Nurses’ Experience of Caring for Patients with Delirium: Systematic Review and Qualitative Evidence Synthesis
Abstract
1. Introduction
1.1. Background
1.2. Aim
2. Materials and Methods
2.1. Inclusion and Exclusion Criteria
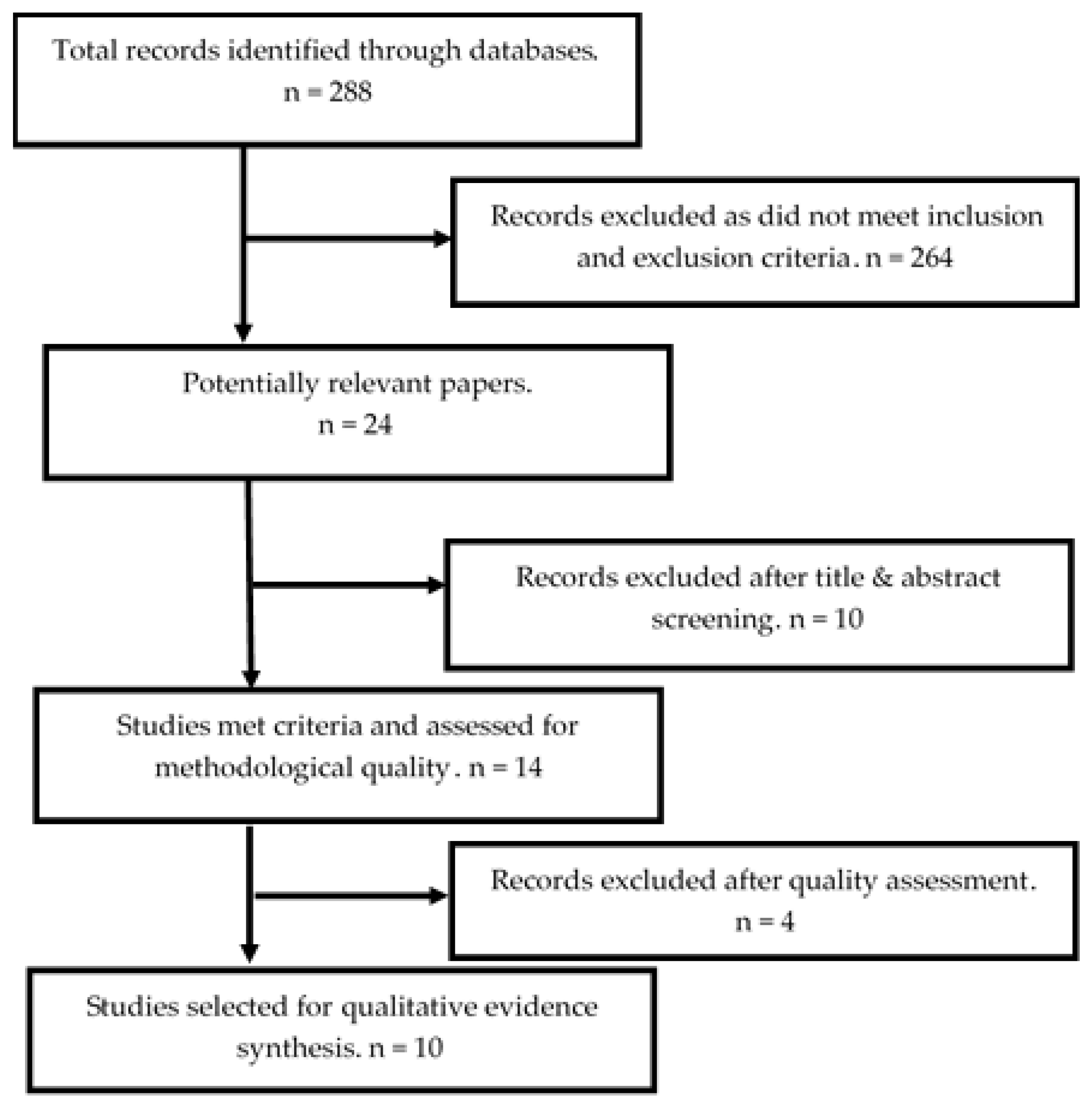
2.2. Search Strategy
2.3. Study Screening
2.4. Assessment of Methodological Quality
2.5. Data Extraction and Synthesis
3. Results
3.1. The Deficit in Updated Knowledge, Education and Resources
“Assessment is usually crucial, but it just knows how to assess… I don’t know what the questions would be.”[18] (p. 823)
“Both novice and experienced nurses talked about learning to deal with patients with delirium from watching how other nurses dealt with it. They stated that they had not learned or could not remember learning much about delirium in their formal education.”[15] (p. 331)
“A nurse reported: ‘…when we actually have a delirious patient, and nothing seems to be working. I don’t know what would be better, I guess, and that’s what makes it very frustrating because you feel very helpless.’”[27] (p. 333)
3.2. Caring for Patients with Delirium, Impacts Heavily on the Nurses’ Workload
“… so, whilst one person might help the nursing staff with that confused patient, that nursing staff member still has to deal with everything around that patient like medications, treatment…”[16] (p. 892)
“Caring for delirious patients was described as not only emotionally challenging and frustrating, but also physically exhausting…”[20] (p. 97)
“For me it is extremely distressing, because most of the time you are short staffed, and you are on your own and have eight patients, and you have two confused patients, and you are just everywhere.”[25] (p. 330)
3.3. The Unpredictable Nature of Patients with Delirium, which Creates Safety Concerns
“A lot of patients are difficult to get along. When we are trying to help them stay quiet and comfortable, they may hit us…”[19] (p. 6)
“I’m always concerned about their safety when I go in and they are confused, not directable.”[15] (p. 330)
3.4. Provision of Care Achieved Using Various Strategies
“We sat down, and we talked about the behaviours that had been happening over the last few days…”[18] (p. 1360)
4. Discussion
4.1. Implications of Research
4.2. Implications for Practice
4.3. Limitations of the Review
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Ozaban, A.; Acaroglu, R. Delirium assessment in intensive care units: Practices and perceptions of Turkish nurses. Nurs. Crit. Care 2015, 21, 271–278. [Google Scholar] [CrossRef] [PubMed]
