Examining Associations Among Orthorexia Nervosa and Anthropometric Factors and Lifestyle Habits in an Italian University Community
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Anthropologic and Sociodemographic and Lifestyle Data
2.3. Assessment of ON Tendency
2.4. An Assessment of the Adherence to the Mediterranean Diet Pattern
2.5. Statistical Analysis
3. Results
3.1. Sample Characteristics
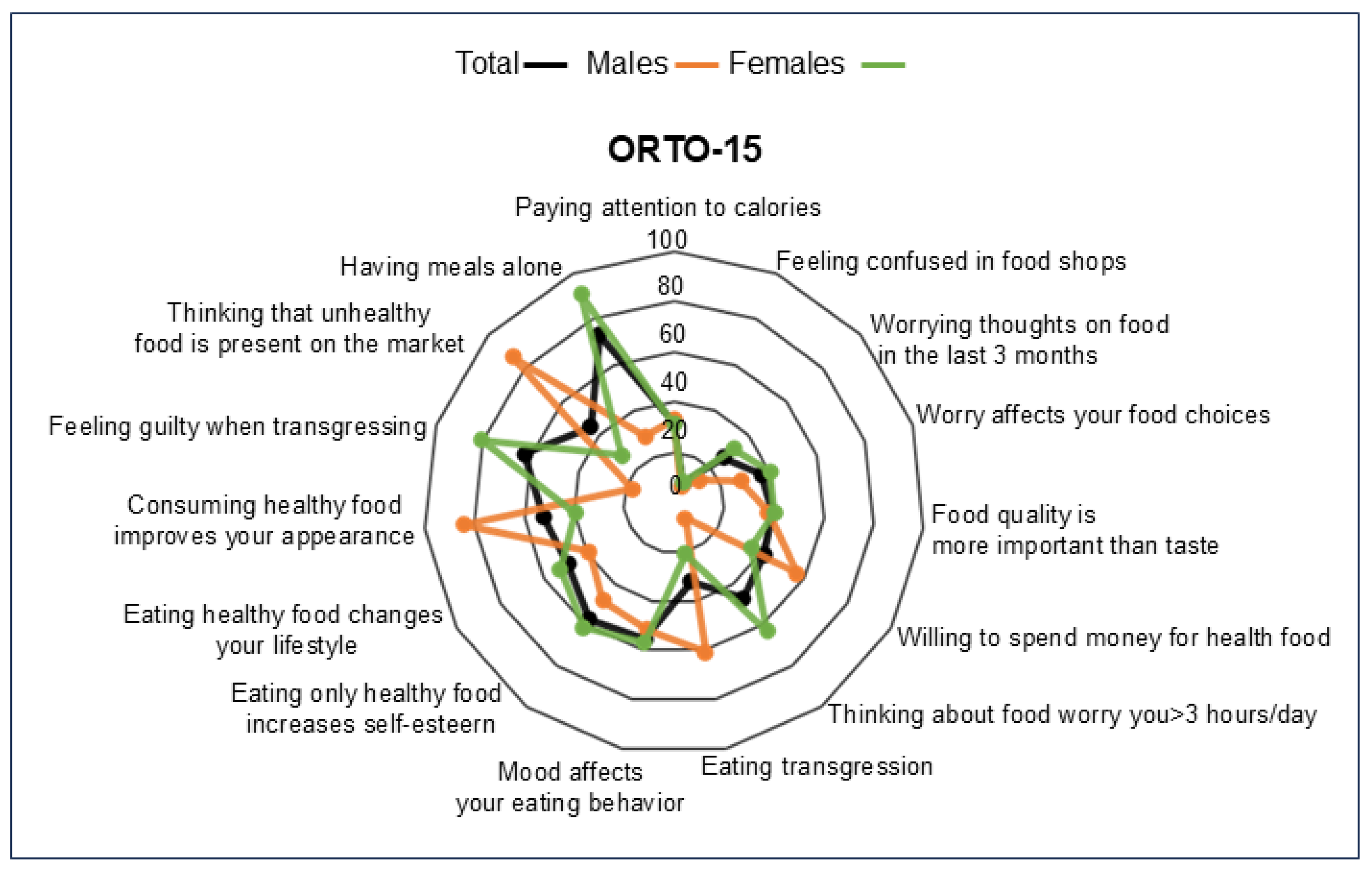
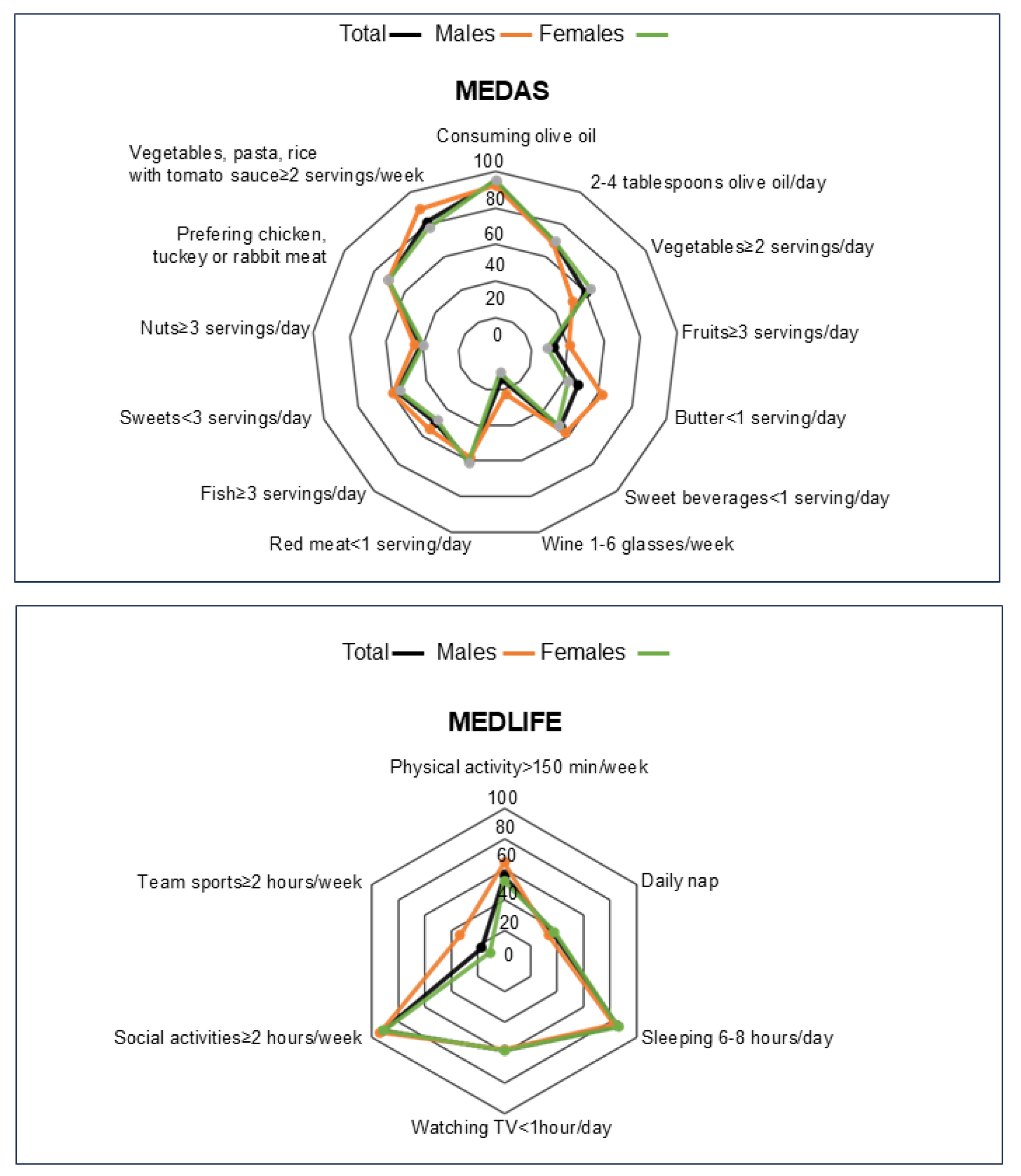
3.2. ORTO-15, MEDAS and MEDLIFE Questionnaires Scores in the Population
3.3. Orthorexia Nervosa Tendency in Our Sample Population
3.4. Influence of Anthropometric Parameters and LifeStyle Habits on the Tendency Toward Orthorexia Nervosa
3.5. Association Between ON Tendency and Different Parameters
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bratman, S. The health food eating disorder. Yoga J. 1997, 42, 50. [Google Scholar]
- Fugh-Berman, A. Health Food Junkies: Orthorexia Nervosa: Overcoming the Obsession with Healthful Eating. JAMA-J. Am. Med. Assoc. 2001, 285, 2255. [Google Scholar] [CrossRef]
- Koven, N.S.; Abry, A.W. The clinical basis of orthorexia nervosa: Emerging perspectives. Neuropsychiatr. Dis. Treat. 2015, 11, 385–394. [Google Scholar] [CrossRef] [PubMed]
- Strahler, J.; Hermann, A.; Walter, B.; Stark, R. Orthorexia nervosa: A behavioral complex or a psychological condition? J. Behav. Addict. 2018, 7, 1143–1156. [Google Scholar] [CrossRef]
- Horovitz, O.; Argyrides, M. Orthorexia and Orthorexia Nervosa: A Comprehensive Examination of Prevalence, Risk Factors, Diagnosis, and Treatment. Nutrients 2023, 15, 3851. [Google Scholar] [CrossRef]
- Association, A.P. Feeding and Eating Disorders: Dsm-5(r) Selections, 1st ed.; American Psychiatric Publishing: Washington, DC, USA, 2015. [Google Scholar]
- Domaszewski, P.; Rogowska, A.M.; Żylak, K. Examining Associations Between Fasting Behavior, Orthorexia Nervosa, and Eating Disorders. Nutrients 2024, 16, 4275. [Google Scholar] [CrossRef]
- Uriegas, N.A.; Winkelmann, Z.K.; Pritchett, K.; Torres-McGehee, T.M. Examining Eating Attitudes and Behaviors in Collegiate Athletes, the Association Between Orthorexia Nervosa and Eating Disorders. Front. Nutr. 2021, 8, 763838. [Google Scholar] [CrossRef]
- Yargic, M.P.; Celen, M.C. Assessing Orthorexia Nervosa by Questionnaires. In Eating Disorders; Patel, V.B., Preedy, V.R., Eds.; Springer International Publishing: Cham, Switzerland, 2023; pp. 1435–1449. [Google Scholar]
- Donini, L.M.; Marsili, D.; Graziani, M.P.; Imbriale, M.; Cannella, C. Orthorexia nervosa: Validation of a diagnosis questionnaire. Eat. Weight Disord. 2005, 10, e28–e32. [Google Scholar] [CrossRef]
