Abstract
Congenital syngnathia is a very rare condition of unknown etiology with multiple clinical manifestations due to different combinations of bony or soft tissue adhesions between the mandible and maxilla. It shares possible association with other congenital anomalies in the head and neck region, or with other syndromes. The aims of the present work were: (1) to perform a literature review on bony syngnathia in order to obtain a general framework on epidemiology and management protocol; (2) to describe a case of a two-year-old boy with a left unilateral bony fusion treated with a distraction protocol of three months. Original articles were searched through PubMed, Cochrane Central database and Embase with a cut-off date of June 2022. In total, 94 articles were identified through database searching. After 39 exclusions, 55 articles were included in the review process. Eighty-seven cases of bony syngnathia have been reported from 1936 to 2022, and different classifications have been suggested in terms of location, extension, functional outcomes and management protocol. Complications may range from feeding difficulty to aspiration pneumonia and respiratory arrest. Early surgery is generally required to release the ankylosis and to establish good mandible function.
1. Introduction
The term “syngnathia” defines the congenital fusion of the maxilla and mandible. It may involve either a single mucosal band (synechiae) or maxillary and mandibular bones (complete synostosis) [1].
The first case was reported by Burket [2] in 1936, who described a facial hemiatrophy associated with congenital bony ankylosis of the temporomandibular joint in a newborn.
Currently, few studies in the literature deal with congenital syngnathia, so the etiology is still unclear. Some of the suggested causes include persistence of buccopharyngeal membrane, amniotic constriction bands in the region of the developing first branchial arch, environmental insults and the use of vitamin A during pregnancy. There is no evidence of familial tendency, though some cases of consanguinity have been reported [3].
From a genetical point of view, the most accredited etiopathogenesis is the interaction of Foxc1, a key regulator of the jaw, with FGF8. The overall dosage of FGF8 affects the severity of the syngnathic phenotype [4].
Syngnathia can be isolated or associated with several syndromes [5,6]: oromandibular-limb hypogenesis syndrome, popliteal pterygium syndrome, aglossia-adactylia syndrome, Van der Woude syndrome, cleft palate lateral alveolar synechiae syndrome, Nager syndrome, Horner syndrome and Dobrow syndrome.
Cases of acquired syngnathia have been reported as complications of myositis ossificans or other limitations of mouth opening [7].
In 1997, Dawson proposed the first classification of bony congenital syngnathia in terms of treatment and functional outcome. The classification comprises Type 1 (Simple Syngnathia): bony fusion between mandible and maxilla or zygoma in the absence of other congenital anomalies in the head and neck; Type 2a (Complex Syngnathia): bony fusion between the mandible and the maxilla or zygoma with aglossia; Type 2b (Complex Syngnathia): bony fusion between the mandible and the maxilla or zygoma with agenesis or hypoplasia of the proximal mandible [8].
In 2001, Laster et al. proposed the following classification for bony syngnathia based on location [9]: Type 1a (Simple Anterior Syngnathia): bony fusion of the alveolar ridges without other congenital deformities in the head and neck; Type 1b (Complex Anterior Syngnathia): bony fusion of the alveolar ridges associated with other congenital deformities in the head and neck; Type 2a (Simple Zygomatico-Mandibular Syngnathia): bony fusion of the mandible to the zygomatic complex causing mandibular micrognathia; Type 2b (Complex Zygomatico-Mandibular Syngnathia): bony fusion of the mandible to the zygomatic complex and associated clefts or TMJ ankylosis.
In 2012, Tauro et al. proposed a classification that did not address the nature of the fused tissue, but the location and extension, along with syndromic association [10]: Type 1 (True Syngnathia): fusion between maxillary and mandibular alveolar ridges; Type 1a: unilateral bony fusion of the alveolar ridges; Type 1b: Bilateral Bony Fusion of the alveolar ridges; Type 1c: Complex Anterior Unilateral Syngnathia, associated with other congenital anomalies in the head and neck; Type 1d: Complex Anterior Bilateral Syngnathia; Type 2: Pseudosyngnathia or fusion of the mandible with cranial bones other than maxilla; Type 2a: Simple Unilateral Zygomatico-Mandibular Fusion; Type 2b: Simple Bilateral Zygomatico-Mandibular fusion; Type 2c: Complex Unilateral Zygomatico-Mandibular Fusion; Type 2d: Complex Bilateral Zygomatico-Mandibular fusion.
