Abstract
Background: The impact of muscle-training treatment on quality of life and functional outcomes in people with pelvic floor dysfunction may be related to adherence rates. Methods: Nine electronic databases were searched for studies published up to 15 October 2024. A qualitative synthesis was used to describe the relationship between adherence or compliance with treatment, quality of life, and symptomatic severity. A meta-analysis of data from selected studies was performed that assessed quality of life and symptomatic severity in the short term. Results: Seven studies with 2190 participants were included. Of these studies, 42% showed rates greater than 80% in terms of adherence. A beneficial effect was found in terms of urinary incontinence severity without statistical differences between the groups (p = 0.813), while quality of life showed statistically significant improvements favoring the experimental group (p = 0.036). The quality of the evidence was collected or measured from low to high. Conclusions: People with pelvic floor disorders show high rates of adherence to pelvic floor muscle exercise and experience an improved quality of life in the short term, but more research is needed on the design of homogeneous systems to measure compliance and adherence to exercise-based treatments.
1. Introduction
The pelvic floor, composed of muscular tissue, fibromuscular, and fascial elements, extends from the pubis to the coccyx and contains several layers. The middle layer of the pelvic floor is made up predominantly of muscle tissue, which, through contraction and relaxation, supports the pelvic organs [1]. It plays an important role in urinary and fecal continence and sexual and reproductive function and is essential for good health and well-being [2,3]. However, its normal function can be altered by increasing or decreasing muscle tone, pain due to impaired muscle coordination, or involvement of the pudendal nerve [4]. In women, the disorders of pelvic floor muscle are related to pregnancy and childbirth [5] or menopause [6]. The general prevalence is 46%, but the most common condition is urinary incontinence (hereafter UI), affecting 30–60% of individuals [7]. In men, diagnoses are classified [8] as storage disorders, voiding dysfunction, and mixed storage and voiding dysfunction, reflecting lower urinary tract function and related to sexual health impairment [9]. The risk factors for UI in men include older age, lower urinary tract symptoms, infections, functional and cognitive impairment, neurological disorders, and prostatectomy [10]. People with pelvic floor disorders develop a disability (a symptom of pelvic floor dysfunction) that has a negative impact on their activity or participation (quality of life) [11,12,13]. Sexual health affects not only people with pelvic floor dysfunctions in their lives but also that of their partners [14,15].
The therapeutic approach to pelvic floor disorders is commonly multidisciplinary. Pelvic floor muscle training (hereafter PFMT) is a therapy to improve endurance, strength, power, relaxation, or a combination of these, and because of its effectiveness is considered the first line of treatment for stress UI in women [2,6,16,17], and in men [18]. Thus, PFMT, by improving muscle function, has been reported to ameliorate patient disability, activity, and participation [12], which leads to improved psychosocial outcomes [19,20]. Exercise, in general and PFMT in particular, seems to be positive in sexual function in males after prostate cancer, but further research would be necessary to determine appropriate exercise interventions [21].
In both male and female populations, the effectiveness of treatments based on exercise depends on several factors, including maintenance of the routine over time, for which the concept of compliance and adherence to treatment is fundamental [22,23].
The National Library of Medicine [24] defines compliance and adherence to treatment as “The extent to which the patient follows the prescribed treatment, such as keeping appointments and schedules and adherence to medication for the desired therapeutic outcome”. Numerous research studies have shown the importance of adherence [25,26] and compliance [27,28] to treatment in general and to exercise [29] in particular [30,31,32,33]. We also know the complexity derived from the high number and heterogeneity of the barriers and facilitators of adherence to treatment and its multidimensional condition [34,35,36]. The most suitable objective and homogeneous measurement instrument for this concept is the questionnaire [33,37]. The scientific community agrees on two important aspects of adherence: that it tends to decrease over time, especially in the long term [38], and that it is considered to be high when it is above 80% [29,39,40,41,42].
It seems that the importance of adherence and compliance lies in the relationship with the results obtained after applying a given treatment. A high adherence rate is assumed to indicate that the outcome of the intervention derives from it. For this reason, there are studies that only collect data from those patients who have completed treatment as indicated.
Nagpal et al. [29] offered a possible way to analyze the relationship between adherence to exercise-based treatments and therapeutic effectiveness, showing us four possible scenarios: no significant effect of the intervention or improvement is observed compared with the inactive control group related to low (Scenario 1) or high (Scenario 2) adherence; intervention favors the experimental group over the control group related to low (Scenario 3) or high (Scenario 4) adherence. These scenarios give us the opportunity to interpret the results of clinical trials in a very interesting way.
Therefore, the objective of this systematic review was to analyze the effectiveness of exercise-based treatments on quality of life and severity of pelvic floor dysfunction and the relationship between compliance or adherence to exercise-based treatments and therapeutic effectiveness.
2. Materials and Methods
This systematic review was registered (14 October 2024) in PROSPERO (CRD42022349487) and was conducted according to the PRISMA [43] guidelines, and no modifications were made to the initial protocol during this study.
2.1. Data Sources and Searches
A systematic search was conducted independently by two researchers in PubMed, CINAHL, Medes, Web of Science, EMBASE, Scopus, PEDro, The Cochrane Library, and TRIP databases to identify all studies published related to the topic up to 15 October 2024. To minimize publication bias, a search was conducted in the gray literature and clinical trial registry databases. The search strategy detailed in Table A1 was applied, along with specific strategies tailored to each database (Table A2). The search was limited to randomized clinical trials published in Spanish and English without restrictions on the time of publication.
2.2. Study Selection
This process, according to the eligibility criteria, was carried out independently by three researchers as follows: the titles and abstracts were screened; from the studies that met the eligibility criteria, the full texts were recovered and screened. Those studies in which the eligibility criterion “Studies that measure, in addition to effectiveness in terms of symptom improvement, adherence to treatment collected through specific scales or questionnaires” did not appear clearly collected in the abstract were selected full texts to avoid potential losses. The study selection process is described in detail in Table A3.
For collection, filtering, removal of duplicates, and citation and reference management, Zotero v. 6.0.36 software was used.
Eligibility Criteria
Randomized clinical trials (RCT) were selected for inclusion in this study. Participants included patients of both sexes diagnosed with pelvic floor disorders of non-neurological origin. The intervention reviewed was physiotherapy treatment focused on PFMT. As comparators, studies that evaluated other interventions, such as medication or surgery, as well as those in which participants did not receive physiotherapy treatment for pelvic floor dysfunction, were included. Finally, only studies that assessed both symptom improvement and adherence to treatment using specific scales or questionnaires were considered.
2.3. Outcome Measures
2.3.1. Main Outcome
Compliance and adherence to exercise-based physiotherapy for pelvic floor disorders in the short and medium term, collected through specific questionnaires or scales, measured in terms of days of exercise practice, number of exercises performed, or frequency of attendance to physiotherapy sessions.
2.3.2. Secondary Outcomes
Quality of life is a generic concept reflecting concern for the modification and improvement of attributes of life, physical, political, moral, and social environment, as well as health and illness, measured through valid and reliable questionnaires or scales. The severity of pelvic floor dysfunction as levels within a diagnostic group that are established by various measurement criteria applied to the seriousness of a patient’s disorder (urine or fecal loss, leakage episodes, and erectile dysfunction), measured through specific test or questionnaires (pad test and a bladder diary).
