Abstract
Background: COVID-19 has changed the world and strongly affected the health of the people and the quality of their life. These changes might impact employees’ physical activity (PA) and sedentary behavior (SB). This study aimed to summarize the literature focusing on the COVID-19-caused changes in physical activity and sedentary behavior among the adult working population. Methods: Literature searches were conducted in June 2021 using multiple electronic databases. The following keywords and synonyms were used during the searching process: physical activity, sedentary behavior, COVID-19, employee. After the data cleaning process (duplicates, inclusion criteria), the title and the abstract of all manuscripts from the searches were screened independently by two reviewers. Results: Thirty-nine manuscripts were selected as a result of the searching process. Of these, 5 were SB related, 15 were PA related and 19 addressed both PA and SB. There were longitudinal (10), cross-sectional (28) and a case study (1) in the selected manuscripts. The majority of studies were conducted in the USA (6) and Europe (18), and four studies examined the PA and/or SB in multiple countries. The majority (34 studies) of the studies used subjective, self-reported, but mostly before-validated questionnaires. Objective measures were less common and used only 12.8% of the examined studies. Moreover, 76.4% of the studies described an overall decrease in the amount of PA during the COVID-19 pandemic. In three cases, researchers observed an increase in PA among the workers. Five studies reported no significant changes in the amount of PA during the pandemic. As far as SB is concerned, 18 out of 24 of the studies reported an overall increase in the amount of SB between the two periods. Four manuscripts reported no significant change in the amount of SB, and there was only one manuscript in the examined studies that reported an overall decrease in the SB time before and during the COVID-19 pandemic. Discussion: There is no doubt that the COVID-19 pandemic, including lockdown and work from home (WFH) policies, impaired the PA and SB level of the populations. This period has delivered an important message for the adult working population as well. They should be as active as possible and avoid high levels of SB and uninterrupted sitting time. Therefore, organizations, policies and public health bodies should motivate workers, especially office workers, to be more active and interventions must be developed to mitigate the negative effects of the COVID-19 on PA and SB.
1. Introduction
People’s lifestyles have changed significantly in recent years, with an increasing number of people living a sedentary lifestyle, mainly in developed countries. According to Tremblay et al. [1], sedentary behavior can be defined as any waking behavior characterized by an energy expenditure ≤ 1.5 metabolic equivalents (METs), put simply as any time people are sitting or lying down. Due to the significant increase in SB levels in most developed countries over the past century, occupational SB has appeared as a substantial public health issue. The main contributor to the daily sedentary time for workers is the substantial sitting time at the workplace [2]. People may spend three-quarters of the workday in SB [3], and according to Kazi et al., if people spend more time sitting during the workday, they will spend more time sitting during their leisure time [4]. SB should separate from the lack of physical activity because people can be sufficiently active according to the PA guidelines while sitting too much [5,6]. High sedentary times (for example, during work time) have been associated with harmful health effects independent of PA [7], including premature all-cause mortality [8], overweight, obesity, cancer and chronic illnesses such as cardiovascular diseases, metabolic syndrome, type 2 diabetes and low back pain [9,10,11].
Insufficient PA is also a key risk factor for the above-mentioned non-communicable diseases (NCDs) and is currently one of the leading risk factors for mortality worldwide [12,13,14]. According to Lee et al., the inactive lifestyle contribution to global premature deaths is approximately 9% [12]. Therefore, it is indisputable that being regularly physically active is an important determinant of health and plays a crucial role in people’s health and quality of life; consequently, it is an essential issue in public health recommendations. The World Health Organization (WHO) recommends 150 min of moderate-intensity or at least 75 min of vigorous-intensity aerobic physical activity, or an equivalent combination of moderate- and vigorous-intensity activity, throughout the week for substantial health benefits [15]. However, worldwide, approximately 27.5% of adults and 81% of adolescents do not meet the recommendations for aerobic exercise, and therefore, there is an urgent need to increase physical activity and reduce sedentary time [16].
Due to the rapid technological development nowadays, more and more jobs have become sedentary, and more adults are employed in low activity occupations where they could accumulate the time of SB, which may contribute to the risk of NCDs [17,18,19,20].
Furthermore, the COVID-19 pandemic has changed the world and strongly affected the health of the people and the quality of their life (more than 190 million people with COVID-19, causing more than 4.1 million deaths worldwide) [21]. As suggested by the WHO, national containment strategies (e.g., social distancing) were implemented worldwide by national authorities to mitigate the spread of the COVID-19 virus. These national restrictions have interrupted normal daily activities such as PA. This new virus has significantly altered employment as well: businesses had to close for a while or constantly, and many workers (especially office workers) were required to shift to a remote working environment (working for home—WFH) to stay safe [22]. The conventional concept of WFH has been reconsidered by the COVID-19, and WFH has become a policy priority for most governments and presumably, after the pandemic, it will become more common among businesses [23]. The increase in WFH during the pandemic may have negative impacts on working conditions, and workers may have adapted unhealthy lifestyles. This may result in an increase in SB and a decrease in PA [24].
Since the initial lockdown restrictions were implemented, the number of studies related to PA and SB during the COVID-19 pandemic has been growing. Previous literature on PA or SB and the present pandemic has mainly focused on the general population [25,26,27,28,29,30,31,32], the older population [33,34,35], people with different chronic illnesses [36,37,38], health care professionals [39] or athletes [40,41]. Employees, and especially office workers, are underrepresented. Nevertheless, they are often included in the participants of these studies. However, no study, to the best of our knowledge, has yet synthesized the literature in connection with the COVID-19 pandemic and the changes of the employees’ PA and SB. In this paper, we try to conduct a systematic review on the COVID-19-caused changes in the level of PA and SB among employees. The main purposes of this study were, on the one hand, to collect studies which directly or indirectly investigate the employees’ PA and SB overall changes during the COVID-19 pandemic and, on the other hand, to identify the home office effects on the level of PA and SB.
2. Materials and Methods
In June 2021, a literature search was performed, and the scientific journal articles were retrieved from ScienceDirect, PubMed and Scopus. We used these sources since all of them provide immediate access to the relevant studies. Manuscripts were selected according to the following inclusion and exclusion criteria:
Inclusion criteria:
- Study populations involving healthy adult employees (in any country);
- Study outcomes investigating any form of PA and/or SB changes before and during the COVID-19 lockdown;
- Manuscripts written in English language;
- No restriction used in connection with study design;
- Publication type involving research papers.
Exclusion criteria:
- Study population involving children, adolescents, older or retired people or with a specific disease condition;
- Study outcomes not investigating the change of the PA and/or SB before and during the COVID-19 lockdown;
- Study not examining the employees’ subgroup;
- Publication type involving letters to editor, comments, editorials, reviews and recommendations.
At the end of the journal database search and selection process, an additional academic search was conducted, which was not restricted to only journal articles. Dissertations, master theses and project works were examined in connection with the topic. The same inclusion and exclusion criteria were applied.
To cover the relevant studies, literature searches will only include papers published since November 2019. All articles whose topics were related to the present study were taken into consideration. During the search, Boolean operators (such as AND or OR) and the following keywords were used (Table 1):

Table 1.
Search strategy: databases and searching terms.
COVID-19, novel coronavirus, physical activity, sedentary, physical inactivity, sitting, worker, working from home, employment, employee, occupation.
Duplicates were removed with the use of Zotero reference management software. The title and the abstract of all manuscripts from the searches were screened independently by two reviewers (G.R., É.B.B.), who determined the acceptability of the studies according to the inclusion and exclusion criteria. If disagreements aroused between the reviewers during the selection process, a third reviewer (K.R.-Ó.) was consulted; this was necessary on five occasions. Selected full-text manuscripts were then examined by G.R. and reviewed by É.B.B., K.R.-Ó., K.K., Z.B., I.F. and P.L. In order to identify other sources, the reference lists of the selected full-text manuscripts were further manually searched.
