Laser Interventions for Intraoral Halitosis: A Systematic Review of Randomized Controlled Trials
Abstract
1. Introduction
2. Materials and Methods
2.1. Focused Question
2.2. Search Strategy
2.3. Study Selection Process
2.4. Risk of Bias in Individual Studies
2.5. Quality Assessment
2.6. Data Extraction
3. Results
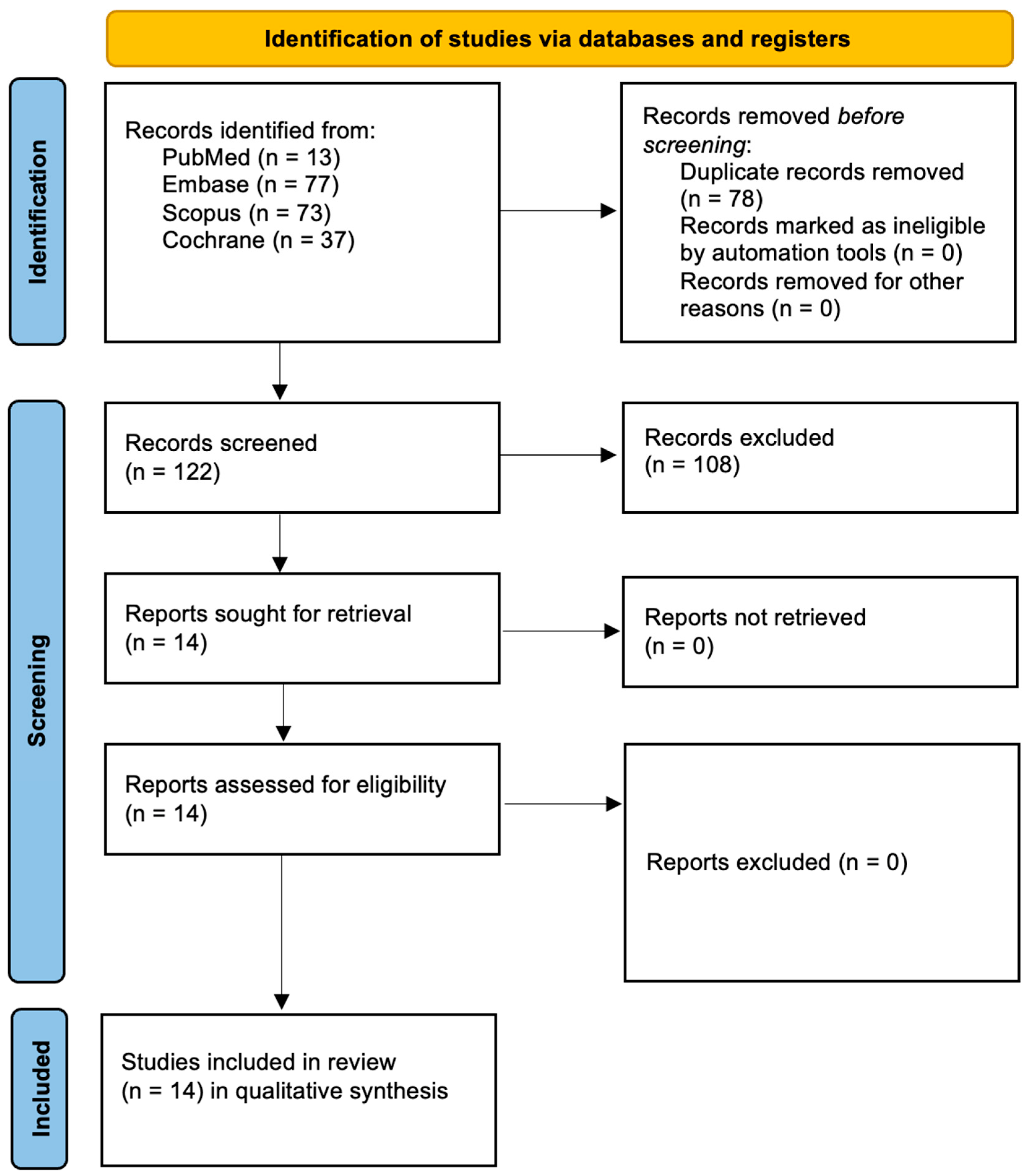
3.1. Study Selection
3.2. Data Presentation
3.3. Overview of Study Characteristics
| Study | Geographic Location | Aim |
|---|---|---|
| Alshahrani et al., 2020 [41] | Saudi Arabia | Evaluate efficacy of PDT with diode laser and methylene blue in halitosis during orthodontic treatment. |
| Joseph et al., 2016 [42] | India | Assess aPDT as adjunct to SRP in chronic periodontitis. |
| Bruno et al., 2024 [43] | Italy | Compare efficacy of aPDT vs. conventional treatment for halitosis in adolescents. |
| Ciarcia et al., 2019 [44] | Italy | Test aPDT with erythrosine and red LED for halitosis in periodontitis patients. |
| Dereci et al., 2016 [45] | Turkey | Evaluate Er,Cr:YSGG laser-assisted periodontal therapy on halitosis and periodontal healing. |
| do Vale et al., 2021 [46] | Brazil | Compare aPDT and tongue scraping for halitosis in older adults with dentures. |
| Gonçalves et al., 2020 [47] | Brazil | Test aPDT with Bixa orellana extract and blue LED in halitosis reduction. |
| Joseph et al., 2014 [48] | United States | Assess laser tongue debridement for oral malodor reduction. |
| Krespi et al., 2021 [49] | Brazil | Evaluate aPDT alone and combined with scraping in adolescent halitosis treatment. |
| Lopes et al., 2014 [50] | Brazil | Compare effect of photodynamic therapy and tongue scraping on halitosis in adolescents using gas chromatography. |
| Lopes et al., 2016 [51] | Brazil | Evaluate antimicrobial effect of annatto-based PDT versus chlorhexidine and tongue scraper on halitosis in children. |
| da Mota et al., 2016 [52] | Brazil | Assess effects of SRP with or without PDT on halitosis and periodontal health in bronchiectasis patients. |
| Pinto et al., 2016 [53] | Brazil | Determine whether oral hygiene behavior combined with aPDT or tongue scraper reduces halitosis over 90 days. |
| Romero et al., 2021 [54] | Brazil | To verify whether modification of oral hygiene behavior associated with aPDT or a lingual scraper can reduce halitosis after a 90-day follow-up. |
3.4. Main Study Outcomes
| Author and Year | Study Groups | Outcomes |
|---|---|---|
| Alshahrani et al., 2020 [41] | 1. (PDT only) 2. (TS only) 3. (PDT + TS) |
|
