Abstract
Background: Developmental dysplasia of the hip (DDH) is a common disorder of atypical hip development. Pelvic osteotomy (e.g., according to Salter, Pemberton or Dega) may be indicated for children with DDH at walking age. The most popular postoperative treatment is a hip spica cast. Alternative postoperative options include abduction braces and non-weightbearing protocols combined with physical therapy. The aim of this systematic review was to determine the most effective form of postoperative treatment after unilateral pelvic osteotomy in children with DDH in terms of clinical and radiological outcomes and complications. Methods: A systematic review was conducted and reported according to Preferred Reporting Items for Systematic Reviews and Meta-Analysis 2020 guidelines and registered in the international prospective register of systematic reviews. Articles were selected from PubMed, Embase and Cochrane databases. The quality of all (non-)randomized included studies was assessed using the Methodological Index for Non-Randomized Studies (MINORS) criteria. Results: The search strategy yielded 3524 articles. Fourteen articles with 367 total hips were included in this review. A total of 312 hips were treated with spica casts, 49 with abduction braces and 6 with non-weightbearing protocols. The quality of evidence was moderate (MINORS, 3–12 points). All types of postoperative treatments had good clinical outcomes overall, without secondary displacement of the osteotomy. Clinical outcomes for spica casts were reported according to McKay’s criteria in 135 hips, with 123 excellent and 12 good results. Clinical outcomes for abduction braces showed satisfaction for all parents (49 of 49). The radiological outcome was overall well preserved with any postoperative treatment. There was a higher complication rate with the use of hip spica casts, including avascular necrosis, pain complaints and superficial infections. Conclusion: This systematic review showed no benefit of postoperative spica casts compared with abduction braces and avoidance of weightbearing after simple pelvic osteotomy for residual DDH.
1. Introduction
Developmental dysplasia of the hip (DDH) is a disorder of abnormal development of the hip joint [1,2,3,4] and can be divided into dislocated, subluxed and dysplastic hips [1,2,3,4]. The incidence of hip dysplasia is 10 in 1000 children, and the incidence of a hip dislocation is approximately 1 in 1000 [5,6]. The cause of DDH is still unknown. Next to mechanical and environmental factors, genetic factors have been studied and associated with the development of DDH. Several risk factors are known, such as positive family history, female sex and breech positioning in the third trimester [7]. In a recent retrospective single-center multifactorial study of Ionescu et al. [8], it was found that there is an association of two or more risk factors with DDH. However, each factor alone did not have an influence on pathological hip development.
Irrespective of the risk factors, the clinical examination of newborns has to be performed on every child. In children with positive risk factors, ultrasound examination is recommended at the age of 6 weeks. Overall, hip ultrasound is considered the gold standard for the diagnosis and monitoring of DDH in children under 6 months old [9].
The standard treatment for DDH in the newborn is an abduction device (e.g., Pavlik harness). In cases of residual dysplasia or missed dislocations after the age of 18–24 months, more invasive treatments such as femoral osteotomies and pelvic osteotomies are required [10,11,12]. Common pelvic osteotomy procedures are the Salter, Dega and Pemberton osteotomies [1]. These osteotomies are suitable for children with an open triradiate cartilage [1,13]. The age of the child, the location and the severity of the acetabular dysplasia and the preference of the surgeon may be important factors in determining which type of pelvic osteotomy will be performed [14].
After a pelvic osteotomy, the most popular immobilization method for children with DDH is a hip spica cast to assist in pain relief and osseous union [15]. There are different types of spica casts: single-leg casts, ‘one and a half’, bilateral short-leg casts, bilateral long-leg casts and hip spica with a reinforcement bar. A spica cast can be applied with plaster or fiberglass. The casts are usually applied for a period of 6–12 weeks. A period of physiotherapy assistance may be required for children, as their muscles and ligaments could be tight and sore after the plaster immobilization. However, spica casting may be inconvenient for the patients and their parents [15]. It could result in superficial skin irritations, redness, blistering, open or draining wound areas, pressure spot lesions and infections. Other side effects mentioned are pain complaints and rigidity of the hip joint [6,15].
There are several alternatives to hip spica casts, such as functional rehabilitation and abduction braces [6,15]. Functional rehabilitation promotes hip function, strengthens the hip joint and maximizes the patient’s range of motion. The abduction brace is used to prevent excessive hip flexion and to provide stability to the hip. It is unknown, however, if alternative forms of postoperative treatment have a comparable result to spica casting after a unilateral pelvic osteotomy.
