Abstract
Inflammasomes are intracellular multiprotein complexes in the cytoplasm that regulate inflammation activation in the innate immune system in response to pathogens and to host self-derived molecules. Recent advances greatly improved our understanding of the activation of nucleotide-binding oligomerization domain-like receptor (NLR) family pyrin domain containing 3 (NLRP3) inflammasomes at the molecular level. The NLRP3 belongs to the subfamily of NLRP which activates caspase 1, thus causing the production of proinflammatory cytokines (interleukin 1β and interleukin 18) and pyroptosis. This inflammasome is involved in multiple neurodegenerative and metabolic disorders including Alzheimer’s disease, multiple sclerosis, type 2 diabetes mellitus, and gout. Therefore, therapeutic targeting to the NLRP3 inflammasome complex is a promising way to treat these diseases. Recent research advances paved the way toward drug research and development using a variety of machine learning-based and artificial intelligence-based approaches. These state-of-the-art approaches will lead to the discovery of better drugs after the training of such a system.
1. Introduction
The human body has the ability to combat a pathogenic attack with the help of two kinds of immune system, i.e., the innate and the adaptive immune systems. There are many markers of the activation of these immune systems; one of them is inflammation. The latter is an evolutionary protective immune response that is tightly controlled by the innate immune system—against pathogens, cellular debris, and harmful stimuli. The innate immune system plays an essential role in the sensing of invading pathogens and of endogenous damage signals [1]. Dysregulation of inflammatory pathways can cause insufficient or excessive inflammation that either causes persistent infection or leads to systematic inflammatory diseases, respectively.
Inflammasomes are multiprotein complexes with an intrinsic ability to initiate an innate immune response upon the recognition of a pathogen-associated molecular pattern (PAMP) or a damage-associated molecular pattern (DAMP). These molecular patterns are recognized by specialized structures, called pattern recognition receptors (PRRs), in the cytoplasm (e.g., RIG-I-like receptors: RLRs), on the cell surface, or in endosomal compartments (e.g., Toll-like receptors: TLRs) [2]. Engagement of these PRRs triggers downstream signaling pathways that lead to the production of proinflammatory cytokines [1,3]. Some of these cytokines are produced in their precursor form, which needs to be matured in order to become functionally active. This maturation requires the action of other key cellular players such as inflammasomes, which eventually cause the secretion of active cytokines from the cell as inflammatory markers. Inflammasome activation is mediated by the innate immune system; the underlying mechanism was explored recently in various studies [4,5,6].
The major components of the inflammasome complex are PRRs, including nucleotide-binding oligomerization domain (NOD)-like receptors (NLRs) and “absent in melanoma 2-like receptors” (ALRs, AIM2-like receptors) in both humans and mice [7]. So far, several inflammasomes have been identified, which include NLR family pyrin domain containing 3 (NLRP3), NLRP1, AIM2, and NLRC4 types. The NLRP3 belongs to the subfamily of NLRP with pyrin domain (PYD) at their N-terminal which is studied thoroughly due to its critical role in inflammatory and immune system-related disorders [8,9,10]. Besides, it contributes to the pathogenesis of a variety of neurodegenerative diseases (multiple sclerosis, Parkinson’s disease, and Alzheimer’s disease [AD]) and metabolic diseases (obesity, type 2 diabetes mellitus [T2D], and atherosclerosis) [11,12]. Moreover, the genetic polymorphisms and mutations in NLR-coding genes and in inflammasome sensor proteins are associated with a variety of autoimmune diseases [13,14]. This association with various diseases has led to the development of therapeutics that target inflammasome activity. The complexity of the biological system has paved the way toward cutting edge machine learning (ML) approaches in the field of discovery and development of drugs with enhanced therapeutic efficacy [15]. In this regard, virtual screening (VS) has played a critical part because it facilitates in silico screening of millions of compounds, and the latter process results in the identification of potential drugs. ML is a subset of artificial intelligence (AI) methods and is emerging as a powerful technique for VS, which compiles and trains a dataset (compounds) to classify it into known “actives” and “inactives.” The accuracy of the trained model is validated by its testing on raw datasets to characterize novel compounds with desired pharmacological properties [15,16].
The focus of this review is on our recent elucidation of NLRP3’s mechanism of activation and its participation in the pathogenesis of obesity/T2D and AD. Furthermore, we will discuss the ability of ML and AI to improve the discovery of new therapeutic approaches.
2. The NLRP3 Inflammasome
NLRP3 was initially characterized in an autoinflammatory disease named Muckle–Wells syndrome [17]. The NLRP3 inflammasome complex is mainly composed of three units: a receptor protein (NLRP3), an adaptor protein (ASC), and an effector protein (caspase 1) [18,19]. The receptor protein acts as a sensor that is switched on after sensing a PAMP and/or DAMP. The ASC adaptor protein contains two death domains: The N-terminal pyrin domain (PYD) and the C-terminal caspase recruitment domain (CARD) [19,20], which serves as a mediator between the sensor and effector protein.
The NLRP3 complex is primarily expressed in immune cells such as inflammatory and antigen-presenting cells (APCs). It is comprised of central nucleotide-binding and oligomerization domain (NBD), a C-terminal leucine-rich repeat LRR domain, and an N-terminal pyrin domain. NLRP3 as a receptor protein is stimulated by the presence of PAMPs and/or DAMPs including nucleic acids, lipooligosaccharide (LPS) and muramyl dipeptide (MDP) [21,22]. NLRP3 activation is divided into two steps: priming and activation [23]. The priming signal (first signal) includes a large number of DAMPs and/or PAMPs which activate PRR (such as TLR) signaling to stimulate the nuclear factor-κB (NFκB) pathway. This pathway promotes the transcription and expression of NLRP3 along with pro-IL-1β and pro-IL-18 that are translocated from the nucleus to cytoplasm in an inactive form [24]. Moreover, the priming signal includes injury-related factors such as oxidized low-density lipoprotein [25], whose accumulation has been identified in metabolically induced obesity-related diseases. The activating signal (second signal)—that initiates NLRP3 inflammasome stimulation—originates from a variety of activators such as PAMPs, DAMPs, exogenous adenosine, amyloid β (Aβ), mitochondrial DNA, or substances (e.g., asbestos and aluminum or silica and uric acid crystals) [26,27,28]. Furthermore, ATP-induced P2X7R activation raises K+ efflux, which is also critical for NLRP3 activation [29]. Eventually, ASC via the CARD domain mediates the recruitment of pro-caspase 1, which drives NLRP3 inflammasome assembly. The proximity to neighboring pro-caspase 1 leads to its autocleavage and conversion into mature caspase 1, which subsequently cleaves the precursor cytokines (pro-IL-1β and pro-IL-18) into their mature forms (IL-1β and IL-18) [3,30]. This event next initiates pyroptosis, an inflammatory type of programmed cell death that is controlled by gasdermin D (GSDMD) [31]. In pyroptosis, pores are formed in the plasma membrane as the N-terminal fragment of GSDMD detaches from its C-terminal inhibitory domain and attaches to phosphoinositides, which oligomerize to produce membrane pores [32,33]. The formation of membrane pores disturbs the cellular osmotic potential, thereby leading to cell swelling and lysis with the ultimate release of mature IL-1β and IL-18 into the extracellular environment [31].
So far, numerous factors have been found to initiate NLRP3 inflammasome activation; however, the exact mechanism remains unclear and represents an area of active investigation. A possible mechanism underlying the initiation of the NLRP3 inflammasome includes reactive oxygen species (ROS) production and mitochondrial dysfunction, oxidized mitochondrial DNA release, K+ efflux, a cathepsin B release from disrupted lysosomes, changes in extracellular Ca2+ ion gradients, and the formation of transmembrane pores [34,35,36,37,38,39]. Moreover, NIMA-related kinase 7 (NEK7) has been reported to bind to the LRR domain of NLRP3 thus leading to its activation and oligomerization (Figure 1) [40]. On the other hand, opposing evidence highlights the controversial role of mitochondrial ROS in the inhibition of NLRP3 activation [41]. Moreover, studies have revealed that post-translational modifications are significantly involved in NLRP3 activation [3,42,43]. Nonetheless, ubiquitination and post-translational modifications at the priming step have been found to induce NLRP3 inflammasome inactivation [44,45], whereas dephosphorylation and deubiquitination cause its activation [43,46]. Additionally, protein kinase A–associated NLRP3 phosphorylation on residue Ser291 is important for NLRP3 inflammasome inactivation [47]. Moreover, recent studies uncovered the function of microRNAs in the regulation of the NLRP3 inflammasome. For example, myeloid-derived miR-223 controls intestinal inflammation by repressing the NLRP3 inflammasome [48]. miR-33 has also been demonstrated to regulate the NLRP3 inflammasome in macrophages because this pathway plays a critical part in the development of rheumatoid arthritis [49]. This observation provides further insights into the events that epigenetic regulators induce in this inflammasome.
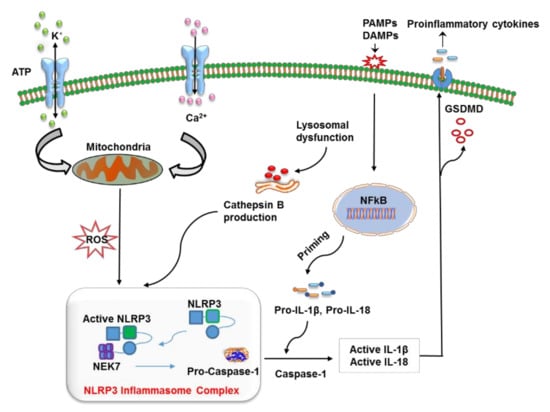
Figure 1.
The mechanism of action of the nucleotide-binding oligomerization domain-like receptor (NLR) family pyrin domain containing 3 (NLRP3) inflammasome. The priming step involves the recognition of a pathogen-associated molecular pattern (PAMP) or a damage-associated molecular pattern (DAMP) by a specific pattern recognition receptors (PRR), which activates the NF-κB pathway to release precursor forms of IL-1β and IL-18 into the cytoplasm. NLRP3 is turned on by lysosome-mediated cathepsin B, K+ efflux, reactive oxygen species (ROS) production via dysfunctional mitochondria, the release of mitochondrial DNA in oxidized form, and alterations in Ca2+ concentration. The oligomerization and activation of NLRP3 take place after it interacts with the leucine-rich repeat (LRR) domain of NEK7. This event is followed by the cleavage of pro-caspase 1 into caspase 1, which converts pro-IL-1β and pro-IL-18 into their respective mature forms, which are finally released from the cell via pores generated by gasdermin D (GSDMD) (N-terminal fragments).
Thus, numerous stimuli are recognized by their receptors and serve as first, second, or both signals to make NLRP3 active; nevertheless, further research is necessary to determine the exact mechanism.
3. Roles of NLRP3 Inflammasomes in Metabolic and Neurodegenerative Diseases
NLRP3 was initially characterized as a major causative factor of inflammation owing to NLRP3’ involvement in a group of rare heterogeneous autoinflammatory conditions, known as cryopyrin-associated periodic syndrome [50]. On the other hand, its activation by damage-associated stimuli activates innate response to tissue damage. Therefore, inflammasomes significantly contribute to the pathogenesis of various diseases including dementia, multiple sclerosis, cancer, and gout [51,52,53]. The most common form of dementia (60–80%) is Alzheimer’s disease (AD) which leads to neurodegeneration by various mechanisms such as mitochondrial dysfunction, oxidative stress, and inflammation. Metabolic disorders such as obesity and type 2 diabetes (T2D) have a strong correlation to increased risk of AD [54,55,56]. This association involves increased accumulation of amyloid-β (Aβ) which is confirmed in various mouse models [57,58,59]. Obesity, T2D, and AD are affected by the involvement of NLRP3; here, we focus on their association with each other from a therapeutic point of view.
