Abstract
Background/Objectives: Chronic Obstructive Pulmonary Disease (COPD) is highly prevalent among individuals residing in care homes, where effective disease management can enhance quality of life by slowing disease progression. Care home staff are central to COPD management in these settings, and their capacity to deliver optimal care may be strengthened through targeted education and training interventions. This scoping review aimed to synthesise existing evidence on education and training intended to enhance COPD care delivery by care home staff. Methods: A scoping review was conducted in accordance with Joanna Briggs Institute (JBI) guidelines and reported in line with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) framework. Four electronic databases (CINAHL, EMBASE, MEDLINE, and PsycINFO) were systematically searched for studies evaluating educational or training interventions regarding COPD for care home staff. Results: Only one study met the eligibility criteria for inclusion. This mixed methods study encompassed both a randomised control trial and semi-structured interviews, evaluating the effects of a COPD education programme for healthcare professionals working in a care home setting. This education intervention led to increased COPD-related knowledge and improved support for staff managing residents with COPD. Conclusions: Evidence for educational interventions for care home staff caring for individuals with COPD is extremely limited. While the included study shows potential for educational programmes, substantial gaps persist. Further research is needed to develop, implement, and rigorously assess education and training interventions to support high-quality COPD care in care homes.
1. Introduction
Chronic Obstructive Pulmonary Disease (COPD) is a progressive lung disease characterised by obstruction of airflow in the lungs and is a common cause of death globally [1,2,3]. COPD symptoms can present as tightness of chest, wheezing, breathlessness (dyspnea), chronic cough and sputum production, with varying levels of severity [2,3]. Multiple cells play a role in COPD pathophysiology, including macrophages, epithelial cells, and T-lymphocytes [4]. Substance exposure causes dysfunction of these cells, resulting in elevated production of inflammatory mediators and therefore furthering disease progression [4]. As the disease progresses, airflow is reduced and gas exchange becomes increasingly impaired, leading to degradation of lung tissue and, ultimately, the development of chronic respiratory failure. This often results in dependency on long-term oxygen therapy [5].
COPD exacerbations are associated with physical decline and worsening symptoms, such as shortness of breath, increased sputum production, cough, and sore throat [2,6,7]. These events are believed to result from a combination of respiratory viruses and bacteria, individual susceptibility, and environmental pollutants, leading to an increased inflammatory burden [8]. The frequency of exacerbations can vary between patients, but those who experience them more often tend to have a poorer quality of life [6,9].
There is limited data regarding prevalence within care homes, although one retrospective analysis of data in the United States of America found 21.5% of residents with cognitive impairment had a diagnosis of COPD [10]. Whilst the exact figures are undetermined, COPD is prevalent within care homes [10,11]. COPD exacerbations can result in prolonged recovery periods, with some individuals becoming housebound and dependent on others [12]. The disease is also associated with reduced physical activity and a progressive decline in quality of life (QoL) [6,12]. Care home residents experience higher dependency on others to meet their daily living needs, by virtue of their health conditions and medical history [13]. Care home residents are more likely to be frail and have an increased risk of acute hospitalisations [14], similarly to those with COPD. Therefore, it can be inferred that prevalence in care homes may be high due to disease implications.
Optimal COPD care requires attention to nutrition and physical functioning, in addition to pharmacological management [15,16]. Malnutrition and low muscle mass are common in COPD and are associated with poorer lung function, increased exacerbations, reduced exercise tolerance, and higher mortality [17,18]. Nutritional support and pulmonary rehabilitation programmes, including exercise training and early rehabilitation after exacerbations, can improve nutritional status, functional capacity, and health-related quality of life, particularly when nutrition therapy is combined with rehabilitation [16,19,20,21,22]. However, these multidisciplinary approaches have been largely developed in hospital and community settings, and there is little evidence on how care home staff are prepared, through structured education and training, to recognise and respond to malnutrition, functional decline, and rehabilitation needs in residents with COPD.
The nurse role can enable effective management of COPD as nurses are often the initial point of contact for patients and are involved in care throughout every stage of life [23,24]. The NHS in England has planned to invest in further training for all staff, and a new desirable criterion for senior staff is an MSc qualification relevant to their role [25]. However, whilst healthcare providers offer education tools, a significant percentage of staff do not complete professional development courses following their original training [26]. This suggests difficulty in ensuring nurse education post-qualification as training is often optional and based on individual interest. Further training is, however, a mandatory part of the Nursing Midwifery Council (NMC) revalidation process, but it does not specify which training [27]. Perhaps in-depth COPD education should be an essential component of undergraduate training for all nurses, ensuring they are equipped with knowledge of the disease prior to qualifying. The NMC and university stakeholders ensure undergraduate education is relevant to contemporary health [28], but specific teachings are not regulated.
The need for education and training in care homes regarding both pharmacological and non-pharmacological interventions for COPD is clear. Although the evidence is dated, early diagnosis and intervention have been shown to slow disease progression and improve residents’ QoL, with the potential for a partial reversal of the condition [29,30]. Supporting care home staff to care for COPD residents can also enhance residents’ holistic well-being [31]. However, previous research implies those in primary care lack sufficient knowledge to provide optimal care for those with COPD when compared to hospital staff [32,33]. For example, nurses and other healthcare professionals have demonstrated a lack of competence in inhaler technique for those with COPD [34,35]. This lack of knowledge is highlighted by the fact that adults newly admitted to care homes, from hospitals, have a high acute re-admission rate when COPD is part of their medical history [36].
Care homes’ statements of purpose for categories of care vary throughout the sector; however, whether it is dementia care, or care of an older adult, COPD can be a diagnosis for many of these residents. One example of educational interventions improving patient outcomes in care homes is a training programme on care for people with dementia, which found challenging behaviour decreased significantly three months post-training [37]. Another scoping review found that, although resident outcomes did not improve, interprofessional communication and staff ability to conduct heart failure assessments did improve post-educational intervention; moreover, nurses expressed appreciation for the additional training [38]. This supports the idea that further educational interventions can improve practice and nurse confidence in the management of long-term health conditions and therefore may be beneficial within the context of COPD.
