Abstract
A 63-year-old man with a history of right plantar malignant melanoma (T3bN0M0, IIb) developed multiple metastases in bilateral lungs 19 months after surgery. Subsequent 18F-FDG PET/CT revealed multiple pulmonary metastases with intense FDG uptake and detected a hypermetabolic lesion in the lateral wall of the left ventricle, which was considered to be a cardiac metastasis of malignant melanoma. This lesion was later confirmed in the dynamic myocardial perfusion MR. This case demonstrates the effectiveness of 18F-FDG PET/CT in detecting occult cardiac metastases of malignant melanoma.
Cardiac metastases are rare, occurring in 4.71% of adult patients with solid cancers, and lung cancer accounted for most primary tumors. In terms of locations, the pericardium was the most frequent site of cardiac metastases, followed by myocardial metastases [1]. Cardiac involvement of malignant melanoma was reported to occur in less than 2% of patients. As most patients are asymptomatic, cardiac metastasis from melanoma is usually found in autopsy [2,3] or detected opportunistically [4,5], and it was associated with poor prognosis compared to those without cardiac metastases [6,7]. The sensitivity of routine cardiac examinations for cardiac metastasis is limited [8]. 18F-FDG PET/CT is a useful tool to assess distant metastases of melanoma, including detecting occult cardiac metastases [9]. However, myocardium usually presents variable physiological 18F-FDG uptake [10], and cardiac lesions may often be overlooked. Therefore, reducing the physiological 18F-FDG uptake in the myocardium is necessary for this situation. Several methods for inhibiting physiological myocardial 18F-FDG uptake have been proposed, including long fasting (longer than 18 h) [11], a low-carbohydrate diet [12] or prolonged high-fat, high-protein, and very-low-carbohydrate diet [13]. These procedures may lead to an increase in circulating free fatty acid (FFA) levels as well as a decrease in blood insulin. However, there is no definite conclusion as to which procedure is optimal, and the choice needs to be made based on clinical practice. Nuclear medicine physicians should keep this in mind when reading images with abnormal cardiac uptake and be aware of the procedures to suppress the background uptake of the myocardium.
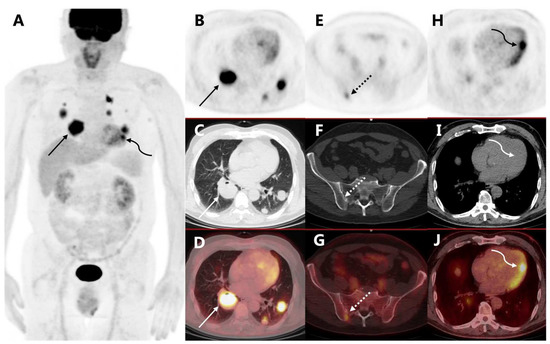
Figure 1.
A 61-year-old man was recently diagnosed with cutaneous melanoma in the right planta (Breslow thickness 2 mm). The patient had no family history of malignancy. Preoperative 18F-FDG PET/CT did not show any nodal or distant metastasis. He then underwent enlarged excision of the tumor and sentinel lymph-node biopsy, and his tumor was staged T3bN0M0 (IIb). He did not receive adjuvant treatment and was closely followed postoperatively. Nineteen months after surgery, he presented with blood-stained sputum and CT revealed multiple masses and nodules in bilateral lungs, which were confirmed to be pulmonary metastases from malignant melanoma after biopsy. The immunohistochemical results were AE1/AE3 (−), HMB45 (+), Melan-A (+), Ki-67 (index 50%), TTF-1 (−), S-100 (+). The follow-up 18F-FDG PET/CT ((A) PET MIP, (B) axial PET, (C) coregistered CT, (D) fusion image) showed multiple hypermetabolic masses in bilateral lungs (arrows, SUVmax 10.6), consistent with pulmonary metastases. Bone metastasis in the right ilium was also detected ((E)–(G), dotted arrows, SUVmax 3.1). His left ventricular myocardium exhibited diffuse uptake, which was physiological (Figure 1). Notably, a nodular hypermetabolic lesion was found in the lateral wall of the left ventricle ((H)–(J), curved arrows, SUVmax 7.1), which was abnormal, possibly a cardiac metastasis from melanoma.
Figure 1.
