Abstract
Background: There is uncertainty regarding the impact of multidrug-resistant organisms on patients that undergo cardiac surgery. Methods: A retrospective cohort study was performed by using 2016–2019 data from the National Inpatient Sample in the United States to evaluate the proportion of admissions with a diagnosis of antimicrobial resistance who also underwent coronary artery bypass graft or valve surgery. Results: A total of 1,260,630 admissions were included in the analysis, of which 2045 (0.16%) had antimicrobial resistance. Compared to patients without resistance, those with antimicrobial resistance were more likely to be female (52.8% vs. 31.5%, p < 0.001), and die in a hospital (7.1% vs. 2.4%, p < 0.001). The length of stay and cost were significantly higher for patients with antimicrobial resistance (15 vs. 7 days and USD 69,135 vs. USD 43,740, respectively). Antimicrobial resistance was not associated with increased in-hospital mortality (OR 1.38; 95% CI 0.86–2.21, p = 0.18), although it was associated with an increase in length of stay (coefficient 7.65; 95% CI 6.91–8.39, p < 0.001), and cost (coefficient USD 25,240 [21,626–28,854], p < 0.001). Conclusions: Antimicrobial resistance in patients that undergo cardiac surgery is not common, yet its burden is substantial as it can double the length of stay and increase costs by more than USD 20,000.
1. Introduction
It is estimated that 4000 cardiothoracic surgeons perform more than 530,000 cardiothoracic cases each year [1]. Coronary artery bypass graft (CABG) is the most common cardiothoracic surgical procedure in the United States and costs USD 6.5 billion in healthcare bills annually [2]. Infections are unfortunately common following cardiac surgery and have been reported to affect between 4% and 21% of operations [3,4] and are associated with prolonged length of hospitalization, cost, and mortality [3,4,5].
The importance of antibiotic therapy in reducing postoperative infections, mortality, and costs has been suggested in a guideline [6], a systematic review [7], and clinical studies [8,9]. Prophylactic antibiotics are important as infection risk increases with chronic lung disease, heart failure, longer surgery, stress hyperglycemia, intubation times of 24 to 48 h, and ventilation > 48 h [10]. The Society of Thoracic Surgeons Practice Guideline recommended β-lactam antibiotic as the antibiotic of choice for prophylaxis in cardiac surgeries, especially if a high incidence of methicillin-resistant Staphylococcus aureus is not expected [6].
Antimicrobial resistance, defined as the situation, where bacteria, viruses, fungi, and parasites change over time and no longer respond to medicines, is a global concern as it threatens the ability of clinicians to treat infections [11]. In 2019, it was estimated that there were nearly 5 million deaths associated with bacterial antimicrobial resistance, including over 1 million deaths attributed to antimicrobial resistance [12]. In 2014, the estimated national cost of multidrug-resistant organisms on inpatient hospitalizations in the United States was estimated to be at least USD 2.4 billion [13] and the cost of antimicrobial resistance in Canada in 2018 was USD 1.4 billion [14]. As a result, the World Health Organization declared that antimicrobial resistance is one of the top 10 global public health threats facing humanity [11].
A recent review highlights the growing threat of multidrug resistance for invasive cardiac procedures and suggests that the concept is underappreciated and is expected to rise due to the overuse of antibiotics [15]. Furthermore, it claims that this problem is not hypothetical but present and that patients with multidrug-resistant infections have higher mortality than those infected with non-multidrug-resistant bacteria [15]. As it is estimated that multidrug-resistant organisms cause infectious complications in between 0.6% and 10% of patients who undergo a variety of cardiac surgeries [15], we analyzed nationally representative data from the United States to estimate the prevalence of antimicrobial resistance in patients receiving CABG and valve surgery and evaluate its impact on in-hospital mortality, length of stay, and cost.