In 2020, Olusanya et al. introduced a new classification-based management protocol [11] comprising Type 1: Soft tissue; Type 2: Bony fusion; Subtype a: Anterior Fusion (midline); Subtype b: Posterior Fusion (bilateral); Subtype c: Zygomatico-Mandibular Fusion (unilateral).
In the same article, the authors selected 72 cases of hard tissue fusion: four cases were classified as 2a, sixteen cases as 2b and fifty cases as 2c. Two cases were not otherwise specified. Their statistical analysis showed that 44.9% of the cases were isolated, 42.0% of cases were associated with other malformations and only 9.0% of cases were syndromic. On the contrary, the soft tissue fusion (Type 1) was significantly syndromic (55.8%). Almost half of the patients showed clefts, whereas 85.5% of the Type 1 patients were affected by clefts.
In 2021 Kumar et al. proposed a new classification (FLS) based on the nature of fusion tissue (F1: Bony, F2: Fibrous, F3: Combination), on location of fusion (L1: Unilateral; L2: bilateral without involving midline; L3: anterior fusion; L4: complete fusion of alveolar arches; L5: multiple sites of fusion within the arch) and on its association with any syndrome (S0: not associated with syndromes; S1: associated) [12].
Ultrasound examination can accurately diagnose fetal micrognathia and polyhydramnios [13]. A prenatal diagnosis can also be made via fetal MRI findings, such as micrognathia or the presence of a closed mouth on prenatal sonography [14].
The aims of the present work were (1) to review the available literature about bony syngnathia in order to clarify epidemiology and protocol management and (2) to describe a case of a two-year-old boy with a left unilateral bony fusion.
2. Materials and Methods
2.1. Review of Literature
A systematic review of the literature was conducted. Original articles were searched through PubMed, Cochrane Central database and Embase, with a cut-off date of June 2022. The research was carried out using the following terms: Syngnathia or Congenital Syngnathia or Bony Syngnathia or Maxillomandibular fusion. Additional studies were taken from reference lists of previous review articles. The “related article” tool was used to improve the PubMed searches, and references of included studies were checked by a research librarian. Unpublished studies, studies not published in English or studies without an abstract were excluded. Moreover, soft tissue or fibrous synechiae were not considered in this review.
2.2. Case Report
A 2-year-old baby boy was referred to the Department of Maxillofacial Surgery of the F. Miulli Hospital in Bari from an expedition in Afghanistan by the head of the Department.
The baby was born to non-consanguineous parents; his mother had previous abortions and there was a positive history of problems during her pregnancies. The Apgar status of the baby at birth was not known.
Clinically, the child presented with left hemimandibular hypoplasia and low-set ears, whereas there were no other abnormal features including limbs (Figure 1).
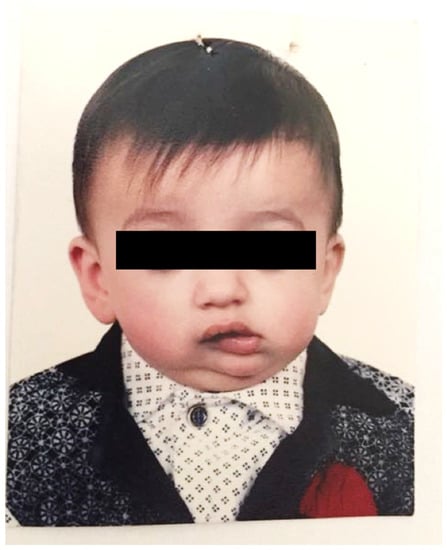
Figure 1.
The frontal view of the baby showing the laterodeviation of mandible to the left.
An intraoral examination showed a normal tongue and the absence of clefts.
A three-dimensional computer tomography scan showed a unilateral bony fusion among the ramus of the mandible, the temporal process of the zygomatic bone and the maxilla on the left. The coronoid process was normal, and the condyle did not appear ankylosed. The coronal section of the CT showed the deviation of the corpus of the mandible homolaterally to the fusion. The right TMJ appeared normal (Figure 2).
