Development and Validation of the Short Healthy Eating Index Survey with a College Population to Assess Dietary Quality and Intake
Abstract
1. Introduction
- Determine whether the Short Healthy Eating Index (sHEI) could be used to accurately estimate dietary intake of food groups by comparing the newly developed sHEI survey outputs to those of the Dietary Screener Questionnaires (DSQs) [33], 24 h recalls, and carotenoid measurements.
- Determine whether the sHEI could be used to accurately estimate the HEI score calculated from 24 h recall data.
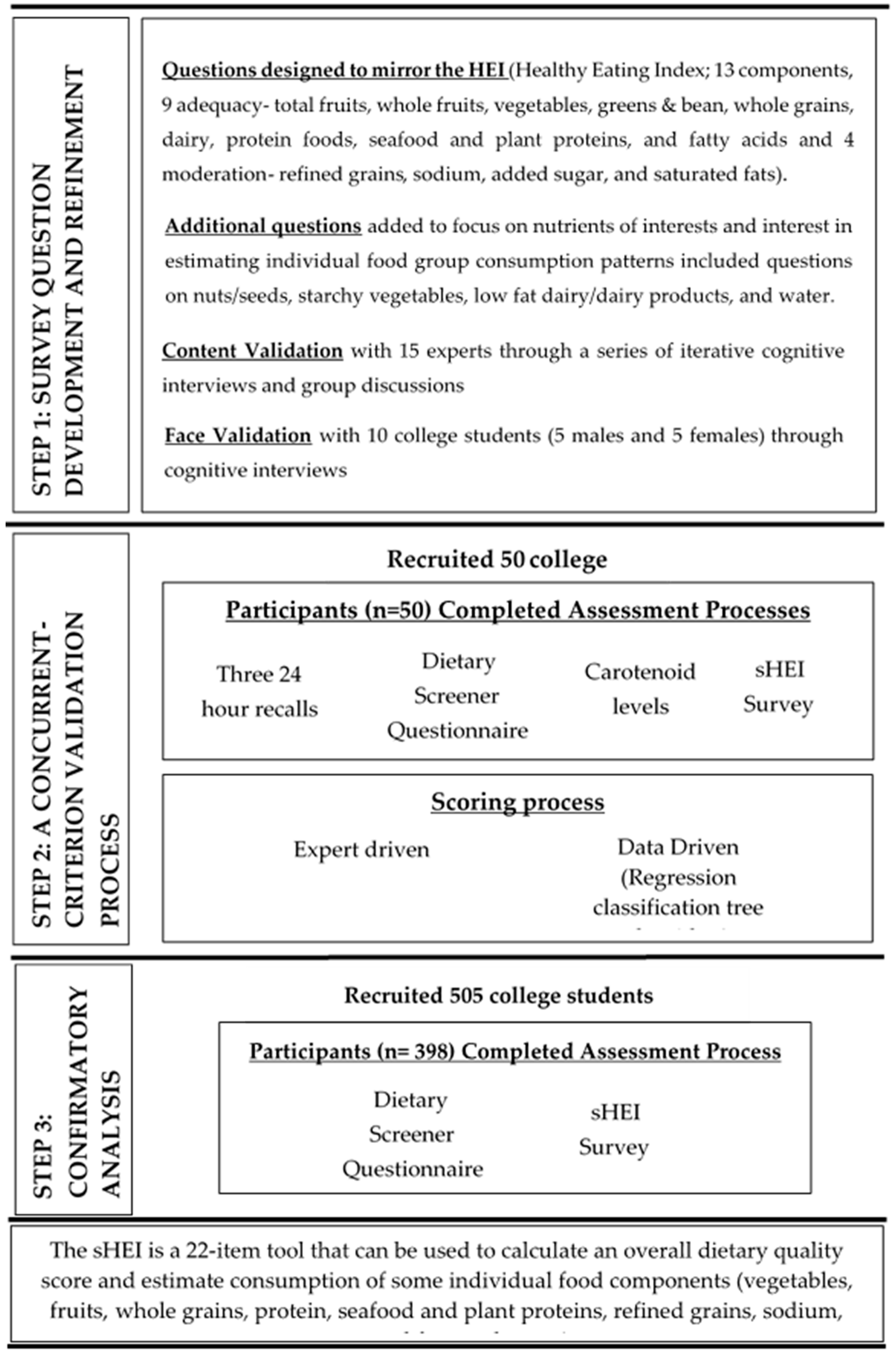
2. Materials and Methods
2.1. Survey Question Development and Refinement
2.2. A Concurrent Criterion Validation Process
2.3. Confirmatory Analysis
3. Results
3.1. DQ Scoring Rules Interpretation
3.2. Food Group Intake Correlation
3.3. Confirmatory Analysis
3.4. Overall Tool
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A. The sHEI Survey (The Original Survey Has Pictures with Each Question. That Version Is Available upon Request with the Contact Author.)