- Pontillo, M.; Zanna, V.; Demaria, F.; Averna, R.; Di Vincenzo, C.; De Biase, M.; Di Luzio, M.; Foti, B.; Tata, M.C.; Vicari, S. Orthorexia Nervosa, Eating Disorders, and Obsessive-Compulsive Disorder: A Selective Review of the Last Seven Years. J. Clin. Med. 2022, 11, 6134. [Google Scholar] [CrossRef]
- Donini, L.M.; Marsili, D.; Graziani, M.P.; Imbriale, M.; Cannella, C. Orthorexia nervosa: A preliminary study with a proposal for diagnosis and an attempt to measure the dimension of the phenomenon. Eat. Weight Disord. 2004, 9, 151–157. [Google Scholar] [CrossRef]
- Segura-Garcia, C.; Ramacciotti, C.; Rania, M.; Aloi, M.; Caroleo, M.; Bruni, A.; Gazzarrini, D.; Sinopoli, F.; De Fazio, P. The prevalence of orthorexia nervosa among eating disorder patients after treatment. Eat. Weight Disord. 2015, 20, 161–166. [Google Scholar] [CrossRef] [PubMed]
- Barnes, M.A.; Caltabiano, M.L. The interrelationship between orthorexia nervosa, perfectionism, body image and attachment style. Eat. Weight Disord. 2017, 22, 177–184. [Google Scholar] [CrossRef] [PubMed]
- Depa, J.; Barrada, J.R.; Roncero, M. Are the Motives for Food Choices Different in Orthorexia Nervosa and Healthy Orthorexia? Nutrients 2019, 11, 697. [Google Scholar] [CrossRef] [PubMed]
- Di Daniele, N.; Noce, A.; Vidiri, M.F.; Moriconi, E.; Marrone, G.; Annicchiarico-Petruzzelli, M.; D’Urso, G.; Tesauro, M.; Rovella, V.; De Lorenzo, A. Impact of Mediterranean diet on metabolic syndrome, cancer and longevity. Oncotarget 2017, 8, 8947–8979. [Google Scholar] [CrossRef]
- Gardener, H.; Caunca, M.R. Mediterranean Diet in Preventing Neurodegenerative Diseases. Curr. Nutr. Rep. 2018, 7, 10–20. [Google Scholar] [CrossRef]
- Martínez-González, M.A.; Gea, A.; Ruiz-Canela, M. The Mediterranean Diet and Cardiovascular Health. Circ. Res. 2019, 124, 779–798. [Google Scholar] [CrossRef]
- Lassale, C.; Batty, G.D.; Baghdadli, A.; Jacka, F.; Sanchez-Villegas, A.; Kivimaki, M.; Akbaraly, T. Healthy dietary indices and risk of depressive outcomes: A systematic review and meta-analysis of observational studies. Mol. Psychiatry 2019, 24, 965–986. [Google Scholar] [CrossRef]
- Leone, A.; Martinez-Gonzalez, M.A.; Lahortiga-Ramos, F.; Molero Santos, P.; Bertoli, S.; Battezzati, A.; Bes-Rastrollo, M. Adherence to the Mediterranean dietary pattern and incidence of anorexia and bulimia nervosa in women: The SUN cohort. Nutrition 2018, 54, 19–25. [Google Scholar] [CrossRef]
