Abstract
Background/Objectives: Wolf–Hirschhorn syndrome (WHS; OMIM #194190) is a rare neurodevelopmental disorder, caused by deletions in the distal short arm of chromosome 4. It is characterized by developmental delay, epilepsy, intellectual disability, and distinctive facial dysmorphism. Clinical presentation varies widely, complicating prognosis and individualized care. Methods: We assembled a cohort of 140 individuals with genetically confirmed WHS from Spain and Latin-America, and developed and validated a multidimensional, Clinician-Reported Outcome Assessment (ClinRO) based on the Global Functional Assessment of the Patient (GFAP), derived from standardized clinical questionnaires and weighted by HPO (Human Phenotype Ontology) term frequencies. The GFAP score quantitatively captures key functional domains in WHS, including neurodevelopment, epilepsy, comorbidities, and age-corrected developmental milestones (selected based on clinical experience and disease burden). Results: Higher GFAP scores are associated with worse clinical outcomes. GFAP showed strong correlations with deletion size, presence of additional genomic rearrangements, sex, and epilepsy severity. Ward’s clustering and discriminant analyses confirmed GFAP’s discriminative power, classifying over 90% of patients into clinically meaningful groups with different prognoses. Conclusions: Our findings support GFAP as a robust, WHS-specific ClinRO that may aid in stratification, prognosis, and clinical management. This tool may also serve future interventional studies as a standardized outcome measure. Beyond its clinical utility, GFAP also revealed substantial social implications. This underscores the broader socioeconomic burden of WHS and the potential value of GFAP in identifying high-support families that may benefit from targeted resources and services.
1. Introduction
Wolf–Hirschhorn syndrome (WHS; OMIM #194190) is a rare genetic disorder resulting from partial deletions on the short arm of chromosome 4, particularly within the 4p16.3 region [1,2,3]. The size of the deletion can vary between 700 Kb to 35 Mb, which includes the WSHC1 (NSD2) gene within the putative main responsible region for the syndrome [4,5,6,7,8]. The clinical phenotype includes growth and developmental delay, intellectual disability, seizures, microcephaly, and distinct craniofacial features commonly described as a “Greek warrior helmet” profile. The syndrome has an estimated prevalence of 1 in 20,000 to 50,000 live births and is more frequently diagnosed in females than in males. Our most recent work with the Spanish individuals of this cohort established a frequency of 1/172,904 newborns [9], suggesting that this syndrome may be underdiagnosed, as it occurs in other near countries [10]. While the causative genetic alterations are well established, the wide spectrum of phenotypic variability remains poorly understood, posing challenges for clinical management and prognostic counseling.
Existing clinical guidelines for WHS emphasize the need for multidisciplinary follow-up; however, standardized tools for assessing disease severity and monitoring patient progress over time are lacking. Clinical Outcome Assessments (COAs), particularly those developed for rare diseases, have demonstrated value in providing structured evaluations of patient status and in guiding treatment decisions [11,12,13,14,15,16,17,18,19]. In WHS, no syndrome-specific COA currently exists. This gap limits our ability to objectively evaluate interventions and to offer families reliable information about likely disease trajectories. Indeed, there are neither enough data on adulthood, life expectancy, nor longitudinal work in these patients [20,21,22,23,24,25,26] that helps clinicians to adequately monitor and predict their evolution.
To address this need, we developed a disease-specific Clinician-Reported Outcome (ClinRO) tool for WHS: the Global Functional Assessment of the Patient (GFAP). This measure integrates multiple domains of patient function, including developmental milestones, epilepsy characteristics, and comorbidities, to provide a composite score reflecting overall clinical severity. The GFAP was constructed using data from one of the largest and most clinically diverse WHS cohorts (140 individuals) to date, incorporating individuals from both Spain and Latin America. Our previous work in this syndrome was taken as sufficient to achieve expertise and in-depth understanding of the medical aspects of the knowledge of the concept of interest (COI). Here, we present the development and validation of the GFAP score and its utility in identifying phenotypic subgroups within WHS. We demonstrate its association with key clinical and genetic features and evaluate its discriminatory capacity through cluster and discriminant analysis.
2. Materials and Methods
2.1. Cohort Description
We enrolled 140 individuals with a confirmed genetic diagnosis of WHS between 2013 and 2023. Participants were recruited primarily from Spain (n = 75) and various Latin-American countries (n = 65), including Argentina, Mexico, Chile, Peru, Venezuela, Ecuador, and Colombia (see Figure 1). Some of the patients were previously described by us [9,27,28,29,30,31,32,33]. Figure 1 also shows the recruitment procedure of the patients over these years. Informed consent was obtained from the families, and all procedures complied with institutional ethical guidelines.
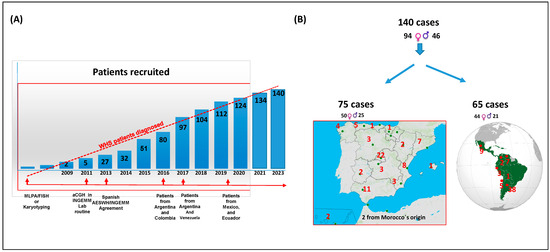
Figure 1.
Recruitment of the cohort, and segregation by countries and gender.
2.2. Clinical Data Collection
Clinical data were extracted from two standardized questionnaires and completed by referring physicians. Finally, they are validated through direct interviews with families and review of medical records. The data covered core WHS features, neurodevelopmental milestones, epilepsy characteristics, comorbidities, and social impacts. Two independent geneticists interviewed most of the parents to ensure consistency, minimize recall bias, and ensure standardized data from the questionnaires through manual review.