Q1 (Fruit)
Q2 (Fruitjuice)
Q3 (Vege)
Q4 (Greenvege)
Q5 (Starchy)
Q6 (Grains)
Q7 (Grains2) If “Less Than 1” is Selected for Q6
Q8 (Wholegrains)
Q9 (Wholegrains2) If “Less Than 1” is Selected for Q8
Q10 (Milk)
Q11 (Milk2) If “Less Than 1” is Selected for Q10
Q12 (Lowfatmilk)
Q13 (Lowfatmilk2) If “Less Than 1” is Selected for Q12
Q14 (Beans)
Q15 (Nutseeds)
Q16 (Seafood)
Q17 (Seafood2) If “Less Than 1” is Selected for Q16
Q18 (Ssb)
Q19 (Ssb2) If “Less Than 1” is Selected for Q18
Q20 (Addedsugars)
Q21 (Satfat)
Q22 (Water)
Appendix B. sHEI Scoring Instructions for Estimating sHEI Total Dietary Quality Score
| Total Fruits Component (total_fruits), 0–5 |
| IF Q1 (fruit) = 1 THEN total_fruits_Q1 = 0; IF Q1 (fruit) = 2 THEN total_fruits_Q1 = 2; IF Q1 (fruit) = 3 THEN total_fruits_Q1 = 3.5; IF Q1 (fruit) = 4,5,6,7 THEN total_fruits_Q1 = 5. IF Q2 (fruitjuice) = 1 THEN total_fruits_Q2 = 0; IF Q2 (fruitjuice) = 2 THEN total_fruits_Q2 = 2; IF Q2 (fruitjuice) = 3 THEN total_fruits_Q2 = 3.5; IF Q2 (fruitjuice) = 4,5,6,7 THEN total_fruits_Q2 = 5. total_fruits = total_fruits_Q1 + total_fruits_Q2. IF total_fruits > 5 THEN total_fruits = 5. |
| Whole Fruits Component (whole_fruits), 0–5 |
| IF Q1 (fruit) = 1 THEN whole_fruits = 0; IF Q1 (fruit) = 2 THEN whole_fruits = 2.5; IF Q1 (fruit) = 3,4,5,6,7 THEN whole_fruits = 5. |
| Total Vegetables Component (tot_veg), 0–5 |
| IF Q4 (greenvege) = 1 THEN tot_veg = 1.60; IF Q5 (startchy) = 2,3,4,5,6,7 AND Q4 (greenvege) = 2 THEN tot_veg = 2.46; IF Q5 (startchy) = 2,3,4,5,6,7 AND Q4 (greenvege) = 3,4,5,6,7 THEN tot_veg = 3.24; IF Q5 (startchy) = 1 AND Q4 (greenvege) = 2,3,4,5,6,7 THEN tot_veg = 3.56. |
| Greens and Beans Component (greens_beans), 0–5 |
| IF Q4 (greenvege) = 1 THEN greens_beans_Q7 = 0; IF Q4 (greenvege) = 2,3,4,5,6,7 THEN greens_beans_Q7 = 5. IF Q14 (beans) = 1 THEN greens_beans_Q14 = 0; IF Q14 (beans) = 2,3,4,5,6,7 THEN greens_beans_Q14 = 5. greens_beans = greens_beans_Q4 + greens_beans_Q14. IF greens_beans > 5 THEN greens_beans = 5. |
| Whole Grains Component (whole_grains), 0–10 |
| IF Q8 (wholegrains) = 1 THEN whole_grains = 0.51; IF Gender = M AND Q8 (wholegrains) = 2,3,4,5,6,7 THEN whole_grains = 2.97; IF Gender = F AND Q8 (wholegrains) = 2,3 THEN whole_grains = 5.20; IF Gender = F AND Q8 (wholegrains) = 4,5,6,7 THEN whole_grains = 6.94. |
| Dairy Component (Dairy), 0–10 |
| IF Gender = M AND Q10 (milk) = 1,2,3 THEN dairy = 3.22; IF Gender = F AND Q10 (milk) = 1,2,3 AND Q12 (lowfatmilk) = 1 THEN dairy = 3.32; IF Gender = F AND Q10 (milk) = 1,2,3 AND Q12 (lowfatmilk) = 2,3,4,5,6,7 THEN dairy = 4.81; IF Q10 (milk) = 4,5,6,7 THEN dairy = 6.51. |
| Total Protein Foods Component (tot_proteins), 0–5 |
| IF Gender = M AND Q16_17 (seafood_combo) = 1,2,3,4 THEN tot_proteins = 4.11; IF Gender = M AND Q16_17 (seafood_combo) = 5,6,7,8,9,10,11 THEN tot_proteins = 4.98; IF Gender = F THEN tot_proteins = 4.97. |
| Seafood and Plant Protein Component (Seafood_Plant), 0–5 |
| IF Gender = M AND Q15 (nutseeds) = 1,2 THEN seafood_plant = 0.49; IF Gender = F AND Q15 (nutseeds) = 1,2 THEN seafood_plant = 1.50; IF Q15 (nutseeds) = 3,4,5,6,7 THEN seafood_plant = 4.20. |
