Simple Summary
Textbook outcome (TO) is a novel composite measure that provides a comprehensive evaluation of a specific treatment which can be useful for procedures’ standardization and reliable comparisons between different centers. This tool is gaining growing interest and widespread importance in many different fields. Considering liver surgery, however, an agreement was reached, and TO assessment was evaluated on a large scale only concerning liver resection. This study aimed to investigate the first TO for laparoscopic microwave ablation for hepatocellular carcinoma. Furthermore, the current study investigated the expendability of this tool for prognostic purposes.
Abstract
In the context of spreading interest in textbook outcome (TO) evaluation in different fields, we aimed to investigate an uncharted procedure, that is, laparoscopic microwave ablation (MWA) for hepatocellular carcinoma (HCC). Absence of post-MWA complications, a hospital stay of three days, no mortality nor readmission within 30 days, and complete response of the target lesion at post-MWA CT scan defined TO achievement. Patients treated between January 2014 and March 2021 were retrospectively reviewed, and of the 521 patients eligible for the study, 337 (64.7%) fulfilled all the quality indicators to achieve the TO. The absence of complications was the main limiting factor for accomplishing TO. At multivariable analysis, Child–Pugh B cirrhosis, age of more than 70 years old, three nodules, and MELD score ≥ 15 were associated with decreased probabilities of TO achievement. A score based on these factors was derived from multivariable analysis, and patients were divided into three risk groups for TO achievement. At survival analysis, overall survival (OS) was significantly (p = 0.001) higher in patients who achieved TO than those who did not. Moreover, OS evaluation in the three risk groups showed a trend coherent with TO achievement probability. The present study, having assessed the first TO for laparoscopic MWA for HCC, encourages further broader consensus on its definition and, on its basis, on the development of clinically relevant tools for managing treatment allocation.
1. Introduction
Textbook outcome (TO) is a composite measure that captures the most desirable outcomes of a specific treatment as a single indicator. This tool is fundamental in the surgical field because treatment outcome is a complex synthesis of multiple variables such as peri-operative factors, postoperative morbidity, and oncological radicality (R0). In the current era, TO is becoming a spreading tool to measure the quality of surgical procedures in multiple specialties such as hepatic, pancreatic, head and neck, lung [1,2,3,4,5], and even transplantation [6,7,8,9] surgery. TO is functional for procedures’ standardization and to weigh their cost-effectiveness considering tailored medicine. Moreover, it allows for comparing different centers’ activities in a more reliable and standardized fashion.
Concerning liver surgery, an international agreement about the definition of TO for resection, both in a laparoscopic and open setting, was recently investigated and reached [10]. Furthermore, its incidence in an extensive international multicenter database was assessed [11].
Serra et al. [12] published the first TO for percutaneous radiofrequency ablation (RFA) for hepatocellular carcinoma (HCC), showing that moderate comorbidities, Eastern Cooperative Oncology Group (ECOG) Performance Status (PS), postoperative complications, number and diameter of nodules were the variables critical for TO achievement.
Given our remarkable experience with laparoscopic microwave ablation (MWA) for HCC [13], with the present study, we aim to investigate the first TO for this minimally invasive surgical procedure.
2. Materials and Methods
This is a retrospective analysis from a prospectively collected database of HCC patients treated with laparoscopic MWA between January 2014 and March 2021 at General Surgery 2-Hepato-pancreato-biliary Surgery and Liver transplantation Unit, Padua University Hospital, Padua, Italy.
Patients included in the study were those undergoing laparoscopic MWA for HCC, either for de novo, treatment-naïve HCC, or for recurrent cases after liver resection (LR) or other treatments. For this study, the exclusion criteria were HCC outside Milan criteria and patients with ECOG PS > 1.
Our center’s selection criteria for laparoscopic MWA were previously described [13], in addition to the surgical procedure [14]. In particular, the laparoscopic approach is indicated when percutaneous is not feasible (Figure 1). A 14-G water-cooled coaxial antenna was inserted into the tumor under US guidance. All MWA utilized a 2.45 MHz microwave generator (AMICA GEN; HS Hospital Service SpA, Aprilia, Italy) with power settings at a median of 40 W (interquartile range (IQR), 30–60 W).
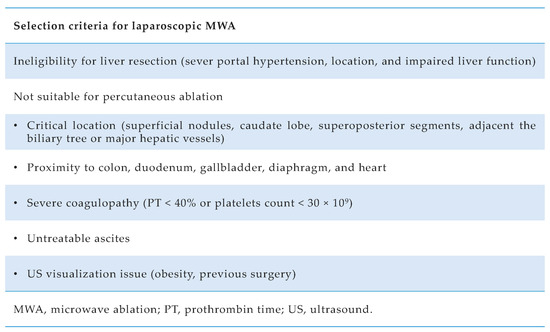
Figure 1.