3.1. Obesity and T2D
Anomalous activation of the innate immune system significantly contributes to the pathogenesis of metabolic disorders such as T2D [60,61]. The latter is a chronic condition that was formerly termed as adult-onset diabetes, which is characterized by hyperglycemia and—according to more recent insights—by relative insulin deficiency triggered by pancreatic β-cell dysfunction [62]. In addition to other factors, obesity is a major factor responsible for T2D worldwide. Its prevalence may further increase globally, with the highest projected prevalence rates in developing or low-income countries [63]. Therefore, deeper insights into obesity pathogenesis as a significant risk factor for T2D hold huge promise for obesity prevention and treatment [64,65].
Obesity has multifactorial pathogenesis, which includes the growth of adipocytes and increased infiltration of macrophages into adipose tissue (AT) thereby activating inflammatory pathways and causing chronic inflammation [66]. Obesity-induced alterations in adipocytes and macrophages cause insulin resistance (IR) with subsequent induction of AT fibrosis [67]. Besides energy conservation, ATs secrete adipokines, molecules that contribute (via endocrine, autocrine, and paracrine signaling mechanisms) to various physiological and pathophysiological conditions, thereby regulating inflammation and immunity, insulin sensitivity, and food intake [68]. Furthermore, a reduction in the secretion of insulin-sensitive adipokines accompanied by oversecretion of proinflammatory cytokines (TNF-α, IL-1β, and IL-6) is closely related to the etiology of various metabolic conditions. Other studies also point to the participation of NLRP3 in obesity because of its overexpression in AT [11,69,70,71,72,73]. Moreover, the results of studies on mouse models of obesity are consistent with this observation [74,75]. The release of proinflammatory cytokines (IL-1β and IL-18) is the main culprit behind the AT inflammation in obese subjects [76] and thus this contributes to the development of T2D. The detailed function of the NLRP3 inflammasome in the pathogenesis of T2D is explained in a systematic review [77].
The activation of innate-immunity cells (such as neutrophils and macrophages) owing to the emergence of a chronic proinflammatory state has been closely associated with IR [78,79]. Furthermore, the activation of inflammasomes is due to the priming signals produced by the engagement of PRRs such as TLRs [61,80,81]. These events contribute to the development of IR and liver fat storage in mice with diet-induced obesity because of macrophage infiltration into AT [82,83,84]. Additionally, overexpression of NLRP3 inflammasome components in AT is associated with the pathogenesis of obesity and therefore is directly associated with T2D, atherosclerosis, and myocardial infarction [11,85]. Increased amyloid polypeptide deposition in pancreatic islets is one of the key inducers of NLRP3 activation [86,87] via lysosomal disruption and high ROS concentrations in pancreas-infiltrating macrophages [88]. Additionally, in comparison to wild-type mice, NLRP3 knockout mice show substantial improvement in insulin sensitivity during a high-fat diet; this approach provides protection against obesity [11,89,90]. Activation of NLRP3 causes oversecretion of inflammatory cytokines such as IL-1β, which impair islet cell function and induce dysregulation of blood glucose levels, thus resulting in the development of T2D [91,92]. The surface expression of functional IL-1β receptors on pancreatic β cells and infiltrating macrophages further enhances the production of IL-1β and the diffusion of inflammatory signals through the NF-kB pathway, which might ultimately cause β-cell dysfunction [91,93]. Even the early stage of T2D is characterized by dysfunctional β cells and a decrease in insulin production.
The mechanism of IL-1β–induced IR is the reduced tyrosine phosphorylation of insulin receptor substrate 1 (IRS1) along with its mRNA expression; this factor significantly contributes to the regulation of blood glucose, thus blocking the downstream insulin signaling pathway; these changes lead to IR [94,95]. Additionally, IL-1β-induced expression of TNF-α promotes IR [95,96]. Abundance of IL-1β and IL-18 in AT stimulates CD8+ T cells thus contributing to the inflammation of AT and to IR by activation and recruitment of macrophages [97,98]. High-fat diet-induced IR in a mouse model can be reversed in the absence of IL1R1 because this approach relieves AT inflammation despite the presence of immune-cell infiltration [90,99]. Similarly, mice deficient in IL-1α are protected against obesity-induced glucose intolerance; therefore, the blockade of IL1R1 and IL-1α could be used in the treatment of IR and obesity. In this context, T2D can be treated through IL-1 antagonism, given that IL-1β has a potential to worsen the function of pancreatic β cells. On the contrary, at low levels, IL-1β activates β-cell proliferation and insulin production, which synergistically stimulate glucose disposal and inflammation [100]. These data confirm the participation of inflammatory mediators in pathological and normal metabolism. The exact mechanism of NLRP3 inflammasome activation in T2D is not completely understood; however, mitochondria have been identified as a key player in this phenomenon [101]. In obese and T2D patients, the substances secreted by dysfunctional mitochondria into the cytoplasm often serve as DAMPs, which activate the NLRP3 inflammasome. Moreover, a diet rich in fats and glucose induces the production of mitochondrial ROS owing to Miro1-induced effects on mitochondria in pancreatic β cells; these effects consequently cause an NLRP3-induced inflammatory response, thereby impairing insulin production [102,103]. Furthermore, thioredoxin (TRX)-interacting protein (TXNIP) disassociation causes the activation of NLRP3 inflammasomes [104,105]. Hence, therapeutics targeting the NLRP3 inflammasome could be employed in the treatment of T2D and obesity because considerable numbers of studies have shown the effectiveness of this strategy. The antagonists (for the associated signaling pathways) that show a good potential for the treatment of symptoms associated with T2D and obesity are shown in Table 1. Nonetheless, the detailed mechanism of inflammasome activation that leads to obesity and causes T2D as well as treatment modalities based on NLRP3 inhibition remains to be explored. In addition, the characterization of specific molecular pathways of immune–metabolic interactions (that induce organ dysfunction due to the damage caused by chronic inflammation) may also give us a new insight into the treatment of obesity and T2D. Thus, in light of various studies, a significant link has been identified connecting NLRP3 with obesity and T2D; therefore, targeting NLRP3 could be beneficial for the treatment of the above-mentioned metabolic diseases.

Table 1.
NLRP3 antagonists in type 2 diabetes mellitus (T2D) and Alzheimer’s disease (AD).
3.2. Alzheimer’s Disease
AD is the most common neurodegenerative disorder. It is clinically characterized by dementia and progressive cognitive impairment, which are caused by two main pathologies: Aβ plaques and neurofibrillary tangles [119]. The estimated yearly incidence and prevalence of AD rise significantly with age. The incidence rate varies among different age groups: among people aged between 65 and 69, the approximate incidence is 0.4%; in people aged over 90, this rate is nearly 10% [120]. A significant contributing factor to the pathogenesis of AD includes aggregation of Aβ into neurotoxic plaques [121]. Accumulation of Aβ launches several cellular responses mediated by microglia, a type of neuroimmune cell located throughout the brain [122]. Recent studies revealed that Aβ can initiate NLRP3 inflammasome signaling in microglia [123], which causes the production of proinflammatory cytokines and consequently induces inflammation [124]. Studies have uncovered the involvement of several inflammatory components including prostaglandins, chemokines, and cytokines that are expressed in postmortem brain tissues isolated from patients with neurodegenerative disorders including AD; moreover, their elevated expression has been identified in cerebrospinal fluid [125,126]. Astrocytes and microglia are the mediators of innate immunity in the brain and they sense pathogens or other inflammatory signals; this property contributes to the activation and assembly of inflammasomes and ultimately leads to caspase-1–induced maturation of the IL-1β cytokine [127,128]. Although a normal level of IL-1β is present in a healthy brain, its overproduction may cause inflammation and the associated pathological complications.
On the other hand, various studies have revealed the overexpression of IL-1β in microglia in the vicinity of Aβ plaques in animal models and AD patients [129,130]. The microglial cells in the CNS phagocytose Aβ plaques; this process initiates lysosomal destabilization and the cytosolic production of cathepsin B, which may act as an endogenous signal and make NLRP3 active [123]. Aβ-mediated NLRP3 activation has been found to upregulate IL-1β, which promotes the formation of microglial cells and the accumulation of neurotoxic inflammatory factors [123,131]. Moreover, NLRP3 triggering plays a substantial role in the pathogenesis of amyloidosis. Similarly, in a transgenic mouse model of AD, an NLRP3 knockout protects from spatial memory dysfunction and reduces the deposition of Aβ [132]. The recruitment of microglia in AD is due to the secretion of neurotoxic components produced by senile neurofibrillary plaques [133]; these cells then phagocytose Aβ deposits and further secrete proinflammatory and chemotactic cytokines to aggravate the neurotoxic effects of Aβ. This observation further supports the functions performed by the activation of endogenous NLRP3 in the brain microglial cells because of formation of a plaque [132]. Therefore, the AD pathogenesis is strongly associated with the microglia-mediated NLRP3 inflammasome activation. Additionally, the restoration of Myb1 (TOM1) also reduces Aβ pathology, thereby highlighting the importance of endosomal adaptors and their associated factors in AD pathogenesis [134]. Depending on AD progression and stage, microglia upon activation adopt the M1 phenotype, and the overexpression of proinflammatory cytokines, such as IL-1β, induces an aberration in microglial cells; this event has a negative impact on the Aβ clearance system [135,136]. Nevertheless, an M2-like phenotype is associated with the production of anti-inflammatory cytokines, which contribute to protection against damage induced by inflammation and promote tissue remodeling [137]. Furthermore, activation of NLRP3 inflammasomes induces the extracellular release of ASC particles that act as DAMPs and consequently attract surrounding macrophages [138]. These micrometer-sized ASC specks have been reported to establish a bond with Aβ and promote plaque formation and misfolded protein accumulation, as observed in the APP/PS1 model of AD [139].
Moreover, the most reliable factor underlying the pathogenesis of AD is chronic localized neuroinflammation. Dysregulation of the interaction pattern between microglia and brain neurons is thought to be a contributing factor of AD pathogenesis [140,141]. The overproduction of cytotoxic molecules and proinflammatory cytokines by brain-resident immune cells, such as microglia, launches signaling pathways in neurons, consequently inducing brain tissue damage [142]. Numerous studies have pointed out that overexpression of IL-1β aggravates AD pathogenesis, owing to tau hyperphosphorylation [143], which inhibits long-term potentiation and affects synaptic plasticity [144,145]. Furthermore, IL-1β inhibition in a mouse model has yielded disease-modifying improvements in the pathology of AD [146]. A recent study suggests that a small-molecule NLRP3 inhibitor (JC-124) exerts a beneficial effect on a mouse model of AD [10], similarly to a knockout mouse model that manifested an improvement in spatial memory [132]. Neuronal damage results in the production of proinflammatory cytokines (IL-1β, TNF-α, and IL-6) and triggers apoptotic mitogen-activated protein kinase p38 (MAPK) [147]. P38 MAPK causes glutamate-mediated neurotoxicity via the N-methyl D-aspartic acid receptor [148,149]. Furthermore, IL-1β production induces nitric oxide synthase (iNOS) surrounding the hippocampus; this induction consequently causes damage and neuronal death [150]. IL-1β expression is significantly associated with NLRP3 inflammasome activation, and pyroptosis induced by the inflammasome is an active area of research. Accordingly, deep insight into the mechanism of NLRP3 inflammasome regulation is urgently needed to further unravel AD pathogenesis.
Moreover, the NLRP3 inflammasome is an attractive drug target in AD and subsequently provides neuroprotection. The development of anti-AD drugs that control the activation of NLRP3 inflammasomes may be a promising way to tackle neuroinflammation. The antagonists for the associated signaling pathways showing the potential to slow down AD progression are listed in Table 1.
The aforementioned studies have provided significant insights into the role NLRP3 inflammasomes play in AD progression; therefore, detailed investigation into the mechanism of inflammasome activation and its contribution to neuroinflammation will be worthwhile. Moreover, Aβ accumulation induces microglial activation via advanced glycation end product (AGE) pathways and TLR [151,152]. All these results support the usefulness of NLRP3 inflammasomes and of their downstream regulators in the identification of protein aggregates or peptides that can drive the pathogenesis of such diseases as systemic amyloidosis, prion diseases, AD, and T2D. Targeting of components of the NLRP3 inflammasome, especially at the initial stages of the disease, may reduce the formation and aggregation of Aβ plaques to delay neurological damage in these patients.