Reviewers picked out the following data from the selected studies: author (year of publication), the title of the manuscript, country, sample size, PA or SB assessment, study design, working population of the sample, change direction in SB, key findings related to SB, change direction in PA, key findings related to PA, main outcomes and types of outcomes.
3. Results
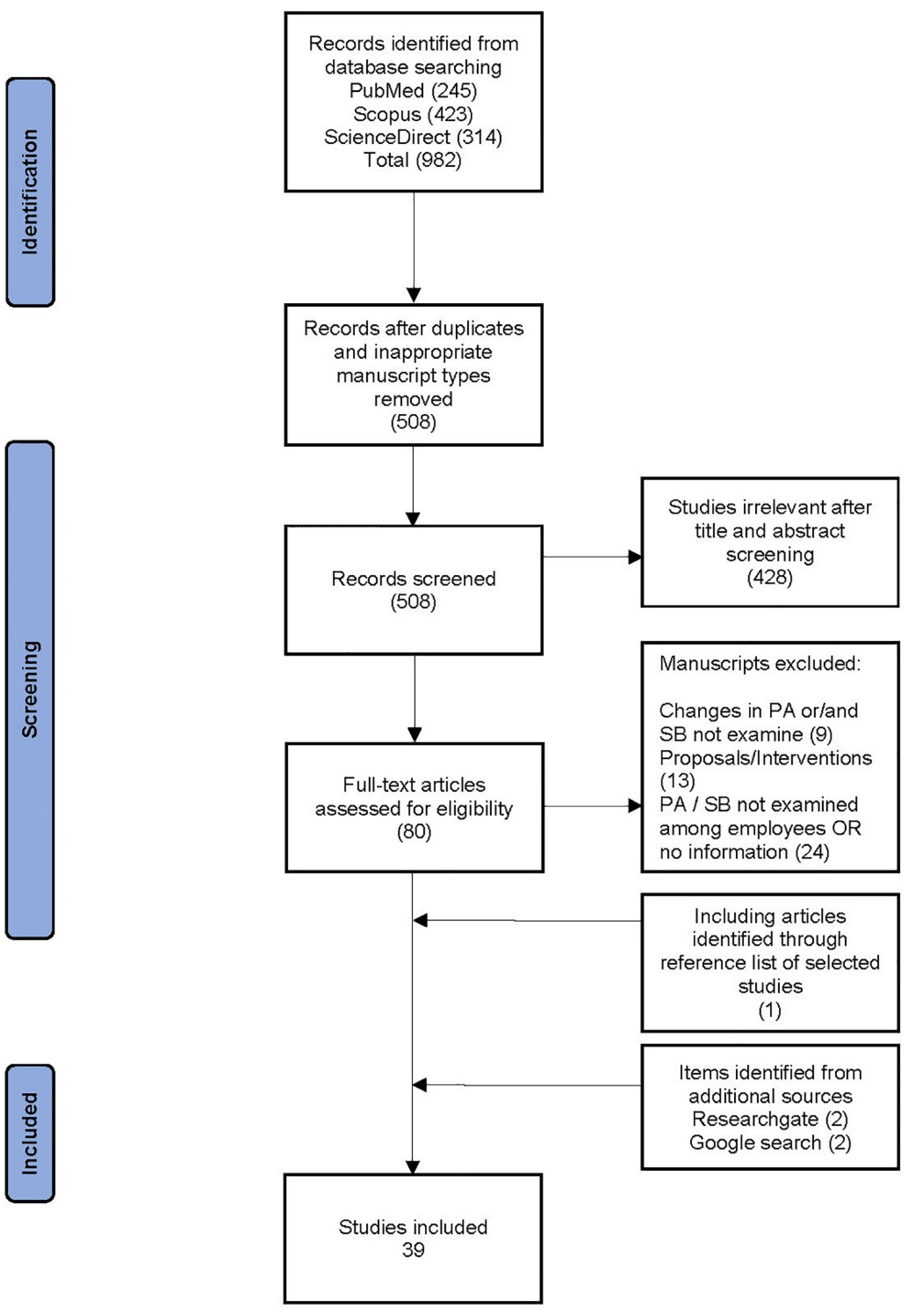
Our search identified a total of 982 records. When duplicates were removed, studies were limited to English and human samples, and inappropriate manuscript types were excluded: a total of 508 records were retained. After title and abstract screening, we located 80 full-text articles. The citations of these papers were then screened. An additional nine eligible papers were identified and one of these was retained after full-text review. At the end of the selection process, additional sources were screened to find other relevant studies, and finally, four studies were added to the selection. Due to the actuality of the research topic, we have found several early-stage studies, and three of them were selected, for which the publications are currently in the peer-review process phase [42,43,44]. In two cases, we selected a high-quality master’s thesis or project work [45,46].
The flowchart of the search and selection process is shown in Figure 1.
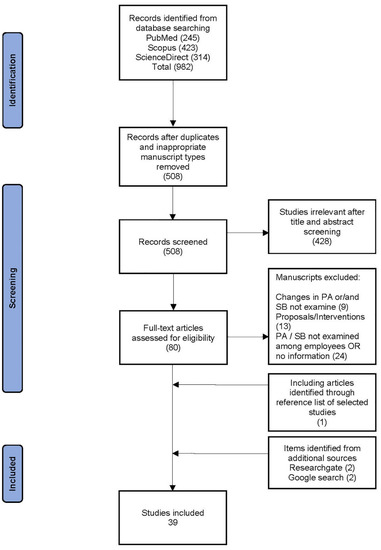
Figure 1.
Study selection process.
3.1. Main Characteristics of the Studies
Table 2 contains a summary of the characteristics of the studies reviewed. Thirty-nine manuscripts were selected as a result of the searching process. Five manuscripts were SB related, 15 manuscripts were PA related and 19 manuscripts addressed both PA and SB. There were longitudinal studies (10), cross-sectional studies (28) and a case study (1) in the selected manuscripts. The majority of the studies were conducted in Europe (18) and the USA (6), and four studies examined the PA and/or SB in multiple countries.

Table 2.
Characteristics of included studies.
Of the studies, 20 out of 39 had focused on only the employees, and 16 manuscripts had studied the general population but directly investigated the employment status. An average 56.35% of the examined population was employed and investigated directly of these studies. In three cases [47,48,49], there was no information about the ratio of employees in the examined population, but the daily occupational PA was determined, and we considered this information. The total of 39 included manuscripts yielded a total of 118,022 participants with a range of job types. Twelve studies especially examined office workers [23,46,50,51,52,53,54,55,56,57,58,59], and 11 studies [22,23,42,44,45,46,52,60,61,62,63] examined WFH or remote working.
3.2. Measurement Types and Outcomes of the Studies
Objective measures were less common and were used in only 12.8% of the examined studies. Different smart technologies were used to identify PA patterns; two times activity trackers [50,51] and accelerometers [52,53] were used, one time a mobile application was used [64] and one time a mixed methodology was used (next to the objective measurement self-report measure International Physical Activity Questionnaire—short form also employed to collect additional information) [65]. The majority (35 studies) of the studies used subjective, self-reported but generally before-validated questionnaires (e.g., International Physical Activity Questionnaire, Global Physical Activity Questionnaire, Occupational Sitting and Physical Activity Questionnaire).
A range of outcomes was used to categorize PA and SB changes in the form of time (e.g., METs/min/week, step counts/day or different types of PA levels in minutes or hours/day or week) and as a percentage of the population.
