Abstract
Cervical cancer is a global public health problem. It is the second leading cause of death among women of childbearing age worldwide. Several factors, including diet, have been shown to influence the risk of persistent HPV infection and tumor progression. This paper determines the relationship between dietary patterns and cervical cancer. It is an ecological study of multiple groups, based on two national sources: the High-Cost Account and the National Survey of Nutritional Situation of Colombia of 2015. The population consisted of 3472 women aged 35 to 64. The incidence of cervical cancer was used as the dependent variable while the independent variables included food consumption according to established patterns, area of residence, age, physical activity, and BMI, among other variables. The statistical analysis performed through associations between variables was evaluated by multiple linear regression using R2. 38.9% of the evaluated population belonged to the first quartile of wealth, and 76.5% resided in the municipal capital. The incidence of cervical cancer in Colombia was associated with being affiliated to a state-subsidized health regime and having diabetes mellitus. A conservative eating pattern, as well as belonging to a rural area, are evidenced as protective factors. These results invite the need to encourage public policies and promote healthy lifestyles.
1. Introduction
Cervical cancer is a global public health problem, particularly in low- and middle-income countries (LMICs) [1]. It is the second most frequent and the second leading cause of death in women of reproductive age in the world [2]. In 2020, an incidence of 604,000 and 342,000 deaths was estimated [3]. According to GLOBOCAN data for 2020, Latin America and the Caribbean ranked second worldwide in incidence and mortality, with 59,439 new cases and 31,582 deaths [4]. It has been suggested that the incidence in these LMICs may be due to several factors, including lifestyle [5].
Human papillomavirus (HPV) is one of the causative agents of cervical cancer and precursor lesions [6]. Several causes have been shown to affect the risk of persistent HPV infection and the progression of neoplasms, including diet [7,8]. HPV survives in a cellular oxidative environment and has been shown to be more likely to evolve into neoplasms by increasing oxidative stress and DNA damage [9]. For these reasons, dietary intake of antioxidants appears to exert a protective effect on HPV infection and persistence [7,8]. According to the results of the EPIC (European Prospective Investigation into Cancer and Nutrition) study, there is a significant inverse association between invasive squamous cervical cancer and daily increases in fruit intake [10].
Regarding dietary patterns, a recent study has established that adhering to the Mediterranean diet reduces the risk of cervical cancer by 60%, while following a Western diet represents a risk factor for its appearance [11]. It is estimated that changes in dietary habits can contribute to preventing the onset of cancer by 30% to 40% [12].
For these reasons, this research was proposed to determine the relationship between dietary patterns and cervical cancer, considering other sociodemographic aspects of different regions in Colombia.
2. Methodology
A multi-group ecological study was conducted based on two national sources, HIGIA (High-Cost Account), and ENSIN 2015 (National Survey of Nutritional Situation of Colombia of 2015). The population consisted of 3472 women aged 35 to 64, distributed across six regions of Colombia: Atlántica, Central, Oriental, Pacífica, Orinoquía, and the Capital District of Bogotá.
The incidence of cervical cancer was used as the outcome variable, taken from the High-Cost Account. Independent variables were obtained from the National Survey of the Nutritional Situation (ENSIN) 2015, including: area of residence, affiliation regime, quartile of wealth, educational level, age ranges, compliance with the recommendations of physical activity, compliance with 30 min of physical exercise per day for at least 5 days, following the recommendations of vigorous physical activity, and BMI according to World Health Organization (WHO) categories [13]. In addition, information was collected on the suffering of hypertension, diabetes mellitus, following a special diet, and following a vegetarian diet. These variables were dichotomized.
The area of residence was structured as a categorical variable, including municipal seat (defined as the urban perimeter limited by agreements of the Municipal Council, where the administrative headquarters of the municipality is located), populated center (refers to the concentration of at least twenty contiguous houses, neighboring or attached to each other, located in the rural area of a municipality or a departmental corregimiento), and rural center, defined by dispersed dwellings with disaggregated farms [14].
The independent variable, consumption of dietary patterns, was taken from the work of Meneses et al., who established four dietary patterns: traditional, industrialized, conservative, and beverages/grilled foods. The traditional pattern was made up of the dairy group, potato/legume groups, cereal group, fried group, coffee/panela, and meat-sausages. The industrialized pattern was characterized by the consumption of soft drinks, fast foods, sweets, and package foods. The conservative pattern referred to individuals who based their diet on the group of vegetables, fruits, light foods, supplements, and whole foods. Finally, the beverages/grilled foods pattern was made up of the group of energy drinks, alcohol, and grilled foods [15]. To introduce the patterns into the statistical models, it was necessary to generate a new dichotomous dependent variable for each one, through the binomial distribution, as follows: those presenting some degree of consumption of the corresponding pattern were categorized as 1, while those who did not report any level of consumption of the pattern were categorized as 0.