A 61-year-old man was recently diagnosed with cutaneous melanoma in the right planta (Breslow thickness 2 mm). The patient had no family history of malignancy. Preoperative 18F-FDG PET/CT did not show any nodal or distant metastasis. He then underwent enlarged excision of the tumor and sentinel lymph-node biopsy, and his tumor was staged T3bN0M0 (IIb). He did not receive adjuvant treatment and was closely followed postoperatively. Nineteen months after surgery, he presented with blood-stained sputum and CT revealed multiple masses and nodules in bilateral lungs, which were confirmed to be pulmonary metastases from malignant melanoma after biopsy. The immunohistochemical results were AE1/AE3 (−), HMB45 (+), Melan-A (+), Ki-67 (index 50%), TTF-1 (−), S-100 (+). The follow-up 18F-FDG PET/CT ((A) PET MIP, (B) axial PET, (C) coregistered CT, (D) fusion image) showed multiple hypermetabolic masses in bilateral lungs (arrows, SUVmax 10.6), consistent with pulmonary metastases. Bone metastasis in the right ilium was also detected ((E)–(G), dotted arrows, SUVmax 3.1). His left ventricular myocardium exhibited diffuse uptake, which was physiological (Figure 1). Notably, a nodular hypermetabolic lesion was found in the lateral wall of the left ventricle ((H)–(J), curved arrows, SUVmax 7.1), which was abnormal, possibly a cardiac metastasis from melanoma.
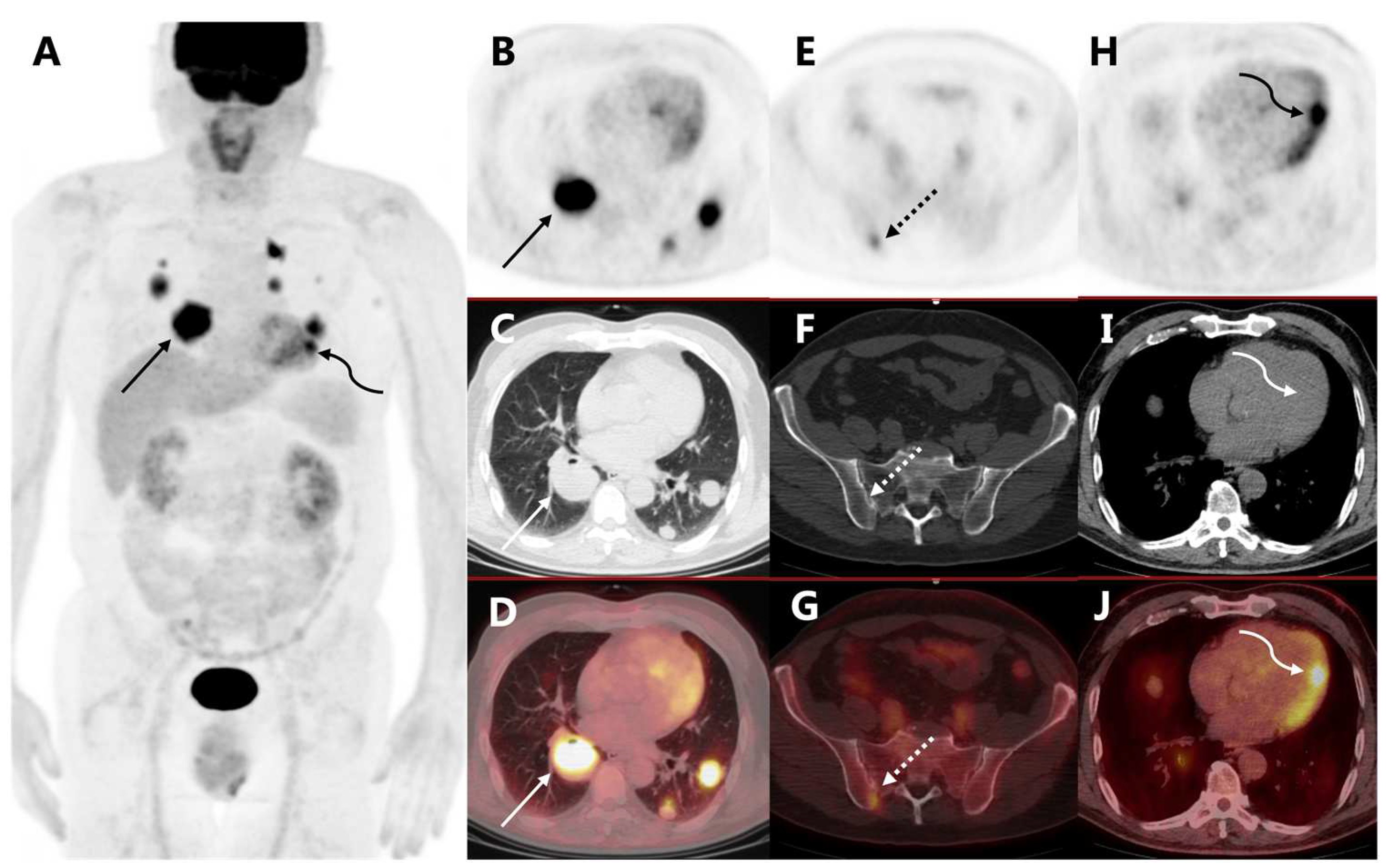
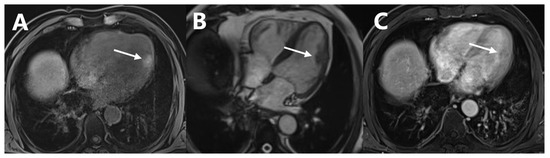
Figure 2.