- Bertoli, S.; Spadafranca, A.; Bes-Rastrollo, M.; Martinez-Gonzalez, M.A.; Ponissi, V.; Beggio, V.; Leone, A.; Battezzati, A. Adherence to the Mediterranean diet is inversely related to binge eating disorder in patients seeking a weight loss program. Clin. Nutr. 2015, 34, 107–114. [Google Scholar] [CrossRef]
- Martinovic, D.; Tokic, D.; Martinovic, L.; Vilovic, M.; Vrdoljak, J.; Kumric, M.; Bukic, J.; Ticinovic Kurir, T.; Tavra, M.; Bozic, J. Adherence to Mediterranean Diet and Tendency to Orthorexia Nervosa in Professional Athletes. Nutrients 2022, 14, 237. [Google Scholar] [CrossRef]
- Ramacciotti, C.E.; Perrone, P.; Coli, E.; Burgalassi, A.; Conversano, C.; Massimetti, G.; Dell’Osso, L. Orthorexia nervosa in the general population: A preliminary screening using a self-administered questionnaire (ORTO-15). Eat. Weight Disord. 2011, 16, e127–e130. [Google Scholar] [CrossRef] [PubMed]
- Gleaves, D.; Graham, E.; Ambwani, S. Measuring “Orthorexia.” Development of the Eating Habits Questionnaire. Int. J. Educ. Psychol. Assess. 2013, 12, 1–18. [Google Scholar]
- García-Conesa, M.T.; Philippou, E.; Pafilas, C.; Massaro, M.; Quarta, S.; Andrade, V.; Jorge, R.; Chervenkov, M.; Ivanova, T.; Dimitrova, D.; et al. Exploring the Validity of the 14-Item Mediterranean Diet Adherence Screener (MEDAS): A Cross-National Study in Seven European Countries around the Mediterranean Region. Nutrients 2020, 12, 2960. [Google Scholar] [CrossRef] [PubMed]
- Sotos-Prieto, M.; Santos-Beneit, G.; Bodega, P.; Pocock, S.; Mattei, J.; Peñalvo, J.L. Validation Of A Questionnaire To Measure Overall Mediterranean Lifestyle Habits For Research Application: The Mediterranean Lifestyle Index (Medlife). Nutr. Hosp. 2015, 32, 1153–1163. [Google Scholar] [CrossRef] [PubMed]
- Niedzielski, A.; Kaźmierczak-Wojtaś, N. Prevalence of Orthorexia Nervosa and Its Diagnostic Tools-A Literature Review. Int. J. Environ. Res. Public Health 2021, 18, 5488. [Google Scholar] [CrossRef]
- Donini, L.M.; Barrada, J.R.; Barthels, F.; Dunn, T.M.; Babeau, C.; Brytek-Matera, A.; Cena, H.; Cerolini, S.; Cho, H.H.; Coimbra, M.; et al. A consensus document on definition and diagnostic criteria for orthorexia nervosa. Eat. Weight Disord. 2022, 27, 3695–3711. [Google Scholar] [CrossRef]
- Association, A.P. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- World Health Organization. ICD-10: International Statistical Classification of Diseases and Related Health Problems, 10th revision; World Health Organization: Geneva, Switzerland, 2004. [Google Scholar]
