A Laboratory Medicine Perspective on the Investigation of Phaeochromocytoma and Paraganglioma
Abstract
1. Introduction
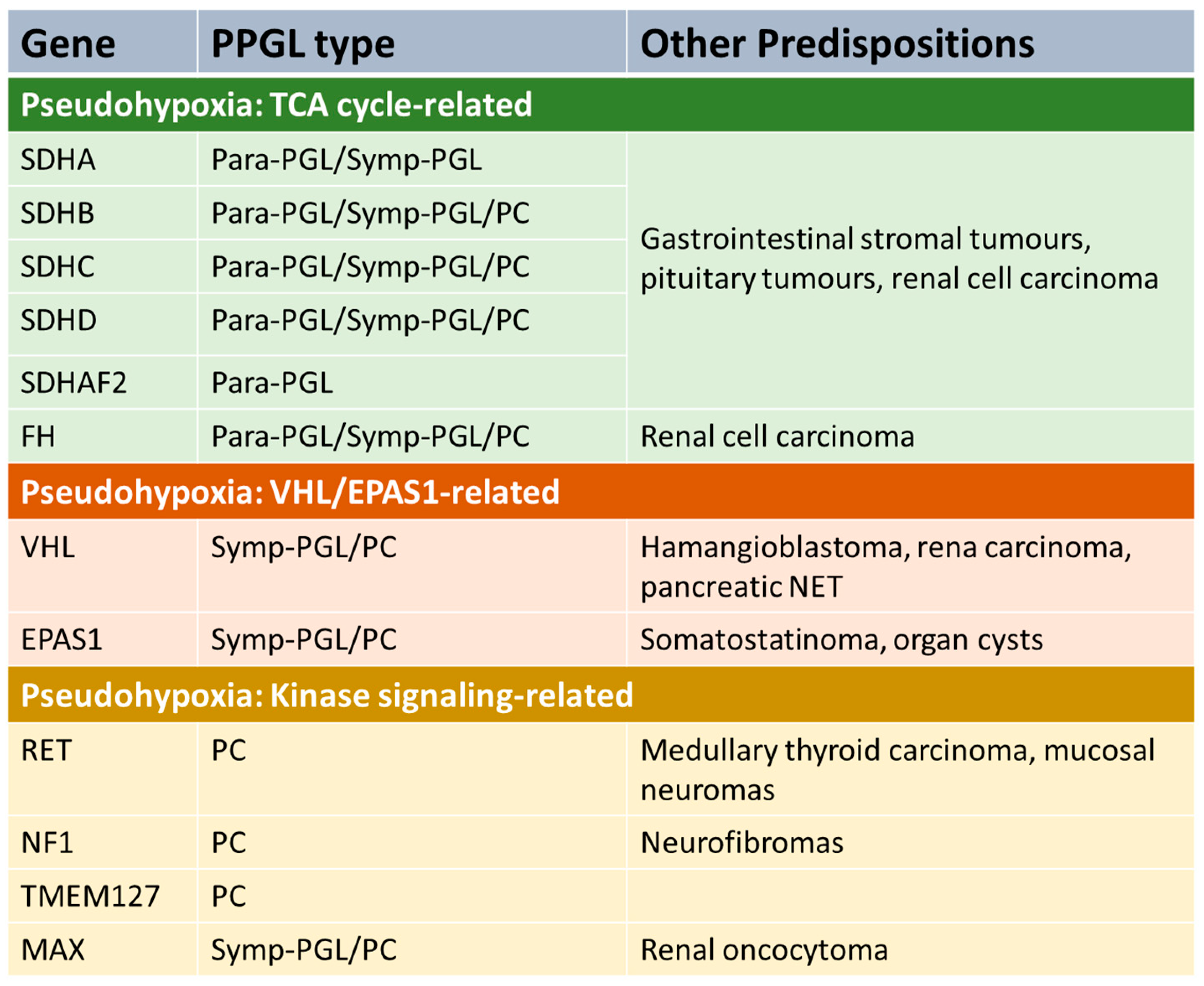
1.1. Biochemical and Genetic Characteristics of PPGL
1.2. Presentation of PPGL—Symptoms, Morbidity and Mortality
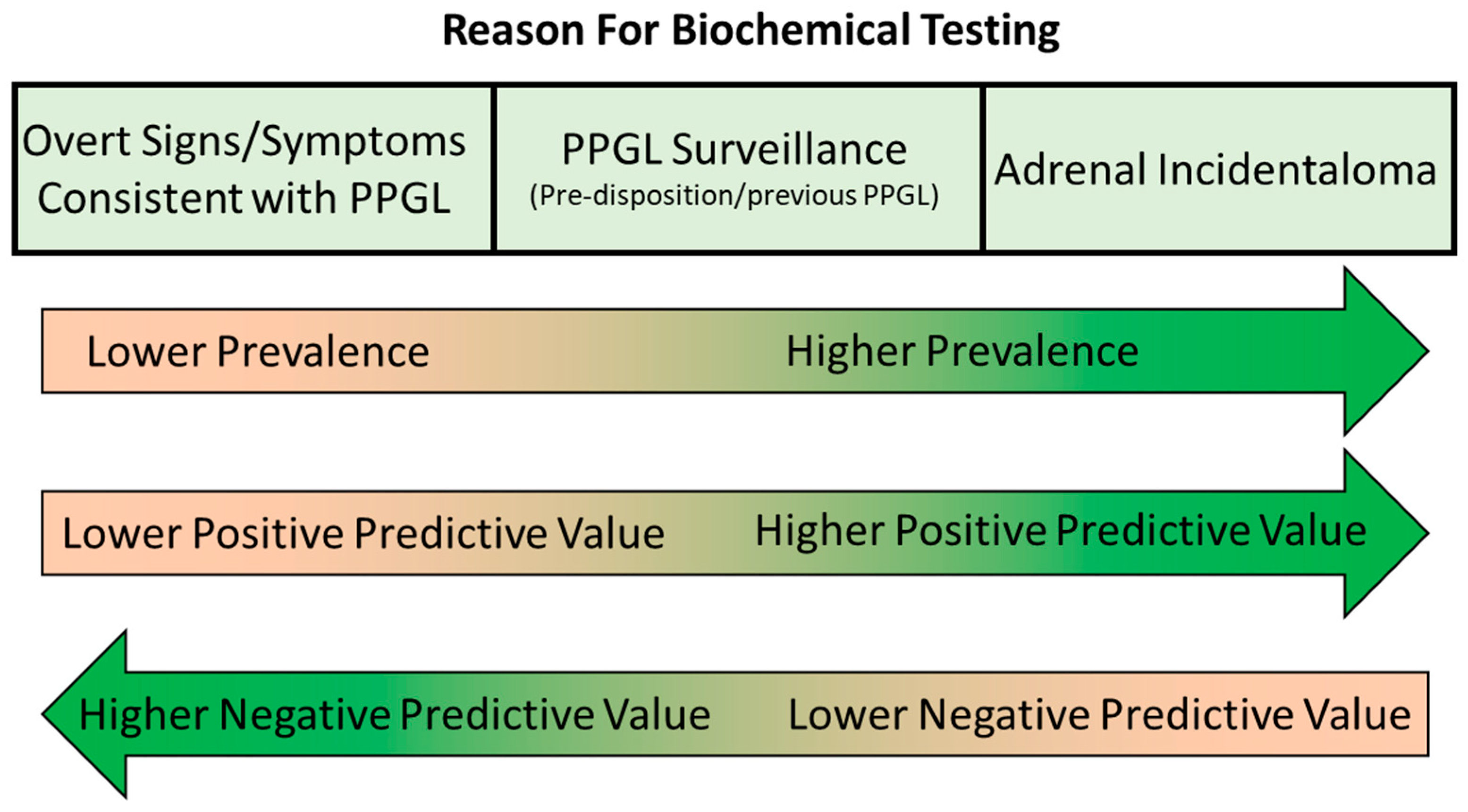
2. The Role of Biochemical Testing in PPGL
2.1. Diagnosis of PPGL
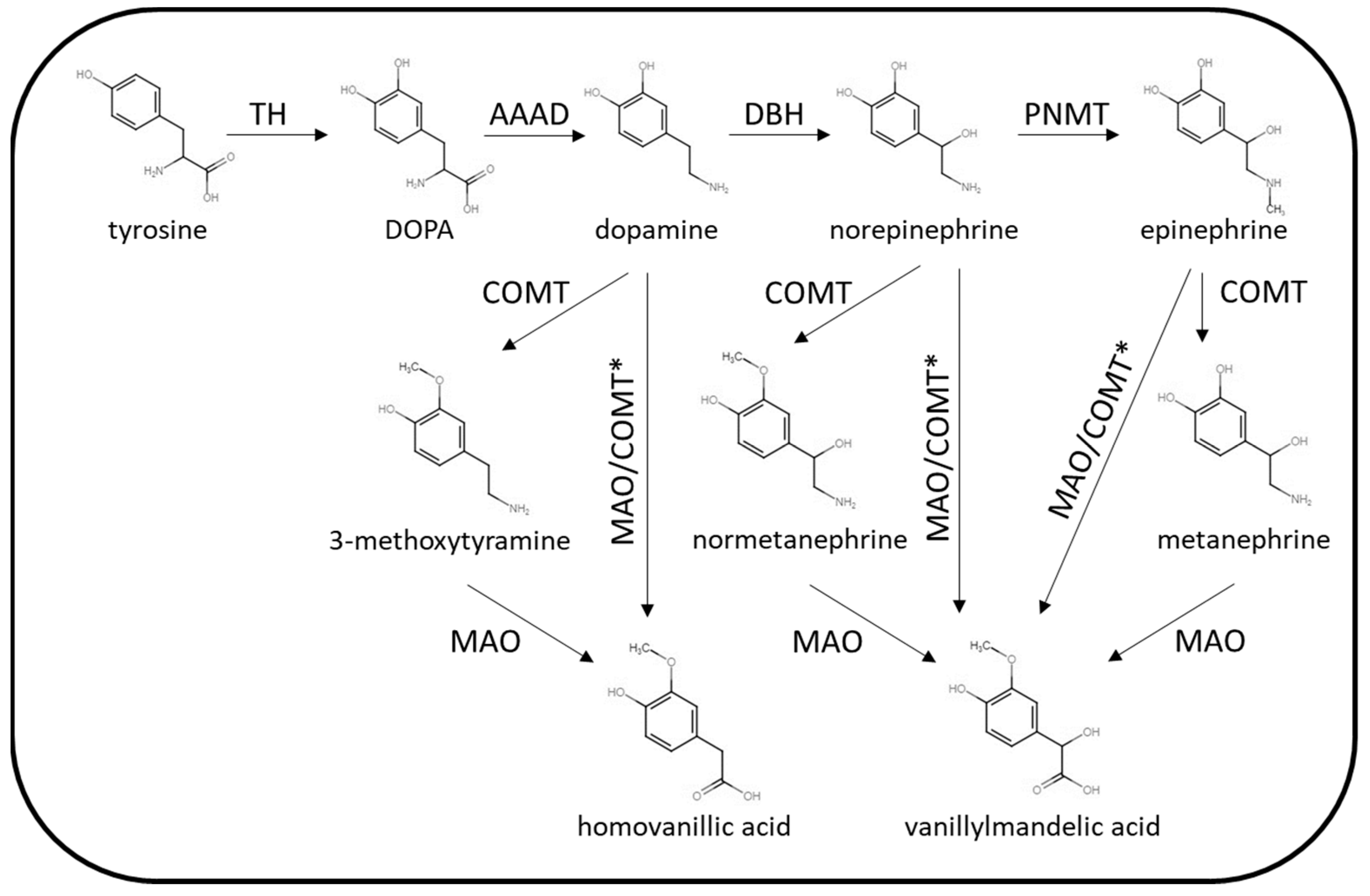
2.2. Biochemical Tests for PPGL
3. Pre-Analytical Considerations
3.1. Effects of Medications
3.2. Patient Preparation
3.3. Sample Collection—Urine Metanephrines
3.4. Sample Collection—Plasma Metanephrines
4. Analytical Considerations
4.1. Colourimetry
4.2. Immunoassay
4.3. Liquid Chromatography—Electrochemical Detection
4.4. Liquid Chromatography–Tandem Mass Spectrometry
5. Post-Analytical Considerations
5.1. Reference Ranges
5.2. Interpretation
6. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mete, O.; Asa, S.L.; Gill, A.J.; Kimura, N.; de Krijger, R.R.; Tischler, A. Overview of the 2022 WHO Classification of Paragangliomas and Pheochromocytomas. Endocr. Pathol. 2022, 33, 90–114. [Google Scholar] [CrossRef] [PubMed]
- Stenman, A.; Zedenius, J.; Juhlin, C.C. The value of histological algorithms to predict the malignancy potential of pheochromocytomas and abdominal paragangliomas—A meta-analysis and systematic review of the literature. Cancers 2019, 11, 225. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.Y.; Kim, J.H.; Hong, A.R.; Seong, M.W.; Lee, K.E.; Kim, S.J.; Kim, S.W.; Shin, C.S.; Kim, S.Y. Disentangling of malignancy from benign pheochromocytomas/paragangliomas. PLoS ONE 2016, 11, e0168413. [Google Scholar] [CrossRef] [PubMed]
- Bima, C.; Bioletto, F.; Lopez, C.; Bollati, M.; Arata, S.; Procopio, M.; Gesmundo, I.; Ghigo, E.; Maccario, M.; Parasiliti-Caprino, M. Clinical and Pathological Tools for Predicting Recurrence and/or Metastasis in Patients with Pheochromocytoma and Paraganglioma. Biomedicines 2022, 10, 1813. [Google Scholar] [CrossRef]
- Crona, J.; Taïeb, D.; Pacak, K. New Perspectives on Pheochromocytoma and Paraganglioma: Toward a Molecular Classification. Endocr. Rev. 2017, 38, 489–515. [Google Scholar] [CrossRef]
- Guerin, C.; Romanet, P.; Taieb, D.; Brue, T.; Lacroix, A.; Sebag, F.; Barlier, A.; Castinetti, F. Looking beyond the thyroid: Advances in the understanding of pheochromocytoma and hyperparathyroidism phenotypes in MEN2 and of non-MEN2 familial forms. Endocr. Relat. Cancer 2018, 25, T15–T28. [Google Scholar] [CrossRef]
- Jhawar, S.; Arakawa, Y.; Kumar, S.; Varghese, D.; Kim, Y.S.; Roper, N.; Elloumi, F.; Pommier, Y.; Pacak, K.; Rivero, J.D. New Insights on the Genetics of Pheochromocytoma and Paraganglioma and Its Clinical Implications. Cancers 2022, 14, 594. [Google Scholar] [CrossRef]
- Rednam, S.P.; Erez, A.; Druker, H.; Janeway, K.A.; Kamihara, J.; Kohlmann, W.K.; Nathanson, K.L.; States, L.J.; Tomlinson, G.E.; Villani, A.; et al. Von Hippel-Lindau and Hereditary Pheochromocytoma/Paraganglioma Syndromes: Clinical Features, Genetics, and Surveillance Recommendations in Childhood. Clin. Cancer Res. 2017, 23, e68–e75. [Google Scholar] [CrossRef]
- Islam, F.; Pillai, S.; Gopalan, V.; Lam, A.K.Y. Identification of Novel Mutations and Expressions of EPAS1 in Phaeochromocytomas and Paragangliomas. Genes 2020, 11, 1254. [Google Scholar] [CrossRef]
- Zhang, X.; Lian, P.; Su, M.; Ji, Z.; Deng, J.; Zheng, G.; Wang, W.; Ren, X.; Jiang, T.; Zhang, P.; et al. Single-cell transcriptome analysis identifies a unique tumor cell type producing multiple hormones in ectopic ACTH and CRH secreting pheochromocytoma. Elife 2021, 10, e68436. [Google Scholar] [CrossRef]
- Elliott, P.F.; Berhane, T.; Ragnarsson, O.; Falhammar, H. Ectopic ACTH-and/or CRH-Producing Pheochromocytomas. J. Clin. Endocrinol. Metab. 2021, 106, 598–608. [Google Scholar] [CrossRef]
- Yee, S.K.; Meyer, J.H.; Wong, L.L. Vasoactive Intestinal Peptide-Secreting Pheochromocytoma: A Case Report and Review of Literature. AACE Clin. Case Rep. 2022, 8, 158–162. [Google Scholar] [CrossRef] [PubMed]
- Smith, S.L.; Slappy, A.L.J.; Fox, T.P.; Scolapio, J.S. Pheochromocytoma producing vasoactive intestinal peptide. Mayo Clin. Proc. 2002, 77, 97–100. [Google Scholar] [CrossRef] [PubMed]