The statistical analysis was performed through the association of contextual variables and was evaluated by multiple linear regression using R2 and the principle of statistical parsimony for multiple linear regression as a goodness of fit measure, which considers the minimum sum of squares [16]. 15 models were performed until the best one was obtained, representing the dietary patterns and accounting for possible confounding effects of the contextual variables on the incidence of cervical cancer. The statistical modeling used a stepwise method, with a criterion of eliminating probability values above 0.10.
Ethical Considerations
The study was endorsed by the Institutional Ethics Committee of the Universidad Santiago de Cali, Approval Act No. 11 of 29 May 2020. The database used was authorized by the Colombian Institute of Family Welfare (ICBF) to conduct the research, and it involved working with available anonymized data, with the consent (verbal or signed) of the participants in these national surveys to the interviewers of the national health system.
3. Results
Information was collected from a sample of 3472 women within the age range of 35 to 64. Through the evaluation of sociodemographic variables, relevant findings are highlighted, including the distribution of wealth, educational level, age, geographical location, and health insurance regime. The results indicate that 38.9% of the evaluated population belonged to the first quartile of wealth (Q1), and the region with the highest percentage in the first quartile of wealth (Q1) was Amazonia-Orinoquia, with 53.5%. 71.4% of respondents had an educational level up to high school, and 53% were in the age range of 35 to 49, occurring most frequently in the Atlantic region (64.7%). In addition, 76.5% resided in municipal capitals, with the Pacific region having the most reported living in rural areas at 32%. 58.1% of the participants belonged to the subsidized health care regime or were unaffiliated. It is important to note that this regime is used by the Colombian State to provide access to health services through granted subsidies for those without the ability to pay. The region with the highest percentage under this regime was the Amazonía-Orinoquia region, at 69.5% (Table 1).

Table 1.
Sociodemographic characteristics.
Likewise, when considering the additional variables evaluated in the study, it was found that 12.6% of the population complied with the recommendations of physical activity, with 1.6% engaging with physical activity for at least 30 min, five times a week, and only 0.7% participating in vigorous physical activity. On the other hand, 100% of the sample did not follow a vegetarian diet or any kind of special diet. In relation to the prevalence of chronic diseases, 48.8% reported having hypertension, 2.7% had diabetes, 38.1% were overweight, and 76.3% were obese. Additional data structured by region are available in Table 2.

Table 2.
Lifestyle and health status.
In relation to dietary patterns, 94.6% of the population had some consumption of pattern 1 (traditional), 92.9% of pattern 3 (conservative), 73.9% of pattern 2 (industrialized), and 57.7% had an intake linked to pattern 4 (food, beverages/grill). The traditional and conservative patterns stood out in the Pacific region, while the industrialized pattern was of higher consumption in the Atlantic region and the beverage/grill food pattern was reported more frequently in the Eastern region. The Department of Tolima, despite belonging to this region, reported no consumption. The Bogotá region was characterized by pattern 2 (industrialized) and the Amazonia-Orinoquia region, compared to the other regions, had the highest consumption of beverage/grilled foods (see Figure 1 and Table 3).
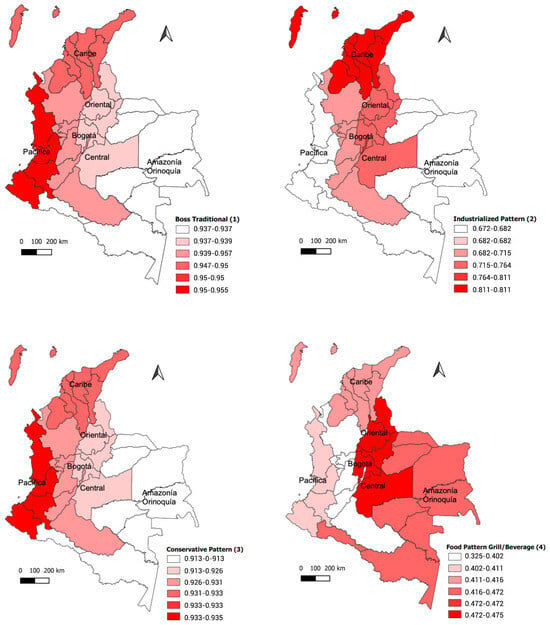
Figure 1.
Dietary pattern by region.

Table 3.
Eating patterns.