- Segura-García, C.; Papaianni, M.C.; Caglioti, F.; Procopio, L.; Nisticò, C.G.; Bombardiere, L.; Ammendolia, A.; Rizza, P.; De Fazio, P.; Capranica, L. Orthorexia nervosa: A frequent eating disordered behavior in athletes. Eat. Weight Disord. 2012, 17, e226–e233. [Google Scholar] [CrossRef]
- Dunn, T.M.; Gibbs, J.; Whitney, N.; Starosta, A. Prevalence of orthorexia nervosa is less than 1 %: Data from a US sample. Eat. Weight Disord. 2017, 22, 185–192. [Google Scholar] [CrossRef]
- Turner, P.G.; Lefevre, C.E. Instagram use is linked to increased symptoms of orthorexia nervosa. Eat. Weight Disord. 2017, 22, 277–284. [Google Scholar] [CrossRef]
- Jerez, F.T.; Hernández, R.L.; Valdés-Badilla, P.; Pacheco, P.E. Prevalence of orthorexic behaviour in high school students of Temuco. Revista Chilena de Nutricion 2015, 42, 41–44. [Google Scholar]
- Fidan, T.; Ertekin, V.; Işikay, S.; Kirpinar, I. Prevalence of orthorexia among medical students in Erzurum, Turkey. Compr. Psychiatry 2010, 51, 49–54. [Google Scholar] [CrossRef]
- Brytek-Matera, A.; Donini, L.M.; Krupa, M.; Poggiogalle, E.; Hay, P. Orthorexia nervosa and self-attitudinal aspects of body image in female and male university students. J. Eat. Disord. 2015, 3, 2. [Google Scholar] [CrossRef] [PubMed]
- Dell’Osso, L.; Abelli, M.; Carpita, B.; Massimetti, G.; Pini, S.; Rivetti, L.; Gorrasi, F.; Tognetti, R.; Ricca, V.; Carmassi, C. Orthorexia nervosa in a sample of Italian university population. Riv. Psichiatr. 2016, 51, 190–196. [Google Scholar] [CrossRef] [PubMed]
- Luck-Sikorski, C.; Jung, F.; Schlosser, K.; Riedel-Heller, S.G. Is orthorexic behavior common in the general public? A large representative study in Germany. Eat. Weight Disord. 2019, 24, 267–273. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, R. Is the prevalence of orthorexia nervosa in an Australian university population 6.5%? Eat. Weight Disord. 2018, 23, 453–458. [Google Scholar] [CrossRef]
- Alleva, J.M.; Tylka, T.L. Body functionality: A review of the literature. Body Image 2021, 36, 149–171. [Google Scholar] [CrossRef]
- Linardon, J.; McClure, Z.; Tylka, T.L.; Fuller-Tyszkiewicz, M. Body appreciation and its psychological correlates: A systematic review and meta-analysis. Body Image 2022, 42, 287–296. [Google Scholar] [CrossRef]
- Aksoydan, E.; Camci, N. Prevalence of orthorexia nervosa among Turkish performance artists. Eat. Weight Disord. 2009, 14, 33–37. [Google Scholar] [CrossRef]
- Almeida, C.; Vieira Borba, V.; Santos, L. Orthorexia nervosa in a sample of Portuguese fitness participants. Eat. Weight Disord. 2018, 23, 443–451. [Google Scholar] [CrossRef]