The present scoping review, therefore, aimed to map and describe the extent, nature, and characteristics of evidence on education and training interventions for care home staff regarding COPD, and to identify gaps to inform future research and practice. A scoping review method was selected because the primary aim was not to evaluate the effectiveness of a well-established body of interventions, but to systematically map any existing COPD-related education and training for care home staff. Current methodological guidance indicates that scoping reviews are particularly appropriate when the evidence base is expected to be heterogeneous, emergent, or sparse, and when clarifying what has and has not yet been studied [39]. Using a scoping review therefore ensured a structured systematic approach capable of accommodating an anticipated paucity of evidence while still producing an informative evidence map.
Objectives:
- To identify and map published studies that report education or training interventions on COPD delivered to staff working in care home settings.
- To describe the key characteristics and reported outcomes of COPD-related education and training interventions for care home staff.
- To identify gaps in the existing evidence on COPD education and training for care home staff, in order to highlight priorities for future intervention development and evaluation.
Research Question: What COPD-related education and training interventions for care home staff have been evaluated in the published literature?
2. Materials and Methods
2.1. Protocol and Registration
This scoping review was conducted in line with the Joanna Briggs Institute (JBI) methodology for scoping reviews [40] and was reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) checklist [41]. A protocol for this scoping review was registered prospectively on Open Science Framework on 16 April 2025 (registration DOI: 10.17605/OSF.IO/VA5PF).
2.2. Eligibility Criteria
2.2.1. Types of Sources
This scoping review considered both experimental and quasi-experimental study designs including randomised controlled trials, non-randomised controlled trials, before-and-after studies, and interrupted time-series studies. Analytical observational studies, including prospective and retrospective cohort studies, case–control studies, and analytical cross-sectional studies, were considered for inclusion. This review also considered descriptive observational study designs including case series, individual case reports, and descriptive cross-sectional studies for inclusion. Studies were also considered that focused on qualitative data, including phenomenology, grounded theory, ethnography, and qualitative description. Identified systematic reviews were searched for relevant papers found in their reference sections that may not have been found in the database searches. Studies published in English only were included due to a lack of language diversity amongst the researchers. No date restrictions were applied, and grey literature was not included to maintain rigour and reliability by focusing on peer-reviewed publications. Further eligibility criteria were developed using the Population, Concept, and Context (PCC) framework, as recommended by JBI [42].
Population
The population of interest was care home staff. No restrictions were placed on care home type, participant gender, age, or ethnicity. Studies were considered for inclusion if at least some of the sample consisted of care home staff, for example, those which included residents.
Concept
All education and training focused on COPD were considered for inclusion. This may have included education related to early diagnosis, assessment, or management. Studies focused primarily on other respiratory illnesses were excluded. Studies which evaluated outcomes such as staff knowledge, confidence, and self-efficacy, as well as resident outcomes, such as improved quality of life, were considered. Additionally, studies which reported on staff experiences of engaging with an education or training intervention on COPD were considered.
Context
No restrictions were placed on geographic location. All studies which reported educational or training interventions in a care home setting were included. Care home environments included nursing homes, residential care homes, supported living settings, residential aged care settings, and other long-term care settings. Long-term hospital wards, rehabilitation units, and skilled nursing facilities were not included due to the varying care structures, goals, and patient populations compared to care home settings.
2.3. Search Strategy
The search strategy was developed iteratively by the review team in close collaboration with an experienced health-sciences subject librarian. The librarian advised on both the formulation of the research question and the operationalisation of the PCC elements into database search terms. An initial limited search of Google Scholar was conducted to identify key articles and index terms related to COPD education and training in care home settings, and these findings were used to inform the search strategy. A comprehensive search strategy was then constructed for MEDLINE (Supplementary Material 2) and systematically adapted to the syntax and subject headings of each database searched (CINAHL, EMBASE, MEDLINE, and PsycINFO). To identify potentially relevant studies, the bibliographic databases were searched on 22 April 2025. To enhance completeness, the reference list and citations of the included study were also screened for additional eligible articles.
2.4. Selection of Sources of Evidence
Following the search, all identified citations were collated and uploaded into Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia, available at https://www.covidence.org/ (accessed on 22 April 2025), a screening and data extraction tool for streamlining the production of reviews. Following the removal of duplicates, BC carried out full screening of the title and abstracts; GM and TA independently repeated this for 50% of the records each. The same procedure was used for full-text screening. Disagreements throughout the screening process were resolved following a discussion between authors.
2.5. Data Charting
Charting the data was carried out in Covidence, guided by the ‘JBI template source for evidence details, characteristics and results extraction instrument’ [43]. BC conducted data extraction from the paper included in the scoping review, and this was checked for accuracy by TA independently. The data extracted included specific details about the author, year, setting, participants, study methods, outcomes, and key findings.
In accordance with JBI guidance for scoping reviews, a formal quality appraisal of the included studies was not undertaken. The purpose of this review was to chart the evidence related to COPD-education for care home staff in order to identify knowledge gaps and priority areas for future education and practice, rather than to assess the methodological quality of existing evidence [40,41].
