Abstract
A primigravida 22-year-old woman, at a gestation of 23 weeks, experienced bleeding from a pial arteriovenous malformation (AVM) located in the right cerebellum. After interdisciplinary consensus and with the informed consent of the patient and her family, AVM embolization was performed. Complete occlusion of the AVM was achieved by embolization with PHIL (precipitating hydrophobic injectable liquid). The calculated dose in the uterus was less than 1 µSv, which represents a negligible risk of harmful effects on the fetus. She delivered a baby at 37 weeks of gestation by cesarean section without complications. No congenital disorders were diagnosed by standard screening methods until the age of the newborn was two years. The angiography protocol must be optimized to minimize the radiation dose. Adequate shielding protection of the uterus is important. Premature termination of pregnancy is not necessary. Multidisciplinary care of neurologists, neurosurgeons, interventional radiologists, anesthesiologists, neonatologists, and obstetricians is necessary.
Keywords:
arteriovenous malformation; rupture; embolization; pregnancy; radiation; dose; EVOH; PHIL; brain 1. Introduction
Brain arteriovenous malformations (bAVMs) are uncommon vascular lesions (the incidence is approximately 1 per 100,000 per year in unselected populations) composed of feeding arteries (usually enlarged), a nidus (with shunt), and draining veins. bAVMs are typically present in young adults with spontaneous intracranial hemorrhage, seizures, or headaches [1,2,3]. Brain arteriovenous malformations have been commonly regarded as congenital, but this suspected origin has been challenged by published reports of de novo bAVMs [4].
The prevalence rate of bAVMs is approximately 0.01–0.5%, and they generally present symptoms between 20 and 40 years of age, most commonly at 30 years of age, and equally affect men and women [5]. The location ratio of bAVMs is 85% vs. 15% for supratentorial (two-thirds superficial and one-third deep) vs. infratentorial [3].
The annual risk of bleeding from unruptured bAVMs was estimated from retrospective studies at 4%, but it has recently been reported in a range of 1–2.2% [6,7]. It was ≈2% in the observation arm of the ARUBA study [6]. The lifetime risk of hemorrhage from non-ruptured bAVMs can be simply approximated with the following formula: lifetime risk (%) = 105—the patient’s age in years [8]. The bleeding originates from the brain arteriovenous malformation itself or from the venous side [6]. The rebleeding rate is higher, especially in the first year after rupture, ranging from 6% to 15.8% [7]. Statistically significant risk factors for hemorrhage are previous hemorrhage, deep bAVM location, exclusive deep venous drainage, and associated aneurysm [2].
ICARUSS investigators positively confirmed a drainage vein diameter as a specific risk factor for AVM rupture with a cutoff ≥ 5 mm [9].
Compared to a nonpregnant period in women with AVMs, the potential risk of intracranial hemorrhage increases 3.27 times during pregnancy and puerperium [10]. Because of the high rate of rebleeding, the alarming maternal mortality rate from rebleeding (up to 28%), and the 14% fetal death rate, the treatment of ruptured bAVMs should not be delayed and must be actively managed [5]. The intervention of ruptured bAVMs is recommended within 2 weeks after initial bleeding in patients of gestational age < 34 weeks, while termination of pregnancy as soon as possible followed by timely intervention of ruptured bAVMs is practicable in patients of gestational age ≥ 34 weeks [11].
The main characteristics of brain AVMs are listed in Table 1.

Table 1.
Characteristics of brain AVMs.
2. Management of Radiation Dose Reduction
At zero doses, there is zero risk of harm. In general, the ALARA principle (As Low As Reasonably Achievable) assumes that exposure to radiation poses a risk. This fundamental principle is even more crucial to adhere to during pregnancy.
2.1. Basic Principles and Radiation Limits
The civil population is constantly exposed to radiation from natural sources. Today, the medical use of X-rays represents the largest source of man-made radiation. Selected radiation doses are listed in Table 2 [12,13].

Table 2.
List of radiation dose examples.
There is no definitive evidence to support the risk at all doses. This remains an active area of research. Depending on the study, approximately 100 mSv, 50 mSv, or 10 s mSv may be quoted as a level below which evidence is difficult to determine [14]. Better predictions of low dose/dose rate effects that are of great concern in the field of radiation protection can be reached by using the negative binomial linear-quadratic model variants [15].
The European Directive 2013/59/Euratom provides a relevant and beneficial practical impact on European radiology [16]. The dose limits for occupational exposure apply to the sum of annual occupational exposures of a worker from all authorized practices listed in Table 3 [17].

Table 3.
List of dose limits for professional workers.
Radiation Limit and Fetal Doses
The International Commission on Radiological Protection (ICRP) recommends that the maximum dose of radiation to the uterus during pregnancy be less than 100 mGy to minimize the teratogenic risks to the fetus [18,19].
The approximate fetal doses from radiological examinations are listed in Table 4 [20].

Table 4.
Approximate fetal doses from radiological examinations.
2.2. Radiation Dose Reduction and Protocol Optimization
It is extremely important to constantly train medical professionals on how to adequately reduce radiation associated with medical imaging techniques [21]. Operators must be familiar with the principles of how to reduce and measure radiation dose in fluoroscopically guided interventions [22,23,24,25,26,27,28,29] and protect themselves [30,31], especially pregnant women who are interventional radiologists [32]. Essential principles are listed in Table 5.

Table 5.
Protocol optimization to reduce the fetal dose.
An absorbed dose threshold to the patient’s brain of 0.5 Gy is exceeded quite often during cerebral embolization procedures, and optimizing the protocol is crucial. Brain doses are almost doubled when the field increases from 8 to 15 cm or more [33].
It is necessary to avoid or at least minimize abdominal fluoroscopy in pregnant patients. The fetal limit can be approached if the fluoroscopy time exceeds 7 min [19]. The shielding of the abdomen with a lead skirt with a lead equivalent of 0.5 mm must be used in the pregnant patient during neurointerventional procedures.
New Technologies
Spot fluoroscopy represents an innovative approach to adequately reducing radiation dose in neurointerventional procedures that led to a reduction of 50% of the total fluoroscopic dose-area product [34].
A new generation of 76 µm pixel high-resolution high-definition (hi-def) zoom mode was developed for use in interventional procedures that require superior image quality over a small field of view [35].
3. Embolization Techniques
Endovascular treatment of brain arteriovenous malformations has evolved considerably over the last few decades. Adaptively, it represents an alternative therapy to and not only a useful adjuvant technique to conventional neurosurgery.