Selection criteria for laparoscopic microwave ablation in hepatocellular carcinoma (HCC) patients at Padua University Hospital.
Tumor burden (number and dimension of HCC nodules) was measured at the last CT scan or MRI before ablation. In addition, the Adult Comorbidity Evaluation-27 (ACE-27) [15] was used to classify patients’ comorbidities other than cirrhosis.
Laparoscopic MWA complications were censored within 30 postoperative days; complications were recorded as follows: fever (requiring prolongation/change in antimicrobial therapy), nausea and vomiting, pleural effusion (if treated with albumin infusion and diuretic therapy or thoracentesis), pneumothorax (if pleural drainage was needed), ascites (requiring albumin supplementation or diuretics), hemoperitoneum and liver function impairment according to the 50-50 criteria [16]. In addition, the Clavien–Dindo classification [17] was used to grade post-operative complications.
Post-MWA mortality was censored in case of mortality during the hospitalization or within 30 days after the procedure. Readmission due to treatment-related complications of any type was edited within 30 days after the MWA. Prolonged length of stay (LOS) was censored if discharge occurred after the cohort’s 75th percentile of the LOS.
Contrast-enhanced CT or MRI was repeated one month after MWA to assess the efficacy of ablation: the disappearance of any intra-tumoral arterial enhancement in the target lesion/s defined complete response (CR) [18,19].
The analysis was designed per patient rather than per procedure. For each patient, only the first MWA procedure was considered, excluding re-treatments on previous MWA, due to incomplete ablation diagnosed at one month by contrast-enhanced CT scan.
As recently proposed for percutaneous procedures [12], the TO was defined as follows: absence of post-MWA complications, a hospital stay of three days, no mortality nor readmission within 30 days, and complete response of the target lesion at 1-month post-MWA CT scan.
The present study was conducted in compliance with regional ethics committees and national laws of the participating institution: no patient approval was needed due to the study’s retrospective design. Patients gave written consent for every procedure performed in the hospital, including data for medical purposes, which were obtained consistent with the Declaration of Helsinki. All procedures were performed in accordance with the Declaration of Istanbul. No one received compensation or was offered any incentive for participating in this study.
Statistical Analysis
Values for categorical variables were expressed as totals and percentages, whereas values for continuous variables were expressed as medians and interquartile ranges (IQR). Statistical analyses were performed using Pearson’s chi-squared test or Fisher’s test for categorical variables and the Kruskal–Wallis rank sum test for continuous variables.
The length of follow-up was calculated from the surgery date to the patient death (overall survival—OS) or the latest follow-up. The duration of follow-up and survival was expressed as median (interquartile ranges). Survival curves were calculated using the Kaplan–Meier technique and compared with the log-rank test.
Simple and multivariable logistic regression was used to investigate the potential predictors of TO achievement. Stepwise selection (backward elimination) was used to compute multivariable regression analyses. A p-value < 0.05 indicated statistical significance; variables with a p-value < 0.1 were considered marginal statistical significance. Statistical analyses were performed using R, RStudio 4.2.1 (2022).
3. Results
From 1 January 2014, to 31 March 2021, 826 patients underwent laparoscopic MWA for HCC at our center. Two hundred and sixty-seven patients had HCC outside Milan criteria, and thirty-eight scored ECOG PS > 1. Once exclusion criteria were applied, 521 patients were eligible for the study. Four hundred and thirty-nine (84%) patients were male, and the median age was 63.3 years old (IQR 56.9–68.1). Mild comorbidities were present in 53% (n = 274) of patients and moderate in 5.4% (n = 28). Comorbidities other than chronic hepatitis/cirrhosis were absent in 42% (n = 216) of the whole cohort, whereas severe comorbidities were absent. Patients graded as ECOG PS 1 were 60 (12%). Hepatitis C virus (HCV) post-necrotic cirrhosis (PNC) was the primary underlying etiology, and it was present in 246 (47%) patients. One hundred and twelve patients (26%) were classified as Child–Pugh B, and 31 patients (6.2%) had a MELD score ≥15; portal hypertension was present in 55% of the whole cohort. Two hundred and sixty-four (51%) patients had de novo, treatment-naïve HCC/s. A single tumor was treated in 265 (51%) patients, and the maximum diameter of the target lesion was <2 cm in 260 (50%) patients. Clinical and perioperative characteristics are listed in Table 1.

Table 1.
Clinical and perioperative characteristics.
Two patients (0.4%) died within 30 days after the procedure. Five (1%) patients developed a severe complication (Clavien–Dindo ≥ 3b), whereas the majority had no complications (n = 398; 76.4%). The most common mild complication observed was post-operative ascites (n = 61; 11.7%). The median LOS was two days (IQR: 1–3); consequently, discharge after three days was considered a prolonged hospital stay. The readmission rate was 2.30% (n = 12). Finally, CT-scan at one month showed CR of the target lesion/s in 491 (94.2%) patients; only 30 (5.8%) failed to achieve CR at one month CT-scan after MWA. Finally, 162 (31.1%) patients were disease-free at the end of the follow-up (Table 2).