| Fatty Acid Ratio Component (Fatty_Acid), 0–10 |
| IF Q10 (milk) = 4,5,6,7 THEN fatty_acid = 2.56; IF Q21 (satfat) = 2,3 AND Q10_11 (milk_combo) = 1,2,3,4,5,6,7 AND Q12–13 (lowfatmilk_combo) = 1,2 THEN fatty_acid = 2.63; IF Q21 (satfat) = 2,3 AND Q10_11 (milk_combo) = 1,2,3,4,5,6,7 AND Q12_13 (lowfatmilk_combo) = 3,4,5,6,7,8,9,10,11 THEN fatty_acid = 4.54; IF Q21 (satfat) = 1 AND Q10_11 (milk_combo) = 1,2,3,4,5,6,7 THEN fatty_acid = 5.93. |
| Refined Grains Component (Refined_Grains), 0–10 |
| IF Q4 (greenvege) = 1 THEN refined_grains = 2.13; IF Q6 (grains) = 3,4,5,6,7 AND Q16 (seafood) = 2,3,4,5,6,7 AND Q4 (greenvege) = 2,3,4,5,6,7 THEN refined_grains = 2.27; IF Q6 (grains) = 3,4,5,6,7 AND Q15 (nutseeds) = 1,2 AND Q16 (seafood) = 1 AND Q4 (greenvege) = 2,3,4,5,6,7 THEN refined_grains = 4.73; IF Q6 (grains) = 3,4,5,6,7 AND Q15 (nutseeds) = 3,4,5,6,7 AND Q16 (seafood) = 1 AND Q4 (greenvege) = 2,3,4,5,6,7 THEN refined_grains = 8.45; IF Q6 (grains) = 1,2 AND Q4 (greenvege) = 2,3,4,5,6,7 THEN refined_grains = 9.25. |
| Sodium Component (Sodium), 0–10 |
| IF Q1 (fruit) = 1,2 AND Q6 (grains) = 3,4,5,6,7 AND Q22 (water) = 3 THEN sodium = 0.70; IF Q1 (fruit) = 3,4,5,6,7 AND Q6 (grains) = 3,4,5,6,7 AND Q22 (water) = 3 THEN sodium = 2.30; IF Q6 (grains) = 3,4,5,6,7 AND Q22 (water) = 1,2 THEN sodium = 4.94; IF Q6 (grains) = 1,2 THEN sodium = 6.07. |
| Added Sugars Component (Added_Sugars), 0–10 |
| IF Q18 (ssb) = 1 THEN sugar_calories_Q18 = 0; IF Q18 (ssb) = 2 THEN sugar_calories_Q18 = 156; IF Q18 (ssb) = 3 THEN sugar_calories_Q18 = 312; IF Q18 (ssb) = 4 THEN sugar_calories_Q18 = 468; IF Q18 (ssb) = 5 THEN sugar_calories_Q18 = 624; IF Q18 (ssb) = 6 THEN sugar_calories_Q18 = 780; IF Q18 (ssb) = 7 THEN sugar_calories_Q18 = 936. IF Q20 (addedsugars) = 1 THEN sugar_calories_Q20 = 130; IF Q20 (addedsugars) = 2 THEN sugar_calories_Q20 = 260; IF Q20 (addedsugars) = 3 THEN sugar_calories_Q20 = 520. sugar_calories = sugar_calories_Q18 + sugar_calories_Q20. IF sugar_calories < =130 THEN added_sugars = 10; IF sugar_calories > 130 AND sugar_calories < 520 THEN added_sugars = 5; IF sugar_calories > =520 THEN added_sugars = 0. |
| Saturated Fats Component (sat_fat), 0–10 |
| IF Q18 (ssb) = 3,4,5,6,7 THEN sat_fat = 1.82; IF Q6 (grains) = 1,2 AND Q18 (ssb) = 1,2 THEN sat_fat = 3.20; IF Q6 (grains) = 3,4,5,6,7 AND Q15 (nutseeds) = 1,2 AND Q18 (ssb) = 1,2 THEN sat_fat = 4.64; IF Q6 (grains) = 3,4,5,6,7 AND Q15 (nutseeds) = 3,4,5,6,7 AND Q18 (ssb) = 1,2 THEN sat_fat = 6.56. |
| Total DQ Score (0–100) |
| tot_score = total_fruits + whole_fruits + tot_veg + greens_beans + whole_grains + dairy + tot_proteins + seafood_plant + fatty_acid + refined_grains + sodium + added_sugars + sat_fat |
Appendix C. sHEI Scoring Instructions for Estimating Food Group Consumption
Total Fruit and Vegetable Servings in Cup Equivalents Including Legumes and French Fries (DSQfvl)
Total Fruit and Vegetable Servings in Cup Equivalents Including Legumes and Excluding French Fries (Dsqfvlnf)
Total Fruit Servings in Cup Equivalents (Dsqfrt)