2.3. Genetic Characterization
All patients underwent high-resolution chromosomal microarray analysis using the Illumina Infinium CytoSNP-850k platform. Genomic deletions and duplications were annotated using GRCh37/hg19 coordinates and visualized via the University of California at Santa Cruz Genome Browser (http://genome.ucsc.edu/; (accessed on 16 January 2025)). Additional diagnostic techniques, including MLPA (MRC-Holland. Amsterdam, The Netherlands) and FISH, were used to confirm or further characterize chromosomal abnormalities when necessary.
2.4. Construction of the GFAP Score
The GFAP (Global Functional Assessment of the Patient) score was developed (using different variables from the questionnaires), as a continuous composite metric integrating four major clinical domains in the syndrome: (i) age-adjusted psychomotor milestones, (ii) epilepsy features, (iii) presence of comorbidities, and (iv) developmental aspects such as IUGR or hypotonia. Each item was scored based on clinical severity and weighted according to Human Phenotype ontology (HPO; https://hpo.jax.org/; (accessed on 20 January 2022)) term frequencies and clinical relevance. Finally, Principal Component Analysis (PCA) was applied to validate the GFAP construct, containing Kaiser–Meyer–Olkin’s measure and Bartlett’s test. The full scoring algorithm is detailed in Table S1.
2.5. Statistical Analyses
Descriptive statistics were used to characterize the cohort. The categorical variables were taken from our two questionnaires curated from medical records and were expressed as “1” (condition present at some point) or “0” (condition not present at any time). Pearson or Spearman correlations were used to assess relationships between GFAP and continuous or categorical variables, respectively. Comparisons between groups were made using Student’s t-test, Chi-square, or ANOVA with Bonferroni correction or T3- Dunnett post-hoc tests, where appropriate. The categorical variables were taken from our two questionnaires curated from medical records and were expressed as “1” (condition present at some point) or “0” (condition not present at any time). Hierarchical cluster analysis (Ward’s method) and discriminant analysis were used to assess the classification performance of GFAP. Statistical significance was defined as p < 0.05. Analyses were performed using SPSS version 28 (IBM Corporation, Chicago, IL, USA).
3. Results
3.1. Cohort Characteristics
The cohort comprised 140 individuals with a genetic diagnosis of WHS (64.3% female), with ages ranging from neonates to 39 years (mean 7.8; median 5 years). The median age at diagnosis was 11 months (mean 27.3 months). A complete list of clinical item frequencies and descriptive variables for the whole cohort is shown in Table S2 of Supplemental Data (Excel-based file; descriptive and frequency windows). Patients were predominantly from Spain and Latin America. Most individuals presented with global developmental delay and characteristic facial features, several comorbidities, and epilepsy. Feeding difficulties and organ anomalies were also common. Data such as neonatal data, dysmorphic traits, and comorbidities were presented in detail at Supplemental Data.
3.2. Genetic Findings
Most patients (96%; 134/140) underwent SNP-array analysis. The 4-pter deletions were graphically represented using the UCSC Genome Browser database (2025 update), in Figure S1 of Supplemental Data. Genomic coordinates are also available in Table S2 of Supplemental Data (Coordinate window). Terminal deletions on 4p were the predominant rearrangement (87.1%; 122/140), with a subset of approximately 46% (65/140) of the cohort harboring complex or additional rearrangements, and 39.5% (51/140) exhibiting terminal duplications, suggestive of derivative chromosomes (see Figure 2). The cytogenetic data and analysis of the parents allowed us to establish the majority of them as de novo (30/51, around 58.82%) The average 4p deletion size was 9.12 ± 6.78 Mb (Table S2 of Supplemental Data; Coordinates window).
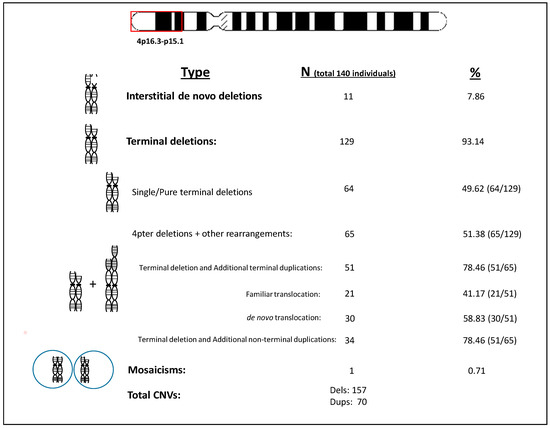
Figure 2.
Type of genomic rearrangements found in the cohort.
3.3. GFAP Score Distribution and Correlates
Table 1 shows the mean ± SD, median, and range values for GFAP and its intermediate “functional” components for this construct, in the whole cohort. The GFAP scores ranged from 64 to 410, with higher scores seeming to indicate a more severe functional impairment.

Table 1.
Median and mean values for this GFAP and its intermediate components in the whole cohort.
Interestingly, significant positive correlations (using Pearson’s analysis) were observed between GFAP and deletion size, number of antiepileptic drugs used, and frequency of seizures and surgeries (p < 0.05). Negative correlations were found with control of epileptic crisis, gestational age, weight at birth, and cognitive/motor milestone achievements (p < 0.05; by Person’s analysis). In addition, a comparison between individuals with lower vs. higher GFAP scores at different functional and clinical items was shown in Figure 3A–C. Briefly, MRI anomalies (which are not shown in the figure), nephro-urological, cardiac anomalies among others functional (A), clinical burden (B), and multisystem (C) impairments were more frequent in high-GFAP individuals.
