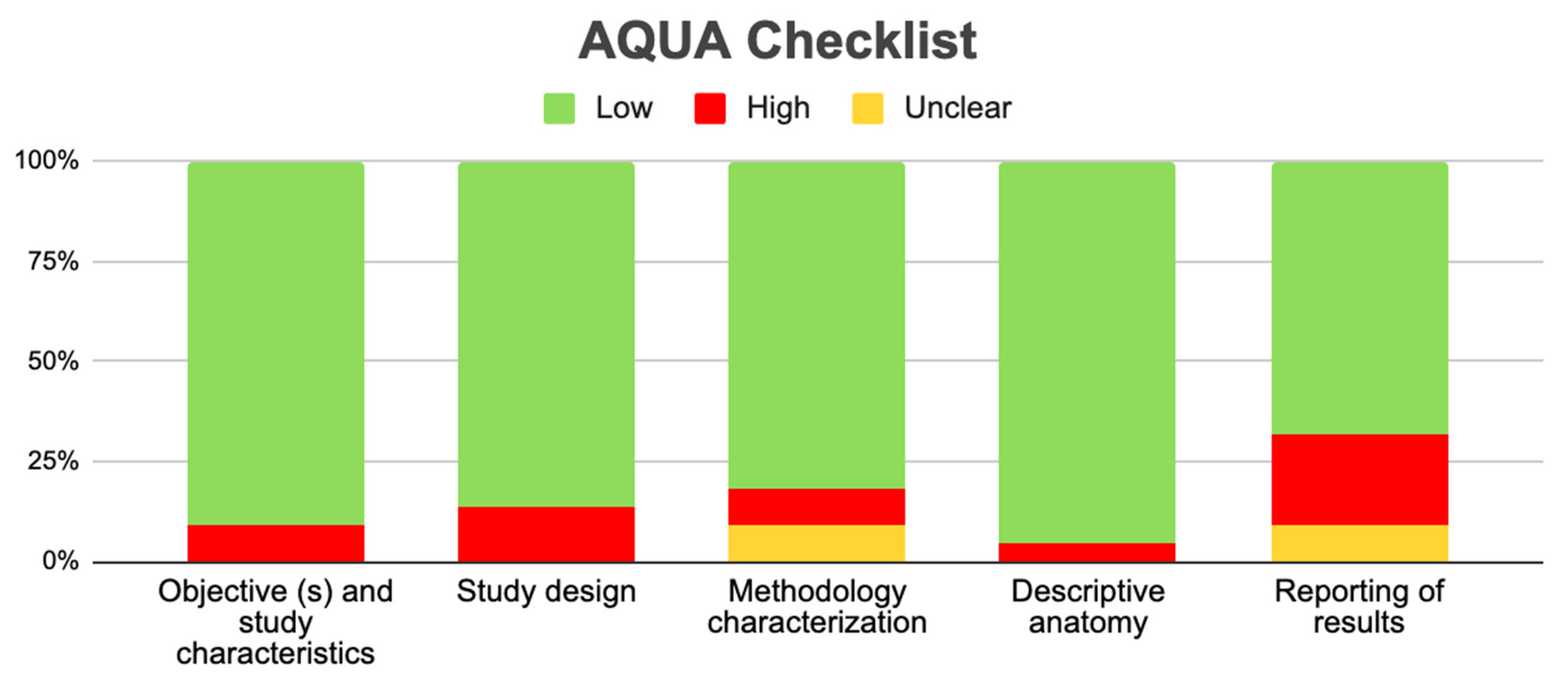
3.3. Prevalence and Risk of Bias
For the meta-analysis of the prevalence of the BMC, 15 studies were included [16,17,22,23,24,25,27,31,32,35,36,37,38,39,47], with a prevalence of 1% with a deviation standard from 1 to 2%, showing a heterogeneity of (I2 = 82%) (Table 3 and Figure 4). Regarding the risk of bias in the case studies, in a total of 11 studies, 100% of the articles analyzed presented a low risk of bias. If we analyze the different items one by one, only question eight remains. “Does the case report provide takeaway lessons?” presented a high risk of bias in eight of the eleven articles analyzed [18,19,20,21,28,29,33,34,40,41,45] (Table 4 and Figure 5). For the analysis of biases using AQUA, 22 studies were included [16,17,22,23,24,25,26,27,30,31,32,35,36,37,38,39,43,44,46,47], of which the main bias presented by the studies was the reporting of results in 7 of 21 studies, and the other items presented a low risk of bias (Table 5 and Figure 6).