3. Results
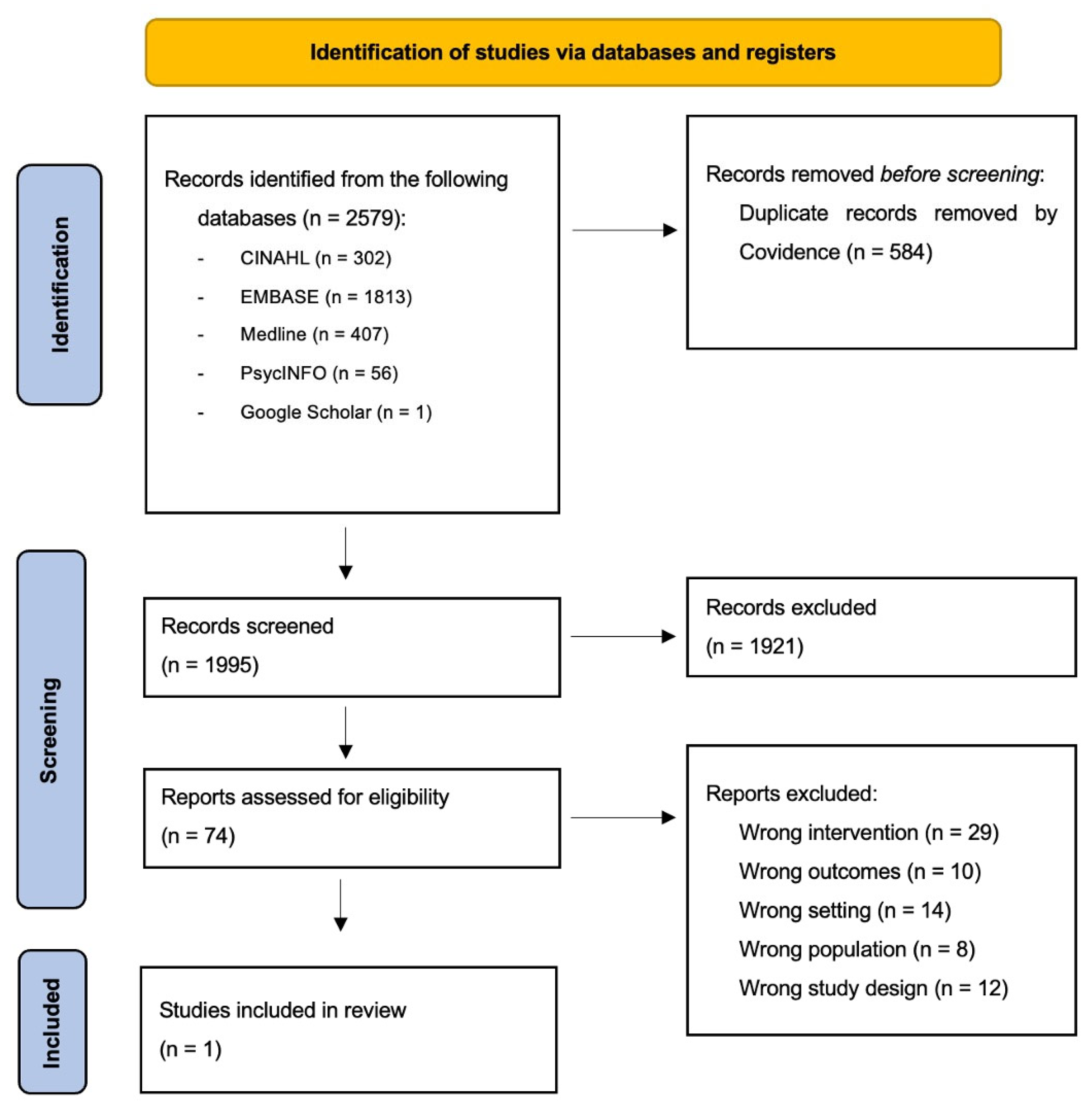
The search strategy yielded 2579 results, which were reduced to 1995 once duplicates were removed. A total of 1921 records were excluded following title and abstract screening. Following full-text review of 74 records, only one study was deemed eligible and included in this review. Reasons for exclusion at the full-text screening stage included the following: wrong study design, for example, commentary pieces or qualitative studies on the management of COPD in care homes; wrong intervention, for example, COPD management interventions such as inhaler techniques; wrong outcome, for example, educational interventions for care home staff on other areas such as palliative care; and wrong population or setting, for example, education for hospital staff, patients, and/or caregivers. The screening and study identification process is presented in a PRISMA-ScR flowchart (Figure 1).
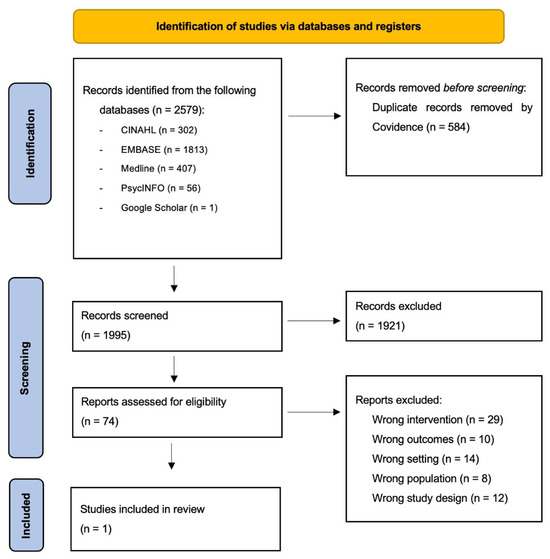
Figure 1.
PRISMA Flow Diagram.
3.1. Characteristics of Included Studies
The one included study was a mixed methods study published in 2022 [44]. Further study characteristics are reported in Table 1.

Table 1.
Characteristics of included studies.
3.2. Summary of Results
The intervention group generally rated the experience as a well-structured, good support. Prioritisation of the programme was difficult during their working day, with several participants advising that they completed it at home in their spare time. Participants stated that all modules were important to acquire knowledge about roles and healthcare services, but rated modules regarding ‘COPD and common problems’ most important and ‘COPD and follow-ups’ least important. The programme gave participants a desire to learn more, complete further courses, and encourage colleagues to complete it. Participants wanted to retain access to the COPD web and found it could be used for patient and peer education.
Pre-intervention interviews revealed that participants were not always informed of a patient’s diagnosis of COPD, and national guidelines for COPD were not routinely implemented in practice. Quantitative data revealed a statistically significant increase from 69% to 89% in objective COPD-related knowledge in the intervention group from pre- to post-test levels. Additionally, knowledge of the national guidelines showed a statistically significant increase from 64% to 80%. Qualitative data supported these knowledge increases with staff feeling more secure, and an increased attentiveness to COPD. Participants discussed an increased awareness of infections and the risks they pose, and an increased knowledge in breathing techniques, physical activity, signs of exacerbations, weight loss/nutrition, and diagnostics.
Although formal quality appraisal is not required within scoping reviews, due to the near-empty nature of the present review, some critical reflection is provided to aid interpretation. The feasibility trial component of the included study applied an a priori sample size calculation, validated measures, and appropriate statistical tests. Randomisation at the level of two municipalities and provision of tablets and email reminders added practical feasibility. The integration of data from the different phases of the study using a weaving approach allowed quantitative changes in knowledge to be interpreted alongside qualitative accounts of confidence, feasibility, and barriers to using the COPD web programme. However, the study’s small, predominantly female, convenience sample, limited description of specific care settings and professional roles, and lack of explicit discussion of data saturation or information power constrain generalisability to the wider care home workforce. Regarding setting, having been conducted in two Swedish municipalities within a publicly funded long-term care system, the findings may not readily transfer to the mixed public–private care home systems in many other countries.
