Simple Summary
Cytoskeleton-associated protein 4 (CKAP4), which has been linked to worse outcomes in several types of cancer, has emerged as a novel biomarker to predict patient outcomes for bladder cancer following radical cystectomy. This study investigated CKAP4 levels in bladder cancer specimens after radical cystectomy, and the association between CKAP4 levels, clinicopathological characteristics, and patient outcomes was analyzed. The analysis revealed that CKAP4 was connected to a higher risk of cancer recurrence, which means that CKAP4 could be a useful clinical tool to predict cancer recurrence after surgery.
Abstract
Background/Objectives: While cytoskeleton-associated protein 4 (CKAP4) has been associated with prognosis in various malignancies, its prognostic value for bladder cancer (BCa) remains unclear. The aim of this study was to evaluate CKAP4 expression in tumor cells and cancer-associated fibroblasts (CAFs) following radical cystectomy (RC) in patients with BCa. Methods: In this study, CKAP4 in tumor cells was defined as CKAP4-1, while CKAP4 expressed in CAFs was defined as CKAP4-2. CKAP4-2 expression was evaluated to explore its potential association with tumor aggressiveness and patient outcomes. CKAP4 expression in 86 RC specimens was assessed using immunohistochemistry. CKAP4-1 positivity was considered when ≥5% cytoplasmic staining of cancer cells, with at least moderate staining intensity, was observed. CKAP4-2 positivity was evaluated using a point scale (0–3), with scores based on the number of CKAP4 positive CAFs in the tumor stroma. Scores of 2 (moderate number of CAFs) and 3 (significant number of CAFs) were considered to indicate positivity. Results: CKAP4-1 and CKAP4-2 were expressed in 53 (61.6%) and 34 (39.5%) patients, respectively. Kaplan–Meier analysis showed that patients with CKAP4-1 had significantly shorter cancer-specific survival and recurrence-free survival (RFS; p = 0.046 and p = 0.0173, respectively). Multivariate analysis showed that CKAP4-1 positivity was an independent predictor of RFS (p = 0.041, hazard ratio: 2.09, 95% confidence interval: 1.03–4.25). Conclusions: This study showed that CKAP4 expression in tumor cells may serve as a useful prognostic biomarker for patients with BCa who undergo RC.
1. Introduction
Bladder cancer (BCa) is the tenth most prevalent cancer globally [1]. Radical cystectomy (RC) with bilateral pelvic lymph node (LN) dissection remains the gold standard treatment for patients with muscle-invasive BCa (MIBC) and non-MIBC (NMIBC) refractory to bacillus Calmette-Guérin. Although the surgical technique has advanced and the role of pelvic lymphadenectomy is better understood, the 5-year overall survival rate after RC without neoadjuvant chemotherapy (NAC) or adjuvant chemotherapy (AC) is approximately 50% [2]. Several clinicopathological factors, such as tumor grade, lymphovascular invasion (LVI), and LN status have been studied in an effort to improve unfavorable prognoses after RC [3]. These risk factors facilitate estimation of the recurrence risk and survival outcomes; however, they do not predict individual patient prognosis. Some studies reported the efficacy of new prognostic biomarkers for BCa after RC, but none of them are available for clinical use [4,5,6]; therefore, novel prognostic biomarkers for BCa are necessary.
Cytoskeleton-associated protein 4 (CKAP4), also termed CLIMP-63 or p63, is a type II transmembrane protein with reversible palmitoylation [7,8]. It is mainly found in the rough endoplasmic reticulum, where it stabilizes its structure [9]. CKAP4 has been associated with various cancers and has attracted considerable attention in recent years. In hepatocellular carcinoma, esophageal cancer, and renal cell carcinoma, CKAP4 overexpression was significantly associated with unfavorable outcomes [10,11,12]. CKAP4 in pancreatic cancer has emerged as a potential therapeutic target for the inhibition of DKK1-CKAP4 binding and Akt activation [13]. Although the literature on CKAP4 remains scarce, a basic study has intensively investigated the mechanism of CKAP4 in the progression of BCa, indicating its potential as a novel biomarker [14]. Verification of the prognostic value of CKAP4 in clinical practice is essential for better BCa management because patients who require RC with curative intent often have poor outcomes.
The aims of this study were to evaluate the expression levels of CKAP4 in tumor cells and cancer-associated fibroblasts (CAFs) using immunohistochemical analyses of archived RC specimens and to assess the impact of CKAP4 on the prognosis of patients who underwent RC for BCa. In this study, to investigate their associations with clinicopathological features and patient outcomes, CKAP4 expressed in tumor cells was defined as CKAP4-1, while CKAP4 expressed in CAFs was defined as CKAP4-2.