| Joseph et al., 2016 [42] | 1. (Control) Tongue scraping only 2. Tongue scraping followed by chlorhexidine mouthwash 3. (Experimental) Tongue scraping followed by aPDT using MB and a diode laser at 660 nm |
|
| Bruno et al., 2024 [43] | 1. (Experimental) aPDT using annatto-based photosensitizer and blue LED 2. (Control) Tongue scraping only |
|
| Ciarcia et al., 2019 [44] | 1. (Experimental) MB-aPDT and a 660 nm diode laser 2. (Control) Received a placebo treatment without laser activation |
|
| Dereci et al., 2016 [45] | 1. (Experimental) aPDT using toluidine blue and a diode laser 2. (Control) Placebo treatment without laser irradiation |
|
| do Vale et al., 2021 [46] | 1. (Experimental) Treated with antimicrobial aPDT using a 660 nm laser and annatto-based photosensitizer 2. (Control) Placebo |
|
| Gonçalves et al., 2020 [47] | 1. aPDT with Bixa orellana extract and blue LED 2. (Control) Tongue scraping only 3. Tongue scraping and aPDT with Bixa orellana extract and blue LED |
|
| Joseph et al., 2014 [48] | 1. (Experimental) Tongue brushing followed by aPDT using methylene blue and a 660 nm diode laser 2. (Control) Tongue brushing only |
|
| Krespi et al., 2021 [49] | 1. (Experimental) Treated with Er,Cr:YSGG laser tongue debridement. 2. (Control) Treated with tongue scraper, each initially comprising 30 patients |
|
| Lopes et al., 2014 [50] | 1. (Experimental) MB-aPDT and a red diode laser after tongue scraping 2. (Control) Underwent tongue scraping only. |
|
| Lopes et al., 2016 [51] | 1. aPDT on the dorsum of the tongue 2. Treatment with a tongue scraper 3. Combination of tongue scraper and photodynamic therapy. |
|
| da Mota et al., 2016 [52] | 1. aPDT only 2. Tongue scraper only, 3. Both photodynamic therapy and a tongue scraper. |
|
| Pinto et al., 2016 [53] | 1. (Experimental) Treated with aPDT using methylene blue and laser 2. (Control) Treated with mechanical tongue scraping only. |
|
| Romero et al., 2021 [54] | 1. (Experimental) Received aPDT with urucum photosensitizer and LED light 2. (Control) Received placebo treatment without active photosensitizer. |
|
| Study | Follow-Up Duration | Key Outcome |
|---|---|---|
| Alshahrani et al. (2020) [41] | Immediate | A 100% reduction in H2S in PDT + scraper group after treatment |
| Gonçalves et al. (2020) [47] | Immediate | Significant VSC reduction immediately; not maintained at 7 days |
| Lopes et al. (2014) [50] | Immediate | Reduction in halitosis at 1 and 24 h after treatment |
| da Mota et al. (2016) [52] | Immediate | Significant VSC reduction; median VSC = 0 in PDT + scraper group |
| Romero et al. (2021) [54] | Immediate | H2S reduced in both aPDT and scraper groups (p = 0.0001) |