The aim of this systematic review was to determine whether there was a difference between the spica cast and alternative postoperative treatments (particularly abduction braces and non-weightbearing) regarding relevant clinical and radiological outcome measures as well as complications in children with DDH who underwent unilateral pelvic osteotomy.
2. Materials and Methods
2.1. Study Design
The review was conducted and reported according to the ‘Preferred Reporting Items for Systematic Reviews and Meta-Analyses’ guidelines (PRISMA 2020) [16,17]. In addition, the review was registered in the international prospective register of systematic reviews (PROSPERO) [16,17] under registration number CRD42021289732.
2.2. Article Selection and Methodological Quality
Articles were searched in multiple databases (PubMed, Embase and Cochrane) on 20 October 2021. The search strategy can be retrieved from Appendix A (Table A1). The selected studies were not blinded with respect to the author, affiliation or source. The systematic review was performed using Rayyan [18], a web application systematic review tool. Duplicate records were identified and removed with the Mendeley citation manager [19]. Two independent reviewers (MM and RvS) screened the titles, abstracts, full texts and reference lists. If there was no agreement between these reviewers, an independent reviewer (CvB) was involved. Data extraction was performed by one researcher (MM). Authors of articles that did not mention the type of postoperative treatment or that did not distinguish between different subgroups regarding the results (in case some patients also underwent concomitant or bilateral procedures) were contacted by mail in order to obtain the original data. The quality of all included (non-)randomized studies was assessed using the ‘Methodological Index for Non-Randomized Studies’ (MINORS index) criteria [17,20].
2.3. Inclusion and Exclusion Criteria
Original studies were selected if they included children with an open triradiate cartilage that had undergone a simple pelvic osteotomy (e.g., according to Salter, Pemberton or Dega) and if postoperative treatment was described. Studies needed to report on at least one relevant outcome parameter, i.e., pain, satisfaction, consolidation, complication rates or clinical and/or radiographic outcomes. Studies were only considered if they included a minimum of five patients and were written in English, French, German or Dutch. Review articles, letters to the editor, case reports, expert opinions and surgical technique papers were excluded. Moreover, studies about other types of pelvic osteotomies were excluded (e.g., Chiari, periacetabular or triple osteotomy). Papers that described simultaneous bilateral procedures and/or combined procedures were also excluded.
2.4. Data Extraction
The following baseline parameters were recorded when available: number of patients, sex, age, type of surgical treatment, type and duration of postoperative treatment and the duration of follow-up. In addition, relevant outcome parameters were recorded, including pain, satisfaction, consolidation and clinical and radiographic complications (graft displacement, loss of integrity and prolonged hospital stay due to complications), as well as functional and radiographic outcomes (the preoperative, first and final postoperative acetabular index (AI), the center-edge angle (CEA) and the Severin score). The clinical methods of evaluation that were used were McKay’s criteria and the Trevor clinical score. McKay’s criteria [21] is a clinical evaluation system for the measurement of the presence of a limp, symptoms of pain in the hip, the Trendelenburg sign and the range of movement, with a possible grading from I to IV (excellent to poor). Trevor’s clinical score [22] is a measure of pain complaints, the range of motion, the function of the hip as considered by the patient and radiological assessment (with a maximum score of 20 points). The score can be excellent (18–20), good (15–17), fair (12–14) and poor (<12). Overall good clinical outcome was defined as either a good/excellent McKay’s criteria or Trevor’s score or satisfaction of the children and parents with the treatment.
2.5. Statistical Analysis
This review presents descriptive data, such as the mean and the range of the age (in months) and the mean follow-up (in months). No meta-analysis of the data was conducted due to the heterogeneity of the included studies. This was mainly because the mean age of the children and follow-up times ranged widely.
