Simple Summary
Breast cancer is a major health concern as it remains the deadliest for women worldwide. As for other cancer types, the immune system is determinant for how the body fights the tumor and responds to therapy. Better medical care and therapy assignment can thus be obtained by a deeper understanding of the immune state of breast cancer patients and how it changes with disease and treatment. Such information becomes more relevant and accessible if collected easily from a blood test. This review summarizes current knowledge on breast cancer patients’ immune profile obtained from peripheral blood and serves as a starting point for further investigation. Finally, we discuss the latest advances and current challenges in experimental models to study the interactions between human cancer and immune cells, with the intent of bridging the gap between patient immune profiling and functional and therapeutic significance.
Abstract
Breast cancer is the deadliest female malignancy worldwide and, while much is known about phenotype and function of infiltrating immune cells, the same attention has not been paid to the peripheral immune compartment of breast cancer patients. To obtain faster, cheaper, and more precise monitoring of patients’ status, it is crucial to define and analyze circulating immune profiles. This review compiles and summarizes the disperse knowledge on the peripheral immune profile of breast cancer patients, how it departs from healthy individuals and how it changes with disease progression. We propose this data to be used as a starting point for validation of clinically relevant biomarkers of disease progression and therapy response, which warrants more thorough investigation in patient cohorts of specific breast cancer subtypes. Relevant clinical findings may also be explored experimentally using advanced 3D cellular models of human cancer–immune system interactions, which are under intensive development. We review the latest findings and discuss the strengths and limitations of such models, as well as the future perspectives. Together, the scientific advancement of peripheral biomarker discovery and cancer–immune crosstalk in breast cancer will be instrumental to uncover molecular mechanisms and putative biomarkers and drug targets in an all-human setting.
Keywords:
breast cancer; biomarker; blood; T cell; NK cell; macrophage; MDSC; 3D cell models; immunosuppression; patient data 1. Introduction
Breast cancer remains the leading cause of cancer-related deaths for women worldwide. In 2018, 2.1 million women were diagnosed with breast cancer and 626,679 died from it [1]. Breast cancer is curable in approximately 70–80% of patients with early-stage disease [2], but, despite new available treatments, advanced/metastatic breast cancer remains an incurable disease with a median overall survival of about three years and a five-year survival rate of around 25% [3].
Breast cancer is a heterogeneous disease, which can be classified according to histology and molecular characteristics. The most common invasive histological subtypes are ductal carcinoma, currently named as “no special type”, and lobular carcinoma. Based on gene expression signature (PAM50), breast tumors can also be divided in intrinsic subtypes: Luminal A, Luminal B, HER2-enriched, Normal-like, and Basal-like [4]. Both histological and molecular features have an impact on prognosis and treatment. In daily clinical practice, surrogate intrinsic subtypes are used. This classification takes in account the histology, the receptor expression, and the proliferation index. Thus, tumors can be classified as: Luminal A-like (high estrogen receptor (ER) and progesterone receptor (PR) expression, HER2 negative, low grade, and low Ki67 index), Luminal B-like HER2 negative (lower expression of ER and PR, HER2 negative, higher grade, and high Ki67 index), Luminal B-like HER2 positive (lower expression of ER and PR, HER2 positive, higher grade, and high Ki67 index), Non-luminal HER2-enriched (ER and PR negative, HER2 positive, high grade, and high Ki67 index), and Triple-negative (ER, PR and HER2 negative, high grade, and high Ki67 index) [2].
In the early setting, with curative intent, Luminal A-like tumors are usually treated with surgery followed by radiotherapy and endocrine therapy. Chemotherapy is usually less used, except for large tumors or nodal involvement. Luminal B-like tumors can be treated with (neo)adjuvant chemotherapy followed by surgery, radiotherapy, and endocrine therapy. HER2 positive tumors are treated with (neo)adjuvant chemotherapy combined with anti-HER2 agents followed by surgery and radiotherapy. Early triple negative tumors are treated with (neo)adjuvant chemotherapy followed by surgery and radiotherapy [5]. In the advanced setting, endocrine therapy and CDK4/6 inhibitors play a crucial role as first lines of treatment of Luminal-like tumors and anti-HER2 agents are central in the treatment of HER2 positive tumors, while immune checkpoint inhibitors combined with chemotherapy can be used in triple negative tumors [6].
The clinical outcome of breast cancer patients is not only dependent on the therapeutic action of drug treatments. The immune system is known to play a major role in all stages of cancer development, initially in the elimination of the first malignant cells and then progressively becoming subverted by the tumor to promote cancer growth and metastization [7]. In these interactions, cells from both the lymphoid (T cells, B cells, and natural killer (NK) cells) and the myeloid (monocytes/macrophages, and dendritic cells (DC), neutrophils, myeloid-derived suppressor cells (MDSC)) lineages are heavily implicated. T cells are a very heterogeneous population: on one hand, CD8+, CD4+, and γδT cells are directly involved in the specific killing of tumor cells, directed by the recognition of tumor antigens. On the other hand, regulatory T cells (TRegs) promote the establishment of a pro-tumoral environment [7,8,9]. NK cells are also able to induce tumor cell killing based on the detection of activating danger signals on the tumor cell surface, while also secreting pro-inflammatory cytokines [7,8,9]. B cells are of major importance for the establishment of anti-tumoral immunity due to their role in antibody production and in the formation of tertiary lymphoid structures in the periphery of the primary tumor, where they also exert the function of presenting antigen to T cells, activating them [7,8,9]. This role of antigen presentation is also performed by dendritic cells, which hold the unique ability to cross-present tumor antigens to CD8+ T cells, promoting direct cell killing [7,8,9]. Monocytes and macrophages hold a dual role in cancer progression given their functional plasticity and the ability to become either tumor-promoting or anti-tumorigenic. Depending on the microenvironmental and systemic cues, macrophages may synergize with CD8+ and NK cell action by killing tumor cells and secreting pro-inflammatory cytokines; more often, they acquire a pro-tumoral phenotype and promote a strong immunosuppressive immune milieu, which leads to cancer growth and metastization [7,8,9]. Neutrophils may also be polarized into a tumor-promoting phenotype, and are currently regarded as being directly involved in metastasis formation [7,8,9]. Other suppressive cells in the cancer context include the MDSC, a group of immature myeloid cells of the monocytic and granulocytic lineages with the capacity to subvert the anti-tumor function of other immune populations [7].
This influence of the immune system upon cancer development has been studied for a long time. In the mid-20th century, Burnet and Thomas postulated the theory of immunosurveillance based on studies using tumor transplantation models [10]. Although the original formulation raised controversy, it inspired numerous studies along the following decades that contributed to a better understanding of the immune system as a key player in tumor development. Dunn et al., 2002 proposed the concept of immunoediting, based on three “E”s—elimination, equilibrium, and escape—and recognized both positive and negative effects of the host–tumor interaction [11]. Later, the involvement of the immune system in the treatment of cancer was also investigated, after several studies showed that conventional chemotherapy effects are also mediated by immunogenic actions [12]. This antitumor immune activation was identified as one of the mechanisms responsible for metronomic (low dose continuous) chemotherapy efficacy [13], with recent reports indicating that the immunogenic cell death induced by anthracycline or taxane treatment also subverts the immunosuppressive environment at the tumor site [14]. Regarding targeted agents, the anti-HER2 antibody trastuzumab may also be considered an immune modulatory agent, due to its ability to induce antibody-dependent cell-mediated cytotoxicity (ADCC) and influence the activity of NK and T cells, macrophages, and dendritic cells [15,16]. Similarly, the two other approved HER2-targeting agents pertuzumab and T-DM1 were also shown to promote immune cell engagement via ADCC [17,18].
The application of immunotherapies to breast cancer became more prominent in recent years, following the trend of other malignancies [19]. In this regard, and considering the currently available immune-targeted drugs, checkpoint inhibitors have already showed benefit in the triple negative breast cancer (TNBC) context. In the Impassion 130 trial, the anti-PD-L1 antibody atezolizumab was used in combination with nab-paclitaxel to treat patients with PD-L1+ advanced TNBC, resulting in a significant clinical benefit not only for progression-free survival (PFS) but also for overall survival (OS) [20]. More recently, data from early phase studies demonstrated that the association of pembrolizumab with neoadjuvant chemotherapy for high-risk early TNBC patients was feasible and had a promising antitumor activity. An exploratory analysis showed a correlation between the occurrence of pathological complete response (pCR) and the expression of tumor PD-L1 and the infiltration by tumor infiltrating lymphocytes (TILs) [21]. In fact, the role of TILs as independent predictors of response to neoadjuvant chemotherapy has been previously validated in patients [22]. In parallel, other trials are ongoing regarding the use of anti-CTLA-4 agents and regimens combining immune checkpoint blockade (ICB) with several targeted therapies [19,23].
Concurrent with the evidence that immunotherapies are beneficial in breast cancer treatment, years of studies with thousands of patients have consistently showed that for early stage HER2+ and TNBC cases the presence and increased numbers of TIL are associated with better disease prognosis and response to therapy [24]. For this reason, it has been proposed to incorporate TIL analysis as predictive and prognostic biomarkers in clinical practice. However, as TIL are by definition contained within the tumor mass, analysis is always dependent on invasive biopsies or surgical resection. Therefore, TIL evaluation is not possible for every patient and it becomes difficult to evaluate patients’ progression at frequent intervals. On the other hand, the use of peripheral blood immune biomarkers would be especially useful to evaluate disease progression and treatment response, allowing for faster, cheaper, and more precise monitoring of patients’ status—and, ideally, for tailoring treatments. Assessing features of systemic immunity would also prove useful in metastatic disease as it would reflect not only events of the primary tumor but also of distant metastasis. Several studies failed in the identification of predictive biomarkers, even in tumor types where immunotherapy had a huge impact [25]. Thus, the area of immune blood biomarkers in solid tumor patients remains underdeveloped and so far there is no validated predictive biomarker for breast cancer. In fact, concise information on the peripheral immune status of breast cancer patients of all stages is still dispersed and often neglected.
This review aims to cover the most relevant immune parameters and biomarkers with current potential to be used as predictive and prognostic tools for breast cancer assessment in the clinic, as well as to further understand the immune mechanisms connected with tumor progression or regression. Finally, we discuss the existing cellular models applicable to explore the mechanisms behind these relationships of peripheral immune state and disease progression, their strengths, and future developments.
2. Systemic Immune Status
2.1. Peripheral Lymphocyte Count
The earliest [26] and easiest way to assess patients’ immune capacity has been through the absolute count of peripheral blood lymphocytes (PBL) or mononuclear cells (PBMC, which encompass all white blood cells minus granulocytes). In this regard, research across all breast cancer subtypes and disease stages has consistently showed that higher lymphocyte count at baseline, prior to therapeutic intervention, is an indicator of better prognosis (Table 1) [26,27,28,29,30,31]. In primary breast cancer patients undergoing neoadjuvant chemotherapy (NAC), lower absolute lymphocyte numbers were predictive of a shorter disease-free survival (DFS) and overall survival [27] and, conversely, higher lymphocyte counts were associated with a higher rate of pCR after NAC and tumor resection [28]. This trend was also observed in a cohort of elderly (over 65 years old) patients, where higher lymphocyte counts were positively associated with a higher three-year DFS both in univariate and multivariate analysis [29]. Additionally, in a subtype-restricted analysis, TNBC [31] and hormone receptor positive (HR+) [30] patients with baseline lymphocyte counts above a cut-off value were found to have significantly longer OS and DFS. On the other hand, no significant associations were found between lymphocyte number and disease prognosis in HER2+ breast cancer patients [30], even though HER2-overexpressing disease may be associated with a higher baseline PBL count [27]. A positive response to NAC was also found more frequently among patients who maintained a consistent level of PBL after the first cycle of treatment [27], already suggesting the potential of chemotherapy regimens to influence the anti-tumor immune response. It is worth noticing, however, that such promising results were observed in cohorts of primary breast cancer patients only, suggesting that metastatic disease requires additional readouts.

Table 1.
Clinical findings associated with peripheral lymphocyte counts.
In recent years, other indexes combining counts of different immune cells with inflammatory potential have gained popularity in clinical oncology as indicators of the systemic immune status. Parameters such as the lymphocyte-to-monocyte (LMR), neutrophil-to-lymphocyte (NLR), and platelet-to-lymphocyte (PLR) ratios, among others, were shown to have a significant prognostic and predictive power in several solid tumors [40,41,42,43]. In breast cancer, NLR and LMR are highlighted in several studies as the indices displaying stronger correlation with disease prognosis (Table 1) [28,29,30,31,32,33,34,35,36,37,38]. In two distinct cohorts, Azab et al. categorized patients in four quartiles according to their baseline measures of NLR and observed a significant increase in short- and long-term mortality rate for patients in the highest NLR quartile [33,34], which corresponded to a 4 to 6 times higher probability of death at five years, depending on the cohort and comparing to the three lowest quartiles. In early-stage breast cancer patients undergoing NAC, NLR was also associated with prognosis. Patients presenting lower NLR values displayed longer DFS and OS [29,32], and had a higher probability of achieving a pCR after NAC [28,29,30]. This observation was especially marked for the TNBC subtype [29], in which low NLR values were associated with an average of 5.5 years longer OS; accordingly, higher NLR values were linked to higher mortality rates [35]. These results are not surprising considering that patients with elevated values of this index often present other indicators of worse prognosis such as higher levels of metastization, hormone receptor negativity, and HER2 positivity [35].
LMR evaluates the ratio between the absolute counts of lymphocytes and monocytes in circulation, and recent research has shown its potential as a prognostic guide in breast cancer [30,31,32,37,38]. Patients with a high LMR display longer DFS [30,32,37] and OS [30,32] than those with lower ratios, including cohorts of luminal [38] and triple-negative [31] breast cancer patients. Higher LMR values were also found more often in patients with less advanced tumor stages [31], hormone receptor positivity [37], and higher prevalence of CD8+ TIL in the tumor microenvironment (TME) [30], although other studies found these associations not significant [29,32]. This heterogeneity may be due to the lack of consensus in the cut-off values chosen for each index, which for LMR was found to range between 2.94 and 5.46 (almost a twofold difference) across studies. Of note, only one group was found to investigate the influence of different cut-off values on the final statistic [35].
The usefulness of the ratio of PLR is still a matter of debate, as literature is scarce and inconsistent (Table 1). While some authors claim there is no association between PLR and breast cancer prognosis [29,30], others present evidence for a significant capacity to predict patient’s survival [34,35,39]. In a group of over 700 breast cancer patients, high PLR was identified as an independent prognostic factor that predicted worse OS and the appearance of distant metastasis [39], with subtype-specific analysis revealing this association to be specific of Luminal B and Basal-like breast cancer. In fact, for the Luminal B subtype, PLR proved to be superior to age and T status in predicting cancer-specific survival. Similarly, patients in the highest PLR categories displayed larger tumors, higher NLR and metastasis rate and were more likely to be HER2+ [34,35]. Their mortality risk at five years was also significantly increased [35] and considered an independent predictive factor in a multivariate analysis, although with inferior capacity compared with NLR [34]. It is interesting to note that platelets seem to have a relevant role in cancer development, as they have been found to increase the local concentrations of VEGF, promoting angiogenesis, and to aggregate with tumor cells, improving their survival in the peripheral blood [34]. One of the reasons for the discrepancies reported may lie once again in the disparity of values chosen for the threshold of low vs. high PLR. In fact, when Koh et al. analyzed the sensitivity of their model to two already published cut-off values (185 [33,34] and 292 [39]), it became obvious that only one of them (185) returned a significant association in a multivariable analysis adjusted for confounders [35]. Given that each patient cohort is different, and that immune ratio cut-off values are often calculated based on receiver operator characteristic (ROC) curve analysis for distinct parameters (like DFS or OS), it is understandable that varying patient populations and prognosis indicators will result in distinct cut-off values. Therefore, it is vital to find a standardized range of acceptable threshold values to obtain more concise and comparable results that can be applied to clinical decision making.
Surprisingly, only one study was found to focus specifically on metastatic patients [36]. These appeared to follow a similar trend to non-metastatic cases, with low NLR and PLR and high LMR providing a survival advantage. Additionally, subtype stratification indicated high LMR as a positive prognostic factor for TNBC and HER2, with the latter benefiting also from a low PLR. In this study, no specific correlation was found between ER+ breast cancer prognosis and immune cell ratio indices.