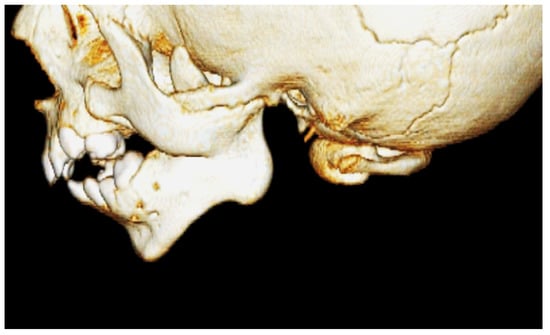
Figure 2.
Three-dimensional reconstructing CT scan showing the bony fusion of the ramus, the zygoma and the maxilla.
According to Dawson’s classification, the patient was considered a 2b while, according to Laster’s classification, he was classified as 2a.
From a surgical point of view, an intraoral buccal approach permitted access to the bony fusion (Figure 3). Intraoperatively, extra-articular ankylosis of the left TMJ was assessed. The osteotomy was taken by Mectron PIEZOSURGERY® and a KLS Martin® internal distractor was placed.

Figure 3.
An intraoral buccal access has been performed. No submandibular or preauricular scars are visible. The vertical distractor has been placed.
3. Results
3.1. Review of Literature
A total of 94 articles were identified through database searching and screened by reviewing their abstracts. After 39 exclusions, 55 articles were included in the review process, with a total of 87 cases of bony syngnathia reported from 1936 to 2022: 39 males (44.8%) and 43 females (49.4%). Five cases were not specified (Table 1).

Table 1.
Summary of reported case from 1936 to 2022 (N.S. stand for not specified).
Prenatal or neonatal diagnosis are suggested. Five cases of diagnosis during adulthood have been reported (in patients aged 19–74 years at diagnosis).
The review highlighted the geographic distribution of the syndrome. The major incidence of bony syngnathia is present in eastern Asia (31.8%), with 18 cases reported in India; 2 cases each in Malaysia, Japan and China; and 1 case each in Bangladesh, Taiwan and Korea. In the Middle East, 13 cases have been documented: in particular, 6 cases have been reported in Iran; 2 from Afghanistan; and 1 each in Iraq, Pakistan, Saudi Arabia, UAE and Israel. The European country with the highest incidence is Turkey, where four cases of bony syngnathia have been reported. Sixteen cases have been reported in the United States, although the origins of the patients were not specified.
According to Dawson’s classification, 37.9% of the patients are affected by Type 1 Syngnathia (Simple Syngnathia: bony fusion between the mandible and the maxilla or zygoma in the absence of other congenital anomalies in the head and neck), 12.6% by Type 2a (Complex Syngnathia: bony fusion between the mandible and the maxilla or zygoma with aglossia) and 44.8% by Type 2b (bony fusion between the mandible and the maxilla or zygoma with agenesis or hypoplasia of the proximal mandible).
According to Laster’s classification, 29.9% of the patients are classified into Type 1a (Simple Anterior Syngnathia), 8.0% into Type 1b (Complex Anterior Syngnathia), 25.3% into Type 2a (Simple Zygomatico-Mandibular Syngnathia) and 29.9% into Type 2b (Complex Zygomatico-Mandibular Syngnathia).
The association with the other systemic syndromes has been specified in only 23.0% of cases. The other cases could be considered as isolated. The syndromes associated with bony syngnathia were: aglossia-adactylia, Dobrow syndrome, Horner syndrome, hemifacial microsomia, Nager syndrome, oromandibular limb hypogenesis syndrome, Siebold–Robin sequence, Tessier’s cleft n. VI and X-linked Cornelia de Large syndrome.
Patients affected by bony syngnathia presented low-set ears or earlobe deformities (8%), as well as tongue deformities such as hypoplastic tongue (11.5%), tongue agenesis (5.7%), bifid tongue (3.5%) and glossopalatal ankylosis (1.2%), as well as temporomandibular joint anomalies such as ankylosis (14.5%), hypoplasia (9.2%), agenesis (10.5%), fusion (3.9%) and dislocation (1.3%). Bony syngnathia does not relate to the palate in 73.3% of patients.