3. Results
3.1. Literature Search Process
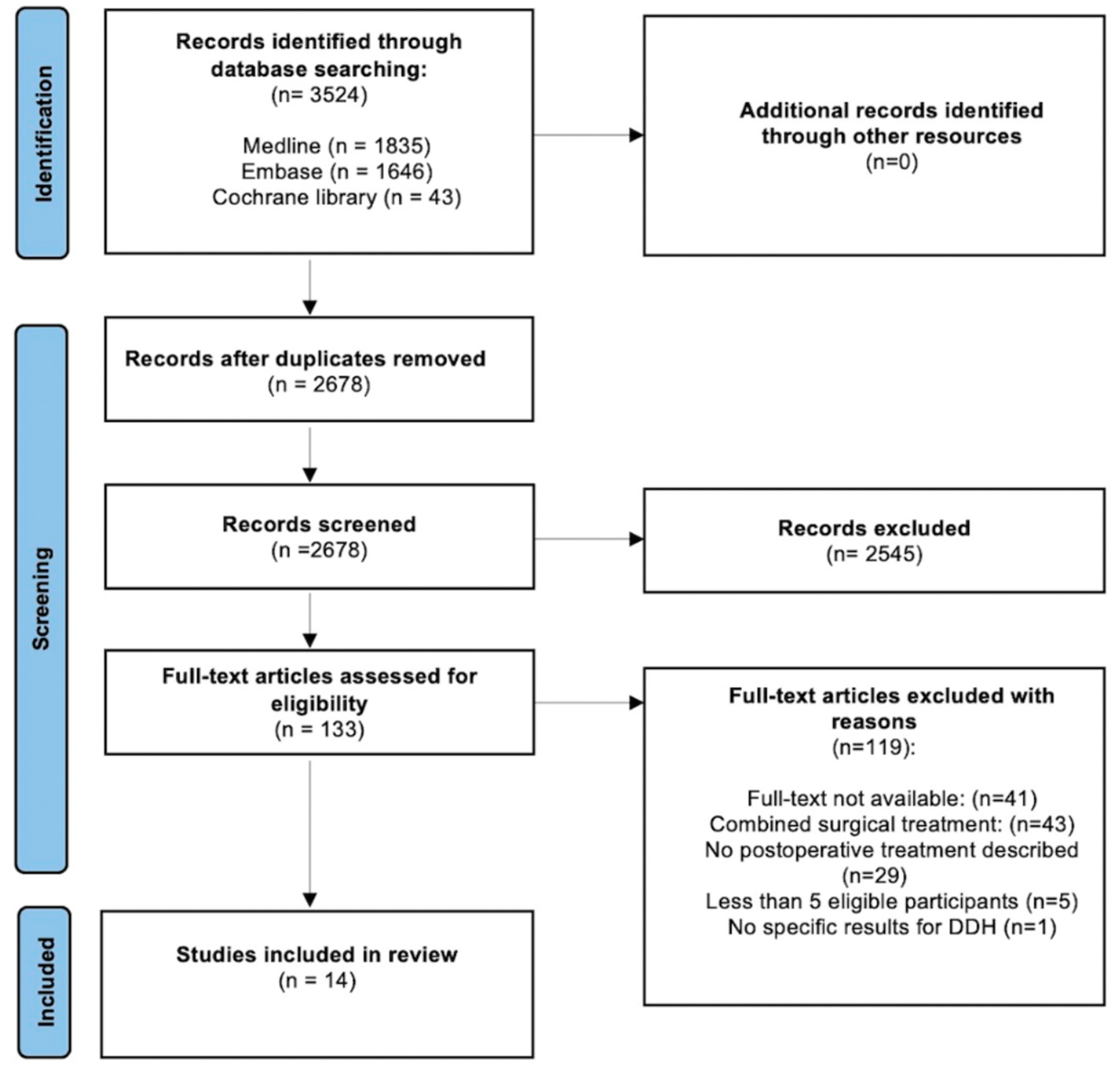
The search strategy yielded a total of 3524 articles (Figure 1). There were 1835 PubMed hits, 1646 Embase hits and 43 Cochrane hits. After the removal of 846 duplicates, a total of 2678 articles were screened based on the title and abstract, of which 133 were found to be eligible for full-text screening. After full-text evaluation, 14 articles were included in our review [23,24,25,26,27,28,29,30,31,32,33,34,35,36], including 3 articles that were added based on additional data/information obtained through contact by mail with several authors [27,35,36].
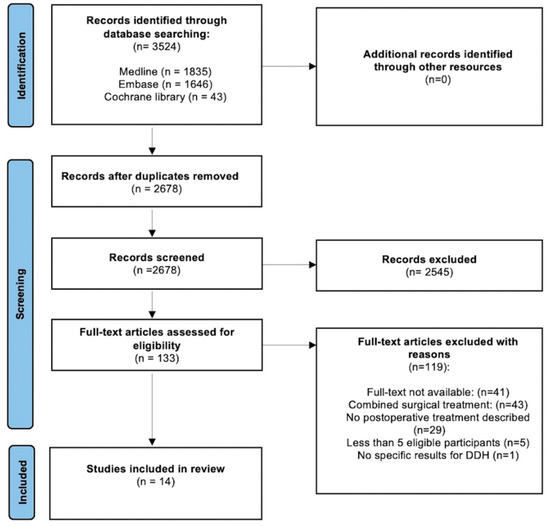
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) flowchart: the study selection process.