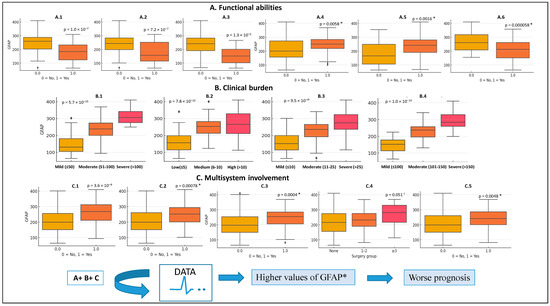
Figure 3.
GFAP score (Arbitrary Units; AU) distribution in different functional abilities (A), clinical burden (B) or multisystem involvement (C) items recruited in our cohort. (A1), To be able to walk unaided; (A2), To be able to eat unaided; (A3), Ability to make sentences; (A4), Hearing problems. (A5), Non-sphincter control; (A6), To be able to sit unaided. (B1), Global epilepsy score (AU); (B2), Comorbidities score (AU); (B3), Developmental delay score corrected by age (AU); (B4), Developmental impact items score (AU). (C1), Cardiac anomalies; (C2), Nephro-urogenital anomalies; (C3), Ophthalmological anomalies; (C4), Number of surgeries; (C5), Recurrent respiratory infections. * p value statistically significant data using different statistical analysis approaches; t-Student, Chi-square, Mann–Whitney, Kruskal–Wallis.
We further compared “functional” data, using the GFAP construct, with the different subpopulations and other different “queries”, such as gender, genetics, etc., in order to establish a potential “functional” variability among individuals with WHS. No significant differences in GFAP scores between subpopulations were found (Table S3 of Supplemental Data). Nevertheless, we did find significant GFAP differences between sexes. Indeed, males exhibited higher GFAP scores than females (p = 0.04; Student t-test, Table 2), consistent with a more severe functional profile, being associated with a higher number of surgeries, and larger size of the deletions, but inversely with neonatal parameters and or crisis control values (Student-t test p < 0.05). We also observed statistically significant differences among sexes comparing categorical variables (chi-square tests). Preferentially, in several motor or cognitive items, such as “able to seat unaided”, “able to walk with help”, “able to walk unaided”, “non-sphincter control” or “communication with alternative method” (p = 0.034, 0.029, 0.049, 0.038, 0.003, respectively), “to be in monotherapy” (p = 0.007), or different comorbidities items (“C-gastrostomy”, “nephro-urogenital”, and “ophthalmology anomalies”; p = 0.015; p = 0.0002; p = 0.024, respectively; Tau_ b Kendal). In all the cases, better numbers were observed in females, which were independent of the subpopulation used.

Table 2.
Median and mean values for this GFAP and its intermediate components by gender.
We also highlight that individuals with isolated (pure) 4p deletions had significantly higher GFAP scores than those with additional duplications (p = 0.03; Student-t test, Table 3). Notably, those differences are mainly established with some neonatal items. In fact, patients with additional duplications showed better neonatal outcomes (such as higher weight at birth and being born later in time; Student’s-test; p = 0.007 and 0.05, respectively) and less frequent intrauterine growth restriction (IUGR; p = 0.001, Fisher test, two sides). However, we have to note that those significant differences between the deletion size and to have or not to have an additional rearrangement could be a consequence of differences in deletion sizes (11.45 + 7.65 Mb, median 10.20 Mb in single 4p minus deletions versus 7.62 + 5.20 Mb, median 7.21 Mb in cases with an additional rearrangement; Student’s-test; p = 0.03).

Table 3.
Median and mean values for this GFAP and its intermediate components by genetic findings.
Other comparisons among variables showing statistically significant differences (at GFAP) are shown in the Supplemental Data. Indeed, we compared individuals within whom non-febrile causes trigger seizures vs. fever as a trigger (Table S4 of Supplemental Data), or who had the ability to make sentences vs. not (Table S5 of Supplemental Data), or who had anomalies in MRI vs. not (Table S6 of Supplemental Data). Finally, families of individuals with higher GFAP scores were significantly more likely to report having quit jobs to provide the child care (p < 0.01), indicating that functional severity may impact caregiver burden (Table S7 of Supplemental Data).
3.4. Genotype/Phenotype Analysis
We further analyzed possible genotype/phenotype correlations based on the deletion size, and the existence of an additional rearrangement may modulate the GFAP score.
3.5. Ward’s Cluster Analysis Using the Size of the Deletion in the Whole Cohort
We performed Ward’s hierarchical cluster analysis by using “deletion size” as a variable (obtaining four clusters, see Table S8 of Supplemental Data) or by using two variables (“deletion size” and “GFAP”, Table 4) in order to verify how individuals may be grouped. Using the latest experimental approach, the individuals, at the end, were mainly grouped into two clusters (Akaike and BIC analysis in SPSS) as follows: cluster-A (deletion size, 18.98 ± 6.75 Mb; GFAP: 267.96 ± 53.12) and cluster-B (deletion size, 6.32 ± 3.40 Mb; GFAP: 215.87 ± 43.46). The number of patients in each group was 30 and 110 subjects, respectively. Table 4 shows the different items collected by both clusters (A and B) and is dissected by their frequencies.

Table 4.
Ward’s hierarchical cluster variable frequency analysis using deletion size and GFAP values.
