Abstract
Background: Acute limb ischaemia (ALI) is of great clinical importance due to its consequent serious complications and high comorbidity and mortality rates. The purpose of this study was to compare the acute success and complication rates of CDT performed via transradial, transbrachial, and transfemoral access sites in patients with acute lower limb vascular occlusion and to investigate the 1-year outcomes of CDT and MT for ALI. Methods: Between 2008 and 2019, 84 consecutive patients with ALI were treated with CDT in a large community hospital. Data were collected and retrospectively analysed. The primary (“safety”) endpoints encompassed major adverse events (MAEs), major adverse limb events (MALEs), and the occurrence of complications related to the access site. Secondary (“efficacy”) endpoints included both technical and clinical achievements, treatment success, fluoroscopy time, radiation dose, procedure time, and the crossover rate to an alternative puncture site. Results: CDT was started with radial (n = 17), brachial (n = 9), or femoral (n = 58) access. CDT was technically successful in 74/84 patients (88%), but additional MT and angioplasty and/or stent implantation was necessary in 17 (20.2%) and 45 cases (53.6%), respectively. Clinical success was achieved in 74/84 cases (88%). The mortality rate at 1 year was 14.3%. The cumulative incidence of MAEs and MALEs at 12 months was 50% and 40.5%, respectively. After conducting multivariate analysis, history of Rutherford stage IIB (hazard ratio [HR], 3.64; 95% confidence interval [CI], 1.58–8.41; p = 0.0025), occlusion of the external iliac artery (HR, 27.52; 95% CI, 2.83–267.33; p = 0.0043), being a case of clinically unsuccessful thrombolysis (HR, 7.72; 95% CI, 2.48–23.10; p = 0.0004), and the presence of diabetes mellitus (HR, 2.18; 95% CI, 1.01–4.71; p = 0.047) were independent predictors of a high MAE mortality rate at 12 months. For MALEs, statistically significant differences were detected with the variables history of Rutherford stage IIB (HR, 4.30; 95% CI, 1.99–9.31; p = 0.0002) and external iliac artery occlusion (HR, 31.27; 95% CI, 3.47–282.23; p = 0.0022). Conclusions: Based on the short-term results of CDT, acute limb ischaemia can be successfully, safely, and effectively treated with catheter-directed thrombolytic therapy with radial, brachial, or femoral access. However, radial access is associated with fewer access site complications. A history of Rutherford stage IIB, occlusion of external iliac artery, unsuccessful thrombolysis, and the presence of diabetes mellitus were independently associated with an increased risk of MAEs. A history of Rutherford stage IIB and external iliac artery occlusion are independent predictors of MALEs.
1. Introduction
Acute lower limb ischaemia (ALI) is a sudden decrease in perfusion of the lower limb that entails a potential threat to the viability of the limb. Symptoms may manifest as pain at rest or, in more severe cases, as tissue damage in the form of ulcers and/or gangrene. Among the treatment options for endangered limbs are catheter-directed thrombolysis (CDT), mechanical thrombectomy (MT), and surgical revascularisation. ALI and its treatment carry the risk of complications such as ischaemia–reperfusion injury, compartment syndrome, systemic inflammatory response syndrome, multiple organ dysfunction syndrome, hyperkalaemia, or bleeding. Current advances in endovascular therapy enable prompt treatment of ALI; however, most treatment is performed via traditional femoral access sites. Alternatives to femoral access in ALI are the upper limb access sites of the radial and brachial arteries [1,2] or pedal access [3,4,5], but these access sites have many limitations in everyday clinical practice.
Our aim was to investigate the rate of complications related to the access site and to evaluate predictors of long-term outcomes of CDT and MT in lower limb arteries.
2. Materials and Methods
Between 2008 and 2019, consecutive patients with ALI were treated with CDT in a large community hospital. We collected the data of these patients and performed a retrospective analysis. We enrolled only patients who, based on the decision of the vascular team, underwent CDT. Based on the artery used as the access site, patients were divided into the RA (radial artery; n = 17), BA (brachial artery; n = 9), and FA (femoral artery; n = 58) groups. The operator selected the access site and all procedures were performed by five skilled operators.
Ad hoc informed consent for the procedure was obtained from all patients. The National Ethical Review Committee approved the study (reference number, BMEÜ/1639-1/2022/EKU) and all patients provided written informed consent prior to their inclusion in the study.