4. Discussion
COPD is one of the most common and deadliest chronic diseases worldwide, requiring ongoing treatment, and in many cases necessitating long-term care placement due to a progressive loss of independence [45,46]. Despite COPD’s significant impact on patient health and healthcare systems, educational interventions regarding COPD management in care homes remains severely under-researched. This is reflected in this near-empty review. The comprehensive analysis in the present review identified only one eligible study on this topic, highlighting a major evidence gap in the development and evaluation of COPD educational interventions in care home settings. Empty and near-empty reviews play an important role by drawing attention to significant gaps in knowledge and highlighting areas that require further investigation [47,48]. The near-empty result of the present review underscores a critical need for further research, and this review provides a foundation for targeted recommendations for such future research and educational interventions.
Evidence from community settings has demonstrated that educational and self-management interventions for COPD can reduce hospital re-admission rates and improve patient outcomes [49]. Such interventions often included telemonitoring, education, empowerment for self-management, rehabilitation, multi-disciplinary teamwork, and post-discharge follow-up [49]. Yet, such interventions have not been adapted to care homes. This may stem from the persistent undervaluation of older adult care, particularly in care homes where care staff are often poorly compensated and older people are sometimes perceived as a drain on healthcare resources [50,51,52,53].
Although care home nurses play a critical role in promoting continuity of care, research into their perspectives and experiences with COPD management in care homes remains scarce. In other contexts, the few existing studies on continuity of care in palliative contexts also suggest a lack of targeted educational resources, as well as limited support for the emotional burden experienced by care home staff [54]. The broader literature on chronic disease management in care homes is primarily focused on dementia, although with promising outcomes [55]. For example, educational interventions in care homes may contribute to reduced behavioural and psychological symptoms of dementia [37,56,57,58]. In other areas, educational interventions have shown increased staff knowledge and confidence in the management of heart failure [38] and diabetes [59] within care home settings. Although these successful approaches do not involve COPD-related education, they act as illustrative examples of what targeted education could achieve in care home settings and call for similar application in COPD care, especially as the included study within the present review highlighted the feasibility and value of a digital COPD-related education resource in care homes [44]. However, the authors acknowledged the necessity for broader organisational change to embed new working practices, and thus, further research into these measures should be conducted [44].
Significant barriers limit the implementation and sustainability of educational interventions for COPD across other settings, which likely also contribute to the lack of COPD-related education in care homes. Reviews exploring the feasibility of chronic disease management interventions in primary care identified persistent concerns with the methodological rigour and sustainability of the studies, highlighting the difficulty of implementing effective education in care homes [60,61,62,63,64]. In care homes, such barriers may be exacerbated by factors such as high staff turnover, with reported rates as high as 56.2% for registered nurses and 78.1% for nursing assistants [65]. This instability can negatively impact efforts to invest in or sustain interventions for care home staff, especially time-consuming educational interventions. However, evidence from dementia training initiatives has suggested that comprehensive training programmes can help reduce staff turnover, likely by improving staff satisfaction and reducing stress [57,66]. Therefore, although implementation of these interventions may be challenging, their potential to produce broader positive effects on staff retention and care quality should not be overlooked.
The lack of training and educational resources for COPD management is especially notable considering expert consensus has already ranked the need to ‘identify optimal approaches to training’ as a key research priority to help reduce the global burden of COPD [67]. Priorities also called for further research on improved screening and accurate diagnostic methods for COPD in low-resource primary care settings. The discussed barriers may account for the lack of research addressing these priorities, while the included study in this review re-iterates these implementation challenges. Organisational barriers to the implementation of the digital educational resource were identified, including time constraints and insufficient programme support, challenges in interprofessional collaboration, limited health promotion services, and discrepancies between treatment guidelines and current practices [44]. These findings echo wider evidence that barriers to nurses’ continuing professional development, such as a lack of cover, using personal time or unpaid leave to complete training, and prioritisation of immediate, task-based responsibilities, are persistent and difficult to overcome [68,69,70].
Addressing organisational barriers is, therefore, crucial. Successfully improving COPD management in care homes will depend not only on bridging clinical knowledge gaps, but also on transforming embedded practices and workplace cultures. Without systemic change, even well-designed educational programmes may fail to deliver sustainable improvements. Removing these barriers will empower nurses, elevate care standards for residents, and foster a positive culture of ongoing education within care homes. The included study has provided evidence that COPD-specific education may increase staff knowledge and confidence [44]. Together with the broader literature, this suggests that care home staff education has the potential to improve chronic-disease management, but for COPD specifically, the evidence remains sparse. Further studies are needed before firm conclusions about the impacts of such interventions can be drawn.
4.1. Implications for Future Research and Practice
Given the lack of evaluated COPD-related education for care home staff identified in this review, future research should prioritise the development of curricula that address core content areas directly relevant to everyday practice. These include early recognition and management of exacerbations, appropriate escalation and communication with primary and emergency care, optimisation of inhaler technique and oxygen use, symptom management, nutrition, and advanced care planning [71]. Given emerging evidence that combining nutrition therapy and rehabilitation can preserve muscle mass and improve functional outcomes following COPD exacerbations [19,21], COPD education for care home staff should explicitly incorporate content on recognising and managing malnutrition, the role of physical activity, and simple rehabilitation strategies in long-term care [16,17,22]. Additionally, information on timely referral pathways and collaboration with dietitians and physiotherapists may help to facilitate early mobilisation and practical ways to support dietary intake and exercise within resource-constrained environments. Incorporating education on interprofessional working and role clarity between nurses, care assistants, and allied health professionals is also likely important, given the multidisciplinary nature of long-term care.
The included study suggests that digital, self-directed learning can improve knowledge but may need additional organisational support and facilitation to ensure uptake in busy care home environments [44]. Future interventions could therefore test blended models that combine flexible web-based modules with brief face-to-face or virtual workshops, peer discussion, and clinical facilitation to support translation into practice [72,73,74]. The co-design of such programmes with care home staff and management, as well as residents and family members, may also help tailor the content and delivery to local constraints and preferences.
Future studies should incorporate outcome measures to explore impacts at the staff, resident, and service level, for example, COPD-specific knowledge measures for staff, as well as measures of confidence and self-efficacy in COPD care, while, for residents, symptom burden and health-related quality of life outcomes would add to the evidence base. Finally, at a service level, key outcomes may include the numbers of emergency hospital visits and unplanned GP appointments. Reporting such outcomes will directly address the gaps highlighted by this near-empty review and enable future reviews to move beyond mapping towards robust assessments of effectiveness.