2.4. Data Extraction and Quality Assessment
Data extraction was carried out independently by two researchers using the full texts of the selected studies. Data related to a study’s participants, intervention, and results according to the main and secondary variables were extracted and collected in tables for analysis. Author/year and country from studies. Information regarding participants (pelvic floor disorder, sample size, and sex). Intervention and outcome variables (exercise protocol, control group intervention, strategy to improve adherence to treatment, outcome measures and measurement instruments, participants who complete the intervention period, and losses in the follow-up).
Methodological quality was assessed using the PEDro Scale [44] by two independent reviewers with the intervention of a third in the event of discrepancies. The PEDro scale allows the identification of randomized clinical trials for external validity (item 1) and internal validity (items 2–9) and which may have sufficient statistical information to make their results interpretable (items 10–11). The scale is measured out of 10 since criterion 1 is not used for the calculation of the score [45].
2.5. Effects Measures
Compliance and adherence: Frequency in terms of attending physiotherapy sessions, days of exercise practice, number of exercises performed, and their means. Quality of life: questionnaire scores in terms of frequency (mean differences). Severity (of pelvic floor dysfunction): frequency (mean differences), relative risks.
2.6. Data Synthesis and Analysis
Data were analyzed using a qualitative synthesis and, whenever possible, a quantitative synthesis (meta-analysis). Standardized mean differences (SMD), estimated effect, and standard error, with 95% confidence intervals (CI) were calculated. Fixed or random effects models were used according to the degree of heterogeneity, using the I2 coefficient. Specifically, for I2 > 50% and p < 0.05, which indicates substantial heterogeneity, random effects models were used, and when I2 < 50% and p > 0.05, which indicates substantial homogeneity, fixed effect models were used. The Jamovi version 2.3.28 software was used to summarize the effects and build the forest plots. Egger’s regression test was used to estimate publication bias.
The approach proposed by the Grading of Recommendations Assessment, Development, and Evaluations (GRADE) [46], which allowed to classify the evidence as high, moderate, low, or very low and to discern the importance of the results, was used.
3. Results
3.1. Flow of Trials Through the Review
A total of 1431 articles were identified. Following the recommendations of PRISMA [43], after eliminating duplicates and those that did not meet the eligibility criteria after reading the title and abstract, the full texts of 559 studies were selected (see Table A3). Finally, seven studies were included in the selection, as shown in Figure 1.
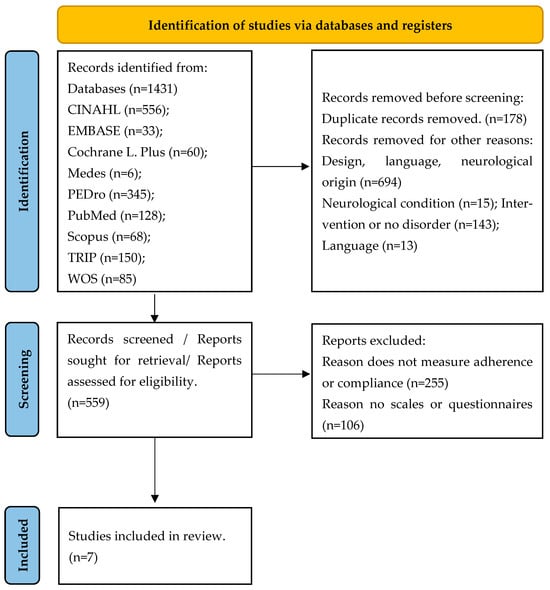
Figure 1.
PRISMA 2020 flow diagram.
3.2. Characteristics of the Included Studies
The main characteristics of the included studies [47,48,49,50,51,52,53] are shown in detail in Table 1. The included studies reported data for 2190 participants. Six trials reported data from 1337 women (61%) [48,49,50,51,52,53] and one from 853 men (39%) [47]. The study conducted in men addressed UI related to radical prostatectomy (hereafter RP) or transurethral prostate resection (hereafter TUPR). Both are surgical interventions performed in patients with prostate cancer (RP) or benign prostatic hyperplasia (TUPR) [47]. Of the investigations conducted in women, two excluded pregnant women [52,53], and four included pregnant [49,51] or postpartum women [48,50,51].

Table 1.
Descriptive characteristics of the included studies.
All clinical trials studied UI. One RCT included fecal incontinence [48]. None of the studies exclusively included fecal incontinence, pelvic organ prolapse, or another pelvic floor disorder. One work does not specify the PFMT protocol [51]. 85% of the protocols are carried out daily: once a day [48,52,53], twice [47,50], or three times a day [49]. Dosage varies widely between studies. Detailed protocols for each intervention can be found in Table 2. All investigations in the sample collected results on the efficacy of PFMT-based physical therapy treatment, quality of life, and compliance or adherence to treatment at some point during the study. The intervention period ranged from a single intervention to 4 months. Three studies did not follow up [49,52,53]. The remaining ranged from 1.5 months to 12 months (see Table 1). The percentages of loss to follow-up, as can be seen in detail in Table 3, ranged from 5% [48] to 87% [51]. One study found losses of less than 15% [47]. The difference between losses was similar between the experimental and control groups in four works [47,51,52,53]. In the rest of the studies, this difference was higher [49] or slightly higher in the control group [48,50].

Table 2.
Pelvic Floor Muscle Training protocols.

Table 3.
Losses in the follow-up period.
3.3. Quality Assessment
The results of the risk of bias assessment of the included studies using the PEDro Scale are shown in Table 4. All studies in the sample met criteria 1–4, 10, and 11. One study (14%) blinded participants [51]. No study blinded therapists. One study (14%) blinded the assessors [49]. One study (14%) met criterion 8 (adequate follow-up) [47]. Intention to treat was not applied in two studies (28%) [52,53].

Table 4.
Methodological classification of quality according to the PEDro Scale.
3.4. Main Outcome
The results in terms of compliance and adherence to treatment of the included studies are shown in detail in Table 5.

Table 5.
Results Main outcome: compliance and adherence to treatment.
Compliance and/or adherence to treatment were measured in the short (85%) [47,49,50,51,52,53], medium (14%) [47], or long-term (28%) [47,48]. During the intervention period, 71% [47,49,51,52,53] measured compliance or adherence to treatment. In the follow-up period, 57% showed results [47,48,50,51].
Different questionnaires were used across studies to measure adherence, including the Knowledge Attitude Practice questionnaire [51], the MAPS questionnaire [47], the Exercise adherence rate scale (EARS) [49], visual analog scales [52,53], or questionnaires used in previous studies [48,50].
One study examined whether participants forgot to exercise [49], and one specifically studied barriers to treatment specifically, including forgetfulness [50].
All works showed strategies to improve compliance and adherence, which were based on contact with clinicians by telephone or face-to-face contact [47,49,51], information leaflet [47,50,53], and reminders in paper, video, or APP format [47,49,51]. These strategies were carried out in the experimental group except in two studies where visits to the clinic for electrostimulation treatment without PFMT [52] or written bladder training instructions were carried out [53] in the control group.
Among the seven included studies, the practice or non-practice of treatment, the frequency [47,49,51,52], the quantity [47,48] (amount of exercises or time, number of repetitions, sets, or sessions) [48,49,50], and perceived compliance with treatment were measured [52,53]. Of these, two showed adherence rates lower than 80% [47,48] (the study by Glazener et al. from 2001 [48] showed 78% of adherence. In surveys conducted at 6 and 12 years [56], the authors observed that adherence had declined to match the control group).
Three RCTs (42%) showed rates greater than 80% [50,52,53]. Two studies showed minimal or significant improvement in adherence but did not show whether it was greater or lower than 80% [49,51]. All studies that showed high adherence measured it in the short term [50,52,53]. The two investigations that showed low adherence measured it in the long term [47,48].