Cluster-B, whose equivalence will be cluster-1 and -2 using the variable “deletion size” as a unique variable for clusterization (see Table S8 of Supplemental Data), showed better frequency/score values in different epilepsy items (up to 13, see “global epilepsy”), cognitive, and motor items than cluster-A. Cluster-B was also associated with a lower size of deletions and, thus, a lower score of GFAP, and its intermediates, aligning with a better prognosis than patients in cluster-A. Interestingly, we highlight that “the ability to make sentences” (expressive language) was associated preferentially with small deletions and, thus, with cluster-B (95%, 18/19). Something similar can be observed for individuals with the ability “to say a few words” (43/46; around 94%; Table 4) versus “no words at all”. Finally, according to the side effects, cluster-B individuals (smaller deletions) were diagnosed later in time (median: 12 months) than larger-size deletions (cluster-A’s individuals; median: 3 months. Student-t test p ≤ 0.05).
3.6. Unsupervised Hierarchical Clusterization and Discriminate Analysis
Unsupervised hierarchical clustering is one of the most common approaches to identify patterns in the data, without any prior knowledge about identifying characteristics, properties or classifications (unlabeled data) [30]. Clustering bietapic stepwise using all variables, but not GFAP or its intermediates, rendered two main groups of segregation that we called groups-1 and -2 (Table 5). Table 5 shows that group-1 segregated globally, with better numbers of the different variables studied. Indeed, Chi-square Student-t and Mann–Whitney tests showed significant differences between the two groups for most of the variables analyzed, including deletion size (10.85 ± 5.65 Mb for group-2, and 5.09 ± 3.68 Mb for group-1). Regarding GFAP, groups clearly also showed differences (261.80 ± 61.91 for group-2 and 176.19 ± 64.51 for group-1). Interestingly, there is a statistically significant association between sex and cluster membership. Indeed, males are overrepresented over females in group-2. The odds ratio indicates that a male is 4.5 times more likely to belong to group-2 than to group-1, compared to a female (p < 0.0031).

Table 5.
Unsupervised hierarchical cluster segregation in the whole cohort. Summary of differences between group-1 and group-2.
Discriminant analysis using GFAP as a unique variant classified 72.1% of patients correctly. Discriminant analysis is a classification challenge used to classify observations into non-overlapping groups, based on scores on one or more quantitative predictor variables. If we add “deletion size”, it is up to 77.2%. However, by applying just one of the GFAP’s intermediates, “Development delay corrected by age”, which reflects six motor and five cognitive milestone items corrected by age, we properly classified up to 89.0% of the original patients. In addition, adding the variable “deletion size” meant we got up to 93.4% of individuals. The threshold using “Development delay corrected by age” as a unique variable gave a value of 18.63. Below this score, individuals will segregate in group-2, with a better prognosis for the syndrome.
4. Discussion
Wolf–Hirschhorn syndrome (WHS) is a rare genetic disorder characterized by complex clinical manifestations and a severe prognosis. Although the general clinical aspects are frequently suggestive of the syndrome, the wide and varied spectrum of clinical manifestations in WHS may cause difficulties in diagnosis. This study presents the development and validation of the Global Functional Assessment of the Patient (GFAP), a clinician-reported outcome measure tailored specifically for individuals with WHS. By leveraging a large, clinically and genetically diverse cohort, we demonstrated that GFAP provides a reliable and quantifiable representation of functional severity in WHS. Our findings confirm that GFAP can capture key elements of disease burden, including neurodevelopmental delay, epilepsy, and comorbidities, while being sensitive to genetic variations such as deletion size and the presence of additional chromosomal rearrangements.
The GFAP score exhibited robust statistical associations with multiple clinical parameters, supporting that higher values of the GFAP score are associated with a worse prognosis (see Figure 3A–C). In addition, larger deletion sizes were significantly associated with worse functional outcomes (higher GFAPs), aligning with previous studies that suggest WHS follows a contiguous gene deletion syndrome, as it was previously indicated [31,32,33,34,35,36,37,38]. Interestingly, the presence of terminal duplications alongside 4p deletions appeared to mitigate some of the clinical severity, particularly in neonatal parameters such as birth weight and gestational age. These findings support the notion that additional genetic material (depending on the origin and type) may have a modulating effect on phenotype severity, a hypothesis also proposed in earlier investigations [39,40]. At this point, it is remarkable that only the adequate use of new genomic tools, such as high-resolution microarrays (CMA), may be used for a complete genetic diagnosis in WHS individuals. In fact, it is noteworthy that in many of the patients we also found an additional terminal duplication, among which those of the 8pter (n = 19) and 11pter (n = 7) chromosomes stood out. Thus, the complete genetic characterization in WHS individuals is important for not only diagnostic purposes, but also for prognosis, since given both the additional genetic alterations associated with 4p-deletions, and a higher/smaller size of it, can lead to a worse or a better functional prognosis, respectively. The observed attenuation of phenotype severity in individuals with additional duplications may reflect a genomic buffering effect, whereby duplicated segments exert compensatory transcriptional influences on pathways disrupted by the 4p deletion. This effect could be mediated by gene dosage interactions, chromatin reorganization, or epigenetic modulation. Alternatively, selective embryonic survival of more balanced rearrangements may contribute to this phenomenon.
Consistent with previous comments, WHS children have IUGR (IntraUterine Growth Restriction), which continues with failure to thrive during infancy [41,42]. However, many authors mentioned the putative relationship between IUGR and low weight at birth, but they do not correlate the weight at birth and gestational age of each patient. Our data showed a positive correlation between these two aspects, and also with the size of the deletions and, most interestingly, with the presence of those additional duplications, supporting that this fact responds to a genetic cause, supporting previous works [43].