3.3. PA in Adult Working Populations
In total, 76.4% of the studies described an overall decrease in the level of PA during the COVID-19 pandemic. In two cases, researchers observed an increase in PA among working adults. In the case of Franco et al. [54], respondents have been participating in health promotion programs during COVID-19 and maybe for this reason an increase has been detected in PA levels. In the other case [42], there were no specific promoting circumstances related to the PA level increase. Five studies [22,55,57,58,76] reported no significant changes in the level of PA between the periods. Studies addressed changes in PA in different forms: time spent on PA, step counts, percentage of the sample, comparison of results with the previous national data.
3.4. SB in Adult Working Populations
As far as SB is concerned, 18 out of 24 of the studies reported an overall increase in the amount of SB between the two periods. Four manuscripts [52,53,57,72] reported no significant change in the amount of SB, and there was only one manuscript in the examined studies that reported an overall decrease in the SB time before and during the COVID-19 pandemic among the working adult population. Studies addressed changes in SB in different forms: time spent on PA, step counts, percentage of the sample, comparison of results with the previous national data.
One paper [71] did not directly examine the changes of the amount of PA or SB pre-COVID-19 versus post-COVID-19 lockdown; however, the possible effect of lockdown can be observed. In Taeymans et al. study [71], the employees had a higher median daily sitting time and lower median summed MET minutes per week than other examined groups and the prevalence of long sitting time is higher compared to national data.
4. Discussion
The present review provides an overview of studies examining the changes in the employment’s PA and SB during the COVID-19 pandemic. We identified 39 studies including different types of employments from several countries. Regardless of the applied methodology, a greater part of the investigated studies found that SB level increased and PA level decreased among the employees during the lockdown period.
Three-quarters of the studies reported negative effects on PA during the COVID-19 pandemic. In two cases, researchers observed an increase in PA among the employees, and six studies reported no significant changes in the amount of PA pre-COVID-19 versus post-COVID-19 lockdown among employees. Although [78] examined the impacts of the pandemic on a general population, our results are in line with the findings by this systematic review [78], which revealed that most of the selected studies found that the level of PA declined during the lockdown period. Several other studies examining different population groups found similar effects of the COVID-19 lockdown on participants’ PA and sedentary patterns. For example, an online survey that examined the effects of the COVID-19 pandemic on PA among children in the USA reported that the parents perceived a decline in the PA level of the children as compared to before the pandemic [79]. In a mini-review [80], the authors reported a significant reduction of PA levels among university students compared to pre-lockdown values. Moreover, another review study investigating adults with physical disabilities and/or chronic diseases found a decrease in PA during the first wave of COVID-19 in almost every examined study [81].
A variety of methodologies and PA measures were used in the investigated articles (Table 2). Most of the studies had a cross-sectional design and applied mostly validated self-reported questionnaires, and only 12.8% of the research used objective measures. To avoid the limitations of the self-reported questionnaires, using objective measurement (e.g., accelerometer, pedometer) might be a solution [64]. Future research should focus on objective, directly comparable, accelerometer-based data where it is possible. For example, worldwide data from different wearable activity trackers revealed an overall decrease in step counts during the COVID-19 lockdown [82,83,84]. Tison et al. [85] examined the changes in step count before and during the COVID-19 lockdown. The study found a decline in smartphone-derived step counts based on aggregated data. Differences can be observed between regions due to the regional variation in COVID-19 timing, enforcement, and behavior change [85].
Another study [64] also examined smartphone-based step counts from 815 Chinese adults before, during and after the lockdown. The study reported a sharp decline in daily step counts due to the abrupt nature of the lockdown, followed by a slow, steady increase, and almost four months after reopening, the total step counts were still slightly below the baseline level [64]. Objective data would be able to highlight the long-term consequences of the pandemic on peoples’ PA level changes. The prediction of the long-term health effects of the lower PA level during and after the COVID-19 pandemic is difficult. However, a study from Japan reported a lasting significant decrease in PA level over three years following the 2011 earthquake and tsunami [24,86].
A potential reason for the decline in PA level among working adults might be that, on the one hand, during COVID-19, national governments prohibited several activities such as the majority of outdoor and social activities and most gyms, leisure and sporting facilities closed, therefore, people found it difficult to be active. On the other hand, additional responsibilities (e.g., school-aged children at home) for working adults and especially home-working employees also decreased opportunities to be active.
In contrast with the studies that showed a decline in PA levels among working adults, in two studies from Sweden and two studies from Switzerland, no changes in PA level were reported during the COVID-19 pandemic. These results can be explained by the less strict lockdown measures in the two countries: the stricter the confinement measures, the more likely that PA patterns are affected.
In most cases, people working remotely were less active during the COVID-19 lockdown [44,46,62], and those who continued to work at normal routine usually did not observe such a high level of changes in their PA level [52,58]. Dispersedly mode-specific and subgroup-specific increases can be found in different PA levels. However, the total PA levels decreased [70]. For example, in an Estonian [56] study, office workers reported a significant decrease in self-reported PA levels (sport, leisure), although an increase was reported in work-related PA level. However, the total level of PA decreased.
To slow down the spread of the coronavirus, several countries introduced enforcing social distancing, and the severity of these containment measures varies between countries. Lockdown restrictions, including self-isolation, stay at home, physical distancing, travel limitations, restrictions on public movement and banned sports activities and exercise outdoors are just some examples introduced during the pandemic [87]. This new virus has significantly altered people lives, and employment as well, businesses had to close permanently or constantly and many workers (especially office-based workers) were required to shift to a remote working environment (WFH) to stay safe [22]. For example, in Spain, remote work rose from almost 5% to 34% during quarantine [54]. Another study reported that nearly 50% of the participated organization had more than 80% of their employees working from home during the first wave of the COVID-19 pandemic [88]. The rise of remote working during the COVID-19 pandemic was confirmed in several other studies as well [89,90,91,92]. Switching to home offices may have a negative impact on employments’ healthy habits. Employees and especially office workers are already at risk for being physically inactive (spending three-quarters of the workday in SB) [93], and it is especially true during the lockdown and the rise of WFH, which was associated with extended sedentary periods and increased screen time [22,52,54,78,94]. Employees who worked from home spent longer uninterrupted SB time during work time than those who never worked at home [95]. Even more alarming, if people spend more time sitting during the workday, they will spend more time sitting during their leisure time [4,96]. Furthermore, additional responsibilities (e.g., school-aged children) for home-working employees also decrease the opportunities to be active. According to a UK survey, 85% of UK employees with school-age children are balancing homeschooling with work [97]. Not surprisingly, 18 studies out of 24 reported an increase in SB time. In contrast with the studies that showed an increase in SB level among working adults, only four studies reported no changes in SB level during the COVID-19 pandemic (two studies from Sweden and two studies from Switzerland) [52,55,57,71]. These different results could be explained by the less strict lockdown measures in the two countries: the stricter the confinement measures, the more likely SB patterns are affected.
Although Stockwell et al. examined the impacts of the pandemic on a general population, our results are in line with the findings by this systematic review [78], which revealed that most of the selected studies found that the level of SB increased during the lockdown period. Moreover, in one study, despite employees have been participating in a health promotion program (10,000 steps/day), SB was negatively affected during the COVID-19 outbreak. The ratio of sedentary participants significantly increased during the pandemic [54].
Another review study investigating adults with physical disabilities and/or chronic diseases found an increase in SB during the first wave of COVID-19 in almost every examined case [81].
According to McDowell et al. switching to WFH due to the COVID-19 pandemic was associated with greater time spent sitting and was associated with more time spent in SB each day [22,45,46]. Fukushima et al. also support the fact that office workers are very much sedentary while working from home during the COVID-19 regulations, as they reported that WFH workers have 111 more minutes of sedentary behavior per day than non-WFH workers [95].
