Social Burden and Healthcare Costs of Colorectal Cancer
Simple Summary
Abstract
1. Introduction
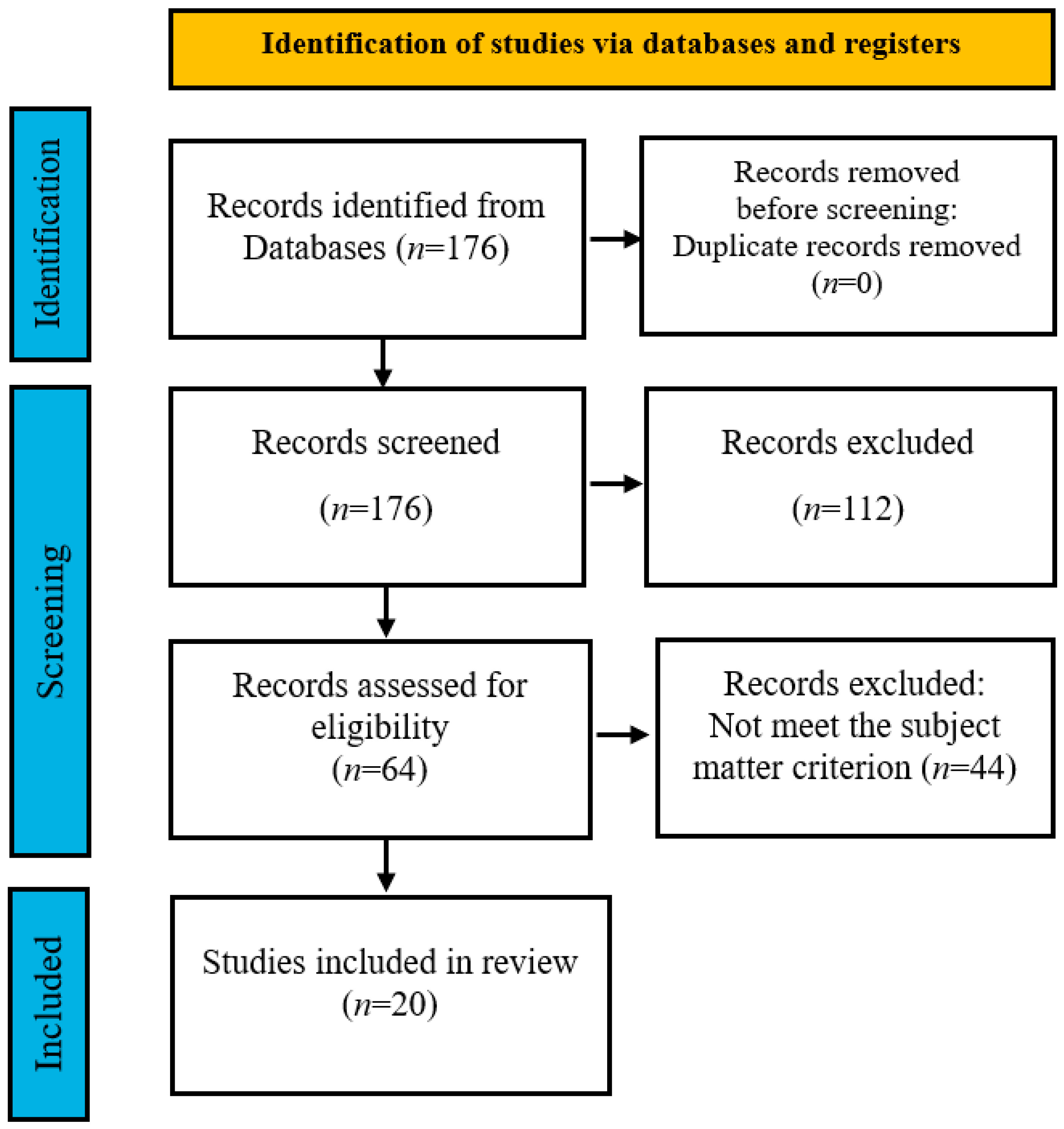
2. Materials and Methods
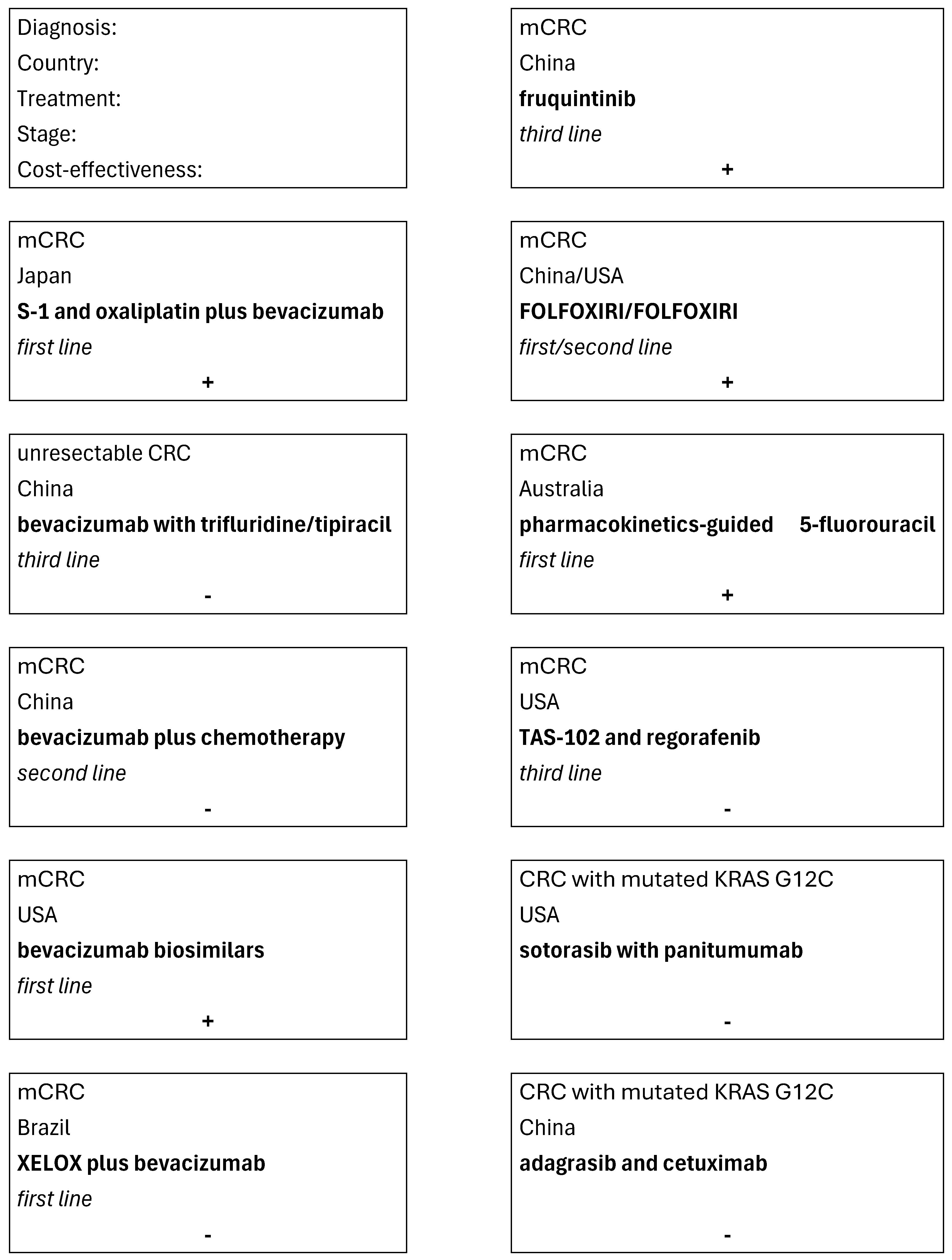
3. Results
3.1. Direct Costs
3.1.1. Treatment of Colorectal Cancer
3.1.2. Screening After Treatment
3.2. Indirect and Social Costs
4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. International Agency for Research on Cancer. Available online: https://gco.iarc.who.int/media/globocan/factsheets/cancers/41-colorectum-fact-sheet.pdf (accessed on 11 November 2025).
- WHO. Cancer Tomorrow. Available online: https://gco.iarc.who.int/tomorrow/en/dataviz/bars?types=0&sexes=0&mode=population&group_populations=0&multiple_populations=1&multiple_cancers=1&cancers=41&populations=903_904_905_908_909_935&apc=cat_ca20v1.5_ca23v-1.5&group_cancers=1&years=2050 (accessed on 11 November 2025).
- WHO. Newsroom. Available online: https://www.who.int/news-room/fact-sheets/detail/colorectal-cancer (accessed on 11 November 2025).