The diversity of patient populations covered in the literature cited above—in terms of disease staging, subtype, treatment regimen, ethnicity, or sample size—is a favorable factor, increasing reliability of the results obtained. Nevertheless, more research is needed to validate the observations obtained from small cohorts, such as the HER2+ or metastatic breast cancer patients, which are usually much smaller than the others. It is also worth noting that most of these studies focus on disease prognosis as the main endpoint/readout, and that this may change throughout the duration of treatment and depending on the therapeutic regimen. It is then essential to complement these measures of prognosis with other readouts assessing response to therapy in the same or similar patient populations; this would facilitate the distinction of (potential) biomarkers that may interact with the treatment applied in each case.
Still, taking together these observations, there are already strong indicators that lymphocytes, monocytes, and neutrophils play a decisive role in shaping the fight against cancer at the organism level, as also highlighted recently in a review of the latest developments in the field [44].
2.2. Lymphocyte Function and Soluble Factors
The general immune state of breast cancer patients may also be gauged by the levels of immune modulatory factors found in plasma and by the functional state of immune cells per se. As reported for other cancer types [45,46,47], circulating immune cells of breast cancer patients display reduced expression of pro-inflammatory markers [48,49,50,51,52,53] and are less amenable to stimulation [49,54,55], when compared with healthy donors. This can be seen by the reduced secretion of typical inflammatory cytokines such as IL-6, IL-12, IL-2, IFN-γ, TNF-α, IL-8, GM-CSF, and IL-1β [48,49,50] and the increase in production of IL-4, IL-10, and PGE2 [48], which are commonly considered drivers of a tumor-promoting microenvironment [56,57,58]. Consistently, Elashi et al. found that patients’ baseline levels of checkpoints TIM-3, TIGIT, and PD-L1 were not only higher than in healthy donors but also than in the tumor site [51]. This apparent lack of pro-inflammatory reactivity, seen also after stimulation with phorbol myristate acetate (PMA) [49], may be explained by a general fragility of circulating immune cells, which appear to have a higher degree of membrane integrity loss than those of healthy donors—as seen by a higher level of spontaneous lactate dehydrogenase (LDH) release, which becomes more pronounced with disease progression [55].
However, it is interesting to note that metastatic disease seems to invert to some extent the tendency for less reactive circulating immune cells. It has been reported that in metastatic patients there was increased production of TNF-α and IL-1β [49] compared with early breast cancer patients, and upregulation of CD14 and CD40 [53], two receptors necessary for macrophage pro-inflammatory function and antigen presentation. This effect may be subtype-dependent though, as another study reports that metastatic HER2− patients exhibited reduced production of IL-2, IL-1β, IL-8, IL-6, and IL-10 compared with HER2+ cases [52]. A stage-dependent increase in the expression of the anti-inflammatory markers FOXP3 and PD-L1 was also found in one cohort of patients of all subtypes (predominantly Luminal and HER2+) [53]. The highest expression of PD-L1 and FOXP3 correlated with a higher production of IFN-γ and diminished secretion of TGF-β2, respectively.
Unfortunately, to date very few studies have investigated putative links between these markers of immune function and breast cancer prognosis or response to therapy. For metastatic patients, high levels of IL-6 may predict worse disease prognosis [59]. There is also evidence that after systemic therapy with taxane regimens there is an increased production of IL-2, IL-6, GM-CSF, and IFN-γ, while secretion of IL-1, TNF-α, and PGE2 declines [50]; however, it is still unknown whether this precludes an actual clinical benefit for the patient. For TNBC, Foulds et al. found a specific inflammation-related mRNA signature, consisting of high expression of CD163 (a scavenger receptor associated with M2 macrophage polarization [60]) and CXCR4 (a chemokine receptor involved in monocyte function and deployment to the tissue [61]) and low expression of THBS1 (an activator of the TGF-β pathway [62] and proposed breast cancer biomarker [63]), which correlated with improved relapse-free survival in a cohort of 186 patients [64].
3. The Lymphoid Lineage
At the interface of cancer development and immune response, lymphocytes have been the core of oncoimmunology research from its inception. The presence and phenotype of TIL are acknowledged as major influencers of disease progression or regression in solid tumors [24], with potent prognostic implications for several malignancies, especially in the case of the so called “hot tumors”. These tumor types are characterized by an increased rate of lymphocyte infiltration, which has been linked to greater mutational load and higher levels of genetic instability, known to lead to the generation of more neoantigens and consequent activation and recruitment of immune cells [23,25,65,66,67]. Traditionally, breast cancer was considered an instance of “cold tumor” given the generally low level of infiltration and its lower rate of somatic mutation compared with highly mutational cancers like non-small cell lung cancer or melanoma [23], where the application of immunotherapies has been a reality for several years [68]. However, reports from the last decade have shown that, when stratified by subtype, HER2+ and TNBC have sufficient genomic instability and proliferation rate to sustain lymphocyte infiltration, while HER2 itself becomes a TAA promoting immune activation [23,69,70]. Accordingly, the presence of elevated numbers of TIL in the tumor microenvironment is associated with better disease prognosis and predicts a positive response to chemotherapy in these subtypes, which are more likely to harbor TIL than Luminal A or B breast cancers [19,23,69,70]. The role of TIL in breast cancer progression and prognosis lies outside the scope of this work as it has been thoroughly discussed elsewhere [24]. Nonetheless, it demonstrates that T, B, and NK cell phenotype and function are fundamental indicators of how the immune system is fighting against cancer.
3.1. T Cells
The peripheral Treg population, associated with suppressive functions [46], was found to be expanded in breast cancer patients compared with healthy individuals [15,52,64,71,72,73,74] (Figure 1, left). It was also correlated with other indicators of poor prognosis, like tumor stage [71] and elevated levels of circulating tumor cells (CTC) [74] and MDSC [71]. In HER2+ patients, therapy regimens containing trastuzumab for primary and metastatic patients were found to reduce the numbers of Tregs [15,73], which rise again only in relapsing patients [73]. When Wang et al. compared the peripheral and intratumoral populations of Treg, they identified a subpopulation of circulating Tregs characterized as FOXP3hi/CD45 RA−, with suppressive phenotype. This population was remarkably similar to the tumor infiltrating counterpart, including overlapping clonal diversity. These data strongly suggest that this is the Treg population that infiltrates the TME [75]. Compared with other peripheral Treg subsets, this type II Treg population upregulated the immunosuppressive markers CD39, CTLA-4, TIGIT, and ICOS and responded better to TGF-β and IL-10, while the response to pro-inflammatory IL-4 and IFN-γ was hampered. This is also supported by the observation that type II Tregs were considerably expanded in breast cancer patients, compared with healthy women. Moreover, patients in which type II Tregs had a stronger suppressor phenotype (improved response to TGF-β and IL-10) displayed shorter relapse-free survival (RFS). In fact, in this cohort of 118 patients, type II Treg suppressive activity was considered a strong indicator of relapse independently of other clinical features, reflecting disease stage (with suppressive activity increasing during disease progression).
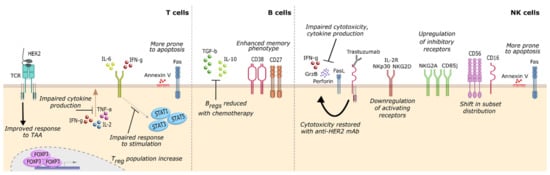
Figure 1.
Surface markers and cytokine response of lymphoid peripheral immune cell populations associated with breast cancer occurrence and/or progression. In the lymphoid lineage, T cells and NK cells acquire a stronger suppressive phenotype in breast cancer patients including diminished response to, and production of, pro-inflammatory cytokines, higher susceptibility to apoptosis and impaired cytotoxic response—although the latter may be reversed upon exposure to tumor-associated antigens (T cells, via binding of HER2 to the TCR) or anti-HER2 therapeutic antibodies (NK cells, via binding of trastuzumab to CD16). B cells were also found to respond to chemotherapy regimens by reducing the Breg population, thus promoting anti-tumor immune function. NK, natural killer cells; TAA, tumor-associated antigen; TCR, T cell receptor.
Regarding the effector CD8+ T cells, there seems to be an imbalance in breast cancer patients towards higher proportions of more differentiated subsets, with signs of activation and possibly exhaustion [76]. This includes the metastatic setting [76], where lower percentages of naïve CD8+ and higher percentages of more differentiated CD8+ confer clinical benefit after treatment with high-dose paclitaxel [77]. However, breast cancer subtype can be determinant of this shift in T cell differentiation, given that HER2− and hormone receptor-positive patients harbor a higher proportion of naïve and TCM (central memory subset) than more mature CD8+ T cell populations [52,78], while the opposite is seen in HER2+ patients [52]. Nevertheless, circulating T cells appear to be at an earlier maturation stage compared with TIL [76], which may be an advantage for the application of immune-based therapies that rely on re-education of T lymphocytes. The memory phenotype of T cells also appears to be temporarily magnified by systemic chemotherapy, with memory and naïve populations returning to baseline only several months after the end of treatment [79].
Overall, there is abundant evidence of functionally deficient T cells in breast cancer patients [48,71,74,80,81,82,83,84,85] (Figure 1, left). Compared with those of healthy individuals, these T lymphocytes display a significant reduction in the secretion of pro-inflammatory cytokines IL-2, IFN-γ, IL-21, TNF-α, and IL-4 [48,74,80,81], with impaired responses to proliferative signals [48,82,83] as well as to IL-6 [71,85], IL-17 [71], and IFN-α and -γ [84]. Concomitantly, defects in several signal transducer and activator of transcription (STAT) signalling pathways (namely, STAT1, 3 and 5) were observed [71,82,84,85], indicating that patient T cells are likely less able to respond to a plethora of immune modulatory soluble factors [86,87]. These findings may have clinical significance, as it has been reported that increased CTC, a known indicator of poor prognosis, is associated with lower levels of IFN-γ, IL-2, and TNF-α secreted by T cells [74,80]. Further, a combination of a low CTC count and a high proportion of IFN-γ secreting CD8+ T cells improves OS [74]. Other studies have also highlighted the relationship between impaired IL-6 signalling and a heightened relapse rate [85], identifying baseline T cell response to IL-6 as a predictor of RFS in breast cancer [71]. Mego et al. reported that low levels of CD4+, IL-2+, CD8+, IFN-γ+, and TNF-α+ T cells posed a significant negative impact in patient survival [74]. Once again, this data points to the relevance of an effective, pro-inflammatory T cell response for better disease management.
T cell function may also be evaluated by the quality and magnitude of response to tumor-associated antigens. This becomes especially useful in the case of HER2+ tumors since HER2 is a well-characterized TAA [88]. In this regard, although overall CD8+ and γδ T cell cytotoxicity was found to be inferior to that of healthy individuals [81,82,89], the specific response to TAA was heightened [90], especially in HER2+ cases [52,88]. This response was found to correlate with improved survival and earlier tumor stage [91,92,93] (Figure 1, left). Similarly, patients who displayed a more diverse T cell receptor (TCR) repertoire and were able to maintain that diversity during chemotherapy (when CD4+ populations usually decline [94,95] and CD8+ increase [79]), were more likely to evolve positively and to harbor HER2+ tumors [96]. Remarkably, Bailur et al. found a clear association between CD8+ T cell response to HER2 and low levels of circulating MDSC, which conferred these patients a 100% survival rate at five years [91,92]. The production of granzyme B is one of the factors affecting the lytic capacity of T cells [89]. This is a protein that induces apoptotic cell death in the target cell. In line with this, a specific mutated genotype of the GRZB gene which leads to inferior cytotoxic function (48 R/R, 88 A/A, and 245 H/H) was found to confer a 16-times higher probability of developing breast cancer than the wild-type [89], emerging as a potential genetic biomarker for cancer susceptibility.
There is also evidence that peripheral T cells of breast cancer patients are more susceptible to apoptosis, as indicated by the expressive proportion of Fas+ AnnexinV+ lymphocytes in circulation [84,97,98] (Figure 1, left); these cells are more often CD25− and occur in patients presenting a decrease in soluble Fas ligand (sFas-L) [97], suggesting that the pool of naïve and non-activated memory T cells is being selectively depleted by binding of sFas-L in circulation. T cell death may also be implicated in worse disease prognosis, as seen by the association between a higher number of CTC and elevated Fas+ T cells [97,98].
3.2. B Cells
The influence of B cells in the cancer promotion/regression axis is still largely understudied. B cells are antigen-presenting cells (APC), with the putative capacity to promote TAA-directed immune responses and the exclusive ability to produce antibodies, which may enhance the anti-tumor response [99]. However, most of the communication between B cells and the tumor contexture (not just locally but also systemically) remains unknown, such as: which factors and signalling pathways mediate the crosstalk between B cells and other immune effectors, how different stimuli may elicit a pro- or anti-inflammatory function in the TME, and the specific roles of each subpopulation (given that B cells exhibit high heterogeneity and plasticity), among others. Furthermore, it is essential to inquire about potential relationships between B cell response or other B cell-related biomarkers and disease prognosis that may be used to improve patients’ treatment in the clinical setting.
The available literature regarding circulating B cells in breast cancer patients is mostly recent and reports conflicting results on the proportion of B cells present in the peripheral blood [64,100,101,102]. While some authors claim that patients do not differ from healthy women in the number of circulating B cells [64,100], others present evidence that the amount of B cells is higher in breast cancer patients [101]. Additionally, the authors reported that increased circulating B cells raised the risk of developing breast cancer by 17% in otherwise healthy, pre-menopausal women [102]. The B cells of breast cancer patients were also found to be enriched for memory subsets [101] (Figure 1, middle), although this tendency was reversed after treatment with systemic chemotherapy [103]. On this note, both NAC and chemotherapy in the adjuvant setting were found to consistently deplete the pool of peripheral B cells [64,94,103,104,105]. The dynamics of depletion and repopulation were dependent on whether the patient received taxane-based therapy. Nonetheless, B cell numbers did not rise to their baseline level even nine months after treatment (contrary to other immune populations) [103]. In the metastatic setting, one cohort of 482 patients displayed a significant association between increased number of circulating CD19+ B cells and prolonged survival, although no connection was found between B cell counts and tumor subtype [106].
In recent years, a new subtype of B cells named B regulatory cells (Bregs) has been brought to attention due to its role in enhancing a pro-tumorigenic environment [107,108]. These cells are highly heterogeneous in surface marker expression and, in fact, may not even constitute one bona fide B cell lineage but rather a functional state [107,109]. However, they were found to have in common the secretion of IL-10 and TGF-β, which renders them able to convert conventional CD4+ T cells into Tregs, and thus subvert several immune effectors at the tumor site [110]. Knowing this, the finding that the population of circulating Bregs is reduced in breast cancer patients after systemic chemotherapy [103] (Figure 1, middle) may suggest that the post-chemotherapy period is a window of opportunity to introduce new immune-activating therapeutic options. This becomes especially relevant if we consider that tumor infiltrating B lymphocytes (B-TIL) have been positively associated with improved prognostic indices in TNBC [111] and highly proliferative breast carcinomas [112], indicating it may be possible to further amplify the beneficial anti-tumoral effects of this immune population [99].
3.3. NK Cells
Natural killer cells were first identified for their role in cancer immunosurveillance given their innate ability to selectively kill transformed cells without the need for previous cellular activation (contrasting with the other major killer of the lymphoid lineage, CD8+ CTLs) [113]. Unsurprisingly, NK cell number and phenotype have long been investigated for their potential use as cancer progression biomarkers and, more recently, strategies for enhancing NK function to improve anti-cancer therapies have become a new research trend in oncoimmunology [113,114,115]. As seen in other solid tumors [113], breast cancer patients typically display impaired NK cell function, albeit to varying degrees [50,54,55,64,81,84,116,117,118,119,120] (Figure 1, right). Although the proportion of circulating NK cells appears in the healthy range [15,64,119,120,121,122], they display a marked reduction in their ability to kill target tumor cells (either by direct cytotoxicity or by CD16-mediated ADCC) and to secrete pro-inflammatory cytokines [50,54,55,116,117,118,119,120]. A clear impairment in their sensitivity to stimulation [54] can also be seen by the decreased response to IFN type I [81,84] and downregulation of IL-2R [120] compared with healthy NK. Moreover, this diminished cytotoxic capacity was associated with indicators of cell death, such as AnnexinV positivity [120] and LDH leakage [55], and shown to deteriorate further with disease progression [54,55,123]. These data indicate that peripheral NK cells are being heavily influenced by the suppressive features of breast cancer. Concomitantly, disease progression promotes further downregulation of activating receptors (NKp30, NKG2D, DNAM1, and 2B4) and upregulation of inhibitory receptors (NKG2A and CD85j) [116], which was already apparent compared with healthy individuals [64,116,121]. NK cells from patients in advanced disease stages also exhibit a declining responsivity to cytokines [81,84], due in part to defects in STAT signalling pathways [54]. When compared with tumor infiltrating NK cells, their peripheral counterparts display a similar downregulation of activating receptors [116] despite maintaining higher functionality [116]. Still, this can be abrogated in presence of TNBC cells [123], tumor supernatant [116,122] or serum from metastatic patients [54]. Surprisingly, serum from early stage breast cancer patients seems to induce the opposite effect of improving NK function [54], suggesting that the level of systemic immune suppression in initial disease stages may still leave room for immune cell activation.