2. Materials and Methods
We analyzed nationally representative data of the United States from the National Inpatient Sample (NIS). The NIS is a database created by the Healthcare Cost and Utilization Project (HCUP), which is the largest publicly available all-payer inpatient healthcare database in the United States that can be utilized to provide national estimates of inpatient utilization, access, costs, quality, and outcomes [16]. The reporting of this manuscript is in accordance with the recommendations of the STROBE statement [17].
We identified all patients with an admission to hospital and an International Statistical Classification of Diseases, Tenth Revision (ICD-10) procedure code corresponding to CABG or valve surgery between 2016 and 2019. The codes for CABG and valve surgery were based on those reported by the Mubashir et al. study [18].
This cohort of cardiac surgery patients was stratified by the primary exposure of interest, which was antimicrobial resistance as defined by the ICD-10 diagnostic code Z16. We excluded patients with ages < 18 years, missing values for age, gender, and mortality.
The additional data retrieved from the NIS dataset is outlined in Table A1. In brief, the discharge diagnosis codes, which were up to 40, and procedural codes, up to 25, were used to define admission diagnoses of coexisting illnesses (hypertension, hyperlipidemia, obesity, diabetes mellitus, previous myocardial infarction, heart failure, atrial fibrillation, previous stroke, peripheral vascular disease, chronic kidney disease, liver failure, chronic lung disease, cancer, and dementia). Additional demographic (age, sex, race, nicotine dependence, and alcohol misuse), hospital information (rural hospital, teaching hospital, hospital region, elective admission, the season of admission, weekend admission, primary expected payer, patient income based on ZIP code, and hospital bed size) and outcome data (length of stay and cost) were available in the NIS dataset. The season of admission was defined as March to May for spring, June to August for Summer, September to November for fall, and December to February for winter. Additional data were collected on the use of central venous lines and the presence of infection or sepsis. The primary outcome of the study was in-hospital mortality. The secondary outcomes were the length of stay and inpatient cost. The cost was defined by the total charge multiplied by the charge-to-cost ratio.
Statistical Analysis
Statistical analysis was performed on Stata 13 (College Station, TX, USA). The hospital admissions were weighted by the discharge weight to obtain nationally representative estimates, as per the recommendations of HCUP [16]. We stratified the cohort by antimicrobial resistance, and descriptive statistics were presented with median and interquartile ranges (IQRs) for continuous variables, and as the percentage for categorical variables. The median test was used to assess for statistical differences for continuous variables and the Chi2 test for categorical variables for the presence or absence of antimicrobial resistance. A multiple logistic regression model with adjustments for demographic, hospital, comorbidity, and the presence of central line, infection, and sepsis was used to identify predictors of antimicrobial resistance. Additional sequentially adjusted logistic regression models were generated to determine the odds of in-hospital mortality with antimicrobial resistance and similar linear regression models were used to explore the impact of antimicrobial resistance on length of stay and inpatient cost. The adjustments were first unadjusted, then, adjusted for demographics (model 1), then, adjusted for demographics and hospital variables (model 2), and finally, adjusted for demographics, hospital, and comorbidity variables (model 3). A p-value of 0.05 was considered to be statistically significant. Sensitivity analyses were performed, where analyses were performed for the subgroup of patients with and without central line, sepsis, and infection, and for those receiving CABG surgery and valve surgery.
3. Results
The flow diagram of hospital admissions with CABG or valve surgery is shown in Figure 1. A total of 1,260,630 admissions were included in the analysis, of which 2045 (0.16%) had antimicrobial resistance.
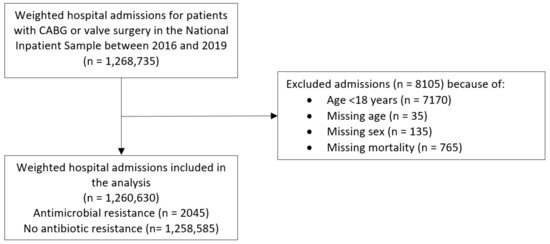
Figure 1.
Flow diagram of hospital admissions included in the analysis.