Regarding the incidence of cervical cancer in people over 35 years of age in 2020, the highest rate was found in the Amazonia-Orinoquia region, with 23.8 cases per 100,000 habitants. This region is the one that reported the highest percentage of the population in Q1 of wealth, affiliation to the subsidized health regime, declarations of diabetes, and consumption of beverage foods/grill. The lowest incidence rate was reported in the Eastern region, with 12.8 per 100,000 hb. This region had the lowest prevalence of obesity (see Figure 2).
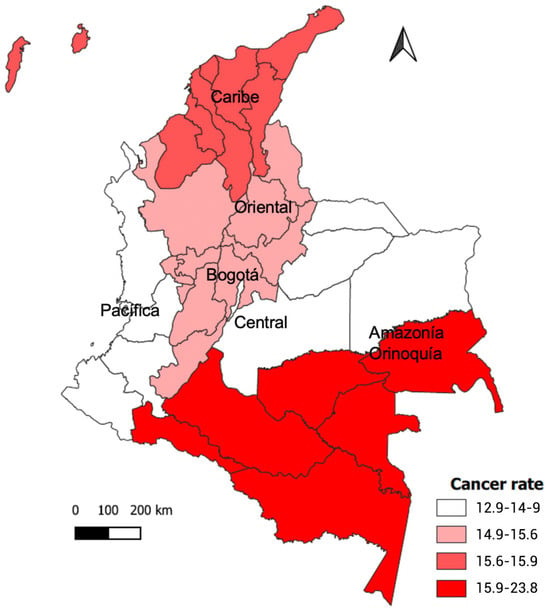
Figure 2.
Incidence of cervical cancer by region.
Modelling was performed using an initial saturated model that contained all available explanatory variables [16]. After the variables in the multivariate model were adjusted, 15 models were generated. 68% of the incidence of cervical cancer can be explained by the explanatory variables of the multiple linear model (Table 4), showing a positive association with certain factors, including belonging to the subsidized regime or not being affiliated (p = 0.002), and having diabetes (p = 0.07). In addition, a negative association was found with the conservative dietary pattern (p = 0.013) and residing in a populated or dispersed rural center (p = 0.003), (Table 5).

Table 4.
Comparison of ecological multiple linear regression models for cervical cancer incidence, adjusting for dietary patterns and other variables. Regions of Colombia. Year 2020.

Table 5.
Model Factors of greatest influence on the incidence of cervical cancer.
4. Discussion
An ecological study was conducted using secondary data from the database of the National Survey of the Nutritional Situation (ENSIN) 2015 and the 2020 incidence rate of cervical cancer for people over 35 years of age, using the High-Cost Account as a source of information.
The incidence rate of cervical cancer has risen worldwide, especially in countries with a high Human Development Index (HDI). Colombia is considered a country with a high HDI [17]. This rate is influenced by aging, population growth, and changes in cancer risk factors, some of which are related to socioeconomic development [18]
The findings of this research showed associations between the incidence rate and variables including the area of residence, populated or rural center, subsidized health regime, having diabetes, and the consumption of the conservative pattern. The results of our study found no association with the quartile of wealth, despite the fact that 62.4% of the population was in quartiles 1 and 2 of wealth, which may be due to early detection and efficient treatment [19]. Several studies have reported that the probability of developing cancer is higher in socially vulnerable populations and that the risk of getting sick and dying is associated with lower levels of income, education, and higher degrees of social discrimination [20,21].
The lack of adequate health insurance coverage is a challenge in communities of poverty and is associated with reduced access to care, prevention, and diagnosis. Patel et al. conducted a study in California and reported that patients with Medicaid, insurance granted by the state, or those without any medical insurance had a higher incidence of cervical cancer [22], which coincides with the results of our research. Another study in the United States showed that Medicaid patients had a 38% increase in mortality (HR = 1.38; CI 95% 1.34–1.43), while uninsured patients had a 32% increase (HR = 1.32; CI 95%, 1.26–1.38), which may be associated with lower quality of care and reduced adherence to medical protocols in public hospitals [23]. On the other hand, the report on the situation of cancer in Colombia in 2021 reported that the incidence of cervical cancer was similar for both the contributory and subsidized regimes [24].
Regarding the area of residence, our research found that living in a populated/rural center decreases the incidence of cervical cancer, which coincides with the findings of Hall et al., who conducted a study in Florida, United States, using Cancer Data System data during the years 2014–2018. They sought to determine age-adjusted incidence and mortality for 22 types of cancer, including cervical cancer. These authors found that the incidence was significantly lower in rural areas than in urban areas [25]. In the same way, the study of Fantin et al., with cancer registries from 2011 to 2015 in Costa Rica, showed that cervical cancer was higher in urban areas [26]. In any case, it should be noted that the results of lower incidence in rural areas may be due to underreporting or poor accessibility to health services in these areas.