Consistent with the establishment of an immune suppressive environment at the systemic level, breast cancer progression is accompanied by a shift in NK cell subset distribution [124] (Figure 1, right), with an increase of cytokine-producing CD56bright CD16lo/− cells in circulation and a decrease in the predominant cytotoxic CD56dim CD16+ subset [122], possibly due to a higher death rate of the latter [120]. This imbalance may negatively impact the pool of available effector killer cells, given that a higher proportion of CD16+ NK cells appears to correlate with more efficient ADCC [125]. The capacity of NK cells to perform ADCC becomes especially important in the context of HER2+ breast cancer treated with the monoclonal antibody trastuzumab [114]. For that reason, several studies have investigated potential predictors of ADCC efficiency and association with clinical response [125,126,127,128,129]. The CD16 (FcγRIII) and CD32 (FcγRII) receptors have received some attention due to their role in recognizing the Fc portion of trastuzumab (and other IgG antibodies), but while some groups claim that the genotype 158 V/V for CD16 confers higher ADCC efficiency [125,126], it appears the opposite may hold true for metastatic patients [126,127]. Reports for CD32 are also inconsistent, with some studies presenting a positive association between FCGRIIA 131 H/H genotype and trastuzumab clinical benefit [126,127], which was found to be non-significant in a larger cohort [128]. Nevertheless, the rate of ADCC itself may indicate which patients have the best likelihood of response to trastuzumab therapy, as seen in different cohorts of early stage [125,126] and metastatic patients [129]. This standard-of-care for HER2+ patients was also reported to improve NK cell cytotoxicity [125] (Figure 1, right), which was correlated with longer PFS in the metastatic setting [129]. Administration of chemotherapy regimens also appears to improve the effector phenotype of NK cells [50], especially in taxane-containing formulations [130], with upregulation of activating receptors [64] and higher production of cytotoxic granules [119]. Of note, women with large and locally advanced breast cancer who benefitted the most from neoadjuvant chemotherapy displayed significantly higher NK cytotoxicity at baseline [119], while another cohort of stage II–IV patients exhibited a positive association between increased NK cytotoxicity post-NAC and metastasis reduction [131]. These results highlight the potential use of NK effector function as biomarker for clinical response. This is further supported by the findings that NK cell function is impaired in families with higher incidence of breast cancer [132], and that former breast cancer patients (in remission for over five years) express NK activating receptors at a similar level as healthy individuals [116].
4. The Myeloid Lineage
Myeloid cell function and polarization are considered instrumental to the general immune response towards cancer in the human organism [133]. Tumor associated macrophages (TAM) are known promoters of metastization and cancer growth and comprise the major leukocyte population in breast cancer infiltrates [134]. However, other cell populations in the tumor milieu must also be acknowledged such as dendritic cells, for their capacity to capture tumor antigens and mount anti-tumor immune reactions [135], and neutrophils, which may become strongly polarized to act against or pro tumorigenesis [136]. The onset and development of breast cancer are also associated with subsets of myeloid-derived suppressor cells (MDSC), which are strongly immunosuppressive cells from the monocytic (m-MDSC) or granulocytic (g-MDSC) lineages. MDSC restrict immune effector function at the tumor site and promote recruitment and survival of Tregs [137]. Most importantly, it is known that part of these tumor-infiltrating populations is replenished from circulating precursors [134,136,137,138]. These data highlight the relevance of characterizing peripheral myeloid subsets to gain insight into the breast cancer–immune system crosstalk, as well as to procure biomarkers of disease progression.
4.1. Dendritic Cells
One of the key events in the establishment of anti-tumor immunity is the presentation of tumor antigens to different T cell subsets and their activation [135]. Although other immune populations (like B cells and macrophages) can also present antigen, dendritic cells are considered professional antigen presenting cells due to their ability to induce a primary immune response in naïve T cells [135]. However, the pivotal role of DC in cancer immunity has two distinct sides, since DC function can also be exploited by the tumor to inhibit immune effectors in the TME, either via checkpoint ligands like PD-1 or soluble factors like IL-10 [138]. In breast cancer patients, circulatory DC also appear to be negatively influenced by the cancer-driven systemic immune suppression. In breast cancer patients, DCs have been described to present impaired function [48,83,139,140,141,142] and reduced numbers [139,143] compared with healthy individuals (Figure 2, up left). This decrease in the DC population is also indicative of disease progression [83,144], as a continued decline of the two major DC subsets has been described in more advanced cancer stages, namely, with conventional DC (cDC) [140,144] and plasmacytoid DC (pDC) [92,140,144].
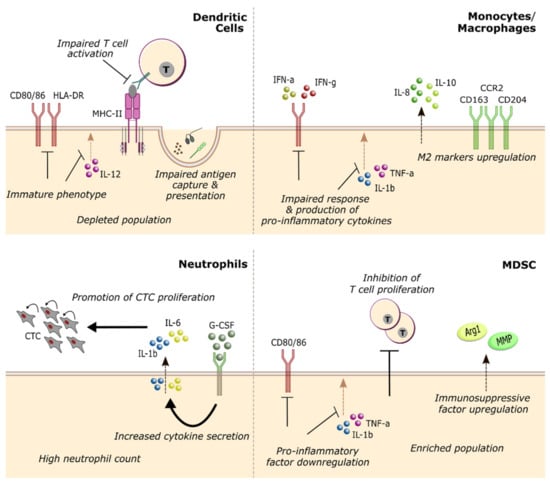
Figure 2.
Surface markers and cytokine response of myeloid peripheral immune cell populations associated with breast cancer occurrence and/or progression. In the myeloid lineage, breast cancer patients display a marked increase in cell populations with pro-tumorigenic functions (like MDSC and neutrophils), while anti-tumorigenic populations of dendritic cells are depleted and the remaining dendritic cells (DC) acquire an immature phenotype, preventing the mounting of effective immune responses. Monocyte and macrophage function is also skewed towards immune suppression, with impaired response to pro-inflammatory stimuli and upregulation of M2 markers. CTC, circulating tumor cell; MDSC, myeloid-derived suppressor cell.
Overall, circulating DC appear to be progressively enriched in immature cells [140,144] and to exhibit marked defects in phagocytosis, antigen capture and presentation [48,140,144], and T cell activation [48,83,141,144] (Figure 2, up left). On the other hand, an earlier study with 53 patients observed an increase in mature CD83+ DC from stage I to stage II breast cancer that was abolished upon tumor resection [139]. These results suggest that the primary tumor may also activate dendritic cells in earlier stages. Phenotypically, patients’ DC display impaired IL-12 production upon stimulation [139,141,142] as well as downregulation of HLA-DR [83,141,144], CD80, and CD86 [48,83,140,141,144], which are essential for antigen presentation and T cell activation [135]. Poor cytokine secretion by cDC was also significantly associated with elevated numbers of CTCs in patient blood [142], further suggesting a progressive decline in DC function. In the few studies where prognostic parameters have been assessed, patients with higher levels of circulating DC post-treatment consistently showed longer survival [77,92], despite the depletion of the DC pool induced by chemotherapy [144]. Nevertheless, there is still a great need for studies clarifying the association between dendritic cells (numbers, subsets, and phenotypes) and the clinical prognosis of breast cancer patients—more so, if one considers the abundance of cancer immunotherapies under development that depend on DC activity [135,138].
4.2. Monocytes and Neutrophils
Monocytes and the monocytic lineage (including macrophages and other subpopulations) have long been associated with breast cancer outcome and response to treatment, considering the role of tumor-associated macrophages in cancer progression [134]. On the other hand, the phenotype and function of circulating monocytes have not been under the same spotlight. Nevertheless, accumulating evidence starts to indicate a prevalence of anti-inflammatory polarization of peripheral monocytes in breast cancer patients [81,85,145,146], akin to what can be found at the tumor site [134]. Peripheral blood monocytes from patients display a decreased responsiveness to IFN-γ [85] and IFN-α [81], and impaired production of pro-inflammatory cytokines [145] compared with healthy individuals. Simultaneously, the secretion of anti-inflammatory IL-8 and IL-10 is increased [145] (Figure 2, up right). Breast cancer patients were also found to carry a higher proportion of M2-like macrophages in circulation [146]. A decline in monocytic pro-inflammatory response is also a sign of disease progression [85] which correlates with poor outcome parameters (e.g., TAM infiltration, CSF-1R upregulation, and shorter RFS in early-stage patients) [85]. Coincidentally, metastatic patients with more M2-like [147] and fewer HLA-DR+ mature monocytes [77] in circulation also presented worse prognostic indicators and survival times, respectively. However, it is interesting to note that one cohort of relapsing patients with metastasis displayed an increase in responsiveness to IFN-α and IL-12 production [81]. Overall, these data advance the possibility of using peripheral monocyte phenotype as a prognostic marker through several disease stages, but also prompts the need for further research on the mechanisms behind their pro- or anti-inflammatory polarization. Moreover, in luminal A breast cancer patients, advanced disease was associated with a shift towards higher representation of intermediate (CD14+ CD16 +) over classical (CD14hi CD16−) monocytes [104], reflecting the lack of immunosuppression associated with this subtype [69].
The predictive potential of monocyte count remains controversial. While some studies indicate an association between high peripheral monocyte counts and increased CD8+ TIL (a positive prognostic indicator) [30], or lower risk of developing breast cancer [102], other cohorts displayed a clear clinical benefit from lower monocyte counts, either due to fewer CTC in blood [36] or prolonged disease-free survival [31,37,77]. Work by Lafrenie et al. also alerts to the distinct prognostic values that can be obtained from monocyte proportions in the peripheral blood depending on the method for calculating such proportions and on patient treatment regimen [77].
On a similar note, the implications of circulating neutrophils for breast cancer have only recently been considered. Still, the available literature has been quite consistent in showing that high neutrophil counts are predictive of poor prognosis for breast cancer patients, associated with higher levels of circulating tumor cells [36] (Figure 2, down left), lymph node invasion [28] and drastically inferior survival probabilities [28,32]. Szczerba et al. describe a close relationship between neutrophil phenotype and promotion of metastasis in a cohort of invasive breast cancer patients [148]. They observe the capacity of CTC-associated neutrophils to induce CTC proliferation via IL-6 and IL-1β and alert that G-CSF containing therapeutics may inadvertently promote an increase in CTC-neutrophil clusters [148].
4.3. MDSC
In breast cancer patients, both MDSC subsets (m-MDSC, CD14+ HLA-DR−; and g-MDSC, CD14− CD11b+ CD15+ [137]) appear to be more abundant than in healthy individuals [64,71,78,145,149,150,151]. These MDSC display typical indicators of suppression: inhibition of T cell proliferation [78,149]; downregulation of CD80/86, TNF-α, and IL-1β [145]; upregulation of matrix metalloproteinases and arginase (ARG1) [145] (Figure 2, down right). Increased numbers of MDSC were found to be associated with advanced tumor stage [71,149,151], higher metastatic burden [145,151] and high Treg frequency [145], all predictors of poor prognosis. The decrease in MDSC after surgical resection of the tumor [150] suggests a preponderant role of tumor-secreted factors in maintaining this immune population. The response of each MDSC subset to systemic chemotherapy appears to be distinct, with an increase of g-MDSC [151,152] and a decline in m-MDSC [153]. Nevertheless, lower levels of g-MDSC at baseline [154] and after NAC [152] were more frequent in patients achieving pCR after this therapy. The predictive power of MDSC count may be more relevant when considered together with another parameter of immune function; in a cohort of elderly breast cancer patients, the presence of reduced levels of m-MDSC and a positive CD8+ T cell response to TAA conferred a 100% probability of survival at 4 years [91].
5. Experimental Models to Interrogate Tumor–Immune Interactions
It is well established that the peripheral immune landscape of breast cancer is characterized by complex cell states and phenotypes, and that some of these populations display strong correlation with disease prognosis and therapeutic outcomes. Nonetheless, current knowledge is not enough to understand the biological interactions between immune populations and tumor cells and how these interactions are modulated by different pharmacological approaches. This knowledge is instrumental to unravel new biomarkers, as well as to define the weak spots of cancer immunosuppression and identify the best effector functions to be exploited for each immune subset. This knowledge can leverage the development of novel immunotherapies and a refined assignment of current standard-of-care regimens to breast cancer patients.
During the last decade, it became increasingly clear that to obtain accurate predictors of drug response it was necessary to develop new experimental cancer models taking into account: the native tri-dimensional (3D) tumor architecture, the cellular composition of the tumor microenvironment, and the human relevance of the underlying interactions [155,156,157,158,159]. Despite the fundamental role of mouse models in many areas of immunology research, it is clear that they are unable to serve as faithful replicas of the human immune system or human tumors [159,160,161], also rendering them less reliable for the testing of immunomodulatory drugs or therapeutic proteins [159,160]. This is in part due to particular differences in the composition and function of both immune systems, some well documented such as NK receptor and major histocompatibility complex (MHC) repertoires or T cell subsets, and potentially others that are still unknown [160]. Further, mice strains lack genetic diversity and exposure to pathogens, and they have a short life span. Altogether, these features contribute to the compromised ability of the murine immune system to generate the variety of processes and cell states observed in the human [161]. Furthermore, the alarmingly high rate of drug failure when transitioning to clinical trials has been pointing to the poor transition of pre-clinical mouse models [162,163]. The use of humanized mice as an alternative to study human immune effects at the system level also falls short of the ideal [159,164,165]. Mice transgenic for human proteins still carry a murine immune system [159], and even the strains used for engraftment of human hematopoietic stem cells do not reflect the full diversity and function of the human immune system [159,164]. Additionally, animal-based research is always more expensive and time consuming, and fails to take into consideration the role of human stromal and endothelial cells [165], which are known to be closely involved in the tumor–immune crosstalk [157].
In this context, 3D heterotypic cellular models of tumor–immune interaction with a human-only cellular composition have surfaced as a valuable alternative to the overly simplistic 2D cancer and immune cell lines-based research and to the often inadequate and more expensive animal-based in vivo models [166,167]. Broadly speaking, to grasp the dynamics of tumor–immune interactions it would be critical to model two key biological contexts: (a) the TME characteristic of each breast cancer subtype, often exerting strong immunosuppression over its immune component; (b) the contact between peripheral immune cells and the already developed TME. While in the first the goal is to either eliminate or repolarize suppressive cells, in the second there is an added clinical opportunity to use the pro-inflammatory potential of immune cells which have not yet been subverted by the tumor. Both these approaches can be used to establish platforms for three areas in which clinical translation remains ineffective: drug testing, biomarker discovery and biomarker validation [168,169]. While patient-derived explants (PDE) have already been used to identify prognostic [170] and predictive [171] biomarkers in solid tumors, other advanced 3D cellular models incorporating key features of the tumor–immune interaction can be essential to identify and validate peripheral immune biomarkers of breast cancer [172,173,174].
At this point, it should be noted that immunocompetent breast cancer 3D models are scarce in the literature, and that existing ones are mostly proof-of-concept studies that have not been replicated or used for further testing (Table 2). Currently available models of the breast cancer microenvironment often incorporate particular immune subpopulations, such as monocytes [175,176,177,178], T cells [179,180], or NK cells [180,181], to capture the reciprocal influence of immune and tumor cells in the suppressive environment [175,176,177,178,181] but also to assess the anti-tumor capacity of killer cells [179,180]. In another approach, several groups have developed models containing distinct immune cell types for drug testing in the TME of different breast cancer subtypes [182,183]. These studies heighten the promise of advanced heterotypic cell models for predictive pre-clinical and co-clinical studies. On the field of patient-derived ex vivo cultures (explants [172] and precision cut slices [184,185]), fewer examples can be found due to the difficulty in maintaining the native immune component, as well as the stroma of the breast cancer TME in prolonged culture [172], similar to what is observed in other cancer types [186]. Our group has recently described a culture method (using alginate-encapsulated tumor tissue from ER+ breast cancer patients, cultured in an agitation-based system) in which expression and functionality of ER receptors are retained after four weeks, as well its CD45+ population [187]. This work highlights the potential of ex vivo cultures to study the temporal dynamics of native TME interactions, although further characterization is necessary to probe putative drug testing applications.