Of the patients, 12.6% were born to consanguineous parents, and in three cases there was familiarity of syngnathia or a history of other maxillofacial deformities.
Of the articles, 23.0% reported abortus or death of patients after birth or surgery due to aspiration pneumonia and respiratory or cardiac arrest.
3.2. Case Report
The post-operative CT showed a reduction in mandible deviation and division of the bony fusion. Four days after the surgical placement, the distractor was activated with an increase of 0.5 mm each day for twenty days, obtaining 1 cm of gain. After that, the distractor remained placed as contention for three months (Figure 4).
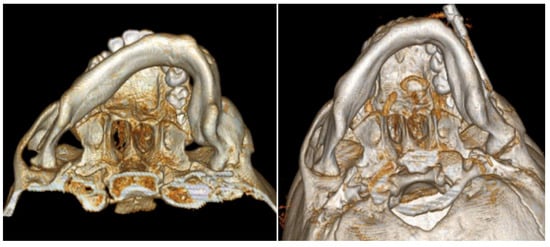
Figure 4.
On the (left), the preoperative 3D reconstruction shows the asymmetrical deviation of the mandible. On the (right), the post-operative 3D scan shows the recovery of the mandible deviation.
There were no complications during nor after the surgical procedures, and no relapses occurred until the patient was checked in Italy. Unfortunately, after the 3-month follow-up, the patient returned to his country, and he never visited again (Figure 5).

Figure 5.
One-month follow-up. Symmetry was improving, the oral aperture was 1 cm wider.
4. Discussion
A multidisciplinary team and early surgical management of syngnathia is mandatory to avoid respiratory and feeding difficulties and prevent ankylosis of the TMJ.
According to Hegab’s surgical therapy protocol [3], the management workflow provides these three steps:
- (1)
- Planning the surgical field through a three-dimensional reconstructed CT, the only radiograph showing the entity of the bony fusion. Moreover, a facial angio-CT scan can be performed to study the cervical vascular anatomy and discard anatomical variants [22].
- (2)
- Management of upper airways and surgical time.
- (3)
- Long-term post-operative physiotherapy [3].
An important step consists of the management of the upper airways, which could be compromised during surgical procedures under general anesthesia. A difficult intubation could be facilitated by using a fiberoptic bronchoscope [23]; alternatively, an elective tracheostomy, maintained until the jaw fusion is released, is performable [17]. However, tracheostomy should be considered the last resort because of the postoperative complications [24]. Gastrostomy or the placing of a nasogastric tube are recommended to provide nutrients, especially in newborns [19].
The main goal of the surgery is to release the ankylosis, establish a well-functioning mandible and prevent recurrence [20]. Surgical exposure depends on the site of fusion [18], and different points of access to the surgical areas have been proposed: a bilateral submandibular approach, the preauricular-condylar area and intraoral incision of the vestibule [25]. The bilateral submandibular approach has been proposed to release the bony fusion, as the entire extent of the upper border of the mandible—including TMJs and the coronoid process—can be explored without trauma to facial nerves.
There is a high risk of recurrence for reattachment of the bony junctions [21], which is related to the loss of attention to long-term post-operative physiotherapy and follow-up, or to the genetic predisposition for bone formation and high osteogenic potential at young ages. Passive and active physical motion, breast feeding or bottle feeding may be beneficial in restoring the motion of the TMJ [15,26].
Internal distraction should be placed between the mandibular segment and the maxillozygomatic complex vertically, with the activation pins placed in the intramandibular areas percutaneously. Bony distraction begins intraoperatively and continues for circa 2 mm in the first few days, and then for 1 mm per day [20]; alternatively, a mold or a silicon sheet could be interposed between the two arches to separate the mucosal areas and prevent recurrence due to secondary scar contraction [16]. The use of intra-alveolar synthetic bite block for 4 weeks post-operatively until the raw area heals completely is also recommended to prevent trismus.