4. AI-Based Interventions in Advanced Therapeutics
The complexity of a biological system in the normal physiological condition as well as in the development of disease can now be systematically explored, and the relevant data can be mined at a faster rate using cutting edge technologies. Moreover, therapeutic development pipelines, which have been expensive, time-consuming, and complex processes, are being revolutionized by computational and high-throughput techniques. The emergence of high-throughput techniques with applications to biology and medicine gives the pharmaceutical and biotechnology industries unprecedented opportunities and challenges. In the present era, the process of drug development is increasingly dependent on the omics technology owing to its substantial role in the investigation of disease etiology, in identification of druggable targets, and in quality control of drugs throughout their life cycle [153].
Drug discovery is a complex and lengthy process which is composed of four broad stages: (a) selection and validation of target; (b) screening of compound and its lead optimization; (c) preclinical studies; and (d) clinical trials. The first step involves the identification of a disease-associated target which is done by bioinformatics predictions, proteomic and genomic analysis, and genetic and cellular target evaluation. In the next step, target-specific hits are identified from molecular libraries by applying methods such as virtual screening, high-throughput screening, and combinatorial chemistry. The functional properties of drug candidates can be improved by combining in silico and structure–activity studies with cell-based functional tests. Later, in vivo analyses such as toxicity and pharmacokinetics are performed in various animal models. Finally, compounds successfully passing preclinical stages get entered into clinical trials on patients. The clinical evaluation consists of three phases: Phase I involves testing of drug safety on a small number of humans, Phase II involves testing of drug efficacy on a small number of patients with associated disease, and Phase III involves testing drug efficacy on a large number of patients. After confirming the safety and efficacy, compounds are approved and commercialized by the agencies such as FDA. The estimated cost of traditional drug discovery is around 2.6 billion USD with a timeline over 12 years. The huge cost and timeline are the main concerns for most of the pharmaceutical companies. These days, it is becoming possible to improve cost and time by implementing AI-based methods at different stages of drug design and development. For example, AI is being used in cell classification [154], cell sorting [155], calculating compound properties [156], designing new drug-like molecules [157], computer-aided synthesis of compounds [158,159], predicting the 3D structure of targets, and assay development [160,161,162,163]. These processes are hard to perform but can be optimized and automated by implementing the AI-approaches which could significantly speed up the drug discovery process.
AI includes computational methodologies that simulate or mimic the procedures supported by human intelligence including sensory understanding, learning, reasoning, interaction, and adaptation. AI implications can be found in various fields like image and voice recognition, natural language processing, expert systems, and robotics. Rapidly growing and dynamic methods of AI ensure its applications in the field of medicine as well (Figure 2) [164]. The successful entry of AI into the field of drug discovery has received much attention due to the penetration of AI into all stages of R&D related to drug discovery. AI has helped to discover novel biologically active molecules through ML and deep learning (DL) algorithms on the previously generated quantitative structure–activity relationships (QSARs) and quantitative structure–property relationships (QSPRs) [165].
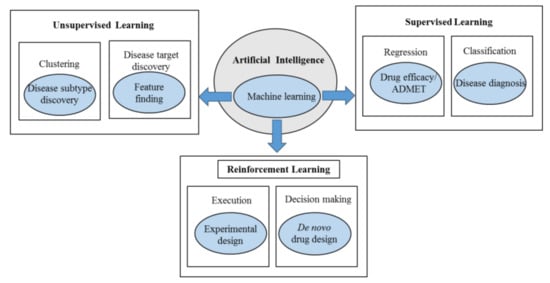
Figure 2.
The applications of artificial intelligence (AI) and its subset (machine learning) in disease diagnosis and drug development.
Investigation of early-phase drug discovery and development has been focused on two levels: activity prediction and classification of molecules. For activity prediction, ML methods including the support vector machine (SVM) algorithm, random forest method, and Bayesian neural networks (BNN) have been employed in the analysis of biological activity of molecules. As far as classification of molecules is concerned, logistic regression, neural networks (NN), and SVM algorithms have been applied to druglike and nondruglike classification. Naïve Bayes (NB) and k-nearest neighbor (KNN) algorithms have also been used to distinguish active molecules from inactive ones. SVM and naïve Bayesian classifications have been successfully employed to categorize lymphocyte-specific protein tyrosine kinase, cytochrome P450, and butyrylcholinesterase inhibitors [166]. Further studies also confirmed the use of SVM-based algorithms to rank molecules based on their activity, whereas BNN and RF are also utilized for activity prediction [167,168,169,170]. More recently a virtual screening was performed to identify cyclin-dependent kinase 2 (CDK2) inhibitors by utilizing protein–ligand interaction fingerprints (PLIF), docking, and SVM. This multistage virtual screening has led to the identification of two novel CDK2 inhibitors that successfully displayed selective inhibition against CDK2 [171]. Table 2 shows programs using ML techniques.

Table 2.
Algorithms/programs using machine learning (ML) techniques.
For VS comparison studies, SVM is extremely reliable [181,182] and has been found to identify novel compounds. This algorithm has been successfully employed to find PTP1B inhibitors for the effective treatment of T2D. In this context, five compounds have been identified, out of which two have been experimentally confirmed to have a better inhibitory effect [182]. Moreover, SVM-based computational workflow was utilized for molecular docking calculations to investigate novel inhibitors of c-Met tyrosine kinase.
However, the evaluation of various virtual screening methods is significantly important to confirm their reliability and output. The quality of the evaluation is directly associated with the quality and availability of benchmarking datasets. The successful utilization of benchmarking datasets to optimize a virtual screening methodology has led to the identification of novel compounds. In this context, several benchmarking datasets are available. The DUD-E database is composed of a large number of datasets with various targets such as ion channels and GPCRs (102 protein targets) with clustered ligands (22886) extracted from ChEMBL [183]. The DUD-E database was designed to address some shortcomings of the original DUD version which are particularly related to the weakness of ligand and decoy as charge was not included at the time of property-matching selection of the decoys. Similarly, the DEKOIS 2.0 library is composed of novel 81 structurally distinct benchmark datasets for a huge variety of target classes which could be used for the identification of both decoys and active compounds. This database also contains the information on non-classical binding sites i.e., allosteric binding sites or target protein–protein interaction [184]. Nuclear receptors (NRs) belong to an important class of proteins for drug-targeting so their associated ligands and structures are being evaluated by the Nuclear Receptors Ligands and Structures Benchmarking Database (NRLiSt BDB) [185]. This database contains both agonists and antagonists for 27 human NRs based on experimentally-resolved ligands and target structures which assist in assessing the performance of virtual screening techniques for NRs. Histone deacetylases (HDACs) are an important class of drug targets for the treatment of neurodegenerative diseases, cancers, and other types of diseases. The maximal unbiased benchmarking datasets were constructed to facilitate the discovery of their associated inhibitors. The relevant database is composed of 14 datasets: five of them (HDAC5, HDAC6, HDAC9, HDAC10, and HDAC11) were used to assess ligand-based virtual screening as no experimentally-resolved structures are available for these protein targets [186,187]. More recently, the DeepScreening web server, designed with an integration of deep learning-based algorithms, uses either the user-provided or publically available datasets to assist virtual screening of drugs against the targets of interest [173].
Recently, DL approaches were developed during research on artificial neurons; the purpose was to design the algorithms that automatically discover convoluted patterns and high-level features in large datasets. Such ML algorithms can deal with a diverse and large dataset and uncover complicated relations in the data [188]. Moreover, DL includes a class of ML algorithms that are skilled enough to combine raw inputs into layers of intermediate attributes. Such DL techniques can really help to decipher problems associated with data-rich disciplines, as automated algorithms mine a significant pattern that could lead to actionable knowledge and change how we study diseases, categorize patients, and treat diseases [165]. The development of therapeutics for polygenic and multifactorial diseases is a cumbersome process. In this context, the polypharmacology of compounds seems promising for treating multifactorial diseases such as T2D and AD because it enables a single drug to inhibit multiple targets; this situation may increase its effectiveness against diseases. This idea has led to the development of approaches to the screening of multitargeted directed ligands (MTDLs) [189]. Recent studies utilized VS for AD drug screening for MTDLs that are intended to inhibit multiple associated targets. In this regard, two significant targets—GSK-3β and CDK5—were inhibited by means of sequential docking to screen compounds, whereas ligand-based virtual screening was performed in another study on inhibition of GSK-3β and BACE1 [190,191]. Nonetheless, recursive partitioning (RP) and NB, ML-based VS methods were used to screen compounds for MTDLs against AD. Screening against 25 targets including GSK-3β, BACE1, CDK5, APP, and mAChR (M1 subtype) was performed to search for the compounds that show bonding with a maximum number of targets. Recently available AD-related drugs have been used to further validate this model.
ANN has emerged as an efficient algorithm, and there is a high-performance technique for ANN-based VS against various diseases such as AD and T2D. The ease with which multitask learning (MTL) can be implemented by ANN makes it suitable for screening of candidate compounds for MTDLs. Moreover, the convolutional neural network (CNN) and its application in QSAR modeling such as AtomNet™ make the prediction of small molecule binding to protein targets more promising. Here we propose a more efficient way to perform VS: by means of deep CNN against MTDLs that inhibit multiple drug targets associated with the aforementioned diseases. In case of MTDLs, it is important not to include those targets that are critical for normal physiological functioning and to not interfere with critical pathways ensuring normal homeostasis. Furthermore, the data should be retrieved from the chemogenomic libraries that serve as a training dataset and should include many known inhibitors against the target of interest. These data should be preprocessed as per the standard procedures prior to the use of these data to train and validate CNN internally. The selection of a specific CNN architecture is an area of further research and cannot be suggested here.
Accordingly, if the model is accurately constructed, it can then be implemented on large datasets that are composed of compounds different from the molecules present in the initial training and data testing. The molecules from the top hits should next be tested experimentally to measure the accuracy and efficacy of each selected compound. In conclusion, extensive research activities are underway to integrate AI tools in order to expedite the drug discovery process, but more research is necessary to achieve the full potential of AI in the context of drug discovery and development.
5. Concluding Remarks
The proper activation of the immune system is beneficial for the human body in order to combat various immune, inflammatory, degenerative, and metabolic diseases. A slight imbalance in a system could induce various metabolic variations at a cellular or organismic level. These variations activate immune cells which consequently switch on the NLRP3 inflammasome. Being a significant component of the innate immune system, this inflammasome plays a crucial part in metabolic and neurodegenerative disorders such as T2D and AD, respectively. Regardless of the complexity of the pathway, some progress has been made in the development of therapeutics that target the NLRP3 inflammasome and its associated pathways. Nevertheless, further insight is necessary to fully elucidate the pathways that will increase our understanding how to locate precise drug targets and which ones may lead to better treatments. Currently, a variety of inhibitors are available that target activation of the NLRP3 inflammasome and that have been proven to be effective in relieving the symptoms of T2D and AD in patients or in animal models. On the other hand, an advanced therapeutic intervention into such multifactorial diseases is needed to obtain better therapeutic results. In this regard, the research on a cutting edge technology such as AI and ML is laying the foundation for the development of therapeutics with greater efficacy. Moreover, such multifactorial diseases as T2D and AD may be treated effectively by means of VS with deep CNN against MTDLs.