- Mumby, C.; Davis, J.R.E.; Trouillas, J.; Higham, C.E. Phaeochromocytoma and Acromegaly: A unifying diagnosis. Endocrinol. Diabetes Metab. Case Rep. 2014, 2014, 140036. [Google Scholar] [CrossRef]
- Soltani, A.; Pourian, M.; Davani, B.M. Does this patient have Pheochromocytoma? A systematic review of clinical signs and symptoms. J. Diabetes Metab. Disord. 2016, 15, 6. [Google Scholar] [CrossRef]
- Lenders, J.W.M.; Duh, Q.Y.; Eisenhofer, G.; Gimenez-Roqueplo, A.P.; Grebe, S.K.G.; Murad, M.H.; Naruse, M.; Pacak, K.; Young, W.F. Pheochromocytoma and paraganglioma: An endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 2014, 99, 1915–1942. [Google Scholar] [CrossRef] [PubMed]
- Taïeb, D.; Kaliski, A.; Boedeker, C.C.; Martucci, V.; Fojo, T.; Adler, J.R.; Pacak, K. Current approaches and recent developments in the management of head and neck paragangliomas. Endocr. Rev. 2014, 35, 795–819. [Google Scholar] [CrossRef]
- Sherlock, M.; Scarsbrook, A.; Abbas, A.; Fraser, S.; Limumpornpetch, P.; Dineen, R.; Stewart, P.M. Adrenal Incidentaloma. Endocr. Rev. 2020, 41, 775–820. [Google Scholar] [CrossRef]
- Ichijo, T.; Ueshiba, H.; Nawata, H.; Yanase, T. A nationwide survey of adrenal incidentalomas in Japan: The first report of clinical and epidemiological features. Endocr. J. 2020, 67, 141–152. [Google Scholar] [CrossRef]
- Ebbehoj, A.; Li, D.; Kaur, R.J.; Zhang, C.; Singh, S.; Li, T.; Atkinson, E.; Achenbach, S.; Khosla, S.; Arlt, W.; et al. Epidemiology of adrenal tumours in Olmsted County, Minnesota, USA: A population-based cohort study. Lancet Diabetes Endocrinol. 2020, 8, 894–902. [Google Scholar] [CrossRef]
- Mantero, F.; Terzolo, M.; Arnaldi, G.; Osella, G.; Masini, A.M.; Alì, A.; Giovagnetti, M.; Opocher, G.; Angeli, A. A survey on adrenal incidentaloma in Italy. Study Group on Adrenal Tumors of the Italian Society of Endocrinology. J. Clin. Endocrinol. Metab. 2000, 85, 637–644. [Google Scholar] [PubMed]
- Geroula, A.; Deutschbein, T.; Langton, K.; Pamporaki, C.; Peitzsch, M.; Fliedner, S.; Timmers, H.J.L.M.; Bornstein, S.R.; Beuschlein, F.; Stell, A.; et al. Pheochromocytoma and paraganglioma: Clinical feature-based disease probability in relation to catecholamine biochemistry and reason for disease suspicion. Eur. J. Endocrinol. 2019, 181, 409–420. [Google Scholar] [CrossRef] [PubMed]
- Lenders, J.W.M.; Kerstens, M.N.; Amar, L.; Prejbisz, A.; Robledo, M.; Taieb, D.; Pacak, K.; Crona, J.; Zelinka, T.; Mannelli, M.; et al. Genetics, diagnosis, management and future directions of research of phaeochromocytoma and paraganglioma: A position statement and consensus of the Working Group on Endocrine Hypertension of the European Society of Hypertension. J. Hypertens 2020, 38, 1443–1456. [Google Scholar] [CrossRef]
- Stolk, R.F.; Bakx, C.; Mulder, J.; Timmers, H.J.L.M.; Lenders, J.W.M. Is the excess cardiovascular morbidity in pheochromocytoma related to blood pressure or to catecholamines? J. Clin. Endocrinol. Metab. 2013, 98, 1100–1106. [Google Scholar] [CrossRef] [PubMed]
- Naranjo, J.; Dodd, S.; Martin, Y.N. Perioperative Management of Pheochromocytoma. J. Cardiothorac. Vasc. Anesth. 2017, 31, 1427–1439. [Google Scholar] [CrossRef]
- Holscher, I.; Van Den Berg, T.J.; Dreijerink, K.M.A.; Engelsman, A.F.; Nieveen Van Dijkum, E.J.M. Recurrence Rate of Sporadic Pheochromocytomas after Curative Adrenalectomy: A Systematic Review and Meta-analysis. J. Clin. Endocrinol. Metab. 2021, 106, 588–597. [Google Scholar] [CrossRef]
- Granberg, D.; Juhlin, C.C.; Falhammar, H. Metastatic Pheochromocytomas and Abdominal Paragangliomas. J. Clin. Endocrinol. Metab. 2021, 106, E1937–E1952. [Google Scholar] [CrossRef]
- Hamidi, O.; Young, W.F.; Gruber, L.; Smestad, J.; Yan, Q.; Ponce, O.J.; Prokop, L.; Murad, M.H.; Bancos, I. Outcomes of patients with metastatic phaeochromocytoma and paraganglioma: A systematic review and meta-analysis. Clin. Endocrinol. 2017, 87, 440–450. [Google Scholar] [CrossRef]
- Plouin, P.F.; Amar, L.; Dekkers, O.M.; Fassnach, M.; Gimenez-Roqueplo, A.P.; Lenders, J.W.M.; Lussey-Lepoutre, C.; Steichen, O. European Society of Endocrinology Clinical Practice Guideline for long-term follow-up of patients operated on for a phaeochromocytoma or a paraganglioma. Eur. J. Endocrinol. 2016, 174, G1–G10. [Google Scholar] [CrossRef]