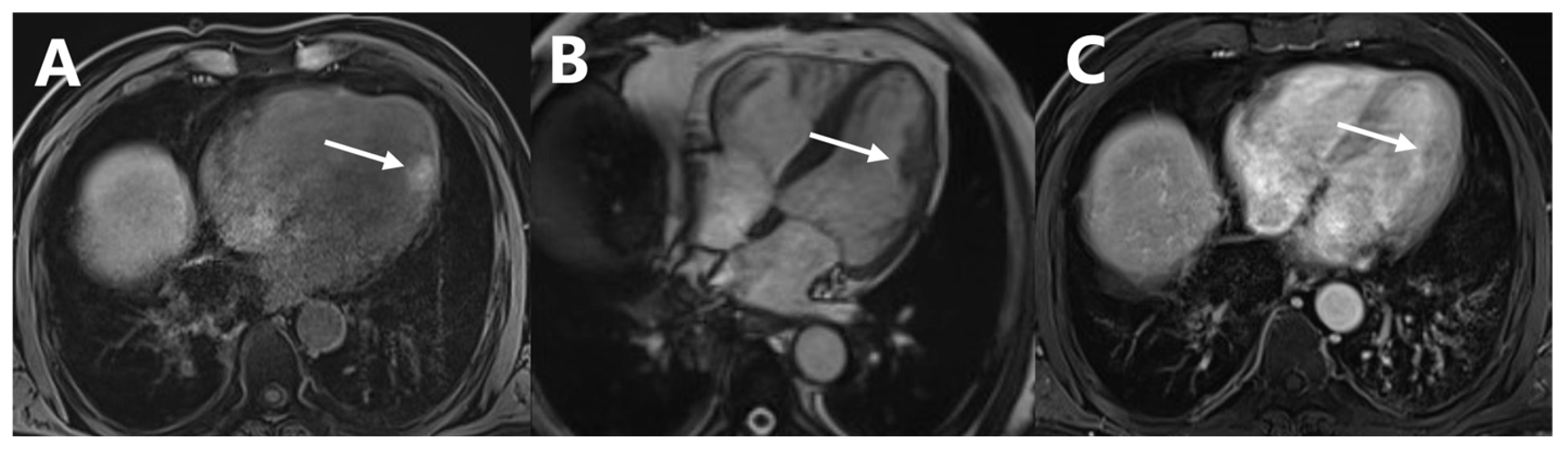
Dynamic myocardial perfusion MRI ((A) T1WI, (B) T2WI, (C) delayed scan of enhanced T1WI) also detected the lesion in the left ventricular lateral wall with a short T1 signal and a long T2 signal intensity with delayed enhancement (Figure 2, arrows). Subsequent gene testing revealed an insertion mutation in exon 11 of the KIT gene and no BRAF mutations were detected. Considering the advanced stage of malignant melanoma, he was treated with imatinib and received radiotherapy of the largest mass in the right lung. However, the treatment of imatinib was discontinued 6 weeks later because of a drug reaction with eosinophilia and systemic symptoms (DRESS). The patient experienced rapid progression of the tumor 4 months thereafter and died of the disease.
Figure 2.
Dynamic myocardial perfusion MRI ((A) T1WI, (B) T2WI, (C) delayed scan of enhanced T1WI) also detected the lesion in the left ventricular lateral wall with a short T1 signal and a long T2 signal intensity with delayed enhancement (Figure 2, arrows). Subsequent gene testing revealed an insertion mutation in exon 11 of the KIT gene and no BRAF mutations were detected. Considering the advanced stage of malignant melanoma, he was treated with imatinib and received radiotherapy of the largest mass in the right lung. However, the treatment of imatinib was discontinued 6 weeks later because of a drug reaction with eosinophilia and systemic symptoms (DRESS). The patient experienced rapid progression of the tumor 4 months thereafter and died of the disease.