| do Vale et al. (2021) [46] | Short Term (7 days) | Halitosis levels remained socially acceptable at 7 days |
| Bruno et al. (2024) [43] | Short Term (7 days) | Sustained reduction in halitosis at 7 days post-treatment |
| Ciarcia et al. (2019) [44] | Short Term (7–14 days) | Reduction in VSC at 7 and 14 days, partially sustained |
| Romero et al. (2021) [54] | Short Term (7 days) | H2S 3x lower in aPDT and 2× lower in scraper group at 7 days |
| Joseph et al. (2014) [48] | Intermediate (30 days) | Significant halitosis reduction at 1 month, then declined |
| Bruno et al. (2024) [43] | Intermediate (30 days) | Reduction in halitosis maintained at 30 days |
| Romero et al. (2021) [54] | Intermediate (90 days) | H2S remained 2–3× lower; halitosis still above clinical threshold |
| Dereci et al. (2016) [45] | Long Term (3–6 months) | Sustained VSC reduction at 3 and 6 months |
| Pinto et al. (2016) [53] | Intermediate (3 months) | Planned follow-up at 3 months; outcomes pending (protocol study) |
3.5. Measuring Halitosis
3.6. Characteristics of Light Sources Used in PDT
3.7. Reported Adverse Effects and Safety
4. Discussion
4.1. Results in the Context of Other Evidence
4.2. Limitations of the Evidence
4.3. Limitations of the Review Process
4.4. Implications for Practice, Policy, and Future Research
4.5. Research Gaps and Translational Outlook
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Teshome, A.; Derese, K.; Andualem, G. The Prevalence and Determinant Factors of Oral Halitosis in Northwest Ethiopia: A Cross-Sectional Study. Clin. Cosmet. Investig. Dent. 2021, 13, 173–179. [Google Scholar] [CrossRef]
- Renvert, S.; Noack, M.J.; Lequart, C.; Roldán, S.; Laine, M.L. The Underestimated Problem of Intra-Oral Halitosis in Dental Practice: An Expert Consensus Review. Clin. Cosmet. Investig. Dent. 2020, 12, 251–262. [Google Scholar] [CrossRef]
- Kapoor, U.; Sharma, G.; Juneja, M.; Nagpal, A. Halitosis: Current concepts on etiology, diagnosis and management. Eur. J. Dent. 2016, 10, 292–300. [Google Scholar] [CrossRef]
- Gokdogan, O.; Catli, T.; Ileri, F. Halitosis in otorhinolaryngology practice. Iran. J. Otorhinolaryngol. 2015, 27, 145–153. [Google Scholar]
- Aylıkcı, B.U.; Colak, H. Halitosis: From diagnosis to management. J. Nat. Sci. Biol. Med. 2013, 4, 14–23. [Google Scholar] [CrossRef]
- Tungare, S.; Zafar, N.; Paranjpe, A.G. Halitosis [Updated 14 August 2023]. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2025. Available online: https://www.ncbi.nlm.nih.gov/books/NBK534859/ (accessed on 1 June 2025).