3.2. Study Characteristics and Methodological Quality
Table 1 shows the baseline characteristics of the 14 included studies [23,24,25,26,27,28,29,30,31,32,33,34,35,36]. Eleven of the studies included were retrospective [24,25,26,27,30,31,32,33,34,35,36], of which five were comparative [26,31,34,35,36] and six were case series [24,25,27,30,32,33]. Three studies were prospective [23,28,29], of which two studies were comparative [23,28] and one study was a case series [29]. A total of 367 hips in 312 children were included. One study included children who had consecutive bilateral hip osteotomy [26]. The number of hips included per study ranged between 5 and 110. The quality of evidence in the included studies was moderate, with a MINORS score ranging from 3 (out of 16) to 12 (out of 24) points (see Table 1).

Table 1.
Baseline characteristics of the included studies.
3.3. Surgical Treatment
The Salter osteotomy [37] (including the less invasive, Kalamchi and angulated variants) was used in eight studies (236 hips) [23,26,27,28,29,33,34,35,36]. Three studies (35 hips) described the results after a (modified) Dega osteotomy [24,30,36] and five studies (96 hips) described the results after a Pemberton osteotomy [32,33,34,36].
3.4. Postoperative treatment
A hip spica cast was used in 13 studies (312 hips) [23,24,26,27,28,29,30,31,32,33,34,35,36]. Three studies (111 hips) [29,34,35] reported the type of spica cast that was used: all were ‘one and a half’ leg spica casts that were used for a duration of 5 or 6 weeks. The study of Wada et al. [35] (61 hips) applied abduction and flexion of 10°–20° after (angulated) Salter osteotomy, while Shin et al. [36] (12 hips) applied hip abduction and flexion of 25°–70° after Salter osteotomy and 30° hip abduction and 30° flexion after Dega osteotomy. An abduction brace was used in 49 hips [25], and avoidance of full weightbearing was used in 6 hips [27].
3.5. Clinical Outcomes
The clinical methods of evaluation that were used were McKay’s criteria [26,31,33] and the Trevor clinical score [26] (see Table 2). A total of 123 hips that underwent hip spica casting (after either Salter, Pemberton or Dega osteotomy) had an excellent McKay’s score [26,31,33]. Regarding the Trevor clinical score, 106 hips were excellent after either Salter or Pemberton osteotomy and spica casting [26]. Clinical scores were not evaluated in the patients treated with an abduction brace or avoidance of weightbearing. Only Chuckwunyerenwa et al. [23] mentioned the satisfaction regarding postoperative management: all 49 parents and children were highly satisfied with the abduction brace.

Table 2.
Outcomes by postoperative treatment.
The mean duration of hospitalization after the use of hip spica casts was 11.6 days in the study of Ezirmik et al. [26] and 7 days in the study of Hedelin et al. [27] (see Table 1).
3.6. Complications
With respect to the 312 hips treated with a spica cast, pain was reported in 34 hips (10.9%) [34], avascular necrosis (AVN) occurred in 49 hips (15.7%) [26,27,34], and 3 hips suffered superficial infections (1%) [26] (see Table 2). Two hips (4.1%) suffered superficial infections [25] after the use of abduction braces, and no AVN or pain complaints were observed in this group (see Table 2). In the avoidance of weightbearing group, none of the aforementioned complications occurred (see Table 2).
3.7. Radiological Results
The Severin score was reported in five studies after the use of a hip spica cast [26,31,32,33,36]. A total of 109 hips (76.8%) were graded as Severin score I (see Table 2).
Four studies [24,25,27,30] presented the radiological results preoperatively, directly postoperatively and at the final postoperative follow-up, which is interesting for assessing the maintenance of acetabular correction (see Table 3). None of the studies reported deterioration of the radiological outcomes during follow-up (see Table 3).

Table 3.
Radiological maintenance of acetabular correction.
4. Discussion
To the best of our knowledge, this is the first systematic review of the effectiveness of postoperative spica casts after a unilateral pelvic osteotomy in children with DDH. With the present review, we have evaluated the clinical and radiological outcomes of all of the available literature about this subject. We included 367 hips in the review, of which 312 were treated with a spica cast, 49 with an abduction brace and 6 with avoidance of weightbearing. The quality of the included studies was moderate. The data show that a hip spica cast, abduction brace and avoidance of weightbearing can all be safe and satisfactory methods of postoperative management according to the clinical results, complication data and radiological findings. No graft displacements occurred, and the consolidation of the pelvic osteotomies was overall preserved. Avascular necrosis was only seen with the use of spica casting. These outcomes question the added value of spica casting in the postoperative management of simple pelvic osteotomies for DDH at walking age.