- Arusoğlu, G.; Kabakçi, E.; Köksal, G.; Merdol, T.K. Orthorexia nervosa and adaptation of ORTO-11 into Turkish. Turk. Psikiyatri Dergisi Turk. J. Psychiatry 2008, 19, 283–291. [Google Scholar]
- Depa, J.; Schweizer, J.; Bekers, S.K.; Hilzendegen, C.; Stroebele-Benschop, N. Prevalence and predictors of orthorexia nervosa among German students using the 21-item-DOS. Eat. Weight Disord. 2017, 22, 193–199. [Google Scholar] [CrossRef] [PubMed]
- Lakritz, C.; Tete, N.; Iceta, S.; Lafraire, J. Orthorexia nervosa tendencies and risk of eating disorders among culinary arts students: A comparative study with dietetics students. J. Hum. Nutr. Diet. 2024, 37, 1547–1557. [Google Scholar] [CrossRef] [PubMed]
- McInerney-Ernst, E.M. Orthorexia Nervosa: Real Construct or Newest Social Trend? University of Missouri: Kansas City, MO, USA, 2011. [Google Scholar]
- Rudolph, S.; Göring, A.; Jetzke, M.; Großarth, D.; Rudolph, H. The Prevalence of Orthorectic Eating Behavior of Student Athletes. Dtsch. Z. Für Sportmed. 2017, 68, 10–13. [Google Scholar] [CrossRef]
- Stutts, L.A. It’s complicated: The relationship between orthorexia and weight/shape concerns, eating behaviors, and mood. Eat. Behav. 2020, 39, 101444. [Google Scholar] [CrossRef]
- Guasch-Ferre, M.; Willett, W.C. The Mediterranean diet and health: A comprehensive overview. J. Intern. Med. 2021, 290, 549–566. [Google Scholar] [CrossRef]
- Augimeri, G.; Avolio, E.; Caparello, G.; Galluccio, A.; De Rose, D.; Vivacqua, A.; Morelli, C.; Barone, I.; Catalano, S.; Andò, S.; et al. Serum from Adolescents with High Polyphenol Intake Exhibits Improved Lipid Profile and Prevents Lipid Accumulation in HepG2 Human Liver Cells. Oxidative Med. Cell. Longev. 2023, 2023, 1555942. [Google Scholar] [CrossRef]
- Augimeri, G.; Bonofiglio, D. The Mediterranean Diet as a Source of Natural Compounds: Does It Represent a Protective Choice against Cancer? Pharmaceuticals 2021, 14, 920. [Google Scholar] [CrossRef]
- Augimeri, G.; Fiorillo, M.; Caparello, G.; Ceraudo, F.; Avolio, E.; Morelli, C.; Barone, I.; Catalano, S.; Andò, S.; Giordano, C.; et al. Impact of COVID-19 Lockdown on Metabolic/Inflammatory Profile in Adolescents: Cellular Studies and Predictive Biomarkers. J. Clin. Endocrinol. Metab. 2024, 109, 711–721. [Google Scholar] [CrossRef]
- Augimeri, G.; Galluccio, A.; Caparello, G.; Avolio, E.; La Russa, D.; De Rose, D.; Morelli, C.; Barone, I.; Catalano, S.; Andò, S.; et al. Potential Antioxidant and Anti-Inflammatory Properties of Serum from Healthy Adolescents with Optimal Mediterranean Diet Adherence: Findings from DIMENU Cross-Sectional Study. Antioxidants 2021, 10, 1172. [Google Scholar] [CrossRef]