- Docherty, E.; Mounsey, C. Delirium: Suspect it, spot it and stop it. Kai Tiaki Nurs. Res. 2016, 22, 12–14. [Google Scholar]
- Australian Commission on Safety and Quality in Health Care. Delirium Care Standard. 2016. Available online: https://www.safetyandquality.gov.au/our-work/clinical-care-standards/delirium-clinical-care-standard/ (accessed on 2 July 2019).
- Partridge, J.S.L.; Martin, F.C.; Harari, D.; Dhesi, J.K. The delirium experience: What is the effect on patients, relatives and staff and what can be done to modify this. Int. J. Geriatr. Psychiatry 2012, 28, 804–812. [Google Scholar] [CrossRef]
- Boot, R. Delirium: A review of the nurse’s role in the intensive care unit. Intensive Crit. Care Nurs. 2012, 28, 185–189. [Google Scholar] [CrossRef] [PubMed]
- Phillips, L.A. Delirium in Geriatric Patients: Identification and Prevention. Med. Surg. Nurs. 2013, 22, 9–12. [Google Scholar]
- Ijkema, R.; Langelaan, M.; Steeg, L.V.; Wagner, C. Do Patient Characteristics Influence Nursing Adherence to a Guideline for Preventing Delirium. J. Nurs. Scholarsh. 2014, 46, 147–153. [Google Scholar] [CrossRef] [PubMed]
- LaFever, S.; Bory, A.; Nelson, J. Delirium in patients with cancer: What nurses need to know to improve care. Clin. J. Oncol. Nurs. 2015, 19, 585–590. [Google Scholar] [CrossRef]
- Bozzo, M. The barriers and enablers related to the early recognition of delirium in older palliative care patients—An integrative literature review. Aust. Nurs. Midwifery Fed. 2015, 23, 28–31. [Google Scholar]
- Munk, L.; Andersen, L.P.H.; Gogenur, I. Emergence Delirium. J. Perioper. Pract. 2013, 23, 251–254. [Google Scholar] [CrossRef] [PubMed]
- Godfrey, M.; Smith, J.; Green, J.; Cheater, F.; Inouye, S.K.; Young, J.B. Developing and implementing an integrated delirium prevention system of care: A theory driven, participatory research study. BMC Health Serv. Res. 2013, 13, 1–15. [Google Scholar] [CrossRef]
- Kristiansen, S.; Konradsen, H.; Beck, M. Nurses’ experiences of caring for older patients afflicted by delirium in a neurological department. J. Clin. Nurs. 2018, 28, 920–930. [Google Scholar] [CrossRef] [PubMed]
- Martins, S.; Pinho, E.; Correia, R.; Moreira, E.; Lopes, L.; Paiva, J.A.; Azevedo, L.; Fernandes, L. What effect does delirium have on family and nurses of older adult patients? Aging Ment. Health 2017, 22, 903–911. [Google Scholar] [CrossRef]
- Christensen, M. Nurses’ knowledge of delirium: A survey of theoretical knowing. Kai Tiaki Nurs. Res. 2016, 7, 11–18. [Google Scholar]