- National Cancer Institute. Colorectal Cancer Screening (PDQ®)–Health Professional Version. Available online: https://www.cancer.gov/types/colorectal/hp/colorectal-screening-pdq (accessed on 11 November 2025).
- Ibarrondo, O.; Lizeaga, G.; Martínez-Llorente, J.M.; Larrañaga, I.; Soto-Gordoa, M.; Álvarez-López, I. Health care costs of breast, prostate, colorectal and lung cancer care by clinical stage and cost component. Gac. Sanit. 2022, 36, 246–252. [Google Scholar] [CrossRef] [PubMed]
- Akobundu, E.; Ju, J.; Blatt, L.; Mullins, C.D. Cost-of-illness studies: A review of current methods. Pharmacoeconomics 2006, 24, 869–890. [Google Scholar] [CrossRef]
- Fudali, K.; Sagan, K.; Kwiatkowska, E.; Kosendiak, A. The impact of the early period of the COVID-19 pandemic on screening programmes of breast, colorectal and cervical cancer. J. Health Inequal. 2023, 9, 37–42. [Google Scholar] [CrossRef]
- Thallinger, C.; Belina, I.; Comanescu, A.; Cufer, T.; Jassem, J.; Kiesewetter, B.; Zielinski, C. Limitations of cancer care in Central and South-Eastern Europe: Results of the international conference organized by the Central European Cooperative Oncology Group (CECOG). J. Health Inequalities 2020, 6, 139–152. [Google Scholar] [CrossRef]
- UN Operational Rates of Exchange. United Nations Treasury. Available online: https://treasury.un.org/operationalrates/OperationalRates.php (accessed on 11 November 2025).
- Morimoto, T.; Fujito, K.; Goto, R. Cost-Effectiveness Analysis of SOX Plus Bevacizumab Versus SOX Plus Cetuximab for First-Line Treatment of KRAS Wild-Type Metastatic Colorectal Cancer in Japan. Clin. Ther. 2025, 47, 347–354. [Google Scholar] [CrossRef]
- Huang, L.Z.; Chen, Y.Q.; Gu, H.Y.; Chen, Y. Cost-effectiveness analysis of trifluridine/tipiracil combined with bevacizumab vs. monotherapy for third-line treatment of colorectal cancer. Front. Public Health 2024, 12, 1465898. [Google Scholar] [CrossRef]
- Li, Y.; Hu, M.; Zhang, Z.; Chu, M.; Xu, R.; Liu, L.; Zhang, R. Cost-effectiveness analysis of continuing bevacizumab plus chemotherapy versus chemotherapy alone after first progression of metastatic colorectal cancer. Cancer Med. 2024, 13, e6904. [Google Scholar] [CrossRef]
- Lu, B.; Dvorani, E.; Nguyen, L.; Beca, J.M.; Mercer, R.E.; Adamic, A.; Munoz, C.; Chan, K.K. Cost-Effectiveness Analysis of Bevacizumab Biosimilars Versus Originator Bevacizumab for Metastatic Colorectal Cancer: A Comparative Study Using Real-World Data. Value Health J. Int. Soc. Pharmacoecon. Outcomes Res. 2024, 27, 1689–1697. [Google Scholar] [CrossRef]
- Ungari, A.Q.; Pereira LR, L.; Nunes, A.A.; Peria, F.M. Cost-effectiveness analysis of XELOX versus XELOX plus bevacizumab for metastatic colorectal cancer in a public hospital school. BMC Cancer 2017, 17, 691. [Google Scholar] [CrossRef][Green Version]
- Huang, Z.; Zhou, L.; Zheng, H.; Zhan, M. Cost-effectiveness analysis of fruquintinib in Chinese patients with refractory metastatic colorectal cancer. Int. J. Clin. Pharm. 2024, 46, 872–880. [Google Scholar] [CrossRef]
- Li, X.; Bao, J.; Ma, J. Cost-effectiveness analysis of FOLFOXIRI/FOLFOXIRI and mFOLFOX6/FOLFIRI treatment in first-line and second-line chemotherapy for metastatic colorectal cancer. BMJ Open 2025, 15, e086372. [Google Scholar] [CrossRef]
- Erku, D.; Martin, J.H.; Michael, M.; Galettis, P.; Scuffham, P. Economic evaluation of personalized vs. standard dosing of 5-fluorouracil in first-line chemotherapy for metastatic colorectal cancer in Australia. Br. J. Clin. Pharmacol. 2025, 91, 1610–1618. [Google Scholar] [CrossRef]