Confrontational 3D models have most often been used to study immune cell recruitment and initial infiltration into the tumor mass [188,189,190,191,192,193], investigating the underlying tumor- and stromal-derived soluble factor-induced signalling [191,192,193]. Alternatively, other models of immune cell contact with the tumor mass have assessed means to activate NK cells [189,190], CTL [194], and monocytes [194] towards tumor cell killing. Work by Wallstabe et al. displayed the proof-of-concept that immunocompetent breast cancer models can be valuable for testing the killing efficacy of CAR-T cells in the pre-clinical setting, while also taking into account T cell extravasation from the tumor vasculature [195].
Nonetheless, these models still reflect a much lower complexity compared to animal models, the current gold standard of mechanistic studies, pre-clinical testing, and biomarker discovery. Moving towards a research paradigm mostly based on human-only systems requires substantial technological advancements in the area of human immune modelling—ideally leading to the development of an “artificial immune system” built from modular units, each representing the function of an essential immune organ or compartment [165,196]. As of today, there are several reports on the development of advanced cellular models for lymph nodes [197], spleen [198], bone marrow [199], tonsil [161], thymus [200], and immunocompetent skin [201], lung [202], gut [203], and liver [204], albeit with varying levels of functionality and native-like architecture. The generation of immune organ-like structures in vitro has been hampered by difficulties in recreating these very complex microenvironments, with uncommonly high cell densities and defined functional zones, on a small scale, and specific dynamics of cellular differentiation, communication and motility [165,205]. The field of microphysiological systems (MPS) (also known as “organs-on-chip”) combined with advancements on bioprinting can be instrumental in the development of novel advanced models that more closely resemble human tumor–immune interactions, and that allow the modular integration of several immune “organs” or compartments [165,196,206]. At the moment, the main challenge of this technology is the implementation of sensors for live monitoring of cellular processes, which can be based on the miniaturization of existing analytical techniques or in the integration of novel biosensors [207]. By bringing together the potential for broad customization of culture conditions, the advantage of miniaturization and throughput (compared with traditional bioreactors or culture plates), and the possibility of replicating different biological compartments of the TME in the same system [208,209], MPS technology may be a starting platform to refocus on basic and applied human immunology research [165,196].


Table 2.
3D cellular models of breast cancer and immune system interaction.
Table 2.
3D cellular models of breast cancer and immune system interaction.
| Model Type | Immune Cell Types | Culture Time | Model Objective | Major Observations | Refs. |
|---|---|---|---|---|---|
| Tumor Microenvironment Models | |||||
| Spheroid-based | Monocytes (+ stroma) | 7 days | MΦ polarization in the TME | TNBC TME induces stronger M2-like MΦ polarization including secretion of pro-tumoral cytokines and MMPs | [175] |
| Organoid | T cells | 6 h | T cell killing | Vδ2+ T cells effectively kill BC cells in response to bisphosphonate drugs | [179] |
| Spheroid-based | T cells, NK cells | 4 days | Tumor interaction with Treg and NK cells | Immune mediation affects morphology of the tumor mass and secretion of CCL4 | [180] |
| Spheroid-based | Monocytes | 7 days | MΦ-induced angiogenesis | MΦ induce increasing VEGF production in the TME over time | [176] |
| Spheroid-based | Monocytes | 5 days | MΦ polarization in the TME | Aggressiveness of BC subtype correlates with upregulation of MMP1/9 and COX2, collagen degradation and production of PGE2 | [177] |
| Spheroid-based | Monocytes | 7 days | Monocyte differentiation in the TME | Monocytes in the TME may have the potential to differentiate into endothelial cells | [178] |
| Spheroid-based | NK cells | 2 days | Tumor escape from NK surveillance | Tumor exposure induces a transcriptional “resting” state in NK cells that promotes tumor growth | [181] |
| Spheroid-based | CD45+ (+ stroma) | 10 days | Drug testing in ER+ TME | Inhibition of PDGF and IL-1 signalling synergizes with tamoxifen treatment in ER+ BC | [182] |
| MPS | PBMC (+ stroma) | 4 days | Drug testing in HER2+ TME | Long-term cancer-immune interactions and ADCC induced by trastuzumab treatment are counteracted by cancer-associated fibroblasts | [183] |
| PDE | CD45+ (+ stroma) | 4 weeks | Maintenance of ER+ TME | CD45+ cells can be maintained in a long-term culture of patient-derived explants | [187] |
| Precision-cut slices | CD45+ (+ stroma) | 1 day | Drug testing in the TME | Rapamycin modulates expression of several genes associated with biosynthetic and catabolic processes in HER2+ and HER2− BC | [185] |
| Peripheral immunity—TME Confrontational Models | |||||
| MPS | Monocytes, T cells (+ endothelial) | 6 days | T cell recruitment | T cell recruitment to the tumor site is promoted by a hypoxic TME containing monocytes | [188] |
| MPS | NK cells (+ endothelial) | 3 days | NK cell recruitment, infiltration, and cytotoxicity | NK cells actively migrate and infiltrate the tumor mass and respond to antibody-cytokine conjugates with enhanced cytotoxicity | [189] |
| Spheroid-based | NK cells | 2 days | NK recruitment and infiltration | Bispecific CD16/mesothelin antibody promotes NK cell recruitment, infiltration, and dose dependent ADCC | [190] |
| Spheroid-based | Macrophages | 2 days | Monocyte migration and tumor invasion, tumor-immune communication | Tumor-secreted miR-375 enhances MΦ migration, infiltration and pro-tumoral phenotype | [191] |
| Spheroid-based | Monocytes (+ stroma) | 40 h | Monocyte migration and invasion | Monocyte migration and invasion capacity depends on BC subtype and is promoted by presence of fibroblasts partly via CCL2 signalling | [192] |
| Spheroid-based | Monocytes | 2 days | Monocyte recruitment and invasion | Increased ROS production upon disruption of mammary epithelium polarization enhances monocyte recruitment and infiltration | [193] |
| Spheroid-based | PBMC | 2 days | Initial anti-tumor immune response | CD80 expression on phagocytes is required to induce CTL activation and is negatively regulated by PGE2 | [194] |
| MPS | T cells | 3 days | Test anti-tumor CAR T function | ROR1-CAR T cells actively migrate from the periphery, infiltrate, and eliminate several layers of the tumor mass | [195] |
ADCC, antibody-dependent cell-mediated cytotoxicity; BC, breast cancer; CTL, cytotoxic T lymphocyte; ER, estrogen receptor; MΦ, macrophage; MPS, microphysiological system; PBMC, peripheral blood mononuclear cells; PDE, patient-derived explant; TME, tumor microenvironment; TNBC, triple negative breast cancer.
6. Conclusions and Future Perspectives
The current burden of breast cancer for women worldwide requires new and better measures for disease management, monitoring, and treatment tailoring. Predictive and prognostic immune biomarkers obtained from the peripheral blood would certainly make for faster, cheaper, and more individualized decision making, but as of today much of the relationship between the peripheral immune system and breast cancer is not uncovered. In this review, we have summarized the available knowledge of the peripheral immune landscape of breast cancer but, as it became clear, this is a field that still requires attentive interrogation and standardization to generate meaningful clinical information. Currently, only a limited number of immune features have shown plausible association with clinical data for breast cancer. These include the marked relationship of neutrophils with poor prognosis across subtypes (Section 2.1), as well as the link between more reactive cytotoxic lymphocytes (CD8+ T cells and NK cells) and better outcome for HER2+ breast cancer patients (Section 3.1 and Section 3.3, respectively). However, these indicators still require thorough research and validation before being introduced as prognostic biomarkers in clinical practice. In future studies, attention must be paid to evaluate separately patients from different breast cancer subtypes, as these have been shown to display distinct immune profiles. An important caveat to consider is that findings from profiling of small patient samples require further validation in larger patient cohorts. The identification of clinically relevant peripheral immune biomarkers will also boost the development of advanced cellular models of cancer–immune interaction, much needed to uncover molecular mechanisms and putative drug targets in an all-human setting. Despite major advancements made in recent years, including the rise in popularity of “organs/tumors-on-chip”, immunocompetent tumor models still face two considerable challenges: the need to incorporate tissue-specific stroma (which may be easier for a cancer environment, but more difficult for, e.g., lymph node models) and the requirement for functional vascularization, allowing for immune cell perfusion and communication with functional endothelial cells. Above all, it is essential to keep in mind that improvements in advanced models of human immunity need to be preceded by a new look on basic human immunology, one that also includes extensive patient-based research for biomarkers of interest.
Author Contributions
Conceptualization, S.B. and C.B.; writing—original draft preparation, S.B. and S.F.; writing—review and editing, S.B., S.F., and C.B.; visualization: S.B. All authors have read and agreed to the published version of the manuscript.
Funding
This work was funded by iNOVA4 Health–UIDB/04462/2020, a program financially supported by Fundação para a Ciência e Tecnologia (FCT)/Ministério da Ciência, Tecnologia e Ensino Superior (MCTES), through national funds, and by FEDER under the PT2020 Partnership Agreement. S.B. was funded by FCT through individual PhD fellowship PD/BD/135550/2018.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| ADCC | antibody-dependent cell-mediated cytotoxicity |
| APC | antigen-presenting cell |
| BC | breast cancer |
| BReg | B regulatory cell |
| CAR-T | chimeric antigen receptor T cell |
| cDC | conventional dendritic cell |
| CTC | circulating tumor cells |
| CTL | cytotoxic T lymphocyte |
| DC | dendritic cell |
| DFS | disease-free survival |
| ER | estrogen receptor |
| g-MDSC | granulocytic myeloid-derived suppressor cell |
| HR | hormone receptor |
| LDH | lactate dehydrogenase |
| LMR | lymphocyte-to-monocyte ratio |
| MΦ | macrophage |
| MDSC | myeloid-derived suppressor cell |
| MHC | Major histocompatibility complex |
| m-MDSC | monocytic myeloid-derived suppressor cell |
| MPS | microphysiological system |
| NAC | neoadjuvant chemotherapy |
| NLR | neutrophil-to-lymphocyte ratio |
| NK | Natural Killer cells |
| OS | overall survival |
| PBL | peripheral blood lymphocytes |
| PBMC | peripheral blood mononuclear cells |
| pCR | pathological complete response |
| pDC | plasmacytoid dendritic cell |
| PDE | patient-derived explants |
| PLR | platelet-to-lymphocyte ratio |
| PMA | phorbol myristate acetate |
| PR | progesterone receptor |
| RFS | relapse-free survival |
| ROC | receiver operator characteristic |
| STAT | Signal transducer and activator of transcription |
| TAA | tumor-associated antigen |
| TAM | tumor-associated macrophage |
| TCM | central memory T cell |
| TCR | T cell receptor |
| T-DM1 | trastuzumab emtansine |
| TIL | tumor-infiltrating lymphocytes |
| TME | tumor microenvironment |
| TNBC | triple negative breast cancer |
| TReg | T regulatory cells |
References
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef]
- Harbeck, N.; Penault-Llorca, F.; Cortes, J.; Gnant, M.; Houssami, N.; Poortmans, P.; Ruddy, K.; Tsang, J.; Cardoso, F. Breast cancer. Nat. Rev. Dis. Prim. 2019, 5, 1–31. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, F.; Spence, D.; Mertz, S.; Corneliussen-James, D.; Sabelko, K.; Gralow, J.; Cardoso, M.-J.; Peccatori, F.; Paonessa, D.; Benares, A.; et al. Global analysis of advanced/metastatic breast cancer: Decade report (2005–2015). Breast 2018, 39, 131–138. [Google Scholar] [CrossRef]
- Cheang, M.C.; Martin, M.; Nielsen, T.O.; Prat, A.; Voduc, D.; Rodriguez-Lescure, A.; Ruiz, A.; Chia, S.; Shepherd, L.; Ruiz-Borrego, M.; et al. Defining Breast Cancer Intrinsic Subtypes by Quantitative Receptor Expression. Oncologist 2015, 20, 474–482. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, F.; Kyriakides, S.; Ohno, S.; Penault-Llorca, F.; Poortmans, P.; Rubio, I.; Zackrisson, S.; Senkus, E. Early breast cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2019, 30, 1194–1220. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, F.; Paluch-Shimon, S.; Senkus, E.; Curigliano, G.; Aapro, M.; André, F.; Barrios, C.; Bergh, J.; Bhattacharyya, G.; Biganzoli, L.; et al. 5th ESO-ESMO international consensus guidelines for advanced breast cancer (ABC 5). Ann. Oncol. 2020, 31, 1623–1649. [Google Scholar] [CrossRef]
- Chimal-Ramírez, G.K.; Espinoza-Sánchez, N.A.; Fuentes-Pananá, E.M. Protumor Activities of the Immune Response: Insights in the Mechanisms of Immunological Shift, Oncotraining, and Oncopromotion. J. Oncol. 2013, 2013, 1–16. [Google Scholar] [CrossRef]