- Gruber, L.M.; Strajina, V.; Bancos, I.; Murad, M.H.; Dy, B.M.; Young, W.F.; Farley, D.R.; Lyden, M.L.; Thompson, G.B.; Mckenzie, T.J. Not all adrenal incidentalomas require biochemical testing to exclude pheochromocytoma: Mayo clinic experience and a meta-analysis. Gland. Surg. 2020, 9, 362–371. [Google Scholar] [CrossRef]
- Patel, J.; Davenport, M.S.; Cohan, R.H.; Caoili, E.M. Can established CT attenuation and washout criteria for adrenal adenoma accurately exclude pheochromocytoma? AJR Am. J. Roentgenol. 2013, 201, 122–127. [Google Scholar] [CrossRef]
- Motta-Ramirez, G.A.; Remer, E.M.; Herts, B.R.; Gill, I.S.; Hamrahian, A.H. Comparison of CT findings in symptomatic and incidentally discovered pheochromocytomas. AJR Am. J. Roentgenol. 2005, 185, 684–688. [Google Scholar] [CrossRef] [PubMed]
- Canu, L.; Van Hemert, J.A.W.; Kerstens, M.N.; Hartman, R.P.; Khanna, A.; Kraljevic, I.; Kastelan, D.; Badiu, C.; Ambroziak, U.; Tabarin, A. CT Characteristics of Pheochromocytoma: Relevance for the Evaluation of Adrenal Incidentaloma. J. Clin. Endocrinol. Metab. 2019, 104, 312–318. [Google Scholar] [CrossRef] [PubMed]
- Taïeb, D.; Hicks, R.J.; Hindié, E.; Guillet, B.A.; Avram, A.; Ghedini, P.; Timmers, H.J.; Scott, A.T.; Elojeimy, S.; Rubello, D.; et al. European Association of Nuclear Medicine Practice Guideline/Society of Nuclear Medicine and Molecular Imaging Procedure Standard 2019 for radionuclide imaging of phaeochromocytoma and paraganglioma. Eur. J. Nucl. Med. Mol. Imaging 2019, 46, 2112–2137. [Google Scholar] [CrossRef]
- Muth, A.; Crona, J.; Gimm, O.; Elmgren, A.; Filipsson, K.; Stenmark Askmalm, M.; Sandstedt, J.; Tengvar, M.; Tham, E. Genetic testing and surveillance guidelines in hereditary pheochromocytoma and paraganglioma. J. Intern. Med. 2019, 285, 187–204. [Google Scholar] [CrossRef]
- Ganeshan, D.; Menias, C.O.; Pickhardt, P.J.; Sandrasegaran, K.; Lubner, M.G.; Ramalingam, P.; Bhalla, S. Tumors in von Hippel–Lindau syndrome: From head to toe—Comprehensive state-of-the-art review. Radiographics 2018, 38, 849–866. [Google Scholar] [CrossRef]
- Boyle, J.G.; Davidson, D.F.; Perry, C.G.; Connell, J.M.C. Comparison of Diagnostic Accuracy of Urinary Free Metanephrines, Vanillyl Mandelic Acid, and Catecholamines and Plasma Catecholamines for Diagnosis of Pheochromocytoma. J. Clin. Endocrinol. Metab. 2007, 92, 4602–4608. [Google Scholar] [CrossRef]
- Lenders, J.W.M.; Pacak, K.; Walther, M.M.; Marston Linehan, W.; Mannelli, M.; Friberg, P.; Keiser, H.R.; Goldstein, D.S.; Eisenhofer, G. Biochemical diagnosis of pheochromocytoma: Which test is best? JAMA 2002, 287, 1427–1434. [Google Scholar] [CrossRef]
- Hickman, P.E.; Leong, M.; Chang, J.; Wilson, S.R.; McWhinney, B. Plasma free metanephrines are superior to urine and plasma catecholamines and urine catecholamine metabolites for the investigation of phaeochromocytoma. Pathology 2009, 41, 173–177. [Google Scholar] [CrossRef]
- Garcia-Carbonero, R.; Matute Teresa, F.; Mercader-Cidoncha, E.; Mitjavila-Casanovas, M.; Robledo, M.; Tena, I.; Alvarez-Escola, C.; Arístegui, M.; Bella-Cueto, M.R.; Ferrer-Albiach, C.; et al. Multidisciplinary practice guidelines for the diagnosis, genetic counseling and treatment of pheochromocytomas and paragangliomas. Clin. Transl. Oncol. 2021, 23, 1995–2019. [Google Scholar] [CrossRef]
- Fassnacht, M.; Arlt, W.; Bancos, I.; Dralle, H.; Newell-Price, J.; Sahdev, A.; Tabarin, A.; Terzolo, M.; Tsagarakis, S.; Dekkers, O.M. Management of adrenal incidentalomas: European Society of Endocrinology Clinical Practice Guideline in collaboration with the European Network for the Study of Adrenal Tumors. Eur. J. Endocrinol. 2016, 175, G1–G34. [Google Scholar] [CrossRef] [PubMed]
- Fassnacht, M.; Assie, G.; Baudin, E.; Eisenhofer, G.; de la Fouchardiere, C.; Haak, H.R.; de Krijger, R.; Porpiglia, F.; Terzolo, M.; Berruti, A. Adrenocortical carcinomas and malignant phaeochromocytomas: ESMO-EURACAN Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2020, 31, 1476–1490. [Google Scholar] [CrossRef] [PubMed]
- Eisenhofer, G.; Huynh, T.T.; Hiroi, M.; Pacak, K. Understanding Catecholamine Metabolism as a Guide to the Biochemical Diagnosis of Pheochromocytoma. Rev. Endocr. Metab. Disord. 2001, 2, 297–311. [Google Scholar] [CrossRef]