According to WHO recommendations, physical activity confers several benefits, including reducing mortality from any cause, cardiovascular diseases, hypertension, specific cancers, and type 2 diabetes, in addition to contributing to mental health. For these reasons, the WHO emphasizes that adults should perform moderate activity for two or more days a week, with a duration of 150–300 min of moderate to intense activity, or 75–150 min of vigorous activity to obtain these benefits [27]. In our research research, we found that only 8.5% meet these recommendations for physical activity, 0.8% meet the recommendations for 30 min of physical activity five times a week and 0.5% meet the recommendations for vigorous activity. These figures reflect a significant decrease, taking into account that in Colombia in 2010, the prevalence of moderate physical activity per week was 53.5% [28]. In high-income countries, the prevalence of physical inactivity was double (36.8%, 35–38) that of LMICs (16.2%, 14.2–17.9) [29]. Despite this, our study did not find an association between cervical cancer and physical activity, possibly due to the low percentage of the population that performs it regularly, which may have been decisive in finding a statistical relationship. Contrary to these findings, Lee et al. in their study in Korea, using cancer registries from 2006 to 2012 in women with intracervical neoplasia and cancer, showed that the risk of grade 2 and 3 intracervical neoplasia was inversely associated with physical activity [30].
With regard to BMI, our results showed no association with cervical cancer. Wise et al. and Emma et al. found an association between a BMI greater than 30 kg/m2 and endometrial cancer [31,32]. Similarly, high BMI is considered one of the risk factors for all types of cancer, according to the Global Burden of Cancer [33]. The difference in results may be due to the ecological, pooled, and cross-sectional data used in this study, which has been able to reduce the measurement of the effect of obesity on the incidence of cervical cancer. However, the research discussed above [33,34] corresponds to longitudinal and individual studies, where such types of biases are usually controlled.
In relation to the disease declared in our study, diabetes was associated with an increased incidence of cervical cancer, which may be related to hyperglycemia and chronic inflammation caused by this pathology [34], in addition to the imbalance in the proteasome system among these patients, taking into account that the development of cancer requires high protein turnover and involves this system [35]. In a study by Garduño et al. in Mexico involving women with cervical cancer, an association with diabetes was found [36]. These results also coincide with those of Yang et al., who conducted a study in Taiwan with adults over 35 years diagnosed with several types of cancers, including cervical cancer, and found a similar association (adjusted RR 13.4; CI 95% 2.70–66.3) [37].
Regarding the incidence of cervical cancer, the highest rate in 2020 was found in the Amazon-Orinoquia region, in which the highest proportion of individuals was found in Q1, with affiliations to the subsidized health regime, a higher percentage of diabetes in relation to other regions, and more frequently reported consumption of beverage/grill foods. Studies have reported the presence of polycyclic aromatic hydrocarbons (PAHs) and heteroaromatic amines (HAAs) in meat that has been exposed to high temperatures during grilling [38,39]. One of the PAHs, benzo (a) pyrene (BaP), is known as a carcinogen, capable of modulating cellular processes including differentiation, proliferation, immune response, cancer promotion, and apoptosis [40,41].
On the other hand, according to the National Quality of Life Survey in 2018, in the Orinoquia-Amazon region, 69.9% of people aged 2 years and over reported consuming sugary drinks, a figure that exceeds the national record of 68.4% [42].
A diet high in sugar usually leads to weight gain and metabolic parameters associated with obesity, insulin resistance, the bioactivity of steroid hormones, oxidative stress, inflammation, and ultimately, the development and progression of cancer [43]. According to Choi et al., the consumption of sugary drinks is associated with type II endometrial cancer [44]. Therefore, the incidence of cervical cancer in this region may be associated with the consumption of sugary drinks.
In terms of dietary patterns, it was found that the conservative pattern is related to a lower incidence of cervical cancer. These results are consistent with Marziyeh et al., who showed that a high consumption of fruits and vegetables can reduce the risk of cervical cancer [45]. In addition, Barchitta et al., concluded that the risk of cervical cancer was lower in patients with high scores in the healthy diet pattern [8], while Mogge et al. found that patients with cervical cancer had a lower intake of fruits and vegetables [46]. In addition, Hwang et al. found that fruit and vegetable consumption reduces the risk of cervical cancer (OR = 2.84, 95% CI 1.26 to 6.42, p = 0.06 for vegetables; OR = 2.93, 95% CI 1.25 to 6.87, p = 0.01 for fruits) [47]. All of the above is possible because of the antioxidants that fruits and vegetables have, such as vitamin C and a- and b-carotene, which limit the damage caused by free radicals [48].