- Augimeri, G.; Montalto, F.I.; Giordano, C.; Barone, I.; Lanzino, M.; Catalano, S.; Andò, S.; De Amicis, F.; Bonofiglio, D. Nutraceuticals in the Mediterranean Diet: Potential Avenues for Breast Cancer Treatment. Nutrients 2021, 13, 2557. [Google Scholar] [CrossRef]
- Ceraudo, F.; Caparello, G.; Galluccio, A.; Avolio, E.; Augimeri, G.; De Rose, D.; Vivacqua, A.; Morelli, C.; Barone, I.; Catalano, S.; et al. Impact of Mediterranean Diet Food Choices and Physical Activity on Serum Metabolic Profile in Healthy Adolescents: Findings from the DIMENU Project. Nutrients 2022, 14, 881. [Google Scholar] [CrossRef] [PubMed]
- Fan, H.; Wang, Y.; Ren, Z.; Liu, X.; Zhao, J.; Yuan, Y.; Fei, X.; Song, X.; Wang, F.; Liang, B. Mediterranean diet lowers all-cause and cardiovascular mortality for patients with metabolic syndrome. Diabetol. Metab. Syndr. 2023, 15, 107. [Google Scholar] [CrossRef] [PubMed]
- Giugliano, D.; Esposito, K. Mediterranean diet and metabolic diseases. Curr. Opin. Lipidol. 2008, 19, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Godos, J. Decreasing adherence to the Mediterranean diet: Health and environmental foe. Int. J. Food Sci. Nutr. 2023, 74, 797–798. [Google Scholar] [CrossRef]
- Augimeri, G.; Soto, M.; Ceraudo, F.; Caparello, G.; Villegas Figueroa, M.; Cesario, M.; Caputi, L.S.; Calderon, B.; Bonofiglio, D. Comparing the Dietary Habits and the Food Choices Between Italian and Dominican Adult Populations: Focus on Fruit and Vegetable Intakes and Their Association with Skin Carotenoid Levels. Foods 2024, 13, 3323. [Google Scholar] [CrossRef]
- Augimeri, G.; Soto, M.; Ceraudo, F.; Caparello, G.; Villegas Figueroa, M.; Cesario, M.; Caputi, L.S.; Calderón, B.; Bonofiglio, D. Differences of skin carotenoids and adherence to the Mediterranean Diet pattern in adults from Southern Italy and Dominican Republic. J. Transl. Med. 2024, 22, 424. [Google Scholar] [CrossRef]
- Rozmiarek, M.; Grajek, M.; Krupa-Kotara, K.; Malchrowicz-Mosko, E. Orthorectic behavior among students and motivation for physical activity, dietary habits, and restrictive eating. Front. Nutr. 2024, 11, 1367767. [Google Scholar] [CrossRef]
- Strahler, J.; Wachten, H.; Neuhofer, S.; Zimmermann, P. Psychological Correlates of Excessive Healthy and Orthorexic Eating: Emotion Regulation, Attachment, and Anxious-Depressive-Stress Symptomatology. Front. Nutr. 2022, 9, 817047. [Google Scholar] [CrossRef]
- Strahler, J. Trait mindfulness differentiates the interest in healthy diet from orthorexia nervosa. Eat. Weight Disord. 2021, 26, 993–998. [Google Scholar] [CrossRef]