- Eisenhofer, G.; Prejbisz, A.; Peitzsch, M.; Pamporaki, C.; Masjkur, J.; Rogowski-Lehmann, N.; Langton, K.; Tsourdi, E.; Peczkowska, M.; Fliedner, S.; et al. Biochemical diagnosis of chromaffin cell tumors in patients at high and low risk of disease: Plasma versus urinary free or deconjugated o-methylated catecholamine metabolites. Clin. Chem. 2018, 64, 1646–1656. [Google Scholar] [CrossRef]
- Joyce, C.M.; Melvin, A.; O’Shea, P.M.; Costelloe, S.J.; O’Halloran, D.J. Case report of a phantom pheochromocytoma. Biochem. Med. 2020, 30, 325–330. [Google Scholar] [CrossRef]
- Davidson, F.D. Paracetamol-associated interference in an HPLC-ECD assay for urinary free metadrenalines and catecholamines. Ann. Clin. Biochem. Int. J. Lab. Med. 2004, 41, 316–320. [Google Scholar] [CrossRef]
- Peitzsch, M.; Adaway, J.E.; Eisenhofer, G. Interference from 3-O-Methyldopa with Ultra–High Performance LC-MS/MS Measurements of Plasma Metanephrines: Chromatographic Separation Remains Important. Clin. Chem. 2015, 61, 993–996. [Google Scholar] [CrossRef]
- Emms, H.; Farah, G.; Shine, B.; Boot, C.; Toole, B.; McFadden, M.; Lam, L.; Ou, Z.; Woollard, G.; Madhavaram, H.; et al. Falsely elevated plasma metanephrine in patients taking midodrine. Ann. Clin. Biochem. Int. J. Lab. Med. 2018, 55, 509–515. [Google Scholar] [CrossRef]
- Eisenhofer, G.; Goldstein, D.S.; Walther, M.M.; Friberg, P.; Lenders, J.W.M.; Keiser, H.R.; Pacak, K. Biochemical Diagnosis of Pheochromocytoma: How to Distinguish True- from False-Positive Test Results. J. Clin. Endocrinol. Metab. 2003, 88, 2656–2666. [Google Scholar] [CrossRef]
- Neary, N.M.; King, K.S.; Pacak, K. Drugs and Pheochromocytoma—Don’t Be Fooled by Every Elevated Metanephrine. N. Engl. J. Med. 2011, 364, 2268–2270. [Google Scholar] [CrossRef]
- Lefebvre, H.; Noblet, C.; Moore, N.; Wolf, L.M. Pseudo-phaeochromocytoma after multiple drug interactions involving the selective monoamine oxidase inhibitor selegiline. Clin. Endocrinol. 1995, 42, 95–98. [Google Scholar] [CrossRef] [PubMed]
- Davidson, D.F.; Grosset, K.; Grosset, D. Parkinson’s disease: The effect of L-dopa therapy on urinary free catecholamines and metabolites. Ann. Clin. Biochem. Int. J. Lab. Med. 2007, 44, 364–368. [Google Scholar] [CrossRef] [PubMed]
- Eisenhofer, G.; Brown, S.; Peitzsch, M.; Pelzel, D.; Lattke, P.; Glöckner, S.; Stell, A.; Prejbisz, A.; Fassnacht, M.; Beuschlein, F.; et al. Levodopa therapy in Parkinson’s disease: Influence on liquid chromatographic tandem mass spectrometric-based measurements of plasma and urinary normetanephrine, metanephrine and methoxytyramine. Ann. Clin. Biochem. Int. J. Lab. Med. 2014, 51, 38–46. [Google Scholar] [CrossRef] [PubMed]
- de Jong, W.H.A.; Post, W.J.; Kerstens, M.N.; de Vries, E.G.E.; Kema, I.P. Elevated Urinary Free and Deconjugated Catecholamines after Consumption of a Catecholamine-Rich Diet. J. Clin. Endocrinol. Metab. 2010, 95, 2851–2855. [Google Scholar] [CrossRef] [PubMed][Green Version]
- de Jong, W.H.A.; Eisenhofer, G.; Post, W.J.; Muskiet, F.A.J.; de Vries, E.G.E.; Kema, I.P. Dietary Influences on Plasma and Urinary Metanephrines: Implications for Diagnosis of Catecholamine-Producing Tumors. J. Clin. Endocrinol. Metab. 2009, 94, 2841–2849. [Google Scholar] [CrossRef] [PubMed]
- Därr, R.; Pamporaki, C.; Peitzsch, M.; Miehle, K.; Prejbisz, A.; Peczkowska, M.; Weismann, D.; Beuschlein, F.; Sinnott, R.; Bornstein, S.R.; et al. Biochemical diagnosis of phaeochromocytoma using plasma-free normetanephrine, metanephrine and methoxytyramine: Importance of supine sampling under fasting conditions. Clin. Endocrinol. 2014, 80, 478–486. [Google Scholar] [CrossRef]
- Raber, W.; Raffesberg, W.; Waldhäusl, W.; Gasic, S.; Roden, M. Exercise induces excessive normetanephrine responses in hypertensive diabetic patients. Eur. J. Clin. Investig. 2003, 33, 536–542. [Google Scholar] [CrossRef]
- Zouhal, H.; Jacob, C.; Delamarche, P.; Gratas-Delamarche, A. Catecholamines and the effects of exercise, training and gender. Sports Med. 2008, 38, 401–423. [Google Scholar] [CrossRef]
- Pamporaki, C.; Prejbisz, A.; Małecki, R.; Pistrosch, F.; Peitzsch, M.; Bishoff, S.; Mueller, P.; Meyer, I.; Reimann, D.; Hanus, K.; et al. Optimized Reference Intervals for Plasma Free Metanephrines in Patients With CKD. Am. J. Kidney Dis. 2018, 72, 907–909. [Google Scholar] [CrossRef]