2. Materials and Methods
2.1. Patients
We retrospectively analyzed the clinical data and archived specimens of patients with BCa who underwent RC with pelvic and iliac lymphadenectomies between 1990 and 2015 at the Kitasato University Hospital (Kanagawa, Japan). We also examined normal urothelial tissue specimens from adjacent tumor tissues using NMIBCs as a negative control. RC was performed in patients with pathologically proven MIBC and in those with NMIBC who failed to respond to intravesical therapy [15]. Patient characteristics were obtained from medical records, including age at RC, sex, pathological status (pT and pN stages), tumor grade, LVI status, carcinoma in situ (CIS), history of AC and salvage chemotherapy (SC), recurrence, and cancer-specific death. Pathological staging was performed according to the 2002 TNM classification. Pathological grading was performed according to the 1973 World Health Organization classification. LVI was defined as the presence of cancer cells within the endothelial space; however, cancer cells merely invading the vascular lumen were considered negative [16]. AC was performed in patients with pT ≥ 3 disease or a positive LN status. All the patients with AC or SC received platinum-based chemotherapy. Because this was a retrospective study, all patients found to be eligible during the study period were included, and no formal sample size calculation was performed. This study was conducted in accordance with the guidelines of the Declaration of Helsinki and was approved by the Ethics Committee of Kitasato University School of Medicine on 24 May 2017 (B17-010). Participants were informed of the study and provided with the opportunity to opt out at any time. As this was a retrospective study, individual written informed consent was not required.
2.2. Immunohistochemistry and Scoring
Three-micrometer thick sections from 10% formalin-fixed and paraffin-embedded BCa tissue blocks were deparaffinized in xylene and rehydrated in a descending ethanol series. After treatment with 3% hydrogen peroxide for 10 min, the antigen was retrieved by autoclaving in Tris-EDTA buffer (0.01 M Tris-hydroxymethyl aminomethane, 0.001 M EDTA-2Na, pH 9.0) at 121 °C for 10 min. After washing in Tris-buffered saline (TBS) for 5 min and blocking in 0.5% casein for 10 min, the sections were reacted with 1000 times diluted anti-CKAP4 polyclonal antibody (HPA000792; Sigma Life Science, St. Louis, MO, USA) for 18 h at room temperature. After rinsing with TBS three times for 5 min each, samples were treated with horseradish peroxidase-labeled polymer reagent (EnVisoin+ Dual Link System-HRP Kit; Dako, Glostrup, Denmark) for 30 min at room temperature. After rinsing with TBS three times for 5 min each, the sections were visualized with a Stable DAB solution (Invitrogen, Carlsbad, CA, USA) and counterstained with Mayer’s hematoxylin. The protocol for immunohistochemical analyses was based on a previously reported method by Yanagita et al. [17].
The expression levels of CKAP4 were evaluated in tumor cells and in CAFs located in the tumor stroma. We defined CKAP4-1 as CKAP4 in tumor cells and CKAP4-2 as CKAP4 in CAFs. CKAP4-1 was immunohistochemically evaluated by determining the intensity and percentage of positive tumor cells. Normal urothelial cells were used as an internal control. The staining intensity of the tumor cell cytoplasm was categorized into four groups: 0, no staining; 1, weak staining; 2, moderate staining; and 3, strong staining. CKAP4-1 positivity was defined as cases where ≥5% of tumor cells exhibited a staining score of 2 or 3. These scoring criteria were adapted from the study by Nagoya et al. [18]. Immunohistochemical staining for CKAP4-2 was performed based on the number of CKAP4 positive CAFs in the tumor stroma. We categorized CKAP4-2 expression into four groups: 0, no staining of CAF; 1, few CAFs; 2, moderate number of CAFs; and 3, significant number of CAFs. CKAP4-2 positivity was defined as patients with scores of 2 or 3. Because no study has evaluated CKAP4 expression in CAFs, this scoring method was adapted from a previous report by Akanda et al. [19]. Two investigators (H.K. and Y.S.) blinded to the clinical and pathological data, reviewed all the immunostained sections. Discordant cases were reviewed and discussed until consensus was reached.
2.3. Statistical Analyses
In immunohistochemical analysis, the age (<65 vs. ≥65), pathological stage (pT ≤ 2 vs. ≥3), LN status (N0 vs. N1 and N2), and pathological grade (1 and 2 vs. 3) were evaluated as dichotomized variables. The association between CKAP4 expression and clinicopathological status (sex, age, pathological stage, LN status, pathological grade, LVI, CIS, history of AC and SC, recurrence, and cancer-specific death) was evaluated using Fisher’s exact test. The correlation between CKAP4-1 and CKAP4-2 expression was also examined. Cancer-specific survival (CSS) and recurrence-free survival (RFS) were estimated using the Kaplan–Meier method with log-rank tests. Univariate and multivariate analyses were performed using Cox proportional hazards analysis to estimate the association between CKAP4 expression and clinicopathological variables. Statistical significance was set at p < 0.05. All reported p values are two-sided. Stata 17 for Windows (Stata, Chicago, IL, USA) was used for all analyses.