2.1. Procedural Endpoints
The primary endpoints of the study were “safety endpoints”: major adverse events (MAEs), major adverse limb events (MALEs), and occurrences of complications related to the access site. Secondary endpoints were “efficacy endpoints”: technical and clinical success, efficacy of the treatment, fluoroscopy time, radiation dose, procedure time, and the crossover rate to an alternative puncture site.
2.2. Inclusion and Exclusion Criteria
Inclusion criteria: Patients with ALI classified as Rutherford stage I, IIA, or IIB; acute lower extremity vascular occlusion confirmed based on emergency diagnostic angiography; clinic attendance starting within 14 days; age > 18 years; and had signed the patient information sheet and consent form were included.
Exclusion criteria: Patients were excluded if they had a non-viable lower limb (Rutherford stage III); did not sign the patient information sheet or the consent form; had haemodynamic instability; did not have significant vascular occlusion on diagnostic angiography; were not admitted to the clinic within 14 days; age < 18 years; or had inflammatory skin lesions at the planned penetration sites.
2.3. Antithrombotic and Thrombolytic Regimen
CDT involved the use of a recombinant tissue plasminogen activator administered directly into the artery. It consisted of an initial dose of 10 mg followed by a maintenance dose of 1 mg/h. Intravenous sodium heparin was administered to prevent catheter thrombosis. The heparin was administered as an initial bolus of 60 IU/kg and a maintenance dose of 1000 IU/h, adjusted based on the activated partial thromboplastin time.
Following the administration of an initial dose of 300 mg aspirin and 300 mg clopidogrel, individuals who underwent stenting procedures were prescribed a dual antiplatelet therapy regimen consisting of 100 mg aspirin and 75 mg clopidogrel daily for 2 months. Conversely, patients who solely underwent balloon angioplasty were prescribed lifelong aspirin therapy.
2.4. Catheter Directed Thrombolysis
CDT was performed after selective angiography over a 5F pigtail catheter. The CDT was always initiated after a guidewire transversal test was conducted (the lesion was passed with a 0.18-inch guidewire) over a multiport thrombolytic catheter. If a CDT therapy was initiated, a control angiography was performed 24 h after local administration of a thrombolytic drug. If the thrombus continued to impede or completely block the flow despite the use of thrombolysis, additional thrombus aspiration was conducted. Similarly, if the lesion was significantly stenosed or dissected, additional balloon angioplasty or stent implantation was performed (Figure 1). The choice of treatment varied based on the location of the occlusion, the extent of clot formation, and the aetiology.
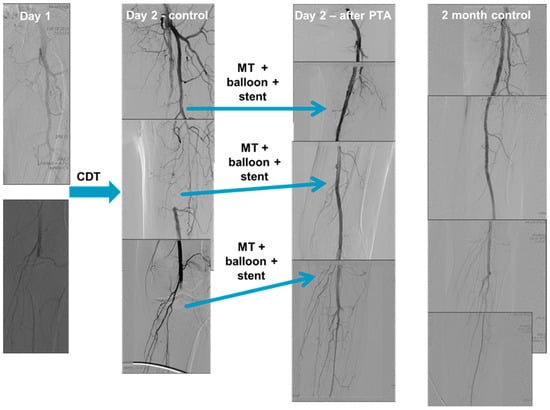
Figure 1.
Catheter-directed thrombolysis (CDT) performed via access from a radial artery. Selective angiography performed using a radial approach (over a 5F pigtail catheter) shows a left common femoral artery occlusion without distal run-off. (Day 1) A guidewire transversal test, in which the lesion was passed with an 0.18-inch guidewire, was conducted over a multiport thrombolytic catheter. CDT was then initiated. On the first postoperative day, control angiography shows incomplete thrombus resolution and distal embolisation. (Day 2—control) Mechanical thrombectomy, additional balloon angioplasty, and stent implantation was performed in the left superficial femoral artery and in the left popliteal artery. Control angiography shows successful recanalisation with acceptable flow in the below the knee arteries. (Day 2—after PTA). Abbreviations: CDT—catheter-directed thrombolytic therapy; MT—mechanical thrombectomy; PTA—percutaneous transluminal angioplasty.
In cases of thromboembolism, vascular surgery was the preferred treatment and the decision was reached after consultation among the members of the vascular team. In cases of atherothrombosis, CDT was the preferred treatment, and the vascular team also made this decision. Based on the above, only patients who underwent thrombolysis were included in our present study.