Table 2.
Postoperative outcomes.
3.1. TO Achievement, Determinants, and Risk Groups
A total of 337 (64.7%) patients fulfilled all the parameters to achieve the TO. Achievement of each TO item was calculated separately with cumulative percentages to identify which indicator was the main limiting factor for accomplishing TO. The absence of complications is the item found to have the lowest achievement incidence compared to the others (76%) (Figure 2).
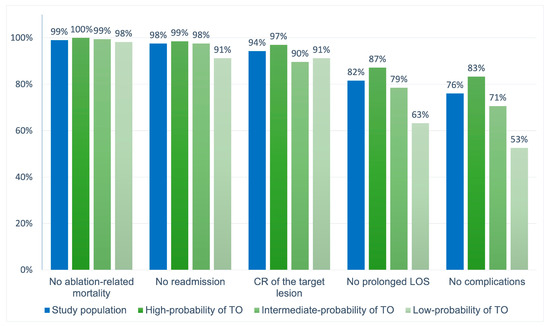
Figure 2.
The proportion of patients who achieved each desired health outcome forming the textbook outcome (TO) in the whole population, and in the three risk groups individually.
Moreover, simple and multivariable logistic regression for determinants of TO achievement was performed, and the results are listed in Table 3.

Table 3.
Simple and multivariable logistic regression for determinants of TO achievement.
As a result of the multivariable analysis, probabilities of TO achievement decreased in patients with Child–Pugh B cirrhosis (comparator: Child–Pugh A; OR: 0.28; 95% CI: 0.17–0.46; p < 0.001), patients more than 70 years old (comparator: age < 70; OR: 0.49; 95% CI: 0.27–0.88; p = 0.017), patients with three nodules (comparator: 1 nodule; OR: 0.54; 95% CI: 0.32–0.93; p = 0.025) and MELD score ≥ 15 (comparator: MELD < 15; OR: 0.44; 95% CI: 0.17–1.09; p = 0.086). The presence of mild or moderate comorbidities other than chronic hepatitis/cirrhosis showed no influence on TO achievement.
At a further analysis, the highest OR value from the multivariable model was used as the lowest common denominator to derive risk points for TO determinants, which were consequently assigned as follows: age ≥ 70, 2 points; MELD ≥ 15, 2 points; 3 nodules, 2 points; Child–Pugh B, 1 point. Three risk groups were then identified based on the cumulative score reached by each patient: patients who scored 0 had a high probability of TO achievement (77.3% TO achievement), those who scored 1–2 had an intermediate-probability of TO achievement (55.8% TO achievement), and those who scored ≥ 3 had low-probability of TO attainment (33.3% TO achievement) (Figure 3). Moreover, Figure 1 shows the accomplishment of every quality indicator forming the TO considered individually in each risk group.
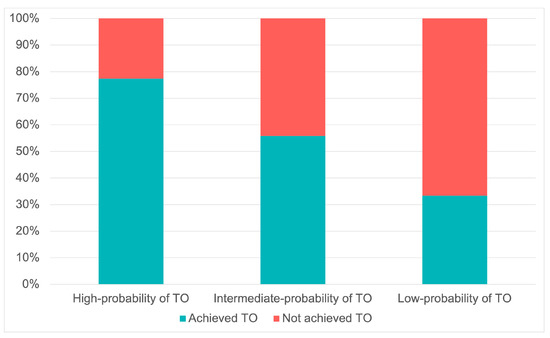
Figure 3.
The proportion of textbook outcome (TO) achievement related to the three risk groups identified.
3.2. Survival Analysis
The median follow-up was 28.7 months (IQR: 14.2–49.9), and the median survival was 51.3 months (95% CI: 45.8–67.1) in the study population. The median survival in the cohort of patients who achieved TO was 62.2 months (95% CI: 49.5–not reached) compared to 32.6 months (95% CI: 27.1–51.4) in the cohort of patients who did not. The OS of patients who achieved TO was 93.9%, 65.7%, and 50.5% at 1, 3, and 5 years, respectively, compared to 1-, 3- and 5-year OS of patients who did not achieve TO that was 79.8%, 47%, and 40.3%, respectively (p = 0.001) (Figure 4).
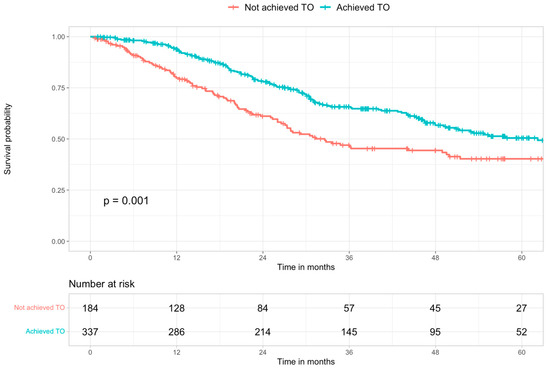
Figure 4.