- Pamporaki, C.; Prejbisz, A.; Małecki, R.; Pistrosch, F.; Peitzsch, M.; Bishoff, S.; Mueller, P.; Meyer, I.; Reimann, D.; Hanus, K.; et al. Optimized procedures for testing plasma metanephrines in patients on hemodialysis. Sci. Rep. 2021, 11, 14706. [Google Scholar] [CrossRef]
- Boyd, C.; Wood, K.; Whitaker, D.; Ashorobi, O.; Harvey, L.; Oster, R.; Holmes, R.P.; Assimos, D.G. Accuracy in 24-hour Urine Collection at a Tertiary Center. Rev. Urol. 2018, 20, 119–124. [Google Scholar]
- John, K.A.; Cogswell, M.E.; Campbell, N.R.; Nowson, C.A.; Legetic, B.; Hennis, A.J.M.; Patel, S.M. Accuracy and Usefulness of Select Methods for Assessing Complete Collection of 24-Hour Urine: A Systematic Review. J. Clin. Hypertens 2016, 18, 456–467. [Google Scholar] [CrossRef]
- Kawano, Y.; Kawasaki, T.; Kawazoe, N.; Abe, I.; Uezono, K.; Ueno, M.; Fukiyama, K.; Omae, T. Circadian variations of urinary dopamine, norepinephrine, epinephrine and sodium in normotensive and hypertensive subjects. Nephron 1990, 55, 277–282. [Google Scholar] [CrossRef] [PubMed]
- Peaston, R.T.; Lennard, T.W.; Lai, L.C. Overnight excretion of urinary catecholamines and metabolites in the detection of pheochromocytoma. J. Clin. Endocrinol. Metab. 1996, 81, 1378–1384. [Google Scholar] [PubMed]
- Peitzsch, M.; Kaden, D.; Pamporaki, C.; Langton, K.; Constantinescu, G.; Conrad, C.; Fliedner, S.; Sinnott, R.O.; Prejbisz, A.; Därr, R.; et al. Overnight/first-morning urine free metanephrines and methoxytyramine for diagnosis of pheochromocytoma and paraganglioma: Is this an option? Eur. J. Endocrinol. 2020, 182, 499–509. [Google Scholar] [CrossRef] [PubMed]
- Eugster, P.J.; Centeno, C.; Dunand, M.; Seghezzi, C.; Grouzmann, E. Stabilization of urinary biogenic amines measured in clinical chemistry laboratories. Clin. Chim. Acta 2021, 514, 24–28. [Google Scholar] [CrossRef]
- Willemsen, J.J.; Ross, H.A.; Lenders, J.W.; Sweep, F.C. Stability of Urinary Fractionated Metanephrines and Catecholamines during Collection, Shipment, and Storage of Samples. Clin. Chem. 2007, 53, 268–272. [Google Scholar] [CrossRef]
- Peitzsch, M.; Pelzel, D.; Lattke, P.; Siegert, G.; Eisenhofer, G. Preservation of urine free catecholamines and their free O-methylated metabolites with citric acid as an alternative to hydrochloric acid for LC-MS/MS-based analyses. Clin. Chem. Lab. Med. (CCLM) 2016, 54, 37–43. [Google Scholar] [CrossRef]
- Boot, C.; Toole, B.; Harris, S.; Tetlow, L.; Wassif, W.S. A UK national audit of the laboratory investigation of phaeochromocytoma and paraganglioma. Ann. Clin. Biochem. Int. J. Lab. Med. 2022, 59, 65–75. [Google Scholar] [CrossRef]
- Kline, G.A.; Boyd, J.; Polzin, B.; Harvey, A.; Pasieka, J.L.; Sadrzadeh, H.S.M.; Leung, A.A. Properly Collected Plasma Metanephrines Excludes PPGL after False-Positive Screening Tests. J. Clin. Endocrinol. Metab. 2021, 106, e2900–e2906. [Google Scholar] [CrossRef]
- Lenders, J.W.M.; Willemsen, J.J.; Eisenhofer, G.; Ross, H.A.; Pacak, K.; Timmers, H.J.L.M.; Sweep, C.G.J. Is supine rest necessary before blood sampling for plasma metanephrines? Clin. Chem. 2007, 53, 352–354. [Google Scholar] [CrossRef] [PubMed]
- Chortis, V.; Bancos, I.; Crowley, R.K.; Arlt, W. Supine or sitting plasma metanephrine screening? A unifying solution for patients and doctors. Clin. Endocrinol. 2015, 82, 776–777. [Google Scholar] [CrossRef] [PubMed]
- Chortis, V.; Bancos, I.; Crowley, R.K.; Arlt, W. Supine or sitting? Economic considerations regarding patient position during plasma metanephrine analysis for the exclusion of chromaffin tumours. Clin. Endocrinol. 2015, 82, 462–463. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.; Wang, M.; Cao, Y. Establishment of reference intervals for plasma metanephrines in seated position measured by LC-MS/MS and assessment of diagnostic performance in pheochromocytoma/paraganglioma. Ann. Clin. Biochem. Int. J. Lab. Med. 2023, 60, 160–168. [Google Scholar] [CrossRef]
- Boot, C.; Toole, B.; Johnson, S.J.; Ball, S.; Neely, D. Single-centre study of the diagnostic performance of plasma metanephrines with seated sampling for the diagnosis of phaeochromocytoma/paraganglioma. Ann. Clin. Biochem. 2017, 54, 143–148. [Google Scholar] [CrossRef]