3. Results
The clinical data and archived specimens of 125 patients with BCa who underwent RC with pelvic and iliac lymphadenectomies were initially included. Of the total, 39 patients were excluded for the following reasons: 10 with histological variants, including squamous cell carcinoma, adenocarcinoma, and small cell carcinoma; 15 who had been previously treated with NAC; and 14 who were lost to follow-up. The final study group (n = 86) comprised 67 men (78%) and 19 women (22%). None of the patients received preoperative NAC or radiotherapy, and no distant metastases were observed at the time of diagnosis.
3.1. Immunohistochemistry
Figure 1 shows CKAP4 staining in normal urothelial and tumor tissues of the study group. In normal urothelial tissues, umbrella cells showed strong cytoplasmic staining, whereas the normal urothelium showed negative to weak staining, with scattered weakly positive normal fibroblasts (Figure 1a). In tumor tissues, CKAP4 was observed in the cytoplasm of tumor cells and CAFs at various degrees and intensities (Figure 1b–d).
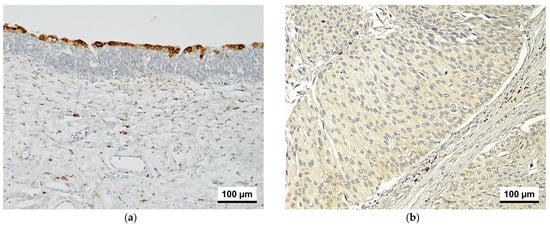
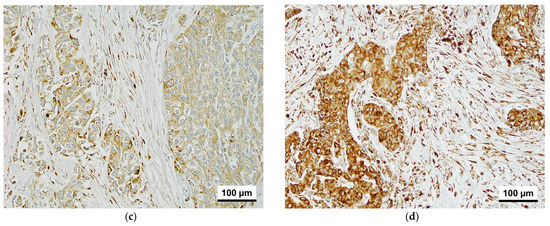
Figure 1.
CKAP4 immunoreactivity in normal urothelium and bladder cancer tissue (200× magnification). (a) Normal urothelium. (b) Tumor cells with weak staining and a few positive CAFs. (c) Tumor cells with moderate staining and a moderate number of positive CAFs. (d) Tumor cells with strong staining and a significant number of positive CAFs. CKAP4, cytoskeleton-associated protein 4; CAFs, cancer-associated fibroblasts.
3.2. Association of CKAP4 Expression with Clinicopathological Characteristics
Table 1 summarizes the clinicopathological characteristics of the 86 patients. CKAP4-1 and CKAP4-2 were positive in 61.6% (n = 53) and 39.5% (n = 34) of the patients, respectively. During a median follow-up of 36.0 months, the proportion of patients who died of BCa or other causes was 44.2% (n = 38) and 14.0% (n = 12), respectively. The CKAP4-1 positive group had significantly higher proportions of patients with pT ≥ 3 (67.9% vs. 39.4%) and positive LVI (72.0% vs. 48.4%) compared to the CKAP4-1 negative group. Similarly, the CKAP4-2 positive group had significantly higher proportions of patients with pT ≥ 3 (73.5% vs. 46.2%), positive LVI (84.4% vs. 49.0%), positive LN metastasis (40.6% vs. 16.0%), Grade 3 tumors (82.4% vs. 46.2%), and a history of AC (44.1% vs. 11.5%) than did the CKAP4-2 negative group.

Table 1.
Relationship between CKAP4 and clinicopathological characteristics.
3.3. Survival Outcomes and CKAP4 Expression
Kaplan–Meier analysis showed that patients with positive CKAP4-1 had significantly shorter CSS and RFS (p = 0.046, and p = 0.017, respectively; Figure 2) than patients with negative CKAP4-1. Similarly, patients with positive CKAP4-2 had shorter CSS and RFS than patients with negative CKAP4-2, but the differences were not significant (p = 0.085 and p = 0.058, respectively; Figure 3). The median times to cancer death and recurrence for patients with positive CKAP4-1 were 39.3 and 28.8 months, respectively. However, for patients with negative CKAP4-1, the median times to cancer death and recurrence were not reached.
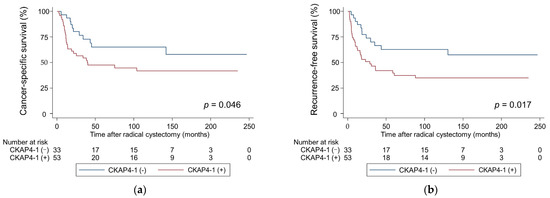
Figure 2.
Probability of survival in patients with bladder cancer according to CKAP4-1 expression estimated using Kaplan–Meier analysis. (a) Cancer-specific survival; (b) Recurrence-free survival. CKAP4, cytoskeleton-associated protein 4.
Figure 3.