The characteristics of the patients that underwent a coronary artery bypass and/or valve procedure stratified by the presence of antimicrobial resistance are shown in Table 1. Patients with antimicrobial resistance were proportionately more likely to be female (52.8% vs. 31.5%, p < 0.001) and either African American (7.8% vs. 6.7%) or Hispanic (13.7% vs. 7.3%) (p < 0.001). These patients were also more frequently admitted on weekends (17.4% vs. 9.1%, p < 0.001) and less likely to be admitted as elective procedures (34.4% vs. 58.5%, p < 0.001). The primary expected payer for patients with antimicrobial resistance was more likely to have Medicaid (13.9% vs. 7.0%) or be self-paying (2.9% vs. 2.3%) and less likely to have Medicare (58.7% vs. 61.3%) or private insurance (21.5% vs. 26.6%) (p < 0.001). In terms of comorbidities, patients with antimicrobial resistance were in the greater proportion likely to have heart failure (54.8% vs. 40.4%, p < 0.001), atrial fibrillation (48.9% vs. 39.3%, p < 0.001), chronic kidney disease (37.2% vs. 22.8%, p < 0.001), and liver failure (7.1% vs. 1.6%, p < 0.001), although they were less likely to have hypertension (81.2% vs. 85.6%, p = 0.011) and hypercholesterolemia (59.4% vs. 72.8%, p < 0.001). The proportion of patients with CABG only, the valve only, and both procedures were 44.7%, 45.0%, and 10.3%, respectively, for patients with antimicrobial resistance, compared to 56.0%, 36.1%, and 7.9%, respectively, for patients without antimicrobial resistance. Insertion of a central venous line was more common in patients with antimicrobial resistance (28.4% vs. 9.1%, p < 0.001), while both sepsis (20.8% vs. 2.8%, p < 0.001) and infection (88.8% vs. 23.1%, p < 0.001) were more common in patients with antimicrobial resistance. In-hospital mortality occurred in 7.1% of patients with antimicrobial resistance and 2.4% of patients without antimicrobial resistance (p < 0.001). The length of stay and cost were significantly higher for patients with antimicrobial resistance (15 vs. 7 days and USD 69,135 vs. USD 43,740, respectively).

Table 1.
Characteristics of patients that underwent a coronary artery bypass graft and/or valve surgery stratified by the presence of antimicrobial resistance.
The predictors of antimicrobial resistance among patients who underwent CABG and/or valve surgery are shown in Table 2. Infection was the strongest predictor of antimicrobial resistance (OR 18.33; 95% CI 13.24–25.37, p < 0.001). Other factors associated with antimicrobial resistance were female sex (OR 2.13; 95% CI 1.72–2.62, p < 0.001), alcohol misuse (OR 1.97; 95% CI 1.07–3.63, p = 0.31), central line insertion (OR 1.56; 95% CI 1.22–1.98, p < 0.001), and sepsis (OR 1.50; 95% CI 1.13–2.00, p = 0.005). Elective admission was associated with a reduction in antimicrobial resistance (OR 0.70; 95% CI 0.55–0.88, p = 0.003).

Table 2.
Predictors of antimicrobial resistance among patients that underwent a coronary artery bypass graft or valve surgery.
The unadjusted and adjusted impacts of antimicrobial resistance on in-hospital mortality, length of stay, and cost are shown in Table 3. After adjustments for comorbidities, there was no significant increase in in-hospital mortality with antimicrobial resistance (OR 1.38; 95% CI 0.86–2.21, p = 0.18). Antimicrobial resistance was associated with an increase in length of stay (coefficient 7.65; 95% CI 6.91–8.39, p < 0.001), and cost (coefficient: USD 25,240 [21,626–28,854], p < 0.001).

Table 3.
Logistic regression and linear regression to evaluate the unadjusted and adjusted impact of antimicrobial resistance on in-hospital mortality, length of stay, and cost on patients that underwent a coronary artery bypass graft or valve surgery.