Enormous progress has been made in the development of liquid embolic materials and microcatheters. New polymers enable better penetration of an AVM nidus and a more excessive rate of complete AVM occlusion. Current commercially available liquid embolic materials are listed in Table 6.

Table 6.
List of liquid embolic material.
The availability of detachable microcatheters optionally allows for long-time injection of embolic material. The distal tip (1.5 to 5 cm) of these microcatheters can be left naturally in the access vessel, and the proximal part of the catheter is carefully removed at the end of the treatment procedure. The unique combination of the new embolic material and the detachable microcatheter typically allows for the performing of control angiography during the complex procedure. The injection of embolic material can be interrupted and continued several times as needed.
New imaging techniques are highly needed for the selection of the optimal treatment strategy, a more precise visualization of the origin of the main draining vein of the bAVM, and the depiction of more accurate intranidal aneurysms [36,37].
3.1. Transarterial Embolization
Endovascular embolization by the transarterial approach is preferred in most bAVMs as a conventional technique. The purpose of this technique is to reduce intranidal pressure before occlusion of the drainage vein. Such embolization can be used as a single therapeutic procedure or as neoadjuvant therapy prior to microsurgery or stereotactic radiosurgery.
A possible combination with microsurgical resection can also be used for grade III–V bAVMs as well. A high rate of total obliteration was achieved: 96.8% (in 30/31) was achieved with relatively low rates of permanent morbidity and mortality [38].
Specific modifications of the transarterial technique traditionally represent the plug technique, the pressure cooker technique, the occlusion balloon technique, and multiple catheter techniques.
3.1.1. Plug Technique and Prolonged Intranidal Injection
The plug mitigates the potential risk of backflow and catheter entrapment, thus the “reverse plug then push” technique, allowing the operator to inject higher volumes of embolic material at greater injection rates [39].
Detachable microcatheters allow for long-time injection. A higher rate (51%; 179/350) of AVM obliteration was achieved with prolonged intranidal injection compared to the technique previously used [40].
3.1.2. Pressure Cooker Technique
The pressure cooker technique was designed to block the backflow of embolic material to the nontarget artery by quickly creating an antireflux plug by trapping the detachable part of the microcatheter with coils and glue [41].
The modified coil-protected transarterial n-butyl cyanoacrylate injection technique using a single microcatheter to typically prevent reflux can be efficiently preferred when rapid hemostasis and short procedure time are required in hemodynamically unstable conditions [42].
3.1.3. Occlusion Balloon Technique
The dual-lumen balloon catheter technique was uniquely created to minimize the necessary procedure and fluoroscopy times to promptly form an adequate proximal plug that allows the forwarding of nidal penetration while preventing reflux and nontargeted embolization [43].
The present generation of modern devices (the Scepter Mini) can be additionally handled for superselective flow arrest and navigation support due to its ability to be correctly placed on small-diameter feeders [44].
Balloon catheters also play a substantial role in AVM embolization. Inflation of a compliant balloon in the parent artery immediately after the origin of the feeder is a simple but effective maneuver during microcatheter navigation [45].
3.1.4. Multiple Catheter Technique
Occlusion of the draining veins before complete exclusion of the nidus typically carries a procedural risk of bleeding. Two or more arterial feeders can be catheterized and simultaneously embolized to achieve total embolization of the nidus before reaching the venous drainage [46,47].
3.2. Transvenous and Combined Techniques
Unlike the transarterial approach, curative embolization of AVMs can be achieved more easily with a transvenous approach. The proposed indications for this approach include a small (diameter < 3 cm) and compact AVM nidus, deep AVM location, hemorrhagic presentation, single draining vein, lack of an accessible arterial pedicle, exclusive arterial supply by perforators, and en passage feeding arteries [48].
Transvenous retrograde AVM nidus sclerotherapy under controlled hypotension (TRENSH) technique using temporary systemic hypotension with or without temporary occlusion of the main arterial feeders was first conceptualized by Massoud and Hademenos [49]. Extensive knowledge of the venous anatomy is crucial to prevent some of the potential complications of the procedure [50,51].
Hudak established a novel strategy of combined transarterial and transvenous embolization with a new liquid embolic agent based on pol-urethane. A combined transarterial and transvenous embolization technique was carefully applied for 46 high-grade bAVMs. Patients experienced subarachnoid or intracerebral hemorrhage (29/46), drug-resistant epilepsy, and/or severe focal deficit (17/46). The principal author precisely measured the local arterial and venous pressure of the nidus during the specific procedure. Transarterial embolization was initially used at the beginning of the complex procedure. After a sufficient reduction in the inflow to the nidus, temporary controlled systemic hypotension was typically induced. At the last moment, the new liquid embolic agent performed a proper transvenous penetration of the nidus. Despite the exclusive inclusion of high-grade bAVMs in the published study, the contributing author achieved complete occlusion of AVMs in 20 specific patients. In the remaining 26 cases, an occlusion rate of 80–90% was reasonably achieved [52]. The fundamental limitation of this study remains the fact that the embolic material used is commercially unavailable.
In most published data, the transvenous approach is typically used in extraordinary cases with the infeasibility of arterial embolization, including supply by tiny perforating arteries, feeders ‘in passage’, or no clear arterial pedicle, and/or in combination with other arterial approaches where the intention of the intervention was endovascular cure. There was an exceedingly higher rate of complete AVM obliteration (38/41; 92.6%) and excellent functional outcomes (0% procedure-related mortality and 2.5% overall mortality) in patients with ruptured and unruptured AVMs treated with transvenous embolization in another prospective study. The mean size of the AVM nidus was 2.8 ± 1.2 cm, and low Spetzler-Martin grade AVMs comprised 41.5% of the lesions. Most of the patients (23/41; 56%) were treated in one session. The new Dyna 4D technique was incorporated into the preprocedural analysis. The distinguished authors slowly injected Onyx and tolerated a maximum reflux of 3 cm. After completion of the operative procedure, the microcatheter was typically cut at the optimal level of the jugular sheath [53].
In the review of the literature of 13 studies (69 patients with 70 AVMs) on transvenous embolization, the complete AVM obliteration rate was reported in 93% of specific cases [48].
The transvenous retrograde pressure cooker technique using coils and n-butyl-2-cyanoacrylate as a venous plug can be curative if the main inclusion criteria (AVM < 3 cm and single main drain vein) are accepted without reserve [54].
Solely transvenous embolization can be used in selected small-sized ruptured bAVMs. Fusion of magnetic resonance imaging and 3D angiography is helpful in controlling and fully achieving bAVM penetration by the embolic agent [55].