Table 3.
Prevalence of included observational articles.
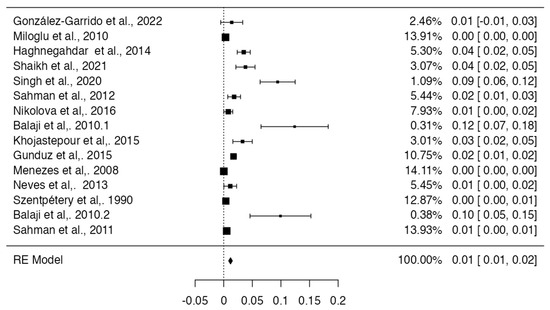
Figure 4.
Forest plot prevalence of the included studies with BMC [16,17,22,23,24,25,27,31,32,35,36,37,38,39,47].

Table 4.
Risk of case study bias.
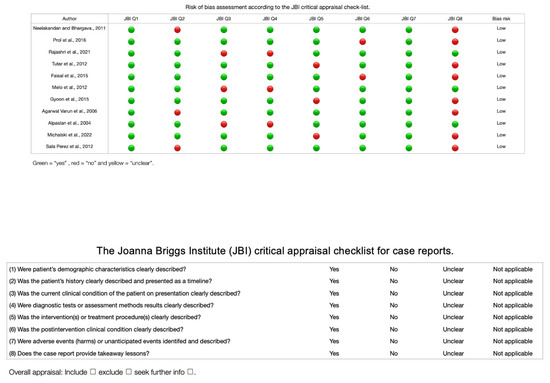
Figure 5.
Risk of bias graph of the included case studies [18,19,20,21,28,29,33,34,40,41,45].

Table 5.
Risk of bias in observational studies (AQUA).
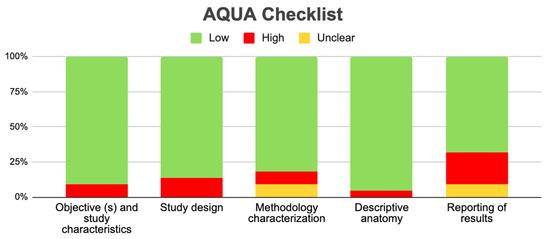
Figure 6.
Risk of bias graph of the included observational studies.
3.4. Clinical Implications
In TMJ, various symptoms or alterations of the joint have been studied with variants such as the BMC or other variants of morphology at the condylar level that can cause symptoms, such as clicking, ankylosis, or pain associated with the joint. This study investigated the frequency or prevalence of bifurcation of the mandibular condyle with its clinical implications. Of all the studies analyzed, only 10 showed a relationship between the BMC and clinical alterations of the TMJ or surrounding structures. All these studies will be detailed below. In the study by Haghnegahdar et al. [22], a third of the 35 cases of bifid mandibular condyle detected presented clicking, associated pain, or both, but these symptoms only occurred at an advanced age in life without previous symptoms. Knowing that this variant is present for life, this study does not report any traumatic factors triggering the symptoms, which is why the only relationship with the symptoms is advanced age. On the other hand, in the study by Sahma et al. [25], of the ten patients with the BMC, two reported a history of facial trauma due to traffic accidents and clicking when opening their mouth. In the study by Gunduz et al. [25], two patients reported clicking when opening their mouth and a history of trauma, so although the BMC was analyzed as a persistent variant over time, the trigger for the symptoms was trauma.