In general, only a few complications were reported, which mostly occurred after the use of a spica cast, irrespective of the position of the cast of the prior pelvic osteotomy technique. This is in line with the literature [6,15], since it is known that immobilization with spica casts may lead to several complications. Most of these complications were related to the procedure, such as pain and AVN. The complications were independent of the duration of spica cast application (generally 6 weeks) and the surgical treatment used. In the population treated with an abduction brace, there were two superficial infections. Despite these two complications, all parents and children were satisfied with the use of the plastic abduction brace. Pisecky et al. [6,15] and Gather et al. [38] suggested that abduction foam braces may be more suitable alternatives for spica casting to prevent complications in children with DDH. However, in the current review, no studies that used a foam splint as a postoperative treatment were included.
Another important outcome measure was the radiological outcome. Since the improvement of the AI and CEA is mostly caused by the pelvic osteotomy performed, it is important to consider the maintenance of the AI and CEA postoperatively up to the final postoperative treatment to determine the radiological effect of postoperative treatment, since a dislocation of the graft could result in the deterioration of the AI and CEA. The maintenance of acetabular correction after pelvic osteotomy in children with DDH is essential for the stability of the hip. Consequently, even if the use of alternative postoperative management may result in more convenience compared to the use of a hip spica cast, it may not be of added value in the case of a lost acetabular correction.
Nevertheless, the AI and CEA correction were overall well maintained after any postoperative method. In the current review, avoidance of weightbearing (for 6 weeks) resulted in no complications, and maintenance of the radiological outcomes was comparable to hip spica casts. Therefore, the avoidance of weightbearing may be as safe as the use of hip spica casting. However, only six children were included in this study, and it may be challenging for young children to remain non-weightbearing. In addition to the postoperative methods reviewed, Miller et al. [39] suggested initial non-weightbearing of a maximum of four days, followed by physical therapy, with promising outcomes.
A strength of this review is the comprehensive systematic search method to find all relevant studies on this subject. Most of the postoperative treatment modalities had a similar mean duration of approximately six weeks. Also, only children with DDH who underwent unilateral pelvic osteotomy without concomitant procedures were included. The authors have used the numbers and results of all of the children with DDH from the available articles to demonstrate an overview of the results of different postoperative methods in children with DDH.
The review also has limitations. The relatively low number of 367 included hips is a clear limitation. It must be mentioned that the minority of included studies used alternative postoperative treatments. Also, the immediate postoperative AI and the follow-up AI were not available for all studies, which are important for comparing the maintenance of the surgical correction. Consequently, the authors only presented the maintenance of AI and CEA correction for four studies. Moreover, insufficient information was found for differentiating between types of casts and durations of immobilization. Furthermore, we applied strict inclusion and exclusion criteria, which led us to the exclusion of a relatively large number of studies. In addition, no meta-analysis could be performed because of the heterogeneity of the data. Higher-quality research is needed to determine the optimal postoperative treatment protocol.
5. Conclusions
In conclusion, this systematic review shows no advantage of hip spica casting postoperatively compared to abduction braces and avoidance of weightbearing. However, the number of hips included that used the alternative types of postoperative management is relatively few in this review.
Author Contributions
Conceptualization, M.M., R.A.v.S., S.M. and C.J.A.v.B.; methodology, M.M.; validation, C.J.A.v.B., R.A.v.S. and S.M.; formal analysis, M.M.; investigation, M.M. and R.A.v.S.; resources, M.M.; data curation, M.M. and R.A.v.S.; writing—original draft preparation, M.M.; writing—review and editing, C.J.A.v.B., R.A.v.S. and S.M.; visualization, M.M.; supervision, C.J.A.v.B.; project administration, M.M. and C.J.A.v.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
Appendix A

Table A1.
Search strategy.
Table A1.
Search strategy.