3.5. Secondary Outcomes
The results in terms of the severity of pelvic floor disorders and the quality of life and its relation to sexual health outcomes of the included studies are shown in detail in Table 6.

Table 6.
Results Secondary outcomes: Symptomatic Severity–Quality of life and direct or indirect relationship with sexual health outcomes.
Six studies (85%) measured both severity of symptoms and quality of life in the short (1–3 months) [47,49,50,51,52,53], one (14%) in the medium (6–9 months) [47], and two (28%) in the long term [47,48].
To collect results on symptomatic severity, the ICIQ-Urinary Incontinence Short Form (ICIQ-UI-SF) [47,49,50,51], The Incontinence Severity Index (ISI) [52,53] and a UI frequency question [48] were used as instruments.
Quality of life was measured by ICIQ-UI-SF (third question) [47,50,51], European Quality of Life-5 Dimensions EQ-5D [47], Short Form questionnaire-12 items SF-12 [47], ICIQ-Lower Urinary Tract Symptoms quality of life (LUTSqol) questionnaires ICIQ-LUTSqol [49], The Kings Health Questionnaire (KHQ) [52], Urogenital Distress Inventory, and Short Form UDI-6 with Incontinence impact questionnaire short form IIQ-7 [53]. One study used the Hospital Anxiety and Depression Scale HADS [48].
Of the eight questionnaires used, two measure sexual health directly: ICIQ-Lower Urinary Tract Symptoms quality of life (LUTSqol) questionnaires ICIQ-LUTSqol [49] directly measures how incontinence affects sex life. The Kings Health Questionnaire (KHQ) [52] directly measures the impact of incontinence on sexual health.
The remainder measured it indirectly: ICIQ-UI-SF (third question) [47,50,51], indirectly related to sexual health (impact of incontinence). European Quality of Life-5 Dimensions EQ-5D [47], indirectly related to anxiety and pain affect sexuality. Short Form questionnaire-12 items SF-12 [47], indirectly related (as physical and emotional well-being affect sexuality). Urogenital Distress Inventory, Short Form UDI-6 [53], indirectly related (as urogenital complaints affect sexuality). Incontinence impact questionnaire short form IIQ-7 [53], indirectly related (incontinence affects sex life). The Hospital Anxiety and Depression Scale HADS [48] is indirectly related (anxiety/depression affects sex life).
In 86% of the included studies [48,49,50,51,52,53], changes in symptomatic severity were related to changes in the quality of life. There was an improvement in symptomatic severity in 71% of studies [48,50,51,52,53], and 86% showed an improvement in the quality of life [47,48,50,51,52,53]. Symptomatic severity did not improve in the study in men during the intervention period or at follow-up [47]. In this trial, the quality of life improved at follow-up but because of recovery from surgery.
Three studies (42%) showed significant statistical differences in favor of the experimental group in both severity of symptoms and quality of life [48,51,53]. The rest did not show differences between the groups in any variable [47,49,50,52]. No study showed better results in the control group.
3.6. Relationship Between Sexual Health and Secondary Outcomes
Sexual health was measured directly through symptomatic severity in one study [47] and through quality of life in two studies [49,52]. In the remaining studies in the sample, sexual health was measured indirectly, as shown in Table 6.
A total of 71% of the sample studies [48,50,51,52,53] showed improved sexual health, as measured by symptomatic severity or quality of life. Of these studies, the improvement was in favor of the experimental group in 42% of the sample [48,51,53].
3.7. Relationship Between the Main and Secondary Outcomes
From the studies in the sample and in accordance with the scenarios proposed by Nagpal et al. [29], this review found the following results (Table 7). One study was related to Scenario 1 (no significant effect of intervention or improvement is observed in comparison with the inactive control group related to low adherence) [47]. Two were related to Scenario 2 (no significant effect of intervention or improvement is observed in comparison with the inactive control group related to high adherence) [50,52]. Scenario 3 was related to a study (intervention favors the experimental group over the control group related to low adherence) [48]. Finally, one study was related to Scenario 4 (intervention favors the experimental group over the control group related to high adherence) [53]. This review could not analyze this issue in two studies because of the lack of information in terms of adherence percentages. Both showed minimal or significant improvement in adherence but did not show whether it was greater or lower than 80% [49,51].

Table 7.
Relationship between the main and secondary outcomes.
In relation to treatment adherence rates, these were high in three [50,52,53] of the five studies [48,50,51,52,53] in which patients’ sexual health (through improvement in symptomatic severity or quality of life) improved but only in one study with significant differences between groups [53].
3.8. Results of the Quantitative Syntheses
Figure 2 shows the forest plot of the meta-analysis of the selected studies that evaluated the severity of symptoms and quality of life in the short term. There were no statistically significant differences between the groups (SMD = 0.07; 95% CI [−0.48, 0.61], p = 0.813) in terms of the severity of symptoms. There was a statistically significant difference in favor of the experimental group (SMD = −0.12; 95% CI [−0.28, −0.01], p = 0.036) in terms of quality of life. The timing and instruments for collecting results and meta-analyses can be consulted in Table A4.
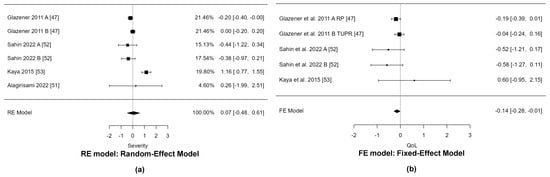
Figure 2.
(a) Forest plot of the meta-analyses of disability (Urinary incontinence severity); (b) Forest plot of the meta-analyses of activity or participation (quality of life) in the short term.
3.9. Publication Bias Assessment
The Egger’s test did not reveal publication bias (p > 0.05). Figures S1 and S2 in Supplementary Materials show the funnel plots for the meta-analyses.
3.10. Evidence Synthesis
The evidence synthesis carried out using GRADEpro v. 3.0 tool considered severity, quality of life, compliance, and adherence to treatment in Table S1. All results were classified as “not important”. The level of certainty in treatment and the outcome of adherence was low. There was a high level of certainty in the meta-analysis performed with respect to the quality of life and moderate severity of symptoms.
4. Discussion
The purpose of this systematic review was to analyze the adherence to exercise-based treatments in patients with pelvic floor disorders, given its importance in interpreting the effectiveness of exercise intervention studies [29]. In a recent scoping review [57] aimed at reviewing research priorities in physiotherapy, nine categories of research priorities were identified. Of these, the study of adherence appears as a line of research in two of them (patient needs, expectations, experience, and context; technology and big data). This review included both the male and female populations in accordance with reference studies on adherence carried out in patients with other pathologies [25,26,27,28]. However, the sample had a larger number of studies conducted in women than in men; only one study [47] carried out in the male population met the eligibility criteria.
Most of the sample was conducted in a population with urinary incontinence, so there appears to be a lack of studies that measure the adherence to PFMT in populations with other pelvic floor dysfunctions.
4.1. Qualitative Analysis
Qualitative analysis of the included studies revealed that adherence and compliance with treatment appeared to be high in the short term and decreased in the long term. This fact is well known and therefore, recommendations for improvements in the lines of research [38] are based on efforts to maintain adherence rates in the medium and long term. In this review, the studies agreed on the response criteria, characterizing adherence as high when it exceeded 80%. This is in line with previous publications submitted between 1996 and 2023 [29,39,40,41,42]. Although data show that high short-term adherence predicts high long-term adherence, rates are also known to decline over time [29,38]. This review found that studies tend to measure outcomes in the short term and a deficit in the medium and long term. The review studies used strategies based on contact with the therapist, reinforcement, and reminders. This is because forgetfulness is known to be a major barrier, and increased contact with the therapist is a relevant facilitator [25,27]. However, despite these strategies, this review found studies that did not show high adherence rates.