Author Contributions
Conceptualization Y.L.; investigation, H.Z. and Y.L.; writing—original draft preparation, H.Z. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the National High-Level Hospital Clinical Research Funding (2022-PUMCH-A-046, 2022-PUMCH-B-070).
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board of Peking Union Medical College Hospital (zs-1810).
Informed Consent Statement
Written informed consent was obtained from the patient to publish this paper.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Nova-Camacho, L.M.; Gomez-Dorronsoro, M.; Guarch, R.; Cordoba, A.; Cevallos, M.I.; Panizo-Santos, A. Cardiac Metastasis from Solid Cancers: A 35-Year Single-Center Autopsy Study. Arch. Pathol. Lab. Med. 2022, 147, 177–184. [Google Scholar] [CrossRef] [PubMed]
- Tas, F.; Mudun, A.; Kırma, C. Cardiac involvement in melanoma: A case report and review of the literature. J. Cancer Res. Ther. 2010, 6, 359–361. [Google Scholar] [CrossRef] [PubMed]
- Bussani, R.; De-Giorgio, F.; Abbate, A.; Silvestri, F.J.D.I. Cardiac metastases. J Clin Pathol. 2007, 60, 27–34. [Google Scholar] [CrossRef] [PubMed]
- Butany, J.; Nair, V.; Naseemuddin, A.; Nair, G.M.; Catton, C.; Yau, T. Cardiac tumours: Diagnosis and management. Lancet Oncol. 2005, 6, 219–228. [Google Scholar] [CrossRef] [PubMed]
- Wood, A.; Markovic, S.N.; Best, P.J.; Erickson, L.A. Metastatic malignant melanoma manifesting as an intracardiac mass. Cardiovasc. Pathol. 2010, 19, 153–157. [Google Scholar] [CrossRef] [PubMed]
- Noël, A.; Toquet, C.; Dewilde, J. Prolonged survival after surgery for cardiac metastasis from malignant melanoma. J. Cardiol. Cases 2014, 10, 150–152. [Google Scholar] [CrossRef] [PubMed]
- Balinski, A.M.; Vasbinder, A.L.; Kerndt, C.C.; Catalan, T.C.; Parry, N.P.; Rehman, R.A.; Blakely, P.; Yeow, R.Y.; Leja, M.J.; Lao, C.D.; et al. Metastatic melanoma of the heart: Retrospective cohort study and systematic review of prevalence, clinical characteristics, and outcomes. Cancer Med. 2023, 12, 2356–2367. [Google Scholar] [CrossRef] [PubMed]
- Ramchand, J.; Wong, G.R.; Yudi, M.B.; Sylivris, S. Cardiac metastatic melanoma. BMJ Case Rep. 2016, 2016, bcr2016215881. [Google Scholar] [CrossRef] [PubMed]
- Allen, B.C.; Mohammed, T.L.; Tan, C.D.; Miller, D.V.; Williamson, E.E.; Kirsch, J.S. Metastatic Melanoma to the Heart. Curr. Probl. Diagn. Radiol. 2012, 41, 159–164. [Google Scholar] [CrossRef] [PubMed]
- Lobert, P.; Brown, R.; Dvorak, R.; Corbett, J.; Kazerooni, E.; Wong, K. Spectrum of physiological and pathological cardiac and pericardial uptake of FDG in oncology PET-CT. Clin. Radiol. 2013, 68, e59–e71. [Google Scholar] [CrossRef] [PubMed]
- Morooka, M.; Moroi, M.; Uno, K.; Ito, K.; Wu, J.; Nakagawa, T.; Kubota, K.; Minamimoto, R.; Miyata, Y.; Okasaki, M.; et al. Long fasting is effective in inhibiting physiological myocardial 18F-FDG uptake and for evaluating active lesions of cardiac sarcoidosis. EJNMMI Res. 2014, 4, 1. [Google Scholar] [CrossRef] [PubMed]
- Coulden, R.; Chung, P.; Sonnex, E.; Ibrahim, Q.; Maguire, C.; Abele, J. Suppression of myocardial 18F-FDG uptake with a preparatory “Atkins-style” low-carbohydrate diet. Eur. Radiol. 2012, 22, 2221–2228. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Grant, C.; Xie, K.; Sweiss, N.J. Suppression of Myocardial 18F-FDG Uptake Through Prolonged High-Fat, High-Protein, and Very-Low-Carbohydrate Diet Before FDG-PET/CT for Evaluation of Patients with Suspected Cardiac Sarcoidosis. Clin. Nucl. Med. 2017, 42, 88–94. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