Probability of survival in patients with bladder cancer according to CKAP4-2 expression estimated using Kaplan–Meier analysis. (a) Cancer-specific survival; (b) Recurrence-free survival. CKAP4, cytoskeleton-associated protein 4.
In the univariate Cox regression analysis, independent risk factors for worse CSS and RFS were pT ≥ 3, positive LN metastasis, and positive CKAP4-1. In the multivariate Cox regression analysis, positive CKAP4-1 was as an independent factor for worse RFS (hazard ratio: 2.09, 95% confidence interval: 1.03–4.25, p = 0.041), whereas the other clinicopathological features did not have prognostic impact regarding CSS and RFS (Table 2).

Table 2.
Univariate and multivariate Cox proportional hazard analyses to predict cancer-specific survival and recurrence-free survival.
4. Discussion
In this retrospective analysis, we investigated the prognostic relevance of CKAP4 expression in patients with BCa who underwent RC and observed two striking findings. First, positive CKAP4 expression was associated with more aggressive pathological features, such as advanced pT stage and presence of LVI in tumor cells, and advanced pT stage, tumor grade 3, presence of LVI, and LN metastasis in CAFs. Second, the multivariate analysis adjusted for clinicopathological features revealed that CKAP4 expression in tumor cells was an independent prognostic factor for poor RFS, whereas CKAP4 expression in CAFs did not have a prognostic impact.
Although data on CKAP4 expression in BCa are scarce, pioneering work on the mechanism of CKAP4 expression in BCa cells has been reported by Sun et al. [14]. Biomarker analysis using the cell-SELEX method identified CKAP4 as having the highest affinity for the aptamer spl3, which had the best binding ability to BLCA 5637 cells. CKAP4 was involved in the progression of BCa through two potential mechanisms. First, CKAP4 facilitates cancer invasiveness by orchestrating a central-to-peripheral gradient of cell surface stiffness. For example, 5637 cells with CKAP4 exhibited a four-fold increase in motility compared to CKAP4-depleted 5637 cells, with the formation of lamellipodia in the CKAP4 positive cells presumably supporting the high migration potential. Second, exosomal CKAP4 promoted cancer metastasis. Injection of 5637 cells treated with CKAP4-containing exosome in mice exhibited approximately twice as much metastasis compared to the control 5637 cells. To assess the clinical relevance of CKAP4, the association between CKAP4 expression and the clinicopathological characteristics of patients with BCa was investigated by immunohistochemical analysis using a tissue microarray [14]. CKAP4 expression was observed in the tumor cytoplasm and nucleus and was significantly associated with MIBC and LN metastasis. As such, the mechanical properties of central-to-peripheral stiffness, lamellipodia formation, and exosomal CKAP4 significantly correlated with the invasiveness and metastasis of several cancers. In line with these findings, the worse prognostic value of CKAP4-1 demonstrated in the current multivariate analysis appears reasonable [18,20,21,22].
Another mechanism of CKAP4 underlying the biological aggressiveness of BCa is the interaction between CKAP4 and DKK1. The Wnt/β-catenin pathway plays a central role in cancer progression, and intensive research has found DKK1 as a Wnt/β-catenin pathway inhibitor [23,24]. However, recent preclinical and clinical studies have revealed that the interaction of DKK1 and CKAP4 on the cell membrane activates the Akt signaling pathway, wherein various types of cancers predominantly rely on cell proliferation [25,26]. In surgically resected esophageal squamous cell carcinoma, patients with both CKAP4 and DKK1 positivity showed significantly worse overall survival and RFS than those negative for both biomarkers [25]. Moreover, either DKK1 or CKAP4 knockdown suppressed cell growth in vitro and xenograft tumor formation via the Akt signaling pathway, and anti-CKAP4 antibody has also been demonstrated to show an antitumor effect in pancreatic cancer cells [25,26]. Although no study has reported an association between CKAP4 and DKK1, Shen et al., using western blotting, reported higher DKK1 expression levels in urothelial carcinoma tissues than in the normal urothelium [27]. The correlation between CKAP4 expression in tumor cells and poor RFS with advanced clinicopathological characteristics in the present study may represent the interaction of CKAP4 and DKK1. We believe that CKAP4 is worth highlighting as a novel prognostic and therapeutic biomarker for advanced BCa, and our findings encourage further studies to validate this hypothesis.