For the study by Perez et al. [45], the clinical examination of the cases of detected bifid mandibular condyle associated it with limitation in mouth opening, moderate pain, and joint sounds in the temporomandibular joint. In addition to joint sounds, movement restriction, or ankylosis, was also reported, progressing without prior detection of the BMC. In the Rehman et al. [46] study, ten cases of bifid mandibular condyle were detected; all presented with ankylosis, nine reported a history of trauma, and one reported a history of infection causing facial deformity. In the study by Michalski et al. [30], the case of a nine-year-old male child is presented. His medical history does not report any history of trauma or infection, but ankylosis of the temporomandibular joint is detected with difficulty in opening the mouth. Mandibular asymmetries associated with prognathism, retraction, or mandibular deviations also occur. In the study by Lee et al. [30], 28 patients with asymmetric mandibular prognathism and 23 patients with symmetrical mandibular prognathism were identified based on differences in bilateral condyles. This study is also associated with the research by Anzola et al. [46]. In this case, a progressive unilateral condylar growth was found that caused a difference in the global elongation of the condylar neck and the body and ramus of the mandible, presenting facial asymmetry in 16 women and 9 men. Finally, another clinical implication reported in some publications corresponds to malocclusion. In the study by Balaji et al. [31], six patients had limitations in mouth opening accompanied by joint sounds (four males and two females). Finally, in the study by Katti et al. [42], a case of a male patient with limited mandibular opening was reported. What is mentioned in these articles means that in the presence of a BMC, alterations will occur in the normal mobility of the TMJ, especially in the closing movement if the presence of a BMC is unilateral, which in turn produces muscle imbalances, especially of the lateral and medial pterygoid muscles. Finally, the presence of BMC can also be associated with TMJ pain which is accentuated in the presence of TMJ ankylosis.
4. Discussion
This systematic review and meta-analysis aimed to report the prevalence of BMC variants and their association with pathologies of the TMJ, infratemporal region, pterygoid muscles, and capsular-ligamentous complex of the temporomandibular region. A prevalence calculation was performed for studies that met the eligibility criteria set by the research team. Using the inclusion criteria, this review attempted to elucidate the characteristics of different anatomical variants of the mandibular condyle. The main finding of our review was that the prevalence of the BMC variant was very low—less than 1%—which correlates with the scientific literature regarding the BMC. Regarding the clinical literature, there is research that shows a relationship, with a greater probability of having some type of chronic and acute symptoms in the TMJ or the infratemporal region.
Other articles have clinically associated the anatomical variants of the BMC with different pathologies of the TMJ. Our review presents a detailed anatomical and clinical approach to the BMC, using updated terminology of the anatomical structures that make up the TMJ. We also provide a functional description and a brief description of the pathophysiology of temporomandibular disorders. It should be noted that we have not found any systematic review and meta-analysis of the BMC, and in the last review with a clinical case, five years have passed since the last anatomical review of the BMC. Regarding the aforementioned reviews, the one by Borras et al. (2018) [48] showed that the BMC can have a congenital or traumatic etiology; hypomobility and arthralgia are the most frequent symptoms, and the treatment options are usually conservative. Unlike this review, we exhaustively detail the anatomy of the mandibular condyle; we also believe that it is necessary to detail whether the condylar variant is a condition of fetal development or one that was caused during life associated with a traumatic event. For the review by Sonneveld et al. (2018) [49], we showed that the BMC is an important anatomical variation that has implications in any mandibular surgery, including implant surgery. A little over 1% of patients have this variation, but not recognizing it in a patient can lead to a bad result. Unlike this study, we show the prevalence and a more detailed anatomy of the variant in addition to saying that the variant can be a structural alteration that, when present, will cause pain and ankylosis, among other symptoms. In the review by Lopez et al. (2010) [50], it is suggested that additional tests, such as MRI or CT, be performed only in cases where the therapeutic approach involves active treatment. It is proposed that the bifid condyle be described as having two condylar heads emerging from the neck of the condyle or below. Unlike our review, these studies only show the anatomy without talking about the prevalence, and they do not give any type of clinical correlation. Finally, the review by Ayat et al. (2019) [51] showed that the anomaly of the mandibular condyle has been described as a condition of unknown etiology and uncertain pathogenesis. Some authors see it as the result of accidental trauma or forceps