- Garner, H.; De Visser, K.E. Immune crosstalk in cancer progression and metastatic spread: A complex conversation. Nat. Rev. Immunol. 2020, 20, 483–497. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhang, Z. The history and advances in cancer immunotherapy: Understanding the characteristics of tumor-infiltrating immune cells and their therapeutic implications. Cell. Mol. Immunol. 2020, 17, 807–821. [Google Scholar] [CrossRef]
- Burnet, M. Cancer—A Biological Approach: I. The Processes Of Control. II. The Significance of Somatic Mutation. BMJ 1957, 1, 779–786. [Google Scholar] [CrossRef]
- Dunn, G.P.; Bruce, A.T.; Ikeda, H.; Old, L.J.; Schreiber, R.D. Cancer immunoediting: From immunosurveillance to tumor escape. Nat. Immunol. 2002, 3, 991–998. [Google Scholar] [CrossRef]
- Zitvogel, L.; Apetoh, L.; Ghiringhelli, F.; Kroemer, G. Immunological aspects of cancer chemotherapy. Nat. Rev. Immunol. 2008, 8, 59–73. [Google Scholar] [CrossRef] [PubMed]
- Biziota, E.; Mavroeidis, L.; Hatzimichael, E.; Pappas, P. Metronomic chemotherapy: A potent macerator of cancer by inducing angiogenesis suppression and antitumor immune activation. Cancer Lett. 2017, 400, 243–251. [Google Scholar] [CrossRef]
- Lu, J.; Liu, X.; Liao, Y.-P.; Wang, X.; Ahmed, A.; Jiang, W.; Ji, Y.; Meng, H.; Nel, A.E. Breast Cancer Chemo-immunotherapy through Liposomal Delivery of an Immunogenic Cell Death Stimulus Plus Interference in the IDO-1 Pathway. ACS Nano 2018, 12, 11041–11061. [Google Scholar] [CrossRef]
- Horlock, C.; Stott, B.; Dyson, P.J.; Morishita, M.; Coombes, R.C.; Savage, P.; Stebbing, J. The effects of trastuzumab on the CD4+CD25+FoxP3+ and CD4+IL17A+ T-cell axis in patients with breast cancer. Br. J. Cancer 2009, 100, 1061–1067. [Google Scholar] [CrossRef] [PubMed]
- Stanton, S.E.; Disis, M.L. Clinical significance of tumor-infiltrating lymphocytes in breast cancer. J. Immunother. Cancer 2016, 4, 59. [Google Scholar] [CrossRef] [PubMed]
- Yamashita-Kashima, Y.; Shu, S.; Harada, N.; Fujimoto-Ouchi, K. Enhanced antitumor activity of trastuzumab emtansine (T-DM1) in combination with pertuzumab in a HER2-positive gastric cancer model. Oncol. Rep. 2013, 30, 1087–1093. [Google Scholar] [CrossRef] [PubMed]
- Junttila, T.T.; Li, G.; Parsons, K.; Phillips, G.L.; Sliwkowski, M.X. Trastuzumab-DM1 (T-DM1) retains all the mechanisms of action of trastuzumab and efficiently inhibits growth of lapatinib insensitive breast cancer. Breast Cancer Res. Treat. 2010, 128, 347–356. [Google Scholar] [CrossRef]
- Emens, L.A. Breast Cancer Immunotherapy: Facts and Hopes. Clin. Cancer Res. 2018, 24, 511–520. [Google Scholar] [CrossRef]
- Schmid, P.; Adams, S.; Rugo, H.S.; Schneeweiss, A.; Barrios, C.H.; Iwata, H.; Diéras, V.; Hegg, R.; Im, S.A.; Shaw Wright, G.; et al. Atezolizumab and Nab-Paclitaxel in Advanced Triple-Negative Breast Cancer. N. Engl. J. Med. 2018, 379, 2108–2121. [Google Scholar] [CrossRef]
- Schmid, P.; Salgado, R.; Park, Y.; Muñoz-Couselo, E.; Kim, S.; Sohn, J.; Im, S.-A.; Foukakis, T.; Kuemmel, S.; Dent, R.; et al. Pembrolizumab plus chemotherapy as neoadjuvant treatment of high-risk, early-stage triple-negative breast cancer: Results from the phase 1b open-label, multicohort KEYNOTE-173 study. Ann. Oncol. 2020, 31, 569–581. [Google Scholar] [CrossRef] [PubMed]
- Denkert, C.; Loibl, S.; Noske, A.; Roller, M.; Müller, B.M.; Komor, M.; Budczies, J.; Darb-Esfahani, S.; Kronenwett, R.; Hanusch, C.; et al. Tumor-Associated Lymphocytes As an Independent Predictor of Response to Neoadjuvant Chemotherapy in Breast Cancer. J. Clin. Oncol. 2010, 28, 105–113. [Google Scholar] [CrossRef] [PubMed]
- Adams, S.; Gatti-Mays, M.E.; Kalinsky, K.; Korde, L.A.; Sharon, E.; Amiri-Kordestani, L.; Bear, H.; McArthur, H.L.; Frank, E.; Perlmutter, J.; et al. Current Landscape of Immunotherapy in Breast Cancer. JAMA Oncol. 2019, 5, 1205. [Google Scholar] [CrossRef] [PubMed]
- Savas, P.P.; Salgado, R.; Denkert, C.; Sotiriou, C.; Darcy, P.K.P.; Smyth, M.J.M.; Loi, S. Clinical relevance of host immunity in breast cancer: From TILs to the clinic. Nat. Rev. Clin. Oncol. 2016, 13, 228–241. [Google Scholar] [CrossRef] [PubMed]
- Buder-Bakhaya, K.; Hassel, J.C. Biomarkers for Clinical Benefit of Immune Checkpoint Inhibitor Treatment—A Review From the Melanoma Perspective and Beyond. Front. Immunol. 2018, 9, 1474. [Google Scholar] [CrossRef]
- Papatestas, A.E.; Kark, A.E. Peripheral lymphocyte counts in breast carcinoma:An index of immune competence. Cancer 1974, 34, 2014–2017. [Google Scholar] [CrossRef]
- Conesa, M.A.V.; Garcia-Martinez, E.; Billalabeitia, E.G.; Benito, A.C.; Garcia, T.G.; Garcia, V.V.; de la Peña, F.A. Predictive value of peripheral blood lymphocyte count in breast cancer patients treated with primary chemotherapy. Breast 2012, 21, 468–474. [Google Scholar] [CrossRef]
- Qian, Y.; Tao, J.; Li, X.; Chen, H.; Lu, Q.; Yang, J.; Pan, H.; Wang, C.; Zhou, W.; Liu, X. Peripheral inflammation/immune indicators of chemosensitivity and prognosis in breast cancer patients treated with neoadjuvant chemotherapy. OncoTargets Ther. 2018, 11, 1423–1432. [Google Scholar] [CrossRef]
- Losada, B.; Guerra, J.A.; Malón, D.; Jara, C.; Rodriguez, L.; Del Barco, S. Pretreatment neutrophil/lymphocyte, platelet/lymphocyte, lymphocyte/monocyte, and neutrophil/monocyte ratios and outcome in elderly breast cancer patients. Clin. Transl. Oncol. 2019, 21, 855–863. [Google Scholar] [CrossRef]
- Lee, K.H.; Kim, E.Y.; Yun, J.S.; Park, Y.L.; Do, S.-I.; Chae, S.W.; Park, C.H. The prognostic and predictive value of tumor-infiltrating lymphocytes and hematologic parameters in patients with breast cancer. BMC Cancer 2018, 18, 938. [Google Scholar] [CrossRef]
- He, J.; Lv, P.; Yang, X.; Chen, Y.; Liu, C.; Qiu, X. Pretreatment lymphocyte to monocyte ratio as a predictor of prognosis in patients with early-stage triple-negative breast cancer. Tumor Biol. 2016, 37, 9037–9043. [Google Scholar] [CrossRef]
- Hernández, C.M.; Madrona, A.P.; Gil Vázquez, P.J.; Fernández, P.J.G.; Merino, G.R.; Romero, J.L.A.; Paricio, P.P. Usefulness of lymphocyte-to-monocyte, neutrophil-to-monocyte and neutrophil-to-lymphocyte ratios as prognostic markers in breast cancer patients treated with neoadjuvant chemotherapy. Clin. Transl. Oncol. 2017, 20, 476–483. [Google Scholar] [CrossRef]
- Azab, B.; Bhatt, V.R.; Phookan, J.; Murukutla, S.; Kohn, N.; Terjanian, T.; Widmann, W.D. Usefulness of the Neutrophil-to-Lymphocyte Ratio in Predicting Short- and Long-Term Mortality in Breast Cancer Patients. Ann. Surg. Oncol. 2011, 19, 217–224. [Google Scholar] [CrossRef] [PubMed]
- Azab, B.; Shah, N.; Radbel, J.; Tan, P.; Bhatt, V.; Vonfrolio, S.; Habeshy, A.; Picon, A.; Bloom, S. Pretreatment neutrophil/lymphocyte ratio is superior to platelet/lymphocyte ratio as a predictor of long-term mortality in breast cancer patients. Med Oncol. 2013, 30, 1–11. [Google Scholar] [CrossRef]
- Koh, C.-H.; Bhoopathy, N.; Ng, K.-L.; Jabir, R.S.; Tan, G.-H.; See, M.-H.; Jamaris, S.; A Taib, N. Utility of pre-treatment neutrophil–lymphocyte ratio and platelet–lymphocyte ratio as prognostic factors in breast cancer. Br. J. Cancer 2015, 113, 150–158. [Google Scholar] [CrossRef] [PubMed]
- De Giorgi, U.; Mego, M.; Scarpi, E.; Giordano, A.; Giuliano, M.; Valero, V.; Alvarez, R.H.; Ueno, N.T.; Cristofanilli, M.; Reuben, J.M. Association between circulating tumor cells and peripheral blood monocytes in metastatic breast cancer. Ther. Adv. Med Oncol. 2019, 11, 175883591986606. [Google Scholar] [CrossRef] [PubMed]
- Ni, X.-J.; Zhang, X.-L.; Ou-Yang, Q.-W.; Qian, G.-W.; Wang, L.; Chen, S.; Jiang, Y.-Z.; Zuo, W.-J.; Wu, J.; Hu, X.; et al. An Elevated Peripheral Blood Lymphocyte-to-Monocyte Ratio Predicts Favorable Response and Prognosis in Locally Advanced Breast Cancer following Neoadjuvant Chemotherapy. PLoS ONE 2014, 9, e111886. [Google Scholar] [CrossRef] [PubMed]
- Ji, H.; Xuan, Q.; Yan, C.; Liu, T.; Nanding, A.; Zhang, Q. The prognostic and predictive value of the lymphocyte to monocyte ratio in luminal-type breast cancer patients treated with CEF chemotherapy. Oncotarget 2016, 7, 34881–34889. [Google Scholar] [CrossRef] [PubMed]
- Krenn-Pilko, S.; Langsenlehner, T.; Thurner, E.-M.; Stojakovic, T.; Pichler, M.; Gerger, A.; Kapp, K.S. The elevated preoperative platelet-to-lymphocyte ratio predicts poor prognosis in breast cancer patients. Br. J. Cancer 2014, 110, 2524–2530. [Google Scholar] [CrossRef] [PubMed]
- Maeda, K.; Shibutani, M.; Otani, H.; Nagahara, H.; Ikeya, T.; Iseki, Y.; Tanaka, H.; Muguruma, K.; Hirakawa, K. Inflammation-based factors and prognosis in patients with colorectal cancer. World J. Gastrointest. Oncol. 2015, 7, 111–117. [Google Scholar] [CrossRef] [PubMed]
- Hu, P.; Shen, H.; Wang, G.; Zhang, P.; Liu, Q.; Du, J. Prognostic Significance of Systemic Inflammation-Based Lymphocyte- Monocyte Ratio in Patients with Lung Cancer: Based on a Large Cohort Study. PLoS ONE 2014, 9, e108062. [Google Scholar] [CrossRef] [PubMed]
- Lieto, E.; Galizia, G.; Auricchio, A.; Cardella, F.; Mabilia, A.; Basile, N.; Del Sorbo, G.; Castellano, P.; Romano, C.; Orditura, M.; et al. Preoperative Neutrophil to Lymphocyte Ratio and Lymphocyte to Monocyte Ratio are Prognostic Factors in Gastric Cancers Undergoing Surgery. J. Gastrointest. Surg. 2017, 21, 1764–1774. [Google Scholar] [CrossRef]
- Guo, Y.-H.; Sun, H.-F.; Zhang, Y.-B.; Liao, Z.-J.; Zhao, L.; Cui, J.; Wu, T.; Lu, J.-R.; Nan, K.-J.; Wang, S.-H. The clinical use of the platelet/lymphocyte ratio and lymphocyte/monocyte ratio as prognostic predictors in colorectal cancer: A meta-analysis. Oncotarget 2017, 8, 20011–20024. [Google Scholar] [CrossRef]
- Chen, L.; Kong, X.; Yan, C.; Fang, Y.; Wang, J. The Research Progress on the Prognostic Value of the Common Hematological Parameters in Peripheral Venous Blood in Breast Cancer. OncoTargets Ther. 2020, ume 13, 1397–1412. [Google Scholar] [CrossRef]
- Chang, J.H.; Jiang, Y.; Pillarisetty, V.G. Role of immune cells in pancreatic cancer from bench to clinical application. Medicine 2016, 95, e5541. [Google Scholar] [CrossRef]
- Duray, A.; Demoulin, S.; Hubert, P.; Delvenne, P.; Saussez, S. Immune Suppression in Head and Neck Cancers: A Review. Clin. Dev. Immunol. 2010, 2010, 1–15. [Google Scholar] [CrossRef]
- Evans, C.; Dalgleish, A.G.; Kumar, D. Review article: Immune suppression and colorectal cancer. Aliment. Pharmacol. Ther. 2006, 24, 1163–1177. [Google Scholar] [CrossRef]
- Pockaj, B.A.; Basu, G.D.; Pathangey, L.B.; Gray, R.J.; Hernandez, J.L.; Gendler, S.J.; Mukherjee, P. Reduced T-Cell and Dendritic Cell Function Is Related to Cyclooxygenase-2 Overexpression and Prostaglandin E2 Secretion in Patients with Breast Cancer. Ann. Surg. Oncol. 2004, 11, 328–339. [Google Scholar] [CrossRef] [PubMed]
- Panis, C.; Victorino, V.J.; Herrera, A.C.S.A.; Freitas, L.F.; De Rossi, T.; Campos, F.C.; Simão, A.N.C.; Barbosa, D.S.; Pinge-Filho, P.; Cecchini, R.; et al. Differential oxidative status and immune characterization of the early and advanced stages of human breast cancer. Breast Cancer Res. Treat. 2012, 133, 881–888. [Google Scholar] [CrossRef] [PubMed]
- Tsavaris, N.; Kosmas, C.; Vadiaka, M.; Kanelopoulos, P.; Boulamatsis, D. Immune changes in patients with advanced breast cancer undergoing chemotherapy with taxanes. Br. J. Cancer 2002, 87, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Elashi, A.A.; Nair, V.S.; Taha, R.Z.; Shaath, H.; Elkord, E. DNA methylation of immune checkpoints in the peripheral blood of breast and colorectal cancer patients. OncoImmunology 2019, 8, e1542918. [Google Scholar] [CrossRef]
- Muraro, E.; Martorelli, D.; Turchet, E.; Miolo, G.; Scalone, S.; Comaro, E.; Talamini, R.; Mastorci, K.; Lombardi, D.; Perin, T.; et al. A different immunologic profile characterizes patients with HER-2-overexpressing and HER-2-negative locally advanced breast cancer: Implications for immune-based therapies. Breast Cancer Res. 2011, 13, R117. [Google Scholar] [CrossRef]
- Kawaguchi, K.; Suzuki, E.; Yamaguchi, A.; Yamamoto, M.; Morita, S.; Toi, M. Altered expression of major immune regulatory molecules in peripheral blood immune cells associated with breast cancer. Breast Cancer 2016, 24, 111–120. [Google Scholar] [CrossRef] [PubMed]
- Konjević, G.; Jurišić, V.; Jovic, V.; Vuletić, A.; Martinović, K.M.; Radenkovic, S.; Spužić, I. Investigation of NK cell function and their modulation in different malignancies. Immunol. Res. 2012, 52, 139–156. [Google Scholar] [CrossRef] [PubMed]
- Konjević, G.; Jurišić, V.; Spužić, I. Association of NK Cell Dysfunction with Changes in LDH Characteristics of Peripheral Blood Lymphocytes (PBL) in Breast Cancer Patients. Breast Cancer Res. Treat. 2001, 66, 255–263. [Google Scholar] [CrossRef] [PubMed]
- Mizuno, R.; Kawada, K.; Sakai, Y. Prostaglandin E2/EP Signaling in the Tumor Microenvironment of Colorectal Cancer. Int. J. Mol. Sci. 2019, 20, 6254. [Google Scholar] [CrossRef] [PubMed]
- Sawant, D.V.; Yano, H.; Chikina, M.; Zhang, Q.; Liao, M.; Liu, C.; Callahan, D.J.; Sun, Z.; Sun, T.; Tabib, T.; et al. Adaptive plasticity of IL-10+ and IL-35+ Treg cells cooperatively promotes tumor T cell exhaustion. Nat. Immunol. 2019, 20, 724–735. [Google Scholar] [CrossRef]
- Wang, H.-W.; Joyce, J.A. Alternative activation of tumor-associated macrophages by IL-4. Cell Cycle 2010, 9, 4824–4835. [Google Scholar] [CrossRef]