- Anastasiades, E.; Argyrides, M. Healthy orthorexia vs orthorexia nervosa: Associations with body appreciation, functionality appreciation, intuitive eating and embodiment. Eat. Weight Disord. 2022, 27, 3197–3206. [Google Scholar] [CrossRef]
- Brodock, J.L.; Hopfer, H.; Masterson, T.D.; Hayes, J.E. Orthorexia Nervosa and Healthy Orthorexia in a Physically Active North American Population. Nutrients 2024, 16, 1107. [Google Scholar] [CrossRef]
| Characteristics | Total Sample | Men | Women |
|---|---|---|---|
| Number of participants (%) | 500 | 143 (28.6) | 357 (71.4) |
| Age (years) mean ± SD | 23.48 ± 5.08 | 23.10 ± 4.52 | 23.64 ± 5.29 |
| BMI (kg/m2) mean ± SD | 22.91 ± 3.95 | 24.37 ± 3.88 | 22.14 ± 3.80 |
| Nationality, n (%) | |||
| Italian | 492 (98.4) | 140 (97.9) | 352 (98.6) |
| International | 8 (1.6) | 3 (2.10) | 5 (1.4) |
| Residential distribution, n (%) | |||
| Living on-campus | 84 (16.8) | 23 (16.08) | 61 (17.09) |
| Living off-campus | 289 (57.8) | 86 (60.14) | 203 (56.86) |
| Commuter students | 127 (25.4) | 34 (23.78) | 93 (26.05) |
| Faculty, n (%) | |||
| Health sciences | 338 (67.6) | 91 (63.64) | 247 (69.19) |
| Engineering and technological sciences | 37 (7.4) | 23 (16.08) | 14 (3.92) |
| Economic and legal sciences | 18 (3.6) | 7 (4.90) | 11 (3.08) |
| Social and political sciences | 25 (5) | 7 (4.90) | 18 (5.04) |
| Natural sciences | 37 (7.4) | 8 (5.59) | 29 (8.13) |
| Humanities | 45 (9) | 7 (4.90) | 38 (10.64) |
| Lunch location, n (%) | |||
| Home | 192 (38.4) | 35 (24.47) | 157 (43.98) |
| University canteen | 50 (10) | 19 (13.29) | 31 (8.68) |
| Home and university canteen | 252 (50.4) | 88 (61.54) | 164 (45.94) |
| Bar | 3 (0.60) | 1 (0.70) | 2 (0.56) |
| Skipped lunch | 3 (0.60) | 0 | 3 (0.84) |
| ORTO-15 Score | Total Sample, n (%) | Men, n (%) | Women, n (%) | p-Value |
|---|---|---|---|---|
| <35 | 99 (19.8) | 23 (16.08) | 76 (21.28) | 0.09 |
| >35, <40 | 112 (24.4) | 25 (17.48) | 97 (27.17) | |
| >40 | 279 (55.8) | 95 (66.43) | 184 (51.54) |
| Scores | Total Sample | Men | Women | p-Value |
|---|---|---|---|---|
| ORTO-15 Score Mean ± SD | 39.63 ± 6.35 | 41.06 ± 5.58 | 39.06 ± 6.56 | 0.001 |
| MEDAS Mean ± SD | 7.32 ± 2.24 | 7.72 ± 2.47 | 7.15 ± 2.12 | 0.009 |
| MEDLIFE Mean ± SD | 3.45 ± 1.17 | 3.66 ± 1.24 | 3.36 ± 1.13 | 0.01 |
| Characteristics | n | % | Minimum–Maximum | ORTO-15 Score | p-Value |
|---|---|---|---|---|---|
| BMI | |||||
| Underweight | 40 | 8 | 30–53 | 42.3 ± 5.53 | 0.003 |
| Normal weight | 354 | 70.8 | 20–53 | 39.71 ± 6.22 | |
| Overweight | 77 | 15.4 | 22–50 | 39.01 ± 6.16 | |
| Obesity | 29 | 5.8 | 24–60 | 36.72 ± 8.18 | |