Total Vegetable Servings in Cup Equivalents Including Legumes and French Fries (Dsqvlall)
Total Vegetable Servings in Cup Equivalents Including Legumes and Excluding French Fries (Dsqvlnf)
Dairy Servings in Cup Equivalents (Dsqdairy)
Added Sugars in Teaspoon Equivalents (Dsqsug)
Added Sugars from Sugar-Sweetened Beverages in Teaspoon Equivalents (DSQssb)
Whole Grains in Ounce Equivalents (DSQwhgr)
Fiber in Grams (DSQfib)
Calcium in Milligrams (DSQcalc)
Green Vegetables in Cup Equivalents
References
- Kant, A.K. Dietary patterns and health outcomes. JAND 2004, 104, 615–635. [Google Scholar] [CrossRef] [PubMed]
- Wirt, A.; Collins, C.E. Diet quality—What is it and does it matter? Public Health Nutr. 2009, 12, 2473–2492. [Google Scholar] [CrossRef] [PubMed]
- Larson, N.; Neumark-Sztainer, D.; Laska, M.N.; Story, M. Young adults and eating away from home: Associations with dietary intake patterns and weight status differ by choice of restaurant. J. Am. Diet. Assoc. 2011, 111, 1696–1703. [Google Scholar] [CrossRef] [PubMed]
- Johnson, K.R.; Appel, J.L.; Brands, V.M.; Howard, H.B.; Lefevre, M.M.; Lustig, M.R.; Sacks, M.F.; Steffen, M.L.; Wylie-Rosett, M.J. Dietary sugars intake and cardiovascular health: A scientific statement from the American Heart Association. Circulation 2009, 120, 1011–1020. [Google Scholar] [CrossRef]
- He, F.J.; Nowson, C.A.; Lucas, M.; MacGregor, G.A. Increased consumption of fruit and vegetables is related to a reduced risk of coronary heart disease: Meta-analysis of cohort studies. J. Hum. Hypertens. 2007, 21, 717–728. [Google Scholar] [CrossRef]
- Willett, W.C. Dietary fats and coronary heart disease. J. Intern. Med. 2012, 272, 13–24. [Google Scholar] [CrossRef]
- Dauchet, L.; Amouyel, P.; Dallongeville, J. Fruit and vegetable consumption and risk of stroke. Neurology 2005, 65, 1193. [Google Scholar] [CrossRef]
- Aune, D.; Chan, D.S.M.; Lau, R.; Vieira, R.; Greenwood, D.C.; Kampman, E.; Norat, T. Dietary fibre, whole grains, and risk of colorectal cancer: Systematic review and dose-response meta-analysis of prospective studies. BMJ 2011, 343, d6617. [Google Scholar] [CrossRef]
- Aune, D.; Chan, D.S.M.; Greenwood, D.C.; Vieira, A.R.; Rosenblatt, D.A.N.; Vieira, R.; Norat, T. Dietary fiber and breast cancer risk: A systematic review and meta-analysis of prospective studies. Ann. Oncol. 2012, 23, 1394–1402. [Google Scholar] [CrossRef]
- Carter, P.; Gray, L.J.; Troughton, J.; Khunti, K.; Davies, M.J. Fruit and vegetable intake and incidence of type 2 diabetes mellitus: Systematic review and meta-analysis. BMJ 2010, 341, c4229. [Google Scholar] [CrossRef]
- Morris, M.C. Nutrition and risk of dementia: Overview and methodological issues. Ann. N. Y. Acad. Sci. 2016, 1367, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Thompson, F.E.; Subar, A.F. Dietary assessment methodology. In Nutrition in the Prevention and Treatment of Disease; Coulston, A., Boushey, C., Eds.; Academic Press: San Diego, CA, USA, 2017; pp. 5–48. [Google Scholar]