Kaplan–Meier survival curves of the study population stratified according to textbook outcome (TO) achievement.
When survival analysis was performed, taking into account the risk groups stratification, the highest OS (90.9%, 65.8%, and 52.3% at 1-, 3- and five years, respectively), was observed in the group with the highest probability of TO achievement, with a progressive and significant (p = 0.0055) OS reduction, consensual to the decreasing of TO achievement probability (80.3%, 36.9% and 34.7% at 1-, 3- and 5-years, respectively, in the low-probability group) (Figure 5).
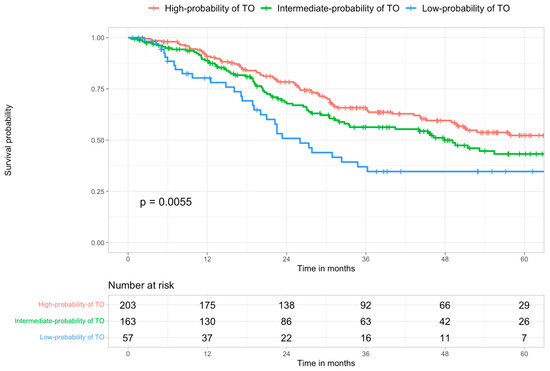
Figure 5.
Kaplan–Meier survival curves of the study population stratified according to the three risk groups identified. High vs. intermediate probability p = 0.0827; high vs. low probability p = 0.0039; intermediate vs. low probability p = 0.1170.
4. Discussion
Individual outcome variables represent the conventional tools for evaluating healthcare quality. However, TO was recently introduced as a composite measure to capture the multidimensional aspect of the care pathway and is progressively spreading and gaining importance in various surgical fields. For example, in hepato-pancreato-biliary (HPB) surgery, given the complex procedures and patients involved, TO development is considered of primary importance, as recently demonstrated by Pretzsch et al., who systematically reviewed 30 papers on this topic [20].
One of the main issues with the TO definition is the item selection. The ones we used in our study are based on the choice made by Serra et al. [12] in their similar analysis of percutaneous RFA and recall the ones formerly suggested by Merath et al. [21]. The limit of this choice is the need for a broad consensus for the definition of these criteria, which, based on the opinion of a small group of experts, are at increased risk of individual bias. Nevertheless, items were chosen based on what is commonly considered a surrogate of safety (i.e., postoperative complications, LOS, and the need for readmission) and efficacy (i.e., response to treatment) so that a consensus could be expected even in the absence of a rigorous methodology.
While for ablation therapy, an international agreement about TO definition criteria needs to be improved, advances have been recently made in the field of LR. Görcec et al. [10,11] made a cohesive effort to provide an international expert consensus-based definition of TO in liver surgery (TOLS). A panel of 44 expert surgeons, through a modified 4-round Delphi process, defined TOLS as the absence of intraoperative grade ≥ 2 incidents (described according to the Oslo classification [22]), postoperative bile leak of grade B or C (according to the severity grading of the International Study Group of Liver Surgery [23]), postoperative liver failure grade B or C (according to the severity grading of the International Study Group of Liver Surgery [24]), major postoperative complications within 90 days (Clavien–Dindo grade III or higher [25]), readmission within 90 days after discharge due to surgery related major complications (Clavien–Dindo Grade III or higher), in-hospital or 90-day mortality and the presence of R0 resection margin (i.e., 1 mm or more tumor-free margin).
One of the main differences between the TO items used in the current study and the ones established by Görcec et al. is the length of hospital stay as a parameter of evaluation. Although a consensus about LOS duration could not be reached in an international setting, the assessment of this aspect was considered significant by Görcec et al., so they suggested the development of an extended definition of TOLS including LOS (TOLS+) to be used on a national level. Another difference between the current study’s TO items and internationally established ones is how complications, readmissions, and mortality were evaluated at 30 days and 90 days, respectively. A more extended observation period was chosen in TOLS based on studies proving that shorter periods were inadequate for evaluation due to their incomplete representativeness [26,27]. However, the magnitude of MWA is undoubtedly minor compared to LR and, consequently, its short-term effect on patient morbidity; hence, a shorter observation period seems justifiable.
In addition to the high attention reserved for TO in HPB surgery, it was still missing in this particular field of liver surgery. To our knowledge, this is the first study on the TO of laparoscopic MWA for HCC. Our choice to base the current analysis on a comparison with the one published by Serra et al. [12] was due to the treatment technique considered. Since that was the first and only study developing a TO in the field of ablative therapy for HCC, we decided to use the same TO items, thus obtaining comparable results.