Selective temporary flow arrest during transvenous endovascular embolization (TFATVE) represents a novel adaptation of the transvenous approach, which employs hyper-compliant balloons intraarterially for the careful blocking of arterial feeders at the time of injection of ethylene-vinyl copolymer to reduce intranidal pressure and increase nidus occlusion rates [56].
Modern dual microcatheterization techniques with arterial and/or venous access, graciously according to angioarchitecture, was curative for low-grade Spetzler-Martin (SM I vs. II was 22% vs. 78%) bAVMs in 95%. More than 60% of prospective patients had ruptured AVMs [57].
Combined embolization therapy appears to be safe and potentially curative for certain deep AVM, e.g., in the basal ganglia, insula, and thalamus. Such a specific location is extremely demanding for all treatment techniques, and microsurgery might not be indicated. Complication rates that may, fortunately, reach radiosurgery profiles were demonstrated in a cohort study of 22 patients. A single transarterial approach was used precisely in nine (41%) unique cases, double catheterization in four (18%) cases, and the transvenous approach was required in eight (36%) cases. The mean size of the AVM was 2.98 ± 1.28 cm, and the mean number of sessions was 2.1 per patient. Most of the patients had cerebral hemorrhage (18/21, 82%), and three (14%) patients had a deteriorated neurological state (modified Rankin Scale > 2) at presentation. Sixty-eight percent of ruptured AVMs had a size ≤ 3 cm [58].
The ongoing study of the transvenous approach for the treatment of cerebral arteriovenous malformations (TATAM) was designed to adequately test the hypothesis that transvenous embolization is superior to transarterial embolization for obliteration of arteriovenous malformations [59].
4. Case
A primigravida 22-year-old female with no medical history, at a gestation of 23 weeks, experienced bleeding from a pial arteriovenous malformation (AVM) located in the right cerebellum. She presented with acute-onset headache with accompanying meningeal and cerebellar syndrome, nausea, and vomiting. The patient underwent magnetic resonance imaging, which confirmed bleeding from the right cerebellar AVM.
Less than 2% of infants <24 weeks’ gestation and approximately half of infants from 24 to 27 weeks’ gestation survived to discharge home from the neonatal intensive care unit [60]. Compared to a nonpregnant period in women with AVMs, the potential risk of intracranial hemorrhage increases 3.27 times during pregnancy and puerperium [10]. Because of the high rate of rebleeding, the alarming maternal mortality rate from rebleeding (up to 28%), and the 14% fetal death rate, the treatment of ruptured bAVMs should not be delayed and must be actively managed [5]. Surgical treatment of posterior fossa AVMs is associated with a higher rate of complications. Most posterior fossa AVMs are associated with an increased hemorrhage rate. Thus, they are a predictor of a poor outcome and should be treated even if unruptured to maintain good neurological function [61]. The potential risk of maternal blood pressure instability during surgery may negatively affect the fetus. Cerebellar location and deep venous drainage are predictors of hemorrhage. Endovascular embolization is useful and safe for infratentorial AVMs [62].
All the mentioned arguments were discussed in detail during the interdisciplinary meeting. After interdisciplinary consensus and with the informed consent of the patient and her family, AVM embolization was performed. The procedure was performed under general anesthesia. The abdominal area of the patient was protected with the shielding of a lead skirt with a 0.5 mm lead equivalency.
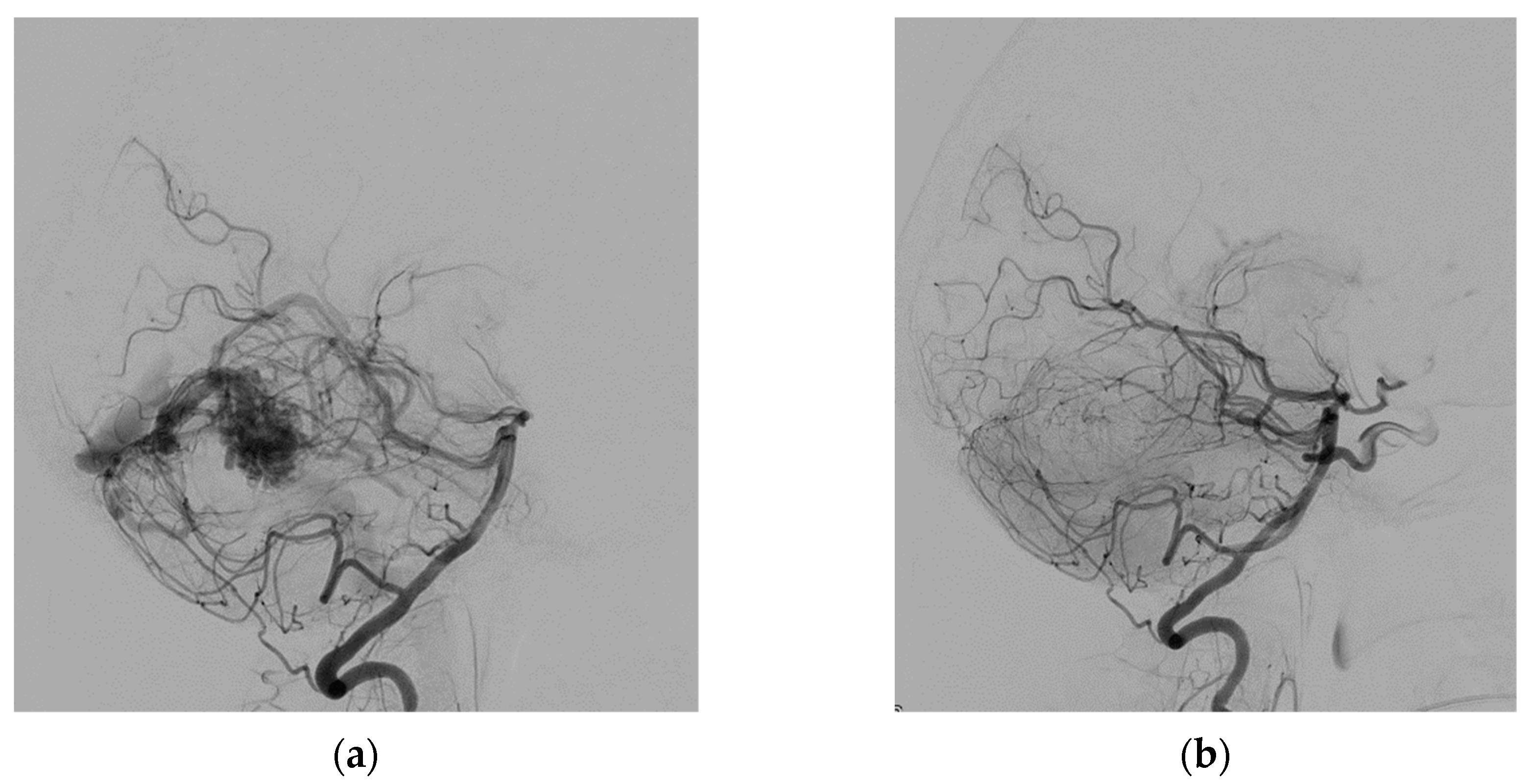
The right common femoral artery was punctured under ultrasound guidance, and a 6F short sheath was placed by the Seldinger technique. The patient was not heparinized. Over the guidewire, the sheath was replaced by a 6F 80 cm long introducer, which was placed in the aortic arch without the use of fluoroscopy. Fluoroscopy was used only in the head and neck area of the patient. The procedure continued by positioning the introducer into the left subclavian artery. Then a 6F guiding catheter was advanced and positioned coaxially into the left vertebral artery. All catheters were flushed continuously with saline solution. The left vertebral artery angiogram confirmed the pial AVM located in the right cerebellum, which was supplied by three branches of the right superior cerebral artery and drain into the straight sinus (Figure 1). Apollo microcatheters (ev3 Neurovascular, Irvine, CA, USA), with a 3 cm long detachable tip length, were navigated into three supplying arteries by guidewires: Hybrid 008.J and Hybrid 007.J (Balt, Montmorency, France), Synchro-10/300 (Stryker Neurovascular, Fremont CA, USA), and Asahi 008/300 (Asahi Intecc, Aichi, Japan). Three feeding arteries were embolized one by one with 25% liquid embolic material PHIL (MicroVention, Tustin, CA, USA) in amounts of 1.55, 0.45, and 1.5 mL. The complete embolization of the AVM was achieved at the end of the procedure (Figure 1). The total procedure time was 1 h and 50 min. The total amount of Visipaque 320 iso-osmolar iodine contrast medium (GE Healthcare, Oslo, Norway) applied to the patient was 54.7 mL.

Figure 1.
Angiogram of the left vertebral artery (lateral view) before (a) and after (b) AVM embolization.