We observed varying levels of CKAP4 expression in CAFs within the tumor stroma, which were significantly associated with more aggressive clinicopathological features. These findings suggest that CKAP4 expression in CAFs may also be a useful biomarker for predicting the aggressive BCa phenotype. Although there are no reports on CKAP4 expression in CAFs, Gladka et al. identified CKAP4 as a novel biomarker for activated cardiac fibroblasts in a single-cell sequencing analysis, and CKAP4 was shown to be involved in myofibroblast activation in in vitro experiments [28]. Yang et al. reported the classification of CAFs into distinct subtypes that function as specific markers; in particular, myofibroblast-like CAFs (myCAFs) were found to be activated through direct interaction with cancer cells and exhibited dual tumor-restraining and tumor-promoting roles [29]. Du et al. performed an analysis using the TCGA database and reported that high expression of the myCAF marker gene was significantly associated with more advanced T-stage and worse overall survival and RFS in BCa [30]. Because myCAFs share many characteristics with myofibroblasts, it is reasonable that CKAP4 activates myCAFs similarly to myofibroblasts, promotes an aggressive phenotype of BCa and worsens survival outcomes [31,32]. However, CKAP4 expression in CAFs was not significantly associated with poor CSS or RFS. In terms of RFS, the CKAP4 positive group was significantly associated with cases that received prior AC, suggesting that CKAP4 expression did not induce poor RFS due to the treatment effect of AC. In contrast, CKAP4 positivity was not associated with SC, and the reason it did not cause significantly poorer CSS remains unclear. Although these findings are intriguing, the functional role of CKAP4 in CAFs was not analyzed in this study. Further investigations, including in vitro and in vivo studies, are needed to elucidate its biological significance.
To our knowledge, this is the first clinical study to demonstrate that CKAP4 expression in tumor tissue may be a useful prognostic biomarker for patients with BCa who undergo RC. Unlike currently available diagnostic biomarkers such as NMP22 and BTA, CKAP4 provided a novel insight into the risk of postoperative recurrence. Moreover, recent studies have reported serum or urine-based biomarkers [33,34]. In the present study, CKAP4 was evaluated in surgical specimens, and its expression can be considered to be independent of serum or urinary biomarkers. This suggests that CKAP4 could be used in combination with serum or urinary biomarkers to improve clinical decision-making.
While searching for literature on CKAP4 in PubMed and other databases, reports related to p63 were often presented in the results. Although both gene products have a molecular weight of 63,000, the CKAP4 protein is mainly localized in the cytoplasm and cell membrane [12,17,35], whereas the p63 protein is expressed in the nucleus and is known as one of the p53-related antigens [36]. Furthermore, the CKAP4 gene is located on chromosome 12q23.3 (OMIM: 618595), while the p63 gene is on chromosome 3q27-28 (OMIM: 603273). Therefore, these are different molecules. The expression of CKAP4 in human normal tissues and various tumors, as reported by The Human Protein Atlas (http://www.proteinatlas.org), is also localized in the cytoplasm and cell membrane; therefore, these proteins should not be confused with one another.
The present study had some limitations. First, it was a single-center, retrospective study with a limited sample size. Second, RC was performed by different surgeons, and the selection of postoperative chemotherapy regimens such as AC and SC depended on the preference of each doctor; this may have affected the results. Third, we did not include patients who received immune-checkpoint inhibitors or enfortumab vedotin. Future studies including these therapies may show different results. Fourth, some patient characteristics such as smoking status and occupational exposure to industrial chemicals or toxins were not included, although they may have influenced patients’ prognosis. Further studies addressing these limitations are required to validate our findings. Finally, although CKAP4 expression in CAFs was evaluated, its biological function was not investigated in this study. The functional significance should be explored using in vitro and in vivo models in future studies.
5. Conclusions
The expression CKAP4 in tumor cells and CAFs was significantly associated with an aggressive BCa phenotype. CKAP4 expression in tumors was an independent prognostic factor for RFS in patients with BCa who underwent RC. The findings of this study indicate that CKAP4 expression in tumors has potential as a novel biomarker for predicting tumor aggressiveness and poor prognosis in cases of BCa. Previous studies on CKAP4 in BCa are limited and involved basic research. Therefore, this clinical study using real-world data is crucial for determining the usefulness of CKAP4 as a novel clinical biomarker for BCa.
Author Contributions
Conceptualization, H.K., Y.S. (Yuichi Sato) and K.M.; methodology, A.S., K.Y., Y.S. (Yuriko Shimizu), Y.S. (Yuichi Sato) and K.M.; formal analysis, H.K., D.K. and Y.S. (Yuichi Sato); investigation, H.K., D.K., S.H., Y.S. (Yuriko Shimizu), W.H., S.S., M.I., H.T. and D.I.; data curation, H.K.; writing—original draft preparation, H.K.; writing—review and editing, D.K., Y.S. (Yuichi Sato) and K.M.; supervision, K.M. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported in part by the Japan Society for the Promotion of Science Grants-in-Aid for Scientific Research (KAKENHI; Grant No. JP24K12515 to K.M.).
Institutional Review Board Statement
This study was conducted in accordance with the guidelines of the Declaration of Helsinki and was approved by the Institutional Review Board of Kitasato University School of Medicine and Hospital on 24 May 2017 (Protocol code B17-010).