Author Contributions
Writing—Original draft preparation and visualization, R.H.P., N.J. and R.H.P.; Conceptualization and Writing—Review and editing, S.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the National Research Foundation of Korea, grant numbers NRF-2019M3A9A8065098, 2019M3D1A1078940 and 2019R1A6A1A11051471.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Lamkanfi, M.; Dixit, V.M. Mechanisms and functions of inflammasomes. Cell 2014, 157, 1013–1022. [Google Scholar] [CrossRef]
- Kanneganti, T.D. The inflammasome: Firing up innate immunity. Immunol. Rev. 2015, 265, 1–5. [Google Scholar] [CrossRef]
- Yang, Y.; Wang, H.; Kouadir, M.; Song, H.; Shi, F. Recent advances in the mechanisms of NLRP3 inflammasome activation and its inhibitors. Cell Death Dis. 2019, 10, 128. [Google Scholar] [CrossRef]
- Jin, C.; Flavell, R.A. Molecular mechanism of NLRP3 inflammasome activation. J. Clin. Immunol. 2010, 30, 628–631. [Google Scholar] [CrossRef]
- Petrilli, V.; Dostert, C.; Muruve, D.A.; Tschopp, J. The inflammasome: A danger sensing complex triggering innate immunity. Curr. Opin. Immunol. 2007, 19, 615–622. [Google Scholar] [CrossRef]
- Bryant, C.; Fitzgerald, K.A. Molecular mechanisms involved in inflammasome activation. Trends Cell Biol. 2009, 19, 455–464. [Google Scholar] [CrossRef]
- Takeuchi, O.; Akira, S. Pattern recognition receptors and inflammation. Cell 2010, 140, 805–820. [Google Scholar] [CrossRef]
- Schroder, K.; Zhou, R.; Tschopp, J. The NLRP3 inflammasome: A sensor for metabolic danger? Science 2010, 327, 296–300. [Google Scholar] [CrossRef]
- Strowig, T.; Henao-Mejia, J.; Elinav, E.; Flavell, R. Inflammasomes in health and disease. Nature 2012, 481, 278–286. [Google Scholar] [CrossRef]
- Yin, J.; Zhao, F.; Chojnacki, J.E.; Fulp, J.; Klein, W.L.; Zhang, S.; Zhu, X. NLRP3 Inflammasome Inhibitor Ameliorates Amyloid Pathology in a Mouse Model of Alzheimer’s Disease. Mol. Neurobiol. 2018, 55, 1977–1987. [Google Scholar] [CrossRef]
- Vandanmagsar, B.; Youm, Y.H.; Ravussin, A.; Galgani, J.E.; Stadler, K.; Mynatt, R.L.; Ravussin, E.; Stephens, J.M.; Dixit, V.D. The NLRP3 inflammasome instigates obesity-induced inflammation and insulin resistance. Nat. Med. 2011, 17, 179–188. [Google Scholar] [CrossRef]
- Freeman, L.C.; Ting, J.P. The pathogenic role of the inflammasome in neurodegenerative diseases. J. Neurochem. 2016, 136 Suppl 1, 29–38. [Google Scholar] [CrossRef]
- Cordero, M.D.; Alcocer-Gomez, E.; Ryffel, B. Gain of function mutation and inflammasome driven diseases in human and mouse models. J. Autoimmun. 2018, 91, 13–22. [Google Scholar] [CrossRef]
- Da Silva, W.C.; Reis, E.C.; Oshiro, T.M.; Pontillo, A. Genetics of Inflammasomes. Exp. Suppl. 2018, 108, 321–341. [Google Scholar] [CrossRef]
- Murphy, R.F. An active role for machine learning in drug development. Nat. Chem. Biol. 2011, 7, 327–330. [Google Scholar] [CrossRef]
- Carpenter, K.A.; Huang, X. Machine Learning-based Virtual Screening and Its Applications to Alzheimer’s Drug Discovery: A Review. Curr. Pharm. Des. 2018, 24, 3347–3358. [Google Scholar] [CrossRef]
- Martinon, F.; Burns, K.; Tschopp, J. The inflammasome: A molecular platform triggering activation of inflammatory caspases and processing of proIL-beta. Mol. Cell 2002, 10, 417–426. [Google Scholar] [CrossRef]
- von Moltke, J.; Ayres, J.S.; Kofoed, E.M.; Chavarria-Smith, J.; Vance, R.E. Recognition of bacteria by inflammasomes. Annu. Rev. Immunol. 2013, 31, 73–106. [Google Scholar] [CrossRef]
- Rathinam, V.A.; Fitzgerald, K.A. Inflammasome Complexes: Emerging Mechanisms and Effector Functions. Cell 2016, 165, 792–800. [Google Scholar] [CrossRef]
- Broz, P.; Dixit, V.M. Inflammasomes: Mechanism of assembly, regulation and signalling. Nat. Rev. Immunol. 2016, 16, 407–420. [Google Scholar] [CrossRef]
- Kanneganti, T.D.; Body-Malapel, M.; Amer, A.; Park, J.H.; Whitfield, J.; Franchi, L.; Taraporewala, Z.F.; Miller, D.; Patton, J.T.; Inohara, N.; et al. Critical role for Cryopyrin/Nalp3 in activation of caspase-1 in response to viral infection and double-stranded RNA. J. Biol. Chem. 2006, 281, 36560–36568. [Google Scholar] [CrossRef]
- Marina-Garcia, N.; Franchi, L.; Kim, Y.G.; Miller, D.; McDonald, C.; Boons, G.J.; Nunez, G. Pannexin-1-mediated intracellular delivery of muramyl dipeptide induces caspase-1 activation via cryopyrin/NLRP3 independently of Nod2. J. Immunol. 2008, 180, 4050–4057. [Google Scholar] [CrossRef]
- Ozaki, E.; Campbell, M.; Doyle, S.L. Targeting the NLRP3 inflammasome in chronic inflammatory diseases: Current perspectives. J. Inflamm. Res. 2015, 8, 15–27. [Google Scholar] [CrossRef]
- Franchi, L.; Eigenbrod, T.; Munoz-Planillo, R.; Ozkurede, U.; Kim, Y.G.; Arindam, C.; Gale, M., Jr.; Silverman, R.H.; Colonna, M.; Akira, S.; et al. Cytosolic double-stranded RNA activates the NLRP3 inflammasome via MAVS-induced membrane permeabilization and K+ efflux. J. Immunol. 2014, 193, 4214–4222. [Google Scholar] [CrossRef]
- Sheedy, F.J.; Grebe, A.; Rayner, K.J.; Kalantari, P.; Ramkhelawon, B.; Carpenter, S.B.; Becker, C.E.; Ediriweera, H.N.; Mullick, A.E.; Golenbock, D.T.; et al. CD36 coordinates NLRP3 inflammasome activation by facilitating intracellular nucleation of soluble ligands into particulate ligands in sterile inflammation. Nat. Immunol. 2013, 14, 812–820. [Google Scholar] [CrossRef]
- Chen, M.; Lu, X.; Lu, C.; Shen, N.; Jiang, Y.; Chen, M.; Wu, H. Soluble uric acid increases PDZK1 and ABCG2 expression in human intestinal cell lines via the TLR4-NLRP3 inflammasome and PI3K/Akt signaling pathway. Arthritis Res. Ther. 2018, 20, 20. [Google Scholar] [CrossRef]
- Latz, E.; Xiao, T.S.; Stutz, A. Activation and regulation of the inflammasomes. Nat. Rev. Immunol. 2013, 13, 397–411. [Google Scholar] [CrossRef]
- Zhao, L.R.; Xing, R.L.; Wang, P.M.; Zhang, N.S.; Yin, S.J.; Li, X.C.; Zhang, L. NLRP1 and NLRP3 inflammasomes mediate LPS/ATPinduced pyroptosis in knee osteoarthritis. Mol. Med. Rep. 2018, 17, 5463–5469. [Google Scholar] [CrossRef]
- Franchi, L.; Kanneganti, T.D.; Dubyak, G.R.; Nunez, G. Differential requirement of P2X7 receptor and intracellular K+ for caspase-1 activation induced by intracellular and extracellular bacteria. J. Biol. Chem. 2007, 282, 18810–18818. [Google Scholar] [CrossRef]
- Kesavardhana, S.; Kanneganti, T.D. Mechanisms governing inflammasome activation, assembly and pyroptosis induction. Int. Immunol. 2017, 29, 201–210. [Google Scholar] [CrossRef]
- Shi, J.; Gao, W.; Shao, F. Pyroptosis: Gasdermin-Mediated Programmed Necrotic Cell Death. Trends Biochem. Sci. 2017, 42, 245–254. [Google Scholar] [CrossRef] [PubMed]
- Shi, J.; Zhao, Y.; Wang, K.; Shi, X.; Wang, Y.; Huang, H.; Zhuang, Y.; Cai, T.; Wang, F.; Shao, F. Cleavage of GSDMD by inflammatory caspases determines pyroptotic cell death. Nature 2015, 526, 660–665. [Google Scholar] [CrossRef] [PubMed]
- Ding, J.; Wang, K.; Liu, W.; She, Y.; Sun, Q.; Shi, J.; Sun, H.; Wang, D.C.; Shao, F. Pore-forming activity and structural autoinhibition of the gasdermin family. Nature 2016, 535, 111–116. [Google Scholar] [CrossRef] [PubMed]
- Petrilli, V.; Papin, S.; Dostert, C.; Mayor, A.; Martinon, F.; Tschopp, J. Activation of the NALP3 inflammasome is triggered by low intracellular potassium concentration. Cell Death Differ. 2007, 14, 1583–1589. [Google Scholar] [CrossRef] [PubMed]
- Shimada, K.; Crother, T.R.; Karlin, J.; Dagvadorj, J.; Chiba, N.; Chen, S.; Ramanujan, V.K.; Wolf, A.J.; Vergnes, L.; Ojcius, D.M.; et al. Oxidized mitochondrial DNA activates the NLRP3 inflammasome during apoptosis. Immunity 2012, 36, 401–414. [Google Scholar] [CrossRef] [PubMed]
- Zhou, R.; Yazdi, A.S.; Menu, P.; Tschopp, J. A role for mitochondria in NLRP3 inflammasome activation. Nature 2011, 469, 221–225. [Google Scholar] [CrossRef] [PubMed]
- Hornung, V.; Latz, E. Critical functions of priming and lysosomal damage for NLRP3 activation. Eur. J. Immunol. 2010, 40, 620–623. [Google Scholar] [CrossRef]
- Rossol, M.; Pierer, M.; Raulien, N.; Quandt, D.; Meusch, U.; Rothe, K.; Schubert, K.; Schoneberg, T.; Schaefer, M.; Krugel, U.; et al. Extracellular Ca2+ is a danger signal activating the NLRP3 inflammasome through G protein-coupled calcium sensing receptors. Nat. Commun. 2012, 3, 1329. [Google Scholar] [CrossRef]
- Locovei, S.; Wang, J.; Dahl, G. Activation of pannexin 1 channels by ATP through P2Y receptors and by cytoplasmic calcium. Febs Lett. 2006, 580, 239–244. [Google Scholar] [CrossRef]
- He, Y.; Zeng, M.Y.; Yang, D.; Motro, B.; Nunez, G. NEK7 is an essential mediator of NLRP3 activation downstream of potassium efflux. Nature 2016, 530, 354–357. [Google Scholar] [CrossRef]
- Bauernfeind, F.; Bartok, E.; Rieger, A.; Franchi, L.; Nunez, G.; Hornung, V. Cutting edge: Reactive oxygen species inhibitors block priming, but not activation, of the NLRP3 inflammasome. J. Immunol. 2011, 187, 613–617. [Google Scholar] [CrossRef] [PubMed]
- Juliana, C.; Fernandes-Alnemri, T.; Kang, S.; Farias, A.; Qin, F.; Alnemri, E.S. Non-transcriptional priming and deubiquitination regulate NLRP3 inflammasome activation. J. Biol. Chem. 2012, 287, 36617–36622. [Google Scholar] [CrossRef] [PubMed]