Limitations
Studies based on nutritional patterns rather than the measurement of dietary intakes do not allow us to know what type of foods or nutritional values could be more closely related with the development of this type of cancer. In any case, they are frequently used tools in ecological designs based on health surveys, as they represent food and nutrient consumption from a more comprehensive and community-based view on diet as a factor of exposure to a health event [49,50]. For these reasons, there is a need for longitudinal studies to establish a more precise association between dietary intakes and the development of cervical cancer. Another notable limitation is the lack of data on medical and gyneco-obstetrical factors, which were not collected in the health survey used for this secondary analysis. These factors could also be related to the development of this type of cancer. On the other hand, because it is a secondary source, the participants’ responses may have recall bias. It should be noted that the sample size of the study decreases the probability of incurring type II errors.
5. Conclusions
It is concluded that, at the ecological level, the increase in the incidence of cervical cancer in Colombia was associated with affiliation to a health regime subsidized by the state and comorbidity with diabetes mellitus. In addition, the conservative dietary pattern, consisting of fruits and vegetables, as well as belonging to a rural area, were evidenced as protective variables. These results invite us to encourage public health policies that reduce population inequity and to make educational efforts for the promotion of healthy lifestyles to prevent cervical cancer.
Author Contributions
L.A.M.-U. and M.H.-C. conceptualized the study. L.A.M.-U. and M.H.-C. conducted the analysis and drafted the manuscript. L.A.M.-U., M.H.-C., D.V.A., N.B.S., G.M.-R. and M.V.-A. reviewed and revised the draft. All authors have read and agreed to the published version of the manuscript.
Funding
This study was funded by Dirección General de Investigaciones of Universidad Santiago de Cali under call No. 03-2020, call No. 10 of 2022 and call No. 02 of 2023.
Institutional Review Board Statement
This study was reviewed and approved by The Human Research Ethics Committee of Santiago of Cali University (Act N_11 from the May 29th session). Written informed consent for participation was not required for this study in accordance with national legislation (Resolution 8430 of 1993) and international requirements (Declaration of Helsinki and standards of Good Clinical Practice/Harmonized Tripartite Guide of the International Council for Harmonisation).
Informed Consent Statement
Informed consents are unavailable since the article was conducted through secondary analysis of databases corresponding to national health surveys in Colombia. However, all participants in these national surveys gave their consent (verbal or signed) to the interviewers of the national health system.
Data Availability Statement
The data will be made available to anyone who requests it from the corresponding author through a reasoned request.
Acknowledgments
This research has been funded by Dirección General de Investigaciones of Universidad Santiago de Cali under call No. DGI-02-2023. The authors thank the Colombian Institute of Family Welfare (ICBF) for providing the original database of the National Survey of Nutritional Situation of Colombia (ENSIN) and the University of Córdoba for providing the methodological tools for data analysis.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Bouvard, V.; Wentzensen, N.; Mackie, A.; Berkhof, J.; Brotherton, J.; Giorgi-Rossi, P.; Kupets, R.; Smith, R.; Arrossi, S.; Bendahhou, K.; et al. The IARC Perspective on Cervical Cancer Screening. N. Engl. J. Med. 2021, 385, 1908–1918. [Google Scholar] [CrossRef] [PubMed]
- Arbyn, M.; Weiderpass, E.; Bruni, L.; de Sanjosé, S.; Saraiya, M.; Ferlay, J.; Bray, F. Estimates of incidence and mortality of cervical cancer in 2018: A worldwide analysis. Lancet Glob. Health 2019, 8, e191–e203. [Google Scholar] [CrossRef] [PubMed]
- Organizacion Mundial de la Salud. Cancer Cervicouterino [Internet]. 2022. Available online: https://www.who.int/es/news-room/fact-sheets/detail/cervical-cancer (accessed on 1 March 2023).
- International Agency for Research on Cancer; World Health Organization. Cervix uteri. Source Globocan 2020 [Internet]. The Global Cancer Observatory. 2020, Volume 86. Available online: https://gco.iarc.fr/today/data/factsheets/cancers/23-Cervix-uteri-fact-sheet.pdf (accessed on 6 January 2023).