Informed Consent Statement
Informed consent was not individually obtained from all participants, as this study was conducted retrospectively. Information regarding the study and the opportunity to opt-out was provided through our institutional website and posters.
Data Availability Statement
The datasets used and/or analyzed during the study are available from the corresponding author upon reasonable request.
Conflicts of Interest
Author Yuichi Sato was employed by the company KITASATO-OTSUKA Biomedical Assay Laboratories Co., Ltd. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| CKAP4 | Cytoskeleton-associated protein 4 |
| BCa | Bladder cancer |
| RC | Radical cystectomy |
| RFS | Recurrence-free survival |
| LN | Lymph node |
| MIBC | Muscle-invasive bladder cancer |
| NMIBC | Non-muscle-invasive bladder cancer |
| NAC | Neoadjuvant chemotherapy |
| AC | Adjuvant chemotherapy |
| LVI | Lymphovascular invasion |
| CAF | Cancer-associated fibroblast |
| CIS | Carcinoma in situ |
| SC | Salvage chemotherapy |
| TBS | Tris-buffered saline |
| CSS | Cancer-specific survival |
| myCAF | Myofibroblast-like cancer-associated fibroblast |
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Hautmann, R.E.; de Petriconi, R.C.; Pfeiffer, C.; Volkmer, B.G. Radical cystectomy for urothelial carcinoma of the bladder without neoadjuvant or adjuvant therapy: Long-term results in 1100 patients. Eur. Urol. 2012, 61, 1039–1047. [Google Scholar] [CrossRef]
- Witjes, J.A.; Compérat, E.; Cowan, N.C.; De Santis, M.; Gakis, G.; Lebret, T.; Ribal, M.J.; Van der Heijden, A.G.; Sherif, A. EAU guidelines on muscle-invasive and metastatic bladder cancer. Eur. Urol. 2014, 65, 778–792. [Google Scholar] [CrossRef] [PubMed]
- Shariat, S.F.; Tokunaga, H.; Zhou, J.H.; Kim, J.H.; Ayala, G.E.; Benedict, W.F.; Lerner, S.P. p53, p21, pRB, and p16 expression predict clinical outcome in cystectomy with bladder cancer. J. Clin. Oncol. 2004, 22, 1014–1024. [Google Scholar] [CrossRef]
- Shariat, S.F.; Bolenz, C.; Godoy, G.; Fradet, Y.; Ashfaq, R.; Karakiewicz, P.I.; Isbarn, H.; Jeldres, C.; Rigaud, J.; Sagalowsky, A.I.; et al. Predictive value of combined immunohistochemical markers in patients with pT1 urothelial carcinoma at radical cystectomy. J. Urol. 2009, 182, 78–84; discussion 84. [Google Scholar] [CrossRef] [PubMed]
- Lotan, Y.; Bagrodia, A.; Passoni, N.; Rachakonda, V.; Kapur, P.; Arriaga, Y.; Bolenz, C.; Margulis, V.; Raj, G.V.; Sagalowsky, A.I.; et al. Prospective evaluation of a molecular marker panel for prediction of recurrence and cancer-specific survival after radical cystectomy. Eur. Urol. 2013, 64, 465–471. [Google Scholar] [CrossRef]
- Schweizer, A.; Ericsson, M.; Bächi, T.; Griffiths, G.; Hauri, H.P. Characterization of a novel 63 kDa membrane protein. Implications for the organization of the ER-to-Golgi pathway. J. Cell Sci. 1993, 104, 671–683. [Google Scholar] [CrossRef]
- Li, S.X.; Li, J.; Dong, L.W.; Guo, Z.Y. Cytoskeleton-associated protein 4, a promising biomarker for tumor diagnosis and therapy. Front. Mol. Biosci. 2020, 7, 552056. [Google Scholar] [CrossRef]
- Schweizer, A.; Rohrer, J.; Hauri, H.P.; Kornfeld, S. Retention of p63 in an ER-Golgi intermediate compartment depends on the presence of all three of its domains and on its ability to form oligomers. J. Cell Biol. 1994, 126, 25–39. [Google Scholar] [CrossRef]
- Chen, Z.Y.; Wang, T.; Gan, X.; Chen, S.H.; He, Y.T.; Wang, Y.Q.; Zhang, K.H. Cytoskeleton-associated membrane protein 4 is upregulated in tumor tissues and is associated with clinicopathological characteristics and prognosis in hepatocellular carcinoma. Oncol. Lett. 2020, 19, 3889–3898. [Google Scholar] [CrossRef]