On the other hand, working from home, or in the office is even better than being unemployed during the pandemic as regards PA and SB. Recent research [22,60,63,69], in accordance with previous research [98], reported a lower level of PA and increased level of SB among unemployed people. In line with these results, previously inactive or low active people at baseline had become less physically active during the COVID-19 pandemic [29,57]. It is important to note that activity change during the COVID-19 lockdown depends on the level of lockdown and the habitual PA [64].
Lack of PA and accumulated SB is a known major health risk factor for poor overall health, premature mortality, and NCDs such as obesity, diabetes, and cardiovascular disease [8,9,11,99,100]. Moreover, it is even more important for older people and people with different chronic illnesses to be active in order to avoid the deterioration of their condition [70,101].
Office or desk workers probably have lower PA levels than other workers [102], therefore, it would be important, on the one hand, for organizations to be able to identify and help to preserve their employees’ health regardless of whether they work from home or go to the office, and on the other hand, for governments and health professionals to encourage workers to be more active. Public health interventions are needed to break uninterrupted SB for all workers and motivate them to increase their PA, especially those who work from home. Innovative smart technologies may also contribute to prevent employees from a sedentary lifestyle and increase PA. For example, digital health coach technology can play in enhancing people’s healthy behavior [103].
A strength of our study was that we conducted a systematic review in connection with the COVID-19 pandemic impacts on a specific population: the employees’ PA and SB. Hence, our review may provide initial insight into the effects of the pandemic on the workers’ activity behavior, and the results may contribute to the development of public health interventions among the adult working population.
Limitations
Although this is a review, the study has some limitations. First of all, the still ongoing pandemic and the novelty of the topic is one of the main limitations of the manuscript. Reviewers made great efforts in the searching process to find all relevant manuscripts; however, some articles may have been overlooked due to the examined databases and the selected searching terms. The majority of the studies applied self-reported subjective questionnaires, which were often based on participants’ retrospective answers where accuracy and objectivity may be questionable. In several studies, the selected sample did not represent the population at a national level. The different occupations and workplaces included in the selected studies also can be a bias. Different methods of assessing SB and PA in the studies also affect the comparison of the results. Finally, our inclusion criteria could be another bias since the present study investigated only the adult working populations and excluded other parts of the population such as adults with physical disabilities and/or chronic diseases or adolescents and children.
5. Conclusions
Despite the variety of measurement types and study methodologies of the selected studies, the majority of them reported that PA levels have significantly decreased and, at the same time, that SB levels have significantly increased in the adult working population during the COVID-19 pandemic. The stricter the confinement measures, the more likely that PA and SB patterns are affected. People working from home were less active during the COVID-19 lockdown. In contrast, those who continued to work in a normal routine usually did not observe such a high level of changes in their PA level. On the other hand, being unemployed is even worse than WFH, or working from the office, because unemployed people have a lower level of PA and increased level of SB. The lack of PA and accumulated SB is a known major health risk factor for poor overall health, premature mortality and NCDs. The findings of the present review and the well-known health risk factors of the inactive lifestyle illustrate the urgent need to support people, especially sitting-based workers, to increase PA and decrease sedentary time during the pandemic. The workplace is an outstanding opportunity for promoting PA and reducing sedentary time in the working population. Considering that the COVID-19 is an ongoing pandemic, the adult working population should be continuously surveyed, and interventions and strategies should be developed by organizations, governments and health professionals to increase the level of PA and decrease sedentary time among workers, with a special focus on people working from home.
Author Contributions
Conceptualization, G.R., K.K., É.B.B. and K.R.-Ó.; methodology, G.R. and É.B.B.; software, G.R.; validation, I.F., P.L., É.B.B., K.R.-Ó., K.K., Z.B. and G.R.; formal analysis, G.R.; investigation, G.R., K.R.-Ó. and É.B.B.; resources, É.B.B.; data curation, G.R.; writing—original draft preparation, G.R.; writing—review and editing, G.R., É.B.B. and K.R.-Ó.; visualization, I.F. and P.L.; supervision, K.K., Z.B., É.B.B. and K.R.-Ó.; project administration, É.B.B. and Z.B.; funding acquisition, É.B.B. and Z.B. All authors have read and agreed to the published version of the manuscript.
Funding
The publication is supported by the EFOP-3.6.1-16-2016-00022 project. The project is co-financed by the European Union and the European Social Fund.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Tremblay, M.S.; Aubert, S.; Barnes, J.D.; Saunders, T.J.; Carson, V.; Latimer-Cheung, A.E.; Chastin, S.F.M.; Altenburg, T.M.; Chinapaw, M.J.M.; On Behalf of Sbrn Terminology Consensus Project Participants. Sedentary Behavior Research Network (SBRN)—Terminology Consensus Project process and outcome. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 75. [Google Scholar] [CrossRef] [Green Version]
- Wang, N.X.; Chen, J.; Wagner, N.L.; Rebello, S.A.; Petrunoff, N.; Owen, N.; Müller-Riemenschneider, F. Understanding and Influencing Occupational Sedentary Behavior: A Mixed-Methods Approach in a Multiethnic Asian Population. Health Educ. Behav. 2019, 47, 419–429. [Google Scholar] [CrossRef] [PubMed]
- Ryan, C.G.; Dall, P.M.; Granat, M.; Grant, P.M. Sitting patterns at work: Objective measurement of adherence to current recommendations. Ergonomics 2011, 54, 531–538. [Google Scholar] [CrossRef] [Green Version]
- Kazi, A.; Duncan, M.; Clemes, S.; Haslam, C. A survey of sitting time among UK employees. Occup. Med. 2014, 64, 497–502. [Google Scholar] [CrossRef] [Green Version]
- Van Der Ploeg, H.P.; Hillsdon, M. Is sedentary behaviour just physical inactivity by another name? Int. J. Behav. Nutr. Phys. Act. 2017, 14, 142. [Google Scholar] [CrossRef]