The Allura Clarity biplane interventional X-ray system (Philips, The Netherlands) was used. A low X-ray dose level mode was selected except for the time of critical embolization moments. A maximum of 12.5 frames per second fluoroscopy rate was used. The total fluoroscopy time was 33 min and 20 s. The dose in the uterus, calculated by the Monte Carlo program for calculating patient doses in medical X-ray examinations, PCXMC 2.0 software version, was less than 1 µSv. She delivered a baby at 37 weeks of gestation by cesarean section without complications. No congenital disorders were diagnosed by standard screening methods until the age of the newborn was two years. The patient recovered without a focal neurological deficit and returned to her normal life. The follow-up magnetic resonance confirmed total AVM occlusion.
5. Discussion
Ruptured pial AVM in pregnancy is a rare but extraordinarily complex situation, associated with high maternal and fetal mortality [5,11]. Most bAVMs occur in the supratentorial region [11], but, in our case, the AVM was located in the infratentorial region. This location of the AVM is usually more difficult to treat surgically. AVMs of the posterior fossa brain are twice as likely to cause hemorrhage compared to supratentorial AVMs. Cerebellar location and deep venous drainage are predictors of hemorrhage. Endovascular embolization is useful and safe for infratentorial AVMs [62]. Three feeding arteries were embolized one by one with liquid embolic material PHIL 25% in our case.
The International Commission on Radiological Protection (ICRP) recommends that the maximum dose of radiation to the uterus during pregnancy be less than 100 mGy to minimize the teratogenic risks to the fetus [18,19]. Extremely limited information on the dose of fetal radiation during embolization is available in the literature. Asano et al. reported an exposure level of the uterus of 0.14 mGy [63]. Although three feeding branches were embolized in our case in one session to achieve complete occlusion of the AVM, the dose in the uterus was less than 1 µSv. The fetal dose can be close to zero with proper shielding, and premature termination of the pregnancy is not necessary. The dose achieved in our case represents a negligible risk of harmful effects on the fetus.
Nagayama et al. reported an average exposure dose to the abdominal surface in the presence of lead sheets during stereotactic radiosurgery of 14.05 mGy, and the fetus was exposed to a radiation dose of 8.26 mGy [64]. Radiosurgery does not reduce the risk of rebleeding immediately after application. Radiosurgery has a limited indication for the treatment of ruptured AVMs in pregnancy. Yu reported that fetal radiation doses approximately corresponded to 0.01% of the maximum tumor dose in a pregnant patient who underwent stereotactic radiosurgery with a gamma knife [65].
Surgery must be indicated in active hydrocephalus requiring shunting, associated with signs of imminent herniation, progressive neurological deficit, or both [66].
Visipaque 320 (iodixanol) is not contraindicated in pregnancy [67]. Only 54.7 mL of iso-osmolar iodine contrast media and 3.5 mL of a new generation of liquid embolic material, precipitating the hydrophobic injectable liquid (PHIL) embolic agent, were applied. She delivered a baby at 37 weeks of gestation by cesarean section without complications. No congenital disorders were diagnosed by standard screening methods until the age of the newborn was two years. No teratogenic effects were observed. The patient recovered completely.
Different embolic materials were used for embolization during pregnancy, including NBCA, Glubran, and Onyx—Table 7. The iodine-based embolic material PHIL was selected for use in our case because of its unique ability to penetrate the AVM nidus and create fewer artifacts compared to tantalum. PHIL is believed to flow forward rather than like a column and with less lava-like behavior with precipitation from the outside to the inside [68].

Table 7.
List of publications reporting embolization of bAVMs during pregnancy.
There are no definitive guidelines on how to properly treat ruptured bAVMs during pregnancy. Only a few authors report the radiation dose to the fetus, which is a limit to creating a comparison group. Our center reports only one case.
6. Conclusions
There are no definitive guidelines on how to properly treat ruptured bAVMs in pregnancy. The decision is challenging due to its rarity. Patients may benefit from early therapy due to a higher rate of excessive rebleeding during pregnancy. The purpose of treatment is to preserve the life of the mother as well as the viability of the fetus. Limited data on the dose of fetal radiation during embolization are published, but the available data are acceptable and smaller compared to radiosurgery. Embolization of ruptured AVMs during pregnancy can be used alone as a curative treatment or as an essential part of therapeutic management. Embolization of ruptured AVMs during pregnancy is a feasible treatment technique. The angiography protocol must be optimized to minimize the radiation dose. Adequate shielding protection of the uterus is important. In our case, the calculated dose in the uterus was less than 1 µSv, which represents a negligible risk of harmful effects on the fetus. Premature termination of pregnancy is not necessary. Multidisciplinary care involving neurologists, neurosurgeons, interventional radiologists, anesthesiologists, neonatologists, and obstetricians is necessary.