- Cho, S.K.; Hay, J.W.; Barzi, A. Cost-effectiveness Analysis of Regorafenib and TAS-102 in Refractory Metastatic Colorectal Cancer in the United States. Clin. Color. Cancer 2018, 17, e751–e761. [Google Scholar] [CrossRef]
- Liu, T.; Yao, Y.; Teng, X.; Tong, Z.; Dong, M.; Yao, R. Cost-effectiveness analysis of sotorasib plus panitumumab in the treatment of refractory colorectal cancer with mutated KRAS G12C in the USA. Expert Rev. Pharmacoecon. Outcomes Res. 2025, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Yao, R.; Yao, Y.; Teng, X.; Jin, Y.; Guan, S.; Dong, M.; Liu, T. Cost-effectiveness analysis of adagrasib with or without cetuximab in the treatment of colorectal cancer patients with mutated KRAS G12C. Expert Rev. Pharmacoecon. Outcomes Res. 2025, 1–9. [Google Scholar] [CrossRef]
- Gana, A.I.; Bica, C.; Ciocan, C.A.; Moșteanu, E.O.; Pop, T.A.; Berindan-Neagoe, I.; Vlad, I.C.; Achimaș-Cadariu, P.A. Cost, Cost-effectiveness and Survival Impact Assessment for A Better Management of Colorectal Cancer Patients: A Single Centre Comprehensive Analysis. J. Gastrointest. Liver Dis. 2024, 33, 496–502. [Google Scholar] [CrossRef]
- Yang, O.; Zhang, Y.; To, Y.H.; IJzerman, M.M.; Liu, J.; Gibbs, P.; Franchini, F.; PRIMCAT Group. Effects of clinical and socioeconomic factors on Medicare and patient costs for colorectal cancer in Australia: A retrospective multivariate regression analysis. BMJ Open 2024, 14, e081483. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Z.X.; Peng, Y.X.; Ye, J.H.; Wei, Y. The Economic Burden of Colorectal Cancer in Type 2 Diabetes Mellitus (T2DM) in Shanghai, China. Cancer Med. 2025, 14, e70651. [Google Scholar] [CrossRef]
- Garg, R.; Sayre, E.C.; Pataky, R.; McTaggart-Cowan, H.; Peacock, S.; Loree, J.M.; De Vera, M.A. Direct Medical Spending on Young and Average-Age Onset Colorectal Cancer before and after Diagnosis: A Population-Based Costing Study. Cancer Epidemiol. Biomark. Prev. 2024, 33, 72–79. [Google Scholar] [CrossRef]
- Bovell, A.A.; Ncayiyana, J.; Ginindza, T.G. Analysis of the Direct Medical Costs of Colorectal Cancer in Antigua and Barbuda: A Prevalence-Based Cost-of-Illness Study. Int. J. Environ. Res. Public Health 2025, 22, 552. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Li, Y.J.; Lei, L.; Liu, C.C.; Chen, W.Q.; Dai, M.; He, J. Estimating the economic burden of colorectal cancer in China, 2019–2030: A population-level prevalence-based analysis. Cancer Med. 2024, 13, e6787. [Google Scholar] [CrossRef] [PubMed]
- Gorasso, V.; Vandevijvere, S.; Van der Heyden, J.; Pelgrims, I.; Hilderink, H.; Nusselder, W.; Devleesschauwer, B. The incremental healthcare cost associated with cancer in Belgium: A registry-based data analysis. Cancer Med. 2024, 13, e6659. [Google Scholar] [CrossRef] [PubMed]
- Takashima, A.; Ishiguro, M.; Sasaki, K.; Machida, R.; Nagashima, F.; Imaizumi, J.; Hamaguchi, T.; Yamamoto, Y.; Masuishi, T.; Asayama, M.; et al. Real-world treatment costs of first-line treatment for metastatic colorectal cancer: A survey of the JCOG colo-rectal cancer study group. Jpn. J. Clin. Oncol. 2024, 54, 1107–1114. [Google Scholar] [CrossRef]
- Takayama, Y.; Tsukamoto, S.; Kudose, Y.; Takamizawa, Y.; Moritani, K.; Esaki, M.; Igarashi, A. Cost-effectiveness of surveillance intervals after curative resection of colorectal cancer. Jpn. J. Clin. Oncol. 2024, 54, 637–646. [Google Scholar] [CrossRef]