- Salgado, R.; Junius, S.; Benoy, I.; Van Dam, P.; Vermeulen, P.; Van Marck, E.; Huget, P.; Dirix, L.Y. Circulating interleukin-6 predicts survival in patients with metastatic breast cancer. Int. J. Cancer 2002, 103, 642–646. [Google Scholar] [CrossRef] [PubMed]
- Shabo, I.; Stål, O.; Olsson, H.; Doré, S.; Svanvik, J. Breast cancer expression of CD163, a macrophage scavenger receptor, is related to early distant recurrence and reduced patient survival. Int. J. Cancer 2008, 123, 780–786. [Google Scholar] [CrossRef]
- Chong, S.Z.; Evrard, M.; Devi, S.; Chen, J.; Lim, J.Y.; See, P.; Zhang, Y.; Adrover, J.M.; Lee, B.; Tan, L.; et al. CXCR4 identifies transitional bone marrow premonocytes that replenish the mature monocyte pool for peripheral responses. J. Exp. Med. 2016, 213, 2293–2314. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Z.-Q.; Cao, W.-H.; Xie, J.-J.; Lin, J.; Shen, Z.-Y.; Zhang, Q.-Y.; Shen, J.-H.; Xu, L.-Y.; Li, E.-M. Expression and prognostic significance of THBS1, Cyr61 and CTGF in esophageal squamous cell carcinoma. BMC Cancer 2009, 9, 291. [Google Scholar] [CrossRef] [PubMed]
- Suh, E.J.; Kabir, M.H.; Kang, U.-B.; Lee, J.W.; Yu, J.; Noh, D.-Y.; Lee, C. Comparative profiling of plasma proteome from breast cancer patients reveals thrombospondin-1 and BRWD3 as serological biomarkers. Exp. Mol. Med. 2012, 44, 36–44. [Google Scholar] [CrossRef] [PubMed]
- Foulds, G.A.; Vadakekolathu, J.; Abdel-Fatah, T.M.A.; Nagarajan, D.; Reeder, S.; Johnson, C.; Hood, S.; Moseley, P.M.; Chan, S.Y.T.; Pockley, A.G.; et al. Immune-Phenotyping and Transcriptomic Profiling of Peripheral Blood Mononuclear Cells From Patients With Breast Cancer: Identification of a 3 Gene Signature Which Predicts Relapse of Triple Negative Breast Cancer. Front. Immunol. 2018, 9. [Google Scholar] [CrossRef]
- McGranahan, N.; Furness, A.J.S.; Rosenthal, R.; Ramskov, S.; Lyngaa, R.B.; Saini, S.K.; Jamal-Hanjani, M.; Wilson, G.A.; Birkbak, N.J.; Hiley, C.T.; et al. Clonal neoantigens elicit T cell immunoreactivity and sensitivity to immune checkpoint blockade. Science 2016, 351, 1463–1469. [Google Scholar] [CrossRef]
- Lauss, M.; Donia, M.; Harbst, K.; Andersen, R.; Mitra, S.; Rosengren, F.; Salim, M.; Vallon-Christersson, J.; Törngren, T.; Kvist, A.; et al. Mutational and putative neoantigen load predict clinical benefit of adoptive T cell therapy in melanoma. Nat. Commun. 2017, 8, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Duan, Q.; Zhang, H.; Zheng, J.; Zhang, L. Turning Cold into Hot: Firing up the Tumor Microenvironment. Trends Cancer 2020, 6, 605–618. [Google Scholar] [CrossRef]
- Nixon, A.B.; Schalper, K.A.; Jacobs, I.; Potluri, S.; Wang, I.-M.; Fleener, C. Peripheral immune-based biomarkers in cancer immunotherapy: Can we realize their predictive potential? J. Immunother. Cancer 2019, 7, 325. [Google Scholar] [CrossRef]
- Dieci, M.V.; Griguolo, G.; Miglietta, F.; Guarneri, V. The immune system and hormone-receptor positive breast cancer: Is it really a dead end? Cancer Treat. Rev. 2016, 46, 9–19. [Google Scholar] [CrossRef]
- Nagarajan, D.; McArdle, S.E.B. Immune Landscape of Breast Cancers. Biomedicines 2018, 6, 20. [Google Scholar] [CrossRef]
- Wang, J.; Yang, J. Identification of CD4+CD25+CD127− regulatory T cells and CD14+HLA−DR−/low myeloid-derived suppressor cells and their roles in the prognosis of breast cancer. Biomed. Rep. 2016, 5, 208–212. [Google Scholar] [CrossRef]
- Hueman, M.T.; Stojadinovic, A.; Storrer, C.E.; Foley, R.J.; Gurney, J.M.; Shriver, C.D.; Ponniah, S.; Peoples, G.E. Levels of circulating regulatory CD4+CD25+ T cells are decreased in breast cancer patients after vaccination with a HER2/neu peptide (E75) and GM-CSF vaccine. Breast Cancer Res. Treat. 2006, 98, 17–29. [Google Scholar] [CrossRef]
- Perez, S.A.; Karamouzis, M.V.; Skarlos, D.V.; Ardavanis, A.; Sotiriadou, N.N.; Iliopoulou, E.G.; Salagianni, M.L.; Orphanos, G.; Baxevanis, C.N.; Rigatos, G.; et al. CD4+CD25+ Regulatory T-Cell Frequency in HER-2/neu (HER)-Positive and HER-Negative Advanced-Stage Breast Cancer Patients. Clin. Cancer Res. 2007, 13, 2714–2721. [Google Scholar] [CrossRef] [PubMed]
- Mego, M.; Gao, H.; Cohen, E.; Anfossi, S.; Giordano, A.; Sanda, T.; Fouad, T.; De Giorgi, U.; Giuliano, M.; Woodward, W.; et al. Circulating Tumor Cells (CTC) Are Associated with Defects in Adaptive Immunity in Patients with Inflammatory Breast Cancer. J. Cancer 2016, 7, 1095–1104. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Simons, D.L.; Lu, X.; Tu, T.Y.; Solomon, S.; Wang, R.; Rosario, A.; Avalos, C.; Schmolze, D.; Yim, J.; et al. Connecting blood and intratumoral Treg cell activity in predicting future relapse in breast cancer. Nat. Immunol. 2019, 20, 1220–1230. [Google Scholar] [CrossRef] [PubMed]
- Poschke, I.; De Boniface, J.; Mao, Y.; Kiessling, R. Tumor-induced changes in the phenotype of blood-derived and tumor-associated T cells of early stage breast cancer patients. Int. J. Cancer 2011, 131, 1611–1620. [Google Scholar] [CrossRef]
- Lafrenie, R.M.; Speigl, L.; Buckner, C.A.; Pawelec, G.; Conlon, M.S.; Shipp, C. Frequency of Immune Cell Subtypes in Peripheral Blood Correlates With Outcome for Patients With Metastatic Breast Cancer Treated With High-Dose Chemotherapy. Clin. Breast Cancer 2019, 19, 433–442. [Google Scholar] [CrossRef]
- Speigl, L.; Burow, H.; Bailur, J.K.; Janssen, N.; Walter, C.-B.; Pawelec, G.; Shipp, C. CD14+ HLA-DR−/low MDSCs are elevated in the periphery of early-stage breast cancer patients and suppress autologous T cell proliferation. Breast Cancer Res. Treat. 2017, 168, 401–411. [Google Scholar] [CrossRef]
- Bailur, J.K.; Pawelec, G.; Hatse, S.; Brouwers, B.; Smeets, A.; Neven, P.; Laenen, A.; Wildiers, H.; Shipp, C. Immune profiles of elderly breast cancer patients are altered by chemotherapy and relate to clinical frailty. Breast Cancer Res. 2017, 19, 20. [Google Scholar] [CrossRef] [PubMed]
- Campbell, M.J.; Scott, J.; Maecker, H.T.; Park, J.W.; Esserman, L.J. Immune dysfunction and micrometastases in women with breast cancer. Breast Cancer Res. Treat. 2005, 91, 163–171. [Google Scholar] [CrossRef]
- Verronese, E.; Delgado, A.; Valladeauguilemond, J.; Garin, G.; Guillemaut, S.; Tredan, O.; Raycoquard, I.; Bachelot, T.; N’Kodia, A.; Bardin-Dit-Courageot, C.; et al. Immune cell dysfunctions in breast cancer patients detected through whole blood multi-parametric flow cytometry assay. OncoImmunology 2016, 5, e1100791. [Google Scholar] [CrossRef]
- Vudattu, N.K.; Magalhaes, I.; Schmidt, M.; Seyfert-Margolis, V.; Maeurer, M.J. Reduced numbers of IL-7 receptor (CD127) expressing immune cells and IL-7-signaling defects in peripheral blood from patients with breast cancer. Int. J. Cancer 2007, 121, 1512–1519. [Google Scholar] [CrossRef]
- I Gabrilovich, D.; Corak, J.; Ciernik, I.F.; Kavanaugh, D.; Carbone, D.P. Decreased antigen presentation by dendritic cells in patients with breast cancer. Clin. Cancer Res. 1997, 3, 483–490. [Google Scholar]
- Critchley-Thorne, R.J.; Simons, D.L.; Yan, N.; Miyahira, A.K.; Dirbas, F.M.; Johnson, D.L.; Swetter, S.M.; Carlson, R.W.; Fisher, G.A.; Koong, A.; et al. Impaired interferon signaling is a common immune defect in human cancer. Proc. Natl. Acad. Sci. USA 2009, 106, 9010–9015. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Simons, D.L.; Lu, X.; Tu, T.Y.; Avalos, C.; Chang, A.Y.; Dirbas, F.M.; Yim, J.H.; Waisman, J.; Lee, P.P. Breast cancer induces systemic immune changes on cytokine signaling in peripheral blood monocytes and lymphocytes. EBioMedicine 2020, 52, 102631. [Google Scholar] [CrossRef]
- Seif, F.; Khoshmirsafa, M.; Aazami, H.; Mohsenzadegan, M.; Sedighi, G.; Bahar, M. The role of JAK-STAT signaling pathway and its regulators in the fate of T helper cells. Cell Commun. Signal. 2017, 15, 1–13. [Google Scholar] [CrossRef]
- Owen, K.L.; Brockwell, N.K.; Parker, B.S. JAK-STAT Signaling: A Double-Edged Sword of Immune Regulation and Cancer Progression. Cancers 2019, 11, 2002. [Google Scholar] [CrossRef] [PubMed]
- Kuznetsova, M.; Lopatnikova, J.; Shevchenko, J.; Silkov, A.; Maksyutov, A.; Sennikov, S. Cytotoxic Activity and Memory T Cell Subset Distribution of in vitro-Stimulated CD8+ T Cells Specific for HER2/neu Epitopes. Front. Immunol. 2019, 10, 10. [Google Scholar] [CrossRef] [PubMed]
- Gaafar, A.; Aljurf, M.D.; Al-Sulaiman, A.; Iqniebi, A.; Manogaran, P.S.; Mohamed, G.E.H.; Al-Sayed, A.; Alzahrani, H.; Alsharif, F.; Mohareb, F.; et al. Defective γδ T-cell function and granzyme B gene polymorphism in a cohort of newly diagnosed breast cancer patients. Exp. Hematol. 2009, 37, 838–848. [Google Scholar] [CrossRef] [PubMed]
- Inokuma, M.; Rosa, C.D.; Schmitt, C.; Haaland, P.; Siebert, J.; Petry, D.; Tang, M.; Suni, M.A.; Ghanekar, S.A.; Gladding, D.; et al. Functional T Cell Responses to Tumor Antigens in Breast Cancer Patients Have a Distinct Phenotype and Cytokine Signature. J. Immunol. 2007, 179, 2627–2633. [Google Scholar] [CrossRef]
- Bailur, J.K.; Gueckel, B.; Derhovanessian, E.; Pawelec, G. Presence of circulating Her2-reactive CD8 + T-cells is associated with lower frequencies of myeloid-derived suppressor cells and regulatory T cells, and better survival in older breast cancer patients. Breast Cancer Res. 2015, 17, 34. [Google Scholar] [CrossRef]
- Bailur, J.K.; Gueckel, B.; Pawelec, G. Prognostic impact of high levels of circulating plasmacytoid dendritic cells in breast cancer. J. Transl. Med. 2016, 14, 1–10. [Google Scholar] [CrossRef]
- Datta, J.; Fracol, M.; McMillan, M.T.; Berk, E.; Xu, S.; Goodman, N.; Lewis, D.A.; DeMichele, A.; Czerniecki, B.J. Association of Depressed Anti-HER2 T-Helper Type 1 Response With Recurrence in Patients With Completely Treated HER2-Positive Breast Cancer. JAMA Oncol. 2016, 2, 242–246. [Google Scholar] [CrossRef]
- Sewell, H.F.; Halbert, C.F.; Robins, R.A.; Galvin, A.; Chan, S.; Blamey, R.W. Chemotherapy-induced differential changes in lymphocyte subsets and natural-killer-cell function in patients with advanced breast cancer. Int. J. Cancer 1993, 55, 735–738. [Google Scholar] [CrossRef] [PubMed]
- Mozaffari, F.; Lindemalm, C.; Choudhury, A.; Granstam-Björneklett, H.; Helander, I.; Lekander, M.; Mikaelsson, E.; Nilsson, B.; Ojutkangas, M.-L.; Österborg, A.; et al. NK-cell and T-cell functions in patients with breast cancer: Effects of surgery and adjuvant chemo- and radiotherapy. Br. J. Cancer 2007, 97, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Lin, K.-R.; Pang, D.-M.; Jin, Y.-B.; Hu, Q.; Pan, Y.-M.; Cui, J.-H.; Chen, X.-P.; Lin, Y.-X.; Mao, X.-F.; Duan, H.-B.; et al. Circulating CD8+ T-cell repertoires reveal the biological characteristics of tumors and clinical responses to chemotherapy in breast cancer patients. Cancer Immunol. Immunother. 2018, 67, 1743–1752. [Google Scholar] [CrossRef]
- Bauernhofer, T.; Kuss, I.; Friebe-Hoffmann, U.; Baum, A.S.; Dworacki, G.; Vonderhaar, B.K.; Whiteside, T.L. Role of prolactin receptor and CD25 in protection of circulating T lymphocytes from apoptosis in patients with breast cancer. Br. J. Cancer 2003, 88, 1301–1309. [Google Scholar] [CrossRef] [PubMed]
- Gruber, I.V.; El Yousfi, S.; Dürr-Störzer, S.; Wallwiener, D.; Solomayer, E.F.; Fehm, T. Down-Regulation of CD28, TCR-Zeta (Zeta) and up-Regulation of FAS in Peripheral Cytotoxic T-Cells of Primary Breast Cancer Patients. Anticancer. Res. 2008, 28, 779–784. [Google Scholar] [PubMed]
- Shen, M.; Wang, J.; Ren, X. New Insights into Tumor-Infiltrating B Lymphocytes in Breast Cancer: Clinical Impacts and Regulatory Mechanisms. Front. Immunol. 2018, 9, 470. [Google Scholar] [CrossRef] [PubMed]
- Van Der Pompe, G.; Antoni, M.H.; Visser, A.; Heijnen, C.J. Effect of mild acute stress on immune cell distribution and natural killer cell activity in breast cancer patients. Biol. Psychol. 1998, 48, 21–35. [Google Scholar] [CrossRef]
- Tsuda, B.; Miyamoto, A.; Yokoyama, K.; Ogiya, R.; Oshitanai, R.; Terao, M.; Morioka, T.; Niikura, N.; Okamura, T.; Miyako, H.; et al. B-cell populations are expanded in breast cancer patients compared with healthy controls. Breast Cancer 2017, 25, 284–291. [Google Scholar] [CrossRef]
- Kresovich, J.K.; O’Brien, K.M.; Xu, Z.; Weinberg, C.R.; Sandler, D.P.; Taylor, J.A. Prediagnostic Immune Cell Profiles and Breast Cancer. JAMA Netw. Open 2020, 3, e1919536. [Google Scholar] [CrossRef] [PubMed]
- Verma, R.; Foster, R.E.; Horgan, K.; Mounsey, K.; Nixon, H.; Smalle, N.; Hughes, T.A.; Carter, C.R. Lymphocyte depletion and repopulation after chemotherapy for primary breast cancer. Breast Cancer Res. 2016, 18, 10. [Google Scholar] [CrossRef]
- Holl, E.K.; Frazier, V.N.; Landa, K.; Beasley, G.M.; Hwang, E.S.; Nair, S.K. Examining Peripheral and Tumor Cellular Immunome in Patients With Cancer. Front. Immunol. 2019, 10, 1767. [Google Scholar] [CrossRef]
- Wijayahadi, N.; Haron, M.; Stanslas, J.; Yusuf, Z. Changes in Cellular Immunity during Chemotherapy for Primary Breast Cancer with Anthracycline Regimens. J. Chemother. 2007, 19, 716–723. [Google Scholar] [CrossRef]
- Yang, J.; Xu, J.; E, Y.; Sun, T. Predictive and prognostic value of circulating blood lymphocyte subsets in metastatic breast cancer. Cancer Med. 2019, 8, 492–500. [Google Scholar] [CrossRef]
- Mauri, C.; Menon, M. Human regulatory B cells in health and disease: Therapeutic potential. J. Clin. Investig. 2017, 127, 772–779. [Google Scholar] [CrossRef] [PubMed]
- Tsou, P.; Katayama, H.; Ostrin, E.J.; Hanash, S.M. The Emerging Role of B Cells in Tumor Immunity. Cancer Res. 2016, 76, 5597–5601. [Google Scholar] [CrossRef]