Author Contributions
K.Z.: conceptualization, writing—original draft preparation; D.Š., B.K., E.K., J.Z. and N.K.: review and editing. All authors have read and agreed to the published version of the manuscript.
Funding
This publication was created thanks to the support under the Operational Program Integrated Infrastructure for the project: TENSION—Complementary project, IMTS: 313011W875, co-financed by the European Regional Development Fund.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of Etická komisia Univerzitnej nemocnice Martin—Ethical committee of University Hospital Martin (EK UNM 10/2023).
Informed Consent Statement
Informed consent was obtained from the patient and family members.
Data Availability Statement
Data are available from the authors upon reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Al-Shahi, R.; Warlow, C. A systematic review of the frequency and prognosis of arteriovenous malformations of the brain in adults. Brain 2001, 124, 1900–1926. [Google Scholar] [CrossRef]
- Derdeyn, C.P.; Zipfel, G.J.; Albuquerque, F.C.; Cooke, D.L.; Feldmann, E.; Sheehan, J.P.; Torner, J.C.; American Heart Association Stroke Council. Management of Brain Arteriovenous Malformations: A Scientific Statement for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke 2017, 48, e200–e224. [Google Scholar] [CrossRef]
- Gaillard, F.; Weerakkody, Y. Brain Arteriovenous Malformation. Reference Article. Available online: Radiopaedia.org (accessed on 6 February 2022). [CrossRef]
- Dogan, S.N.; Bagcilar, O.; Mammadov, T.; Kizilkilic, O.; Islak, C.; Kocer, N. De Novo Development of a Cerebral Arteriovenous Malformation: Case Report and Review of the Literature. World Neurosurg. 2019, 126, 257–260. [Google Scholar] [CrossRef] [PubMed]
- Lv, X.; Li, Y. The clinical characteristics and treatment of cerebral AVM in pregnancy. Neuroradiol. J. 2015, 28, 385–388. [Google Scholar] [CrossRef] [PubMed]
- Mohr, J.P.; Parides, M.K.; Stapf, C.; Moquete, E.; Moy, C.S.; Overbey, J.R.; Salman, R.A.-S.; Vicaut, E.; Young, W.L.; Houdart, E.; et al. Medical management with or without interventional therapy for unruptured brain arteriovenous malformations (ARUBA): A multicentre, non-blinded, randomised trial. Lancet 2014, 383, 614–621. [Google Scholar] [CrossRef]
- Can, A.; Gross, B.A.; Du, R. The natural history of cerebral arteriovenous malformations. Handb. Clin. Neurol. 2017, 143, 15–24. [Google Scholar] [CrossRef]
- Ogilvy, C.S.; Stieg, P.E.; Awad, I.; Brown, R.D., Jr.; Kondziolka, D.; Rosenwasser, R.; Young, W.L.; Hademenos, G.; Special Writing Group of the Stroke Council, American Stroke Association. AHA Scientific Statement: Recommendations for the management of intracranial arteriovenous malformations: A statement for healthcare professionals from a special writing group of the Stroke Council, American Stroke Association. Stroke 2001, 32, 1458–1471. [Google Scholar] [CrossRef] [PubMed]
- de Castro-Afonso, L.H.; Vanzim, J.R.; Trivelato, F.P.; Rezende, M.T.; Ulhôa, A.C.; Chodraui-Filho, S.F.; Mattos, L.G.D.A.; Mounayer, C.; Nakiri, G.S.; Colli, B.O.; et al. Association between draining vein diameters and intracranial arteriovenous malformation hemorrhage: A multicentric retrospective study. Neuroradiology 2020, 62, 1497–1505. [Google Scholar] [CrossRef]
- Lee, S.; Kim, Y.; Navi, B.B.; Abdelkhaleq, R.; Salazar-Marioni, S.; Blackburn, S.L.; Bambhroliya, A.B.; Lopez-Rivera, V.; Vahidy, F.; I Savitz, S.; et al. Risk of intracranial hemorrhage associated with pregnancy in women with cerebral arteriovenous malformations. J. NeuroInterv. Surg. 2021, 13, 707–710. [Google Scholar] [CrossRef]
- Zhong, Z.; Ni, H.; Zhu, J.; Jiang, H.; Hu, J.; Lin, D.; Bian, L. Management of Acute Hemorrhage Caused by Cerebral Arteriovenous Malformation During Pregnancy–Case Series and Literature Review. World Neurosurg. 2021, 152, e688–e699. [Google Scholar] [CrossRef]
- Health Risks. Available online: https://www.epa.ie/environment-and-you/radiation/radiation-exposure-and-your-health/health-risks/ (accessed on 12 February 2022).
- UNSCEAR 2000 REPORT Vol. I. SOURCES AND EFFECTS OF IONIZING RADIATION. Available online: http://www.unscear.org/unscear/en/publications/2000_1.html (accessed on 12 February 2022).
- Walsh, C. Interpretation of risk for low dose radiation exposures: Inconsistencies, philosophical problems and fallacies. J. Radiol. Prot. 2020, 40, 646–653. [Google Scholar] [CrossRef] [PubMed]
- Shuryak, I.; Cornforth, M.N. Accounting for overdispersion of lethal lesions in the linear quadratic model improves performance at both high and low radiation doses. Int. J. Radiat. Biol. 2021, 97, 50–59. [Google Scholar] [CrossRef] [PubMed]
- European Council Directive. 2013/59/Euratom on basic safety standards for protection against the dangers arising from ex-posure to ionising radiation and repealing directives 89/618/Euratom, 90/641/ Euratom, 96/29/Euratom, 97/43/Euratom and 2003/122/Euratom. Off. J. Eur. Union 2014, L13, 1–73. [Google Scholar]
- European Society of Radiology (ESR). Summary of the European Directive 2013/59/Euratom: Essentials for health professionals in radiology. Insights Imaging 2015, 6, 411–417. [Google Scholar] [CrossRef] [PubMed]
- Wrixon, A.D. New ICRP recommendations. J. Radiol. Prot. 2008, 28, 161–168. [Google Scholar] [CrossRef]
- ICRP. Publication 84: Pregnancy and medical radiation. Ann. ICRP 2000, 30, 1–43. Available online: https://journals.sagepub.com/doi/pdf/10.1177/ANIB_30_1 (accessed on 20 February 2022).