- Haines, P.S.; Siega-Riz, A.M.; Popkin, B.M. The Diet Quality Index revised: A measurement instrument for populations. J. Am. Diet. Assoc. 1999, 99, 697–704. [Google Scholar] [CrossRef]
- Kim, S.; Haines, P.S.; Siega-Riz, A.M.; Popkin, B.M. The Diet Quality Index-International (DQI-I) provides an effective tool for cross-national comparison of diet quality as illustrated by China and the United States. J. Nutr. 2003, 133, 3476–3484. [Google Scholar] [CrossRef] [PubMed]
- Serra-Majem, L.; Ribas, L.; Ngo, J.; Ortega, R.M.; García, A.; Pérez-Rodrigo, C.; Aranceta, J. Food, youth and the Mediterranean diet in Spain. Development of KIDMED, Mediterranean Diet Quality Index in children and adolescents. Public Health Nutr. 2004, 7, 931–935. [Google Scholar] [CrossRef] [PubMed]
- Štefan, L.; Prosoli, R.; Juranko, D.; Čule, M.; Milinović, I.; Novak, D.; Sporiš, G. The reliability of the Mediterranean Diet Quality Index (KIDMED) questionnaire. Nutrients 2017, 9, 419. [Google Scholar] [CrossRef] [PubMed]
- Burggraf, C.; Teuber, R.; Brosig, S.; Meier, T. Review of a priori dietary quality indices in relation to their construction criteria. Nutr. Rev. 2018, 76, 747–764. [Google Scholar] [CrossRef]
- Kant, A.K.; Leitzmann, M.F.; Park, Y.; Hollenbeck, A.; Schatzkin, A. Patterns of recommended dietary behaviors predict subsequent risk of mortality in a large cohort of men and women in the United States. J. Nutr. 2009, 139, 1374–1380. [Google Scholar] [CrossRef]
- Yang, J.; Farioli, A.; Korre, M.; Kales, S.N. Modified Mediterranean diet score and cardiovascular risk in a North American working population. PLoS ONE 2014, 9, e87539. [Google Scholar] [CrossRef]
- Asghari, G.; Mirmiran, P.; Yuzbashian, E.; Azizi, F. A systematic review of diet quality indices in relation to obesity. Br. J. Nutr. 2017, 117, 1055–1065. [Google Scholar] [CrossRef]
- Waijers, P.M.; Feskens, E.J.; Ocké, M.C. A critical review of predefined diet quality scores. Br. J. Nutr. 2007, 97, 219–231. [Google Scholar] [CrossRef]
- Healthy Eating Index. Available online: https://www.fns.usda.gov/hei-scores-americans (accessed on 11 May 2020).
- 2015–2020 Dietary Guidelines for Americans. Available online: https://health.gov/our-work/food-nutrition/2015-2020-dietary-guidelines/guidelines/ (accessed on 1 May 2020).
- Reedy, J.; Lerman, J.L.; Krebs-Smith, S.M.; Kirkpatrick, S.I.; Pannucci, T.E.; Wilson, M.M.; Subar, A.F.; Kahle, L.L.; Tooze, J.A. Evaluation of the Healthy Eating Index-2015. J. Acad. Nutr. Diet. 2018, 118, 1622–1633. [Google Scholar] [CrossRef] [PubMed]
- Guenther, P.M.; Kirkpatrick, S.I.; Reedy, J.; Krebs-Smith, S.M.; Buckman, D.W.; Dodd, K.W.; Casavale, K.O.; Carroll, R.J. The Healthy Eating Index-2010 is a valid and reliable measure of diet quality according to the 2010 Dietary Guidelines for Americans. J. Nutr. 2014, 144, 399–407. [Google Scholar] [CrossRef] [PubMed]
- Guenther, P.M.; Reedy, J.; Krebs-Smith, S.M.; Reeve, B.B.; Basiotis, P.P. Development and Evaluation of the Healthy Eating Index-2005; Technical Report; U.S. Department of Agriculture, Center for Nutrition Policy and Promotion: Washington, DC, USA, 2007.