Sexual health was measured indirectly in most of the studies in the sample through the severity and/or quality of life of the patients. In the qualitative analysis, the severity of symptoms appeared to be related to the quality of life. There was an improvement in symptomatic severity in 71% of studies [48,50,51,52,53], and 86% showed an improvement in the quality of life [47,48,50,51,52,53]. With these data, this review attempted to correlate treatment effectiveness with adherence and compliance rates using the scenarios proposed by evidence [29]. In the sample, the studies were related to Scenarios 1 [47], 2 [50,52], 3 [48], and 4 [53].
However, these results should be viewed with caution. As could be analyzed with the GRADEpro v. 3.0 tool, the level of certainty in treatment and adherence outcomes was low. Heterogeneity in the PFMT protocols and adherence measurement systems makes it difficult to interpret the results correctly. In the particular case of the pelvic floor pathology approach, due to the difficulty of blinding subjects and therapists, scores of 8 can be considered high quality and between 4 and 6 moderate quality according to the PEDro scale [44]. All studies included in the sample are of moderate quality according to the PEDro scale and meet the 11 criteria (this study provides both point measures and measures of variability for at least one key outcome). However, when the statistical information comes from adherence and/or compliance, it appears heterogeneous.
This review did not find a clear relationship between improvements in symptomatic severity or quality of life (and sexual health) and adherence rates to exercise-based treatment. In fact, of the studies in which the experimental group showed improvements compared with the control group, the adherence rates ranged from high to low. It seems reasonable to think that if adherence is high, the effectiveness of the treatments will be higher. However, Nagpal et al. [29] offered a possible way to analyze the relationship between adherence to exercise-based treatments and therapeutic effectiveness, showing four possible scenarios. In the sample, one study showed low adherence and low effectiveness [47]. This study, which falls into Scenario 1, suggests that we should strive to increase adherence to see if we could achieve better results in terms of effectiveness. However, this review also found studies in which high adherence did not lead to better outcomes in the experimental group compared with the control group. In fact, all four possible scenarios proposed in the study by Nagpal et al. [29] were met; therefore, a clear relationship between the variables could not be established.
4.2. Quantitative Analysis
The quantitative analysis of the results revealed that PFMT seems to be associated with improvements in the global quality of life in the short term. There were no statistically significant differences in terms of the severity of symptoms related to urinary incontinence. Therefore, a quantitative analysis could not be performed to interpret these data in detail, nor could a detailed study of the relationship between exercise adherence and exercise efficacy be carried out. It seems that the main drawback lies in the lack of homogeneity in the way the results of this variable are measured. Nevertheless, this is not the case for instruments that measure the quality of life or symptomatic severity. Moreover, this review found questionnaires (i.e., ICIQ-UI-SF) that were commonly used in a diverse population, were easy to use, and allowed us to carry out a more rigorous analysis of the results.
4.3. The Challenge of Adherence
During the screening process, 255 studies were eliminated because they did not measure adherence to treatment. A total of 106 were eliminated because they measured compliance or adherence through the patient’s diary, reports made verbally, or through information approved by clinicians. Furthermore, this review detected more than 15 studies that specifically stated in their limitations that they did not measure adherence. From some of these, lines of research on the measurement of adherence were created in 1998 [58] and 2006 [59]. However, the rest of the studies with this limitation were subsequently published; eight were published in the last five years, including 2024 [60]. This is echoed in similar reviews conducted recently in male [23] and female [61] populations in which this outcome appeared as secondary. Although they had different samples, all three studies agreed on the problem of measuring adherence to treatment. Therefore, this seems to be the first meta-analysis carried out in people with pelvic floor disorders that highlights the lack of importance given to adherence and compliance to treatment in trials of the effectiveness of pelvic floor muscle exercise treatment, despite the relevance given to these variables by the scientific community. Aware of the multidimensionality of adherence and although there are questionnaires that take it into account [33,55], perhaps the key lies in the use or design of a general questionnaire on adherence and compliance, from which, as in other cases, such measurement of quality of life, specific questionnaires can be derived. In this way, in addition to homogenizing the results and being able to perform a quantitative synthesis, we will address an additional problem. If data obtained on adherence are based only on participants who completed the questionnaires, we are losing valuable information [29].
4.4. Clinical Implications
For future research and clinical practice in the pelvic floor disorder area, we may need to strive for high rates of compliance with questionnaires or scale submissions, just as we strive for high rates of adherence to treatment. Until we can adequately relate exercise adherence to exercise effectiveness, we will not be able to address the disability of people suffering from pelvic floor dysfunction. If we do not measure adherence and compliance with treatment of people with pelvic floor dysfunctions with tools such as those used to measure variables such as quality of life, we will never really know the clinical effectiveness of treatments.
4.5. Limitations and Future Considerations
This systematic review has some limitations. The sample is small, but this is perhaps one of the most interesting results because it is related to the lack of available evidence to measure adherence and compliance through objective systems. Likewise, the search restricted to studies in English and Spanish could have generated a language bias, potentially excluding evidence published in other languages. The lack of significance in Egger’s test does not completely rule out the possibility of publication bias due to the small sample size. A meta-analysis of the main outcome could not be performed because of the variability in the measurement instruments and statistical data provided by the studies. Finally, limited clinical implications can be drawn from the meta-analyses. The results of the meta-analysis of symptomatic severity have a confidence interval that ranges from a moderately harmful effect to a moderately helpful effect, so pooled data do not narrow down the possible effect enough to draw any coherent clinical implication from this imprecise estimate. The results of the quality of life meta-analysis had a confidence interval ranging from a small to moderate effect to a trivial effect (−0.01), so we redetermined whether the effect of the intervention was clinically relevant or clinically insignificant.
5. Conclusions
The results appear to indicate, with a low level of certainty of evidence, that people with pelvic floor disorders show high rates of adherence to pelvic floor muscle exercise in the short term and experience an improved quality of life with a high level of certainty of evidence. However, a robust relationship between adherence rates and intervention efficacy cannot be established. More randomized clinical trials are required to support these findings.
Therefore, more research is needed on the design and implementation of a scientifically recommended and easy-to-administer system to measure compliance and adherence to exercise-based treatments. This would allow the establishment of a clear relationship between compliance or adherence data and the efficacy of treatment, quality of life, or disability caused by pelvic floor disorders.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/life15040613/s1, Figure S1: Symptomatic Severity (UI) Funnel plot for selection bias.; Figure S2: Quality of life Funnel plot for selection bias.; Table S1: Summary of the evidence of the results according to their certainty and their importance using the Grading of Recommendations Assessment, Development, and Evaluations (GRADE tool).
Author Contributions
Conceptualization, I.V.-D.-P., M.R.-S. and C.-M.S.-S.; methodology, J.-J.J.-R. and Á.-J.R.-D.; formal analysis, J.-J.J.-R. and Á.-J.R.-D.; investigation, I.V.-D.-P., C.-M.S.-S. and M.R.-S.; data curation, J.-J.J.-R. and Á.-J.R.-D.; writing—original draft preparation, I.V.-D.-P., C.-M.S.-S. and M.R.-S.; writing—review and editing, I.V.-D.-P., C.-M.S.-S., M.R.-S., J.-J.J.-R. and Á.-J.R.-D.; visualization, I.V.-D.-P., C.-M.S.-S., M.R.-S., J.-J.J.-R. and Á.-J.R.-D. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data supporting the findings of this study can be made available upon request.