2.5. Definitions
2.5.1. Major Adverse Event
An MAE was evaluated by considering a combination of outcomes, including death, myocardial infarction, stroke, major amputation of the lower limb, and the need for repeat revascularisation procedures of the target vessel by percutaneous transluminal angioplasty or by arterial bypass graft surgery during the follow-up period.
2.5.2. Major Adverse Limb Event
A MALE was defined as either untreated loss of patency of the revascularisation, re-intervention on the revascularised segment, or major amputation (above or below the knee) of the revascularised limb.
2.5.3. Vascular Complication
Major vascular complications referred to a reduction in, or total loss of, the arterial pulse or the emergence of a pseudoaneurysm or arteriovenous fistula as identified during the patient’s follow-up examination. Minor vascular complications were characterised as haematomas that did not necessitate any specific intervention. These haematomas were limited to a size of 2 cm in diameter in the puncture areas of the radial or ulnar artery, or 5 cm in diameter in the puncture areas of the femoral or brachial arteries. A drop in the haemoglobin level of more than 3 g/dL was considered major bleeding, as was bleeding that required transfusion.
2.5.4. Technical Success
The successful outcome of a technical procedure occurred when a percutaneous transluminal angioplasty led to a residual stenosis of less than 30% while ensuring satisfactory anterograde blood flow. A suboptimal result was identified by a slow flow and/or a residual stenosis of between 30% and 50% after percutaneous transluminal angioplasty.
2.5.5. Clinical Success
The primary measure of clinical success involved observing an enhancement of at least one clinical category within the Rutherford classification [6]. Primary patency referred to the condition where a treated lesion remained open and unobstructed over time, without requiring any additional medical procedures such as angioplasty, surgery, or amputation. Limb salvage was the successful prevention of major amputation, preserving the affected limb. We also evaluated the treatment as a success if the functionality of the limb was maintained in the first 7 days and no major amputation occurred.
2.5.6. Access Site Crossover
If technical difficulties arose in connection with the intervention performed through the primary penetration site, or if performing the intervention from this puncture point was not possible, the use of a ‘crossover’ site was deemed necessary. That is, the puncture area was switched to another puncture area.
2.6. Follow-Up
All patients underwent a physical examination immediately after the procedure and every day during hospitalisation. In the third, sixth, and twelfth months after the intervention, a detailed clinical follow-up examination was performed on all patients.
2.7. Statistical Analysis
The unordered chi-squared test with a simulated p-value (107 replicates) was employed to evaluate categorical data. Pairwise comparisons were made using Fisher’s exact test adjusted according to the Benjamini–Hochberg method to account for multiple comparisons [7]. For ordered larger contingency tables, the ordered approximative general independence test (107 resamples) was employed. All continuous parameters showed non-normal distribution; therefore, they were described using the median and interquartile range. The three treatment groups were evaluated using the approximative Kruskal–Wallis’s test (107 resamples), using the Dunn’s test and the Holm adjustment as a post hoc test in cases of statistical significance. The null hypothesis was rejected if p was ≤0.025. All analyses were carried out with R version 4.3.1 (R Foundation for Statistical Computing, Vienna, Austria) using the additional packages coin 1.4-2, R companion 2.4.30, and Dunn test 1.3.5. All analyses were conducted on an intention-to-treat basis. Cox regression was performed using MedCalc version 22.016 (MedCalc Software Ltd., Ostend, Belgium) statistical software. p < 0.05 was considered statistically significant.
3. Results
Between 2008 and 2019, 84 consecutive patients fulfilling the inclusion criteria underwent CDT for ALI, and their data were analysed retrospectively. CDT was initiated using radial (RA group, n = 17), brachial (BA group, n = 9), and femoral (FA group, n = 58) approaches. The demographic and clinical data are summarised in Table 1.

Table 1.
Demographic and clinical data.
3.1. Angiographic and Procedural Data
The angiographic and procedural data are summarised in Table 2 and Table 3. CDT was technically successful in 74/84 patients (88%), but additional MT and angioplasty and/or stent implantation was necessary in 17 (20.2%) and 45 (53.6%) cases, respectively, to obtain good angiographic results. Clinical success was achieved in 74/84 cases (88%). Procedurally related factors were not statistically different in the subgroups (see Table 3) and hospitalisation time (15.9 ± 14.5 days vs. 7.7 ± 2.8 days vs. 11.5 ± 6 days) was also not statistically different among the three groups (p = ns).