| Pubmed: | |
| #1 | ((Osteotomy[Mesh:NoExp] OR osteom*[tiab] AND (hip[tiab] OR pelvi*[tiab] OR acetabul*[tiab])) OR “Acetabuloplasty”[Mesh] OR Acetabuloplast*[tiab] OR “acetabulum plasty”[tiab] OR Salter[tiab] OR Pemberton[tiab] OR Dega[tiab] OR “hip reconstruction*”[tiab] NOT arthroplast*[tiab] |
| #2 | “Developmental Dysplasia of the Hip”[Mesh] OR “Hip Dislocation, Congenital”[Mesh] OR DDH[tiab] OR ((hip[tiab]) AND (dislocat*[tiab] OR luxation[tiab] OR dysplasia[tiab] OR displacement[tiab] AND (congenital[tiab] OR development[tiab])) |
| Embase: | |
| #1 | ‘Pelvis osteotomy’/de OR ((osteotom*:ti,ab,kw) AND (hip:ti,ab,kw OR pelvi*:ti,ab,kw OR acetabul*:ti,ab,kw)) OR ‘acetabuloplasty’/exp OR acetabuloplast*:ti,ab,kw OR ‘acetabulum plasty’:ti,ab,kw OR Salter:ti,ab,kw OR Pemberton:ti,ab,kw, OR Dega:ti,ab,kw OR ‘hip reconstruction’:ti,ab,kw NOT arthroplast*”ti,ab,kw |
| #2 | ‘Hip dysplasia’/exp OR ‘congenital hip dislocation’/exp OR ddh:ti,ab,kw OR ((hip:ti,ab,kw) AND (dislocat*:ti,ab,kw OR luxation:ti,ab,kw OR dysplasia:ti,ab,kw OR displacement:ti,ab,kw) AND (congenital:ti,ab,kw OR developmental:ti,ab,kw)) |
| #3 | NOT ‘conference abstract’/it |
| Cochrane: | |
| #1 | ((Osteotom*:ti,ab,kw) AND (hip:ti,ab,kw OR pelvi*:ti,ab,kw OR acetabul*:ti,ab,kw)) OR acetabuloplast*:ti,ab,kw OR “acetabulum plasty”:ti,ab,kw OR Salter:ti,ab,kw OR Pemberton:ti,ab,kw OR Dega:ti,ab,kw OR “hip reconstruction”:ti,ab,kw NOT artrhoplast*:ti,ab,kw |
| #2 | DDH:ti,ab,kw OR ((hip:ti,ab,kw) AND (dislocat*:ti,ab,kw OR luxation:ti,ab,kw OR dysplasia:ti,ab,kw OR displacement:ti,ab,kw) AND (congenital:ti,ab,kw OR developmental:ti,ab,kw)) |
* (asterisk) = truncation symbol to search for multiple variants of a word at once in databases.
References
- de Witte, P.B.; van Bergen, C.J.; de Geest, B.L.; Willeboordse, F.; van Linge, J.H.; den Hartog, Y.M.; Foreman-van Drongelen, M.; Pereboom, R.M.; Robben, S.G.F.; Burger, B.J.; et al. Treatment of decentered developmental dysplasia of the hip under the age of 1 year: An evidence-based clinical practice guideline—Part 2. EFORT Open Rev. 2022, 7, 542–553. [Google Scholar] [CrossRef] [PubMed]
- Kotlarsky, P.; Haber, R.; Bialik, V.; Eidelman, M. Developmental dysplasia of the hip: What has changed in the last 20 years? World J. Orthop. 2015, 6, 886–901. [Google Scholar] [CrossRef] [PubMed]
- Hauk, L. Developmental Dysplasia of the Hip in Infants: A Clinical Report from the AAP on Evaluation and Referral. Am. Fam. Physician 2017, 96, 196–197. [Google Scholar] [PubMed]
- van Bergen, C.J.; de Witte, P.B.; Willeboordse, F.; de Geest, B.L.; Foreman-van Drongelen, M.; Burger, B.J.; den Hartog, Y.M.; van Linge, J.H.; Pereboom, R.M.; Robben, S.G.F.; et al. Treatment of centered developmental dysplasia of the hip under the age of 1 year: An evidence-based clinical practice guideline—Part 1. EFORT Open Rev. 2022, 7, 498–505. [Google Scholar] [CrossRef] [PubMed]
- Fillingham, Y.A.; Erickson, B.J.; Hellman, M.D.; Cvetanovich, G.; Kogan, M. Surgical Technique: Pavlik Harness and Closed Reduction for Developmental Dysplasia of the Hip. In Hip Arthroscopy and Hip Joint Preservation Surgery; Nho, S., Leunig, M., Larson, C., Bedi, A., Kelly, B., Eds.; Springer: New York, NY, USA, 2014; pp. 415–428. [Google Scholar]
- Pisecky, L.; Großbötzl, G.; Gahleitner, M.; Haas, C.; Gotterbarm, T.; Klotz, M.C. Results after Spica cast immobilization following hip reconstruction in 95 cases: Is there a need for alternative techniques? Arch. Orthop. Trauma Surg. 2021, 142, 969–977. [Google Scholar] [CrossRef] [PubMed]