Interestingly, sex-based differences were also observed, with males presenting with higher GFAP scores and more pronounced functional impairments. Although WHS is more frequently diagnosed in females, the increased burden in males suggests a potential sex-linked modifier effect or differences in healthcare access, reporting bias, or societal caregiving practices—areas that should have further investigation.
Cluster and discriminant analyses validated GFAP’s ability to stratify patients into clinically meaningful groups. Individuals in the lower-GFAP cluster demonstrated better cognitive and motor development, more effective seizure control, and fewer comorbidities. These insights offer clinicians a practical framework for anticipating patient trajectories and tailoring interventions. Notably, the GFAP subdomain related to age-corrected developmental milestones alone achieved near-equivalent classification performance, underscoring its value as a core prognostic indicator. Beyond its clinical utility, GFAP also revealed substantial social implications. Families of children with higher GFAP scores were more likely to experience significant life disruptions, such as leaving employment to provide care. This underscores the broader socioeconomic burden of WHS and the potential value of GFAP in identifying high-support families that may benefit from targeted resources and services. Although we did not observe significant differences in GFAP scores between Spanish and Latin-American cohorts, we acknowledge that underlying disparities in access to specialized care, early interventions, or educational support services may influence long-term outcomes beyond what is captured in the current analysis.
While our current data are cross-sectional, the GFAP may serve as a longitudinal outcome measure in natural history studies or therapeutic trials, capturing subtle shifts in developmental trajectories or responses to targeted interventions. Its use in future prospective cohorts may also allow evaluation of its sensitivity to clinical change, treatment response, and health service utilization. The framework underlying GFAP—integrating age-adjusted milestones, comorbidities, and seizure burden—may prove adaptable to other contiguous gene syndromes where functional heterogeneity poses similar clinical challenges. With appropriate recalibration, the GFAP concept may serve as a model for syndrome-specific ClinRO tools across the spectrum of rare neurodevelopmental disorders. In this sense, some previous experiences can be found in other rare diseases [44,45,46].
5. Future Address
Future studies may integrate GFAP scoring with detailed gene-level analyses to better understand how specific genes within the 4p16.3 region—such as NSD2 (associated with developmental delay), LETM1 (epilepsy), or CPLX1 (synaptic function)—modulate individual trajectories. This could aid in refining prognostic models and targeting emerging precision therapies. A major strength of this study is the size and diversity of the cohort, which enhances the generalizability of our findings. However, limitations include the cross-sectional nature of data and the reliance on retrospective questionnaire-based assessments. Future longitudinal studies are needed to assess GFAP’s sensitivity to change over time and its responsiveness to interventions.
In future work, incorporating age-stratified analyses may help delineate how functional trajectories evolve with age and identify potential developmental plateaus or critical windows. Lastly, internal cross-validation techniques could be applied to confirm the robustness of the GFAP model and its subdomains across different clinical subgroups.
6. Conclusions
This study introduces and validates the Global Functional Assessment of the Patient (GFAP) as a potential first clinician-reported outcome assessment specifically designed for individuals with Wolf–Hirschhorn syndrome. The GFAP score represents a novel, WHS-specific ClinRO capable of stratifying patients by functional severity and supporting clinical decision-making. Its integration into both clinical practice and research protocols may improve care planning and enable more precise evaluation of future therapeutic strategies. Importantly, GFAP demonstrates the capacity to distinguish between clinically meaningful subgroups of WHS patients, facilitating tailored care approaches and offering valuable insights into the impact of chromosomal complexity on disease expression. The integration of GFAP into clinical practice could enhance patient monitoring, support family counseling, and guide future interventional trials. Practical implementation could involve embedding the GFAP score into electronic health records for routine use during clinical assessments, and its application as an endpoint in prospective natural history or treatment studies.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/genes16070820/s1, Figure S1: SNP array results for the whole cohort; Table S1: Items for constructing GFAP; Table S2: Descriptive and frequency data for the whole cohort; Table S3: Median and Mean Values for this GFAP and its intermediate components in the subpopulations. Table S4: Median and Mean Values for this GFAP and its intermediate components by individuals with seizures without fever vs not; Table S5: Median and Mean Values for this GFAP and its intermediate components by individuals with the ability to make sentences vs not; Table S6: Median and Mean Values for this GFAP and its intermediate components by individuals with MRI anomalies vs not.; Table S7: Median and Mean Values for this GFAP and its intermediate components by individuals who quit the job vs not; Table S8: Ward’s hierarchical cluster analysis using “deletion size” as unique variable; Table S9: Descriptive and frequency data for Subpopulations; Auxiliary Methods; Additional Results.
Author Contributions
All authors contributed to revising the manuscript. The design of the study was made by J.N. and R.B.-L., and supervised by P.L.; the article was written by J.N., P.L., R.B.-L., H.P., J.A.T.-C. and C.B.-F. A.H. and J.N. made the statistical analyses, M.A.M.-Á., Y.M.-G., P.B. and J.N. made the microarrays, and E.M., F.A.G.-S. and I.V. made the cytogenetic and FISH studies. H.P., P.L., R.B.-L., I.M. and E.M. participated in patient recruitment. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by FIS18/01433 (PI-3569) from ISCIII (Ministry of Health of Spain) and co-funded by the European Union (ERDF, “A way to make Europe”), and PI-2734 (21 July 2017), from FIBHULP.