Table 2.
Angiographic data.

Table 3.
Results.
3.2. Procedural Complications and 1-Year Follow-Up
The procedural complications and long-term follow-up data are summarised in Table 3 and Table 4. The cumulative incidence of MAEs at 12 months was 50%. The major amputation rate was 22.6% and the mortality rate 21.5% (regarding patients who have undergone major amputation). Among the major amputations performed, a significant proportion (73,7%) were femoral amputations. Four patients were identified as having stage IIA according to the Rutherford classification, while 10 had stage IIB. Crural amputations represented 26.3% of the overall number of amputations. Within this subset, four patients were classified as having stage IIA according to the Rutherford classification and one as having stage IIB. The overall rate of stroke was 9.5%: five (5.9%) cases of ischaemic stroke and three (3.5%) of haemorrhagic stroke, with a 50% mortality rate. The overall rate of major vascular complication was 9.5% (0%, 11.1%, and 12.1% in the RA, BA, and FA groups, respectively), with a 25% mortality rate.

Table 4.
Perioperative and long-term complications.
3.3. MAE and MALE Predictors
The adjusted variables used in the Cox regression model used to investigate MAEs and MALEs, which were considered together as the reference model, were entry site, Rutherford stage, target vessel, clinical success, additional procedure, and diabetes mellitus. In all cases, data from the 12-month follow-up period were taken into account during the analysis, and p < 0.05 was considered statistically significant.
Among the adjusted variables examined for MAEs, statistically significant differences were observed for Rutherford stage IIB (HR, 3.64; 95% CI, 1.58–8.41; p = 0.0025), occlusion at the level of the external iliac artery (HR, 27.52; 95% CI, 2.83–267.33; p = 0.0043), cases of clinically unsuccessful thrombolysis (HR, 7.72; 95% CI, 2.48–23.10; p = 0.0004), the presence of diabetes mellitus (HR, 2.18; 95% CI, 1.01–4.71; p = 0.047), and cases of radial penetration (HR, 0.27; 95% CI, 0.07–0.96; p = 0.0429; Table 5).

Table 5.
Cox proportional hazards regression, major adverse events.
In the case of MALEs, statistically significant differences were detected for the variables Rutherford stage IIB (HR, 4.30; 95% CI, 1.99–9.31; p = 0.0002) and external iliac artery occlusion (HR, 31.27; 95% CI, 3.47–282.23; p = 0.0022; Table 6).

Table 6.
Cox proportional hazards regression, major adverse limb events.
4. Discussion
This is the first study to compare the use of femoral, brachial, and radial access for the treatment of ALI. We demonstrated several important findings: (1) based on the short-term results, CDT was a safe and effective method to treat ALI; however, additional intervention was necessary in 73.8% of cases; (2) access site complications were very rare in the RA group; (3) long-term MAEs were frequent, despite CDT being successful; and (4) significant independent predictors of long-term MAEs and MALEs were identified.
ALI treatment encompasses various methods, including surgical interventions such as thromboembolectomy and bypass surgery, and endovascular techniques such as CDT, percutaneous thrombus aspiration, mechanical thrombectomy, angioplasty, and stent placement. A hybrid treatment approach that combines both surgical and endovascular therapies is also available.
According to the 2016 American Heart Association/American College of Cardiology (AHA/ACC) consensus guidelines for managing peripheral arterial disease, thrombectomy is indicated as ‘IIa’ in patients with ALI caused by embolism and whose limbs can still be saved [8]. Two major studies were published in the 1990s that proved the noninferiority of endovascular therapy over surgical thrombectomy. These were the Surgery or Thrombolysis in Lower Extremity Ischemia (STILE) and Thrombolysis Or Peripheral Artery Surgery (TOPAS) trials, which randomly assigned patients to arteriography and lysis therapy with urokinase versus arteriography and embolectomy or urgent bypass [9,10]. The TOPAS study showed that local thrombolysis with urokinase is associated with a higher rate of bleeding complications, but simultaneously reduces the need for open surgical interventions without significantly increasing the risk of amputation or death [10]. The data interpreted in the studies are reliable and the test results are well founded; however, in both studies, the majority of patients had stage I and IIA limb ischaemia, while stage IIB and III ischaemia occurred in less than 25% of patients.