delivery, with the two heads one behind the other in the sagittal plane. The reported cases are mostly unilateral and generally asymptomatic; unlike what we found, it was mainly not demonstrated that there is no difference between the unilateral and bilateral BMC. In the context of geographical distribution, most of the included studies were conducted in Asia and Europe, but the largest number of samples in the analyzed cohort was from South America. This is a limitation, although we conducted an expanded literature search. Reports were missing from Africa and Oceania, so a more homogeneous geographical distribution was not possible. Consequently, we could not infer whether the BMC is influenced by ethnic factors; however, the included reviews and studies did not show a relationship between ethnic factors that may predispose to the appearance of the BMC. There was no study that showed that variants of the mandibular condyle occurred only unilaterally and bilaterally, which could be more prevalent if it were bilateral in relation to the presence of pathologies such as ankylosis or temporomandibular dysfunctions. Regarding the sex of the subjects who presented the BMC, there was no type of difference between female and male sex, which is why this variant does not present the relationship between presence and sex. Moreover, we have not found any type of study that shows the relationship between sex and BMC. Regarding the prevalence of the BMC, the studies that met the inclusion criteria presented a prevalence of 1%. The literature shows that the prevalence is between 1% and 3%; therefore, what we report in this meta-analysis correlates with previous primary studies. It is possible that we have overestimated or underestimated the prevalence, because the included studies specifically selected patients with the BMC or left out a study that changes these values; however, this was not reported in any of the articles analyzed. Regarding bias, the included case studies and observational studies presented a low risk of bias; however, it should be noted that the latter had a greater bias in the outcome measures. The heterogeneity of the included studies means that the reported data must be taken with caution, and it is also proposed to carry out more studies that establish the association between anatomical variants and clinical implications. This was not detailed in any study though, which is important because there could be overestimated or underestimated data in their conclusions. Regarding the clinical considerations related to the presence of the BMC, the most associated and evidently studied biomechanical phenomenon is the alteration in the fit of the accessory region of the condyle, which causes the joint to be altered during opening and closing movements. This produces a closing movement that is mainly altered because the presence of the BMC often causes there to be an anticipated stop between the articular surfaces of the condyle and the mandibular fossa. If the presence is bilateral, the mechanizing literature reports that the movements in the sagittal plane will be altered and could be more symptomatic in these patients. If the BMC is unilateral, the functional and mechanical alteration will be mainly the lateral movement, and it is reported that the dysfunction and symptoms will mainly depend on the length of the BMC; if it is longer, symptomatology will be ipsilateral, while if it is shorter, the symptomatology will be contralateral. Finally, in this condition of unilaterality, the functional alteration will be contralateral to the presence of the BMC. In the presence of these symptoms and ruling out other possible pathologies that are more prevalent, it is important to perform imaging studies that allow the observation of the BMC. The importance of early diagnosis lies in early detection, and more importantly, in preventing the development of functional and symptomatic alterations in the TMJ. The main symptoms that could suggest the presence of the BMC are pain in the joint space of the TMJ, clicking when moving(which can be painless or with the presence of symptoms in the TMJ),and finally, a symptom that is also repeatedly described in the articles, namely, ankylosis of the TMJ, which presents with little movement and problems in the chewing process and speech of the subjects studied. Finally, it should be noted that, although these are cardinal signs in the face of other pathologies, the presence of these could prompt professionals to analyze the joint through imaging and be able to see the presence of the BMC [52,53]. The symptoms are also varied, but a significant group of studies showed that this anatomical variant could also present asymptomatically throughout life, going unnoticed by many patients.
5. Limitations
The limitations of this review were the publication and authorship bias of the included studies. Studies with different results that were in non-indexed literature in the selected databases may have been excluded, and there is the possibility that the most sensitive and specific search regarding the topic to be studied was not carried out. Finally, the individual sessions of the authors for the selection of articles all resulted in a higher probability of excluding potential cases that are not being reported in the scientific community from countries other than those on the Asian and European continents.