Institutional Review Board Statement
The study was conducted in accordance with the Decla-ration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of Hospital Universitario La Paz (protocol code: PI-3569; approval 13 May 2019; PI-2734, approval 21 July 2017).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
We deposited data from SNP-arrays in the DECIPHER database (v11.33) repository (#562946 to 563086; IMMGWHS1-140). Additional data is available in the Supplemental Data Section.
Acknowledgments
We thank all the families with WHS, and our special acknowledgements go to the AESWH and the Latin-American groups of WHS. Our special acknowledgements also to Natalia Graña, Ivana Gennari, María José Bisci, and Izaskun Ruíz.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Wright, T.J.; Ricke, D.O.; Denison, K.; Abmayr, S.; Cotter, P.D.; Hirschhorn, K.; Keinänen, M.; McDonald-McGinn, D.; Somer, M.; Spinner, N.; et al. A transcript map of the newly defined 165 kb Wolf-Hirschhorn syndrome critical region. Hum. Mol. Genet. 1997, 6, 317–324. [Google Scholar] [CrossRef] [PubMed]
- Zollino, M.; Lecce, R.; Fischetto, R.; Murdolo, M.; Faravelli, F.; Selicorni, A.; Buttè, C.; Memo, L.; Capovilla, G.; Neri, G. Mapping the Wolf-Hirschhorn syndrome phenotype outside the currently accepted WHS critical region and defining a new critical region, WHSCR-2. Am. J. Hum. Genet. 2003, 72, 590–597. [Google Scholar] [CrossRef]
- Battaglia, A.; Carey, J.C.; South, S.T. Wolf-Hirschhorn syndrome: A review and update. Am. J. Med. Genet. Part C 2015, 169, 216–223. [Google Scholar] [CrossRef]
- Zollino, M.; Doronzio, P.N. Dissecting the Wolf- Hirschhorn syndrome phenotype: WHSC1 is a neurodevelopmental gene contributing to growth delay, intellectual disability, and to the facial dysmorphism. J. Hum. Genet. 2018, 63, 859–861. [Google Scholar] [CrossRef] [PubMed]
- Gandelman, K.Y.; Gibson, L.; Meyn, M.S.; Yang-Feng, T.-L. Molecular definition of the smallest region of deletion overlap in the Wolf-Hirschhorn syndrome. Am. J. Hum. Gene 1992, 51, 571–578. [Google Scholar]
- South, S.T.; Bleyl, S.B.; Carey, J.C. Two unique patients with novel microdeletions in 4p16.3 that exclude the WHS critical regions: Implications for critical region designation. Am. J. Med. Genet. Part A 2007, 143, 2137–2142. [Google Scholar] [CrossRef]
- South, S.T.; Hannes, F.; Fisch, G.S.; Vermeesch, J.R.; Zollino, M. Pathogenic significance of deletions distal to the currently described Wolf-Hirschhorn syndrome critical regions on 4p16.3. Am. J. Med. Genet. Part C 2008, 148, 270–274. [Google Scholar] [CrossRef]
- Corrêa, T.; Mergener, R.; Leite, J.C.L.; Galera, M.F.; Moreira, L.M.D.A.; Vargas, J.E.; Riegel, M. Cytogenomic Integrative Network Analysis of the Critical Region Associated with Wolf-Hirschhorn Syndrome. Biomed. Res. Int. 2018, 2018, 5436187. [Google Scholar] [CrossRef]
- da Silva Mori, X.; Cristina, B.F.; Diéguez, M.; MLÁ, M.Á. Prevalence and geographic distribution of the Wolf-Hirschhorn syndrome in Spain. Rev. Esp. Salud Publica 2022, 96, e202206045. [Google Scholar]
- Taruscio, D.; Vittozi, L.; Rocchetti, A.; Torreri, P.; Ferrari, L. The Occurrence of 275 Rare Diseases and 47 Rare Disease Groups in Italy. Results from the National Registry of Rare Diseases. Int. J. Environ. Res. Public Health 2018, 15, 1470. [Google Scholar] [CrossRef]
- Martínez-Martín, P.; Jiménez-Jiménez, F.J.; García, E.C.; Alonso-Navarro, H.; Rubio, L.; Calleja, P.; Díaz-Sánchez, M.; Benito-León, J. Most of the Quality of Life in Essential Tremor Questionnaire (QUEST) psychometric properties resulted in satisfactory values. J. Clin. Epidemiol. 2010, 63, 767–773. [Google Scholar] [CrossRef]
- Martinez-Martin, P. Composite rating scales. J. Neurol. Sci. 2010, 289, 7–11. [Google Scholar] [CrossRef]
- Weldring, T.; Smith, S.M. Patient-Reported Outcomes (PROs) and Patient-Reported Outcome Measures (PROMs). Health Serv. Insights 2013, 6, 61–68. [Google Scholar] [PubMed]
- Relja, M. Clinical rating scales. Parkinsonism Relat. Disord. 2012, 18 (Suppl. S1), S229–S232. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Powers, J.H.; Patrick, D.L.; Walton, M.K.; Marquis, P.; Cano, S.; Hobart, J.; Isaac, M.; Vamvakas, S.; Slagle, A.; Molsen, E.; et al. Clinician-Reported Outcome Assessments of Treatment Benefit: Report of the ISPOR Clinical Outcome Assessment Emerging Good Practices Task Force John. Value Health 2017, 20, 2–14. [Google Scholar] [CrossRef]