| Faculty | |||||
| Health sciences | 338 | 67.6 | 22–53 | 40.07 ± 6.28 | 0.03 |
| Others | 162 | 36.4 | 20–60 | 38.7 ± 6.44 | |
| Follows a food plan | |||||
| Yes | 206 | 41.2 | 22–52 | 37.36 ± 6.06 | |
| Ketogenic diet | 20 | 4 | 22–45 | 33.25 ± 6.96 | 0.002 |
| Hypocaloric diet | 114 | 22.8 | 24–52 | 36.6 ± 6.12 | |
| Mediterranean diet | 24 | 4.8 | 25–49 | 36.08 ± 5.65 | |
| High-protein diet | 14 | 2.8 | 32–48 | 41.14 ± 5.33 | |
| High-calorie diet | 27 | 5.4 | 28–50 | 38.7 ± 5.45 | |
| Others | 7 | 1.4 | 29–48 | 40 ± 6.24 | |
| No | 294 | 58.8 | 20–60 | 41.23 ± 6.07 | |
| Has ≥ 2 servings of vegetables/day | |||||
| Yes | 298 | 59.6 | 20–53 | 39.04 ± 6.28 | 0.01 |
| No | 202 | 40.4 | 22–60 | 40.52 ± 6.38 | |
| Performs physical activity | |||||
| Yes | 278 | 55.6 | 20–53 | 39 ± 5.99 | 0.01 |
| No | 222 | 44.4 | 22–60 | 40.44 ± 6.71 | |
| Model 1 | β (95% CI) | SE | p-Values |
|---|---|---|---|
| Gender [F] | −2.98 (−4.23; −1.73) | 0.64 | 4 × 10−6 |
| BMI | −0.41 (−0.57; −0.25) | 0.08 | 6.71 × 10−7 |
| Adj.R2 | 0.06 | ||
| Model 2 | β (95% CI) | SE | p-Values |
| Gender [F] | −2.98 (−4.20; −1.76) | 0.62 | 2 × 10−5 |
| BMI | −0.27 (−0.42; −0.1) | 0.08 | 0.002 |
| Health science faculty | 1.26 (0.15; 2.37) | 0.57 | 0.03 |
| Follows a food plan | −3.14 (−4.29; −1.99) | 0.57 | 1 × 10−7 |
| Has ≥ 2 servings of vegetables/day | −0.42 (−1.52; 0.68) | 0.56 | 0.45 |
| Performs physical activity | −1.20 (−2.28; −0.122) | 0.55 | 0.03 |
| Adj.R2 | 0.14 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Augimeri, G.; Marchese, M.; Plastina, P.; Bonofiglio, D. Examining Associations Among Orthorexia Nervosa and Anthropometric Factors and Lifestyle Habits in an Italian University Community. Nutrients 2025, 17, 537. https://doi.org/10.3390/nu17030537
Augimeri G, Marchese M, Plastina P, Bonofiglio D. Examining Associations Among Orthorexia Nervosa and Anthropometric Factors and Lifestyle Habits in an Italian University Community. Nutrients. 2025; 17(3):537. https://doi.org/10.3390/nu17030537
Chicago/Turabian StyleAugimeri, Giuseppina, Martina Marchese, Pierluigi Plastina, and Daniela Bonofiglio. 2025. "Examining Associations Among Orthorexia Nervosa and Anthropometric Factors and Lifestyle Habits in an Italian University Community" Nutrients 17, no. 3: 537. https://doi.org/10.3390/nu17030537
APA StyleAugimeri, G., Marchese, M., Plastina, P., & Bonofiglio, D. (2025). Examining Associations Among Orthorexia Nervosa and Anthropometric Factors and Lifestyle Habits in an Italian University Community. Nutrients, 17(3), 537. https://doi.org/10.3390/nu17030537