4.2. Strengths and Limitations
The present review applied a rigorous, systematic approach to mapping existing evidence on COPD-related education for care home staff, yet identified only one eligible study in the area. This near-empty result means that conclusions draw on a single study, but also clearly signals a profound evidence gap in the evaluation of COPD educational interventions within care home settings. This review, therefore, offers a valuable contribution by making explicit the scarcity of evaluated interventions and by outlining key avenues for future intervention development and testing in this field.
This review followed internationally recognised methodological and reporting guidance for scoping reviews, including a pre-specified protocol, and a comprehensive search strategy across multiple databases. However, some limitations should be acknowledged, including the inclusion of only studies in the English language, and the exclusion of grey literature such as policy reports and other non-peer-reviewed evidence. These restrictions may have led to the relevant literature not in the English language, or unpublished evidence, being missed. Grey literature was not systematically searched, in order to focus on peer-reviewed studies. However, in the context of care home education, it may be likely that initiatives are developed and evaluated locally without progressing to journal publication, which may have contributed to the near-empty outcome of this review. This could limit the completeness of the evidence map and the extent to which the findings capture real-world implementation practices in diverse care home contexts. Future evidence synthesis on COPD education may benefit from consideration of a broader approach which incorporates grey literature.
5. Conclusions
In conclusion, this scoping review demonstrates that, despite the high burden of COPD among care home residents, and the central role of staff in recognising and managing symptoms, there is almost no empirically evaluated education or training available. The identification of only one eligible intervention highlights a critical missed opportunity to strengthen nurses’ and care assistants’ knowledge, confidence, and skills in COPD management. Addressing this gap has clear implications for nursing practice, ultimately enhancing the quality of care, and the quality of life, for those with COPD in care home settings.
Future studies should prioritise co-design, implementation, and robust evaluation of comprehensive COPD educational programmes tailored to care home staff. Practice-relevant outcomes such as staff knowledge and behaviour, rates of hospital admissions, and residents’ quality of life and symptom burden should be explored. By generating such evidence, consistent and effective COPD management within care homes may be improved.
Overall, this scoping review serves as a foundation for future research into COPD education in care homes. By highlighting the lack of evaluated interventions, future research and quality improvement initiatives may build on the strengths of the existing study and the recommendations provided. Any future interventions provide an opportunity for meaningful advancement in practice and care quality.
Supplementary Materials
The following supporting information (Search Strategy, PRISMA-ScR Checklist) can be downloaded at: https://www.mdpi.com/article/10.3390/nursrep16020043/s1. Supplementary Material 1: PRISMA-ScR Checklist; Supplementary Material 2: Search Strategy.
Author Contributions
Conceptualization, B.C., T.A., S.C., and G.M.; methodology, B.C., T.A., S.C., and G.M.; software, B.C., T.A., and G.M.; formal analysis, B.C., T.A., and G.M.; writing—original draft preparation, B.C.; writing—review and editing, B.C., T.A., S.C., and G.M.; supervision, G.M.; project administration, T.A., S.C., and G.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study.
Public Involvement Statement
No public involvement in any aspect of this research.
Guidelines and Standards Statement
This manuscript was drafted against the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) Checklist.
Use of Artificial Intelligence
Neither AI nor AI-assisted tools were not used in drafting any aspect of this manuscript.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| COPD | Chronic Obstructive Pulmonary Disease |
| JBI | Joanna Briggs Institute |
| PRISMA-ScR | Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Review |
| QoL | Quality of Life |
| MSc | Master of Science |
| NMC | Nursing and Midwifery Council |
References
- Agarwal, A.K.; Raja, A.; Brown, B.D. Chronic Obstructive Pulmonary Disease. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2025. Available online: http://www.ncbi.nlm.nih.gov/books/NBK559281/ (accessed on 27 October 2025).
- Christenson, S.A.; Smith, B.M.; Bafadhel, M.; Putcha, N. Chronic obstructive pulmonary disease. Lancet 2022, 399, 2227–2242. [Google Scholar] [CrossRef]
- Chen, S.; Kuhn, M.; Prettner, K.; Yu, F.; Yang, T.; Bärnighausen, T.; Bloom, D.E.; Wang, C. The global economic burden of chronic obstructive pulmonary disease for 204 countries and territories in 2020–50: A health-augmented macroeconomic modelling study. Lancet Glob. Health 2023, 11, e1183–e1193. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, S.d.O.; Cunha, C.M.C.; Soares, G.M.V.; Silva, P.L.; Silva, A.R.; Gonçalves-de-Albuquerque, C.F. Mechanisms, pathophysiology and currently proposed treatments of chronic obstructive pulmonary disease. Pharmaceuticals 2021, 14, 979. [Google Scholar] [CrossRef] [PubMed]
- Rzadkiewicz, M.; Nasiłowski, J. Psychosocial interventions for patients with severe COPD—An up-to-date literature review. Medicina 2019, 55, 597. [Google Scholar] [CrossRef]