- Kelso, A.; Reimers, A.K.; Abu-Omar, K.; Wunsch, K.; Niessner, C.; Wäsche, H.; Demetriou, Y. Locations of Physical Activity: Where Are Children, Adolescents, and Adults Physically Active? A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 1240. [Google Scholar] [CrossRef] [PubMed]
- Owen, N.; Healy, G.N.; Matthews, C.E.; Dunstan, D.W. Too Much Sitting: The population health science of sedentary behavior. Exerc. Sport Sci. Rev. 2010, 38, 105–113. [Google Scholar] [CrossRef]
- Chau, J.Y.; Grunseit, A.; Chey, T.; Stamatakis, E.; Brown, W.J.; Matthews, C.; Bauman, A.E.; van der Ploeg, H. Daily Sitting Time and All-Cause Mortality: A Meta-Analysis. PLoS ONE 2013, 8, e80000. [Google Scholar] [CrossRef] [Green Version]
- Thorp, A.A.; Owen, N.; Neuhaus, M.; Dunstan, D.W. Sedentary Behaviors and Subsequent Health Outcomes in Adults: A Systematic Review of Longitudinal Studies, 1996–2011. Am. J. Prev. Med. 2011, 41, 207–215. [Google Scholar] [CrossRef] [PubMed]
- De Rezende, L.F.M.; Rodrigues Lopes, M.; Rey-López, J.P.; Matsudo, V.K.R.; do Carmo Luiz, O. Sedentary Behavior and Health Outcomes: An Overview of Systematic Reviews. PLoS ONE 2014, 9, e105620. [Google Scholar] [CrossRef]
- Biswas, A.; Oh, P.I.; Faulkner, G.E.; Bajaj, R.R.; Silver, M.A.; Mitchell, M.S.; Alter, D.A. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults a systematic review and meta-analysis. Ann. Intern. Med. 2015, 162, 123–132. [Google Scholar] [CrossRef] [PubMed]
- Lee, I.-M.; Shiroma, E.J.; Lobelo, F.; Puska, P.; Blair, S.N.; Katzmarzyk, P.T. Lancet Physical Activity Series Working Group. Effect of physical inactivity on major non-communicable diseases worldwide: An analysis of burden of disease and life expectancy. Lancet 2012, 380, 219–229. [Google Scholar] [CrossRef] [Green Version]
- Booth, F.W.; Roberts, C.K.; Laye, M.J. Lack of Exercise Is a Major Cause of Chronic Diseases. Compr. Physiol. 2012, 2, 1143–1211. [Google Scholar] [CrossRef] [Green Version]
- Warburton, D.E.; Nicol, C.W.; Bredin, S.S. Health benefits of physical activity: The evidence. Can. Med. Assoc. J. 2006, 174, 801–809. [Google Scholar] [CrossRef] [Green Version]
- WHO. Prevalence of Insufficient Physical Activity among Adults; Global Health Observatory: Cork, Ireland, 2018. [Google Scholar]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.-P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Koohsari, M.J.; Nakaya, T.; McCormack, G.R.; Shibata, A.; Ishii, K.; Oka, K. Changes in Workers’ Sedentary and Physical Activity Behaviors in Response to the COVID-19 Pandemic and Their Relationships With Fatigue: Longitudinal Online Study. JMIR Public Health Surveill. 2021, 7, e26293. [Google Scholar] [CrossRef]
- Hadgraft, N.T.; Healy, G.N.; Owen, N.; Winkler, E.A.; Lynch, B.M.; Sethi, P.; Eakin, E.G.; Moodie, M.; LaMontagne, A.D.; Wiesner, G.; et al. Office workers’ objectively assessed total and prolonged sitting time: Individual-level correlates and worksite variations. Prev. Med. Rep. 2016, 4, 184–191. [Google Scholar] [CrossRef] [Green Version]
- Sugiyama, T.; Hadgraft, N.; Clark, B.K.; Dunstan, D.W.; Owen, N. Sitting at work & waist circumference—A cross-sectional study of Australian workers. Prev. Med. 2020, 141, 106243. [Google Scholar] [CrossRef]
- O’Dolan, C.; Grant, M.; Lawrence, M.; Dall, P. A randomised feasibility study to investigate the impact of education and the addition of prompts on the sedentary behaviour of office workers. Pilot Feasibility Study 2018, 4, 33. [Google Scholar] [CrossRef] [Green Version]
- Worldometer. COVID-19 Coronavirus Pandemic. 2021. Available online: https://www.worldometers.info/coronavirus/ (accessed on 20 July 2021).
- McDowell, C.P.; Herring, M.P.; Lansing, J.; Brower, C.; Meyer, J.D. Working From Home and Job Loss Due to the COVID-19 Pandemic Are Associated With Greater Time in Sedentary Behaviors. Front. Public Health 2020, 8, 597619. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Y.; Becerik-Gerber, B.; Lucas, G.; Roll, S.C. Impacts of Working from Home during COVID-19 Pandemic on Physical and Mental Well-Being of Office Workstation Users. J. Occup. Environ. Med. 2021, 63, 181–190. [Google Scholar] [CrossRef] [PubMed]
- Hall, G.; Laddu, D.R.; Phillips, S.A.; Lavie, C.J.; Arena, R. A tale of two pandemics: How will COVID-19 and global trends in physical inactivity and sedentary behavior affect one another? Prog. Cardiovasc. Dis. 2021, 64, 108–110. [Google Scholar] [CrossRef]
- Ammar, A.; Brach, M.; Trabelsi, K.; Chtourou, H.; Boukhris, O.; Masmoudi, L.; Bouaziz, B.; Bentlage, E.; How, D.; Ahmed, M.; et al. Effects of COVID-19 Home Confinement on Eating Behaviour and Physical Activity: Results of the ECLB-COVID19 International Online Survey. Nutrients 2020, 12, 1583. [Google Scholar] [CrossRef] [PubMed]
- Stanton, R.; To, Q.G.; Khalesi, S.; Williams, S.L.; Alley, S.J.; Thwaite, T.L.; Fenning, A.S.; Vandelanotte, C. Depression, Anxiety and stress during COVID-19: Associations with changes in physical activity, sleep, tobacco and alcohol use in australian adults. Int. J. Environ. Res. Public Health 2020, 17, 4065. [Google Scholar] [CrossRef] [PubMed]
- Reyes-Olavarría, D.; Latorre-Román, P.Á.; Guzmán-Guzmán, I.P.; Jerez-Mayorga, D.; Caamaño-Navarrete, F.; Delgado-Floody, P. Positive and Negative Changes in Food Habits, Physical Activity Patterns, and Weight Status during COVID-19 Confinement: Associated Factors in the Chilean Population. Int. J. Environ. Res. Public Health 2020, 17, 5431. [Google Scholar] [CrossRef]
- Constandt, B.; Thibaut, E.; De Bosscher, V.; Scheerder, J.; Ricour, M.; Willem, A. Exercising in Times of Lockdown: An Analysis of the Impact of COVID-19 on Levels and Patterns of Exercise among Adults in Belgium. Int. J. Environ. Res. Public Health 2020, 17, 4144. [Google Scholar] [CrossRef]
- Lesser, I.A.; Nienhuis, C.P. The Impact of COVID-19 on Physical Activity Behavior and Well-Being of Canadians. Int. J. Environ. Res. Public Health 2020, 17, 3899. [Google Scholar] [CrossRef]
- Gallo, L.A.; Gallo, T.F.; Young, S.L.; Moritz, K.M.; Akison, L.K. The Impact of Isolation Measures Due to COVID-19 on Energy Intake and Physical Activity Levels in Australian University Students. Nutrients 2020, 12, 1865. [Google Scholar] [CrossRef] [PubMed]
- Górnicka, M.; Drywień, M.; Zielinska, M.; Hamułka, J. Dietary and Lifestyle Changes During COVID-19 and the Subsequent Lockdowns among Polish Adults: A Cross-Sectional Online Survey PLifeCOVID-19 Study. Nutrients 2020, 12, 2324. [Google Scholar] [CrossRef] [PubMed]
- Ugbolue, U.; Duclos, M.; Urzeala, C.; Berthon, M.; Kulik, K.; Bota, A.; Thivel, D.; Bagheri, R.; Gu, Y.; Baker, J.; et al. An Assessment of the Novel COVISTRESS Questionnaire: COVID-19 Impact on Physical Activity, Sedentary Action and Psychological Emotion. J. Clin. Med. 2020, 9, 3352. [Google Scholar] [CrossRef] [PubMed]
- Carriedo, A.; Cecchini, J.A.; Fernandez-Rio, J.; Méndez-Giménez, A. COVID-19, Psychological Well-being and Physical Activity Levels in Older Adults During the Nationwide Lockdown in Spain. Am. J. Geriatr. Psychiatry 2020, 28, 1146–1155. [Google Scholar] [CrossRef]