TO achievement rate was as good as 64.7%. Indeed, the TO achievement rate in general HPB surgery ranged between 15.8% and 69.1% [20]. On the other hand, Serra et al. reported 50.3% TO achievement, with CR of the target lesion being the limiting factor. Concerning the laparoscopic procedure, quite the opposite, CR was the most frequently achieved item while TO achievement was limited by the onset of complications, probably reflecting a worse hepatic function in this population (26% Child B patients in the current study vs. 16.2% in Serra et al.). These results reinforce our previous findings showing the superiority of laparoscopic MWA over laparoscopic RFA [14] in terms of recurrence profile, most likely due to the already demonstrated technical advantages of MWA. In particular, microwave induces tumor necrosis within a shorter period of ablation, does not result in tissue desiccation or charring, achieves a more significant zone of intra-tumoral thermal injury, and has an attenuated heat sink effect [28,29]. Those factors contributed to the current popularity of percutaneous MWA. Notably, even if a slight difference in median overall population survival was observed (i.e., 60.6 months in the paper by Serra et al. and 51.3 months in the current study), when considering only the TO achieving population, median survivals were comparable, respectively, 63.5 months for percutaneous RFA and 62.2 months for laparoscopic MWA.
These findings prompt the development of further studies that could demonstrate the non-inferiority of laparoscopic procedure, especially in the current era of therapeutic hierarchy for HCC treatment allocation [30,31], since it has already been shown that laparoscopic technique can overcome many limitations of percutaneous one (i.e., critical locations, proximity to other organs, severe coagulopathy, ascites, US visualization issues) [13,32,33,34]. As previously observed, indeed, the use of this surgical approach, also in comparison with other techniques such as transcatheter arterial chemoembolization (TACE) and liver transplantation, even if not strictly established and recommended by guidelines, could be justifiable in terms of results and survival, widening the audience of patients who can undergo potentially curative treatment [35,36].
Looking at risk stratification based on the parameters that impact the probability of TO achievement, our study showed concordance between a higher chance of TO achievement and better long-term results in terms of OS.
Serra et al. [12] found that moderate comorbidities, ECOG PS 1, and tumor burden (>2 nodules and nodules > 3 cm) had a negative impact on TO. We partially confirmed the previous findings: our study showed that age ≥ 70 years, MELD ≥ 15, Child B, and three nodules were associated with decreased probability of TO achievement.
Remarkably, all the characteristics proposed so far are evaluable in pre-operative settings, suggesting the development of tools for the pre-operative evaluation of the best treatment allocation for the patients based on their characteristics. Considering the previously described results, we can see the ideal candidate for MWA: relatively young, with preserved liver function and few HCC nodules. Furthermore, those patients have a higher probability of TO achievement and long-term survival. Notably, five years OS in our cohort of patients who did not achieve TO and who had a low likelihood of TO achievement was 40.3% and 34.7%, respectively, which are not poor results considering the characteristics of those patients (i.e., more frequently old, high MELD, Child B, multinodular). Indeed, TO is not a parameter to exclude patients from treatment when only a few therapeutic alternatives are available with poor outcomes (most likely, TACE). Consequently, tools derived from the TO analysis can help clinicians to allocate each patient to the best treatment based on the expected outcome, as dictated by therapeutic hierarchy, in the context of a multiparametric and multidisciplinary approach.
The present study has several limitations. First, it includes data from a single center activity; additionally, although prospectively collected, these data were retrospectively analyzed. Nonetheless, the definition of TO items for liver ablation procedure cannot be set only by these sparse experiences, and a comprehensive agreement is desirable. Hence, we advocate for further consensus by experts in the field and more robust evidence from multicentric studies. Once a widely accepted instrument is obtained, it will be helpful and informative for comparing the results obtained by different centers.
5. Conclusions
In conclusion, with the present study, we investigate the first TO for laparoscopic MWA for HCC based on a single institution experience, encouraging further broader consensus on its definition and, on its basis, on the development of clinically relevant tools for the management of treatment allocation.
Author Contributions
Conceptualization, J.L. and S.C.; methodology, A.V., J.L., S.C. and I.B.; software, I.B.; formal analysis, I.B.; investigation, J.L. and S.C.; data curation, E.G., F.D., G.G., D.B., F.E.D., R.B., A.B., A.M., S.L., M.B. (Marco Brolese) and M.B. (Mattia Ballo); writing—original draft preparation, J.L. and S.C.; writing—review and editing, A.V. and U.C.; supervision, A.V. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the ethical guidelines of the 1975 Declaration of Helsinki. Ethical review and approval were waived for this study since, according to Italian laws, no specific patient approval is needed for any retrospective analysis; however, patients provided written informed consent for every diagnostic and therapeutic procedure (laparoscopic microwave ablation included).
Informed Consent Statement
Specific patient consent to this study was waived since, according to Italian laws, no specific patient approval is needed for any retrospective analysis; however, patients provided written informed consent for every diagnostic and therapeutic procedure (laparoscopic microwave ablation included).