- Stolz, D.; Mkorombindo, T.; Schumann, D.M.; Agusti, A.; Ash, S.Y.; Bafadhel, M.; Bai, C.; Chalmers, J.D.; Criner, G.J.; Dharmage, S.C.; et al. Towards the elimination of chronic obstructive pulmonary disease: A Lancet Commission. Lancet 2022, 400, 921–972. [Google Scholar] [CrossRef] [PubMed]
- Alqahtani, J.S.; Aquilina, J.; Bafadhel, M.; Bolton, C.E.; Burgoyne, T.; Holmes, S.; King, J.; Loots, J.; McCarthy, J.; Quint, J.K.; et al. Research priorities for exacerbations of COPD. Lancet Respir. Med. 2021, 9, 824–826. [Google Scholar] [CrossRef]
- Soler-Cataluña, J.J.; Miravitlles, M.; Fernández-Villar, A.; Izquierdo, J.L.; García-Rivero, J.L.; Cosio, B.G.; López-Campos, J.L.; Agustí, A. Exacerbations in COPD: A personalised approach to care. Lancet Respir. Med. 2023, 11, 224–226. [Google Scholar] [CrossRef]
- Wedzicha, J.A.; Seemungal, T.A. COPD exacerbations: Defining their cause and prevention. Lancet 2007, 370, 786–796. [Google Scholar] [CrossRef]
- Zarowitz, B.J.; O’Shea, T. Chronic Obstructive Pulmonary Disease: Prevalence, characteristics, and pharmacologic treatment in nursing home residents with cognitive impairment. J. Manag. Care Pharm. 2012, 18, 598–606. [Google Scholar] [CrossRef]
- Osundolire, S.; Goldberg, R.J.; Lapane, K.L. Anxiety and depression among US nursing home residents with chronic obstructive pulmonary disease. Int. J. Chronic Obstr. Pulm. Dis. 2023, 18, 1867–1882. [Google Scholar] [CrossRef]
- Miravitlles, M.; Ribera, A. Understanding the impact of symptoms on the burden of COPD. Respir. Res. 2017, 18, 67. [Google Scholar] [CrossRef]
- Schweighart, R.; O’Sullivan, J.L.; Klemmt, M.; Teti, A.; Neuderth, S. Wishes and needs of nursing home residents: A scoping review. Healthcare 2022, 10, 854. [Google Scholar] [CrossRef]
- Kristensen, G.S.; Kjeldgaard, A.H.; Søndergaard, J.; Andersen-Ranberg, K.; Pedersen, A.K.; Mogensen, C.B. Associations between care home residents’ characteristics and acute hospital admissions—A retrospective, register-based cross-sectional study. BMC Geriatr. 2023, 23, 234. [Google Scholar] [CrossRef]
- Crolly-Burton, G.; McCloy, O.; Bennett, M.; Craig, S. Optimising health outcomes in exacerbations of chronic obstructive pulmonary disease. Nurs. Stand. 2025, 40, 53–59. [Google Scholar] [CrossRef]
- Rochester, C.L.; Alison, J.A.; Carlin, B.; Jenkins, A.R.; Cox, N.S.; Bauldoff, G.; Bhatt, S.P.; Bourbeau, J.; Burtin, C.; Camp, P.G.; et al. Pulmonary rehabilitation for adults with chronic respiratory disease: An Official American Thoracic Society Clinical Practice Guideline. Am. J. Respir. Crit. Care Med. 2023, 208, e7–e26. [Google Scholar] [CrossRef]
- Keogh, E.; Mark Williams, E. Managing malnutrition in COPD: A review. Respir. Med. 2021, 176, 106248. [Google Scholar] [CrossRef]
- Tuna, T.; Samur, G. The role of nutrition and nutritional supplements in the prevention and treatment of malnutrition in chronic obstructive pulmonary disease: Current approaches in nutrition therapy. Curr. Nutr. Rep. 2025, 14, 21. [Google Scholar] [CrossRef] [PubMed]
- Collins, P.F.; Yang, I.A.; Chang, Y.-C.; Vaughan, A. Nutritional support in chronic obstructive pulmonary disease (COPD): An evidence update. J. Thorac. Dis. 2019, 11, S2230–S2237. [Google Scholar] [CrossRef]
- Savino-Lloreda, P.; López-Daza, D.; Casas-Herrera, A. Medical nutrition therapy in chronic obstructive pulmonary disease: A narrative review. Nutr. Clin. Pract. 2025, 40, 793–804. [Google Scholar] [CrossRef] [PubMed]
- Oyama, Y.; Tatsumi, H.; Takikawa, H.; Taniguchi, N.; Masuda, Y. Combined effect of early nutrition therapy and rehabilitation for patients with chronic obstructive pulmonary disease exacerbation: A prospective randomized controlled trial. Nutrients 2024, 16, 739. [Google Scholar] [CrossRef] [PubMed]
- Hansen, T.S.; Poulsen, I.; Nørholm, V.; Loft, M.I.; Jensen, P.S. Nutritional support and physical activity intervention programs with a person-centred approach in people with chronic obstructive pulmonary disease: A scoping review. Int. J. Chronic Obstr. Pulm. Dis. 2024, 19, 2193–2216. [Google Scholar] [CrossRef]
- Fletcher, M.J.; Dahl, B.H. Expanding nurse practice in COPD: Is it key to providing high quality, effective and safe patient care? Prim. Care Respir. J. 2013, 22, 230–233. [Google Scholar] [CrossRef]
- Aranburu-Imatz, A.; López-Carrasco, J.d.l.C.; Moreno-Luque, A.; Jiménez-Pastor, J.M.; Valverde-León, M.d.R.; Rodríguez-Cortés, F.J.; Arévalo-Buitrago, P.; López-Soto, P.J.; Morales-Cané, I. Nurse-led interventions in chronic obstructive pulmonary disease patients: A systematic review and meta-analysis. Int. J. Environ. Res. Public Health 2022, 19, 9101. [Google Scholar] [CrossRef] [PubMed]
- NHS England. Respiratory Disease Training Directory: A Guide to Career Frameworks and Education Offers; NHS England: London, UK, 2023. Available online: https://www.hee.nhs.uk/sites/default/files/documents/Respiratory%20Disease%20Training%20Directory.pdf (accessed on 27 October 2025).
- Walter, J.K.; Terry, L.M. Factors influencing nurses’ engagement with CPD activities: A systematic review. Br. J. Nurs. 2021, 30, 60–68. [Google Scholar] [CrossRef] [PubMed]
- NMC. Revalidation—The Nursing and Midwifery Council; NMC: London, UK, 2021; Available online: https://www.nmc.org.uk/revalidation/ (accessed on 27 October 2025).
- NMC. Standards Framework for Nursing and Midwifery Education; NMC: London, UK, 2023; Available online: https://www.nmc.org.uk/globalassets/sitedocuments/standards/2024/standards-framework-for-nursing-and-midwifery-education.pdf (accessed on 27 October 2025).
- Beecham, N.; Doherty, D.E. Improving COPD management in the nursing home—Part 2. Director 2004, 12, 42, 44–49. Available online: https://europepmc.org/article/med/19178117 (accessed on 27 October 2025).