The sensitivity analysis considering the impact of infection, sepsis, central line insertion, and type of surgery is shown in Table 4. The presence of infection did not significantly increase in-hospital mortality (p = 0.38), although it increased the length of stay (p < 0.001) and cost (p = 0.009). Sepsis had no significant effect on in-hospital mortality (p = 0.18), length of stay (p = 0.30), and cost (p = 0.38). The insertion of a central line did not significantly affect in-hospital mortality (p = 0.65), although it did increase the length of stay (p = 0.001) and cost (p < 0.001). For both CABG and valve surgery, there was no difference in in-hospital mortality with antimicrobial resistance (p = 0.52 and p = 0.13, respectively), yet there was an increase in the length of stay (p < 0.001), and cost (p < 0.001).

Table 4.
Logistic regression and linear regression to evaluate the adjusted impact of antimicrobial resistance on in-hospital mortality, length of stay, and cost in subgroups of patients.
4. Discussion
4.1. Key Findings
Our evaluation has several key findings. From a national perspective using discharge summary codes, rates of antimicrobial resistance in cardiac surgery are low: at less than 1%. Compared to patients who do not have antimicrobial resistance as a diagnosis, those with antimicrobial resistance have greater mortality, length of stay, and cost, although once adjustments were made there was no significant increase in in-hospital mortality for patients with antimicrobial resistance. Nevertheless, the increase in length of stay and cost among patients with antimicrobial resistance was substantial, whereby they were more than double and more than USD 20,000, respectively. The rate of antimicrobial resistance increased in 2019 compared to other years. A major predictor of antimicrobial resistance was an infection, although other factors associated with it included female gender, alcohol misuse, central line insertion, sepsis, chronic kidney disease, and atrial fibrillation. Our study highlights antimicrobial resistance on a national level and shows that it carries a high burden in terms of increased length of stay and cost for admissions with cardiac surgery.
4.2. Key Considerations Regarding the Findings
A major consideration of the current study is that we do not know the definition of antimicrobial resistance used at each hospital, which justified the diagnosis and how testing for antimicrobial resistance was performed. The definition used by the World Health Organization, encompasses antibiotic resistance, antiviral resistance, and antifungal resistance [19]. Furthermore, the degree of resistance is not specified and there may be a difference between a microbe that is resistant to a single agent compared to one that is multidrug-resistant, which could both be classified as antimicrobial resistance. This may be important as a prospective study of 138 patients who underwent cardiac surgery found that multidrug-resistant bacterial isolates were widespread and there are increasingly emerging strains of extended-spectrum beta-lactamases-producing Gram-negative bacteria Klebsiella pneumoniae, Pseudomonas aeruginosa, and Escherichia coli, especially, among patients with prolonged admission to intensive care units [20]. The studies of multidrug resistance have been evaluated in other types of patient cohorts [21,22,23]. In a study of patients with in-hospital cardiac arrest and nosocomial infection, 10 out of 35 patients (28%) had multidrug-resistant pathogens [21]. In another study, 31% of 82 patients with a bacterial infection within 1 year of a heart transplant had multidrug-resistant pathogens [22]. A further evaluation of 147 patients with heart transplants and infections with 259 pathogens found that there were 64 multidrug-resistant bacteria [23]. The low rates of antimicrobial resistance in the current study may be explained by some degree of underreporting of the diagnosis. The underreporting of antibiotic resistance has been highlighted in a previous study and it was suggested that medical records are notoriously unclear with respect to distinguishing between a number of clinical diagnoses, particularly nosocomial infections [24]. The extent of the underreporting and the reason for underreporting are not clear, and this study does not have the laboratory culture sensitivity results to confirm the diagnoses.