- Kajiwara, C.; Fumoto, K.; Kimura, H.; Nojima, S.; Asano, K.; Odagiri, K.; Yamasaki, M.; Hikita, H.; Takehara, T.; Doki, Y.; et al. p63-dependent Dickkopf3 expression promotes esophageal cancer cell proliferation via CKAP4. Cancer Res. 2018, 78, 6107–6120. [Google Scholar] [CrossRef] [PubMed]
- Sun, C.M.; Geng, J.; Yan, Y.; Yao, X.; Liu, M. Overexpression of CKAP4 is associated with poor prognosis in clear cell renal cell carcinoma and functions via cyclin B signaling. J. Cancer 2017, 8, 4018–4026. [Google Scholar] [CrossRef]
- Kimura, H.; Yamamoto, H.; Harada, T.; Fumoto, K.; Osugi, Y.; Sada, R.; Maehara, N.; Hikita, H.; Mori, S.; Eguchi, H.; et al. CKAP4, a DKK1 receptor, is a biomarker in exosomes derived from pancreatic cancer and a molecular target for therapy. Clin. Cancer Res. 2019, 25, 1936–1947. [Google Scholar] [CrossRef]
- Sun, X.; Xie, L.; Qiu, S.; Li, H.; Zhou, Y.; Zhang, H.; Zhang, Y.; Zhang, L.; Xie, T.; Chen, Y. Elucidation of CKAP4-remodeled cell mechanics in driving metastasis of bladder cancer through aptamer-based target discovery. Proc. Natl. Acad. Sci. USA 2022, 119, e2110500119. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, K.; Tabata, K.; Hirayama, T.; Shimura, S.; Nishi, M.; Ishii, D.; Fujita, T.; Iwamura, M. Robot-assisted laparoscopic radical cystectomy is a safe and effective procedure for patients with bladder cancer compared to laparoscopic and open surgery: Perioperative outcomes of a single-center experience. Asian J. Surg. 2019, 42, 189–196. [Google Scholar] [CrossRef]
- Matsumoto, K.; Ikeda, M.; Sato, Y.; Kuruma, H.; Kamata, Y.; Nishimori, T.; Tomonaga, T.; Nomura, F.; Egawa, S.; Iwamura, M. Loss of periplakin expression is associated with pathological stage and cancer-specific survival in patients with urothelial carcinoma of the urinary bladder. Biomed. Res. 2014, 35, 201–206. [Google Scholar] [CrossRef] [PubMed]
- Yanagita, K.; Nagashio, R.; Jiang, S.X.; Kuchitsu, Y.; Hachimura, K.; Ichinoe, M.; Igawa, S.; Fukuda, E.; Goshima, N.; Satoh, Y.; et al. Cytoskeleton-associated protein 4 is a novel serodiagnostic marker for lung cancer. Am. J. Pathol. 2018, 188, 1328–1333. [Google Scholar] [CrossRef]
- Nagoya, A.; Sada, R.; Kimura, H.; Yamamoto, H.; Morishita, K.; Miyoshi, E.; Morii, E.; Shintani, Y.; Kikuchi, A. CKAP4 is a potential exosomal biomarker and therapeutic target for lung cancer. Transl. Lung Cancer Res. 2023, 12, 408–426. [Google Scholar] [CrossRef]
- Akanda, M.R.; Ahn, E.J.; Kim, Y.J.; Salam, S.M.A.; Noh, M.G.; Kim, S.S.; Jung, T.Y.; Kim, I.Y.; Kim, C.H.; Lee, K.H.; et al. Different Expression and Clinical Implications of Cancer-Associated Fibroblast (CAF) Markers in Brain Metastases. J. Cancer 2023, 14, 464–479. [Google Scholar] [CrossRef]
- Saito, D.; Tadokoro, R.; Nagasaka, A.; Yoshino, D.; Teramoto, T.; Mizumoto, K.; Funamoto, K.; Kidokoro, H.; Miyata, T.; Tamura, K.; et al. Stiffness of primordial germ cells is required for their extravasation in avian embryos. IScience 2022, 25, 105629. [Google Scholar] [CrossRef]
- Innocenti, M. New insights into the formation and the function of lamellipodia and ruffles in mesenchymal cell migration. Cell Adh. Migr. 2018, 12, 401–416. [Google Scholar] [CrossRef] [PubMed]
- Carmona, G.; Perera, U.; Gillett, C.; Naba, A.; Law, A.L.; Sharma, V.P.; Wang, J.; Wyckoff, J.; Balsamo, M.; Mosis, F.; et al. Lamellipodin promotes invasive 3D cancer cell migration via regulated interactions with Ena/VASP and SCAR/WAVE. Oncogene 2016, 35, 5155–5169. [Google Scholar] [CrossRef]