- Allisy-Roberts, P.J.; Williams, J. Farr’s Physics for Medical Imaging, 2nd ed.; Elsevier Health Sciences: Amsterdam, The Netherlands, 2008. [Google Scholar] [CrossRef]
- Ploussi, A.; Efstathopoulos, E.P.; Brountzos, E. The Importance of Radiation Protection Education and Training for Medical Professionals of All Specialties. Cardiovasc. Interv. Radiol. 2021, 44, 829–834. [Google Scholar] [CrossRef]
- Paulo, G.; Bartal, G.; Vano, E. Radiation Dose of Patients in Fluoroscopically Guided Interventions: An Update. Cardiovasc. Interv. Radiol. 2021, 44, 842–848. [Google Scholar] [CrossRef]
- Rehani, M.M.; Miller, D.L.; Baliyan, V. High-Dose Fluoroscopically Guided Procedures in Patients: Radiation Management Recommendations for Interventionalists. Cardiovasc. Interv. Radiol. 2021, 44, 849–856. [Google Scholar] [CrossRef]
- Ploussi, A.; Brountzos, E.; Rammos, S.; Apostolopoulou, S.; Efstathopoulos, E.P. Radiation Exposure in Pediatric Interventional Procedures. Cardiovasc. Interv. Radiol. 2021, 44, 857–865. [Google Scholar] [CrossRef]
- Torresin, A.; Evans, S.; Lizio, D.; Pierotti, L.; Stasi, M.; Salerno, S. Practical recommendations for the application of DE 59/2013. Radiol. Med. 2019, 124, 721–727. [Google Scholar] [CrossRef] [PubMed]
- Cornacchia, S.; Errico, R.; La Tegola, L.; Maldera, A.; Simeone, G.; Fusco, V.; Niccoli-Asabella, A.; Rubini, G.; Guglielmi, G. The new lens dose limit: Implication for occupational radiation protection. Radiol. Med. 2019, 124, 728–735. [Google Scholar] [CrossRef] [PubMed]
- Guglielmi, G.; Pinto, A.; Salerno, S. Editorial from guest editors current Euratom legislation (DE 59/2013): New patient management in radiation protection. Radiol. Med. 2019, 124, 711–713. [Google Scholar] [CrossRef]
- Loose, R.; Wucherer, M. How to Measure/Calculate Radiation Dose in Patients? Cardiovasc. Interv. Radiol. 2021, 44, 835–841. [Google Scholar] [CrossRef]
- Bohrer, E.; Schäfer, S.B.; Krombach, G.A. Die neue Strahlenschutzgesetzgebung—Teil 1: Änderungen für die arbeitstägliche Routine in der Radiologie [The new radiation protection legislation-part 1: Modifications in radiology for the workflow in clinical routine]. Radiologe 2020, 60, 721–728. [Google Scholar] [CrossRef] [PubMed]
- Bartal, G.; Vano, E.; Paulo, G. Get Protected! Recommendations for Staff in IR. Cardiovasc. Interv. Radiol. 2021, 44, 871–876. [Google Scholar] [CrossRef]
- Wojcik, A.; Harms-Ringdahl, M. Radiation protection biology then and now. Int. J. Radiat. Biol. 2019, 95, 841–850. [Google Scholar] [CrossRef]
- Englander, M.J.; Ghatan, C. Radiation and the Pregnant IR: Myth versus Fact. Cardiovasc. Interv. Radiol. 2021, 44, 877–882. [Google Scholar] [CrossRef]
- Sanchez, R.; Vano, E.; Fernández, J.; Moreu, M.; Lopez-Ibor, L. Brain Radiation Doses to Patients in an Interventional Neuroradiology Laboratory. AJNR Am. J. Neuroradiol. 2014, 35, 1276–1280. [Google Scholar] [CrossRef]
- Borota, L.; Jangland, L.; Åslund, P.-E.; Ronne-Engström, E.; Nyberg, C.; Mahmoud, E.; Sakaguchi, T.; Patz, A. Spot fluoroscopy: A novel innovative approach to reduce radiation dose in neurointerventional procedures. Acta Radiol. 2017, 58, 600–608. [Google Scholar] [CrossRef]
- Nagesh, S.V.S.; Vakharia, K.; Waqas, M.; Fennell, V.S.; Atwal, G.S.; Shallwani, H.; Bednarek, D.R.; Davies, J.M.; Snyder, K.V.; Mokin, M.; et al. High-Definition Zoom Mode: A High Resolution X-ray Microscope for Neurointerventional Treatment Procedures. J. Neuroimaging 2019, 29, 565–572. [Google Scholar] [CrossRef] [PubMed]
- Clarençon, F.; Maizeroi-Eugène, F.; Maingreaud, F.; Bresson, D.; Ayoub, D.; Sourour, N.-A.; de Champfleur, N.M.; Chiras, J.; Yardin, C.; Mounayer, C. Interest of convex spherical anamorphosis in better understanding of brain AVMs’ angioarchitecture. J. NeuroInterv. Surg. 2016, 8, 959–964. [Google Scholar] [CrossRef] [PubMed]
- Keil, F.; Bergkemper, A.; Birkhold, A.; Kowarschik, M.; Tritt, S.; Berkefeld, J. 4D Flat Panel Conebeam CTA for Analysis of the Angioarchitecture of Cerebral AVMs with a Novel Software Prototype. AJNR Am. J. Neuroradiol. 2022, 43, 102–109. [Google Scholar] [CrossRef]
- Kocer, N.; Kandemirli, S.G.; Dashti, R.; Kizilkilic, O.; Hanimoglu, H.; Sanus, G.Z.; Tunali, Y.; Tureci, E.; Islak, C.; Kaynar, M.Y. Single-stage planning for total cure of grade III–V brain arteriovenous malformations by embolization alone or in combination with microsurgical resection. Neuroradiology 2019, 61, 195–205. [Google Scholar] [CrossRef] [PubMed]
- Durst, C.R.; Starke, R.M.; Gaughen, J.; Evans, A.J. A method for complete angiographic obliteration of a brain arteriovenous malformation in a single session through a single pedicle. J. Clin. Neurosci. 2015, 22, 391–395. [Google Scholar] [CrossRef]
- Saatci, I.; Geyik, S.; Yavuz, K.; Cekirge, H.S. Endovascular treatment of brain arteriovenous malformations with prolonged intranidal Onyx injection technique: Long-term results in 350 consecutive patients with completed endovascular treatment course. J. Neurosurg. 2011, 115, 78–88. [Google Scholar] [CrossRef]