The primary goal of CDT is to restore anterograde flow, clear the outflow tract of thrombus, minimise the level of amputation, and allow for further peripheral intervention without distal embolisation developing. MT can be used to supplement CDT. MT utilises the fusion of mechanical energy and thrombolytic infusion to actively disintegrate and dissolve the thrombus. MT enables quicker dissolution of clots compared to CDT, although it may also entail an increased risk of bleeding and the occurrence of distal embolisation [11].
In the past, CDT was associated with a longer treatment time (infusion of the thrombolytic), often wasting valuable days to achieve any degree of recanalisation. Nowadays, the time to perfusion can be significantly shortened using thrombolytic protocols, which have been accelerated by technical advances. In our study, we verified and confirmed that currently, CDT is an effective therapeutic intervention in ALI, as local thrombolytic therapy was technically and clinically successful in 88% of patients.
Advances in endovascular techniques are increasingly enabling ALI to be treated; however, most treatments are still performed via the traditional femoral access. Alternative entry points, such as brachial or radial artery punctures, can also be used [12,13]. The main disadvantages of transfemoral access are the high rate of vascular complications related to the puncture and the longer duration of hospitalisation [14]. Ultrasound-guided puncture might result in fewer vascular complications and avoidance of multiple punctures.
Compared to femoral penetration, using radial penetration offers the main advantages of a much lower rate of bleeding complications, greater comfort of the patient, enabling of rapid mobilisation, and shorter hospital stays [13,14]. Despite its many advantages, the anatomical and technical limitations of the radial approach have prevented it from being widely used and accepted as a penetration approach. The most important disadvantage of this approach is the difficulty in delivering devices to the lesion to be treated and the high crossover rate to the femoral access site [15]. Owing to technological improvements, the use of transradial access for endovascular interventions has become much more feasible [16]. One of the main advantages of radial penetration was confirmed by our present study: the overall rate of major vascular complications was 9.5% (0%, 11.1%, and 12.1% in the RA, BA, and FA groups, respectively), with a 25% mortality rate.
4.1. Acute and Long-Term Results of CDT
Our technical success rate of 88% is similar to the reported rates of previous studies investigating ALI and thrombolysis [10,17]. CDT shows high angiographic success in treating ALI; however, long-term outcomes are relatively poor, with a relatively high risk of MAEs (the cumulative incidence of MAEs at 12 months was 50%, with a 22.6% rate of major amputation). Potential confounding factors such as age and comorbidities may underlie the outcomes of CDT. In the present study, the comorbidities among the patient population and potential risk factors were clearly visible: the majority of patients had hypertension and were previous or active smokers, while approximately one third of the patients had diabetes or previous PTA.
Using multiple regression analysis enabled those factors that significantly increased the rate of MAEs during long-term follow-up to be determined. These risk factors were primarily a high initial Rutherford stage, a high degree of occlusion, diabetes mellitus present as a comorbidity, or failure of thrombolysis. Regarding the occurrence of MAEs, patients who underwent the intervention from a radial penetration site had a significant advantage compared to those who underwent the intervention, for example, from a femoral penetration site. Regarding MALEs, patients with Rutherford stage IIB and external iliac artery occlusion who underwent treatment fared worse than did those with Rutherford stage IIA or, for example, patients with superficial femoral artery occlusion.
4.2. Complications of CDT
Intracranial bleeding is the most serious, and often fatal, complication of CDT, despite therapy being initiated immediately. An urgent computed tomography scan of the skull, the immediate cessation of lysis, and the initiation of maximum supportive therapy are necessary if the patient’s neurological status is to be changed. However, even with the greatest care and maximum supportive therapy, the prognosis is very poor.
A published Cochrane meta-analysis assessed five trials with 1283 randomised patients comparing thrombolysis and surgery. The authors concluded that no significant difference in limb salvage or death at 30 days, 6 months, or 1 year existed between initial surgery and thrombolysis. However, major bleeding, stroke, and distal embolisation were more likely to be associated with thrombolysis than with thrombectomy [18]. This fact was confirmed by our present study, as the overall rate of stroke was 9.5% (five [5.9%] cases of ischaemic and three [3.5%] of haemorrhagic stroke), with a 50% mortality rate.
Another dreaded adverse event is major access site complications, which can increase the risk of mortality and the length of hospital stay and medical costs [19]. These complications comprise pseudoaneurysms or arteriovenous fistulae at the puncture site, or retroperitoneal haemorrhage, which requires immediate surgical intervention. The severity of these complications is confirmed by the results of the present study: the overall rate of major vascular complications was 9.5%, with a 25% intrahospital mortality rate.