- Patel, M.N.; Carroll, R.G.; Galvan-Pena, S.; Mills, E.L.; Olden, R.; Triantafilou, M.; Wolf, A.I.; Bryant, C.E.; Triantafilou, K.; Masters, S.L. Inflammasome Priming in Sterile Inflammatory Disease. Trends Mol. Med. 2017, 23, 165–180. [Google Scholar] [CrossRef] [PubMed]
- Stutz, A.; Kolbe, C.C.; Stahl, R.; Horvath, G.L.; Franklin, B.S.; van Ray, O.; Brinkschulte, R.; Geyer, M.; Meissner, F.; Latz, E. NLRP3 inflammasome assembly is regulated by phosphorylation of the pyrin domain. J. Exp. Med. 2017, 214, 1725–1736. [Google Scholar] [CrossRef]
- Spalinger, M.R.; Kasper, S.; Gottier, C.; Lang, S.; Atrott, K.; Vavricka, S.R.; Scharl, S.; Raselli, T.; Frey-Wagner, I.; Gutte, P.M.; et al. NLRP3 tyrosine phosphorylation is controlled by protein tyrosine phosphatase PTPN22. J. Clin. Investig. 2016, 126, 1783–1800. [Google Scholar] [CrossRef]
- Py, B.F.; Kim, M.S.; Vakifahmetoglu-Norberg, H.; Yuan, J. Deubiquitination of NLRP3 by BRCC3 critically regulates inflammasome activity. Mol. Cell 2013, 49, 331–338. [Google Scholar] [CrossRef]
- Guo, C.; Xie, S.; Chi, Z.; Zhang, J.; Liu, Y.; Zhang, L.; Zheng, M.; Zhang, X.; Xia, D.; Ke, Y.; et al. Bile Acids Control Inflammation and Metabolic Disorder through Inhibition of NLRP3 Inflammasome. Immunity 2016, 45, 802–816. [Google Scholar] [CrossRef]
- Neudecker, V.; Haneklaus, M.; Jensen, O.; Khailova, L.; Masterson, J.C.; Tye, H.; Biette, K.; Jedlicka, P.; Brodsky, K.S.; Gerich, M.E.; et al. Myeloid-derived miR-223 regulates intestinal inflammation via repression of the NLRP3 inflammasome. J. Exp. Med. 2017, 214, 1737–1752. [Google Scholar] [CrossRef]
- Xie, Q.; Wei, M.; Zhang, B.; Kang, X.; Liu, D.; Zheng, W.; Pan, X.; Quan, Y.; Liao, D.; Shen, J. MicroRNA33 regulates the NLRP3 inflammasome signaling pathway in macrophages. Mol. Med. Rep. 2018, 17, 3318–3327. [Google Scholar] [CrossRef]
- Rowczenio, D.M.; Gomes, S.M.; Arostegui, J.I.; Mensa-Vilaro, A.; Omoyinmi, E.; Trojer, H.; Baginska, A.; Baroja-Mazo, A.; Pelegrin, P.; Savic, S.; et al. Late-Onset Cryopyrin-Associated Periodic Syndromes Caused by Somatic NLRP3 Mosaicism-UK Single Center Experience. Front. Immunol. 2017, 8, 1410. [Google Scholar] [CrossRef]
- Jiang, D.; Chen, S.; Sun, R.; Zhang, X.; Wang, D. The NLRP3 inflammasome: Role in metabolic disorders and regulation by metabolic pathways. Cancer Lett. 2018, 419, 8–19. [Google Scholar] [CrossRef] [PubMed]
- He, Q.; Fu, Y.; Tian, D.; Yan, W. The contrasting roles of inflammasomes in cancer. Am. J. Cancer Res. 2018, 8, 566–583. [Google Scholar] [PubMed]
- Lang, Y.; Chu, F.; Shen, D.; Zhang, W.; Zheng, C.; Zhu, J.; Cui, L. Role of Inflammasomes in Neuroimmune and Neurodegenerative Diseases: A Systematic Review. Mediat. Inflamm. 2018, 2018, 1549549. [Google Scholar] [CrossRef]
- Ott, A.; Stolk, R.; Van Harskamp, F.; Pols, H.; Hofman, A.; Breteler, M. Diabetes mellitus and the risk of dementia: The Rotterdam Study. Neurology 1999, 53, 1937. [Google Scholar] [CrossRef] [PubMed]
- Akter, K.; Lanza, E.A.; Martin, S.A.; Myronyuk, N.; Rua, M.; Raffa, R.B. Diabetes mellitus and Alzheimer’s disease: Shared pathology and treatment? Br. J. Clin. Pharmacol. 2011, 71, 365–376. [Google Scholar] [CrossRef] [PubMed]
- Kroner, Z. The Relationship between Alzheimer’s Disease and Diabetes: Type 3 Diabetes. Altern. Med. Rev. 2009, 14. [Google Scholar]
- Ho, L.; Qin, W.; Pompl, P.N.; Xiang, Z.; Wang, J.; Zhao, Z.; Peng, Y.; Cambareri, G.; Rocher, A.; Mobbs, C.V. Diet-induced insulin resistance promotes amyloidosis in a transgenic mouse model of Alzheimer’s disease. Faseb J. 2004, 18, 902–904. [Google Scholar] [CrossRef]
- Jolivalt, C.G.; Hurford, R.; Lee, C.A.; Dumaop, W.; Rockenstein, E.; Masliah, E. Type 1 diabetes exaggerates features of Alzheimer’s disease in APP transgenic mice. Exp. Neurol. 2010, 223, 422–431. [Google Scholar] [CrossRef]
- Takeda, S.; Sato, N.; Uchio-Yamada, K.; Sawada, K.; Kunieda, T.; Takeuchi, D.; Kurinami, H.; Shinohara, M.; Rakugi, H.; Morishita, R. Diabetes-accelerated memory dysfunction via cerebrovascular inflammation and Aβ deposition in an Alzheimer mouse model with diabetes. Proc. Natl. Acad. Sci. USA 2010, 107, 7036–7041. [Google Scholar] [CrossRef]
- Kanneganti, T.D.; Dixit, V.D. Immunological complications of obesity. Nat. Immunol. 2012, 13, 707–712. [Google Scholar] [CrossRef]
- Donath, M.Y.; Shoelson, S.E. Type 2 diabetes as an inflammatory disease. Nat. Rev. Immunol. 2011, 11, 98–107. [Google Scholar] [CrossRef] [PubMed]
- Scheen, A.J. Pathophysiology of type 2 diabetes. Acta Clin. Belg. 2003, 58, 335–341. [Google Scholar] [CrossRef] [PubMed]
- Magliano, D.J.; Islam, R.M.; Barr, E.L.M.; Gregg, E.W.; Pavkov, M.E.; Harding, J.L.; Tabesh, M.; Koye, D.N.; Shaw, J.E. Trends in incidence of total or type 2 diabetes: Systematic review. Bmj 2019, 366, l5003. [Google Scholar] [CrossRef] [PubMed]
- Henao-Mejia, J.; Elinav, E.; Thaiss, C.A.; Flavell, R.A. Inflammasomes and metabolic disease. Annu. Rev. Physiol. 2014, 76, 57–78. [Google Scholar] [CrossRef]
- Eckel, R.H.; Kahn, S.E.; Ferrannini, E.; Goldfine, A.B.; Nathan, D.M.; Schwartz, M.W.; Smith, R.J.; Smith, S.R. Obesity and type 2 diabetes: What can be unified and what needs to be individualized? J. Clin. Endocrinol. Metab. 2011, 96, 1654–1663. [Google Scholar] [CrossRef]
- Weisberg, S.P.; McCann, D.; Desai, M.; Rosenbaum, M.; Leibel, R.L.; Ferrante, A.W., Jr. Obesity is associated with macrophage accumulation in adipose tissue. J. Clin. Investig. 2003, 112, 1796–1808. [Google Scholar] [CrossRef]
- Thomas, D.; Apovian, C. Macrophage functions in lean and obese adipose tissue. Metab. Clin. Exp. 2017, 72, 120–143. [Google Scholar] [CrossRef]
- Francisco, V.; Pino, J.; Gonzalez-Gay, M.A.; Mera, A.; Lago, F.; Gomez, R.; Mobasheri, A.; Gualillo, O. Adipokines and inflammation: Is it a question of weight? Br. J. Pharmacol. 2018, 175, 1569–1579. [Google Scholar] [CrossRef]
- Esser, N.; L’Homme, L.; De Roover, A.; Kohnen, L.; Scheen, A.J.; Moutschen, M.; Piette, J.; Legrand-Poels, S.; Paquot, N. Obesity phenotype is related to NLRP3 inflammasome activity and immunological profile of visceral adipose tissue. Diabetologia 2013, 56, 2487–2497. [Google Scholar] [CrossRef]
- Yin, Z.; Deng, T.; Peterson, L.E.; Yu, R.; Lin, J.; Hamilton, D.J.; Reardon, P.R.; Sherman, V.; Winnier, G.E.; Zhan, M.; et al. Transcriptome analysis of human adipocytes implicates the NOD-like receptor pathway in obesity-induced adipose inflammation. Mol. Cell. Endocrinol. 2014, 394, 80–87. [Google Scholar] [CrossRef]
- Bando, S.; Fukuda, D.; Soeki, T.; Nishimoto, S.; Uematsu, E.; Matsuura, T.; Ise, T.; Tobiume, T.; Yamaguchi, K.; Yagi, S.; et al. Expression of NLRP3 in subcutaneous adipose tissue is associated with coronary atherosclerosis. Atherosclerosis 2015, 242, 407–414. [Google Scholar] [CrossRef] [PubMed]
- Kursawe, R.; Dixit, V.D.; Scherer, P.E.; Santoro, N.; Narayan, D.; Gordillo, R.; Giannini, C.; Lopez, X.; Pierpont, B.; Nouws, J.; et al. A Role of the Inflammasome in the Low Storage Capacity of the Abdominal Subcutaneous Adipose Tissue in Obese Adolescents. Diabetes 2016, 65, 610–618. [Google Scholar] [CrossRef] [PubMed]
- Sokolova, M.; Sjaastad, I.; Louwe, M.C.; Alfsnes, K.; Aronsen, J.M.; Zhang, L.; Haugstad, S.B.; Bendiksen, B.A.; Ogaard, J.; Bliksoen, M.; et al. NLRP3 Inflammasome Promotes Myocardial Remodeling During Diet-Induced Obesity. Front. Immunol. 2019, 10, 1621. [Google Scholar] [CrossRef] [PubMed]
- Nagareddy, P.R.; Kraakman, M.; Masters, S.L.; Stirzaker, R.A.; Gorman, D.J.; Grant, R.W.; Dragoljevic, D.; Hong, E.S.; Abdel-Latif, A.; Smyth, S.S.; et al. Adipose tissue macrophages promote myelopoiesis and monocytosis in obesity. Cell Metab. 2014, 19, 821–835. [Google Scholar] [CrossRef] [PubMed]
- Mocanu, A.O.; Mulya, A.; Huang, H.; Dan, O.; Shimizu, H.; Batayyah, E.; Brethauer, S.A.; Dinischiotu, A.; Kirwan, J.P. Effect of Roux-en-Y Gastric Bypass on the NLRP3 Inflammasome in Adipose Tissue from Obese Rats. PLoS ONE 2015, 10, e0139764. [Google Scholar] [CrossRef] [PubMed]
- Stienstra, R.; Tack, C.J.; Kanneganti, T.D.; Joosten, L.A.; Netea, M.G. The inflammasome puts obesity in the danger zone. Cell Metab. 2012, 15, 10–18. [Google Scholar] [CrossRef] [PubMed]
- Rheinheimer, J.; de Souza, B.M.; Cardoso, N.S.; Bauer, A.C.; Crispim, D. Current role of the NLRP3 inflammasome on obesity and insulin resistance: A systematic review. Metab. Clin. Exp. 2017, 74, 1–9. [Google Scholar] [CrossRef]
- Talukdar, S.; Oh, D.Y.; Bandyopadhyay, G.; Li, D.; Xu, J.; McNelis, J.; Lu, M.; Li, P.; Yan, Q.; Zhu, Y.; et al. Neutrophils mediate insulin resistance in mice fed a high-fat diet through secreted elastase. Nat. Med. 2012, 18, 1407–1412. [Google Scholar] [CrossRef]
- Chawla, A.; Nguyen, K.D.; Goh, Y.P. Macrophage-mediated inflammation in metabolic disease. Nat. Rev. Immunol. 2011, 11, 738–749. [Google Scholar] [CrossRef]
- Konner, A.C.; Bruning, J.C. Toll-like receptors: Linking inflammation to metabolism. Trends Endocrinol. Metab. 2011, 22, 16–23. [Google Scholar] [CrossRef]
- Rogero, M.M.; Calder, P.C. Obesity, Inflammation, Toll-Like Receptor 4 and Fatty Acids. Nutrients 2018, 10, 432. [Google Scholar] [CrossRef] [PubMed]