- Leite, L.F.; Noronha, M.M.; de Menezes, J.S.A.; da Conceição, L.D.; Almeida LF, C.; Cappellaro, A.P.; Megid, T.B.C. Anti-EGFR Therapy in Metastatic Colorectal Cancer: Identifying, Tracking, and Overcoming Resistance. Cancers 2025, 17, 2804. [Google Scholar] [CrossRef]
- Han, J.; Xiao, D.; Tan, C.; Zeng, X.; Hu, H.; Zeng, S.; Shen, L. Cost-Effectiveness Analysis of First-Line FOLFIRI Combined with Cetuximab or Bevacizumab in Patients with RAS Wild-Type Left-Sided Metastatic Colorectal Cancer. Cancer Control. J. Moffitt Cancer Cent. 2020, 27, 1073274820902271. [Google Scholar] [CrossRef]
- Cervantes, A.; Adam, R.; Roselló, S.; Arnold, D.; Normanno, N.; Taïeb, J.; Seligmann, J.; De Baere, T.; Osterlund, P.; Yoshino, T.; et al. Metastatic colorectal cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up. Ann. Oncol. 2023, 34, 10–32. [Google Scholar] [CrossRef] [PubMed]
| Year | Africa | Latin America and the Caribbean | Northern America | Europe | Oceania | Asia | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Risk (%) | n | Risk (%) | n | Risk (%) | n | Risk (%) | n | Risk (%) | n | Risk (%) | |
| 2022 | 70,428 | 0 | 145,120 | 0 | 183,973 | 0 | 538,262 | 0 | 22,243 | 0 | 966,399 | 0 |
| 2025 | 77,410 | 9.9 | 152,882 | 5.3 | 194,879 | 5.9 | 552,399 | 2.6 | 24,383 | 9.6 | 1,046,155 | 8.3 |
| 2030 | 91,835 | 30.4 | 177,077 | 22.0 | 211,254 | 14.8 | 592,761 | 10.1 | 27,683 | 24.5 | 1,209,940 | 25.2 |
| 2035 | 108,656 | 54.3 | 203,323 | 40.1 | 226,382 | 23.1 | 629,311 | 16.9 | 31,032 | 39.5 | 1,383,209 | 43.1 |
| 2040 | 127,972 | 81.7 | 230,655 | 58.9 | 239,441 | 30.2 | 659,365 | 22.5 | 34,229 | 53.9 | 1,553,816 | 60.8 |
| 2045 | 149,855 | 112.8 | 258,059 | 77.8 | 250,208 | 36.0 | 681,867 | 26.7 | 37,299 | 67.7 | 1,714,698 | 77.4 |
| 2050 | 174,396 | 147.6 | 284,828 | 96.3 | 259,177 | 40.9 | 696,727 | 29.4 | 40,280 | 81.1 | 1,866,959 | 93.2 |
| Population (P) | Patients Diagnosed with Colorectal Cancer |
|---|---|
| Intervention (I) | Costs, Economics |
| Comparator (C) | Any or none |
| Outcomes (O) | Direct costs of colorectal cancer treatment, indirect costs of colorectal cancer, economic burden |
| Studies (S) | Case studies, prospective studies, retrospective studies, systematic review, RCT |
| Limitations | Publications in English assessing the impact of colorectal cancer on the quality of life, publication period 01.01.2023–30.05.2025 |
| Exclusion | Non-English publications, studies not directly linked to colorectal cancer |
| Author/Year | Country | Unit of Measure | Currency | Methodology | Type of Costs | Group of Patients |
|---|---|---|---|---|---|---|
| Morimoto, T. et al., 2025 [10] | Japan | QALY, ICER | USD | Cost-effectiveness analysis | Direct costs | Patients with Kirsten rat sarcoma virus wild-type metastatic colorectal cancer |
| Huang, L. et al., 2024 [11] | China | QALY, ICER | CNY | Cost-effectiveness analysis | Direct costs | Patients with colorectal cancer |
| Li, Y. et al., 2024 [12] | China | QALY, ICER | USD | Cost-effectiveness analysis | Direct costs | Patients with metastatic colorectal cancer |
| Lu, B. et al., 2024 [13] | United States | QALY, ICER | USD | Cost-effectiveness analysis | Direct costs | Patients with metastatic colorectal cancer |
| Ungari, A. et al., 2017 [14] | Brazil | QALY, ICER | BRL | Cost evaluation | Direct costs | Patients with metastatic colorectal cancer |