- Kjorven, M.; Rush, K.; Hole, R. A discursive exploration of the practices that shape and discipline nurses’ responses to postoperative delirium. Nurs. Inq. 2011, 18, 325–335. [Google Scholar] [CrossRef] [PubMed]
- Agar, M.; Draper, B.; Phillips, P.A.; Phillips, J.; Collier, A.; Harlum, J.; Currow, D. Making decisions about delirium: A qualitative comparison of decision making between nurses working in palliative care, aged care, aged care psychiatry, and oncology. Palliat. Med. 2011, 26, 887–896. [Google Scholar] [CrossRef] [PubMed]
- Schofield, I.; Tolson, D.; Fleming, V. How nurses understand and care for older people with delirium in the acute hospital: A Critical Discourse Analysis. Nurs. Inq. 2012, 19, 165–176. [Google Scholar] [CrossRef]
- Hosie, A.; Agar, M.; Lobb, E.; Davidson, P.M.; Phillips, J. Identifying the barriers and enablers to Palliative Care Nurses’ recognition and assessment of delirium symptoms: A qualitative study. J. Pain Symptom Manag. 2014, 48, 815–830. [Google Scholar] [CrossRef]
- Yue, P.; Wang, L.; Liu, C.; Wu, Y. A qualitative study on experience of nurses caring for patients with delirium in ICUs in China: Barriers, burdens and decision making dilemmas. Int. J. Nurs. Sci. 2015, 2, 2–8. [Google Scholar] [CrossRef]
- Zamoscik, K.; Godbold, R.; Freeman, P. Intensive care nurses’ experiences and perceptions of delirium and delirium care. Intensive Crit. Care Nurs. 2017, 40, 94–100. [Google Scholar] [CrossRef]
- Tong, A.; Flemming, K.; McInnes, E.; Oliver, S.; Sandy, C. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med. Res. Methodol. 2012, 12, 181–188. [Google Scholar] [CrossRef] [PubMed]
- Dixon-Woods, M.; Agarwal, S.; Jones, D.; Young, B.; Sutton, A. Synthesizing qualitative and quantitative evidence: A review of possible methods. J. Health Serv. Res. Policy. 2005, 10, 45–53. [Google Scholar] [CrossRef]
- Lockwood, C.; Porrit, K.; Munn, Z.; Rittenmeyer, L.; Salmond, S.; Bjerrum, M.; Loveday, H.; Carrier, J.; Stannard, D. Chapter 2: Systematic reviews of qualitative evidence. In Aromataris; Munn, Z.E., Ed.; Joanna Briggs Institute Reviewer’s Manual, The Joanna Briggs Institute: Adelaide, Australia, 2017; Available online: https://reviewersmanual.joannabriggs.org/ (accessed on 2 July 2019).
- The Joanna Briggs Institute. Joanna Briggs Institute Reviews Manual 2014. 2014. Available online: http://www.joannabriggs.org/assets/docs/sumari/ReviewersManual-2014.pdf (accessed on 2 July 2019).