- Poggi, M.; Bastelica, D.; Gual, P.; Iglesias, M.A.; Gremeaux, T.; Knauf, C.; Peiretti, F.; Verdier, M.; Juhan-Vague, I.; Tanti, J.F.; et al. C3H/HeJ mice carrying a toll-like receptor 4 mutation are protected against the development of insulin resistance in white adipose tissue in response to a high-fat diet. Diabetologia 2007, 50, 1267–1276. [Google Scholar] [CrossRef] [PubMed]
- Caricilli, A.M.; Nascimento, P.H.; Pauli, J.R.; Tsukumo, D.M.; Velloso, L.A.; Carvalheira, J.B.; Saad, M.J. Inhibition of toll-like receptor 2 expression improves insulin sensitivity and signaling in muscle and white adipose tissue of mice fed a high-fat diet. J. Endocrinol. 2008, 199, 399–406. [Google Scholar] [CrossRef]
- Lumeng, C.N.; Bodzin, J.L.; Saltiel, A.R. Obesity induces a phenotypic switch in adipose tissue macrophage polarization. J. Clin. Investig. 2007, 117, 175–184. [Google Scholar] [CrossRef]
- Sokolova, M.; Ranheim, T.; Louwe, M.C.; Halvorsen, B.; Yndestad, A.; Aukrust, P. NLRP3 Inflammasome: A Novel Player in Metabolically Induced Inflammation-Potential Influence on the Myocardium. J. Cardiovasc. Pharmacol. 2019, 74, 276–284. [Google Scholar] [CrossRef]
- Boni-Schnetzler, M.; Meier, D.T. Islet inflammation in type 2 diabetes. Semin. Immunopathol. 2019, 41, 501–513. [Google Scholar] [CrossRef] [PubMed]
- Morikawa, S.; Kaneko, N.; Okumura, C.; Taguchi, H.; Kurata, M.; Yamamoto, T.; Osawa, H.; Nakanishi, A.; Zako, T.; Masumoto, J. IAPP/amylin deposition, which is correlated with expressions of ASC and IL-1beta in beta-cells of Langerhans’ islets, directly initiates NLRP3 inflammasome activation. Int. J. Immunopathol. Pharmacol. 2018, 32, 2058738418788749. [Google Scholar] [CrossRef] [PubMed]
- Masters, S.L.; Dunne, A.; Subramanian, S.L.; Hull, R.L.; Tannahill, G.M.; Sharp, F.A.; Becker, C.; Franchi, L.; Yoshihara, E.; Chen, Z.; et al. Activation of the NLRP3 inflammasome by islet amyloid polypeptide provides a mechanism for enhanced IL-1beta in type 2 diabetes. Nat. Immunol. 2010, 11, 897–904. [Google Scholar] [CrossRef] [PubMed]
- Stienstra, R.; van Diepen, J.A.; Tack, C.J.; Zaki, M.H.; van de Veerdonk, F.L.; Perera, D.; Neale, G.A.; Hooiveld, G.J.; Hijmans, A.; Vroegrijk, I.; et al. Inflammasome is a central player in the induction of obesity and insulin resistance. Proc. Natl. Acad. Sci. USA 2011, 108, 15324–15329. [Google Scholar] [CrossRef] [PubMed]
- Wen, H.; Gris, D.; Lei, Y.; Jha, S.; Zhang, L.; Huang, M.T.; Brickey, W.J.; Ting, J.P. Fatty acid-induced NLRP3-ASC inflammasome activation interferes with insulin signaling. Nat. Immunol. 2011, 12, 408–415. [Google Scholar] [CrossRef] [PubMed]
- Tsalamandris, S.; Antonopoulos, A.S.; Oikonomou, E.; Papamikroulis, G.A.; Vogiatzi, G.; Papaioannou, S.; Deftereos, S.; Tousoulis, D. The Role of Inflammation in Diabetes: Current Concepts and Future Perspectives. Eur. Cardiol. 2019, 14, 50–59. [Google Scholar] [CrossRef]
- Dinarello, C.A.; Donath, M.Y.; Mandrup-Poulsen, T. Role of IL-1beta in type 2 diabetes. Curr. Opin. Endocrinol. Diabetes Obes. 2010, 17, 314–321. [Google Scholar] [CrossRef] [PubMed]
- Alexandraki, K.; Piperi, C.; Kalofoutis, C.; Singh, J.; Alaveras, A.; Kalofoutis, A. Inflammatory process in type 2 diabetes: The role of cytokines. Ann. N. Y. Acad. Sci. 2006, 1084, 89–117. [Google Scholar] [CrossRef] [PubMed]
- Jager, J.; Gremeaux, T.; Cormont, M.; Le Marchand-Brustel, Y.; Tanti, J.F. Interleukin-1beta-induced insulin resistance in adipocytes through down-regulation of insulin receptor substrate-1 expression. Endocrinology 2007, 148, 241–251. [Google Scholar] [CrossRef] [PubMed]
- Hotamisligil, G.S.; Peraldi, P.; Budavari, A.; Ellis, R.; White, M.F.; Spiegelman, B.M. IRS-1-mediated inhibition of insulin receptor tyrosine kinase activity in TNF-alpha- and obesity-induced insulin resistance. Science 1996, 271, 665–668. [Google Scholar] [CrossRef] [PubMed]
- Ledesma, E.; Martinez, I.; Cordova, Y.; Rodriguez-Sosa, M.; Monroy, A.; Mora, L.; Soto, I.; Ramos, G.; Weiss, B.; Santiago Osorio, E. Interleukin-1 beta (IL-1beta) induces tumor necrosis factor alpha (TNF-alpha) expression on mouse myeloid multipotent cell line 32D cl3 and inhibits their proliferation. Cytokine 2004, 26, 66–72. [Google Scholar] [CrossRef]
- Wang, Q.; Wu, H. T Cells in Adipose Tissue: Critical Players in Immunometabolism. Front. Immunol. 2018, 9, 2509. [Google Scholar] [CrossRef]
- Nishimura, S.; Manabe, I.; Nagasaki, M.; Eto, K.; Yamashita, H.; Ohsugi, M.; Otsu, M.; Hara, K.; Ueki, K.; Sugiura, S.; et al. CD8+ effector T cells contribute to macrophage recruitment and adipose tissue inflammation in obesity. Nat. Med. 2009, 15, 914–920. [Google Scholar] [CrossRef]
- McGillicuddy, F.C.; Harford, K.A.; Reynolds, C.M.; Oliver, E.; Claessens, M.; Mills, K.H.; Roche, H.M. Lack of interleukin-1 receptor I (IL-1RI) protects mice from high-fat diet-induced adipose tissue inflammation coincident with improved glucose homeostasis. Diabetes 2011, 60, 1688–1698. [Google Scholar] [CrossRef]
- Dror, E.; Dalmas, E.; Meier, D.T.; Wueest, S.; Thevenet, J.; Thienel, C.; Timper, K.; Nordmann, T.M.; Traub, S.; Schulze, F.; et al. Postprandial macrophage-derived IL-1beta stimulates insulin, and both synergistically promote glucose disposal and inflammation. Nat. Immunol. 2017, 18, 283–292. [Google Scholar] [CrossRef]
- Gao, A.W.; Canto, C.; Houtkooper, R.H. Mitochondrial response to nutrient availability and its role in metabolic disease. Embo Mol. Med. 2014, 6, 580–589. [Google Scholar] [CrossRef] [PubMed]
- Gao, J.; Sang, M.; Zhang, X.; Zheng, T.; Pan, J.; Dai, M.; Zhou, L.; Yang, S. Miro1-mediated mitochondrial dysfunction under high nutrient stress is linked to NOD-like receptor 3 (NLRP3)-dependent inflammatory responses in rat pancreatic beta cells. Free Radic. Biol. Med. 2015, 89, 322–332. [Google Scholar] [CrossRef]
- Chen, L.; Liu, C.; Gao, J.; Xie, Z.; Chan, L.W.C.; Keating, D.J.; Yang, Y.; Sun, J.; Zhou, F.; Wei, Y.; et al. Inhibition of Miro1 disturbs mitophagy and pancreatic beta-cell function interfering insulin release via IRS-Akt-Foxo1 in diabetes. Oncotarget 2017, 8, 90693–90705. [Google Scholar] [CrossRef] [PubMed]
- Zhou, R.; Tardivel, A.; Thorens, B.; Choi, I.; Tschopp, J. Thioredoxin-interacting protein links oxidative stress to inflammasome activation. Nat. Immunol. 2010, 11, 136–140. [Google Scholar] [CrossRef] [PubMed]
- Yoshihara, E.; Masaki, S.; Matsuo, Y.; Chen, Z.; Tian, H.; Yodoi, J. Thioredoxin/Txnip: Redoxisome, as a redox switch for the pathogenesis of diseases. Front. Immunol. 2014, 4, 514. [Google Scholar] [CrossRef] [PubMed]
- Larsen, C.M.; Faulenbach, M.; Vaag, A.; Volund, A.; Ehses, J.A.; Seifert, B.; Mandrup-Poulsen, T.; Donath, M.Y. Interleukin-1-receptor antagonist in type 2 diabetes mellitus. N. Engl. J. Med. 2007, 356, 1517–1526. [Google Scholar] [CrossRef] [PubMed]
- Rissanen, A.; Howard, C.P.; Botha, J.; Thuren, T.; Global, I. Effect of anti-IL-1beta antibody (canakinumab) on insulin secretion rates in impaired glucose tolerance or type 2 diabetes: Results of a randomized, placebo-controlled trial. Diabetes Obes. Metab. 2012, 14, 1088–1096. [Google Scholar] [CrossRef] [PubMed]
- Honda, H.; Nagai, Y.; Matsunaga, T.; Okamoto, N.; Watanabe, Y.; Tsuneyama, K.; Hayashi, H.; Fujii, I.; Ikutani, M.; Hirai, Y.; et al. Isoliquiritigenin is a potent inhibitor of NLRP3 inflammasome activation and diet-induced adipose tissue inflammation. J. Leukoc. Biol. 2014, 96, 1087–1100. [Google Scholar] [CrossRef]
- Chi, Y.; Chai, J.; Xu, C.; Luo, H.; Zhang, Q. Apelin inhibits the activation of the nucleotide-binding domain and the leucine-rich, repeat-containing family, pyrin-containing 3 (NLRP3) inflammasome and ameliorates insulin resistance in severely burned rats. Surgery 2015, 157, 1142–1152. [Google Scholar] [CrossRef]
- Wang, X.; He, G.; Peng, Y.; Zhong, W.; Wang, Y.; Zhang, B. Sodium butyrate alleviates adipocyte inflammation by inhibiting NLRP3 pathway. Sci. Rep. 2015, 5, 12676. [Google Scholar] [CrossRef]
- Ye, Y.; Bajaj, M.; Yang, H.C.; Perez-Polo, J.R.; Birnbaum, Y. SGLT-2 Inhibition with Dapagliflozin Reduces the Activation of the Nlrp3/ASC Inflammasome and Attenuates the Development of Diabetic Cardiomyopathy in Mice with Type 2 Diabetes. Further Augmentation of the Effects with Saxagliptin, a DPP4 Inhibitor. Cardiovasc. Drugs Ther. 2017, 119–132. [Google Scholar] [CrossRef] [PubMed]
- Benetti, E.; Mastrocola, R.; Vitarelli, G.; Cutrin, J.C.; Nigro, D.; Chiazza, F.; Mayoux, E.; Collino, M.; Fantozzi, R. Empagliflozin Protects against Diet-Induced NLRP-3 Inflammasome Activation and Lipid Accumulation. J. Pharmacol. Exp. Ther. 2016, 359, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Coll, R.C.; Robertson, A.A.; Chae, J.J.; Higgins, S.C.; Munoz-Planillo, R.; Inserra, M.C.; Vetter, I.; Dungan, L.S.; Monks, B.G.; Stutz, A.; et al. A small-molecule inhibitor of the NLRP3 inflammasome for the treatment of inflammatory diseases. Nat. Med. 2015, 21, 248–255. [Google Scholar] [CrossRef] [PubMed]
- Youm, Y.H.; Nguyen, K.Y.; Grant, R.W.; Goldberg, E.L.; Bodogai, M.; Kim, D.; D’Agostino, D.; Planavsky, N.; Lupfer, C.; Kanneganti, T.D.; et al. The ketone metabolite beta-hydroxybutyrate blocks NLRP3 inflammasome-mediated inflammatory disease. Nat. Med. 2015, 21, 263–269. [Google Scholar] [CrossRef]