- Trabelsi, K.; Ammar, A.; Masmoudi, L.; Boukhris, O.; Chtourou, H.; Bouaziz, B.; Brach, M.; Bentlage, E.; How, D.; Ahmed, M.; et al. Sleep Quality and Physical Activity as Predictors of Mental Wellbeing Variance in Older Adults during COVID-19 Lockdown: ECLB COVID-19 International Online Survey. Int. J. Environ. Res. Public Health 2021, 18, 4329. [Google Scholar] [CrossRef] [PubMed]
- Goethals, L.; Barth, N.; Guyot, J.; Hupin, D.; Celarier, T.; Bongue, B. Impact of Home Quarantine on Physical Activity Among Older Adults Living at Home During the COVID-19 Pandemic: Qualitative Interview Study. JMIR Aging 2020, 3, e19007. [Google Scholar] [CrossRef]
- Di Stefano, V.; Battaglia, G.; Giustino, V.; Gagliardo, A.; D’Aleo, M.; Giannini, O.; Palma, A.; Brighina, F. Significant reduction of physical activity in patients with neuromuscular disease during COVID-19 pandemic: The long-term consequences of quarantine. J. Neurol. 2020, 268, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Caruso, I.; Di Molfetta, S.; Guarini, F.; Giordano, F.; Cignarelli, A.; Natalicchio, A.; Perrini, S.; Leonardini, A.; Giorgino, F.; Laviola, L. Reduction of hypoglycemia, lifestyle modifications and psychological distress during lockdown following SARS-CoV-2 outbreak in type 1 diabetic patients using flash continuous glucose monitoring: A retrospective cohort study. Diabetes/Metab. Res. Rev. 2020, e3404. [Google Scholar] [CrossRef]
- Ruiz-Roso, M.B.; Knott-Torcal, C.; Matilla-Escalante, D.C.; Garcimartín, A.; Sampedro-Nuñez, M.A.; Dávalos, A.; Marazuela, M. COVID-19 Lockdown and Changes of the Dietary Pattern and Physical Activity Habits in a Cohort of Patients with Type 2 Diabetes Mellitus. Nutrients 2020, 12, 2327. [Google Scholar] [CrossRef]
- Mota, I.A.; Sobrinho, G.D.D.O.; Morais, I.P.S.; Dantas, T.F. Impact of COVID-19 on eating habits, physical activity and sleep in Brazilian healthcare professionals. Arq. De Neuro-Psiquiatr. 2021, 79, 429–436. [Google Scholar] [CrossRef]
- Shepherd, H.; Evans, T.; Gupta, S.; McDonough, M.; Doyle-Baker, P.; Belton, K.; Karmali, S.; Pawer, S.; Hadly, G.; Pike, I.; et al. The Impact of COVID-19 on High School Student-Athlete Experiences with Physical Activity, Mental Health, and Social Connection. Int. J. Environ. Res. Public Health 2021, 18, 3515. [Google Scholar] [CrossRef] [PubMed]
- Santos, A.M.D.S.; Rossi, F.E.; Moura, H.P.D.S.N.D.; Junior, A.V.M.d.S.; Machado, D.C.D.; Neves, L.M.; Brito, A.S.; Moura, P.; Monteiro, P.A.; Junior, I.F.F.; et al. COVID-19 pandemic impacts physical activity levels and sedentary time but not sleep quality in young badminton athletes. Sport Sci. Health 2021, 1–9. [Google Scholar] [CrossRef]
- Hernandez, Y.A.T.; Parente, F.; Faghy, M.A.; Roscoe, C.M.P.; Maratos, F. Influence of the COVID-19 lockdown on remote workers’ physical and psychosocial wellbeing and work productivity. JMIRx Med. 2021, 1–42. [Google Scholar] [CrossRef]
- Castañeda-Babarro, A.; Arbillaga-Etxarri, A.; Gutiérrez-Santamaria, B.; Coca, A. Impact of COVID-19 confinement on the time and intensity of physical activity in the Spanish population. Res. Sq. 2020, 1–14. [Google Scholar] [CrossRef]
- Mata, J.; Wenz, A.; Rettig, T.; Reifenscheid, M.; Moehring, K.; Krieger, U.; Friedel, S.; Fikel, M.; Cornesse, C.; Blom, A.G.; et al. Health Behaviors and Mental Health before and during the COVID-19 Pandemic: A Longitudinal Population Based Survey. PsyArXiv 2020. [Google Scholar] [CrossRef]
- Huntley, D. Effects of Working at Home During COVID-19 on Sedentary Behavior, Use of Strategies to Decrease Sedentary Behavior, and Perceived Work Performance. Retrieved from the University of Minnesota Digital Conservancy. 2021. Available online: https://hdl.handle.net/11299/220401 (accessed on 30 June 2021).
- Schaap, G. Occupational Sedentary Behaviour during COVID-19 Regulations-Related Working from Home; University of Twente: Enschede, The Netherlands, 2020. [Google Scholar]
- Bourdas, D.I.; Zacharakis, E.D. Impact of COVID-19 Lockdown on Physical Activity in a Sample of Greek Adults. Sports 2020, 8, 139. [Google Scholar] [CrossRef] [PubMed]
- Bourdas, D.I.; Zacharakis, E.D. Evolution of changes in physical activity over lockdown time: Physical activity datasets of four independent adult sample groups corresponding to each of the last four of the six COVID-19 lockdown weeks in Greece. Data Brief 2020, 32, 106301. [Google Scholar] [CrossRef] [PubMed]
- Wilke, J.; Mohr, L.; Tenforde, A.; Edouard, P.; Fossati, C.; González-Gross, M.; Ramírez, C.S.; Laiño, F.; Tan, B.; Pillay, J.; et al. A Pandemic within the Pandemic? Physical Activity Levels Substantially Decreased in Countries Affected by COVID-19. Int. J. Environ. Res. Public Health 2021, 18, 2235. [Google Scholar] [CrossRef]
- Adamakis, M. Physical activity, sleep and weight management in the COVID-19 era: A case report. J. Phys. Educ. Sport 2021, 21, 60–65. [Google Scholar] [CrossRef]
- Ong, J.L.; Lau, T.; A A Massar, S.; Chong, Z.T.; Ng, B.K.L.; Koek, D.; Zhao, W.; Yeo, B.T.T.; Cheong, K.; Chee, M.W.L. COVID-19-related mobility reduction: Heterogenous effects on sleep and physical activity rhythms. Sleep 2021, 44, 1–13. [Google Scholar] [CrossRef]
- Hallman, D.M.; Januario, L.B.; Mathiassen, S.E.; Heiden, M.; Svensson, S.; Bergström, G. Working from home during the COVID-19 outbreak in Sweden: Effects on 24-h time-use in office workers. BMC Public Health 2021, 21, 1–10. [Google Scholar] [CrossRef]
- Brusaca, L.; Barbieri, D.; Mathiassen, S.; Holtermann, A.; Oliveira, A. Physical Behaviours in Brazilian Office Workers Working from Home during the COVID-19 Pandemic, Compared to before the Pandemic: A Compositional Data Analysis. Int. J. Environ. Res. Public Health 2021, 18, 6278. [Google Scholar] [CrossRef]
- Franco, E.; Urosa, J.; Barakat, R.; Refoyo, I. Physical Activity and Adherence to the Mediterranean Diet among Spanish Employees in a Health-Promotion Program before and during the COVID-19 Pandemic: The Sanitas-Healthy Cities Challenge. Int. J. Environ. Res. Public Health 2021, 18, 2735. [Google Scholar] [CrossRef]
- Aegerter, A.M.; Deforth, M.; Sjøgaard, G.; Johnston, V.; Volken, T.; Luomajoki, H.; Dratva, J.; Dressel, H.; Distler, O.; Melloh, M.; et al. No Evidence for a Decrease in Physical Activity Among Swiss Office Workers During COVID-19: A Longitudinal Study. Front. Psychol. 2021, 12, 1–10. [Google Scholar] [CrossRef]
- Argus, M.; Pääsuke, M. Effects of the COVID-19 lockdown on musculoskeletal pain, physical activity, and work environment in Estonian office workers transitioning to working from home. Work 2021, 69, 741–749. [Google Scholar] [CrossRef]
- Blom, V.; Lönn, A.; Ekblom, B.; Kallings, L.V.; Väisänen, D.; Hemmingsson, E.; Andersson, G.; Wallin, P.; Stenling, A.; Ekblom, Ö.; et al. Lifestyle Habits and Mental Health in Light of the Two COVID-19 Pandemic Waves in Sweden, 2020. Int. J. Environ. Res. Public Health 2021, 18, 3313. [Google Scholar] [CrossRef]