- Brooke, J.; Manneh, C. Caring for a patient with delirium in an acute hospital: The lived experience of cardiology, elderly care, renal, and respiratory nurses. Int. J. Nurs. Pract. 2018, 24, e12643. [Google Scholar] [CrossRef]
- Leblanc, A.; Bourbonnais, F.F.; Harrison, D.; Tousignant, K. The experience of intensive care nurses caring for patients with delirium: A phenomenological study. Intensive Crit. Care Nurs. 2018, 44, 92–98. [Google Scholar] [CrossRef]
- Schmitt, E.M.; Gallagher, J.; Albuquerque, A.; Tabloski, P.; Lee, H.J.; Gleason, L.; Weiner, L.S.; Marcantonio, E.R.; Jones, R.N.; Inouye, S.K.; et al. Perspectives on the delirium experience and its burden: Common themes among older patients, their family caregivers, and nurses. Gerontologist 2019, 59, 327–337. [Google Scholar] [CrossRef]
- Hosie, A.; Agar, M.; Lobb, E.; Davidson, P.M.; Phillips, J. Palliative care nurses’ recognition and assessment of patients with delirium symptoms: A qualitative study using critical incident technique. Int. J. Nurs. Stud. 2014, 51, 1353–1365. [Google Scholar] [CrossRef] [PubMed]
- Dahlke, S.; Phinney, A. Caring for Hospitalized Older Adults at Risk for Delirium. J. Gerontol. Nurs. 2008, 34, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Brooks, P.B. Postoperative delirium in elderly patients. Am. J. Nurs. 2012, 112, 38–49. [Google Scholar] [CrossRef] [PubMed]
- Schofield, I. Delirium: Challenges for clinical governance. J. Nurs. Manag. 2008, 16, 127–133. [Google Scholar] [CrossRef]
- Donnell, S.M.; Timmis, F. A quantitative exploration of the subjective burden experienced by nurses when caring for patients with delirium. J. Clin. Nurs. 2012, 21, 2488–2498. [Google Scholar] [CrossRef]
- Luetz, A.; Heymann, A.; Radtke, F.M.; Chenitir, C.; Neuhaus, U.; Nachtigall, I.; von Dossow, V.; Marz, S.; Eggers, V.; Heinz, A.; et al. Different assessment tools for intensive care unit delirium: Which score to use. Crit. Care Med. 2010, 38, 409–418. [Google Scholar] [CrossRef]
| Authors | Purpose | Participants | Methods | Analysis |
|---|---|---|---|---|
| Agar et al., [16] | To explore nurses’ assessment and management of delirium when caring for people with cancer, the elderly or older people requiring psychiatric care in the inpatient setting. | n = 40 registered nurses working in public hospital inpatient dedicated units in palliative care, aged care, aged care psychiatry or oncology in South West Sydney, Australia. | Open ended semi-structured interviews. | Thematic content analysis. |
| Hosie et al., [18] | To explore the experiences, views and practices of inpatient palliative care nurses in delirium recognition and assessment. | n = 30 nurses from nine specialist palliative care inpatient services, Australia | Critical incident technique and semi-structured interviews. | Thematic content analysis |
| Kjroven et al. [15] | To examine the language practices and discourses that shape and discipline nurses care for patients with post-operative delirium. | n = 6 nurses working in a surgical ward in Canora Jubilee Hospital, Canada. | Face to face in-depth interviews | Foucauldian post structural/postmodern model and Content analysis |
| Hosie et al., [18] | To identify was to identify nurses’ perceptions of the barriers and enablers to recognising and assessing delirium symptoms in palliative inpatient settings. | n = 31 nurses from 9 specialist palliative care inpatient services in Australia. | Semi structured questionnaire. | Thematic analysis. |
| Yue et al., [19] | To explore the experiences of nurses caring for patients with delirium in ICU in China. | n = 14 ICU nurses in Beijing, China. | Semi-structured | Thematic analysis. |
| Zamoscik et al., [20] | To explore nurses’ experiences and perceptions of delirium, managing delirious patients, and screening for delirium, five years after introduction of the Confusion Assessment Method for Intensive Care into standard practice. | n = 12 nurses from a medical- surgical intensive care unit at a large teaching hospital in the United Kingdom. | qualitative interviews. | Thematic analysis |
| Brooke & Manneh, [25] | To explore the lived experiences of caring for a patient during an acute episode of delirium by nurses working in cardiology, elderly care, renal, or respiratory specialities. | n = 23 nurses were recruited, including nurses from: cardiology (n = 6), elderly care (n = 5), renal (n = 6), and respiratory (n = 6), UK. | Focus group discussions | Thematic analysis |
| LeBlanc et al., [26] | To explore the lived experience of ICU nurses caring for patients with delirium | n = 8 Participants in this study were recruited from two ICUs in a university- affiliated, tertiary care academic health care centre in Canada | Semi-structured interview | Thematic analysis |
| Kristiansen et al., [12] | To investigate nurses’ experiences of caring for older (65+ years) patients afflicted by delirium in a neurological department. | n = 14 nurses from the neurology department in Denmark. | Interview | Thematic analysis |
| Schmitt et al. [27] | To investigate common delirium burdens from the perspectives of patients, family caregivers, and nurses. | n = 15 nurses from an urban teaching hospital in Boston, Massachusetts, US | Focus groups and interviews | Thematic analysis |
| Category | Summary | Credibility Rating | Illustration |
|---|---|---|---|