- Yin, H.; Yang, L.; Ye, Q. A systematic review of the effectiveness of clinical nurse specialist interventions in patients with chronic obstructive pulmonary disease (COPD). Front. Nurs. 2018, 5, 147–156. [Google Scholar] [CrossRef]
- Lee, D.T.F.; Lee, I.F.K.; Mackenzie, A.E.; Ho, R.N.L. Effects of a care protocol on care outcomes in older nursing home patients with chronic obstructive pulmonary disease. J. Am. Geriatr. Soc. 2002, 50, 870–876. [Google Scholar] [CrossRef]
- Berland, A.; Bentsen, S.B. Patients with chronic obstructive pulmonary disease in safe hands: An education programme for nurses in primary care in Norway. Nurse Educ. Pract. 2015, 15, 271–276. [Google Scholar] [CrossRef]
- Cross, A.J.; Liang, J.; Thomas, D.; Zairina, E.; Abramson, M.J.; George, J. Educational interventions for health professionals managing chronic obstructive pulmonary disease in primary care. Cochrane Database Syst. Rev. 2022, 2022, CD012652. [Google Scholar] [CrossRef]
- Baverstock, M.; Woodhall, N.; Maarman, V. P94 Do healthcare professionals have sufficient knowledge of inhaler techniques in order to educate their patients effectively in their use? Thorax 2010, 65, A117–A118. [Google Scholar] [CrossRef]
- Ng, S.-W.; Lit, M.P.; Lai, A.Y. Nurses’ reports of inhaler use errors in patients with chronic obstructive pulmonary disease in Hong Kong. Int. J. Chronic Obstr. Pulm. Dis. 2024, 19, 2775–2785. [Google Scholar] [CrossRef]
- Kristensen, G.S.; Søndergaard, J.; Andersen-Ranberg, K.; Mogensen, C.B. Acute readmissions among care home residents aged 65+ years: A register-based study. Eur. Geriatr. Med. 2025, 16, 827–838. [Google Scholar] [CrossRef]
- Piirainen, P.; Pesonen, H.-M.; Siira, H.; Elo, S. The impact of a training intervention on nursing care for people with dementia in long-term care: A quasi-experimental study. Nord. J. Nurs. Res. 2023, 43, 20571585221106066. [Google Scholar] [CrossRef]
- McMahon, J.; Thompson, D.R.; Cameron, J.; Wilson, C.B.; Hill, L.; Tierney, P.; Yu, D.; Moser, D.K.; Spilsbury, K.; Srisuk, N.; et al. Heart failure in nursing homes: A scoping review of educational interventions for optimising care provision. Int. J. Nurs. Stud. Adv. 2024, 6, 100178. [Google Scholar] [CrossRef] [PubMed]
- Munn, Z.; Pollock, D.; Khalil, H.; Alexander, L.; Mclnerney, P.; Godfrey, C.M.; Peters, M.; Tricco, A.C. What are scoping reviews? Providing a formal definition of scoping reviews as a type of evidence synthesis. JBI Evid. Synth. 2022, 20, 950. [Google Scholar] [CrossRef] [PubMed]
- Peters, M.D.J.; Marnie, C.; Tricco, A.C.; Pollock, D.; Munn, Z.; Alexander, L.; McInerney, P.; Godfrey, C.M.; Khalil, H. Updated methodological guidance for the conduct of scoping reviews. JBI Evid. Synth. 2020, 18, 2119. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Peters, M.; Godfrey, C.; McInerney, P.; Munn, Z.; Tricco, A.; Khalil, H. Scoping Reviews (2020 Version) JBI Manual for Evidence Synthesis. In Scoping Reviews (2020 Version); JBI: Adelaide, Australia, 2020. [Google Scholar] [CrossRef]
- Joanna Briggs Institute (JBI). Appendix 11.1 JBI Template Source of Evidence Details, Characteristics and Results Extraction Instrument—JBI Manual for Evidence Synthesis—JBI Global Wiki. Available online: https://jbi-global-wiki.refined.site/space/MANUAL/4687579/Appendix+11.1+JBI+template+source+of+evidence+details%2C+characteristics+and+results+extraction+instrument (accessed on 7 February 2024).
- Nyberg, A.; Lundell, S.; Pesola, U.-M.; Audulv, Å.; Wadell, K. Evaluation of a digital COPD education Pprogram for healthcare professionals in long-term care—A mixed methods study. Int. J. Chronic Obstr. Pulm. Dis. 2022, 17, 905–918. [Google Scholar] [CrossRef]
- World Health Organization (WHO). The Top 10 Causes of Death. Available online: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death (accessed on 27 October 2025).
- Lundell, S.; Pesola, U.-M.; Nyberg, A.; Wadell, K. Groping around in the dark for adequate COPD management: A qualitative study on experiences in long-term care. BMC Health Serv. Res. 2020, 20, 1025. [Google Scholar] [CrossRef]
- Gray, R. Empty systematic reviews: Identifying gaps in knowledge or a waste of time and effort? Nurse Author Ed. 2021, 31, 42–44. [Google Scholar] [CrossRef]
- Slyer, J.T. Unanswered questions: Implications of an empty review. JBI Evid. Synth. 2016, 14, 1–2. [Google Scholar] [CrossRef]
- Corcoran, R.; Moore, Z.; Avsar, P.; Murray, B. Home-based management on hospital re-admission rates in COPD patients: A systematic review. J. Adv. Nurs. 2024, 80, 3955–3964. [Google Scholar] [CrossRef]
- Allan, S.; Vadean, F. The impact of wages on care home quality in England. Gerontologist 2023, 63, 1428–1436. [Google Scholar] [CrossRef]
- Meeuwesen, J. Working with Less, Giving More: The Impact of Undervaluation on Healthcare Personnel in Dutch Elderly Homes; Radbound University: Nijmegen, The Netherlands, 2020; Available online: https://theses.ubn.ru.nl/items/8907cdc7-de1b-4337-9a14-1f46311fd205 (accessed on 8 January 2026).
- Mallorie, S. The Adult Social Care Workforce in a Nutshell; The King’s Fund: London, UK, 2024; Available online: https://www.kingsfund.org.uk/insight-and-analysis/data-and-charts/social-care-workforce-nutshell (accessed on 19 January 2026).
- Schlepper, L.; Dodsworth, E. The Decline of Publicly Funded Social Care for Older Adults; Nuffield Trust: London, UK, 2023; Available online: https://www.nuffieldtrust.org.uk/resource/the-decline-of-publicly-funded-social-care-for-older-adults (accessed on 19 January 2026).