- Giralt, I.; Gallo-Oller, G.; Navarro, N.; Zarzosa, P.; Pons, G.; Magdaleno, A.; Segura, M.F.; Sábado, C.; Hladun, R.; Arango, D.; et al. Dickkopf-1 inhibition reactivates Wnt/β-catenin signaling in rhabdomyosarcoma, induces myogenic markers in vitro and impairs tumor cell survival in vivo. Int. J. Mol. Sci. 2021, 22, 12921. [Google Scholar] [CrossRef] [PubMed]
- Niida, A.; Hiroko, T.; Kasai, M.; Furukawa, Y.; Nakamura, Y.; Suzuki, Y.; Sugano, S.; Akiyama, T. DKK1, a negative regulator of Wnt signaling, is a target of the β-catenin/TCF pathway. Oncogene 2004, 23, 8520–8526. [Google Scholar] [CrossRef]
- Shinno, N.; Kimura, H.; Sada, R.; Takiguchi, S.; Mori, M.; Fumoto, K.; Doki, Y.; Kikuchi, A. Activation of the Dick-kopf1-CKAP4 pathway is associated with poor prognosis of esophageal cancer and anti-CKAP4 antibody may be a new therapeutic drug. Oncogene 2018, 37, 3471–3484. [Google Scholar] [CrossRef] [PubMed]
- Sada, R.; Yamamoto, H.; Matsumoto, S.; Harada, A.; Kikuchi, A. Newly developed humanized anti-CKAP4 antibody suppresses pancreatic cancer growth by inhibiting DKK1-CKAP4 signaling. Cancer Sci. 2024, 115, 3358–3369. [Google Scholar] [CrossRef] [PubMed]
- Shen, C.H.; Hsieh, H.Y.; Wang, Y.H.; Chen, S.Y.; Tung, C.L.; Wu, J.D.; Lin, C.T.; Chan, M.W.Y.; Hsu, C.D.; Chang, D. High Dickkopf-1 expression is associated with poor prognosis in patients with advanced urothelial carcinoma. Exp. Ther. Med. 2010, 1, 893–898. [Google Scholar] [CrossRef]
- Gladka, M.M.; Molenaar, B.; de Ruiter, H.; van der Elst, S.; Tsui, H.; Versteeg, D.; Lacraz, G.P.A.; Huibers, M.M.H.; van Oudenaarden, A.; van Rooij, E. Single-cell sequencing of the healthy and diseased heart reveals cytoskeleton-associated protein 4 as a new modulater of fibroblasts activation. Circulation 2018, 138, 166–180. [Google Scholar] [CrossRef]
- Yang, D.; Liu, J.; Qian, H.; Zhuang, Q. Cancer-associated fibroblasts: From basic science to anticancer therapy. Exp. Mol. Med. 2023, 55, 1322–1332. [Google Scholar] [CrossRef]
- Du, Y.H.; Sui, Y.Q.; Cao, J.; Jiang, X.; Wang, Y.; Yu, J.; Wang, B.; Wang, X.Z.; Xue, B.X. Dynamic changes in myofibroblasts affect the carcinogenesis and prognosis of bladder cancer associated with tumor microenvironment remodeling. Front. Cell Dev. Biol. 2022, 10, 833578. [Google Scholar] [CrossRef]
- Thinyakul, C.; Sakamoto, Y.; Shimoda, M.; Liu, Y.; Thongchot, S.; Reda, O.; Nita, A.; Sakamula, R.; Sampattavanich, S.; Maeda, A.; et al. Hippo pathway in cancer cells induces NCAM1+αSMA+ fibroblasts to modulate tumor microenvironment. Commun. Biol. 2024, 7, 1343. [Google Scholar] [CrossRef] [PubMed]
- Lavie, D.; Ben-Shmuel, A.; Erez, N.; Scherz-Shouval, R. Cancer-associated fibroblasts in the single-cell era. Nat. Cancer 2022, 3, 793–807. [Google Scholar] [CrossRef] [PubMed]
- Ofner, H.; Laukhtina, E.; Hassler, M.R.; Shariat, S.F. Blood-Based Biomarkers as Prognostic Factors of Recurrent Disease after Radical Cystectomy: A Systematic Review and Meta-Analysis. Int. J. Mol. Sci. 2023, 24, 5846. [Google Scholar] [CrossRef] [PubMed]
- Malinaric, R.; Mantica, G.; Monaco, L.L.; Mariano, F.; Leonardi, R.; Simonato, A.; der Merwe, A.V.; Terrone, C. The Role of Novel Bladder Cancer Diagnostic and Surveillance Biomarkers-What Should a Urologist Really Know? Int. J. Environ. Res. Public Health 2022, 19, 9648. [Google Scholar] [CrossRef]
- Tuffy, K.M.; Planey, S.L. Cytoskeleton-associated protein 4: Functions beyond the endoplasmic reticulum in physiology and disease. ISRN Cell Biol. 2012, 2012, 142313. [Google Scholar] [CrossRef][Green Version]
- Di Como, C.J.; Urist, M.J.; Babayan, I.; Drobnjak, M.; Hedvat, C.V.; Teruya-Feldstein, J.; Pohar, K.; Hoos, A.; Cordon-Cardo, C. p63 expression profiles in human normal and tumor tissues. Clin. Cancer Res. 2002, 8, 494–501. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).