- Cecilia, N.C.; Rosliza, A.M.; Suriani, I. Global Burden of Cervical Cancer: A literature Review. Int. J Public Health Clin. Sci. 2017, 4, 10–18. [Google Scholar]
- Schiffman, M.H.; Brinton, L.A. The epidemiology of cervical carcinogenesis. Cancer 1995, 76, 1888–1901. [Google Scholar] [CrossRef]
- García-Closas, R.; Castellsagué, X.; Bosch, X.; González, C.A. The role of diet and nutrition in cervical carcinogenesis: A review of recent evidence. Int. J. Cancer 2005, 117, 629–637. [Google Scholar] [CrossRef] [PubMed]
- Barchitta, M.; Maugeri, A.; La Mastra, C.; La Rosa, M.C.; Favara, G.; Magnano San Lio, R.; Agodi, A. Dietary antioxidant intake and human papillomavirus infection: Evidence from a cross-sectional study in Italy. Nutrients 2020, 12, 1384. [Google Scholar] [CrossRef]
- De Marco, F. Oxidative stress and HPV carcinogenesis. Viruses 2013, 5, 708–731. [Google Scholar] [CrossRef]
- González, C.A.; Travier, N.; Luján-Barroso, L.; Castellsagué, X.; Bosch, F.X.; Roura, E.; Bueno-de-Mesquita, H.B.; Palli, D.; Boeing, H.; Pala, V. Dietary factors and in situ and invasive cervical cancer risk in the European prospective investigation into cancer and nutrition study. Int. J. Cancer 2011, 129, 449–459. [Google Scholar] [CrossRef]
- Barchitta, M.; Maugeri, A.; Quattrocchi, A.; Agrifoglio, O.; Scalisi, A.; Agodi, A. The association of dietary patterns with high-risk human papillomavirus infection and cervical cancer: A cross-sectional study in Italy. Nutrients 2018, 10, 4046. [Google Scholar] [CrossRef]
- World Cancer Research Fund; American Institute for Cancer Research. Diet, Nutrition, Physical Activity and Cancer: A Global Perspective [Internet]. 2018. Available online: https://www.wcrf.org/wp-content/uploads/2021/02/Summary-of-Third-Expert-Report-2018.pdf (accessed on 3 May 2023).
- OMS. Obesidad y Sobrepeso [Internet]. 2021. Available online: https://www.who.int/es/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 27 January 2023).
- DANE. Conceptos Básicos. Análisis de Circuitos Eléctricos Estado Estable. Chrome. 2018. Available online: https://www.dane.gov.co/files/inf_geo/4Ge_ConceptosBasicos.pdf (accessed on 3 September 2023).
- Meneses Urrea, L.A.; Vaquero Abellán, M.; Benachi Sandoval, N.; Villegas Arenas, D.; Osorio Murillo, O.; Molina-Recio, G. Dietary Patterns in Colombia: An Exploratory and Con fi rmatory Factor Analysis. Front. Food Sci. Technol. 2022, 2, 897877. [Google Scholar] [CrossRef]
- Ohtani, K.; Tanizaki, H. Exact Distributions of R 2 and Ajusted r2 in a Linear Regression Model with Multivariate t Error Term. J. Jpn. Stat. Soc. 2004, 34, 101–109. [Google Scholar] [CrossRef][Green Version]
- Programa de Naciones Unidas para el Desarrollo (PNUD). Informe sobre Desarrollo Humano 2015: Trabajo al Servicio del desarrollo Humano. [Internet]. Informe. 2015, pp. 1–290. Available online: https://hdr.undp.org/system/files/documents/hdr2015reportsppdf.pdf (accessed on 1 June 2023).
- Yi, M.; Li, T.; Niu, M.; Luo, S.; Chu, Q.; Wu, K. Epidemiological trends of women’s cancers from 1990 to 2019 at the global, regional, and national levels: A population-based study. Biomark. Res. 2021, 9, 55. [Google Scholar] [CrossRef] [PubMed]
- Pardo, C.; de Vries, E. Breast and cervical cancer survival at instituto nacional de cancerología, Colombia. Colomb. Med. 2018, 49, 102–108. [Google Scholar] [CrossRef]
- Krieger, N. Defining and investigating social disparities in cancer: Critical issues. Cancer Causes Control 2005, 16, 5–14. [Google Scholar] [CrossRef] [PubMed]
- López, F.E.; Pérez, P.T.; Murillo, E.N.; Quintero, G.C. Desigualdades sociales en la mortalidad por VIH y tumores malignos en municipios del departamento de Valle del Caua (Colombia) segun indicadores económicos 2009–2013. Arch. Med. 2018, 18, 373–384. [Google Scholar]
- Parikh-Patel, A.; Morris, C.R.; Kizer, K.W. Disparities in quality of cancer care: The role of health insurance and population demographics. Medicine 2017, 96, e9125. [Google Scholar] [CrossRef]
- Cherston, C.; Yoh, K.; Huang, Y.; Melamed, A.; Gamble, C.R.; Prabhu, V.S.; Li, Y.; Hershman, D.L.; Wright, J.D. Relative importance of individual insurance status and hospital payer mix on survival for women with cervical cancer. Gynecol. Oncol. 2022, 166, 552–560. [Google Scholar] [CrossRef]
- de Alto, C.C. Situación del Cáncer en la Población Adulta Atendida en el SGSSS de Colombia 2021 [Internet]. Bogota-Colombia. 2021. Available online: https://cuentadealtocosto.org/site/wp-content/uploads/2022/08/01_agosto_libro_cancer_2021_final.pdf (accessed on 8 March 2022).