Our finding that antimicrobial resistance increased mortality, length of stay, and cost is not surprising, yet the interesting finding is that once adjustments were made mortality was no longer statistically significant with antimicrobial resistance. A propensity-matched analysis of 370 patients with hospital-acquired infection after cardiac surgery had significantly greater crude hospital mortalities compared to 370 matched patients (15.4% vs. 5.7%) [4]. As patients who undergo cardiac procedures without complication are unlikely to be routinely tested for antimicrobial resistance, those who undergo testing are likely to be suspected of having an infection. With antimicrobial resistance, there may be limitations as to the agents available to treat infection and this would result in greater mortalities, associated prolonged hospitalizations, and associated costs through attempting various treatments and supporting the patient in recovering from the infection, including the need for intensive care support. The observation in the current study that adjustments for comorbidity made the association between antimicrobial resistance and mortality no longer significant is interesting because it suggests that existing illnesses are important factors that contribute to mortality risk in patients with antimicrobial-resistant organisms.
Our study highlights the need for greater awareness regarding antimicrobial resistance in cardiac surgery and the need to reduce the burden of this problem. This requires education of healthcare professionals as early detection of infection postoperatively and appropriate action may avert poor outcomes for patients. The findings of the current study, whereby antimicrobial resistance appears to be more common in female patients, and those with a history of alcohol misuse, chronic kidney disease, and atrial fibrillation are interesting as this may be useful information about high-risk groups for clinical practices. There may also be a role for greater awareness of the importance of following antimicrobial guidelines as proper usage of antibiotics is very important to reduce the chance of the development of drug-resistant organisms in patients [25]. Furthermore, efforts may be needed to reduce clinical misdiagnosis of infections as excessive use of antibiotic misuse, when not clinically indicated, can contribute to antibiotic resistance [26].
In the current study, we found low rates of antimicrobial resistance and we suspect that antimicrobial resistance may be underreported. Antimicrobial resistance is only present as a diagnosis in a patient discharge summary if patients underwent testing and the healthcare team managing patients documented this finding. Patients may not be tested for antimicrobial resistance, or the test was a false negative, while it is further possible that the diagnosis was not documented. However, the concept of antimicrobial resistance among patients with coronary artery bypass graft and valve surgery is not well explored from a national perspective and our study would call for more studies in this area.
4.3. Generalizability
The current study evaluates a dataset from hospital records, which is designed to provide estimates that are nationally representative of the United States. Therefore, this study is generalizable to practices in America, although it may not be entirely applicable to other countries with different ethnic populations, demographic profiles, healthcare services, and patterns of infectious organisms from cardiac surgery.
4.4. Limitations
This analysis has several limitations that need to be considered prior to interpretation. The accuracy of patient identification relies on accurate ICD-10 diagnosis and procedure codes. This is particularly important in relation to the codes for antimicrobial resistance, CABG, and valve surgery. In the case of antimicrobial resistance, as previously discussed, we cannot exclude the possibility of underreporting as we do not know the criteria for making this diagnosis. Moreover, we do not have information on the management of patients, including the microorganism, antimicrobial testing and sensitivities, and antimicrobials or drugs used for treatment. Considering the higher prevalence in the literature, the code for antimicrobial resistance is probably an underutilized administrative code. Moreover, the data is retrospective and observational, so the findings may be limited by potential confounders. The design of the NIS is such that a patient may appear more than once within the same calendar year and there is no way of determining whether patients appeared across different years. Another limitation of the current study is that we do not know the operative risk for the patients who undergo cardiac surgery. Future studies of antimicrobial resistance in patients who undergo cardiac surgery should consider the major risk scores for cardiac surgery, such as EuroScore and Parsonnet scores. Finally, this dataset included hospitalization until 2019, the pre-COVID-19 era, and thus, we cannot extrapolate our findings to the COVID-19 pandemic.
5. Conclusions
On a national level, antimicrobial resistance in patients that undergo cardiac surgery is not common, yet those who have this diagnosis have greater mortality, length of stay, and cost attached; however, once adjustments are made there is no significant increase in in-hospital mortality. The burden of antimicrobial resistance is substantial as it can double the length of hospitalization and increase the median cost by more than USD 20,000. Measures should be taken to better understand how we can reduce antimicrobial resistance and better manage patients who undergo cardiac surgery and are identified with this problem.