- Rimm, E.B.; Giovannucci, E.L.; Stampfer, M.J.; Colditz, G.A.; Litin, L.B.; Willett, W.C. Reproducibility and validity of an expanded self-administered semiquantitative food frequency questionnaire among male health professionals. Am. J. Epidemiol. 1992, 135, 1114–1126, discussion 1127–1136. [Google Scholar] [CrossRef]
- Block, C.L.; Hartman, A.M.; Scoppa, S.M. Revision of dietary analysis software for the Health Habits and History Questionnaire. Am. J. Epidemiol. 1994, 139, 1190–1196. [Google Scholar] [CrossRef] [PubMed]
- Millen, A.E.; Midthune, D.; Thompson, F.E.; Kipnis, V.; Subar, A.F. The National Cancer Institute Diet History Questionnaire: Validation of Pyramid Food Servings. Am. J. Epidemiol. 2005, 163, 279–288. [Google Scholar] [CrossRef] [PubMed]
- Poslusna, K.; Ruprich, J.; de Vries, J.H.M.; Jakubikova, M.; van’t Veer, P. Misreporting of energy and micronutrient intake estimated by food records and 24 hour recalls, control and adjustment methods in practice. Br. J. Nutr. 2009, 101, S73–S85. [Google Scholar] [CrossRef]
- Prentice, R.L.; Mossavar-Rahmani, Y.; Huang, Y.; Van Horn, L.; Beresford, S.A.A.; Caan, B.; Tinker, L.; Schoeller, D.; Bingham, S.; Eaton, C.B.; et al. Evaluation and comparison of food records, recalls, and frequencies for energy and protein assessment by using recovery biomarkers. Am. J. Epidemiol. 2011, 174, 591–603. [Google Scholar] [CrossRef]
- Neuhouser, M.L.; Tinker, L.; Shaw, P.A.; Schoeller, D.; Bingham, S.A.; Horn, L.V.; Beresford, S.A.A.; Caan, B.; Thomson, C.; Satterfield, S.; et al. Use of recovery biomarkers to calibrate nutrient consumption self-reports in the Women’s Health Initiative. Am. J. Epidemiol. 2008, 167, 1247–1259. [Google Scholar] [CrossRef]
- Thompson, F.E.; Midthune, D.; Kahle, L.; Dodd, K.W. Development and evaluation of the National Cancer Institute’s Dietary Screener Questionnaire Scoring Algorithms. J. Nutr. 2017, 147, 1226–1233. [Google Scholar] [CrossRef]
- Scalbert, A.; Brennan, L.; Manach, C.; Andres-Lacueva, C.; Dragsted, L.O.; Draper, J.; Rappaport, S.M.; van der Hooft, J.J.J.; Wishart, D.S. The food metabolome: A window over dietary exposure. Am. J. Clin. Nutr. 2014, 99, 1286–1308. [Google Scholar] [CrossRef]
- Manach, C.; Brennan, L.; Dragsted, L.O. Using metabolomics to evaluate food intake: Applications in nutritional epidemiology. In Metabolomics as a Tool in Nutrition Research; Sebedio, J.L., Brennan, L., Eds.; Elsevier Science & Technology: Oxford, UK, 2014. [Google Scholar]
- Morgan, E.H.; Graham, M.L.; Marshall, G.A.; Hanson, K.L.; Seguin-Fowler, R.A. Serum carotenoids are strongly associated with dermal carotenoids but not self-reported fruit and vegetable intake among overweight and obese women. Int. J. Behav. Nutr. Phy. 2019, 16, 104. [Google Scholar] [CrossRef] [PubMed]
- Couillard, C.; Lemieux, S.; Vohl, M.-C.; Couture, P.; Lamarche, B. Carotenoids as biomarkers of fruit and vegetable intake in men and women. Br. J. Nutr. 2016, 116, 1206–1215. [Google Scholar] [CrossRef] [PubMed]
- Mayne, S.T.; Cartmel, B.; Scarmo, S.; Jahns, L.; Ermakov, I.V.; Gellermann, W. Resonance Raman spectroscopic evaluation of skin carotenoids as a biomarker of carotenoid status for human studies. Arch. Biochem. Biophys. 2013, 539, 163–170. [Google Scholar] [CrossRef] [PubMed]