Conflicts of Interest
The authors declare no conflicts of interest.
Appendix A

Table A1.
Search strategy.
Table A1.
Search strategy.
| Intervention | AND | Participants | AND | Outcome | AND | Design |
| (“Physical Therapy Modalities” OR “exercise therapy” OR “exercise” OR “Exercise Movement Techniques”) | (“Urinary Incontinence” OR “Pelvic Floor Disorders”) | (“Patient Compliance” OR “Treatment Adherence and Compliance”) | “effectiveness” |
Limits in study design: randomized clinical trials or pilot study. Language limits: Spanish and English. Limits on the time of publication: no limit established. Studies published up to 15 October 2024.

Table A2.
Specific search strategy for each database.
Table A2.
Specific search strategy for each database.
| Database | Search Strategy |
|---|---|
| CINAHL | ((((“Patient Compliance” OR “Treatment Adherence and Compliance”) AND (“Physical Therapy Modalities” OR “exercise therapy” OR “exercise” OR “Exercise Movement Techniques”) AND (“Urinary Incontinence” OR “Pelvic Floor Disorders”) AND (“effectiveness”)))) Limit “academic publications” in source type. |
| EMBASE | (’pelvic floor disorder’/exp OR ’urine incontinence’/exp) AND (’physiotherapy’/exp OR ’exercise’/exp) AND patient compliance/exp AND randomized controlled trial/exp |
| The Cochrane Plus Library | ((((“Patient Compliance” OR “Treatment Adherence and Compliance”) AND (“Physical Therapy Modalities” OR “exercise therapy” OR “exercise” OR “Exercise Movement Techniques”) AND (“Urinary Incontinence” OR “Pelvic Floor Disorders”) AND (“effectiveness”)))) Limit “Randomized controlled Trial”. |
| Medes | (((((((((““Cooperación del paciente” “[todos]) OR ““Cumplimiento y adherencia al tratamiento” “[todos]) AND “ “Modalidades de Fisioterapia”“[todos]) OR “ “terapia por ejercicio” “[todos]) OR “ “ejercicio físico” “[todos]) OR “ “Técnicas de ejercicio con movimiento” “[todos]) AND “ “Incontinencia urinaria” “[todos]) OR ““Trastornos del suelo pélvico” “[todos]) AND ““efectividad”“[todos]) |
| PEDro | Therapy: strength training/Problem: incontinence/Body part: perineum or genitor-urinary system/Sub discipline: continence and women’s health/Topic: no appropriate value in this field/Method: Clinical Trial |
| PubMed | “Patient Compliance” OR “Treatment Adherence and Compliance” AND “Physical Therapy Modalities” OR “exercise therapy” OR “exercise” OR “Exercise Movement Techniques” AND “Urinary Incontinence” OR “Pelvic Floor Disorders” AND “effectiveness” Limit “Randomized controlled Trial”. |
| Scopus | “Patient Compliance” OR “Treatment Adherence and Compliance” AND “Physical Therapy Modalities” OR “exercise therapy” OR “exercise” OR “Exercise Movement Techniques” AND “Urinary Incontinence” OR “Pelvic Floor Disorders” AND “effectiveness” |
| TRIP | “Urinary incontinence” OR “pelvic floor disorders” AND “patient compliance” OR “treatment adherence AND compliance” AND “physical therapy modalities” OR “exercise therapy” OR “exercise” OR “exercise movement techniques” Limit Key primary research. |
| WOS Filtered by WOS categories: rehabilitation, sport sciences, gerontology, communication, obstetrics gynecology, urology nephrology, pediatrics, cultural studies, medicine research experimental. | ((((((((AB = (“Patient Compliance”)) OR AB = (“Treatment Adherence and Compliance”)) AND AB = (“Physical Therapy Modalities”)) OR AB = (“exercise therapy” )) OR AB = (“exercise”)) OR AB = (“Exercise Movement Techniques”)) AND AB = (“Urinary Incontinence”)) OR AB = (“Pelvic Floor Disorders”)) AND AB = (“effectiveness”) Limit “Clinical Trial”. |

Table A3.
Study selection.
Table A3.
Study selection.
| Database | Identified | Duplicated | Design | Language | Neurological Origin | Selected for Screening | No Pelvic Floor Muscle Training (PFMT) /Intervention Based on PMFT in Both Groups/No Pelvic Floor Disorder | Eliminated After Reading the Full Text for Not Measuring Adherence or Compliance | Eliminated for Not Measuring Adherence to Treatment by Scales or Questionnaires | Included in the Review |
|---|---|---|---|---|---|---|---|---|---|---|
| CINAHL | 556 | 3 | 509 | 11 | 1 | 32 | 29 | 3 | 0 | 0 |
| EMBASE | 33 | 11 | 13 | 0 | 1 | 8 | 3 | 4 | 1 | 0 |
| The Cochrane Plus Library | 60 | 41 | 5 | 0 | 0 | 14 | 9 | 2 | 3 | 0 |
| Medes * | 6 | 0 | 5 | 0 | 0 | 1 | 0 | 1 | 0 | 0 |
| PEDro ** | 345 | 35 | 1 | 11 | 12 | 286 | 22 | 179 | 82 | 3 |
| PubMed | 128 | 10 | 18 | 2 | 2 | 96 | 29 | 50 | 14 | 3 |
| Scopus | 68 | 27 | 35 | 0 | 0 | 6 | 0 | 2 | 3 | 1 |
| TRIP | 150 | 16 | 37 | 0 | 0 | 97 | 87 | 9 | 1 | 0 |
| WOS | 85 | 35 | 31 | 0 | 0 | 19 | 12 | 5 | 2 | 0 |
| TOTAL | 1431 | 178 | 654 | 24 | 16 | 559 | 191 | 255 | 106 | 7 |
* Since 1 April 2024, the MEDES database has been suspended indefinitely as the Fundación Lilly wishes to promote the rest of the initiatives that make up the “MEDES-MEDicina en ESpañol project”, and to devote all its resources to them. ** In the PEDro database, this review selected studies that scored ≥4. This eligibility criterion was applied in all studies in all databases and is applied because although studies are considered good (with scores between 6 and 8) or excellent (between 9 and 10) by the scientific literature, in the particular case of the pelvic floor pathology approach, it is considered that due to the difficulty of blinding subjects and therapists, scores of 8 can be considered high quality and between 4 and 6 moderate quality [38].

Table A4.
Timing and instruments for collecting results and Meta-Analyses.
Table A4.