Based on the above, one can conclude that close monitoring and physical examination of the patient is essential after the interventions have been performed.
4.3. Study Limitation
The primary limitation of the study was the nonrandomised, retrospective design. The small and unequal number of patients in each subgroup made extrapolation of their result over the entire population of ALI patients difficult.
5. Conclusions
According to the initial outcomes, acute limb ischaemia can be treated successfully and safely using radial, brachial, or femoral access sites; however, radial access is associated with fewer access site complications. Good patient outcomes depend on how quickly and effectively the arterial blood flow can be restored to the limb. Patients with greater ischaemic tissue damage (e.g., acute aortic occlusion) have much worse outcomes than those with segmental arterial occlusion have. Concerning long-term outcomes, MAEs are frequent despite CDT being conducted successfully. The reason for this could be the significant comorbidity of the patient population, the presence of a chronic component that frequently accompanies the acute clinic, and an initial high Rutherford stage.
Author Contributions
Conceptualisation, A.C., K.T., N.K., S.R., Z.V., B.B., F.Z.K., O.F.B., I.H. and Z.R.; methodology, A.C., I.H. and Z.R.; formal analysis, A.C. and Z.R.; investigation, A.C., K.T., N.K., S.R., Z.V., B.B. and Z.R.; resources, A.C. and Z.R.; data curation, A.C.; statistical analysis, A.C., F.Z.K., I.H. and Z.R.; writing—original draft preparation, A.C. and Z.R.; writing—review and editing, A.C. and Z.R.; visualisation, A.C. and Z.R.; supervision, Z.R. and B.B.; project administration, A.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Hungarian Medical Research Council, Scientific and Research Ethics Committee (reference number BMEÜ/1639-1/2022/EKU).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are contained within the article.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
| AHA | American Heart Association |
| ACC | American College of Cardiology |
| ALI | acute limb ischemia |
| BA | brachial artery |
| CDT | catheter-directed thrombolysis |
| CI | confidence interval |
| FA | femoral artery |
| HR | hazard ratio |
| MAE | major adverse event |
| MALE | major adverse limb event |
| MT | mechanical thrombectomy |
| PTA | percutaneous transluminal angioplasty |
| RA | radial artery |
| STILE | Surgery or Thrombolysis in Lower Extremity Ischemia |
| TOPAS | Thrombolysis Or Peripheral Artery Surgery |
References
- Shammas, N.W.; Radaideh, Q. A Combined Radial and Pedal Access to Treat a Flush Chronic Total Occlusion of the Superficial Femoral Artery in a Critical Limb Ischemia Patient. Open J. Cardiovasc. Surg. 2019, 11, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Ernst, S.; Fischbach, R.; Brochhagen, H.G.; Heindel, W.; Landwehr, P. Transbrachial thrombolysis, PTA and stenting in the lower extremities. Cardiovasc. Intervent. Radiol. 2003, 26, 516–521. [Google Scholar] [CrossRef] [PubMed]
- Bazan, H.A.; Le, L.; Donovan, M.; Sidhom, T.; Smith, T.A.; Sternbergh, W.C., 3rd. Retrograde pedal access for patients with critical limb ischemia. J. Vasc. Surg. 2014, 60, 375–381. [Google Scholar] [CrossRef] [PubMed]
- Kwan, T.W.; Shah, S.; Amoroso, N.; Diwan, R.; Makker, P.; Ratcliffe, J.A.; Lala, M.; Huang, Y.; Nanjundappa, A.; Daggubati, R.; et al. Feasibility and safety of routine transpedal arterial access for treatment of peripheral artery disease. J. Invasive Cardiol. 2015, 27, 327–330. [Google Scholar] [PubMed]
- Ruzsa, Z.; Nemes, B.; Bánsághi, Z.; Toth, K.; Kuti, F.; Kudrnova, S.; Berta, B.; Huettl, K.; Merkely, B. Transpedal access after failed anterograde recanalization of complex below-the-knee and femoropopliteal occlusions in critical limb ischemia. Catheter. Cardiovasc. Interv. 2014, 83, 997–1007. [Google Scholar] [CrossRef] [PubMed]