5. Conclusions
Maxillomandibular syngnathia is a very rare disease of unknown origin, which can occur with different degrees of severity, ranging from synechia (mucosal band fusion) to bony fusion (synostosis). Although different classifications have been proposed to facilitate diagnosis and surgical approaches, currently, no univocal consensus on the best operational approach is available. On the contrary, it seems to be accepted that a multidisciplinary team is required to manage this condition and that surgery must take place as early as possible. Moreover, difficult socio-economic conditions can affect the surgical times and management of patients, as well as the post-operative follow-up, as in the case we reported in the present work.
Author Contributions
Conceptualization, V.C. and R.C.; methodology, V.C.; software, C.D.B.; validation, C.D.B., M.D. and A.P.C.; formal analysis, V.C.; investigation, A.P.C.; resources, A.C.; data curation, M.G.P.; writing—original draft preparation, C.D.B. and M.D.C.; writing—review and editing, V.C.; visualization, L.M.; supervision, M.D.C.; project administration, V.C.; funding acquisition, M.D.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
PubMed, Cochrane Central database and Embase.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Ugurlu, K.; Karsidag, S.; Huthut, I.; Yildiz, K.; Bas, L. Congenital fusion of the maxilla and mandible. J. Craniofacial Surg. 2005, 16, 287–291. [Google Scholar] [CrossRef]
- Burket, L.W. Congenital bony temporomandibular ankylosis and facial hemiatrophy: Review of the literature and report of a case. J. Am. Med. Assoc. 1936, 106, 1719–1722. [Google Scholar] [CrossRef]
- Hegab, A.; ElMadawy, A.; Shawkat, W. Congenital maxillomandibular fusion: A report of three cases. Int. J. Oral Maxillofac. Surg. 2012, 41, 1248–1252. [Google Scholar] [CrossRef]
- Inman, K.E.; Purcell, P.; Kume, T.; Trainor, P.A. Interaction between Foxc1 and Fgf8 during mammalian jaw patterning and in the pathogenesis of syngnathia. PLoS Genet. 2013, 9, e1003949. [Google Scholar] [CrossRef]
- Mohan, A. Syngnathia—Congenital maxillomandibular fusion: Case report and literature review. J. Oral Maxillofac. Surg. 2018, 76, 1096.e1–1096.e6. [Google Scholar] [CrossRef]
- Campobasso, A.; Cosola, M.D.; Testa, N.F.; Lacarbonara, V.; Dioguardi, M.; Muzio, L.L.; Muzio, E.L.; Scarpa, M.; Covelli, M.; Crincoli, V.; et al. The influence of abnormal head posture on facial asymmetry. J. Biol. Regul. Homeost. Agents 2022, 36, 325–335. [Google Scholar]
- Choi, J.; Min, C.; Myoung, H.; Hwang, S.; Kim, M.; Lee, J. Acquired syngnathia. Br. J. Oral Maxillofac. Surg. 2004, 42, 448–450. [Google Scholar] [CrossRef]
- Dawson, K.H.; Gruss, J.S.; Myall, R.W. Congenital bony syngnathia: A proposed classification. Cleft Palate-Craniofacial J. 1997, 34, 141–146. [Google Scholar] [CrossRef]
- Laster, Z.; Temkin, D.; Zarfin, Y.; Kushnir, A. Complete bony fusion of the mandible to the zygomatic complex and maxillary tuberosity: Case report and review. Int. J. Oral Maxillofac. Surg. 2001, 30, 75–79. [Google Scholar] [CrossRef] [PubMed]
- Tauro, D.P.; Kallappanavar, N.; Kiran, H.; Girhe, V.J. Congenital zygomatico-mandibular fusion (pseudo-syngnathia?) in conjunction with unilateral anophthalmia: Review of terminology and classification. Cleft Palate-Craniofacial J. 2012, 49, 626–629. [Google Scholar] [CrossRef] [PubMed]