- Awano, S.; Gohara, K.; Kurihara, E.; Ansai, T.; Takehara, T. The relationship between the presence of periodontopathogenic bacteria in saliva and halitosis. Int. Dent. J. 2002, 52, 212–216. [Google Scholar] [CrossRef]
- Waler, S.M. On the transformation of sulfur-containing amino acids and peptides to volatile sulfur compounds (VSC) in the human mouth. Eur. J. Oral Sci. 1997, 105, 534–537. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Huang, Z.; Tang, Z.; Huang, Y.; Huang, M.; Liu, H.; Ziebolz, D.; Schmalz, G.; Jia, B.; Zhao, J. More Than Just a Periodontal Pathogen—The Research Progress on Fusobacterium nucleatum. Front. Cell Infect. Microbiol. 2022, 12, 815318. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wang, B.; Deng, J.; Donati, V.; Merali, N.; Frampton, A.E.; Giovannetti, E.; Deng, D. The Roles and Interactions of Porphyromonas gingivalis and Fusobacterium nucleatum in Oral and Gastrointestinal Carcinogenesis: A Narrative Review. Pathogens 2024, 13, 93. [Google Scholar] [CrossRef] [PubMed]
- Pignatelli, P.; Romei, F.M.; Bondi, D.; Giuliani, M.; Piattelli, A.; Curia, M.C. Microbiota and Oral Cancer as A Complex and Dynamic Microenvironment: A Narrative Review from Etiology to Prognosis. Int. J. Mol. Sci. 2022, 23, 8323. [Google Scholar] [CrossRef]
- Hampelska, K.; Jaworska, M.M.; Babalska, Z.; Karpiński, T.M. The Role of Oral Microbiota in Intra-Oral Halitosis. J. Clin. Med. 2020, 9, 2484. [Google Scholar] [CrossRef] [PubMed]
- Harrandah, A.M.; Chukkapalli, S.S.; Bhattacharyya, I.; Progulske-Fox, A.; Chan, E.K.L. Fusobacteria Modulate Oral Carcinogenesis and Promote Cancer Progression. J. Oral. Microbiol. 2020, 13, 1849493. [Google Scholar] [CrossRef] [PubMed]
- Kumbargere Nagraj, S.; Eachempati, P.; Uma, E.; Singh, V.P.; Ismail, N.M.; Varghese, E. Interventions for managing halitosis. Cochrane Database Syst. Rev. 2019, 12, CD012213. [Google Scholar] [CrossRef] [PubMed]
- Oliveira-Neto, J.M.; Sato, S.; Pedrazzi, V. How to deal with morning bad breath: A randomized, crossover clinical trial. J. Indian Soc. Periodontol. 2013, 17, 757–761. [Google Scholar] [CrossRef]
- Acar, B.; Berker, E.; Tan, C.; Ilarslan, Y.D.; Tekcicek, M.; Tezcan, I. Effects of oral prophylaxis including tongue cleaning on halitosis and gingival inflammation in gingivitis patients—A randomized controlled clinical trial. Clin. Oral Investig. 2019, 23, 1829–1836. [Google Scholar] [CrossRef]
- Ademovski, S.E.; Lingström, P.; Winkel, E.; Tangerman, A.; Persson, G.R.; Renvert, S. Comparison of different treatment modalities for oral halitosis. Acta Odontol. Scand. 2012, 70, 224–233. [Google Scholar] [CrossRef]
- Poppolo Deus, F.; Ouanounou, A. Chlorhexidine in Dentistry: Pharmacology, Uses, and Adverse Effects. Int. Dent. J. 2022, 72, 269–277. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dumitriu, A.S.; Păunică, S.; Nicolae, X.A.; Bodnar, D.C.; Albu, Ș.D.; Suciu, I.; Ciongaru, D.N.; Giurgiu, M.C. The Effectiveness of the Association of Chlorhexidine with Mechanical Treatment of Peri-Implant Mucositis. Healthcare 2023, 11, 1918. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Raszewski, Z.; Nowakowska-Toporowska, A.; Wezgowiec, J.; Nowakowska, D. Design and characteristics of new experimental chlorhexidine dental gels with anti-staining properties. Adv. Clin. Exp. Med. 2019, 28, 885–890. [Google Scholar] [CrossRef] [PubMed]