- Schams, M.; Labruyère, R.; Zuse, A.; Walensi, M. Diagnosing developmental dysplasia of the hip using the Graf ultrasound method: Risk and protective factor analysis in 11,820 universally screened newborns. Eur. J. Pediatr. 2017, 176, 1193–1200. [Google Scholar] [CrossRef]
- Ionescu, A.; Dragomirescu, M.-C.; Herdea, A.; Ulici, A. Developmental Dysplasia of the Hip: How Many Risk Factors Are Needed? Children 2023, 10, 968. [Google Scholar] [CrossRef]
- Zhang, S.; Doudoulakis, K.J.; Khurwal, A.; Sarraf, K.M. Developmental dysplasia of the hip. Br. J. Hosp. Med. 2020, 81, 1–8. [Google Scholar] [CrossRef]
- Vaquero-Picado, A.; González-Morán, G.; Gil Garay, E.; Moraleda, L. Developmental dysplasia of the hip: Update of management. EFORT Open Rev. 2019, 4, 548–556. [Google Scholar] [CrossRef]
- Alassaf, N. Treatment of developmental dysplasia of the hip (DDH) between the age of 18 and 24 months. Eur. J. Orthop. Surg. Traumatol. 2019, 30, 637–641. [Google Scholar] [CrossRef]
- Venkatadass, K.; Prasad, V.D.; Al Ahmadi, N.M.M.; Rajasekaran, S. Pelvic osteotomies in hip dysplasia: Why, when and how? EFORT Open Rev. 2022, 7, 153–163. [Google Scholar] [CrossRef]
- Abdullah, E.-S.A.H.; Razzak, M.Y.A.; Hussein, H.T.K.; El-Adwar, K.L.; Abdel-Razek Youssef, A. Evaluation of the results of operative treatment of hip dysplasia in children after the walking age. Alex. J. Med. 2012, 48, 115–122. [Google Scholar] [CrossRef]
- Feeley, I.H.; Green, C.J.; Rowan, F.E.; Moore, D.P. International variance in the treatment of developmental dysplasia of the hip. J. Child. Orthop. 2014, 8, 381–386. [Google Scholar] [CrossRef]
- Pisecky, L.; Großbötzl, G.; Gahleitner, M.; Stadler, C.; Stevoska, S.; Haas, C.; Gotterbarm, T.; Klotz, M.C.M. Foam Splint versus Spica Cast—Early Mobilization after Hip Reconstructive Surgery in Children—Preliminary Data from a Prospective Randomized Clinical Trial. Children 2022, 9, 288. [Google Scholar] [CrossRef]
- Sideri, S.; Papageorgiou, S.N.; Eliades, T. Registration in the international prospective register of systematic reviews (PROSPERO) of systematic review protocols was associated with increased review quality. J. Clin. Epidemiol. 2018, 100, 103–110. [Google Scholar] [CrossRef] [PubMed]
- Prill, R.; Karlsson, J.; Ayeni, O.R.; Becker, R. Author guidelines for conducting systematic reviews and meta-analyses. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 2739–2744. [Google Scholar] [CrossRef] [PubMed]
- Johnson, N.; Phillips, M. Rayyan for systematic reviews. J. Electron. Resour. Libr. 2018, 30, 46–48. [Google Scholar] [CrossRef]
- Reiswig, J. Mendeley. J. Med. Libr. Assoc. 2010, 98, 193–194. [Google Scholar] [CrossRef]
- Zeng, X.; Zhang, Y.; Kwong, J.S.; Zhang, C.; Li, S.; Sun, F.; Niu, Y.; Du, L. The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: A systematic review. J. Evid. Based Med. 2015, 8, 2–10. [Google Scholar] [CrossRef]
- Mckay, D. A Comparison of the Innominate and the Pericapsular Osteotomy in the Treatment of Congenital Dislocation of the Hip. Clin. Orthop. Relat. Res. 1974, 98, 124–132. [Google Scholar] [CrossRef]
- Trevor, D.; Johns, D.; Fixsen, J. Acetabuloplasty in the treatment of congenital dislocation of the hip. J. Bone Jt. Surg. Br. 1975, 57, 167–174. [Google Scholar] [CrossRef]
- Akman, B.; Ozkan, K.; Cift, H.; Akan, K.; Eceviz, E.; Eren, A. Treatment of Tönnis type II hip dysplasia with or without open reduction in children older than 18 months: A preliminary report. J. Child. Orthop. 2009, 3, 307–311. [Google Scholar] [CrossRef] [PubMed]
- Aksoy, C.; Yilgor, C.; Demirkiran, G.; Caglar, O. Evaluation of a 308 cetabular development after Dega acetabuloplasty in developmental dysplasia of the hip. J. Pediatr. Orthop. 2013, 22, 91–95. [Google Scholar] [CrossRef]