Timing and instruments for collecting results and Meta-Analyses.
| Treatment Compliance and Adherence | |||||
| Study | 1 mo.–2 mo. | 3 mo. | 6 mo. | 9 mo. | 12 mo. |
| Glazener et al. (2011) [47] | MAPS Q. | MAPS Q. Practice y—no | MAPS Q. | ||
| Glazener et al. (2001) [48] | Modified version Questionnaire [54]. | ||||
| Jaffar et al. (2022) [49] | EARS 21 points (KAP) Q Section 5 | ||||
| Sacomori et al. (2020) [50] | Q Validated Alewijnse D. et al. 2003) [55] | ||||
| Alagirisamy et al. (2022) [51] | (KAP) Q Section 5 | KAP Q (4 mo.) | |||
| Sahin et al. (2022) [52] | 100 mm VAS complete exercises (no in G3) | ||||
| Kaya et al. (2015) [53] | 100 mm VAS scale. Compliance. (1.5 mo.) | ||||
| Quality of Life | |||||
| Study | 1 mo.–2 mo. | 3 mo. | 6 mo. | 9 mo. | 12 mo. |
| Glazener et al. (2011) [47] | Q3 ICIQ | EQ-5D and SF-12 Q3 ICIQ | EQ-5D and SF-12 Q3 ICIQ | ||
| Glazener et al. (2001) [48] | HADS | ||||
| Jaffar et al. (2022) [49] | ICIQ-LUTSqol 1 mo. and 2 mo. | ||||
| Sacomori et al. (2020) [50] | ICIQ-UI SF Q3 ICIQ | ||||
| Alagirisamy et al. (2022) [51] | ICIQ-UI SF No specific data from Q3 | ICIQ-UI SF 4 mo. No specific data from Q3 | |||
| Sahin et al. (2022) [52] | KHQ baseline 2 mo. | ||||
| Kaya et al. (2015) [53] | UDI-6 + IIQ-7 baseline 6 weeks | ||||
| Severity | |||||
| Study | 1 mo.–2 mo. | 3 mo. | 6 mo. | 9 mo. | 12 mo. |
| Glazener et al. (2011) [47] | ICIQ-UI SF Q1-3 p.57 pad use | ICIQ-UI SF Q1-3 pad use | ICIQ-UI SF Q1-3 pad use | ICIQ-UI SF Q1-3 pad use | |
| Glazener et al. (2001) [48] | Question about frequency | ||||
| Jaffar et al. (2022) [49] | ICIQ-UI SF 1 mo. and 2 mo. | ||||
| Sacomori et al. (2020) [50] | ICIQ-UI SF | ||||
| Alagirisamy et al. (2022) [51] | ICIQ-UI SF | ICIQ-UI SF 4 mo. | |||
| Sahin et al. (2022) [52] | Baseline 2 mo. 24 h pad test/ ISI/UDI-6 | ||||
| Kaya et al. (2015) [53] | ISI baseline and 6 weeks | ||||
References
- Messelink, B.; Benson, T.; Berghmans, B.; Bø, K.; Corcos, J.; Fowler, C.; Laycock, J.; Lim, P.H.-C.; van Lunsen, R.; Lycklama á Nijeholt, G.; et al. Standardization of Terminology of Pelvic Floor Muscle Function and Dysfunction: Report from the Pelvic Floor Clinical Assessment Group of the International Continence Society. Neurourol. Urodyn. 2005, 24, 374–380. [Google Scholar] [CrossRef] [PubMed]
- Ramírez García, I.; Blanco Ratto, L.; Kaufmann Frau, S. Rehabilitación Del Suelo Pélvico Femenino: Práctica Clínica Basada en la Evidencia; Médica Panamericana: Washington, DC, USA, 2014; ISBN 978-84-9110-475-9. [Google Scholar]
- Cohen, D.; Gonzalez, J.; Goldstein, I. The Role of Pelvic Floor Muscles in Male Sexual Dysfunction and Pelvic Pain. Sex. Med. Rev. 2016, 4, 53–62. [Google Scholar] [CrossRef] [PubMed]
- Frawley, H.; Shelly, B.; Morin, M.; Bernard, S.; Bø, K.; Digesu, G.A.; Dickinson, T.; Goonewardene, S.; McClurg, D.; Rahnama’i, M.S.; et al. An International Continence Society (ICS) Report on the Terminology for Pelvic Floor Muscle Assessment. Neurourol. Urodyn. 2021, 40, 1217–1260. [Google Scholar] [CrossRef] [PubMed]
- Hage-Fransen, M.A.H.; Wiezer, M.; Otto, A.; Wieffer-Platvoet, M.S.; Slotman, M.H.; Nijhuis-van der Sanden, M.W.G.; Pool-Goudzwaard, A.L. Pregnancy- and Obstetric-related Risk Factors for Urinary Incontinence, Fecal Incontinence, or Pelvic Organ Prolapse Later in Life: A Systematic Review and Meta-analysis. Acta Obstet. Gynecol. Scand. 2021, 100, 373–382. [Google Scholar] [CrossRef]
- Mohedo, E.D.; Sánchez, E.M.M.; Serrano, C.M.S. Guía de Práctica Clínica Para Fisioterapeutas en la Incontinencia Urinaria Femenina, 1st ed.; Ilustra Colegio Oficial de Fisioterapeutas de Andalucía: Sevilla, Spain, 2013; ISBN 13978-84-616-4903-7. [Google Scholar]
- Milsom, I.; Altman, D.; Lapitan, M.C.; Nelson, R.; Sillen, U.; Thom, D. Epidemiology of Urinary (UI) and Faecal (FI) Incontinence and Pelvic Organ Prolapse (POP). Incontinence 2009, 15–107. Available online: https://www.ics.org/publications/ici_3/v1.pdf/chap5.pdf (accessed on 2 April 2025).
- D’Ancona, C.; Haylen, B.; Oelke, M.; Abranches-Monteiro, L.; Arnold, E.; Goldman, H.; Hamid, R.; Homma, Y.; Marcelissen, T.; Rademakers, K.; et al. The International Continence Society (ICS) Report on the Terminology for Adult Male Lower Urinary Tract and Pelvic Floor Symptoms and Dysfunction. Neurourol. Urodyn. 2019, 38, 433–477. [Google Scholar] [CrossRef]
- Kocjancic, E.; Chung, E.; Garzon, J.A.; Haylen, B.; Iacovelli, V.; Jaunarena, J.; Locke, J.; Millman, A.; Nahon, I.; Ohlander, S.; et al. International Continence Society (ICS) Report on the Terminology for Sexual Health in Men with Lower Urinary Tract (LUT) and Pelvic Floor (PF) Dysfunction. Neurourol. Urodyn. 2022, 41, 140–165. [Google Scholar] [CrossRef]
- Thüroff, J.W.; Abrams, P.; Andersson, K.-E.; Artibani, W.; Chapple, C.R.; Drake, M.J.; Hampel, C.; Neisius, A.; Schröder, A.; Tubaro, A. Guías EAU Sobre Incontinencia Urinaria. Actas Urol. Esp. 2011, 35, 373–388. [Google Scholar]
- Mazariego, C.G.; Egger, S.; King, M.T.; Juraskova, I.; Woo, H.; Berry, M.; Armstrong, B.K.; Smith, D.P. Fifteen Year Quality of Life Outcomes in Men with Localised Prostate Cancer: Population Based Australian Prospective Study. BMJ 2020, 371, m3503. [Google Scholar] [CrossRef]
- Bø, K.; Berghmans, B.; Mørkved, S.; Van Kampen, M. Evidence-Based Physical Therapy for the Pelvic Floor, 3rd ed.; Elsevier Health Sciences: Amsterdam, The Netherlands, 2023; ISBN 978-0-7020-8308-2. [Google Scholar]
- World Health Organization. International Classification of Functioning, Disability and Health (ICF). Available online: https://www.who.int/standards/classifications/international-classification-of-functioning-disability-and-health (accessed on 1 May 2024).