6. Conclusions
In the present study, we have found a correlation between BMC and TMJ pathologies. Through a meta-analysis, we found that the presence of BMC has a relatively low prevalence in studies that presented a considerable number of subjects. From a clinical point of view, a direct association between the presence of BMC and TMJ pathologies or symptoms cannot be established. Considering the above, we believe that knowing this variant is of utmost importance for dental surgeons, especially for those who treat the TMJ region, since it is important to have in-depth knowledge to generate the best guidelines for the treatment and diagnosis of this type of pathology. We also recommend that in the presence of BMC, the masticatory muscles be dynamically worked unilaterally or bilaterally depending on how the BMC presents, in addition to therapies for the symptoms of TMJ. Finally, we believe that it is important to carry out new anatomical and clinical studies that clearly define this condition in the jaw.
Author Contributions
Conceptualization, J.J.V.-F. and M.T.-R.; methodology, P.U.; software, K.-l.K.N.; validation, M.R.-L., A.B.F. and P.N.-B.; formal analysis, J.J.V.-F.; investigation, M.O.-D.; resources, P.U.; data curation, M.R.-L.; writing—original draft preparation, J.J.V.-F. and J.A.S.-G.; writing—review and editing, M.T.-R.; visualization, P.N.-B.; supervision, J.J.V.-F.; project administration, J.J.V.-F.; funding acquisition, none. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kendirci, M.; Göksel, S.; Özcan, İ. Multiheaded mandibular condyles. J. Orofac. Orthop. 2023, 84 (Suppl. S3), 165–171. [Google Scholar] [CrossRef]
- Bettoni, J.; Olivetto, M.; Bouaoud, J.; Duisit, J.; Dakpé, S. Bilateral bifid condyles: A rare etiology of temporomandibular joint disorders. Cranio 2021, 39, 270–273. [Google Scholar] [CrossRef] [PubMed]
- Antoniades, K.; Karakasis, D.; Elephtheriades, J. Bifid mandibular condyle resulting from a sagittal fracture of the condylar head. Br. J. Oral. Maxillofac. Surg. 1993, 31, 124–126. [Google Scholar] [CrossRef] [PubMed]
- Cowan, D.F.; Ferguson, M.M. Bifid mandibular condyle. Dentomaxillofac. Radiol. 1997, 26, 70–73. [Google Scholar] [CrossRef] [PubMed]
- Loh, F.C.; Yeo, J.F. Bifid mandibular condyle. Oral Surg. Oral Med. Oral Pathol. 1990, 69, 24–27. [Google Scholar] [CrossRef]
- Antoniades, K.; Hadjipetrou, L.; Antoniades, V.; Paraskevopoulos, K. Bilateral bifid mandibular condyle. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. Endod. 2004, 97, 535–538. [Google Scholar] [CrossRef]
- Hersek, N.; Ozbek, M.; Taşar, F.; Akpinar, E.; Firat, M. Bifid mandibular condyle: A case report. Dent. Traumatol. 2004, 20, 184–186. [Google Scholar] [CrossRef]
- Balciunas, B.A. Bifid mandibular condyle. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 1986, 44, 324–325. [Google Scholar] [CrossRef]
- Nagpal, A.; Vaddi, A.; Tadinada, A. Shifting the Spotlight From the Mandibular Condyle to the Coronoid Process: A Report of a Unique Case of Trifid Mandibular Coronoid Process. Cureus 2023, 15, e37593. [Google Scholar] [CrossRef]
- Plevnia, J.R.; Smith, J.A.; Stone, C.G. Bifid mandibular condyle without history of trauma or pain: Report of a case. J. Oral Maxillofac. Surg. 2009, 67, 1555–1561. [Google Scholar] [CrossRef]
- Shriki, J.; Lev, R.; Wong, B.F.; Sundine, M.J.; Hasso, A.N. Bifid mandibular condyle: CT and MR imaging appearance in two patients: Case report and review of the literature. AJNR Am. J. Neuroradiol. 2005, 26, 1865–1868. [Google Scholar] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Jordan, Z.; Lockwood, C.; Munn, Z.; Aromataris, E. Redeveloping the JBI Model of Evidence Based Healthcare. Int. J. Evid. Based Healthc. 2018, 16, 227–241. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing, Version 4.0; Computer Software; R Packages Retrieved from MRAN Snapshot 2021-04-01; R Core Team: Vienna, Austria, 2021. Available online: https://cran.r-project.org (accessed on 18 October 2023).