- Danese, E.; Montagnana, M.; Brentegani, C.; Lippi, G. Short-term stability of free metanephrines in plasma and whole blood. Clin. Chem. Lab. Med. 2020, 58, 673–681. [Google Scholar] [CrossRef]
- Willemsen, J.J.; Sweep, C.G.J.; Lenders, J.W.M.; Ross, H.A. Stability of Plasma Free Metanephrines during Collection and Storage as Assessed by an Optimized HPLC Method with Electrochemical Detection. Clin. Chem. 2003, 49, 1951–1953. [Google Scholar] [CrossRef]
- Gupta, R.N.; Price, D.; Keane, P.M. Modified Pisano method for estimating urinary metanephrines. Clin. Chem. 1973, 19, 611–614. [Google Scholar] [CrossRef]
- Plsano, J.J. A simple analysis for normetanephrine and metanephrine in urine. Clin. Chim. Acta 1960, 5, 406–414. [Google Scholar] [CrossRef]
- Iinuma, K.; Ikeda, I.; Ogihara, T.; Hashizume, K.; Kurata, K.; Kumahara, Y. Radioimmunoassay of metanephrine and normetanephrine for diagnosis of pheochromocytoma. Clin. Chem. 1986, 32, 1879–1883. [Google Scholar] [CrossRef]
- Bílek, R.; Zelinka, T.; Vlček, P.; Dušková, J.; Michalský, D.; Novák, K.; Václavíková, E.; Widimský, J. Radioimmunoassay of chromogranin A and free metanephrines in diagnosis of pheochromocytoma. Physiol. Res. 2017, 66, S397–S408. [Google Scholar] [CrossRef] [PubMed]
- Wassell, J.; Reed, P.; Kane, J.; Weinkove, C. Freedom from drug interference in new immunoassays for urinary catecholamines and metanephrines. Clin. Chem. 1999, 45, 2216–2223. [Google Scholar] [CrossRef] [PubMed]
- Weismann, D.; Peitzsch, M.; Raida, A.; Prejbisz, A.; Gosk, M.; Riester, A.; Willenberg, H.S.; Klemm, R.; Manz, G.; Deutschbein, T.; et al. Measurements of plasma metanephrines by immunoassay vs liquid chromatography with tandem mass spectrometry for diagnosis of pheochromocytoma. Eur. J. Endocrinol. 2015, 172, 251–260. [Google Scholar] [CrossRef] [PubMed]
- Shoup, R.E.; Kissinger, P.T. Determination of urinary normetanephrine, metanephrine, and 3 methoxytyramine by liquid chromatography, with amperometric detection. Clin. Chem. 1977, 23, 1268–1274. [Google Scholar] [CrossRef] [PubMed]
- Jouve, J.; Mariotte, N.; Sureau, C.; Muh, J.P. High-performance liquid chromatography with electrochemical detection for the simultaneous determination of the methoxylated amines, normetanephrine, metanephrine and 3-methoxytyramine, in urine. J. Chromatogr. B Biomed. Sci. Appl. 1983, 274, 53–62. [Google Scholar] [CrossRef]
- Bertani-Dziedzic, L.M.; Krstulovic, A.M.; Dziedzic, S.W.; Gitlow, S.E.; Cerqueira, S. Analysis of urinary metanephrines by reversed-phase high-performance liquid chromatography and electrochemical detection. Clin. Chim. Acta 1981, 110, 1–8. [Google Scholar] [CrossRef]
- Eisenhofer, G.; Peitzsch, M. Laboratory evaluation of pheochromocytoma and paraganglioma. Clin. Chem. 2014, 60, 1486–1499. [Google Scholar]
- Pagliari, R.; Cottet-Emard, J.M.; Peyrin, L. Determination of free and conjugated normetanephrine and metanephrine in human plasma by high-performance liquid chromatography with electrochemical detection. J. Chromatogr. B Biomed. Sci. Appl. 1991, 563, 23–36. [Google Scholar] [CrossRef]
- Lenders, J.W.M.; Eisenhofer, G.; Armando, I.; Keiser, H.R.; Goldstein, D.S.; Kopin, I.J. Determination of metanephrines in plasma by liquid chromatography with electrochemical detection. Clin. Chem. 1993, 39, 97–103. [Google Scholar] [CrossRef]
- Bouhanick, B.; Fauvel, J.; Pont, F. Biochemical misdiagnosis of pheochromocytoma in patients treated with sulfasalazine. JAMA 2010, 304, 1898–1901. [Google Scholar] [CrossRef]
- Feldman, J.M. Falsely Elevated Urinary Excretion of Catecholamines and Metanephrines in Patients Receiving Labetalol Therapy. J. Clin. Pharmacol. 1987, 27, 288–292. [Google Scholar] [PubMed]
- Barco, S.; Alpigiani, M.G.; Ghiggeri, G.M.; Talio, M.; Maffia, A.; Tripodi, G.; Cangemi, G. Amoxicillin-associated interference in an HPLC-EC assay for urinary fractionated metanephrines: Potential pitfall in pheochromocytoma biochemical diagnosis. Clin. Biochem. 2014, 47, 119–121. [Google Scholar] [PubMed]
- Van Laarhoven, H.W.M.; Willemsen, J.J.; Alec Ross, H.; Beex, L.V.A.M.; Lenders, J.W.M.; Sweep, F.C.G.J. Pitfall in HPLC assay for urinary metanephrines: An unusual type of interference caused by methenamine intake. Clin. Chem. 2004, 50, 1097–1099. [Google Scholar]
- Cook, F.J.; Chandler, D.W.; Snyder, D.K. Effect of Buspirone on Urinary Catecholamine Assays. N. Engl. J. Med. 1995, 332, 401. [Google Scholar] [PubMed]