- Tian, Z.; Wang, X.; Fu, L.; Du, Z.; Sun, Z. Impact of Female Stress Urinary Incontinence and Related Treatments on the Sexual Function of Male Partners: A Systematic Review and Meta-Analysis. J. Sex. Med. 2023, 20, 1069–1077. [Google Scholar] [CrossRef]
- Gupta, N.; Zebib, L.; Wittmann, D.; Nelson, C.J.; Salter, C.A.; Mulhall, J.P.; Byrne, N.; Nolasco, T.S.; Loeb, S. Understanding the Sexual Health Perceptions, Concerns, and Needs of Female Partners of Prostate Cancer Survivors. J. Sex. Med. 2023, 20, 651–660. [Google Scholar] [CrossRef]
- Dumoulin, C.; Cacciari, L.P.; Hay-Smith, E.J.C. Pelvic Floor Muscle Training versus No Treatment, or Inactive Control Treatments, for Urinary Incontinence in Women. Cochrane Database Syst. Rev. 2018, 10, CD005654. [Google Scholar] [CrossRef]
- Khandelwal, C. Diagnosis of Urinary Incontinence. Urin. Incontinence 2013, 87, 8. [Google Scholar]
- Anderson, C.A.; Omar, M.I.; Campbell, S.E.; Hunter, K.F.; Cody, J.D.; Glazener, C.M.A. Conservative Management for Postprostatectomy Urinary Incontinence. Cochrane Database Syst. Rev. 2015, 1, CD001843. [Google Scholar] [CrossRef] [PubMed]
- Mungovan, S.F.; Carlsson, S.V.; Gass, G.C.; Graham, P.L.; Sandhu, J.S.; Akin, O.; Scardino, P.T.; Eastham, J.A.; Patel, M.I. Preoperative Exercise Interventions to Optimize Continence Outcomes Following Radical Prostatectomy. Nat. Rev. Urol. 2021, 18, 259–281. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, R.; Fink, H.A.; Huckabay, C.; Monga, M.; Wilt, T.J. Pelvic Floor Muscle Training to Improve Urinary Incontinence after Radical Prostatectomy: A Systematic Review of Effectiveness. BJU Int. 2007, 100, 76–81. [Google Scholar] [CrossRef]
- Reimer, N.; Zopf, E.M.; Böwe, R.; Baumann, F.T. Effects of Exercise on Sexual Dysfunction in Patients with Prostate Cancer—A Systematic Review. J. Sex. Med. 2021, 18, 1899–1914. [Google Scholar] [CrossRef]
- Bø, K. Physiotherapy Management of Urinary Incontinence in Females. J. Physiother. 2020, 66, 147–154. [Google Scholar] [CrossRef]
- Johnson, E.E.; Mamoulakis, C.; Stoniute, A.; Omar, M.I.; Sinha, S. Conservative Interventions for Managing Urinary Incontinence after Prostate Surgery. Cochrane Database Syst. Rev. 2023, 2023, CD014799. [Google Scholar] [CrossRef]
- National Library of Medecine. Treatment Adherence and Compliance. Available online: http://id.nlm.nih.gov/mesh/D000074822 (accessed on 20 July 2022).
- Jack, K.; McLean, S.M.; Moffett, J.K.; Gardiner, E. Barriers to Treatment Adherence in Physiotherapy Outpatient Clinics: A Systematic Review. Man. Ther. 2010, 15, 220–228. [Google Scholar] [CrossRef]
- Rizzo, J. Patients’ Mental Models and Adherence to Outpatient Physical Therapy Home Exercise Programs. Physiother. Theory Pract. 2015, 31, 253–259. [Google Scholar] [CrossRef]
- Campbell, R. Why Don’t Patients Do Their Exercises? Understanding Non-Compliance with Physiotherapy in Patients with Osteoarthritis of the Knee. J. Epidemiol. Community Health 2001, 55, 132–138. [Google Scholar] [CrossRef] [PubMed]
- McLean, S.M.; Burton, M.; Bradley, L.; Littlewood, C. Interventions for Enhancing Adherence with Physiotherapy: A Systematic Review. Man. Ther. 2010, 15, 514–521. [Google Scholar] [CrossRef] [PubMed]
- Nagpal, T.S.; Mottola, M.F.; Barakat, R.; Prapavessis, H. Adherence Is a Key Factor for Interpreting the Results of Exercise Interventions. Physiotherapy 2021, 113, 8–11. [Google Scholar] [CrossRef] [PubMed]
- Latorre, G.F.S.; de Fraga, R.; Seleme, M.R.; Mueller, C.V.; Berghmans, B. An Ideal E-Health System for Pelvic Floor Muscle Training Adherence: Systematic Review. Neurourol. Urodyn. 2019, 38, 63–80. [Google Scholar] [CrossRef]
- Navarro-Brazález, B.; Vergara-Pérez, F.; Prieto-Gómez, V.; Sánchez-Sánchez, B.; Yuste-Sánchez, M.J.; Torres-Lacomba, M. What Influences Women to Adhere to Pelvic Floor Exercises after Physiotherapy Treatment? A Qualitative Study for Individualized Pelvic Health Care. J. Pers. Med. 2021, 11, 1368. [Google Scholar] [CrossRef]
- Dumoulin, C.; Hay-Smith, J.; Frawley, H.; McClurg, D.; Alewijnse, D.; Bo, K.; Burgio, K.; Chen, S.-Y.; Chiarelli, P.; Dean, S.; et al. 2014 Consensus Statement on Improving Pelvic Floor Muscle Training Adherence: International Continence Society 2011 State-of-the-Science Seminar. Neurourol. Urodyn. 2015, 34, 600–605. [Google Scholar] [CrossRef]
- Venegas, M.; Carrasco, B.; Casas-Cordero, R. Factors Influencing Long-Term Adherence to Pelvic Floor Exercises in Women with Urinary Incontinence. Neurourol. Urodyn. 2018, 37, 1120–1127. [Google Scholar] [CrossRef]
- Bernardes, M.F.V.G.; da Mata, L.R.F.; Azevedo, C.; Izidoro, L.C.d.R.; de Oliveira, C.M.C.; Chianca, T.C.M. Effectiveness of systemic acupuncture in the control of urinary incontinence following radical prostatectomy: A randomized clinical trial. Rev. Esc. Enferm. USP 2022, 56, e20220135. [Google Scholar] [CrossRef]
- Torres-Lacomba, M.; Navarro-Brazález, B.; Yuste-Sánchez, M.J.; Sánchez-Sánchez, B.; Prieto-Gómez, V.; Vergara-Pérez, F. Women’s Experiences with Compliance with Pelvic Floor Home Exercise Therapy and Lifestyle Changes for Pelvic Organ Prolapse Symptoms: A Qualitative Study. J. Pers. Med. 2022, 12, 498. [Google Scholar] [CrossRef]
- Sawettikamporn, W.; Sarit-Apirak, S.; Manonai, J. Attitudes and Barriers to Pelvic Floor Muscle Exercises of Women with Stress Urinary Incontinence. BMC Women’s Health 2022, 22, 477. [Google Scholar] [CrossRef]
- Cobo, C.M.S.; Camarero, A.R.A. Claves para el diseño y validación de cuestionarios en Ciencias de la Salud. Enferm. Cardiol. 2019, 26, 69–73. [Google Scholar]
- Bø, K.; Hilde, G. Does It Work in the Long Term?—A Systematic Review on Pelvic Floor Muscle Training for Female Stress Urinary Incontinence: Long-Term Outcome of Pelvic Floor Muscle Training. Neurourol. Urodyn. 2013, 32, 215–223. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.J., 3rd. Intravaginal Stimulation Randomized Trial. J. Urol. 1996, 155, 127–130. [Google Scholar] [CrossRef] [PubMed]