- Olusanya, A.; Akadiri, O. Congenital syngnathia: Review of clinical profile and proposal of a new classification-based management protocol. Int. J. Oral Maxillofac. Surg. 2020, 49, 505–514. [Google Scholar] [CrossRef] [PubMed]
- Kumar, V.; Rattan, V.; Rai, S. Congenital maxillomandibular syngnathia: Review of literature and proposed new classification system. J. Maxillofac. Oral Surg. 2021, 20, 19–36. [Google Scholar] [CrossRef]
- Broome, M.; Vial, Y.; Jacquemont, S.; Sergi, C.; Kamnasaran, D.; Giannoni, E. Complete maxillo-mandibular syngnathia in a newborn with multiple congenital malformations. Pediatrics Neonatol. 2016, 57, 65–68. [Google Scholar] [CrossRef]
- Vahidi, K.; Joe, B.N.; Glenn, O.A.; Barkovich, A.J.; Filly, R.; Ball, R.; Coakley, F.V. Prenatal imaging of congenital maxillomandibular fusion: Case report and review of the literature. J. Ultrasound Med. 2007, 26, 381–389. [Google Scholar] [CrossRef] [PubMed]
- Rao, S.; Oak, S.; Wagh, M.; Kulkarni, B. Congenital midline palatomandibular bony fusion with a mandibular cleft and a bifid tongue. Br. J. Plast. Surg. 1997, 50, 139–141. [Google Scholar] [CrossRef]
- Knoll, B.; Karas, D.; Persing, J.A.; Shin, J. Complete congenital bony syngnathia in a case of oromandibular limb hypogenesis syndrome. J. Craniofacial Surg. 2000, 11, 398–404. [Google Scholar] [CrossRef] [PubMed]
- Gupta, R.K.; Jadhav, V.; Gupta, A.; Sanghvi, B.; Shah, H.; Parelkar, S. Congenital alveolar fusion. J. Pediatric Surg. 2008, 43, 1421–1425. [Google Scholar] [CrossRef] [PubMed]
- Subramanian, B.; Agrawal, K.; Panda, K. Congenital fusion of the jaws: A management protocol. Int. J. Oral Maxillofac. Surg. 2010, 39, 925–929. [Google Scholar] [CrossRef] [PubMed]
- El-Hakim, I.; Al-Sebaei, M.; Abuzennada, S.; AlYamani, A. Congenital fusion of the maxilla and mandible (congenital bony syngnathia). Int. J. Oral Maxillofac. Surg. 2010, 39, 933–936. [Google Scholar] [CrossRef]
- Konas, E.; Aliyev, A.; Tunçbilek, G. Congenital maxillomandibular syngnathia: A new management technique using distraction techniques. J. Craniofacial Surg. 2015, 26, e68–e70. [Google Scholar] [CrossRef] [PubMed]
- Desai, J.; Smit, C.; Naidoo, S. Release of syngnathia by anticlockwise rotation and mandibular advancement using bilateral alloplastic temporomandibular joint prostheses: A new approach. Br. J. Oral Maxillofac. Surg. 2018, 56, 750–752. [Google Scholar] [CrossRef] [PubMed]
- Rubio-Palau, J.; Prieto-Gundin, A.; de Abreu Graterol, L.M.; Vercruysse Jr, H. Maxillomandibular syngnathia: 3D planning and review of the literature. Craniomaxillofacial Trauma Reconstr. 2018, 11, 124–130. [Google Scholar] [CrossRef]
- Alfery, D.D.; Ward, C.; HARWOOD, I.R.; MANNINO, F.L. Airway management for a neonate with congenital fusion of the jaws. J. Am. Soc. Anesthesiol. 1979, 51, 340–342. [Google Scholar] [CrossRef]
- Brown, T.; Dwyer, M. The problems of anaesthesia for a neonate with fused jaws. Anaesthesia 1985, 40, 597–598. [Google Scholar] [CrossRef] [PubMed]
- Mattos, C.; Vilani, G.; Sant’Anna, E.; Ruellas, A.; Maia, L. Effects of orthognathic surgery on oropharyngeal airway: A meta-analysis. Int. J. Oral Maxillofac. Surg. 2011, 40, 1347–1356. [Google Scholar] [CrossRef]
- Ciavarella, D.; Parziale, V.; Mastrovincenzo, M.; Palazzo, A.; Sabatucci, A.; Suriano, M.M.; Bossù, M.; Cazzolla, A.P.; Lo Muzio, L.; Chimenti, C. Condylar Position Indicator and T-Scan system II in clinical evaluation of temporomandibular intracapsular disease. J. Cranio-Maxillofac. Surg. 2012, 40, 449–455. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).