- Joshipura, K.J.; Munoz-Torres, F.J.; Morou-Bermudez, E.; Patel, R.P. Over-the-counter mouthwash use and risk of pre-diabetes/diabetes. Nitric Oxide 2017, 71, 14–20. [Google Scholar] [CrossRef]
- Poppolo Deus, F.; Ouanounou, A. Mouthwashes and their use in dentistry: A review. Oral Health 2021, 1, 22–34. [Google Scholar]
- Shrimathi, S.; Kemparaj, U.; Umesh, S.; Karuppaiah, M.; Pandian, P.; Krishnaveni, A. Comparative evaluation of cocoa bean husk, ginger and chlorhexidine mouth washes in the reduction of Steptococcus mutans and Lactobacillus count in saliva: A randomized controlled trial. Cureus 2019, 11, e4968. [Google Scholar] [CrossRef]
- Asadoorian, J. Therapeutic oral rinsing with commercially available products: Position paper and statement from the Canadian Dental Hygienists Association. Can. J. Dent. Hyg. 2016, 50, 126–139. [Google Scholar]
- Supranoto, S.C.; Slot, D.E.; Van Der Weijden, G.A.; Addy, M. The effect of chlorhexidine dentifrice or gel versus chlorhexidine mouthwash on plaque, gingivitis, bleeding and tooth discoloration: A systematic review. Int. J. Dent. Hyg. 2015, 13, 83–92. [Google Scholar] [CrossRef]
- Kellesarian, S.V.; Malignaggi, V.R.; Al-Kheraif, A.A.; Al-Askar, M.; Yunker, M.; Javed, F. Effect of antimicrobial photodynamic therapy and laser alone as adjunct to mechanical debridement in the management of halitosis: A systematic review. Quintessence Int. 2017, 48, 575–583. [Google Scholar] [CrossRef] [PubMed]
- Dembicka-Mączka, D.; Kępa, M.; Fiegler-Rudol, J.; Grzech-Leśniak, Z.; Matys, J.; Grzech-Leśniak, K.; Wiench, R. Evaluation of the Disinfection Efficacy of Er: YAG Laser Light on Single-Species Candida Biofilms—An In Vitro Study. Dent. J. 2025, 13, 88. [Google Scholar] [CrossRef] [PubMed]
- Fiegler-Rudol, J.; Kapłon, K.; Kotucha, K.; Moś, M.; Skaba, D.; Kawczyk-Krupka, A.; Wiench, R. Hypocrellin-Mediated PDT: A Systematic Review of Its Efficacy, Applications, and Outcomes. Int. J. Mol. Sci. 2025, 26, 4038. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fiegler-Rudol, J.; Grzech-Leśniak, Z.; Tkaczyk, M.; Grzech-Leśniak, K.; Zawilska, A.; Wiench, R. Enhancing Root Canal Disinfection with Er:YAG Laser: A Systematic Review. Dent. J. 2025, 13, 101. [Google Scholar] [CrossRef] [PubMed]
- Woźniak, A.; Matys, J.; Grzech-Leśniak, K. Effectiveness of lasers and aPDT in elimination of intraoral halitosis: A systematic review based on clinical trials. Lasers Med. Sci. 2022, 37, 3403–3411. [Google Scholar] [CrossRef]
- Kocherova, I.; Bryja, A.; Błochowiak, K.; Kaczmarek, M.; Stefańska, K.; Matys, J.; Grzech-Leśniak, K.; Dominiak, M.; Mozdziak, P.; Kempisty, B.; et al. Photobiomodulation with Red and Near-Infrared Light Improves Viability and Modulates Expression of Mesenchymal and Apoptotic-Related Markers in Human Gingival Fibroblasts. Materials 2021, 14, 3427. [Google Scholar] [CrossRef]