- Peng, B.; Ming, Y.; Yang, C. Regulatory B cells: The cutting edge of immune tolerance in kidney transplantation. Cell Death Dis. 2018, 9, 1–13. [Google Scholar] [CrossRef]
- Olkhanud, P.B.; Damdinsuren, B.; Bodogai, M.; Gress, R.E.; Sen, R.; Wejksza, K.; Malchinkhuu, E.; Wersto, R.P.; Biragyn, A. Tumor-Evoked Regulatory B Cells Promote Breast Cancer Metastasis by Converting Resting CD4+ T Cells to T-Regulatory Cells. Cancer Res. 2011, 71, 3505–3515. [Google Scholar] [CrossRef] [PubMed]
- Yeong, J.; Lim, J.C.T.; Lee, B.; Li, H.; Chia, N.; Ong, C.C.H.; Lye, W.K.; Putti, T.C.; Dent, R.; Lim, E.; et al. High Densities of Tumor-Associated Plasma Cells Predict Improved Prognosis in Triple Negative Breast Cancer. Front. Immunol. 2018, 9, 1209. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, M.; Böhm, D.; Von Törne, C.; Steiner, E.; Puhl, A.; Pilch, H.; Lehr, H.-A.; Hengstler, J.G.; Kölbl, H.; Gehrmann, M. The Humoral Immune System Has a Key Prognostic Impact in Node-Negative Breast Cancer. Cancer Res. 2008, 68, 5405–5413. [Google Scholar] [CrossRef]
- Chiossone, L.; Dumas, P.-Y.; Vienne, M.; Vivier, E. Natural killer cells and other innate lymphoid cells in cancer. Nat. Rev. Immunol. 2018, 18, 671–688. [Google Scholar] [CrossRef]
- Roberti, M.P.; Mordoh, J.; Levy, E.M. Biological role of NK cells and immunotherapeutic approaches in breast cancer. Front. Immunol. 2012, 3, 375. [Google Scholar] [CrossRef]
- Shimasaki, N.; Jain, A.; Campana, D. NK cells for cancer immunotherapy. Nat. Rev. Drug Discov. 2020, 19, 200–218. [Google Scholar] [CrossRef]
- Mamessier, E.; Sylvain, A.; Thibult, M.-L.; Houvenaeghel, G.; Jacquemier, J.; Castellano, R.; Gonçalves, A.; André, P.; Romagné, F.; Thibault, G.; et al. Human breast cancer cells enhance self tolerance by promoting evasion from NK cell antitumor immunity. J. Clin. Investig. 2011, 121, 3609–3622. [Google Scholar] [CrossRef]
- Cunningham-Rundles, S.; Filippa, D.A.; Braun, D.W.; Ashikari, H.; Antonelli, P. Natural Cytotoxicity of Peripheral Blood Lymphocytes and Regional Lymph Node Cells in Breast Cancer in Women23. J. Natl. Cancer Inst. 1981, 67, 585–590. [Google Scholar] [CrossRef] [PubMed]
- White, D.; Jones, D.B.; Cooke, T.; Kirkham, N. Natural killer (NK) activity in peripheral blood lymphocytes of patients with benign and malignant breast disease. Br. J. Cancer 1982, 46, 611–616. [Google Scholar] [CrossRef]
- Verma, C.; Kaewkangsadan, V.; Eremin, J.M.; Cowley, G.P.; Ilyas, M.; A El-Sheemy, M.; Eremin, O. Natural killer (NK) cell profiles in blood and tumor in women with large and locally advanced breast cancer (LLABC) and their contribution to a pathological complete response (PCR) in the tumor following neoadjuvant chemotherapy (NAC): Differential restoration of blood profiles by NAC and surgery. J. Transl. Med. 2015, 13, 1–21. [Google Scholar] [CrossRef]
- Bauernhofer, T.; Kuss, I.; Henderson, B.; Baum, A.S.; Whiteside, T.L. Preferential apoptosis of CD56dim natural killer cell subset in patients with cancer. Eur. J. Immunol. 2003, 33, 119–124. [Google Scholar] [CrossRef]
- Nieto-Velázquez, N.G.; Torres-Ramos, Y.D.; Muñoz-Sánchez, J.L.; Espinosa-Godoy, L.; Gómez-Cortés, S.; Moreno, J.; Moreno-Eutimio, M.A. Altered Expression of Natural Cytotoxicity Receptors and NKG2D on Peripheral Blood NK Cell Subsets in Breast Cancer Patients. Transl. Oncol. 2016, 9, 384–391. [Google Scholar] [CrossRef]
- Mamessier, E.; Pradel, L.C.; Thibult, M.-L.; Drevet, C.; Zouine, A.; Jacquemier, J.; Houvenaeghel, G.; Bertucci, F.; Birnbaum, D.; Olive, D. Peripheral Blood NK Cells from Breast Cancer Patients Are Tumor-Induced Composite Subsets. J. Immunol. 2013, 190, 2424–2436. [Google Scholar] [CrossRef]
- Roberti, M.P.; Rocca, Y.S.; Amat, M.; Pampena, M.B.; Loza, J.; Coló, F.; Fabiano, V.; Loza, C.M.; Arriaga, J.M.; Bianchini, M.; et al. IL-2- or IL-15-activated NK cells enhance Cetuximab-mediated activity against triple-negative breast cancer in xenografts and in breast cancer patients. Breast Cancer Res. Treat. 2012, 136, 659–671. [Google Scholar] [CrossRef] [PubMed]
- Freud, A.G.; Mundy-Bosse, B.L.; Yu, J.; Caligiuri, M.A. The Broad Spectrum of Human Natural Killer Cell Diversity. Immunity 2017, 47, 820–833. [Google Scholar] [CrossRef] [PubMed]
- Varchetta, S.; Gibelli, N.; Oliviero, B.; Nardini, E.; Gennari, R.; Gatti, G.; Silva, L.S.; Villani, L.; Tagliabue, E.; Ménard, S.; et al. Elements Related to Heterogeneity of Antibody-Dependent Cell Cytotoxicity in Patients Under Trastuzumab Therapy for Primary Operable Breast Cancer Overexpressing Her2. Cancer Res. 2007, 67, 11991–11999. [Google Scholar] [CrossRef]
- Boero, S.; Morabito, A.; Banelli, B.; Cardinali, B.; Dozin, B.; Lunardi, G.; Piccioli, P.; Lastraioli, S.; Carosio, R.; Salvi, S.; et al. Analysis of in vitro ADCC and clinical response to trastuzumab: Possible relevance of FcγRIIIA/FcγRIIA gene polymorphisms and HER-2 expression levels on breast cancer cell lines. J. Transl. Med. 2015, 13, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Tamura, K.; Shimizu, C.; Hojo, T.; Akashi-Tanaka, S.; Kinoshita, T.; Yonemori, K.; Kouno, T.; Katsumata, N.; Ando, M.; Aogi, K.; et al. FcγR2A and 3A polymorphisms predict clinical outcome of trastuzumab in both neoadjuvant and metastatic settings in patients with HER2-positive breast cancer. Ann. Oncol. 2010, 22, 1302–1307. [Google Scholar] [CrossRef]
- Hurvitz, S.A.; Betting, D.J.; Stern, H.M.; Quinaux, E.; Stinson, J.; Seshagiri, S.; Zhao, Y.; Buyse, M.; Mackey, J.; Driga, A.; et al. Analysis of Fcγ Receptor IIIa and IIa Polymorphisms: Lack of Correlation with Outcome in Trastuzumab-Treated Breast Cancer Patients. Clin. Cancer Res. 2012, 18, 3478–3486. [Google Scholar] [CrossRef]
- Beano, A.; Signorino, E.; Evangelista, A.; Brusa, D.; Mistrangelo, M.; Polimeni, M.A.; Spadi, R.; Donadio, M.; Ciuffreda, L.; Matera, L. Correlation between NK function and response to trastuzumab in metastatic breast cancer patients. J. Transl. Med. 2008, 6, 25. [Google Scholar] [CrossRef] [PubMed]
- Carson, W.E.; Shapiro, C.L.; Crespin, T.R.; Thornton, L.M.; Andersen, B.L. Cellular Immunity in Breast Cancer Patients Completing Taxane Treatment. Clin. Cancer Res. 2004, 10, 3401–3409. [Google Scholar] [CrossRef] [PubMed]
- Kim, R.; Kawai, A.; Wakisaka, M.; Funaoka, Y.; Yasuda, N.; Hidaka, M.; Morita, Y.; Ohtani, S.; Ito, M.; Arihiro, K. A potential role for peripheral natural killer cell activity induced by preoperative chemotherapy in breast cancer patients. Cancer Immunol. Immunother. 2019, 68, 577–585. [Google Scholar] [CrossRef]
- Strayer, D.R.; Carter, W.A.; Brodsky, I. Familial occurrence of breast cancer is associated with reduced natural killer cytotoxicity. Breast Cancer Res. Treat. 1986, 7, 187–192. [Google Scholar] [CrossRef]
- Engblom, C.; Pfirschke, C.; Pittet, C.E.C.P.M.J. The role of myeloid cells in cancer therapies. Nat. Rev. Cancer 2016, 16, 447–462. [Google Scholar] [CrossRef]
- Williams, C.B.; Yeh, E.S.; Soloff, A.C. Tumor-associated macrophages: Unwitting accomplices in breast cancer malignancy. NPJ Breast Cancer 2016, 2, 15025. [Google Scholar] [CrossRef]
- Gardner, A.; Ruffell, B. Dendritic Cells and Cancer Immunity. Trends Immunol. 2016, 37, 855–865. [Google Scholar] [CrossRef] [PubMed]
- Lecot, P.; Sarabi, M.; Abrantes, M.P.; Mussard, J.; Koenderman, L.; Caux, C.; Bendriss-Vermare, N.; Michallet, M.-C. Neutrophil Heterogeneity in Cancer: From Biology to Therapies. Front. Immunol. 2019, 10, 2155. [Google Scholar] [CrossRef] [PubMed]
- Bergenfelz, C.; Leandersson, K. The Generation and Identity of Human Myeloid-Derived Suppressor Cells. Front. Oncol. 2020, 10, 109. [Google Scholar] [CrossRef] [PubMed]
- Wculek, S.K.; Cueto, F.J.; Mujal, A.M.; Melero, I.; Krummel, M.F.; Sancho, D. Dendritic cells in cancer immunology and immunotherapy. Nat. Rev. Immunol. 2020, 20, 7–24. [Google Scholar] [CrossRef]
- Della Bella, S.; Gennaro, M.; Vaccari, M.; Ferraris, C.; Nicola, S.; Riva, A.; Clerici, M.; Greco, M.; Villa, M.L. Altered maturation of peripheral blood dendritic cells in patients with breast cancer. Br. J. Cancer 2003, 89, 1463–1472. [Google Scholar] [CrossRef]
- Pinzon-Charry, A.; Ho, C.S.; Laherty, R.; Maxwell, T.; Walker, D.; Gardiner, R.A.; O’Connor, L.; Pyke, C.; Schmidt, C.; Furnival, C.; et al. A Population of HLA-DR+ Immature Cells Accumulates in the Blood Dendritic Cell Compartment of Patients with Different Types of Cancer. Neoplasia 2005, 7, 1112–1122. [Google Scholar] [CrossRef]
- Satthaporn, S.; Robins, A.; Vassanasiri, W.; El-Sheemy, M.; A Jibril, J.; Clark, D.; Valerio, D.; Eremin, O. Dendritic cells are dysfunctional in patients with operable breast cancer. Cancer Immunol. Immunother. 2004, 53, 510–518. [Google Scholar] [CrossRef]
- Mego, M.; Gao, H.; Cohen, E.N.; Anfossi, S.; Giordano, A.; Tin, S.; Fouad, T.M.; De Giorgi, U.; Giuliano, M.; Woodward, W.A.; et al. Circulating tumor cells (CTCs) are associated with abnormalities in peripheral blood dendritic cells in patients with inflammatory breast cancer. Oncotarget 2016, 8, 35656–35668. [Google Scholar] [CrossRef]
- Sisirak, V.; Faget, J.; Gobert, M.; Goutagny, N.; Vey, N.; Treilleux, I.; Renaudineau, S.; Poyet, G.; Labidi-Galy, S.I.; Goddard-Leon, S.; et al. Impaired IFN-α Production by Plasmacytoid Dendritic Cells Favors Regulatory T-cell Expansion That May Contribute to Breast Cancer Progression. Cancer Res. 2012, 72, 5188–5197. [Google Scholar] [CrossRef]
- Pinzon-Charry, A.; Ho, C.S.K.; Maxwell, T.; A McGuckin, M.; Schmidt, C.; Furnival, C.; Pyke, C.M.; Lopez, A. Numerical and functional defects of blood dendritic cells in early- and late-stage breast cancer. Br. J. Cancer 2007, 97, 1251–1259. [Google Scholar] [CrossRef]
- Bergenfelz, C.; Larsson, A.-M.; Von Stedingk, K.; Gruvberger-Saal, S.; Aaltonen, K.; Jansson, S.; Jernström, H.; Janols, H.; Wullt, M.; Bredberg, A.; et al. Systemic Monocytic-MDSCs Are Generated from Monocytes and Correlate with Disease Progression in Breast Cancer Patients. PLoS ONE 2015, 10, e0127028. [Google Scholar] [CrossRef]
- Hung, C.-H.; Chen, F.-M.; Lin, Y.-C.; Tsai, M.-L.; Wang, S.-L.; Chen, Y.-C.; Chen, Y.-T.; Hou, M.-F. Altered monocyte differentiation and macrophage polarization patterns in patients with breast cancer. BMC Cancer 2018, 18, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Cao, M.; He, Y.; Liu, Y.; Zhang, G.; Yang, C.; Du, Y.; Xu, J.; Hu, J.; Gao, F. Increased circulating M2-like monocytes in patients with breast cancer. Tumor Biol. 2017, 39, 101042831771157. [Google Scholar] [CrossRef] [PubMed]
- Szczerba, B.M.; Castro-Giner, F.; Vetter, M.; Krol, I.; Gkountela, S.; Landin, J.; Scheidmann, M.C.; Donato, C.; Scherrer, R.; Singer, J.; et al. Neutrophils escort circulating tumor cells to enable cell cycle progression. Nat. Cell Biol. 2019, 566, 553–557. [Google Scholar] [CrossRef]
- Safarzadeh, E.; Hashemzadeh, S.; Duijf, P.H.; Mansoori, B.; Khaze, V.; Mohammadi, A.; Kazemi, T.; Yousefi, M.; Asadi, M.; Mohammadi, H.; et al. Circulating myeloid-derived suppressor cells: An independent prognostic factor in patients with breast cancer. J. Cell. Physiol. 2019, 234, 3515–3525. [Google Scholar] [CrossRef]
- Ohki, S.; Shibata, M.; Gonda, K.; Machida, T.; Shimura, T.; Nakamura, I.; Ohtake, T.; Koyama, Y.; Suzuki, S.; Ohto, H.; et al. Circulating myeloid-derived suppressor cells are increased and correlate to immune suppression, inflammation and hypoproteinemia in patients with cancer. Oncol. Rep. 2012, 28, 453–458. [Google Scholar] [CrossRef]
- Diaz-Montero, C.M.; Salem, M.L.; Nishimura, M.I.; Garrett-Mayer, E.; Cole, D.J.; Montero, A.J. Increased circulating myeloid-derived suppressor cells correlate with clinical cancer stage, metastatic tumor burden, and doxorubicin–cyclophosphamide chemotherapy. Cancer Immunol. Immunother. 2008, 58, 49–59. [Google Scholar] [CrossRef]
- Wesolowski, R.; Duggan, M.C.; Stiff, A.; Markowitz, J.; Trikha, P.; Levine, K.M.; Schoenfield, L.; Abdel-Rasoul, M.; Layman, R.; Ramaswamy, B.; et al. Circulating myeloid-derived suppressor cells increase in patients undergoing neo-adjuvant chemotherapy for breast cancer. Cancer Immunol. Immunother. 2017, 66, 1437–1447. [Google Scholar] [CrossRef]
- Larsson, A.-M.; Roxå, A.; Leandersson, K.; Bergenfelz, C. Impact of systemic therapy on circulating leukocyte populations in patients with metastatic breast cancer. Sci. Rep. 2019, 9, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Montero, A.J.; Diaz-Montero, C.M.; Deutsch, Y.E.; Hurley, J.; Koniaris, L.G.; Rumboldt, T.; Yasir, S.; Jorda, M.; Garret-Mayer, E.; Avisar, E.; et al. Phase 2 study of neoadjuvant treatment with NOV-002 in combination with doxorubicin and cyclophosphamide followed by docetaxel in patients with HER-2 negative clinical stage II–IIIc breast cancer. Breast Cancer Res. Treat. 2011, 132, 215–223. [Google Scholar] [CrossRef] [PubMed]
- Baker, K. Organoids Provide an Important Window on Inflammation in Cancer. Cancers 2018, 10, 151. [Google Scholar] [CrossRef]
- Bar-Ephraim, Y.E.; Kretzschmar, K.; Clevers, H. Organoids in immunological research. Nat. Rev. Immunol. 2020, 20, 279–293. [Google Scholar] [CrossRef]
- Belgodere, J.A.; King, C.T.; Bursavich, J.B.; Burow, M.E.; Martin, E.C.; Jung, J.P. Engineering Breast Cancer Microenvironments and 3D Bioprinting. Front. Bioeng. Biotechnol. 2018, 6, 66. [Google Scholar] [CrossRef] [PubMed]