- Scarmo, S.; Henebery, K.; Peracchio, H.; Cartmel, B.; Lin, H.; Ermakov, I.V.; Gellermann, W.; Bernstein, P.S.; Duffy, V.B.; Mayne, S.T. Skin carotenoid status measured by resonance Raman spectroscopy as a biomarker of fruit and vegetable intake in preschool children. Eur. J. Clin. Nutr. 2012, 66, 555–560. [Google Scholar] [CrossRef]
- Prinz, N.; Bohn, B.; Kern, A.; Püngel, D.; Pollatos, O.; Holl, R.W. Feasibility and relative validity of a digital photo-based dietary assessment: Results from the Nutris-Phone study. Public Health Nutr. 2019, 22, 1160–1167. [Google Scholar] [CrossRef]
- Boushey, C.J.; Spoden, M.; Zhu, F.M.; Delp, E.J.; Kerr, D.A. New mobile methods for dietary assessment: Review of image-assisted and image-based dietary assessment methods. Proc. Nutr. Soc. 2017, 76, 283–294. [Google Scholar] [CrossRef]
- Boushey, C.J.; Spoden, M.; Delp, E.J.; Zhu, F.; Bosch, M.; Ahmad, Z.; Shvetsov, Y.B.; DeLany, J.P.; Kerr, D.A. Reported energy intake accuracy compared to doubly labeled water and usability of the mobile food record among community dwelling adults. Nutrients 2017, 9, 312. [Google Scholar] [CrossRef]
- Tsang, S.; Royse, C.F.; Terkawi, A.S. Guidelines for developing, translating, and validating a questionnaire in perioperative and pain medicine. Saudi J. Anaesth. 2017, 11, S80–S89. [Google Scholar] [CrossRef]
- Cheah, J.H.; Sarstedt, M.; Ringle, C.M.; Ramayah, T.; Ting, H. Convergent validity assessment of formatively measured constructs in PLS-SEM: On using single-item versus multi-item measures in redundancy analyses. Int. J. Contemp. Hosp. Manag. 2018, 30, 3192–3210. [Google Scholar] [CrossRef]
- Yusoff, M.S.B. ABC of response process validation and face validity index calculation. Educ. Med. J. 2019, 11, 55–61. [Google Scholar] [CrossRef]
- Healthy Eating Index (HEI) 2019. Available online: http://www.ncc.umn.edu/healthy-eating-index-hei/ (accessed on 20 May 2019).
- Breiman, L.; Friedman, J.; Olshen, R.; Stone, C. Classification and Regression Trees; CRC Press: Pacific Grove, CA, USA, 1984. [Google Scholar]
- Mukaka, M.M. Statistics corner: A guide to appropriate use of correlation coefficient in medical research. Malawi Med. J. 2012, 24, 69–71. [Google Scholar] [PubMed]
- Frølich, W.; Aman, P. Whole grain for whom and why? Food Nutr. Res. 2010, 54, 5056. [Google Scholar]
| Dietary Factor and Instrument | 24 h Recall | sHEI | DSQ | |||
|---|---|---|---|---|---|---|
| Mean | ±sd | Mean | ±sd | Mean | ±sd | |
| Total vegetable servings in cup equivalents (including legumes and French fries) | 1.37 | ±0.83 | 1.31 | ±0.59 | 1.55 | ±0.35 |
| Total vegetable servings in cup equivalents including legumes and excluding French fries | 1.12 | ±0.82 | 1.04 | ±0.58 | 1.42 | ±0.37 |
| Greens and beans servings in cup equivalents | 0.28 | ±0.31 | 0.22 | ±0.15 | N/A | N/A |
| Total fruit servings in cup equivalents | 0.68 | ±0.72 | 0.57 | ±0.49 | 1.06 | ±0.45 |
| Total fruit and vegetable servings in cup equivalents | 2.05 | ±1.33 | 1.92 | ±0.67 | 2.59 | ±0.74 |
| Total fruit and vegetable servings in cup equivalents including legumes and excluding French fries | 1.80 | ±1.34 | 1.66 | ±0.77 | 2.50 | ±0.73 |
| Whole fruit servings in cup equivalents | 0.59 | ±0.63 | 0.48 | ±0.37 | N/A | N/A |
| Dairy servings in cup equivalents | 1.61 | ±2.18 | 1.35 | ±0.67 | 1.79 | ±0.73 |
| Whole grain servings in ounce equivalents | 1.46 | ±1.41 | 1.23 | ±0.77 | 0.80 | ±0.31 |
| Total protein servings in ounce equivalents | 6.77 | ±2.79 | 6.60 | ±1.67 | N/A | N/A |
| Seafood and plant protein servings in ounce equivalents | 1.37 | ±1.51 | 1.09 | ±0.94 | N/A | N/A |