- Henry, B.M.; Tomaszewski, K.A.; Walocha, J.A. Methods of Evidence-Based Anatomy: A guide to conducting systematic reviews and meta-analysis of anatomical studies. Ann. Anat. 2016, 205, 16–21. [Google Scholar] [CrossRef]
- González-Garrido, L.; Gómez-González, S.; Gonzalo-Orden, J.M.; Wasterlain, S.N. Multi-headed (bifid and trifid) mandibular condyles in archaeological contexts: Two posttraumatic cases. Arch. Oral Biol. 2022, 134, 105326. [Google Scholar] [CrossRef] [PubMed]
- Miloglu, O.; Yalcin, E.; Buyukkurt, M.; Yilmaz, A.; Harorli, A. The frequency of bifid mandibular condyle in a Turkish patient population. Dentomaxillofac. Radiol. 2010, 39, 42–46. [Google Scholar] [CrossRef]
- Neelakandan, R.S.; Bhargava, D. Bifid hyperplastic mandibular condyle. J. Maxillofac. Oral Surg. 2013, 12, 466–471. [Google Scholar] [CrossRef][Green Version]
- Prol, C.; Álvarez, J.; Mendiola, J. Bilateral bifid mandibular condyle. Acta Otorrinolaringol. Esp. (Engl. Ed.) 2017, 68, 303–304, (In English and Spanish). [Google Scholar] [CrossRef]
- Rajashri, P.; Kumar, S.P. Bifid Mandibular Condyle as the Hidden Cause for Temporomandibular Joint Disorder. Cureus 2021, 13, e17609. [Google Scholar] [CrossRef]
- Tutar, O.; Bas, A.; Gülsen, G.; Bayraktarov, E. Bifid mandibular condyle: CT and MRI appearance. BMJ Case Rep. 2012, 2012, bcr2012006976. [Google Scholar] [CrossRef]
- Haghnegahdar, A.A.; Bronoosh, P.; Khojastepour, L.; Tahmassebi, P. Prevalence of bifid mandibular condyle in a selected population in South of iran. J. Dent. 2014, 15, 156–160. [Google Scholar]
- Shaikh, A.H.; Ahmed, S.; Ahmed, A.R.; Das, G.; Taqi, M.; Nisar, S.; Khan, O. Assessment of radiographic morphology of mandibular condyles: A radiographic study. Folia Morphol. 2022, 81, 481–486. [Google Scholar] [CrossRef] [PubMed]
- Singh, B.; Kumar, N.R.; Balan, A.; Nishan, M.; Haris, P.S.; Jinisha, M.; Denny, C.D. Evaluation of Normal Morphology of Mandibular Condyle: A Radiographic Survey. J. Clin. Imaging Sci. 2020, 10, 51. [Google Scholar] [CrossRef] [PubMed]
- Sahman, H.; Sisman, Y.; Sekerci, A.E.; Tarim-Ertas, E.; Tokmak, T.; Tuna, I.S. Detection of bifid mandibular condyle using computed tomography. Med. Oral Patol. Oral Cir. Bucal. 2012, 17, e930–e934. [Google Scholar] [CrossRef] [PubMed]
- Rehman, T.A.; Gibikote, S.; Ilango, N.; Thaj, J.; Sarawagi, R.; Gupta, A. Bifid mandibular condyle with associated temporomandibular joint ankylosis: A computed tomography study of the patterns and morphological variations. Dentomaxillofac. Radiol. 2009, 38, 239–244. [Google Scholar] [CrossRef]
- Nikolova, S.Y.; Toneva, D.H.; Lazarov, N.E. Incidence of a Bifid Mandibular Condyle in Dry Mandibles. J. Craniofac. Surg. 2017, 28, 2168–2173. [Google Scholar] [CrossRef]
- Faisal, M.; Ali, I.; Pal, U.S.; Bannerjee, K. Bifid mandibular condyle: Report of two cases of varied etiology. Natl. J. Maxillofac. Surg. 2010, 1, 78–80. [Google Scholar] [CrossRef]