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy restrictions according to Italian law.
Conflicts of Interest
The authors declare no conflict of interest.
References
- van Roessel, S.; Mackay, T.M.; van Dieren, S.; van der Schelling, G.P.; Nieuwenhuijs, V.B.; Bosscha, K.; van der Harst, E.; van Dam, R.M.; Liem, M.S.L.; Festen, S.; et al. Textbook Outcome: Nationwide Analysis of a Novel Quality Measure in Pancreatic Surgery. Ann. Surg. 2020, 271, 155–162. [Google Scholar] [CrossRef]
- van Der Heide, M.F.; de Jel, D.V.; Hoeijmakers, F.; Hoebers, F.J.; de Boer, J.P.; Hamming-Vrieze, O.; Wouters, M.W.; Smeele, L.E. Defining High-Quality Integrated Head and Neck Cancer Care Through a Composite Outcome Measure: Textbook Outcome. Laryngoscope 2022, 132, 78–87. [Google Scholar] [CrossRef] [PubMed]
- Wiseman, J.T.; Abdel-Misih, S.; Beal, E.W.; Zaidi, M.Y.; Staley, C.A.; Grotz, T.; Leiting, J.; Fournier, K.; Lee, A.J.; Dineen, S.; et al. A multi-institutional analysis of Textbook Outcomes among patients undergoing cytoreductive surgery for peritoneal surface malignancies. Surg. Oncol. 2021, 37, 101492. [Google Scholar] [CrossRef]
- Kulshrestha, S.; Vigneswaran, W.T.; Pawlik, T.M.; Baker, M.S.; Luchette, F.A.; Raad, W.; Abdelsattar, Z.M.; Freeman, R.K.; Grenda, T.; Lubawski, J. Assessment of Textbook Outcome After Surgery for Stage I/II Non-small Cell Lung Cancer. In Seminars in Thoracic and Cardiovascular Surgery; WB Saunders: Philadelphia, PA, USA, 2021; Volume 34, pp. 1351–1359. [Google Scholar] [CrossRef]
- Berge, M.G.T.; Beck, N.; Steup, W.H.; Verhagen, A.F.; Van Brakel, T.J.; Schreurs, W.H.; Wouters, M.W.; the Dutch Lung Cancer Audit for Surgery Group. Textbook outcome as a composite outcome measure in non-small-cell lung cancer surgery. Eur. J. Cardio-Thorac. Surg. Off. J. Eur. Assoc. Cardio-Thorac. Surg. 2021, 59, 92–99. [Google Scholar] [CrossRef]
- Halpern, S.E.; Moris, D.; Gloria, J.N.; Shaw, B.I.; Haney, J.C.; Klapper, J.A.; Barbas, A.S.; Hartwig, M.G. Textbook Outcome: Definition and Analysis of a Novel Quality Measure in Lung Transplantation. Ann. Surg. 2021; Publish Ahead of Print. [Google Scholar] [CrossRef]
- Halpern, S.E.; Moris, D.; Shaw, B.I.; Kesseli, S.J.; Samoylova, M.L.; Manook, M.; Schmitz, R.; Collins, B.H.; Sanoff, S.L.; Ravindra, K.V.; et al. Definition and Analysis of Textbook Outcome: A Novel Quality Measure in Kidney Transplantation. World J. Surg. 2021, 45, 1504–1513. [Google Scholar] [CrossRef] [PubMed]
- Lim, C.; Llado, L.; Salloum, C.; Ramos, E.; Lopez-Dominguez, J.; Cachero, A.; Fabregat, J.; Azoulay, D. Textbook Outcome Following Liver Transplantation. World J. Surg. 2021, 45, 3414–3423. [Google Scholar] [CrossRef]
- Moris, D.; Shaw, B.I.; Gloria, J.; Kesseli, S.J.; Samoylova, M.L.; Schmitz, R.; Manook, M.; McElroy, L.M.; Patel, Y.; Berg, C.L.; et al. Textbook Outcomes in Liver Transplantation. World J. Surg. 2020, 44, 3470–3477. [Google Scholar] [CrossRef]
- Görgec, B.; Cacciaguerra, A.B.; Pawlik, T.M.; Aldrighetti, L.A.; Alseidi, A.A.; Cillo, U.; Kokudo, N.; Geller, D.A.; Wakabayashi, G.; Asbun, H.J.; et al. An International Expert Delphi Consensus on Defining Textbook Outcome in Liver Surgery (TOLS). Ann. Surg. 2022; Publish Ahead of Print. [Google Scholar] [CrossRef]
- Görgec, B.; Cacciaguerra, A.B.; Lanari, J.; Russolillo, N.; Cipriani, F.; Aghayan, D.; Zimmitti, G.; Efanov, M.; Alseidi, A.; Mocchegiani, F.; et al. Assessment of Textbook Outcome in Laparoscopic and Open Liver Surgery. JAMA Surg. 2021, 156, e212064. [Google Scholar] [CrossRef]