- Hall, J.M.; Szurek, S.M.; Cho, H.; Guo, Y.; Gutter, M.S.; Khalil, G.E.; Licht, J.D.; Shenkman, E.A. Cancer disparities related to poverty and rurality for 22 top cancers in Florida. Prev. Med. Rep. 2022, 29, 101922. [Google Scholar] [CrossRef]
- Fantin, R.; Ulloa, C.S.; Solís, C.B. Social gradient in cancer incidence in Costa Rica: Findings from a national population-based cancer registry. Cancer Epidemiol. 2020, 68, 101789. [Google Scholar] [CrossRef]
- WHO. WHO Guidelines on Physical Activity and Sedentary Behaviour. Routledge Handbook of Youth Sport. 2016, pp. 1–582. Available online: https://iris.who.int/bitstream/handle/10665/336656/9789240015128-eng.pdf?sequence=1 (accessed on 8 June 2023).
- Instituto Colombiano de Bienestar Familiar. Resumen Ejecutivo Encuesta Nacional de la Situacion Nutricional en Colombia. ENSIN 2010. 2011. Available online: https://www.icbf.gov.co/sites/default/files/resumenfi.pdf (accessed on 2 July 2023).
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Worldwide trends in insufficient physical activity from 2001 to 2016: A pooled analysis of 358 population-based surveys with 1·9 million participants. Lancet Glob. Health 2018, 6, e1077–e1086. [Google Scholar] [CrossRef]
- Lee, J.K.; So, K.A.; Piyathilake, C.J.; Kim, M.K. Mild Obesity, Physical Activity, Calorie Intake, and the Risks of Cervical Intraepithelial Neoplasia and Cervical Cancer. PLoS ONE 2013, 8, e66555. [Google Scholar] [CrossRef] [PubMed]
- Wise, M.R.; Jordan, V.; Lagas, A.; Showell, M.; Wong, N.; Lensen, S.; Farquhar, C.M. Obesity and endometrial hyperplasia and cancer in premenopausal women: A systematic review. Am. J. Obstet. Gynecol. 2016, 214, e1–e689. [Google Scholar] [CrossRef] [PubMed]
- Crosbie, E.J.; Kitson, S.J.; McAlpine, J.N.; Mukhopadhyay, A.; Powell, M.E.; Singh, N. Seminar Endometrial cancer. Lancet 2022, 399, 1412–1428. [Google Scholar] [CrossRef] [PubMed]
- Bill, F.; Foundation, M.G. The global burden of cancer attributable to risk factors, 2010–19: A systematic analysis for the Global Burden of Disease Study. Lancet 2019, 2019, 9–20. [Google Scholar] [CrossRef]
- Tsilidis, K.K.; Kasimis, J.C.; Lopez, D.S.; Ntzani, E.E.; Ioannidis, J.P.A. Type 2 diabetes and cancer: Umbrella review of meta-analyses of observationlal studies. BMJ 2015, 350, g7607. [Google Scholar] [CrossRef]
- Jang, H.H. Regulation of Protein Degradation by Proteasomes in Cancer. J. Cancer Prev. 2018, 23, 153–161. [Google Scholar] [CrossRef]
- Garduño Orbe, B.; Hernández Wences, B.; Rayon Castañeda, C.J.; García Morales, G. Prevalencia de enfermedades crónicas en pacientes diagnosticadas con lesión intraepitelial del cérvix. Atención Familiar 2022, 29, 97. [Google Scholar] [CrossRef]
- Yang, W.S.; Chen, P.C.; Lin, H.J.; Su, T.C.; Hsu, H.C.; Chen, M.F.; Lee, Y.T.; Chien, K.L. Association between type 2 diabetes and cancer incidence in Taiwan: Data from a prospective community-based cohort study. Acta Diabetol. Acta Diabetol. 2017, 54, 455–461. [Google Scholar] [CrossRef]
- Zachara, A.; Gałkowska, D.; Juszczak, L. Contamination of smoked meat and fish products from Polish market with polycyclic aromatic hydrocarbons. Food Control 2017, 80, 45–51. [Google Scholar] [CrossRef]