- Wang, H.M.; Zhang, T.; Huang, J.K.; Xiang, J.Y.; Chen, J.J.; Fu, J.L.; Zhao, Y.W. Edaravone Attenuates the Proinflammatory Response in Amyloid-beta-Treated Microglia by Inhibiting NLRP3 Inflammasome-Mediated IL-1beta Secretion. Cell. Physiol. Biochem. Int. J. Exp. Cell. Physiol. Biochem. Pharmacol. 2017, 43, 1113–1125. [Google Scholar] [CrossRef]
- Wang, S.; Yang, H.; Yu, L.; Jin, J.; Qian, L.; Zhao, H.; Xu, Y.; Zhu, X. Oridonin attenuates Abeta1–42-induced neuroinflammation and inhibits NF-kappaB pathway. PLoS ONE 2014, 9, e104745. [Google Scholar] [CrossRef]
- Lei, C.; Lin, R.; Wang, J.; Tao, L.; Fu, X.; Qiu, Y.; Lei, B. Amelioration of amyloid beta-induced retinal inflammatory responses by a LXR agonist TO901317 is associated with inhibition of the NF-kappaB signaling and NLRP3 inflammasome. Neuroscience 2017, 360, 48–60. [Google Scholar] [CrossRef]
- Jiang, H.; He, H.; Chen, Y.; Huang, W.; Cheng, J.; Ye, J.; Wang, A.; Tao, J.; Wang, C.; Liu, Q.; et al. Identification of a selective and direct NLRP3 inhibitor to treat inflammatory disorders. J. Exp. Med. 2017, 214, 3219–3238. [Google Scholar] [CrossRef]
- Kinney, J.W.; Bemiller, S.M.; Murtishaw, A.S.; Leisgang, A.M.; Salazar, A.M.; Lamb, B.T. Inflammation as a central mechanism in Alzheimer’s disease. Alzheimer’s Dement. 2018, 4, 575–590. [Google Scholar] [CrossRef]
- Qiu, C.; Kivipelto, M.; von Strauss, E. Epidemiology of Alzheimer’s disease: Occurrence, determinants, and strategies toward intervention. Dialogues Clin. Neurosci. 2009, 11, 111–128. [Google Scholar]
- Hardy, J.; Selkoe, D.J. The amyloid hypothesis of Alzheimer’s disease: Progress and problems on the road to therapeutics. Science 2002, 297, 353–356. [Google Scholar] [CrossRef] [PubMed]
- Prinz, M.; Priller, J.; Sisodia, S.S.; Ransohoff, R.M. Heterogeneity of CNS myeloid cells and their roles in neurodegeneration. Nat. Neurosci. 2011, 14, 1227–1235. [Google Scholar] [CrossRef] [PubMed]
- Halle, A.; Hornung, V.; Petzold, G.C.; Stewart, C.R.; Monks, B.G.; Reinheckel, T.; Fitzgerald, K.A.; Latz, E.; Moore, K.J.; Golenbock, D.T. The NALP3 inflammasome is involved in the innate immune response to amyloid-beta. Nat. Immunol. 2008, 9, 857–865. [Google Scholar] [CrossRef]
- Nakanishi, A.; Kaneko, N.; Takeda, H.; Sawasaki, T.; Morikawa, S.; Zhou, W.; Kurata, M.; Yamamoto, T.; Akbar, S.M.F.; Zako, T.; et al. Amyloid beta directly interacts with NLRP3 to initiate inflammasome activation: Identification of an intrinsic NLRP3 ligand in a cell-free system. Inflamm. Regen. 2018, 38, 27. [Google Scholar] [CrossRef] [PubMed]
- Ojala, J.; Alafuzoff, I.; Herukka, S.K.; van Groen, T.; Tanila, H.; Pirttila, T. Expression of interleukin-18 is increased in the brains of Alzheimer’s disease patients. Neurobiol. Aging 2009, 30, 198–209. [Google Scholar] [CrossRef] [PubMed]
- Cartier, L.; Hartley, O.; Dubois-Dauphin, M.; Krause, K.H. Chemokine receptors in the central nervous system: Role in brain inflammation and neurodegenerative diseases. Brain Res. Brain Res. Rev. 2005, 48, 16–42. [Google Scholar] [CrossRef] [PubMed]
- Lamkanfi, M.; Dixit, V.M. Inflammasomes and their roles in health and disease. Annu. Rev. Cell Dev. Biol. 2012, 28, 137–161. [Google Scholar] [CrossRef]
- Mangan, M.S.J.; Olhava, E.J.; Roush, W.R.; Seidel, H.M.; Glick, G.D.; Latz, E. Targeting the NLRP3 inflammasome in inflammatory diseases. Nat. Rev. Drug Discov. 2018, 17, 588–606. [Google Scholar] [CrossRef]
- Lue, L.F.; Rydel, R.; Brigham, E.F.; Yang, L.B.; Hampel, H.; Murphy, G.M., Jr.; Brachova, L.; Yan, S.D.; Walker, D.G.; Shen, Y.; et al. Inflammatory repertoire of Alzheimer’s disease and nondemented elderly microglia in vitro. Glia 2001, 35, 72–79. [Google Scholar] [CrossRef]
- Apelt, J.; Schliebs, R. Beta-amyloid-induced glial expression of both pro- and anti-inflammatory cytokines in cerebral cortex of aged transgenic Tg2576 mice with Alzheimer plaque pathology. Brain Res. 2001, 894, 21–30. [Google Scholar] [CrossRef]
- Martinon, F.; Petrilli, V.; Mayor, A.; Tardivel, A.; Tschopp, J. Gout-associated uric acid crystals activate the NALP3 inflammasome. Nature 2006, 440, 237–241. [Google Scholar] [CrossRef] [PubMed]
- Heneka, M.T.; Kummer, M.P.; Stutz, A.; Delekate, A.; Schwartz, S.; Vieira-Saecker, A.; Griep, A.; Axt, D.; Remus, A.; Tzeng, T.C.; et al. NLRP3 is activated in Alzheimer’s disease and contributes to pathology in APP/PS1 mice. Nature 2013, 493, 674–678. [Google Scholar] [CrossRef] [PubMed]
- Meyer-Luehmann, M.; Spires-Jones, T.L.; Prada, C.; Garcia-Alloza, M.; de Calignon, A.; Rozkalne, A.; Koenigsknecht-Talboo, J.; Holtzman, D.M.; Bacskai, B.J.; Hyman, B.T. Rapid appearance and local toxicity of amyloid-beta plaques in a mouse model of Alzheimer’s disease. Nature 2008, 451, 720–724. [Google Scholar] [CrossRef] [PubMed]
- Martini, A.C.; Gomez-Arboledas, A.; Forner, S.; Rodriguez-Ortiz, C.J.; McQuade, A.; Danhash, E.; Phan, J.; Javonillo, D.; Ha, J.V.; Tram, M.; et al. Amyloid-beta impairs TOM1-mediated IL-1R1 signaling. Proc. Natl. Acad. Sci. USA 2019, 116, 21198–21206. [Google Scholar] [CrossRef] [PubMed]
- Hickman, S.E.; Allison, E.K.; El Khoury, J. Microglial dysfunction and defective beta-amyloid clearance pathways in aging Alzheimer’s disease mice. J. Neurosci. 2008, 28, 8354–8360. [Google Scholar] [CrossRef] [PubMed]
- Ries, M.; Sastre, M. Mechanisms of Abeta Clearance and Degradation by Glial Cells. Front. Aging Neurosci. 2016, 8, 160. [Google Scholar] [CrossRef]
- Varnum, M.M.; Ikezu, T. The classification of microglial activation phenotypes on neurodegeneration and regeneration in Alzheimer’s disease brain. Arch. Immunol. Ther. Exp. 2012, 60, 251–266. [Google Scholar] [CrossRef]
- Baroja-Mazo, A.; Martin-Sanchez, F.; Gomez, A.I.; Martinez, C.M.; Amores-Iniesta, J.; Compan, V.; Barbera-Cremades, M.; Yague, J.; Ruiz-Ortiz, E.; Anton, J.; et al. The NLRP3 inflammasome is released as a particulate danger signal that amplifies the inflammatory response. Nat. Immunol. 2014, 15, 738–748. [Google Scholar] [CrossRef]
- Venegas, C.; Kumar, S.; Franklin, B.S.; Dierkes, T.; Brinkschulte, R.; Tejera, D.; Vieira-Saecker, A.; Schwartz, S.; Santarelli, F.; Kummer, M.P.; et al. Microglia-derived ASC specks cross-seed amyloid-beta in Alzheimer’s disease. Nature 2017, 552, 355–361. [Google Scholar] [CrossRef]
- Morales, I.; Farias, G.; Maccioni, R.B. Neuroimmunomodulation in the pathogenesis of Alzheimer’s disease. Neuroimmunomodulation 2010, 17, 202–204. [Google Scholar] [CrossRef]
- Wang, H.; Shen, Y.; Chuang, H.; Chiu, C.; Ye, Y.; Zhao, L. Neuroinflammation in Alzheimer’s Disease: Microglia, Molecular Participants and Therapeutic Choices. Curr. Alzheimer Res. 2019, 16, 659–674. [Google Scholar] [CrossRef] [PubMed]
- Maccioni, R.B.; Rojo, L.E.; Fernandez, J.A.; Kuljis, R.O. The role of neuroimmunomodulation in Alzheimer’s disease. Ann. N. Y. Acad. Sci. 2009, 1153, 240–246. [Google Scholar] [CrossRef] [PubMed]
- Griffin, W.S.; Liu, L.; Li, Y.; Mrak, R.E.; Barger, S.W. Interleukin-1 mediates Alzheimer and Lewy body pathologies. J. Neuroinflammation 2006, 3, 5. [Google Scholar] [CrossRef] [PubMed]
- Biundo, F.; Del Prete, D.; Zhang, H.; Arancio, O.; D’Adamio, L. A role for tau in learning, memory and synaptic plasticity. Sci. Rep. 2018, 8, 3184. [Google Scholar] [CrossRef]
- Murray, C.A.; Lynch, M.A. Evidence that increased hippocampal expression of the cytokine interleukin-1 beta is a common trigger for age- and stress-induced impairments in long-term potentiation. J. Neurosci. 1998, 18, 2974–2981. [Google Scholar] [CrossRef]
- Kitazawa, M.; Cheng, D.; Tsukamoto, M.R.; Koike, M.A.; Wes, P.D.; Vasilevko, V.; Cribbs, D.H.; LaFerla, F.M. Blocking IL-1 signaling rescues cognition, attenuates tau pathology, and restores neuronal beta-catenin pathway function in an Alzheimer’s disease model. J. Immunol. 2011, 187, 6539–6549. [Google Scholar] [CrossRef]
- Chaparro-Huerta, V.; Rivera-Cervantes, M.C.; Flores-Soto, M.E.; Gomez-Pinedo, U.; Beas-Zarate, C. Proinflammatory cytokines and apoptosis following glutamate-induced excitotoxicity mediated by p38 MAPK in the hippocampus of neonatal rats. J. Neuroimmunol. 2005, 165, 53–62. [Google Scholar] [CrossRef]
- Poddar, R.; Paul, S. Novel crosstalk between ERK MAPK and p38 MAPK leads to homocysteine-NMDA receptor-mediated neuronal cell death. J. Neurochem. 2013, 124, 558–570. [Google Scholar] [CrossRef]
- Barone, F.C.; Irving, E.A.; Ray, A.M.; Lee, J.C.; Kassis, S.; Kumar, S.; Badger, A.M.; Legos, J.J.; Erhardt, J.A.; Ohlstein, E.H.; et al. Inhibition of p38 mitogen-activated protein kinase provides neuroprotection in cerebral focal ischemia. Med. Res. Rev. 2001, 21, 129–145. [Google Scholar] [CrossRef]
- Serou, M.J.; DeCoster, M.A.; Bazan, N.G. Interleukin-1 beta activates expression of cyclooxygenase-2 and inducible nitric oxide synthase in primary hippocampal neuronal culture: Platelet-activating factor as a preferential mediator of cyclooxygenase-2 expression. J. Neurosci. Res. 1999, 58, 593–598. [Google Scholar] [CrossRef]