- Sterczała, B.; Grzech-Leśniak, K.; Michel, O.; Trzeciakowski, W.; Dominiak, M.; Jurczyszyn, K. Assessment of Human Gingival Fibroblast Proliferation after Laser Stimulation In Vitro Using Different Laser Types and Wavelengths (1064, 980, 635, 450, and 405 nm)-Preliminary Report. J. Pers. Med. 2021, 11, 98. [Google Scholar] [CrossRef] [PubMed]
- Jao, Y.; Ding, S.J.; Chen, C.C. Antimicrobial photodynamic therapy for the treatment of oral infections: A systematic review. J. Dent. Sci. 2023, 18, 1453–1466. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bruno, L.H.; Sobral, A.P.T.; Gonçalves, M.L.L.; Fossati, A.L.; Santos, E.M.; Gallo, J.M.A.S.; Ferri, E.P.; Motta, P.d.B.; Prates, R.A.; Deana, A.M.; et al. Comparative study between photodynamic therapy and the use of probiotics in the reduction of halitosis in mouth breathing children: Study protocol for a randomized controlled clinical trial. Medicine 2023, 102, e33512. [Google Scholar] [CrossRef]
- Wiench, R.; Fiegler-Rudol, J.; Latusek, K.; Brus-Sawczuk, K.; Fiegler, H.; Kasperski, J.; Skaba, D. Indocyanine Green as a Photosensitizer in Periodontitis Treatment: A Systematic Review of Randomized Controlled Trials. Life 2025, 15, 1015. [Google Scholar] [CrossRef]
- Al Balah, O.F.; Rafie, M.; Osama, A.R. Immunomodulatory effects of photobiomodulation: A comprehensive review. Lasers Med. Sci. 2025, 40, 187. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Schardt, C.; Adams, M.B.; Owens, T.; Keitz, S.; Fontelo, P. Utilization of the PICO framework to improve searching PubMed for clinical questions. BMC Med. Inf. Decis. Mak. 2007, 7, 16. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Watson, P.F.; Petrie, A. Method agreement analysis: A review of correct methodology. Theriogenology 2010, 73, 1167–1179. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed]
- Alshahrani, A.A.; Alhaizaey, A.; Kamran, M.A.; Alshahrani, I. Efficacy of antimicrobial photodynamic therapy against halitosis in adolescent patients undergoing orthodontic treatment. Photodiagnosis Photodyn. Ther. 2020, 32, 102019. [Google Scholar] [CrossRef]
- Joseph, B.; Prasanth, C.S.; Baiju, K.V.; Janam, P.; Subhash, N. Patients’ perceptions of antimicrobial photodynamic therapy in the management of chronic periodontitis. Photodiagnosis Photodyn. Ther. 2016, 13, 60–66. [Google Scholar] [CrossRef]
- Bruno, L.H.; Mandetta, A.R.H.; Sobral, A.P.T.; Leal Gonçalves, M.L.; Santos, E.M.; Fossati, A.L.; Gallo, J.M.A.S.; Motta, P.B.; Deana, A.M.; Horliana, A.C.R.T.; et al. Assessment of photodynamic therapy with annatto and LED for the treatment of halitosis in mouth-breathing children: Randomized controlled clinical trial. PLoS ONE 2024, 19, e0307957. [Google Scholar] [CrossRef]
- Ciarcia, A.C.C.M.; Gonçalves, M.L.L.; Horliana, A.C.R.T.; Suguimoto, E.S.A.; Araujo, L.; Laselva, A.; Mayer, M.P.A.; Motta, L.J.; Deana, A.M.; Mesquita-Ferrari, R.A.; et al. Action of antimicrobial photodynamic therapy with red leds in microorganisms related to halitose: Controlled and randomized clinical trial. Medicine 2019, 98, e13939. [Google Scholar] [CrossRef]