- Chapot, R.; Stracke, P.; Velasco, A.; Nordmeyer, H.; Heddier, M.; Stauder, M.; Schooss, P.; Mosimann, P.J. The Pressure Cooker Technique for the treatment of brain AVMs. J. Neuroradiol. 2014, 41, 87–91. [Google Scholar] [CrossRef]
- Nishiyama, T.; Yabuta, M.; Ogawa, R.; Kurihara, Y. n-Butyl Cyanoacrylate Embolization with Coil Protection to Prevent Reflux: A Modified Pressure Cooker Technique Using a Single Microcatheter. J. Vasc. Interv. Radiol. 2022, 33, 721–724. [Google Scholar] [CrossRef]
- Spiotta, A.M.; James, R.F.; Lowe, S.R.; Vargas, J.; Turk, A.S.; Chaudry, M.I.; Bhalla, T.; Janjua, R.M.; Delaney, J.J.; Quintero-Wolfe, S.; et al. Balloon-augmented Onyx embolization of cerebral arteriovenous malformations using a dual-lumen balloon: A multicenter experience. J. NeuroInterv. Surg. 2015, 7, 721–727. [Google Scholar] [CrossRef]
- Vollherbst, D.F.; Chapot, R.; Wallocha, M.; Saatci, I.; Cekirge, S.; Rouchaud, A.; Mounayer, C.; Kocer, N.; Kizilkilic, O.; A Sourour, N.; et al. First clinical multicenter experience with the new Scepter Mini microballoon catheter. J. NeuroInterv. Surg. 2021, 13, 261–266. [Google Scholar] [CrossRef]
- Mendes, G.A.C.; Silveira, E.P.; Saleme, S.; Iosif, C.; Ponomarjova, S.; Caire, F.; Mounayer, C. Balloon-assisted microcatheter navigation for AVM embolization: Technical note. J. Neurosurg. 2015, 123, 1120–1124. [Google Scholar] [CrossRef] [PubMed]
- Abud, D.; Riva, R.; Nakiri, G.; Padovani, F.; Khawaldeh, M.; Mounayer, C. Treatment of Brain Arteriovenous Malformations by Double Arterial Catheterization with Simultaneous Injection of Onyx: Retrospective Series of 17 Patients. AJNR Am. J. Neuroradiol. 2011, 32, 152–158. [Google Scholar] [CrossRef] [PubMed]
- Bendszus, M.; Möhlenbruch, M.; Rohde, S. Comment On: Curative Embolization of Brain Arteriovenous Malformations with Onyx: Patient Selection, Embolization Technique, and Results. Clin. Neuroradiol. 2012, 22, 181–182. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.-J.; Norat, P.; Ding, D.; Mendes, G.A.C.; Tvrdik, P.; Park, M.S.; Kalani, M.Y. Transvenous embolization of brain arteriovenous malformations: A review of techniques, indications, and outcomes. Neurosurg. Focus 2018, 45, E13. [Google Scholar] [CrossRef] [PubMed]
- Massoud, T.F.; Hademenos, G.J. Transvenous Retrograde Nidus Sclerotherapy under Controlled Hypotension (TRENSH): A Newly Proposed Treatment for Brain Arteriovenous Malformations-Concepts and Rationale. Neurosurgery 1999, 45, 351–363; discussion 363–365. [Google Scholar] [CrossRef] [PubMed]
- Rhoton, A.L., Jr. The cerebral veins. Neurosurgery 2002, 51, S159–S205. [Google Scholar] [CrossRef]
- Komiyama, M. Functional Venous Anatomy of the Brain for Neurosurgeons. Jpn. J. Neurosurg. 2017, 26, 488–495. [Google Scholar] [CrossRef]
- Hudak, I.; Botz, L.; Ezero, E.; Doczi, T. A Novel Strategy in the Treatment of High-Grade Brain AVMs: Combined Transarterial and Transvenous Embolization by Means of a Polyurethane Based New Liquid Embolizing Agent. In Abstracts—9th Congress of the WFITN (World Federation of Interventional Neuroradiology)—Jiuhua Resort & Convention Center, Beijing, China, 9–13 September 2007. Interv. Neuroradiol. 2007, 13 (Suppl. 2), 128. [Google Scholar] [CrossRef]
- Mendes, G.A.C.; Kalani, M.Y.S.; Iosif, C.; Lucena, A.F.; Carvalho, R.; Saleme, S.; Mounayer, C. Transvenous Curative Embolization of Cerebral Arteriovenous Malformations: A Prospective Cohort Study. Neurosurgery 2018, 83, 957–964. [Google Scholar] [CrossRef]
- Koyanagi, M.; Mosimann, P.J.; Nordmeyer, H.; Heddier, M.; Krause, J.; Narata, A.-P.; El Serwi, A.; Stracke, C.P.; Chapot, R. The transvenous retrograde pressure cooker technique for the curative embolization of high-grade brain arteriovenous malformations. J. NeuroInterv. Surg. 2021, 13, 637–641. [Google Scholar] [CrossRef]
- Zeleňák, K.; Sýkora, J.; Vorčák, M.; Zeleňáková, J.; Kurča, E.; Deriggo, J.; Hanko, M.; Kolarovszki, B. Transvenous embolization of a ruptured brain arteriovenous malformation. Cesk. Slov. Neurol. N. 2020, 83, 441–443. [Google Scholar] [CrossRef]
- Iosif, C.; Filho, J.A.A.; Gilbert, C.E.; Rafie, A.N.; Saleme, S.; Rouchaud, A.; Mounayer, C. Selective arterial temporary flow arrest with balloons during transvenous embolization for the treatment of brain arteriovenous malformations: A feasibility study with MRI-monitored adverse events. J. NeuroInterv. Surg. 2022, 14, 1234–1238. [Google Scholar] [CrossRef] [PubMed]
- Iosif, C.; de Lucena, A.F.; Abreu-Mattos, L.G.; Ala, V.H.E.; El-Ghanam, A.; Saleme, S.; Caire, F.; Mounayer, C. Curative endovascular treatment for low-grade Spetzler-Martin brain arteriovenous malformations: A single-center prospective study. J. NeuroInterv. Surg. 2019, 11, 699–705. [Google Scholar] [CrossRef] [PubMed]