Author Contributions
Conceptualization, K.A.S. and C.S.K.; methodology and formal analysis, C.S.K.; data curation, A.I.Q.; writing—original draft preparation, C.S.K.; writing—review and editing, K.A.S., M.W. and A.I.Q. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The National Inpatient Sample is a data set where research use does not require institutional review board review.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data used in this analysis may be purchased from the Healthcare Cost and Utilization Project website. The authors do not have permission to share the data used for the analysis.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A

Table A1.
Codes for data analysis and their source.
Table A1.
Codes for data analysis and their source.
| Variable | Source of Data | Detailed Codes/Description |
|---|---|---|
| Coronary artery bypass graft surgery | I10_PR1/25 | 021008, 021009, 02100A, 02100J, 02100K, 02100Z, 021108, 021109, 02110A, 02110J, 02110K, 02110Z, 021208, 021209, 02120A, 02120J, 02120K, 02120Z, 021308, 021309, 02130A, 02130J, 02130K, 02130Z |
| Valve surgery | I10_PR1/25 | 02RF0, 02RF3, 02RG0, 02RG3, 02RH0, 02RH3, 02RJ0, 02RJ3 |
| Antibiotic resistance | I10_DX1/40 | Z16 |
| Age | NIS Core | Derived from “AGE” variable. |
| Sex | NIS Core | Derived from “FEMALE” variable. |
| Race | NIS Core | Derived from “RACE” variable. |
| Rural | See comment | Derived from “PL_NCHS” variable in the NIS Core file where rural = micropolitan counties and not metropolitan or micropolitan counties. |
| Teaching hospital | See comment | Derived from “HOSP_LOCTEACH” variable in the NIS Hospital file where teaching hospitals are those which are urban teaching values. |
| Hospital region | NIS Hospital | Derived from “HOSP_REGION” variable. |
| Elective admission | NIS Core | Derived from “ELECTIVE” variable. |
| Weekend admission | NIS Core | Derived from “AWEEKEND” variable. |
| Primary expected payer | NIS Core | Derived from “PAY1” variable. |
| ZIP income quartile | NIS Core | Derived from “ZIPINC_QRTL” variable. |
| Hospital bed size | NIS Hospital | Derived from “HOSP_BEDSIZE” variable. |
| Smoking | I10_DX1/40 | Z72.0 |
| Alcohol misuse | I10_DX1/40 | F10.1 |
| Chronic kidney disease | I10_DX1/40 | N18 |
| Chronic lung disease | I10_DX1/40 | J40, J41, J42, J43, J44, J45, J46, J47 |
| Previous myocardial infarction | I10_DX1/40 | I25.2 |
| Previous stroke | I10_DX1/40 | I69 |
| Atrial fibrillation | I10_DX1/40 | I48 |
| Hypertension | I10_DX1/40 | I10, I11, I12, I13, I15, I16 |
| Hypercholesterolemia | I10_DX1/40 | E78.0, E78.1, E78.2, E78.3, E78.4, E78.5 |
| Diabetes mellitus | I10_DX1/40 | E08, E09, E10, E11, E13 |
| Cancer | I10_DX1/40 | C * |
| Dementia | I10_DX1/40 | F01, F02, F03, G30, G31 |
| Peripheral vascular disease | I10_DX1/40 | I73 |
| Liver failure | I10_DX1/40 | K72 |
| Obesity | I10_DX1/40 | E66.0, E66.1, E66.2, E66.8, E66.9 |
| Heart failure | I10_DX1/40 | I09.81, I11.0, I50 |
| Season | AMONTH Spring = March to May, Summer = June to August, Fall = September to November, Winter = December to February | |
| Central venous line | I10_PR1/25 | 02HV33Z, 02H633Z |
| Sepsis | I10_DX1/40 | A41 |
| Infection | I10_DX1/40 | A *, B * |
| Death | NIS Core | - |
| Length of stay | NIS Core | - |
| Cost | See comment | Defined by the product of the charge-to-cost ratio and total charge (“TOTCHG” in the NIS core file). |
| Discharge weight | NIS Core | - |
* signifies truncation where there may be any number after the initial letter.