- Dereci, Ö.; Hatipoğlu, M.; Sindel, A.; Tozoğlu, S.; Üstün, K. The efficacy of Er,Cr:YSGG laser supported periodontal therapy on the reduction of periodontal disease related oral malodor: A randomized clinical study. Head Face Med. 2016, 12, 20. [Google Scholar] [CrossRef]
- do Vale, K.L.; Horliana, A.C.R.T.; dos Santos, S.R.; Schalch, T.O.; de Ana, A.M.; Ferrari, R.A.M.; Bussadori, S.K.; Fernandes, K.P.S. Treatment of halitosis with photodynamic therapy in older adults with complete dentures: A randomized, controlled, clinical trial. Photodiagnosis Photodyn. Ther. 2021, 33, 102128. [Google Scholar] [CrossRef] [PubMed]
- Gonçalves, M.L.L.; da Mota, A.C.C.; Deana, A.M.; Cavalcante, L.A.S.; Horliana, A.C.R.T.; Pavani, C.; Motta, L.J.; Fernandes, K.P.S.; Mesquita-Ferrari, R.A.; da Silva, D.F.T.; et al. Antimicrobial photodynamic therapy with Bixa orellana extract and blue LED in the reduction of halitosis: A randomized, controlled clinical trial. Photodiagnosis Photodyn. Ther. 2020, 30, 101751. [Google Scholar] [CrossRef]
- Joseph, B.; Sekhar, P.C.; Baiju, K.V.; Janam, P.; Narayanan, S. Efficacy of antimicrobial photodynamic therapy in the management of chronic periodontitis: A randomized controlled clinical trial. J. Clin. Periodontol. 2014, 41, 573–581. [Google Scholar] [CrossRef] [PubMed]
- Krespi, Y.P.; Kizhner, V.; Wilson, K.A.; Sivriver, A.; Low, S.; Khosravi, Y.; Stoodley, P. Laser tongue debridement for oral malodor: A novel approach to halitosis. Am. J. Otolaryngol. 2021, 42, 102458. [Google Scholar] [CrossRef]
- Lopes, R.G.; de Godoy, C.H.L.; Deana, A.M.; de Santi, M.E.S.O.; Prates, R.A.; França, C.M.; Fernandes, K.P.S.; Mesquita-Ferrari, R.A.; Bussadori, S.K. Photodynamic therapy as a novel treatment for halitosis in adolescents: Study protocol for a randomized controlled trial. Trials 2014, 15, 443. [Google Scholar] [CrossRef] [PubMed]
- Lopes, R.G.; da Mota, A.C.C.; Soares, C.; Tarzia, O.; Deana, A.M.; Prates, R.A.; França, C.M.; Fernandes, K.P.S.; Ferrari, R.A.M.; Bussadori, S.K. Immediate results of photodynamic therapy for the treatment of halitosis in adolescents: A randomized, controlled, clinical trial. Lasers Med. Sci. 2016, 31, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Costa da Mota, A.C.; França, C.M.; Prates, R.; Deana, A.M.; Santos, L.C.; Garcia, R.L.; Gonçalves, M.L.L.; Ferrari, R.A.M.; Fernandes, K.P.S.; Bussadori, S.K. Effect of photodynamic therapy for the treatment of halitosis in adolescents—A controlled, microbiological, clinical trial. J. Biophotonics 2016, 9, 1337–1343. [Google Scholar] [CrossRef]
- Pinto, E.H.; Longo, P.L.; de Camargo, C.C.B.; Dal Corso, S.; Lanza, F.D.C.; Stelmach, R.; Athanazio, R.; Fernandes, K.P.S.; Mayer, M.P.A.; Bussadori, S.K.; et al. Assessment of the quantity of microorganisms associated with bronchiectasis in saliva, sputum and nasal lavage after periodontal treatment: A study protocol of a randomised controlled trial. BMJ Open 2016, 6, e010564. [Google Scholar] [CrossRef]