- Serra, C.; Cossiga, V.; Serenari, M.; Felicani, C.; Mazzotta, E.; Pinato, D.J.; Cescon, M.; Ercolani, G.; Cucchetti, A. Safety and efficacy of percutaneous radiofrequency ablation for hepatocellular carcinoma: A textbook outcome analysis. HPB 2022, 24, 664–671. [Google Scholar] [CrossRef] [PubMed]
- Cillo, U.; Bertacco, A.; Fasolo, E.; Carandina, R.; Vitale, A.; Zanus, G.; Gringeri, E.; D’Amico, F.; Bassi, D.; Neri, D.; et al. Videolaparoscopic microwave ablation in patients with HCC at a European high-volume center: Results of 815 procedures. J. Surg. Oncol. 2019, 120, 956–965. [Google Scholar] [CrossRef] [PubMed]
- Cillo, U.; Noaro, G.; Vitale, A.; Neri, D.; D’Amico, F.; Gringeri, E.; Farinati, F.; Vincenzi, V.; Vigo, M.; Zanus, G.; et al. Laparoscopic microwave ablation in patients with hepatocellular carcinoma: A prospective cohort study. HPB 2014, 16, 979–986. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, A.R.; Garcia, A.R.; Pereira, T.C.; Macedo, F.; Soares, R.F.; Pereira, K.; Serra, T.; Khouri, L.; Ribeiro, J.; Teixeira, M.M. ACE-27 as a prognostic tool of severe acute toxicities in patients with head and neck cancer treated with chemoradiotherapy: A real-world, prospective, observational study. Support Care Cancer Off J. Multinatl. Assoc. Support Care Cancer 2021, 29, 1863–1871. [Google Scholar] [CrossRef] [PubMed]
- Balzan, S.; Belghiti, J.; Farges, O.; Ogata, S.; Sauvanet, A.; Delefosse, D.; Durand, F. The “50-50 criteria” on postoperative day 5: An accurate predictor of liver failure and death after hepatectomy. Ann Surg. 2005, 242, 824–828, discussion 828–829. [Google Scholar] [CrossRef]
- Dindo, D.; Demartines, N.; Clavien, P.A. Classification of Surgical Complications: A New Proposal with Evaluation in a Cohort of 6336 Patients and Results of a Survey. Ann Surg. 2004, 240, 205–213. [Google Scholar] [CrossRef]
- AISF; AIOM; IT-IHPBA; SIC; SIRM; SITO. Raccomandazioni Multisocietarie Italiane (Aisf, Aiom, It-Ihpba, Sic, Sirm, Sito) Per La Gestione Clinica Integrata Del Paziente Con Epatocarcinoma. J. Hepatol. 2018, 69, 182–236. [Google Scholar]
- Galle, P.R.; Forner, A.; Llovet, J.M.; Mazzaferro, V.; Piscaglia, F.; Raoul, J.L.; Schirmacher, P.; Vilgrain, V. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J. Hepatol. 2018, 69, 182–236. [Google Scholar] [CrossRef]
- Pretzsch, E.; Koliogiannis, D.; D’Haese, J.G.; Ilmer, M.; Guba, M.O.; Angele, M.K.; Werner, J.; Niess, H. Textbook outcome in hepato-pancreato-biliary surgery: Systematic review. BJS Open 2022, 6, zrac149. [Google Scholar] [CrossRef] [PubMed]
- Merath, K.; Chen, Q.; Bagante, F.; Beal, E.; Akgul, O.; Dillhoff, M.; Cloyd, J.M.; Pawlik, T.M. Textbook Outcomes Among Medicare Patients Undergoing Hepatopancreatic Surgery. Ann. Surg. 2020, 271, 1116–1123. [Google Scholar] [CrossRef]
- Kazaryan, A.M.; Røsok, B.I.; Edwin, B. Morbidity assessment in surgery: Refinement proposal based on a concept of perioperative adverse events. ISRN Surg. 2013, 2013, 625093. [Google Scholar] [CrossRef]
- Koch, M.; Garden, O.J.; Padbury, R.; Rahbari, N.N.; Adam, R.; Capussotti, L.; Fan, S.T.; Yokoyama, Y.; Crawford, M.; Makuuchi, M.; et al. Bile leakage after hepatobiliary and pancreatic surgery: A definition and grading of severity by the International Study Group of Liver Surgery. Surgery 2011, 149, 680–688. [Google Scholar] [CrossRef]
- Rahbari, N.N.; Garden, O.J.; Padbury, R.; Brooke-Smith, M.; Crawford, M.; Adam, R.; Koch, M.; Makuuchi, M.; Dematteo, R.P.; Christophi, C.; et al. Posthepatectomy liver failure: A definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery 2011, 149, 713–724. [Google Scholar] [CrossRef]