- Roos, S.; Sjöström, M.; Medin, J.; Melin-Johansson, C. Experiences of continuity of care among registered nurses caring for patients with chronic obstructive pulmonary disease in primary care: A qualitative study. J. Adv. Nurs. 2025, 81, 8848–8858. [Google Scholar] [CrossRef] [PubMed]
- Boscart, V.; Crutchlow, L.E.; Sheiban Taucar, L.; Johnson, K.; Heyer, M.; Davey, M.; Costa, A.P.; Heckman, G. Chronic disease management models in nursing homes: A scoping review. BMJ Open 2020, 10, e032316. [Google Scholar] [CrossRef] [PubMed]
- Scerri, A.; Scerri, C. Outcomes in knowledge, attitudes and confidence of nursing staff working in nursing and residential care homes following a dementia training programme. Aging Ment. Health 2019, 23, 919–928. [Google Scholar] [CrossRef]
- Parveen, S.; Smith, S.J.; Sass, C.; Oyebode, J.R.; Capstick, A.; Dennison, A.; Surr, C.A. Impact of dementia education and training on health and social care staff knowledge, attitudes and confidence: A cross-sectional study. BMJ Open 2021, 11, e039939. [Google Scholar] [CrossRef]
- Carrier, D.; Toulouse, É.; Rochefort, C.M. Staff training interventions to prevent or reduce behavioural and psychological symptoms of dementia in nursing home residents: A mixed methods systematic review. Dement. Geriatr. Cogn. Disord. 2023, 52, 117–146. [Google Scholar] [CrossRef]
- Lega, I.C.; Kapur, A.; Leung, F.; Zahedi, A. Type 2 diabetes in older adults in long-term care homes: An educational intervention to improve diabetes care. Can. J. Diabetes 2020, 44, 407–413.e3. [Google Scholar] [CrossRef]
- Stephen, C.; McInnes, S.; Halcomb, E. The feasibility and acceptability of nurse-led chronic disease management interventions in primary care: An integrative review. J. Adv. Nurs. 2018, 74, 279–288. [Google Scholar] [CrossRef]
- Yeoh, E.K.; Wong, M.C.S.; Wong, E.L.Y.; Yam, C.; Poon, C.M.; Chung, R.Y.; Chong, M.; Fang, Y.; Wang, H.H.X.; Liang, M.; et al. Benefits and limitations of implementing Chronic Care Model (CCM) in primary care programs: A systematic review. Int. J. Cardiol. 2018, 258, 279–288. [Google Scholar] [CrossRef]
- Raghavan, D.; Drummond, K.L.; Sanders, S.A.; Kirchner, J. Use of implementation science to qualitatively identify implementation determinants of COPD practice guidelines in primary care. Chron. Respir. Dis. 2025, 22, 14799731251314870. [Google Scholar] [CrossRef]
- Wang, T.; Tan, J.Y.; Liu, X.L.; Zhao, I. Barriers and enablers to implementing clinical practice guidelines in primary care: An overview of systematic reviews. BMJ Open 2023, 13, e062158. [Google Scholar] [CrossRef]
- Federman, A.D.; O’Conor, R.; Nnemnbeng, J.; Ankam, J.; McDermott, D.; Lindenauer, P.K.; Wolf, M.S.; Wisnivesky, J.P. Feasibility trial of a comprehensive, highly patient-centered COPD self-management support program. Chronic Obstr. Pulm. Dis. J. COPD Found. 2023, 11, 13–25. [Google Scholar] [CrossRef]
- Gandhi, A.; Yu, H.; Grabowski, D.C. High nursing staff turnover in nursing homes offers important quality information. Health Aff. 2021, 40, 384–391. [Google Scholar] [CrossRef] [PubMed]
- de Burca, D. Closing the Skills Gap in Adult Social Care. Available online: https://www.skillsforcare.org.uk/news-and-events/blogs/closing-the-skills-gap-in-adult-social-care (accessed on 19 January 2026).
- Adeloye, D.; Agarwal, D.; Barnes, P.J.; Bonay, M.; van Boven, J.F.; Bryant, J.; Caramori, G.; Dockrell, D.; D’Urzo, A.; Ekström, M.; et al. Research priorities to address the global burden of chronic obstructive pulmonary disease (COPD) in the next decade. J. Glob. Health 2021, 11, 15003. [Google Scholar] [CrossRef] [PubMed]
- King, R.; Taylor, B.; Talpur, A.; Jackson, C.; Manley, K.; Ashby, N.; Tod, A.; Ryan, T.; Wood, E.; Senek, M.; et al. Factors that optimise the impact of continuing professional development in nursing: A rapid evidence review. Nurse Educ. Today 2021, 98, 104652. [Google Scholar] [CrossRef]
- Mamba, W.M.; Dludlu, M.S. Exploring barriers to continuing nursing education among nurses: A descriptive qualitative study. Nurs. Sci. Clin. Pract. 2025, 1, 9–18. Available online: https://nscp.cultechpub.com/nscp/article/view/8/5 (accessed on 19 January 2026).
- Yu, X.; Huang, Y.; Liu, Y. Nurses’ perceptions of continuing professional development: A qualitative study. BMC Nurs. 2022, 21, 162. [Google Scholar] [CrossRef]
- Patel, N. An update on COPD prevention, diagnosis, and management: The 2024 GOLD Report. Nurse Pract. 2024, 49, 29. [Google Scholar] [CrossRef]
- Watson, A.; Wilkinson, T.M. Digital healthcare in COPD management: A narrative review on the advantages, pitfalls, and need for further research. Ther. Adv. Respir. Dis. 2022, 16. [Google Scholar] [CrossRef] [PubMed]
- Ramachandran, H.J.; Oh, J.L.; Cheong, Y.K.; Jiang, Y.; Teo, J.Y.C.; Seah, C.W.A.; Yu, M.; Wang, W. Barriers and facilitators to the adoption of digital health interventions for COPD management: A scoping review. Heart Lung 2023, 59, 117–127. [Google Scholar] [CrossRef] [PubMed]
- Siu, D.C.; Gafni-Lachter, L. Addressing barriers to Chronic Obstructive Pulmonary Disease (COPD) care: Three innovative evidence-based approaches: A review. Int. J. Chronic Obstr. Pulm. Dis. 2024, 19, 331–341. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2026 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.