- Glass, C.K.; Saijo, K.; Winner, B.; Marchetto, M.C.; Gage, F.H. Mechanisms underlying inflammation in neurodegeneration. Cell 2010, 140, 918–934. [Google Scholar] [CrossRef] [PubMed]
- Batkulwar, K.; Godbole, R.; Banarjee, R.; Kassaar, O.; Williams, R.J.; Kulkarni, M.J. Advanced Glycation End Products Modulate Amyloidogenic APP Processing and Tau Phosphorylation: A Mechanistic Link between Glycation and the Development of Alzheimer’s Disease. ACS Chem. Neurosci. 2018, 9, 988–1000. [Google Scholar] [CrossRef] [PubMed]
- Bai, J.P.F.; Melas, I.N.; Hur, J.; Guo, E. Advances in omics for informed pharmaceutical research and development in the era of systems medicine. Expert Opin. Drug Discov. 2018, 13, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Oei, R.W.; Hou, G.; Liu, F.; Zhong, J.; Zhang, J.; An, Z.; Xu, L.; Yang, Y. Convolutional neural network for cell classification using microscope images of intracellular actin networks. PLoS ONE 2019, 14, e0213626. [Google Scholar] [CrossRef]
- Nitta, N.; Sugimura, T.; Isozaki, A.; Mikami, H.; Hiraki, K.; Sakuma, S.; Iino, T.; Arai, F.; Endo, T.; Fujiwaki, Y. Intelligent image-activated cell sorting. Cell 2018, 175, 266–276.e213. [Google Scholar] [CrossRef]
- Von Lilienfeld, O.A. Quantum machine learning in chemical compound space. Angew. Chem. Int. Ed. 2018, 57, 4164–4169. [Google Scholar] [CrossRef]
- Popova, M.; Isayev, O.; Tropsha, A. Deep reinforcement learning for de novo drug design. Sci. Adv. 2018, 4, eaap7885. [Google Scholar] [CrossRef]
- Zhou, Z.; Li, X.; Zare, R.N. Optimizing chemical reactions with deep reinforcement learning. ACS Cent. Sci. 2017, 3, 1337–1344. [Google Scholar] [CrossRef]
- Coley, C.W.; Barzilay, R.; Jaakkola, T.S.; Green, W.H.; Jensen, K.F. Prediction of organic reaction outcomes using machine learning. ACS Cent. Sci. 2017, 3, 434–443. [Google Scholar] [CrossRef]
- Hofmarcher, M.; Rumetshofer, E.; Clevert, D.-A.; Hochreiter, S.; Klambauer, G.N. Accurate prediction of biological assays with high-throughput microscopy images and convolutional networks. J. Chem. Inf. Model. 2019, 59, 1163–1171. [Google Scholar] [CrossRef]
- Hochreiter, S.; Klambauer, G.; Rarey, M. Machine Learning in Drug Discovery; ACS Publications: Washington, DC, USA, 2018. [Google Scholar]
- Yin, Z.; Ai, H.; Zhang, L.; Ren, G.; Wang, Y.; Zhao, Q.; Liu, H. Predicting the cytotoxicity of chemicals using ensemble learning methods and molecular fingerprints. J. Appl. Toxicol. 2019. [Google Scholar] [CrossRef]
- Franco Machado, J.; Silva, R.; Melo, R.; Correia, G.; João, D. Less Exploited GPCRs in Precision Medicine: Targets for Molecular Imaging and Theranostics. Molecules 2019, 24, 49. [Google Scholar] [CrossRef]
- Raghavendra, B.N.; Rosen, R.J.; Lam, S.; Riles, T.; Horii, S.C. Deep venous thrombosis: Detection by high-resolution real-time ultrasonography. Radiology 1984, 152, 789–793. [Google Scholar] [CrossRef]
- Ching, T.; Himmelstein, D.S.; Beaulieu-Jones, B.K.; Kalinin, A.A.; Do, B.T.; Way, G.P.; Ferrero, E.; Agapow, P.M.; Zietz, M.; Hoffman, M.M.; et al. Opportunities and obstacles for deep learning in biology and medicine. J. R. Soc. Interface 2018, 15. [Google Scholar] [CrossRef]
- Korkmaz, S.; Zararsiz, G.; Goksuluk, D. MLViS: A Web Tool for Machine Learning-Based Virtual Screening in Early-Phase of Drug Discovery and Development. PLoS ONE 2015, 10, e0124600. [Google Scholar] [CrossRef]
- Jorissen, R.N.; Gilson, M.K. Virtual screening of molecular databases using a support vector machine. J. Chem. Inf. Model. 2005, 45, 549–561. [Google Scholar] [CrossRef]
- Wassermann, A.M.; Geppert, H.; Bajorath, J. Searching for target-selective compounds using different combinations of multiclass support vector machine ranking methods, kernel functions, and fingerprint descriptors. J. Chem. Inf. Model. 2009, 49, 582–592. [Google Scholar] [CrossRef]
- Agarwal, S.; Dugar, D.; Sengupta, S. Ranking chemical structures for drug discovery: A new machine learning approach. J. Chem. Inf. Model. 2010, 50, 716–731. [Google Scholar] [CrossRef]
- Rathke, F.; Hansen, K.; Brefeld, U.; Muller, K.R. StructRank: A new approach for ligand-based virtual screening. J. Chem. Inf. Model. 2011, 51, 83–92. [Google Scholar] [CrossRef]
- Liang, J.W.; Wang, M.Y.; Wang, S.; Li, S.L.; Li, W.Q.; Meng, F.H. Identification of novel CDK2 inhibitors by a multistage virtual screening method based on SVM, pharmacophore and docking model. J. Enzym. Inhib. Med. Chem. 2020, 35, 235–244. [Google Scholar] [CrossRef]
- Wallach, I.; Dzamba, M.; Heifets, A. AtomNet: A deep convolutional neural network for bioactivity prediction in structure-based drug discovery. arXiv 2015, arXiv:1510.02855 2015. [Google Scholar]
- Liu, Z.; Du, J.; Fang, J.; Yin, Y.; Xu, G.; Xie, L. DeepScreening: A deep learning-based screening web server for accelerating drug discovery. Database J. Biol. Databases Curation 2019, 2019. [Google Scholar] [CrossRef]
- Martinez, M.J.; Razuc, M.; Ponzoni, I. MoDeSuS: A Machine Learning Tool for Selection of Molecular Descriptors in QSAR Studies Applied to Molecular Informatics. Biomed Res. Int. 2019, 2019, 2905203. [Google Scholar] [CrossRef] [PubMed]
- Soufan, O.; Ba-Alawi, W.; Magana-Mora, A.; Essack, M.; Bajic, V.B. DPubChem: A web tool for QSAR modeling and high-throughput virtual screening. Sci. Rep. 2018, 8, 9110. [Google Scholar] [CrossRef]
- Dixon, S.L.; Duan, J.; Smith, E.; Von Bargen, C.D.; Sherman, W.; Repasky, M.P. AutoQSAR: An automated machine learning tool for best-practice quantitative structure-activity relationship modeling. Future Med. Chem. 2016, 8, 1825–1839. [Google Scholar] [CrossRef] [PubMed]
- Bordner, A.J. Predicting small ligand binding sites in proteins using backbone structure. Bioinformatics 2008, 24, 2865–2871. [Google Scholar] [CrossRef] [PubMed]
- Volkamer, A.; Kuhn, D.; Rippmann, F.; Rarey, M. DoGSiteScorer: A web server for automatic binding site prediction, analysis and druggability assessment. Bioinformatics 2012, 28, 2074–2075. [Google Scholar] [CrossRef]
- Nayal, M.; Honig, B. On the nature of cavities on protein surfaces: Application to the identification of drug-binding sites. Proteins 2006, 63, 892–906. [Google Scholar] [CrossRef]
- Durrant, J.D.; McCammon, J.A. NNScore 2.0: A neural-network receptor-ligand scoring function. J. Chem. Inf. Model. 2011, 51, 2897–2903. [Google Scholar] [CrossRef]
- Li, Y.; Wang, L.; Liu, Z.; Li, C.; Xu, J.; Gu, Q.; Xu, J. Predicting selective liver X receptor beta agonists using multiple machine learning methods. Mol. Biosyst. 2015, 11, 1241–1250. [Google Scholar] [CrossRef]
- Chandra, S.; Pandey, J.; Tamrakar, A.K.; Siddiqi, M.I. Multiple machine learning based descriptive and predictive workflow for the identification of potential PTP1B inhibitors. J. Mol. Graph. Model. 2017, 71, 242–256. [Google Scholar] [CrossRef]
- Mysinger, M.M.; Carchia, M.; Irwin, J.J.; Shoichet, B.K. Directory of useful decoys, enhanced (DUD-E): Better ligands and decoys for better benchmarking. J. Med. Chem. 2012, 55, 6582–6594. [Google Scholar] [CrossRef]
- Bauer, M.R.; Ibrahim, T.M.; Vogel, S.M.; Boeckler, F.M. Evaluation and optimization of virtual screening workflows with DEKOIS 2.0—A public library of challenging docking benchmark sets. J. Chem. Inf. Model. 2013, 53, 1447–1462. [Google Scholar] [CrossRef]
- Lagarde, N.; Ben Nasr, N.; Jeremie, A.; Guillemain, H.; Laville, V.; Labib, T.; Zagury, J.F.; Montes, M. NRLiSt BDB, the manually curated nuclear receptors ligands and structures benchmarking database. J. Med. Chem. 2014, 57, 3117–3125. [Google Scholar] [CrossRef]
- Xia, J.; Tilahun, E.L.; Kebede, E.H.; Reid, T.E.; Zhang, L.; Wang, X.S. Comparative modeling and benchmarking data sets for human histone deacetylases and sirtuin families. J. Chem. Inf. Model. 2015, 55, 374–388. [Google Scholar] [CrossRef]
- Gaulton, A.; Bellis, L.J.; Bento, A.P.; Chambers, J.; Davies, M.; Hersey, A.; Light, Y.; McGlinchey, S.; Michalovich, D.; Al-Lazikani, B.; et al. ChEMBL: A large-scale bioactivity database for drug discovery. Nucl. Acids Res. 2012, 40, D1100–D1107. [Google Scholar] [CrossRef]
- Cang, Z.; Mu, L.; Wei, G.W. Representability of algebraic topology for biomolecules in machine learning based scoring and virtual screening. PLoS Comput. Biol. 2018, 14, e1005929. [Google Scholar] [CrossRef] [PubMed]
- Ma, X.H.; Shi, Z.; Tan, C.; Jiang, Y.; Go, M.L.; Low, B.C.; Chen, Y.Z. In-silico approaches to multi-target drug discovery: Computer aided multi-target drug design, multi-target virtual screening. Pharm. Res. 2010, 27, 739–749. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Srivastava, G.; Sharma, A. A physicochemical descriptor based method for effective and rapid screening of dual inhibitors against BACE-1 and GSK-3beta as targets for Alzheimer’s disease. Comput. Biol. Chem. 2017, 71, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Xie, H.; Wen, H.; Zhang, D.; Liu, L.; Liu, B.; Liu, Q.; Jin, Q.; Ke, K.; Hu, M.; Chen, X. Designing of dual inhibitors for GSK-3beta and CDK5: Virtual screening and in vitro biological activities study. Oncotarget 2017, 8, 18118–18128. [Google Scholar] [CrossRef] [PubMed]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).