- Melo, S.L.; Melo, D.P.; Oenning, A.C.; Haiter-Neto, F.; Almeida, S.M.; Campos, P.S. Magnetic resonance imaging findings of true bifid mandibular condyle with duplicated mandibular fossa. Clin. Anat. 2012, 25, 650–655. [Google Scholar] [CrossRef]
- Lee, J.S.; Xi, T.; Kwon, T.G. Three-dimensional analysis of mandibular condyle position in patients with deviated mandibular prognathism. Int. J. Oral Maxillofac. Surg. 2017, 46, 1052–1058. [Google Scholar] [CrossRef]
- Balaji, S.M. Bifid mandibular condyle: A study of the clinical features, patterns and morphological variations using CT scans. J. Maxillofac. Oral Surg. 2010, 9, 38–41. [Google Scholar] [CrossRef]
- Khojastepour, L.; Kolahi, S.; Panahi, N.; Haghnegahdar, A. Cone Beam Computed Tomographic Assessment of Bifid Mandibular Condyle. J. Dent. 2015, 12, 868–873. [Google Scholar]
- Gyoon, K.; Jeong, Y.H.; Kosel, E.; Agnew, A.M.; McComb, D.W.; Bodnyk, K.; Hart, R.T.; Kim, M.K.; Han, S.Y.; Johnston, W.M. Regional variation of bone tissue properties at the human mandibular condyle. Bone 2015, 77, 98–106. [Google Scholar] [CrossRef]
- Michalski, C.D.; Pollizzi, A.; Dhar, D.; Hayes, L.L.; Chandra, T. Bifid Mandibular Condyle with Associated Temporomandibular Joint Ankylosis: A Rare Skeletal Abnormality. Cureus 2022, 14, e29624. [Google Scholar] [CrossRef] [PubMed]
- Menezes, A.V.; de Moraes Ramos, F.M.; de Vasconcelos-Filho, J.O.; Kurita, L.M.; de Almeida, S.M.; Haiter-Neto, F. The prevalence of bifid mandibular condyle detected in a Brazilian population. Dentomaxillofac. Radiol. 2008, 37, 220–223. [Google Scholar] [CrossRef]
- Neves, F.; Ramirez, L.; Roque, R.; Lopes, G.; Haiter, F.; Queiroz, D. Detection of bifid mandibular condyle by panoramic radiography and cone beam computed tomography. J. Braz. Oral Sci. 2013, 12, 133–139. [Google Scholar]
- Szentpétery, A.; Kocsis, G.; Marcsik, A. The problem of the bifid mandibular condyle. J. Oral Maxillofac. Surg. 1990, 48, 1254–1257. [Google Scholar] [CrossRef]
- Balaji, S.M. Bifid mandibular condyle with tempromandibular joint ankylosis—A pooled data analysis. Dent. Traumatol. 2010, 26, 332–337. [Google Scholar] [CrossRef]
- Sahman, H.; Sekerci, A.E.; Ertas, E.T.; Etoz, M.; Sisman, Y. Prevalence of bifid mandibular condyle in a Turkish population. J. Oral Sci. 2011, 53, 433–437. [Google Scholar] [CrossRef][Green Version]
- Varun, A.; Suhas, S.; Pai, K.M.; Shetty, C.M.; Auluck, A. Bifid mandibular condyles: Report of four cases. Dent. Update 2006, 33, 368–370. [Google Scholar] [CrossRef]
- Alpaslan, S.; Ozbek, M.; Hersek, N.; Kanli, A.; Avcu, N.; Firat, M. Bilateral bifid mandibular condyle. Dentomaxillofac. Radiol. 2004, 33, 274–277. [Google Scholar] [CrossRef]
- Katti, G.; Najmuddin, M.; Fatima, S.; Unnithan, J. Bifid mandibular condyle. BMJ Case Rep. 2012, 2012, bcr-2012-007051. [Google Scholar] [CrossRef]