- Madhavaram, H.; Woollard, G.A. Interference from Indian diet on the internal standard in a commercial method for the measurement of urinary metanephrines by high-performance liquid chromatography with electrochemical detection. Ann. Clin. Biochem. Int. J. Lab. Med. 2014, 51, 400–405. [Google Scholar]
- Dunand, M.; Donzelli, M.; Rickli, A.; Hysek, C.M.; Liechti, M.E.; Grouzmann, E. Analytical interference of 4-hydroxy-3-methoxymethamphetamine with the measurement of plasma free normetanephrine by ultra-high pressure liquid chromatography-tandem mass spectrometry. Clin. Biochem. 2014, 47, 1100–1103. [Google Scholar]
- Peitzsch, M.; Novos, T.; Kadenm, D.; Kurlbaum, M.; van Herwaarden, A.E.; Müller, D.; Adaway, J.; Grouzmann, E.; McWhinney, B.; Hoad, K.; et al. Harmonization of LC-MS/MS Measurements of Plasma Free Normetanephrine, Metanephrine, and 3-Methoxytyramine. Clin. Chem. 2021, 67, 1098–1112. [Google Scholar]
- Eisenhofer, G.; Peitzsch, M.; Kaden, D.; Langton, K.; Mangelis, A.; Pamporaki, C.; Masjkur, J.; Geroula, A.; Kurlbaum, M.; Deutschbein, T.; et al. Reference intervals for LC-MS/MS measurements of plasma free, urinary free and urinary acid-hydrolyzed deconjugated normetanephrine, metanephrine and methoxytyramine. Clin. Chim. Acta 2019, 490, 46–54. [Google Scholar]
- Kairisto, V.; Koskinen, P.; Mattila, K.; Puikkonen, J.; Virtanen, A.; Kantola, I.; Irjala, K. Reference intervals for 24-h urinary normetanephrine, metanephrine, and 3-methoxy-4-hydroxymandelic acid in hypertensive patients. Clin. Chem. 1992, 38, 416–420. [Google Scholar]
- Griffin, A.; O’Shea, P.; FitzGerald, R.; O’Connor, G.; Tormey, W. Establishment of a paediatric age-related reference interval for the measurement of urinary total fractionated metanephrines. Ann. Clin. Biochem. Int. J. Lab. Med. 2011, 48, 41–44. [Google Scholar]
- Eisenhofer, G.; Lattke, P.; Herberg, M.; Siegert, G.; Qin, N.; Därr, R.; Hoyer, J.; Villringer, A.; Prejbisz, A.; Januszewicz, A.; et al. Reference intervals for plasma free metanephrines with an age adjustment for normetanephrine for optimized laboratory testing of phaeochromocytoma. Ann. Clin. Biochem. Int. J. Lab. Med. 2012, 50, 62–69. [Google Scholar] [CrossRef] [PubMed]
- Kannan, S.; Purysko, A.; Faiman, C.; Remer, E.M.; Shah, L.; Bena, J.; Siperstein, A.; Berber, E.; Fergany, A.; Bravo, E.; et al. Biochemical and radiological relationships in patients with pheochromocytoma: Lessons from a case control study. Clin. Endocrinol. 2014, 80, 790–796. [Google Scholar]
- Tsiomidou, S.; Pamporaki, C.; Geroula, A.; Van Baal, L.; Weber, F.; Dralle, H.; Schmid, K.W.; Führer, D.; Unger, N. Clonidine suppression test for a reliable diagnosis of pheochromocytoma: When to use. Clin. Endocrinol. 2022, 97, 541–550. [Google Scholar] [CrossRef] [PubMed]
- Bílek, R.; Vlček, P.; Šafařík, L.; Michalský, D.; Novák, K.; Dušková, J.; Václavíková, E.; Widimský, J.; Zelinka, T. Chromogranin A in the Laboratory Diagnosis of Pheochromocytoma and Paraganglioma. Cancers 2019, 11, 586. [Google Scholar] [CrossRef]
- Grossrubatscher, E.; Dalino, P.; Vignati, F.; Gambacorta, M.; Pugliese, R.; Boniardi, M.; Rossetti, O.; Marocchi, A.; Bertuzzi, M.; Loli, P. The role of chromogranin A in the management of patients with phaeochromocytoma. Clin. Endocrinol. 2006, 65, 287–293. [Google Scholar] [CrossRef]
- Algeciras-Schimnich, A.; Preissner, C.M.; Young, W.F.; Singh, R.J.; Grebe, S.K.G. Plasma Chromogranin A or Urine Fractionated Metanephrines Follow-Up Testing Improves the Diagnostic Accuracy of Plasma Fractionated Metanephrines for Pheochromocytoma. J. Clin. Endocrinol. Metab. 2008, 93, 91–95. [Google Scholar] [CrossRef]
- Popovici, T.; Moreira, B.; Schlageter, M.H.; Bories, P.N. Automated two-site immunofluorescent assay for the measurement of serum chromogranin A. Clin. Biochem. 2014, 47, 87–91. [Google Scholar]
- Bech, P.R.; Ramachandran, R.; Dhillo, W.; Martin, N.M.; Bloom, S.R. Quantifying the Effects of Renal Impairment on Plasma Concentrations of the Neuroendocrine Neoplasia Biomarkers Chromogranin A, Chromogranin B, and Cocaine- and Amphetamine-Regulated Transcript. Clin. Chem. 2012, 58, 941–943. [Google Scholar]

| Pharmacolgical Effects | ||
|---|---|---|