References
- Moffatt-Bruce, S.; Crestanello, J.; Way, D.P.; Williams, T.E., Jr. Providing cardiothoracic services in 2035: Signs of trouble ahead. J. Thorac. Cardiovasc. Surg. 2018, 155, 824–829. [Google Scholar] [CrossRef] [PubMed]
- Mori, M.; Khera, R. Pumping the breaks on health care costs of cardiac surgery focusing on postacute cardiac spending. Circ. Cardiovasc. Qual. Outcomes 2020, 13, e007253. [Google Scholar] [CrossRef]
- Kollef, M.H.; Sharpless, L.; Vlasnik, J.; Pasque, C.; Murphy, D.; Fraser, V.J. The impact of nosocomial infections on patient outcomes following cardiac surgery. Chest 1997, 112, 666–675. [Google Scholar] [CrossRef] [PubMed]
- Massart, N.; Mansour, A.; Ross, J.T.; Piau, C.; Verhoye, J.P.; Tattevin, P.; Nesseler, N. Mortality due to hospital-acquired infection after cardiac surgery. J. Thorac. Cardiovasc. Surg. 2022, 163, 2131–2140. [Google Scholar] [CrossRef]
- Jenney, A.W.; Harrington, G.A.; Spelman, D.W. Cost of surgical site infections following coronary artery bypass surgery. ANZ J. Surg. 2001, 71, 662–664. [Google Scholar] [CrossRef] [PubMed]
- Engelman, R.; Shahian, D.; Shemin, R.; Guy, T.S.; Bratzler, D.; Edwards, F.; Jacobs, M.; Fernando, H.; Bridges, C. The Society of Thoracic Surgeons Practice Guideline Series: Antibiotic prophylaxis in cardiac surgery, part II: Antibiotic choice. Ann. Thorac. Surg. 2007, 83, 1569–1576. [Google Scholar] [CrossRef]
- Lador, A.; Nasir, H.; Mansur, N.; Sharoni, E.; Biderman, P.; Leibovici, L.; Paul, M. Antibiotic prophylaxis in cardiac surgery: Systematic review and meta-analysis. J. Antimicrob. Chemother. 2012, 67, 541–550. [Google Scholar] [CrossRef]
- Fong, I.W.; Baker, C.B.; McKee, D.C. The value of prophylactic antibiotics in aorta-coronary bypass operations: A double-blind randomized trial. J. Thorac. Cardiovasc. Surg. 1979, 78, 908–913. [Google Scholar] [CrossRef]
- Zanetti, G.; Goldie, S.J.; Platt, R. Clinical consequences and cost of limiting use of vancomycin for perioperative prophylaxis: Example of coronary artery bypass surgery. Emerg. Infect. Dis. 2001, 7, 820–827. [Google Scholar] [CrossRef]
- Gelijns, A.C.; Moskowitz, A.J.; Acker, M.A.; Argenziano, M.; Geller, N.L.; Puskas, J.D.; Perrault, L.P.; Smith, P.K.; Kron, I.L.; Michler, R.E.; et al. Management practices and major infections after cardiac surgery. J. Am. Coll. Cardiol. 2014, 64, 372–381. [Google Scholar] [CrossRef]
- World Health Organization. Antimicrobial Resistance. Available online: https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance (accessed on 24 December 2022).