- Clavien, P.A.; Barkun, J.; de Oliveira, M.L.; Vauthey, J.N.; Dindo, D.; Schulick, R.D.; de Santibañes, E.; Pekolj, J.; Slankamenac, K.; Bassi, C.; et al. The Clavien-Dindo classification of surgical complications: Five-year experience. Ann. Surg. 2009, 250, 187–196. [Google Scholar] [CrossRef]
- Mayo, S.C.; Shore, A.D.; Nathan, H.; Edil, B.H.; Hirose, K.; Anders, R.A.; Wolfgang, C.L.; Schulick, R.D.; Choti, M.A.; Pawlik, T.M. Refining the definition of perioperative mortality following hepatectomy using death within 90 days as the standard criterion. HPB 2011, 13, 473–482. [Google Scholar] [CrossRef]
- Mise, Y.; Vauthey, J.-N.; Zimmitti, G.; Parker, N.H.; Conrad, C.; Aloia, T.A.; Lee, J.E.; Fleming, J.B.; Katz, M.H.G. Ninety-day Postoperative Mortality Is a Legitimate Measure of Hepatopancreatobiliary Surgical Quality. Ann. Surg. 2015, 262, 1071–1078. [Google Scholar] [CrossRef]
- Boutros, C.; Somasundar, P.; Garrean, S.; Saied, A.; Espat, N.J. Microwave coagulation therapy for hepatic tumors: Review of the literature and critical analysis. Surg. Oncol. 2010, 19, e22–e32. [Google Scholar] [CrossRef]
- Salati, U.; Barry, A.; Chou, F.Y.; Ma, R.; Liu, D.M. State of the ablation nation: A review of ablative therapies for cure in the treatment of hepatocellular carcinoma. Future Oncol. Lond. Engl. 2017, 13, 1437–1448. [Google Scholar] [CrossRef]
- Vitale, A.; Trevisani, F.; Farinati, F.; Cillo, U. Treatment of Hepatocellular Carcinoma in the Precision Medicine Era: From Treatment Stage Migration to Therapeutic Hierarchy. Hepatology 2020, 72, 2206–2218. [Google Scholar] [CrossRef] [PubMed]
- Vitale, A.; Farinati, F.; Pawlik, T.M.; Frigo, A.C.; Giannini, E.G.; Napoli, L.; Ciccarese, F.; Rapaccini, G.L.; Di Marco, M.; Caturelli, E.; et al. The concept of therapeutic hierarchy for patients with hepatocellular carcinoma: A multicenter cohort study. Liver Int. 2019, 39, 1478–1489. [Google Scholar] [CrossRef]
- Santambrogio, R.; Barabino, M.; D’Alessandro, V.; Galfrascoli, E.; Zappa, M.A.; Piccolo, G.; Zuin, M.; Opocher, E. Laparoscopic thermoablation for hepatocellular carcinoma in patients with liver cirrhosis: An effective procedure for tricky tumors. Med. Oncol. Northwood Lond. Engl. 2020, 37, 32. [Google Scholar] [CrossRef] [PubMed]
- Santambrogio, R.; Barabino, M.; Bruno, S.; Costa, M.; Ceretti, A.P.; Angiolini, M.R.; Zuin, M.; Meloni, M.F.; Opocher, E. Long-term outcome of laparoscopic ablation therapies for unresectable hepatocellular carcinoma: A single European center experience of 426 patients. Surg. Endosc. 2016, 30, 2103–2113. [Google Scholar] [CrossRef] [PubMed]
- de la Serna, S.; Vilana, R.; Sánchez-Cabús, S.; Calatayud, D.; Ferrer, J.; Molina, V.; Fondevila, C.; Bruix, J.; Fuster, J.; García-Valdecasas, J.-C. Results of laparoscopic radiofrequency ablation for HCC. Could the location of the tumor influence a complete response to treatment? A single European center experience. HPB 2015, 17, 387–393. [Google Scholar] [CrossRef] [PubMed]
- Farinati, F.; Vanin, V.; Giacomin, A.; Pozzan, C.; Cillo, U.; Vitale, A.; Di Nolfo, A.M.; Del Poggio, P.; Benvegnu’, L.; Rapaccini, G.; et al. BCLC stage B hepatocellular carcinoma and transcatheter arterial chemoembolization: A 20-year survey by the Italian Liver Cancer group. Liver Int. 2015, 35, 223–231. [Google Scholar] [CrossRef] [PubMed]
- Cillo, U.; Vitale, A.; Volk, M.L.; Frigo, A.C.; Grigoletto, F.; Brolese, A.; Zanus, G.; D’Amico, F.; Farinati, F.; Burra, P.; et al. The survival benefit of liver transplantation in hepatocellular carcinoma patients. Dig. Liver Dis. 2010, 42, 642–649. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).