| Huang, Z. et al., 2024 [15] | China | QALY, ICER | USD | Cost-effectiveness analysis | Direct costs | Patients with refractory metastatic colorectal cancer |
| Li, X. et al., 2025 [16] | China, United States | QALY, ICER | USD | Cost-effectiveness analysis | Direct costs | Patients with metastatic colorectal cancer |
| Erku, D. et al., 2025 [17] | Australia | QALY, ICER | USD | Cost evaluation | Direct costs | Patients with metastatic colorectal cancer |
| Cho, S. et al., 2018 [18] | United States | QALY, ICER | USD | Cost-effectiveness analysis | Direct costs | Patients with metastatic colorectal cancer |
| Liu, T. et al., 2025 [19] | United States | QALY, ICER | USD | Cost-effectiveness analysis | Direct costs | Patients with metastatic colorectal cancer with mutated KRAS G12C |
| Yao, R. et al., 2025 [20] | United States | QALY, ICER | USD | Cost-effectiveness analysis | Direct costs | Patients with metastatic colorectal cancer with mutated KRAS G12C |
| Gana, A. et al., 2024 [21] | Romania | ICER | EUR | Cost evaluation | Direct costs | Patients with colorectal cancer |
| Yang, O. et al., 2024 [22] | Australia | - | AUD | Cost evaluation | Direct costs | Patients with colorectal cancer |
| Zhu, Z. et al., 2025 [23] | China | QALY | CNY | Cost evaluation | Direct and indirect costs | Patients with colorectal cancer and Type 2 Diabetes Mellitus |
| Garg, R. et al., 2024 [24] | United States | - | USD | Cost evaluation | Direct costs | Patients with young onset colorectal cancer |
| Bovell, A. et al., 2025 [25] | Antigua and Barbuda | - | USD | Cost evaluation | Direct costs | Patients with colorectal cancer |
| Wang, H. et al., 2024 [26] | China | - | CNY | Cost evaluation | Direct and indirect costs | Patients with colorectal cancer |
| Gorasso, V. et al., 2024 [27] | Belgium | - | EUR | Cost evaluation | Direct costs | Patients with colorectal cancer |
| Takashima, A. et al., 2024 [28] | Japan | - | JPY | Cost evaluation | Direct costs | Patients with metastatic colorectal cancer |
| Takayama, Y. et al., 2024 [29] | England | ICER | USD | Cost-effectiveness analysis | Direct costs | Patients after curative resection of colorectal cancer |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gąska, I.; Czerw, A.; Pajewska, M.; Partyka, O.; Deptała, A.; Badowska-Kozakiewicz, A.; Czerw, N.; Mękal, D.; Sygit, K.; Malikowska, K.; et al. Social Burden and Healthcare Costs of Colorectal Cancer. Cancers 2025, 17, 3678. https://doi.org/10.3390/cancers17223678
Gąska I, Czerw A, Pajewska M, Partyka O, Deptała A, Badowska-Kozakiewicz A, Czerw N, Mękal D, Sygit K, Malikowska K, et al. Social Burden and Healthcare Costs of Colorectal Cancer. Cancers. 2025; 17(22):3678. https://doi.org/10.3390/cancers17223678
Chicago/Turabian StyleGąska, Izabela, Aleksandra Czerw, Monika Pajewska, Olga Partyka, Andrzej Deptała, Anna Badowska-Kozakiewicz, Natalia Czerw, Dominika Mękal, Katarzyna Sygit, Klaudia Malikowska, and et al. 2025. "Social Burden and Healthcare Costs of Colorectal Cancer" Cancers 17, no. 22: 3678. https://doi.org/10.3390/cancers17223678
APA StyleGąska, I., Czerw, A., Pajewska, M., Partyka, O., Deptała, A., Badowska-Kozakiewicz, A., Czerw, N., Mękal, D., Sygit, K., Malikowska, K., Drobnik, J., Pobrotyn, P., Waśko-Czopnik, D., Sowiński, T., Bandurska, E., Ciećko, W., Grochans, E., Cybulska, A. M., Schneider-Matyka, D., ... Kozlowski, R. (2025). Social Burden and Healthcare Costs of Colorectal Cancer. Cancers, 17(22), 3678. https://doi.org/10.3390/cancers17223678