- Gibbs, B.B.; E Kline, C.; A Huber, K.; Paley, J.L.; Perera, S. COVID-19 shelter-at-home and work, lifestyle and well-being in desk workers. Occup. Med. 2021, 71, 86–94. [Google Scholar] [CrossRef]
- Majumdar, P.; Biswas, A.; Sahu, S. COVID-19 pandemic and lockdown: Cause of sleep disruption, depression, somatic pain, and increased screen exposure of office workers and students of India. Chronobiol. Int. 2020, 37, 1191–1200. [Google Scholar] [CrossRef] [PubMed]
- da Silva, D.R.P.; Werneck, A.O.; Malta, D.C.; Júnior, P.R.B.D.S.; Azevedo, L.O.; Barros, M.B.D.A.; Szwarcwald, C.L. Changes in the prevalence of physical inactivity and sedentary behavior during COVID-19 pandemic: A survey with 39,693 Brazilian adults. Cadernos De Saúde Pública 2021, 37, e00221920. [Google Scholar] [CrossRef] [PubMed]
- Fearnbach, S.N.; Flanagan, E.W.; Höchsmann, C.; Beyl, R.A.; Altazan, A.D.; Martin, C.K.; Redman, L.M. Factors Protecting against a Decline in Physical Activity during the COVID-19 Pandemic. Med. Sci. Sports Exerc. 2021, 53, 1391–1399. [Google Scholar] [CrossRef]
- Radwan, H.; Al Kitbi, M.; Hasan, H.; Al Hilali, M.; Abbas, N.; Hamadeh, R.; Saif, E.; Naja, F. Indirect Health Effects of COVID-19: Unhealthy Lifestyle Behaviors during the Lockdown in the United Arab Emirates. Int. J. Environ. Res. Public Health 2021, 18, 1964. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, T.; Pawlowski, C.S. Physical Activity in Crisis: The Impact of COVID-19 on Danes’ Physical Activity Behavior. Front. Sports Act. Living 2021, 2, 610255. [Google Scholar] [CrossRef]
- Ding, D.; Cheng, M.; Cruz, B.D.P.; Lin, T.; Sun, S.; Zhang, L.; Yang, Q.; Ma, Z.; Wang, J.; Jia, Y.; et al. How COVID-19 lockdown and reopening affected daily steps: Evidence based on 164,630 person-days of prospectively collected data from Shanghai, China. Int. J. Behav. Nutr. Phys. Act. 2021, 18, 1–10. [Google Scholar] [CrossRef]
- Buoitestella, A.; Ajčevic, M.; Furlanis, G.; Cillotto, T.; Menichelli, A.; Accardo, A.; Manganotti, P. Smart technology for physical activity and health assessment during COVID-19 lockdown. J. Sports Med. Phys. Fit. 2021, 61, 452–460. [Google Scholar]
- Karaca, A.; Aytar, S.H.; Demirci, N.; Akcan, F.; Çağlar, E.; Araç, Ş.N. Sedentary Screen Time in Working Adults Before and During COVID-19 Pandemic. Spor Bilimleri Derg. Hacet. Üniversitesi 2021, 32, 98–108. [Google Scholar] [CrossRef]
- Katewongsa, P.; Widyastari, D.A.; Saonuam, P.; Haemathulin, N.; Wongsingha, N. The effects of the COVID-19 pandemic on the physical activity of the Thai population: Evidence from Thailand’s Surveillance on Physical Activity 2020. J. Sport Health Sci. 2021, 10, 341–348. [Google Scholar] [CrossRef] [PubMed]
- Katewongsa, P.; Potharin, D.; Rasri, N.; Palakai, R.; Widyastari, D. The Effect of Containment Measures during the COVID-19 Pandemic to Sedentary Behavior of Thai Adults: Evidence from Thailand’s Surveillance on Physical Activity 2019–2020. Int. J. Environ. Res. Public Health 2021, 18, 4467. [Google Scholar] [CrossRef]
- López-Bueno, R.; Calatayud, J.; Andersen, L.; Balsalobre-Fernández, C.; Casaña, J.; Casajús, J.; Smith, L.; López-Sánchez, G. Immediate Impact of the COVID-19 Confinement on Physical Activity Levels in Spanish Adults. Sustainability 2020, 12, 5708. [Google Scholar] [CrossRef]
- Rodríguez-Nogueira, Ó.; Leirós-Rodríguez, R.; Benítez-Andrades, J.; Álvarez-Álvarez, M.; Marqués-Sánchez, P.; Pinto-Carral, A. Musculoskeletal Pain and Teleworking in Times of the COVID-19: Analysis of the Impact on the Workers at Two Spanish Universities. Int. J. Environ. Res. Public Health 2020, 18, 31. [Google Scholar] [CrossRef]
- Taeymans, J.; Luijckx, E.; Rogan, S.; Haas, K.; Baur, H. Physical Activity, Nutritional Habits, and Sleeping Behavior in Students and Employees of a Swiss University During the COVID-19 Lockdown Period: Questionnaire Survey Study. JMIR Public Health Surveill. 2021, 7, e26330. [Google Scholar] [CrossRef]
- Yang, Y.; Koenigstorfer, J. Determinants of physical activity maintenance during the COVID-19 pandemic: A focus on fitness apps. Transl. Behav. Med. 2020, 10, 835–842. [Google Scholar] [CrossRef]
- Schuch, F.B.; Bulzing, R.A.; Meyer, J.; López-Sánchez, G.F.; Grabovac, I.; Willeit, P.; Vancampfort, D.; Caperchione, C.M.; Sadarangani, K.P.; Werneck, A.O.; et al. Moderate to vigorous physical activity and sedentary behavior changes in self-isolating adults during the COVID-19 pandemic in Brazil: A cross-sectional survey exploring correlates. Sport Sci. Health 2021, 1–9. [Google Scholar] [CrossRef]
- Hall-López, J.A. Physical activity levels in physical education teachers before and during school suspension brought by the COVID-19 quarantine. Facta Univ. Series Phys. Educ. Sport 2020, 18, 475–481. [Google Scholar] [CrossRef]
- Alfawaz, H.; Amer, O.E.; Aljumah, A.A.; Aldisi, D.A.; Enani, M.A.; Aljohani, N.J.; Alotaibi, N.H.; Alshingetti, N.; Alomar, S.Y.; Khattak, M.N.K.; et al. Effects of home quarantine during COVID-19 lockdown on physical activity and dietary habits of adults in Saudi Arabia. Sci. Rep. 2021, 11, 1–7. [Google Scholar] [CrossRef]
- Barkley, J.E.; Lepp, A.; Glickman, E.; Farnell, G.; Beiting, J.; Wiet, R.; Dowdell, B. The Acute Effects of the COVID-19 Pan-demic on Physical Activity and Sedentary Behavior in University Students and Employees. Int. J. Exerc. Sci. 2020, 13, 1326–1339. [Google Scholar] [PubMed]
- Greaney, M.L.; Kunicki, Z.J.; Drohan, M.M.; Ward-Ritacco, C.L.; Riebe, D.; Cohen, S.A. Self-reported changes in physical activity, sedentary behavior, and screen time among informal caregivers during the COVID-19 pandemic. BMC Public Health 2021, 21, 1–9. [Google Scholar] [CrossRef]
- Stockwell, S.; Trott, M.; Tully, M.; Shin, J.; Barnett, Y.; Butler, L.; McDermott, D.; Schuch, F.; Smith, L. Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: A systematic review. BMJ Open Sport Exerc. Med. 2021, 7, e000960. [Google Scholar] [CrossRef]
- Dunton, G.F.; Do, B.; Wang, S.D. Early effects of the COVID-19 pandemic on physical activity and sedentary behavior in children living in the U.S. BMC Public Health 2020, 20, 1–13. [Google Scholar] [CrossRef]
- López-Valenciano, A.; Suárez-Iglesias, D.; Sanchez-Lastra, M.A.; Ayán, C. Impact of COVID-19 Pandemic on University Students’ Physical Activity Levels: An Early Systematic Review. Front. Psychol. 2021, 11, 624567. [Google Scholar] [CrossRef]
- de Boer, D.; Hoekstra, F.; Huetink, K.; Hoekstra, T.; Krops, L.; Hettinga, F. Physical Activity, Sedentary Behavior and Well-Being of Adults with Physical Disabilities and/or Chronic Diseases during the First Wave of the COVID-19 Pandemic: A Rapid Review. Int. J. Environ. Res. Public Health 2021, 18, 6342. [Google Scholar] [CrossRef]
- Felber, S. Data: Quarantine Isn’t Making Us Gain Weight or Slow Down. Withings. 2020. Available online: https://blog.withings.com/2020/05/01/data-quarantine-isnt-making-us-gain-weight-or-slow-down/ (accessed on 25 May 2021).