- Austin, C.P.; Cutillo, C.M.; Lau, L.P.; Jonker, A.H.; Rath, A.; Julkowska, D.; Thomson, D.; Terry, S.F.; de Montleau, B.; Ardigò, D.; et al. Future of Rare Diseases Research 2017–2027: An IRDiRC Perspective. Clin. Transl. Sci. 2018, 11, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Goetz, C.G.; Tilley, B.C.; Shaftman, S.R.; Stebbins, G.T.; Fahn, S.; Martinez-Martin, P.; Poewe, W.; Sampaio, C.; Stern, M.B.; Dodel, R.; et al. Movement Disorder Society-sponsored revision of the Unified Parkinson’s Disease Rating Scale (MDS-UPDRS): Scale presentation and clinimetric testing results. Movement Disorder Society UPDRS Revision Task Force. Mov. Disord. 2008, 23, 2129–2170. [Google Scholar] [CrossRef]
- Hamilton, M. A rating scale for depression. J. Neurol. Neurosurg. Psychiatry 1960, 23, 5662. [Google Scholar] [CrossRef]
- Hughes, C.P.; Berg, L.; Danziger, W.L.; Coben, L.A.; Martin, R.L. A new clinical scale for the staging of dementia. Br. J. Psychiatry 1982, 140, 566–572. [Google Scholar] [CrossRef]
- Shannon, N.L.; Maltby, E.L.; Rigby, A.S.; Quarrell, O.W.J. An epidemiological study of Wolf-Hirschhorn syndrome: Life expectancy and cause of mortality. J. Med. Genet. 2001, 38, 674–679. [Google Scholar] [CrossRef]
- Battaglia, A.; Carey, J.C.; Wright, T.J. Wolf-Hirschhorn (4P-) syndrome in adults. Genet. Couns. 2001, 12, 35–48. [Google Scholar]
- Battaglia, A.; Carey, J.C. Health supervision and anticipatory guidance of individuals with Wolf-Hirschhorn syndrome. Am. J. Med. Genet. Part A 1999, 89, 111–115. [Google Scholar] [CrossRef]
- Carey, J.C.; Lortz, A.; Mendel, A.; Battaglia, A. Natural history study of adults with Wolf-Hirschhorn syndrome 2: Patient-reported outcomes study. Am. J. Med. Genet. Part A 2021, 185, 2065–2069. [Google Scholar] [CrossRef]
- Battaglia, A.; Carey, J.C. The delineation of the Wolf-Hirschhorn syndrome over six decades: Illustration of the ongoing advances in phenotype analysis and cytogenomic technology. Am. J. Med. Genet. Part A 2021, 185, 2748–2755. [Google Scholar] [CrossRef]
- Battaglia, A. Deletion 4p: Wolf-Hirschhorn syndrome. In Cassidy and Allanson’s Management of Genetic Syndromes, 4th ed.; Carey, J.C., Battaglia, A., Viskochil, D., Cassidy, S.B., Eds.; Wiley Blackwell: Hoboken, NJ, USA, 2021; pp. 265–280. 4p. [Google Scholar]
- Martínez-Quintana, E.; Rodríguez-González, F. Clinical features in adult patient with Wolf-Hirschhorn syndrome. Morphologie 2014, 98, 86–89. [Google Scholar] [CrossRef]
- Blanco-Lago, R.; Malaga-Dieguez, I.; Granizo-Martinez, J.J.; Carrera-Garcia, L.; Barruz-Galian, P.; Lapunzina, P.; Nevado-Blanco, J. Wolf-Hirschhorn syndrome. Description of a Spanish cohort of 51 cases and a literature review. Rev. Neurol. 2017, 64, 393–400. [Google Scholar] [CrossRef]
- Nevado, J.; Ho, K.S.; Zollino, M.; Blanco, R.; Cobaleda, C.; Golzio, C.; Beaudry-Bellefeuille, I.; Berrocoso, S.; Limeres, J.; Barrúz, P.; et al. International meeting on Wolf-Hirschhorn syndrome: Update on the nosology and new insights on the pathogenic mechanisms for seizures and growth delay. Am. J. Med. Genet. Part A 2020, 182, 257–267. [Google Scholar] [CrossRef]
- Cammarata-Scalisi, F.; Araque, D.; Da Silva, G.; Lacruz-Rengel, M.A.; Avendaño, A. Wolf-Hirschhorn syndrome. Description of five cases characterized by means of single nucleotide polymorphism microarrays. Arch. Argent. Pediatr. 2019, 117, e406–e412. [Google Scholar] [PubMed]
- Hastie, T.; Tibshirani, R.; Friedman, J. The Elements of Statistical Learning: Hierarchical Clustering. Stat. Sci. 2001, 16, 222–248. [Google Scholar]
- Wieczorek, D.; Krause, M.; Majewski, F.; Albrecht, B.; Horn, D.; Riess, O.; Gillessen-Kaesbach, G. Effect of the size of the deletion and clinical manifestation in Wolf–Hirschhorn syndrome: Analysis of 13 patients with a de novo deletion. Eur. J. Hum. Genet. 2000, 8, 519–526. [Google Scholar] [CrossRef]