| Refined grains in ounce equivalents | 6.01 | ±6.59 | 5.39 | ±2.86 | N/A | N/A |
| Sodium (g) | 3.39 | ±1.88 | 3.30 | ±1.11 | N/A | N/A |
| Added sugars in tsp equivalents 1 | 14.10 | ±9.32 | 13.28 | ±5.53 | 17.15 | ±8.18 |
| Added sugars from sugar-sweetened beverages in tsp equivalents 2 | 5.81 | ±7.95 | 4.49 | ±4.70 | 7.90 | ±7.02 |
| Fiber (g) | 18.02 | ±9.33 | 17.40 | ±5.32 | 16.68 | ±3.48 |
| Calcium (mg) | 975.59 | ±657.74 | 936.20 | ±404.77 | 1049.21 | ±242.11 |
| HEI Component | Correlation |
|---|---|
| (1) Total Fruits | 0.64 |
| (2) Whole Fruits | 0.57 |
| (3) Total Vegetables | 0.53 |
| (4) Greens and Beans | 0.49 |
| (5) Whole Grains | 0.62 |
| (6) Dairy | 0.48 |
| (7) Total Protein Foods | 0.51 |
| (8) Seafood and Plant Proteins | 0.56 |
| (9) Fatty Acids | 0.44 |
| (10) Refined Grains | 0.62 |
| (11) Sodium | 0.58 |
| (12) Added Sugars | 0.47 |
| (13) Saturated Fats | 0.51 |
| Total Score | 0.79 |
| Dietary Factor from the DSQ (Predicted Intake per Day) | (a) Training Sample (n = 50) | (b) Confirmatory Sample (n = 398) |
|---|---|---|
| Total fruit and vegetable servings in cup equivalents including legumes and French fries (DSQfvl) | 0.74 | 0.49 |
| Total fruit and vegetable servings in cup equivalents including legumes and excluding French fries (DSQfvlnf) | 0.73 | 0.49 |
| Total fruit servings in cup equivalents (DSQfrt) | 0.85 | 0.49 |
| Total vegetable servings in cup equivalents including legumes and French fries (DSQvlall) | 0.63 | 0.60 |
| Total vegetable servings in cup equivalents including legumes and excluding French fries (DSQvlnf) | 0.63 | 0.59 |
| Dairy servings in cup equivalents (DSQdairy) | 0.69 | 0.49 |
| Added sugars in tsp (DSQsug) | 0.70 | 0.49 |
| Added sugars from sugar-sweetened beverages in tsp equivalents (DSQssb) | 0.74 | 0.57 |
| Whole grains in ounce equivalents (DSQwhgr) | 0.65 | 0.29 |
| Fiber in grams (DSQfib) | 0.67 | 0.44 |
| Calcium in milligrams (DSQcalc) | 0.78 | 0.66 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Colby, S.; Zhou, W.; Allison, C.; Mathews, A.E.; Olfert, M.D.; Morrell, J.S.; Byrd-Bredbenner, C.; Greene, G.; Brown, O.; Kattelmann, K.; et al. Development and Validation of the Short Healthy Eating Index Survey with a College Population to Assess Dietary Quality and Intake. Nutrients 2020, 12, 2611. https://doi.org/10.3390/nu12092611
Colby S, Zhou W, Allison C, Mathews AE, Olfert MD, Morrell JS, Byrd-Bredbenner C, Greene G, Brown O, Kattelmann K, et al. Development and Validation of the Short Healthy Eating Index Survey with a College Population to Assess Dietary Quality and Intake. Nutrients. 2020; 12(9):2611. https://doi.org/10.3390/nu12092611
Chicago/Turabian StyleColby, Sarah, Wenjun Zhou, Chelsea Allison, Anne E. Mathews, Melissa D. Olfert, Jesse Stabile Morrell, Carol Byrd-Bredbenner, Geoffrey Greene, Onikia Brown, Kendra Kattelmann, and et al. 2020. "Development and Validation of the Short Healthy Eating Index Survey with a College Population to Assess Dietary Quality and Intake" Nutrients 12, no. 9: 2611. https://doi.org/10.3390/nu12092611
APA StyleColby, S., Zhou, W., Allison, C., Mathews, A. E., Olfert, M. D., Morrell, J. S., Byrd-Bredbenner, C., Greene, G., Brown, O., Kattelmann, K., & Shelnutt, K. (2020). Development and Validation of the Short Healthy Eating Index Survey with a College Population to Assess Dietary Quality and Intake. Nutrients, 12(9), 2611. https://doi.org/10.3390/nu12092611