- Fitbit Staff. The Impact of Coronavirus on Global Activity. Fitbit. 2020. Available online: https://blog.fitbit.com/covid-19-global-activity/ (accessed on 25 May 2021).
- Stables, J. Garmin Data Reveals How the World Is Working out during the Lockdown. 2020. Available online: https://www.wareable.com/garmin/garmin-data-lockdown-7940 (accessed on 25 May 2021).
- Tison, G.H.; Avram, R.; Kuhar, P.; Abreau, S.; Marcus, G.M.; Pletcher, M.J.; Olgin, J.E. Worldwide Effect of COVID-19 on Physical Activity: A Descriptive Study. Ann. Intern. Med. 2020, 173, 767–770. [Google Scholar] [CrossRef] [PubMed]
- Okazaki, K.; Suzuki, K.; Sakamoto, Y.; Sasaki, K. Physical activity and sedentary behavior among children and adolescents living in an area affected by the 2011 Great East Japan earthquake and tsunami for 3 years. Prev. Med. Rep. 2015, 2, 720–724. [Google Scholar] [CrossRef] [Green Version]
- Brancaccio, M.; Mennitti, C.; Gentile, A.; Correale, L.; Buzzachera, C.; Ferraris, C.; Montomoli, C.; Frisso, G.; Borrelli, P.; Scudiero, O. Effects of the COVID-19 Pandemic on Job Activity, Dietary Behaviours and Physical Activity Habits of University Population of Naples, Federico II-Italy. Int. J. Environ. Res. Public Health 2021, 18, 1502. [Google Scholar] [CrossRef] [PubMed]
- Gartner. Gartner HR Survey Reveals 41% of Employees Likely to Work Remotely at Least Some of the Time Post Coro-Navirus Pandemic. Newsroom. 2020. Available online: https://www.gartner.com/en/newsroom/press-releases/2020-04-14-gartner-hr-survey-reveals-41--of-employees-likely-to- (accessed on 30 May 2021).
- De Haas, M.; Faber, R.; Hamersma, M. How COVID-19 and the Dutch ‘intelligent lockdown’ change activities, work and travel behaviour: Evidence from longitudinal data in the Netherlands. Transp. Res. Interdiscip. Perspect. 2020, 6, 100150. [Google Scholar] [CrossRef] [PubMed]
- Deng, Z.; Morissette, R.; Messacar, D. Running the Economy Remotely: Potential for Working from Home during and after COVID-19. Statistics Canada Catalogue. Available online: https://www150.statcan.gc.ca/n1/pub/45-28-0001/2020001/article/00026-eng.htm (accessed on 28 June 2021).
- Koohsari, M.; Nakaya, T.; Shibata, A.; Ishii, K.; Oka, K. Working from Home After the COVID-19 Pandemic: Do Company Employees Sit More and Move Less? Sustainability 2021, 13, 939. [Google Scholar] [CrossRef]
- Brynjolfsson, E.; Horton, J.; Ozimek, A.; Rock, D.; Sharma, G.; TuYe, H.-Y. COVID-19 and Remote Work: An Early Look at US Data; National Bureau of Economic Research Inc: Cambridge, MA, USA, 2020. [Google Scholar]
- A Thorp, A.; Healy, G.N.; Winkler, E.; Clark, B.K.; A Gardiner, P.; Owen, N.; Dunstan, D.W. Prolonged sedentary time and physical activity in workplace and non-work contexts: A cross-sectional study of office, customer service and call centre employees. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 128. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meyer, J.; McDowell, C.; Lansing, J.; Brower, C.; Smith, L.; Tully, M.; Herring, M. Changes in physical activity and sedentary behaviour due to the COVID-19 outbreak and associations with mental health in 3052 US adults. Int. J. Environ. Res. Public Health 2020, 17, 6469. [Google Scholar] [CrossRef] [PubMed]
- Fukushima, N.; Machida, M.; Kikuchi, H.; Amagasa, S.; Hayashi, T.; Odagiri, Y.; Takamiya, T.; Inoue, S. Associations of working from home with occupational physical activity and sedentary behavior under the COVID-19 pandemic. J. Occup. Health 2021, 63, e12212. [Google Scholar] [CrossRef]
- Clemes, S.; O’Connell, S.E.; Edwardson, C.L. Office Workers’ Objectively Measured Sedentary Behavior and Physical Activity During and Outside Working Hours. J. Occup. Environ. Med. 2014, 56, 298–303. [Google Scholar] [CrossRef] [Green Version]
- Learnpatch. Research Reveals Impact of COVID-19 on Working Practices and Remote Working. 2020. Available online: https://learnpatch.com/2020/05/covid-remote-working/ (accessed on 30 May 2021).
- Ali, S.M.; Lindström, M. Psychosocial work conditions, unemployment, and leisure-time physical activity: A population-based study. Scand. J. Public Health 2006, 34, 209–216. [Google Scholar] [CrossRef]
- Katzmarzyk, P.T.; Church, T.S.; Craig, C.L.; Bouchard, C. Sitting Time and Mortality from All Causes, Cardiovascular Disease, and Cancer. Med. Sci. Sports Exerc. 2009, 41, 998–1005. [Google Scholar] [CrossRef]
- Caprara, G. Mediterranean-Type Dietary Pattern and Physical Activity: The Winning Combination to Counteract the Rising Burden of Non-Communicable Diseases (NCDs). Nutrients 2021, 13, 429. [Google Scholar] [CrossRef] [PubMed]
- Schlichtiger, J.; Steffen, J.; Huber, B.C.; Brunner, S. Physical activity during COVID-19 lockdown in older adults. J. Sports Med. Phys. Fit. 2021, 61, 164–166. [Google Scholar]
- Smith, L.; McCourt, O.; Sawyer, A.; Ucci, M.; Marmot, A.; Wardle, J.; Fisher, A. A review of occupational physical activity and sedentary behaviour correlates. Occup. Med. 2016, 66, 185–192. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Santini, S.; Galassi, F.; Kropf, J.; Stara, V. A Digital Coach Promoting Healthy Aging among Older Adults in Transition to Retirement: Results from a Qualitative Study in Italy. Sustainability 2020, 12, 7400. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).