- Chukwunyerenwa, C.K.; Sehgal, R.; Vioreanu, M.; Doyle, F.; Molony, D.; McCormack, D. Less invasive innominate osteotomy. J. Pediatr. Orthop. 2010, 19, 318–322. [Google Scholar] [CrossRef]
- Ezirmik, N.; Yildiz, K. Advantages of single-stage surgical treatment with Salter innominate osteotomy and Pemberton Pericapsular osteotomy for developmental dysplasia of both hips. J. Int. Med. Res. 2012, 40, 748–755. [Google Scholar] [CrossRef] [PubMed]
- Hedelin, H.; Larnert, P.; Hebelka, H.; Brisby, H.; Lagerstrand, K.; Laine, T. Innominate Salter osteotomy using resorbable screws: A retrospective case series and presentation of a new concept for fixation. J. Child. Orthop. 2019, 13, 310–317. [Google Scholar] [CrossRef] [PubMed]
- Kamegaya, M.; Shinohara, Y.; Shinada, Y.; Moriya, H.; Koizumi, W.; Tsuchiya, K. The use of a hydroxyapatite block for innominate osteotomy. J. Bone Jt. Surg. Br. 1994, 76, 123–126. [Google Scholar] [CrossRef]
- Nakamura, Y.; Kimura, M.; Ohishi, H.; Kishiya, M.; Toh, S. Salter innominate osteotomy using T-saw for developmental dysplasia of the hip. Curr. Orthop. Pract. 2011, 22, 447–450. [Google Scholar] [CrossRef]
- Rampal, V.; Klein, C.; Arellano, E.; Boubakeur, Y.; Seringe, R.; Glorion, C.; Wicart, P. Outcomes of modified Dega acetabuloplasty in acetabular dysplasia related to developmental dislocation of the hip. Orthop. Traumatol. Surg. Res. 2014, 100, 207–211. [Google Scholar] [CrossRef]
- Synder, M.; Forlin, E.; Xin, S.; Bowen, J.R. Results of the KALAMCHI modification of Salter osteotomy in the treatment of developmental dysplasia of the hip. J. Pediatr. Orthop. 1992, 12, 449–453. [Google Scholar] [CrossRef]
- Vedantam, R.; Capelli, A.M.; Schoenecker, P.L. Pemberton osteotomy for the treatment of developmental dysplasia of the hip in older children. J. Pediatr. Orthop. 1998, 18, 254–258. [Google Scholar] [CrossRef]
- Wada, A.; Fujii, T.; Takamura, K.; Yanagida, H.; Taketa, M.; Nakamura, T. Pemberton osteotomy for developmental dysplasia of the hip in older children. J. Pediatr. Orthop. 2003, 23, 508–513. [Google Scholar] [CrossRef]
- Wang, C.-W.; Wu, K.-W.; Wang, T.-M.; Huang, S.-C.; Kuo, K.N. Comparison of 333 acetabular anterior coverage after Salter osteotomy and Pemberton acetabuloplasty: A long-term followup. Clin. Orthop. Relat. Res. 2014, 472, 1001–1009. [Google Scholar] [CrossRef][Green Version]
- Wada, A.; Sakalouski, A.; Nakamura, T.; Kubota, H.; Matsuo, A.; Taketa, M.; Nakura, A.; Lee, Y. Angulated Salter osteotomy in the treatment of developmental dysplasia of the hip. J. Pediatr. Orthop. 2021, 31, 254–259. [Google Scholar] [CrossRef]
- Shin, C.H.; Yoo, W.J.; Park, M.S.; Kim, J.H.; Choi, I.H.; Cho, T.-J. Acetabular Remodeling and Role of Osteotomy After Closed Reduction of Developmental Dysplasia of the Hip. J. Bone Jt. Surg. 2016, 98, 952–957. [Google Scholar] [CrossRef]
- Salter, R. Innominate osteotomy in the treatment of congenital dislocation and subluxation of the hip. J. Bone Jt. Surg. Br. 1961, 43, 518–539. [Google Scholar] [CrossRef]
- Gather, K.S.; von Stillfried, E.; Hagmann, S.; Müller, S.; Dreher, T. Outcome after early mobilization following hip reconstruction in children with developmental hip dysplasia and luxation. World J. Pediatr. 2018, 14, 176–183. [Google Scholar] [CrossRef]
- Miller, F.; Girardi, H.; Lipton, G.; Ponzio, R.; Klaumann, M.; Dabney, K.W. Reconstruction of the Dysplastic Spastic Hip with Peri-ilial Pelvic and Femoral Osteotomy Followed by Immediate Mobilization. J. Pediatr. Orthop. 1997, 17, 592–602. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).