- Manonai, J.; Harnsomboon, T.; Sarit-apirak, S.; Wattanayingcharoenchai, R.; Chittacharoen, A.; Suthutvoravut, S. Effect of Colpexin Sphere on Pelvic Floor Muscle Strength and Quality of Life in Women with Pelvic Organ Prolapse Stage I/II: A Randomized Controlled Trial. Int. Urogynecology J. 2012, 23, 307–312. [Google Scholar] [CrossRef]
- Ferro García, R.; García Ríos, M.C.; Vives Montero, M.C. Un análisis de la adherencia al tratamiento en fisioterapia. Fisioterapia 2004, 26, 333–339. [Google Scholar] [CrossRef]
- Fuentes-Aparicio, L.; Rejano-Campo, M.; Lopez-Bueno, L.; Marie Donnelly, G.; Balasch-Bernat, M. The Effect of an Abdominopelvic Exercise Program Alone versus in Addition to Postural Instructions on Pelvic Floor Muscle Function in Climacteric Women with Stress Urinary Incontinence. A Randomized Controlled Trial. Physiother. Theory Pract. 2023, 4, 738–749. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, 71. [Google Scholar] [CrossRef]
- Gomez-Conesa, A.; Serrano, C.S.; Matamoros, D.C.; López-López, J.A. The Spanish Translation and Adaptation of the Pedro Scale. Physiotherapy 2015, 101, e463–e464. [Google Scholar] [CrossRef]
- Cashin, A.G.; McAuley, J.H. Clinimetrics: Physiotherapy Evidence Database (PEDro) Scale. J. Physiother. 2020, 66, 59. [Google Scholar] [CrossRef]
- Sanabria, A.; Rigau, D.; Rotaeche, R.; Selva, A.; Marzo-Castillejo, M.; Alonso-Coello, P. Sistema GRADE: Metodología para la realización de recomendaciones para la práctica clínica. Atención Primaria 2015, 47, 48–55. [Google Scholar] [CrossRef]
- Glazener, C.; Boachie, C.; Buckley, B.; Cochran, C.; Dorey, G.; Grant, A.; Hagen, S.; Kilonzo, M.; McDonald, A.; McPherson, G.; et al. Urinary incontinence in men after formal one-to-one pelvic-floor muscle training following radical prostatectomy or transurethral resection of the prostate (MAPS): Two par-allel randomised controlled trials. Lancet 2011, 378, 328–337. [Google Scholar] [CrossRef]
- Glazener, C.M.; Herbison, G.P.; Wilson, P.D.; MacArthur, C.; Lang, G.D.; Gee, H.; Grant, A.M. Conservative Management of Persistent Postnatal Urinary and Faecal Incontinence: Randomised Controlled Trial. BMJ 2001, 323, 593–596. [Google Scholar] [CrossRef] [PubMed]
- Jaffar, A.; Mohd Sidik, S.; Foo, C.N.; Muhammad, N.A.; Abdul Manaf, R.; Suhaili, N. Preliminary Effectiveness of mHealth App-Based Pelvic Floor Muscle Training among Pregnant Women to Improve Their Exercise Adherence: A Pilot Randomised Control Trial. Int. J. Environ. Res. Public Health 2022, 19, 2332. [Google Scholar] [CrossRef] [PubMed]
- Sacomori, C.; Zomkowski, K.; Dos Passos Porto, I.; Cardoso, F.L.; Sperandio, F.F. Adherence and Effectiveness of a Single Instruction of Pelvic Floor Exercises: A Randomized Clinical Trial. Int. Urogynecology J. 2020, 31, 951–959. [Google Scholar] [CrossRef] [PubMed]
- Alagirisamy, P.; Sidik, S.M.; Rampal, L.; Ismail, S.I.F. Effectiveness of a Pelvic Floor Muscle Exercise Intervention in Improving Knowledge, Attitude, Practice, and Self-Efficacy among Pregnant Women: A Randomized Controlled Trial. Korean J. Fam. Med. 2022, 43, 42–55. [Google Scholar] [CrossRef]
- Sahin, U.K.; Acaroz, S.; Cirakoglu, A.; Benli, E.; Akbayrak, T. Effects of External Electrical Stimulation Added to Pelvic Floor Muscle Training in Women with Stress Urinary Incontinence: A Randomized Controlled Study. Neurourol. Urodyn. 2022, 8, 1781–1792. [Google Scholar] [CrossRef]
- Kaya, S.; Akbayrak, T.; Gursen, C.; Beksac, S. Short-Term Effect of Adding Pelvic Floor Muscle Training to Bladder Training for Female Urinary Incontinence: A Randomized Controlled Trial. Int. Urogynecology J. 2015, 26, 285–293. [Google Scholar] [CrossRef]
- Wilson, P.D.; Herbison, G.P. A Randomized Controlled Trial of Pelvic Floor Muscle Exercises to Treat Postnatal Urinary Incontinence. Int. Urogynecol. J. Pelvic Floor Dysfunct. 1998, 9, 257–264. [Google Scholar] [CrossRef]
- Alewijnse, D.; Mesters, I.; Metsemakers, J.; van den Borne, B. Predictors of Long-Term Adherence to Pelvic Floor Muscle Exercise Therapy among Women with Urinary Incontinence. Health Educ. Res. 2003, 18, 511–524. [Google Scholar] [CrossRef]
- Glazener, C.M.A.; MacArthur, C.; Hagen, S.; Elders, A.; Lancashire, R.; Herbison, G.P.; Wilson, P.D. Twelve-Year Follow-up of Conservative Management of Postnatal Urinary and Faecal Incontinence and Prolapse Outcomes: Randomised Controlled Trial. BJOG Int. J. Obstet. Gynaecol. 2014, 121, 112–120. [Google Scholar] [CrossRef]
- Souto-Miranda, S.; Brazete Cruz, E.; Pires, D.; Ribeiro, F.; Cordeiro, N.; Jácome, C. Priorities in Physical Therapy Research: A Scoping Review. Braz. J. Phys. Ther. 2024, 28, 101135. [Google Scholar] [CrossRef]
- Burgio, K.L.; Locher, J.L.; Goode, P.S.; Hardin, J.M.; McDowell, B.J.; Dombrowski, M.; Candib, D. Behavioral vs Drug Treatment for Urge Urinary Incontinence in Older Women: A Randomized Controlled Trial. JAMA 1998, 280, 1995–2000. [Google Scholar] [CrossRef] [PubMed]
- Borello-France, D.F.; Zyczynski, H.M.; Downey, P.A.; Rause, C.R.; Wister, J.A. Effect of Pelvic-Floor Muscle Exercise Position on Continence and Quality-of-Life Outcomes in Women with Stress Urinary Incontinence. Phys. Ther. 2006, 86, 974–986. [Google Scholar] [PubMed]
- Sanchez-Salas, R.; Tourinho-Barbosa, R.; Sivaraman, A.; Borges, R.C.; Candela, L.; Cathala, N.; Mombet, A.; Marra, G.; Sanchez, L.R.; Boumezrag, C.B.; et al. Assessing the Efficacy of Pelvic Floor Muscle Training and Duloxetine on Urinary Continence Recovery Following Radical Prostatectomy: A Randomized Clinical Trial. Prostate 2024, 84, 158–165. [Google Scholar] [CrossRef] [PubMed]
- Papanikolaou, D.; Lampropoulou, S.; Giannitsas, K.; Skoura, A.; Fousekis, K.; Billis, E. Pelvic Floor Muscle Training: Novel versus Traditional Remote Rehabilitation Methods. A Systematic Review and Meta-Analysis on Their Effectiveness for Women with Urinary Incontinence. Neurourol. Urodyn. 2023, 42, 856–874. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).