- Homicsko, K. Organoid technology and applications in cancer immunotherapy and precision medicine. Curr. Opin. Biotechnol. 2020, 65, 242–247. [Google Scholar] [CrossRef]
- Brinks, V.; Weinbuch, D.; Baker, M.; Dean, Y.; Stas, P.; Kostense, S.; Rup, B.; Jiskoot, W. Preclinical Models Used for Immunogenicity Prediction of Therapeutic Proteins. Pharm. Res. 2013, 30, 1719–1728. [Google Scholar] [CrossRef]
- Brinks, V.; Jiskoot, W.; Schellekens, H. Immunogenicity of Therapeutic Proteins: The Use of Animal Models. Pharm. Res. 2011, 28, 2379–2385. [Google Scholar] [CrossRef]
- Wagar, L.E.; DiFazio, R.M.; Davis, M.M. Advanced model systems and tools for basic and translational human immunology. Genome Med. 2018, 10, 1–14. [Google Scholar] [CrossRef]
- Seyhan, A.A. Lost in translation: The valley of death across preclinical and clinical divide—Identification of problems and overcoming obstacles. Transl. Med. Commun. 2019, 4, 1–19. [Google Scholar] [CrossRef]
- Suntharalingam, G.; Perry, M.R.; Ward, S.; Brett, S.J.; Castello-Cortes, A.; Brunner, M.D.; Panoskaltsis, N. Cytokine Storm in a Phase 1 Trial of the Anti-CD28 Monoclonal Antibody TGN1412. New Engl. J. Med. 2006, 355, 1018–1028. [Google Scholar] [CrossRef]
- De La Rochere, P.; Guil-Luna, S.; Decaudin, D.; Azar, G.; Sidhu, S.S.; Piaggio, E. Humanized Mice for the Study of Immuno-Oncology. Trends Immunol. 2018, 39, 748–763. [Google Scholar] [CrossRef]
- Giese, C.; Marx, U. Human immunity in vitro—Solving immunogenicity and more. Adv. Drug Deliv. Rev. 2014, 69–70, 103–122. [Google Scholar] [CrossRef]
- Pinto, C.; Estrada, M.F.; Brito, C. In Vitro and Ex Vivo Models—The Tumor Microenvironment in a Flask. In Advances in Experimental Medicine and Biology; Springer International Publishing: New York, NY, USA, 2020; Volume 1219, pp. 431–443. [Google Scholar]
- Fiorini, E.; Veghini, L.; Corbo, V. Modeling Cell Communication in Cancer With Organoids: Making the Complex Simple. Front. Cell Dev. Biol. 2020, 8, 166. [Google Scholar] [CrossRef]
- Drucker, E.; Krapfenbauer, K. Pitfalls and limitations in translation from biomarker discovery to clinical utility in predictive and personalised medicine. EPMA J. 2013, 4, 7. [Google Scholar] [CrossRef]
- Simon, R.; Roychowdhury, S. Implementing personalized cancer genomics in clinical trials. Nat. Rev. Drug Discov. 2013, 12, 358–369. [Google Scholar] [CrossRef]
- Mohammed, H.; Russell, I.A.; Stark, R.; Rueda, O.M.; Hickey, T.E.; Tarulli, G.A.; Serandour, A.A.A.; Birrell, S.N.; Bruna, A.; Saadi, A.; et al. Progesterone receptor modulates ERα action in breast cancer. Nature 2015, 523, 313–317. [Google Scholar] [CrossRef]
- Nguyen, E.V.; Centenera, M.M.; Moldovan, M.; Das, R.; Irani, S.; Vincent, A.D.; Chan, H.; Horvath, L.G.; Lynn, D.J.; Daly, R.J.; et al. Identification of Novel Response and Predictive Biomarkers to Hsp90 Inhibitors Through Proteomic Profiling of Patient-derived Prostate Tumor Explants. Mol. Cell. Proteom. 2018, 17, 1470–1486. [Google Scholar] [CrossRef]
- Powley, I.R.; Patel, M.; Miles, G.; Pringle, H.; Howells, L.; Thomas, A.; Kettleborough, C.; Bryans, J.; Hammonds, T.; Macfarlane, M.; et al. Patient-derived explants (PDEs) as a powerful preclinical platform for anti-cancer drug and biomarker discovery. Br. J. Cancer 2020, 122, 735–744. [Google Scholar] [CrossRef]
- Caicedo-Carvajal, C.E.; Liu, Q.; Goy, A.; Pecora, A.; Suh, K.S. Three-Dimensional Cell Culture Models for Biomarker Discoveries and Cancer Research. Transl. Med. 2012, 1. [Google Scholar] [CrossRef]
- Weigelt, B.; Ghajar, C.M.; Bissell, M.J. The need for complex 3D culture models to unravel novel pathways and identify accurate biomarkers in breast cancer. Adv. Drug Deliv. Rev. 2014, 69–70, 42–51. [Google Scholar] [CrossRef]
- Lopes, N.; Cartaxo, A.L.; Batalha, S.; Franchi Mendes, M.T.; Pinto, C.; Domenici, G.; Rebelo, S.; Oliveira, M.J.; Brito, C. Exploiting 3D Cell Models to Study Macrophage Modulation in the Breast Cancer Microenvironment. In Proceedings of the EACR-AACR-ASPIC Conference, Lisboa, Portugal, 2–4 March 2020. [Google Scholar]
- Bingle, L.; E Lewis, C.; Corke, K.P.; Reed, M.W.R.; Brown, N.J. Macrophages promote angiogenesis in human breast tumor spheroids in vivo. Br. J. Cancer 2005, 94, 101–107. [Google Scholar] [CrossRef]
- Chimal-Ramírez, G.K.; Espinoza-Sánchez, N.A.; Utrera-Barillas, D.; Benítez-Bribiesca, L.; Velázquez, J.R.; Arriaga-Pizano, L.A.; Monroy-García, A.; Reyes-Maldonado, E.; Domínguez-López, M.L.; Piña-Sánchez, P.; et al. MMP1, MMP9, and COX2 Expressions in Promonocytes Are Induced by Breast Cancer Cells and Correlate with Collagen Degradation, Transformation-Like Morphological Changes in MCF-10A Acini, and Tumor Aggressiveness. BioMed Res. Int. 2013, 2013, 1–15. [Google Scholar] [CrossRef]
- Lopes-Coelho, F.; Silva, F.; Gouveia-Fernandes, S.; Martins, C.; Lopes, N.; Domingues, G.; Brito, C.; Almeida, A.M.; A Pereira, S.; Serpa, J. Monocytes as Endothelial Progenitor Cells (EPCs), Another Brick in the Wall to Disentangle Tumor Angiogenesis. Cells 2020, 9, 107. [Google Scholar] [CrossRef]
- Zumwalde, N.A.; Haag, J.D.; Sharma, D.; Mirrielees, J.A.; Wilke, L.G.; Gould, M.N.; Gumperz, J.E. Analysis of Immune Cells from Human Mammary Ductal Epithelial Organoids Reveals Vδ2+ T Cells That Efficiently Target Breast Carcinoma Cells in the Presence of Bisphosphonate. Cancer Prev. Res. 2016, 9, 305–316. [Google Scholar] [CrossRef]
- Augustine, T.N.; Dix-Peek, T.; Duarte, R.; Candy, G.P. Establishment of a heterotypic 3D culture system to evaluate the interaction of TREG lymphocytes and NK cells with breast cancer. J. Immunol. Methods 2015, 426, 1–13. [Google Scholar] [CrossRef]
- Chan, I.S.; Knútsdóttir, H.; Ramakrishnan, G.; Padmanaban, V.; Warrier, M.; Ramirez, J.C.; Dunworth, M.; Zhang, H.; Jaffee, E.M.; Bader, J.S.; et al. Cancer cells educate natural killer cells to a metastasis-promoting cell state. J. Cell Biol. 2020, 219, 219. [Google Scholar] [CrossRef]
- Chatterjee, S.; Bhat, V.; Berdnikov, A.; Liu, J.; Zhang, G.; Buchel, E.; Safneck, J.; Marshall, A.J.; Murphy, L.C.; Postovit, L.-M.; et al. Paracrine Crosstalk between Fibroblasts and ER+ Breast Cancer Cells Creates an IL1β-Enriched Niche that Promotes Tumor Growth. iScience 2019, 19, 388–401. [Google Scholar] [CrossRef]
- Nguyen, M.; De Ninno, A.; Mencattini, A.; Mermet-Meillon, F.; Fornabaio, G.; Evans, S.S.; Cossutta, M.; Khira, Y.; Han, W.; Sirven, P.; et al. Dissecting Effects of Anti-cancer Drugs and Cancer-Associated Fibroblasts by On-Chip Reconstitution of Immunocompetent Tumor Microenvironments. Cell Rep. 2018, 25, 3884–3893.e3. [Google Scholar] [CrossRef]
- Carranza-Rosales, P.; Guzmán-Delgado, N.E.; Carranza-Torres, I.E.; Viveros-Valdez, E.; Morán-Martínez, J. Breast Organotypic Cancer Models. In Current Topics in Microbiology and Immunology; Springer International Publishing: New York, NY, USA, 2018; pp. 1–25. [Google Scholar]
- Grosso, S.H.G.; Katayama, M.L.H.; Roela, R.A.; Nonogaki, S.; Soares, F.A.; Brentani, H.; Lima, L.; Folgueira, M.A.A.K.; Waitzberg, A.F.L.; Pasini, F.S.; et al. Breast cancer tissue slices as a model for evaluation of response to rapamycin. Cell and Tissue Research 2013, 352, 671–684. [Google Scholar] [CrossRef] [PubMed]
- Abreu, S.; Silva, F.; Mendes, R.; Mendes, T.F.; Teixeira, M.; Santo, V.E.; Boghaert, E.R.; Félix, A.; Brito, C. Patient-derived ovarian cancer explants: Preserved viability and histopathological features in long-term agitation-based cultures. Sci. Rep. 2020, 10, 1–13. [Google Scholar] [CrossRef]
- Cartaxo, A.L.; Estrada, M.F.; Domenici, G.; Roque, R.; Silva, F.; Gualda, E.J.; Loza-Alvarez, P.; Sflomos, G.; Brisken, C.; Alves, P.M.; et al. A novel culture method that sustains ERα signaling in human breast cancer tissue microstructures. J. Exp. Clin. Cancer Res. 2020, 39, 1–14. [Google Scholar] [CrossRef]
- Aung, A.; Kumar, V.; Theprungsirikul, J.; Davey, S.K.; Varghese, S. An Engineered Tumor-on-a-Chip Device with Breast Cancer–Immune Cell Interactions for Assessing T-cell Recruitment. Cancer Res. 2019, 80, 263–275. [Google Scholar] [CrossRef]
- Ayuso, J.M.; Truttschel, R.; Gong, M.M.; Humayun, M.; Virumbrales-Munoz, M.; Vitek, R.; Felder, M.; Gillies, S.D.; Sondel, P.; Wisinski, K.B.; et al. Evaluating natural killer cell cytotoxicity against solid tumors using a microfluidic model. OncoImmunology 2019, 8, 1553477. [Google Scholar] [CrossRef] [PubMed]
- Del Bano, J.; Florès-Florès, R.; Josselin, E.; Goubard, A.; Ganier, L.; Castellano, R.; Chames, P.; Baty, D.; Kerfelec, B. A Bispecific Antibody-Based Approach for Targeting Mesothelin in Triple Negative Breast Cancer. Front. Immunol. 2019, 10, 1593. [Google Scholar] [CrossRef]
- Frank, A.-C.; Ebersberger, S.; Fink, A.F.; Lampe, S.; Weigert, A.; Schmid, T.; Ebersberger, I.; Syed, S.N.; Brüne, B. Apoptotic tumor cell-derived microRNA-375 uses CD36 to alter the tumor-associated macrophage phenotype. Nat. Commun. 2019, 10, 1–18. [Google Scholar] [CrossRef]
- Ksiazkiewicz, M.; Gottfried, E.; Kreutz, M.; Mack, M.; Hofstaedter, F.; Kunz-Schughart, L.A. Importance of CCL2-CCR2A/2B signaling for monocyte migration into spheroids of breast cancer-derived fibroblasts. Immunobiol. 2010, 215, 737–747. [Google Scholar] [CrossRef]
- Li, L.; Chen, J.; Xiong, G.; Clair, D.K.S.; Xu, W.; Xu, R. Increased ROS production in non-polarized mammary epithelial cells induces monocyte infiltration in 3D culture. J. Cell Sci. 2017, 130, 190–202. [Google Scholar] [CrossRef]
- Olesch, C.; Sha, W.; Angioni, C.; Sha, L.K.; Açaf, E.; Patrignani, P.; Jakobsson, P.-J.; Radeke, H.H.; Grösch, S.; Geisslinger, G.; et al. MPGES-1-derived PGE2 suppresses CD80 expression on tumor-associated phagocytes to inhibit anti-tumor immune responses in breast cancer. Oncotarget 2015, 6, 10284–10296. [Google Scholar] [CrossRef]
- Wallstabe, L.; Göttlich, C.; Nelke, L.C.; Kühnemundt, J.; Schwarz, T.; Nerreter, T.; Einsele, H.; Walles, H.; Dandekar, G.; Nietzer, S.L.; et al. ROR1-CAR T cells are effective against lung and breast cancer in advanced microphysiologic 3D tumor models. JCI Insight 2019, 4. [Google Scholar] [CrossRef] [PubMed]
- Morsink, M.A.J.; Willemen, N.G.A.; Leijten, J.; Bansal, R.; Shin, S.R. Immune Organs and Immune Cells on a Chip: An Overview of Biomedical Applications. Micromachines 2020, 11, 849. [Google Scholar] [CrossRef]
- Giese, C.; Lubitz, A.; Demmler, C.D.; Reuschel, J.; Bergner, K.; Marx, U. Immunological substance testing on human lymphatic micro-organoids in vitro. J. Biotechnol. 2010, 148, 38–45. [Google Scholar] [CrossRef] [PubMed]
- Rigat-Brugarolas, L.G.; Elizalde-Torrent, A.; Bernabeu, M.; De Niz, M.; Martin-Jaular, L.; Fernandez-Becerra, C.; Homs-Corbera, A.; Samitier, J.; Del Portillo, H.A. A functional microengineered model of the human splenon-on-a-chip. Lab Chip 2014, 14, 1715–1724. [Google Scholar] [CrossRef] [PubMed]
- Chou, D.B.; Frismantas, V.; Milton, Y.; David, R.; Pop-Damkov, P.; Ferguson, D.; Macdonald, A.; Bölükbaşı, Ö.V.; Joyce, C.E.; Teixeira, L.S.M.; et al. On-chip recapitulation of clinical bone marrow toxicities and patient-specific pathophysiology. Nat. Biomed. Eng. 2020, 4, 394–406. [Google Scholar] [CrossRef] [PubMed]
- Tajima, A.; Pradhan, I.; Trucco, M.; Fan, Y. Restoration of Thymus Function with Bioengineered Thymus Organoids. Curr. Stem Cell Rep. 2016, 2, 128–139. [Google Scholar] [CrossRef]
- Ramadan, Q.; Ting, F.C.W. In vitro micro-physiological immune-competent model of the human skin. Lab Chip 2016, 16, 1899–1908. [Google Scholar] [CrossRef]
- Huh, D.; Leslie, D.C.; Matthews, B.D.; Fraser, J.P.; Jurek, S.; Hamilton, G.A.; Thorneloe, K.S.; McAlexander, M.A.; Ingber, D.E. A Human Disease Model of Drug Toxicity–Induced Pulmonary Edema in a Lung-on-a-Chip Microdevice. Sci. Transl. Med. 2012, 4, 159ra147. [Google Scholar] [CrossRef]
- Shah, P.; Fritz, J.V.; Glaab, E.; Desai, M.S.; Greenhalgh, K.; Frachet, A.; Niegowska, M.; Estes, M.; Jäger, C.; Seguin-Devaux, C.; et al. A microfluidics-based in vitro model of the gastrointestinal human–microbe interface. Nat. Commun. 2016, 7, 11535. [Google Scholar] [CrossRef]
- Gröger, M.; Rennert, K.; Giszas, B.; Weiß, E.; Dinger, J.; Funke, H.; Kiehntopf, M.; Peters, F.T.; Lupp, A.; Bauer, M.; et al. Monocyte-induced recovery of inflammation-associated hepatocellular dysfunction in a biochip-based human liver model. Sci. Rep. 2016, 6, 21868. [Google Scholar] [CrossRef] [PubMed]
- Cupedo, T.; Stroock, A.D.; Coles, M.C. Application of tissue engineering to the immune system: Development of artificial lymph nodes. Front. Immunol. 2012, 3, 343. [Google Scholar] [CrossRef] [PubMed]
- Radhakrishnan, J.; Varadaraj, S.; Dash, S.K.; Sharma, A.; Verma, R.S. Organotypic cancer tissue models for drug screening: 3D constructs, bioprinting and microfluidic chips. Drug Discov. Today 2020, 25, 879–890. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, E.; Palma, C.; Vesentini, S.; Occhetta, P.; Rasponi, M. Integrating Biosensors in Organs-on-Chip Devices: A Perspective on Current Strategies to Monitor Microphysiological Systems. Biosensors 2020, 10, 110. [Google Scholar] [CrossRef]
- Miller, C.P.; Shin, W.; Ahn, E.H.; Kim, H.J.; Kim, D.-H. Engineering Microphysiological Immune System Responses on Chips. Trends Biotechnol. 2020, 38, 857–872. [Google Scholar] [CrossRef]
- Sun, W.; Luo, Z.; Lee, J.; Kim, H.-J.; Lee, K.; Tebon, P.; Feng, Y.; Dokmeci, M.R.; Sengupta, S.; Khademhosseini, A. Organ-on-a-Chip for Cancer and Immune Organs Modeling. Adv. Heal. Mater. 2019, 8, e1801363. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).