- Antimicrobial Resistance Collaborators. Global burden on bacterial antimicrobial resistance in 2019: A systematic analysis. Lancet 2022, 399, 629–655. [Google Scholar] [CrossRef]
- Johnston, K.J.; Thorpe, K.E.; Jacob, J.T.; Murphy, D.J. The incremental cost of infections associated with multidrug-resistant organisms in the inpatient hospital setting—A national estimate. Health Serv. Res. 2019, 54, 782–792. [Google Scholar] [CrossRef]
- The Expert Panel on The Potential Socio-Economic Impacts of Antimicrobial Resistance in Canada. When Antibiotics Fail. 2019. Available online: https://cca-reports.ca/reports/the-potential-socio-economic-impacts-of-antimicrobial-resistance-in-canada/ (accessed on 24 December 2022).
- Pierce, G.N.; Resch, C.; Mourin, M.; Dibrov, P.; Dibrov, E.; Ravandi, A. Bacteria and growing threat of multidrug resistance for invasive cardiac interventions. Rev. Cardiovasc. Med. 2022, 23, 15. [Google Scholar] [CrossRef]
- Healthcare Cost & Untilization Project. Overview of the National (Nationwide) Inpatient Sample (NIS). Available online: https://www.hcup-us.ahrq.gov/nisoverview.jsp (accessed on 24 December 2022).
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- Mubashir, T.; Balogh, J.; Breland, E.; Rumpel, D.; Waheed, M.A.; Lai, H.; Napolitano, C.A. Risk factors and outcome of protein-calorie malnutrition in chronic heart failure patients undergoing elective cardiac surgery. Cureus 2022, 14, e30378. [Google Scholar] [CrossRef]
- World Health Organization. Global Action Plan on Antimicrobial Resistance. Available online: https://ahpsr.who.int/publications/i/item/global-action-plan-on-antimicrobial-resistance (accessed on 24 December 2022).
- Hamasaeed, P.A. Resistance to bacterial infection, complication occurring after cardiac surgery. Cell. Mol. Biol. 2020, 66, 20–25. [Google Scholar] [CrossRef]
- Ko, R.E.; Huh, K.; Kim, D.H.; Na, S.J.; Chung, C.R.; Cho, Y.H.; Jeon, K.; Suh, G.Y.; Yang, J.H. Nosocomial infections in in-hospital cardiac arrest patients who undergo extracorporeal cardiopulmonary resuscitation. PLoS ONE 2020, 15, e0243838. [Google Scholar] [CrossRef]
- Bhatt, P.J.; Ali, M.; Rana, M.; Patel, G.; Sullivan, T.; Murphy, J.; Pinney, S.; Anyanwu, A.; Huprikar, S.; Taimur, S. Infections due to multidrug-resistant organisms following heart transplantation: Epidemiology, microbiology, and outcomes. Transpl. Infect. Dis. 2020, 22, e13215. [Google Scholar] [CrossRef]
- Zhou, Y.; Cai, J.; Wang, X.; Du, S.; Zhang, J. Distribution and resistance of pathogens in infected patients within 1 year after heart transplantation. Int. J. Infect. Dis. 2020, 103, 132–137. [Google Scholar] [CrossRef]
- Crnich, C.J.; Safdar, N.; Robinson, J.; Zimmerman, D. Longitudinal trends in antibiotic resistance in US nursing homes, 2000–2004. Infect. Control Hosp. Epidemiol. 2007, 28, 1006–1008. [Google Scholar] [CrossRef]
- Menz, B.D.; Charani, E.; Gordon, D.L.; Leather, A.J.M.; Moonesinghe, S.R.; Phillips, C.J. Surgical antibiotic prophylaxis in an era of antibiotic resistance: Common resistant bacteria and wider considerations for practice. Infect. Drug Resist. 2021, 14, 5235–5252. [Google Scholar] [CrossRef] [PubMed]
- Chokshi, A.; Sifri, Z.; Cennimo, D.; Horng, H. Global contributors to antibiotic resistance. J. Glob. Infect. Dis. 2019, 11, 36–42. [Google Scholar] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).