- Hanna, E.B.; Prout, D.L. J combined radial-pedal access strategy and radial-pedal rendezvous in the revascularization of complex total occlusions of the superficial femoral artery (the “No Femoral Access” Strategy). Endovasc. Ther. 2016, 23, 321. [Google Scholar] [CrossRef] [PubMed]
- Benjamini, Y.; Hochberg, Y. Controlling the false discovery rate: A practical and powerful approach to multiple testing. J. R. Stat. Soc. Ser. B 1995, 57, 289–300. [Google Scholar] [CrossRef]
- Norgren, L.; Hiatt, W.R.; Dormandy, J.A.; Nehler, M.R.; Harris, K.A.; Fowkes, F.G.; TASC II Working Group. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). J. Vasc. Surg. 2007, 45, S5–S67. [Google Scholar] [CrossRef] [PubMed]
- Weaver, F.A.; Comerota, A.J.; Youngblood, M.; Froehlich, J.; Hosking, J.D.; Papanicolaou, G. Surgical revascularization versus thrombolysis for nonembolic lower extremity native artery occlusions: Results of a prospective randomized trial. The STILE Investigators. Surgery versus Thrombolysis for Ischemia of the Lower Extremity. J. Vasc. Surg. 1996, 24, 513–521. [Google Scholar] [CrossRef] [PubMed]
- Ouriel, K.; Veith, F.J.; Sasahara, A.A. A comparison of recombinant urokinase with vascular surgery as initial treatment for acute arterial occlusion of the legs. Thrombolysis or Peripheral Arterial Surgery (TOPAS) Investigators. N. Engl. J. Med. 1998, 338, 1105–1111. [Google Scholar] [CrossRef] [PubMed]
- Lyden, S.P. Endovascular treatment of acute limb ischemia: Review of current plasminogen activators and mechanical thrombectomy devices. Perspect. Vasc. Surg. Endovasc. Ther. 2010, 22, 219–222. [Google Scholar] [CrossRef] [PubMed]
- Alvarez-Tostado, J.A.; Moise, M.A.; Bena, J.F.; Pavkov, M.L.; Greenberg, R.K.; Clair, D.G.; Kashyap, V.S. The brachial artery: A critical access for endovascular procedures. J. Vasc. Surg. 2009, 49, 378–385. [Google Scholar] [CrossRef] [PubMed]
- Staniloae, C.S.; Korabathina, R.; Coppola, J.T. Transradial access for peripheral vascular interventions. Catheter. Cardiovasc. Interv. 2013, 81, 1194–1203. [Google Scholar] [CrossRef]
- Siracuse, J.J.; Farber, A.; Cheng, T.W.; Raulli, S.J.; Jones, D.W.; Kalish, J.A.; Smeds, M.R.; Rybin, D.; Schermerhorn, M.L.; Vascular Quality Initiative. Common femoral artery antegrade and retrograde approaches have similar access site complications. J. Vasc. Surg. 2019, 69, 1160–1166. [Google Scholar] [CrossRef] [PubMed]
- Ruzsa, Z.; Bellavics, R.; Nemes, B.; Hüttl, A.; Nyerges, A.; Sótonyi, P.; Bertrand, O.F.; Hüttl, K.; Merkely, B. Combined transradial and transpedal approach for femoral artery interventions. JACC Cardiovasc. Interv. 2018, 11, 1062–1071. [Google Scholar] [CrossRef] [PubMed]
- Kang, W.Y.; Campia, U.; Ota, H.; Didier, R.J.; Negi, S.I.; Kiramijyan, S.; Koifman, E.; Baker, N.C.; Magalhaes, M.A.; Lipinski, M.J.; et al. Vascular access in critical limb ischemia. Cardiovasc. Revasc. Med. 2016, 17, 190–198. [Google Scholar] [CrossRef] [PubMed]
- Kashyap, V.S.; Gilani, R.; Bena, J.F.; Bannazadeh, M.; Sarac, T.P. Endovascular therapy for acute limb ischemia. J. Vasc. Surg. 2011, 53, 340–346. [Google Scholar] [CrossRef]
- Berridge, D.C.; Kessel, D.O.; Robertson, I. Surgery versus thrombolysis for initial management of acute limb ischaemia. Cochrane Database Syst. Rev. 2013, 6, CD002784. [Google Scholar] [CrossRef]
- Brener, M.I.; Bush, A.; Miller, J.M.; Hasan, R.K. Influence of radial versus femoral access site on coronary angiography and intervention outcomes: A systematic review and meta-analysis. Catheter. Cardiovasc. Interv. 2017, 90, 1093–1104. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).