- Sreenivasagan, S.; George, A.M.; Rengalakshmi, S. Variation in condylar morphology in different malocclusion among Indians. Bioinformation 2021, 17, 1134–1137. [Google Scholar] [CrossRef]
- Schmitter, M.; Gabbert, O.; Ohlmann, B.; Hassel, A.; Wolff, D.; Rammelsberg, P.; Kress, B. Assessment of the reliability and validity of panoramic imaging for assessment of mandibular condyle morphology using both MRI and clinical examination as the gold standard. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2006, 102, 220–224. [Google Scholar] [CrossRef] [PubMed]
- Pérez, S.; Vázquez-Delgado, E.; Rodríguez-Baeza, A.; Gay-Escoda, C. Bifid mandibular condyle: A disorder in its own right? J. Am. Dent. Assoc. 2010, 141, 1076–1085. [Google Scholar] [CrossRef] [PubMed]
- Anzola, F.L.K.; Moron, A.S.; Jaramillo, C.M.C.; Quijano, G.D.C.; Hernandez, H.N.; González, A.E.; Rodriguez, I.; Moreno, L.S.M.; Amador, P.E.; Orozco, F.M.; et al. Quantitative bone SPECT analysis of mandibular condyles in an asymptomatic population: An approach to normal reference values. Int. J. Oral Maxillofac. Surg. 2021, 50, 733–739. [Google Scholar] [CrossRef]
- Gunduz, K.; Buyuk, C.; Egrioglu, E. Evaluación de la Prevalencia de Cóndilo Mandibular Bífido Detectado en Tomografía Computadorizada Cone-Beam en una Población Turca. Int. J. Morphol. 2015, 1, 43–47. [Google Scholar] [CrossRef]
- Borrás-Ferreres, J.; Sánchez-Torres, A.; Gay-Escoda, C. Bifid mandibular condyles: A systematic review. Med. Oral Patol. Oral Cir. Bucal. 2018, 23, e672–e680. [Google Scholar] [CrossRef] [PubMed]
- Sonneveld, K.A.; Mai, P.T.; Hogge, M.; Choi, E.Y.; Portnof, J.E. Bifid Mandibular Canal: A Case Review and Retrospective Review of CBCTs. Implant Dent. 2018, 27, 682–686. [Google Scholar] [CrossRef]
- López-López, J.; Ayuso-Montero, R.; Salas, E.J.; Roselló-Llabrés, X. Bifid condyle: Review of the literature of the last 10 years and report of two cases. Cranio 2010, 28, 136–140. [Google Scholar] [CrossRef]
- Ayat, A.; Boudaoud, Z.; Djafer, L. Trifid mandibular condyle: A case report and literature review. J. Stomatol. Oral Maxillofac. Surg. 2019, 120, 601–604. [Google Scholar] [CrossRef]
- Vervaeke, K.; Verhelst, P.J.; Orhan, K.; Lund, B.; Benchimol, D.; Van der Cruyssen, F.; De Laat, A.; Jacobs, R.; Politis, C. Correlation of MRI and arthroscopic findings with clinical outcome in temporomandibular joint disorders: A retrospective cohort study. Head Face Med. 2022, 18, 2. [Google Scholar] [CrossRef] [PubMed]
- Ouyang, N.; Zhang, C.; Xu, F.; Chen, T.; Shen, G.; Si, J.; Yu, H. Evaluation of optimal single-photon emission computed tomography reference value and three-dimensional mandibular growth pattern in 54 Chinese unilateral condylar hyperplasia patients. Head Face Med. 2023, 19, 18. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).