- Nor Hasyimah, A.K.; Jinap, S.; Sanny, M.; Ainaatul, A.I.; Sukor, R.; Jambari, N.N.; Nordin, N.; Jahurul, M.H.A. Effects of Honey-Spices Marination on Polycyclic Aromatic Hydrocarbons and Heterocyclic Amines Formation in Gas-Grilled Beef Satay. Polycyclic. Aromat. Compd. 2022, 42, 1620–1648. [Google Scholar] [CrossRef]
- Sun, K.; Song, Y.; He, F.; Jing, M.; Tang, J.; Liu, R. A review of human and animals exposure to polycyclic aromatic hydrocarbons: Health risk and adverse effects, photo-induced toxicity and regulating effect of microplastics. Sci. Total. Environ. 2021, 773, 145403. [Google Scholar] [CrossRef] [PubMed]
- Nagao, M.; Tsugane, S. Cancer in Japan: Prevalence, prevention and the role of heterocyclic amines in human carcinogenesis. Genes Environ. 2016, 38, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Departamento Administrativo Nacional de Estadística (DANE). Boletín Técnico. Encuesta Nacional de Calidad de Vida (ECV) [Internet]. 2019. Available online: https://www.dane.gov.co/files/investigaciones/condiciones_vida/calidad_vida/2018/Region-bt-ECV-18-amazonia-orinoquia.pdf (accessed on 2 May 2022).
- Secretan, B.L.; Scoccianti, C.; Loomis, D. Special Rep or t Body Fatness and Cancer—Viewpoint of the IARC Working Group. N. Engl. J. Med. 2016, 375, 794–798. [Google Scholar] [CrossRef]
- Inoue-Choi, M.; Robien, K.; Mariani, A.; Cerhan, J.R.; Anderson, K.E. Sugar-sweetened beverage intake and the risk of type I and type II endometrial cancer among postmenopausal women. Cancer Epidemiol. Biomark. Prev. 2013, 22, 2384–2394. [Google Scholar] [CrossRef] [PubMed]
- Najafi, M.; Nazari, Z.; Shamsi, R.; Nikpayam, O.; Bahrami, A.; Hekmatdoost, A.; Hejazi, E. Dietary patterns and risk of cervical cancer: A case-control study. Eur. J. Gynaecol. Oncol. 2020, 41, 943–948. [Google Scholar] [CrossRef]
- Hajiesmaeil, M.; Dahka, S.M.; Khorrami, R.; Rastgoo, S.; Bourbour, F.; Davoodi, S.H.; Shafiee, F.; Gholamalizadeh, M.; Torki, S.A.; Akbari, M.E.; et al. Intake of food groups and cervical cancer in women at risk for cervical cancer: A nested case-control study. Casp. J. Intern. Med. 2022, 13, 599–606. [Google Scholar] [CrossRef]
- Hwang, J.H.; Lee, J.K.; Kim, T.J.; Kim, M.K. The association between fruit and vegetable consumption and HPV viral load in high-risk HPV-positive women with cervical intraepithelial neoplasia. Cancer Causes Control 2010, 21, 51–59. [Google Scholar] [CrossRef]
- Coronado, H.M.; Vega, Y.; León, S.; Gutiérrez, T.R.; Marcela, V.F.; Radilla, V.C. Antioxidantes: Perspectiva actual para la salud humana. Rev. Chil. Nutr. 2015, 42, 206–212. [Google Scholar] [CrossRef]
- Moeller, S.M.; Jill, R.; Millen, A.E.; Newby, P.K.; Tucker, K.L.; Krebs, S.M.; Muñoz, S.E.; Becaria Coquet, J.; Díaz, M.D. Dietary Patterns: Challenges and Opportunities in Evolution of dietary Patterns. J. Am. Diet. Assoc. 2007, 107, 1233–1239. [Google Scholar] [CrossRef]
- Pou, S.A.; Niclis, C.; Aballay, L.R.; Tumas, N.; Román, M.D.; Muñoz, S.E.; Becaria Coquet, J.; del Pilar Díaz, M. Cáncer y Su Asociación Con Patrones Alimentarios En Córdoba (Argentina). Nutr. Hosp. 2014, 29, 618–628. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).