- Mendes, G.A.; Silveira, E.P.; Caire, F.; Martel, M.-P.B.; Saleme, S.; Iosif, C.; Mounayer, C. Endovascular Management of Deep Arteriovenous Malformations. Neurosurgery 2016, 78, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Fahed, R.; E Darsaut, T.; Mounayer, C.; Chapot, R.; Piotin, M.; Blanc, R.; Pereira, V.M.; Abud, D.G.; Iancu, D.; Weill, A.; et al. Transvenous Approach for the Treatment of cerebral Arteriovenous Malformations (TATAM): Study protocol of a randomised controlled trial. Interv. Neuroradiol. 2019, 25, 305–309. [Google Scholar] [CrossRef]
- Draper, E.S.; Zeitlin, J.; Fenton, A.C.; Weber, T.; Gerrits, J.; Martens, G.; Misselwitz, B.; Breart, G.; MOSAIC Research Group. Investigating the variations in survival rates for very preterm infants in 10 European regions: The MOSAIC birth cohort. Arch. Dis. Child Fetal Neonatal Ed. 2009, 94, F158–F163. [Google Scholar] [CrossRef]
- Dinc, N.; Platz, J.; Tritt, S.; Quick-Weller, J.; Eibach, M.; Wolff, R.; Berkefeld, J.; Seifert, V.; Marquardt, G. Posterior fossa AVMs: Increased risk of bleeding and worse outcome compared to supratentorial AVMs. J. Clin. Neurosci. 2018, 53, 171–176. [Google Scholar] [CrossRef]
- Lai, L.-F.; Chen, J.-X.; Zheng, K.; He, X.-Y.; Li, X.-F.; Zhang, X.; Wang, Q.-J.; Duan, C.-Z.; Chen, M. Posterior fossa brain arteriovenous malformations: Clinical features and outcomes of endovascular embolization, adjuvant microsurgery and radiosurgery. Clin. Neuroradiol. 2018, 28, 17–24. [Google Scholar] [CrossRef]
- Asano, S.; Hayashi, N.; Edakubo, S.; Hosokawa, M.; Suwa, J.; Saito, Y.; Ichi, S.; Taneda, M.; Katoh, K. Successful perinatal management of a ruptured brain arteriovenous malformation in a pregnant patient by endovascular embolization followed by elective cesarean section: A single-case experience. JA Clin. Rep. 2016, 2, 21. [Google Scholar] [CrossRef]
- Nagayama, K.; Kurita, H.; Tonari, A.; Takayama, M.; Shiokawa, Y. Radiosurgery for cerebral arteriovenous malformation during pregnancy: A case report focusing on fetal exposure to radiation. Asian J. Neurosurg. 2010, 5, 73–77. [Google Scholar]
- Yu, C.; Jozsef, G.; Apuzzo, M.L.; MacPherson, D.M.; Petrovich, Z. Fetal Radiation Doses for Model C Gamma Knife Radiosurgery. Neurosurgery 2003, 52, 687–693; discussion 693. [Google Scholar] [CrossRef] [PubMed]
- Lv, X.; Liu, P.; Li, Y. Pre-existing, incidental and hemorrhagic AVMs in pregnancy and postpartum: Gestational age, morbidity and mortality, management and risk to the fetus. Interv. Neuroradiol. 2016, 22, 206–211. [Google Scholar] [CrossRef]
- Jermakowicz, W.J.; Tomycz, L.D.; Ghiassi, M.; Singer, R.J. Use of endovascular embolization to treat a ruptured arteriovenous malformation in a pregnant woman: A case report. J. Med. Case Rep. 2012, 6, 113. [Google Scholar] [CrossRef]
- Vollherbst, D.F.; Chapot, R.; Bendszus, M.; Möhlenbruch, M.A. Glue, Onyx, Squid or PHIL? Liquid Embolic Agents for the Embolization of Cerebral Arteriovenous Malformations and Dural Arteriovenous Fistulas. Clin. Neuroradiol. 2022, 32, 25–38. [Google Scholar] [CrossRef] [PubMed]
- Trivedi, R.; Kirkpatrick, P. Arteriovenous malformations of the cerebral circulation that rupture in pregnancy. J. Obstet. Gynaecol. 2003, 23, 484–489. [Google Scholar] [CrossRef] [PubMed]
- Granata, F.; Alafaci, C.; Giacobbe, A.; De Vivo, A.; Mancuso, A.; Conti, A.; Pontoriero, A.; Pitrone, A.; Longo, M. Endovascular Treatment of Cerebral Arteriovenous Malformation Bleeding during Pregnancy—A Case Report. Neuroradiol. J. 2010, 23, 473–478. [Google Scholar] [CrossRef]
- Salvati, A.; Ferrari, C.; Chiumarulo, L.; Medicamento, N.; Dicuonzo, F.; De Blasi, R. Endovascular treatment of brain arteriovenous malformations ruptured during pregnancy—A report of two cases. J. Neurol. Sci. 2011, 308, 158–161. [Google Scholar] [CrossRef]
- Dashti, S.R.; Spalding, A.C.; Yao, T.L. Multimodality treatment of a ruptured grade IV posterior fossa arteriovenous malformation in a patient pregnant with twins: Case report. J. NeuroInterv. Surg. 2012, 4, e21. [Google Scholar] [CrossRef]
- Porras, J.L.; Yang, W.; Philadelphia, E.; Law, J.; Garzon-Muvdi, T.; Caplan, J.M.; Colby, G.P.; Coon, A.L.; Tamargo, R.J.; Huang, J. Hemorrhage Risk of Brain Arteriovenous Malformations During Pregnancy and Puerperium in a North American Cohort. Stroke 2017, 48, 1507–1513. [Google Scholar] [CrossRef]
- Sohail, R.; Bashir, Q.; Kanwal, S.; Ali, M.I. Cerebral arteriovenous malformations during pregnancy: A management dilemma. BMJ Case Rep. 2019, 12, e228759. [Google Scholar] [CrossRef]
- Teik, C.K.; Basri, N.I.; Karim, A.K.A.; Abu, M.A.; Ahmad, M.F.; Ghani, N.A.A.; Hing, E.Y.; Zakaria, R.; Thanabalan, J.A.; Abu Bakar, A.; et al. Management Options and Outcome of Cerebral Arteriovenous Malformation in Pregnancy: Case Series. Arch. Iran. Med. 2019, 22, 340–343. [Google Scholar] [PubMed]
- Yan, K.L.; Ko, N.U.; Hetts, S.W.; Weinsheimer, S.; Abla, A.A.; Lawton, M.T.; Kim, H. Maternal and Fetal Outcomes in Women with Brain Arteriovenous Malformation Rupture during Pregnancy. Cerebrovasc. Dis. 2021, 50, 296–302. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).