| Concept ambiguity | Nurses were unaware about the process and course of delirium, causing difficulties in understanding the patients. | Unawareness regarding process and course of delirium (U) 1 | “It is difficult for me to distinguish delirium from other neurological disorders as I haven’t learned how to tell the difference. For example, temporal lobe damage also results in the same kind of restless movement as delirium. Therefore, I can’t tell if the symptoms are the result of cerebral haemorrhage or delirium. I don’t know what definition of delirium is.” (Yue et al., [19] (p. 5)). |
| Lack of knowledge and education | The deficit in knowledge and education created lack of confidence in nurses to provide appropriate care. | Knowledge deficit (U) | “I just think as nurses we are not trained enough in dealing with delirium.” (Hosie et al., [18] (p. 823)). |
| Resources and staffing | The shortage in staff and lack of resources, left the vulnerable and unsupported. | Level of staffing and other resources (C) 1 | “… so whilst one person might help the nursing staff with that confused patient, that nursing staff member still has to deal with everything around that patient like medications, treatment…” (Agar et al., [16] (p. 892)). |
| Workload | Nurses experienced increased workload, and frustration from the workload, when caring for patients with delirium. | Unyielding workload (U) | “It means putting other things aside and treating the immediate needs. I have to divert my attention to helping them with whatever is happening right now.” (LeBlanc et al., [26] (p. 95)) |
| Time restraints | The care of patients with delirium was time consuming and nurses felt they were unfair to the other patients | Lack of time (C) | “Some participants noticed that nurses often fail to undertake the test due to time constraints and that the results are not always reported to the doctors.” (Zamoscik et al., [20] (p. 96)). |
| “It is sometimes extremely time consuming guiding them 100 times back to bed, and at the same time, I think that I have five other bells also ringing, and I actually need to go complete rounds on all my patients.” (Kristiansen, Konradsen & Beck, [12] (p. 924)) | |||
| Stress and anxiety | Caring for patients with delirium generated stress, anxiety and mental conflicts in the nurses caring for them. | Nurses feeling pressured (C) | “Despite nurse doing her best to prevent patient from removing tubes, the incidence still leaves the nurse feeling very nervous. The nurses are always under pressure.” (Yue et al., [19] (p. 5)). |
| Nurse’s safety | Nurses were concerned and feared for their own safety. | Feeling unsafe (U) | “We had a lovely lady who became confused with a UTI, she was a completely different person, and she was verbally aggressive, she did try to throw things, pinch and punch, but we understood that she was confused” (Brooke et al., [25] (p. 5)) |
| Patient’s safety | Patient safety was a prime priority for all nurses. | Ensuring patient safety (U) | “I’m always concerned about their safety when I go in and they are confused, not directable.” (Kjorven et al., [15] (p. 330)). |
| Constant surveillance | Staying with the patient constantly to ensure safety of the patient. | Closely monitoring and following the patient (C) | “Specials (one on one nursing) was thought an ideal strategy…” (Agar et al., [16] (p. 892)). |
| Restraints | The use of physical and chemical restraints to control the confused patient. | Use of side rails and sedatives (C) | “Non-pharmacological interventions were highly valued…” “Bed rails were sometimes helpful” (Agar et al., [16] (p. 892)). |
| Family support | Family members play a vital role in the management of delirium and provide support to the nurses caring for patients with delirium. | Role of family members in calming the patient (C) | “Sometimes, we call the family member and ask them to come to the ICU to comfort the patient. This approach works well. As soon as the patients see their family members, they calm down and regain their consciousness.” (Yue et al., [19] (p. 6)). |
| Support from peers | Nurses are supported by their peers in care of patients with delirium and learn from the experience of other nurses. | Peer nurses were involved in decision making (U) | ‘‘We sat down and we talked about the behaviours that had been happening over the last few days.” (Hosie et al. [28] (p. 1360)) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thomas, N.; Coleman, M.; Terry, D. Nurses’ Experience of Caring for Patients with Delirium: Systematic Review and Qualitative Evidence Synthesis. Nurs. Rep. 2021, 11, 164-174. https://doi.org/10.3390/nursrep11010016
Thomas N, Coleman M, Terry D. Nurses’ Experience of Caring for Patients with Delirium: Systematic Review and Qualitative Evidence Synthesis. Nursing Reports. 2021; 11(1):164-174. https://doi.org/10.3390/nursrep11010016
Chicago/Turabian StyleThomas, Nissy, Mardhie Coleman, and Daniel Terry. 2021. "Nurses’ Experience of Caring for Patients with Delirium: Systematic Review and Qualitative Evidence Synthesis" Nursing Reports 11, no. 1: 164-174. https://doi.org/10.3390/nursrep11010016
APA StyleThomas, N., Coleman, M., & Terry, D. (2021). Nurses’ Experience of Caring for Patients with Delirium: Systematic Review and Qualitative Evidence Synthesis. Nursing Reports, 11(1), 164-174. https://doi.org/10.3390/nursrep11010016