| Medications | Mechanism of Effects on Catecholamines/Metanephrines | Potential Impact on Results |
| Tricyclic antidepressants Venlafaxine | Inhibition of neuronal uptake of norepinephrine | Increased norepinephrine/normetanephrine |
| Phenoxybenzamine | Antagonism of α-adrenoceptors | Increased norepinephrine/normetanephrine |
| Selective α-adrenoceptor blockers (e.g., doxazosin) | Antagonism of α-adrenoceptors | May increase norepinephrine, but minimal effects on urine/plasma metanephrines |
| Monoamine oxidase inhibitors | Impaired metabolism of O-methylated catecholamine metabolites | Increased urine/plasma metanephrines |
| Atypical antipsychotics (e.g., quetiapine, clozapine, risperidone) | Increased secretion of norepinephrine | Increased norepinephrine/normetanephrine |
| Stimulants (e.g., nicotine, caffeine) | Increased secretion of epinephrine/norepinephrine | Increased epinephrine/metanephrine and/or norepinephrine/normetanephrine |
| Sympathomimetics (e.g., amphetamine, ephedrine) | Release of vesicular monoamines, activation of adrenoreceptors | Increased catecholamines/metanephrines |
| Analytical Interference | ||
| Medications | Methodology Potentially Affected | Potential Impact on Results * |
| Paracetamol | HPLC-ECD | Increased normetanephrine/metanephrine |
| Sulfasalazine | HPLC-ECD | Increased normetanephrine/metanephrine |
| Labetalol | HPLC-ECD | Increased normetanephrine/metanephrine |
| Amoxicillin | HPLC-ECD | Increased normetanephrine/metanephrine |
| Curry leaves | HPLC-ECD (over-recovery of internal standard) | Decreased metanephrines |
| Midodrine (desglymidodrine) | LC-MS/MS | Increased metanephrine and 3-methoxytyramine |
| 3-O-methydopa | LC-MS/MS | Increased 3-methoxytyramine |
| Pre-Analytical Considerations | ||
|---|---|---|
| Plasma Metanephrines | Urine Metanephrines | |
| Diet | Dietary catecholamines have minimal effect on NMN and MN but may cause elevations in 3MT. Fasted sampling recommended. | Dietary catecholamines are more likely to affect measurement of total urine metanephrines. Exclusion of catecholamine-rich foods during sample colleciton recommended. |
| Medications | A range of medications can cause change in metanephrines concentrations through their pharmacological action. The potential for analytical interference is method dependent (e.g., LC-ECD vs. LC-MS/MS). | A range of medications can cause change in metanephrines concentrations through their pharmacological action. The potential for analytical interference is method dependent (e.g., LC-ECD vs. LC-MS/MS). |
| Physical activity/stress | Intense physical activity and physical/psychological stress can increase plasma metanephrines. This should be minimised where possible prior to phlebotomy. | Intense physical activity and physical/psychological stress can increase urine metanephrines. This should be minimised where possible throughout the period of urine collection. |
| Patient Posture | Supine sampling is preferred as this improves diagnostic performance compared to seated sampling. | N/A |
| Accuracy of sample collection | N/A | A significant proportion of 24 h urine collections may suffer from inaccurate timing. |
| Sample stability | Blood samples must be centrifuged ASAP following sample collection. Plasma should be stored and transported frozen if analysis does not take place on the day of collection. | Urine samples are stable for several days at room temperature. Acidification improves sample stability. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Boot, C.S. A Laboratory Medicine Perspective on the Investigation of Phaeochromocytoma and Paraganglioma. Diagnostics 2023, 13, 2940. https://doi.org/10.3390/diagnostics13182940
Boot CS. A Laboratory Medicine Perspective on the Investigation of Phaeochromocytoma and Paraganglioma. Diagnostics. 2023; 13(18):2940. https://doi.org/10.3390/diagnostics13182940
Chicago/Turabian StyleBoot, Christopher S. 2023. "A Laboratory Medicine Perspective on the Investigation of Phaeochromocytoma and Paraganglioma" Diagnostics 13, no. 18: 2940. https://doi.org/10.3390/diagnostics13182940
APA StyleBoot, C. S. (2023). A Laboratory Medicine Perspective on the Investigation of Phaeochromocytoma and Paraganglioma. Diagnostics, 13(18), 2940. https://doi.org/10.3390/diagnostics13182940