- Zollino, M.; Di Stefano, C.; Zampino, G.; Mastroiacovo, P.; Wright, T.J.; Sorge, G.; Selicorni, A.; Tenconi, R.; Zappalà, A.; Battaglia, A.; et al. Genotype-phenotype correlations and clinical diagnostic criteria in Wolf-Hirschhorn syndrome. Am. J. Med. Genet. Part A 2000, 94, 254–261. [Google Scholar] [CrossRef]
- Zollino, M.; Murdolo, M.; Marangi, G.; Pecile, V.; Galasso, C.; Mazzanti, L.; Neri, G. On the nosology and pathogenesis of Wolf-Hirschhorn syndrome: Genotype-phenotype correlation analysis of 80 patients and literature review. Am. J. Med. Genet C 2008, 148, 257–269. [Google Scholar] [CrossRef]
- Shimizu, K.; Wakui, K.; Kosho, T.; Okamoto, N.; Mizuno, S.; Itomi, K.; Hattori, S.; Nishio, K.; Samura, O.; Kobayashi, Y.; et al. Microarray and FISH-based genotype-phenotype analysis of 22 Japanese patients with Wolf-Hirschhorn syndrome. Am. J. Med. Genet. A 2014, 164, 597–609. [Google Scholar] [CrossRef] [PubMed]
- Maas, N.M.C.; Van Buggenhout, G.; Hannes, F.; Thienpont, B.; Sanlaville, D.; Kok, K.; Midro, A.; Andrieux, J.; Anderlid, B.M.; Schoumans, J.; et al. Genotype-phenotype correlation in 21 patients with Wolf-Hirschhorn syndrome using high resolution array comparative genome hybridization (CGH). J. Med. Genet. 2008, 45, 71–80. [Google Scholar] [CrossRef]
- Mekkawy, M.K.; Kamel, A.K.; Thomas, M.M.; Ashaat, E.A.; Zaki, M.S.; Eid, O.M.; Ismail, S.; Hammad, S.A.; Megahed, H.; ElAwady, H.; et al. Clinical and genetic characterization of ten Egyptian patients with Wolf-Hirschhorn syndrome and review of literature. Mol. Genet. Genomic Med. 2021, 9, e1546. [Google Scholar] [CrossRef]
- Chaudhry, C.; Kaur, A.; Panigrahi, I.; Kaur, A. Wolf-Hirschhorn syndrome: A case series from India. Am. J. Med. Genet. A 2020, 182, 3048–3051. [Google Scholar] [CrossRef] [PubMed]
- Battaglia, A.; Filippi, T.; Carey, J.C. Update on the clinical features and natural history of Wolf-Hirschhorn (4p-) syndrome: Experience with 87 patients and recommendations for routine health supervision. Am. J. Med. Genet. Part C 2008, 148, 246–251. [Google Scholar] [CrossRef]
- Wieczorek, D.; Krause, M.; Majewski, F.; Albrecht, B.; Meinecke, P.; Riess, O.; Gillessen-Kaesbach, O. Unexpected high frequency of the novo unbalanced translocation in patients with Wolf –Hirschhorn syndrome (WHS). J. Med. Genet. 2000, 37, 798–804. [Google Scholar] [CrossRef][Green Version]
- South, S.T.; Whitby, H.; Battaglia, A.; Carey, J.C.; Brothman, A.R. Comprehensive analysis of Wolf-Hirschhorn syndrome using array CGH indicates a high prevalence of translocations. Eur. J. Hum. Genet. 2008, 16, 45–52. [Google Scholar] [CrossRef]
- Antonius, T.; Draaisma, J.; Levichenko, E.; Knoers, N.; Renier, W.; Van Ravensawaaii, C. Growth charts for Wolf-Hirschhorn (4p-) syndrome (0-4 years of age). Eur. J. Pediatr. 2008, 167, 807–810. [Google Scholar] [CrossRef]
- Calhoun, A.R.U.L.; Lortz, T.; Casper, C.; Carey, J. Extended Growth Curves for the Wolf-Hirschhorn Syndrome (4p-). Am. J. Med. Genet. A 2025, 197, e64075. [Google Scholar] [CrossRef] [PubMed]
- Kerzendorfer, C.; Hannes, F.; Colnaghi, R.; Abramowicz, I.; Carpenter, G.; Vermeesch, J.R.; O’Driscoll, M. Characterizing the functional consequences of haploinsufficiency of NELF-A (WHSC2) and SLBP identifies novel cellular phenotypes in Wolf-Hirschhorn syndrome. Hum. Mol. Genet. 2012, 21, 2181–2193. [Google Scholar] [CrossRef] [PubMed]
- Nevado, J.; Bel-Fenellós, C.; Sandoval-Talamantes, A.K.; Hernández, A.; Biencinto-López, C.; Martínez-Fernández, M.L.; Barrúz, P.; Santos-Simarro, F.; Mori-Álvarez, M.Á.; Mansilla, E.; et al. Deep Phenotyping and Genetic Characterization of a Cohort of 70 Individuals With 5p Minus Syndrome. Front Genet 2021, 12, 645595. [Google Scholar] [CrossRef] [PubMed]
- Nevado, J.; García-Miñaúr, S.; Palomares-Bralo, M.; Vallespín, E.; Guillén-Navarro, E.; Rosell, J.; Bel-Fenellós, C.; Mori, M.Á.; Milá, M.; Del Campo, M.; et al. Variability in Phelan-McDermid Syndrome in a Cohort of 210 Individuals. Front. Genet. 2022, 13, 652454. [Google Scholar] [CrossRef]
- Nevado, J.; Escalada, B.; Muñoz-GªPorrero, Y.; Adan, C.; Tenorio-Castaño, J.; Lapunzina, P.D. Genotype-Phenotype Associations in Phelan-McDermid Syndrome: Insights into Novel Genes beyond SHANK3. Int. J. Mol. Sci. 2025, 26, 4653. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).