- Romero, S.S.; do Vale, K.L.; Remolina, V.G.; Silva, T.G.; Schalch, T.O.; Ramalho, K.M.; Negreiros, R.M.; Ando, E.S.; Mayer, M.P.A.; Ferrari, R.A.M.; et al. Oral hygiene associated with antimicrobial photodynamic therapy or lingual scraper in the reduction of halitosis after 90 days follow-up: A randomized, controlled, single-blinded trial. Photodiagnosis Photodyn. Ther. 2021, 33, 102057. [Google Scholar] [CrossRef] [PubMed]
- Veeresha, K.L.; Bansal, M.; Bansal, V. Halitosis: A Frequently Ignored Social Condition. J. Int. Soc. Prev. Community Dent. 2011, 1, 9–13. [Google Scholar] [CrossRef] [PubMed]
- Yoo, S.H.; Jung, H.S.; Sohn, W.S.; Kim, B.H.; Ku, B.H.; Kim, Y.S.; Park, S.W.; Hahm, K.B. Volatile sulfur compounds as a predictor for esophagogastroduodenal mucosal injury. Gut Liver 2008, 2, 113–118. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fiegler-Rudol, J.; Lipka, B.; Kapłon, K.; Moś, M.; Skaba, D.; Kawczyk-Krupka, A.; Wiench, R. Evaluating the Efficacy of Rose Bengal as a Photosensitizer in Antimicrobial Photodynamic Therapy Against Candida albicans: A Systematic Review. Int. J. Mol. Sci. 2025, 26, 5034. [Google Scholar] [CrossRef]
- Lopes, R.G.; de Santi, M.E.; Franco, B.E.; Deana, A.M.; Prates, R.A.; França, C.M.; Fernandes, K.P.; Ferrari, R.A.; Bussadori, S.K. Photodynamic therapy as novel treatment for halitosis in adolescents: A case series study. J. Lasers Med. Sci. 2014, 5, 146–152. [Google Scholar] [PubMed] [PubMed Central]
- Fiegler-Rudol, J.; Skaba, D.; Kawczyk-Krupka, A.; Wiench, R. Antibacterial and Bactericidal Effects of the Er: YAG Laser on Oral Bacteria: A Systematic Review of Microbiological Evidence. J. Funct. Biomater. 2025, 16, 209. [Google Scholar] [CrossRef]
- Romano, F.; Pigella, E.; Guzzi, N.; Manavella, V.; Campanelli, L.; Aimetti, M. Etiology and Characteristics of Halitosis in Patients of a Halitosis Center in Northern Italy. Minerva Stomatol. 2020, 69, 174–182. [Google Scholar] [CrossRef]
- Hu, Q.; Li, T.; Yang, J.; Peng, Y.; Liu, Q.; Liu, N. Efficacy of photodynamic therapy in the treatment of oral candidiasis: A systematic review and meta-analysis. BMC Oral Health 2023, 23, 802. [Google Scholar] [CrossRef]
- Wang, N.; Hao, S.; Zhang, J.; Yang, J. Clinical Efficacy of Photodynamic Therapy on Halitosis: A Systematic Review and Meta-Analysis. Lasers Med. Sci. 2023, 38, 29. [Google Scholar] [CrossRef] [PubMed]
- Pratama, A.R.; Rahmawati, Y.; Pratiwi, R. The Efficacy of Photodynamic Therapy in the Treatment of Halitosis. Int. J. Med. Sci. Clin. Res. Stud. 2025, 5, 499–505. [Google Scholar] [CrossRef]
- Silva-Boghossian, C.M.; Avila-Campos, M.J.; Saraiva, M.C.P.; de Barros Motta, P.; Gonçalves, M.L.L.; Gallo, J.M.A.S.; Sobral, A.P.T.; Motta, L.J.; Mayer, M.P.A.; Kawamoto, D.; et al. Short Term Effect of Antimicrobial Photodynamic Therapy and Probiotic L. salivarius WB21 on Halitosis: A Controlled and Randomized Clinical Trial. PLoS ONE 2024, 19, e0297351. [Google Scholar] [CrossRef]
- Dominiak, M.; Niemczyk, W.; Pitułaj, A.; Świenc, W.; Matys, J. Fatty Degenerative Osteonecrosis of the Jaw: Bridging Molecular Insights and Clinical Practice—A Scoping Review. Int. J. Mol. Sci. 2025, 26, 1853. [Google Scholar] [CrossRef]
- Mandetta, A.R.H.; Gallo, J.M.A.S.; Ribeiro, C.D.P.V.; Gonçalves, M.L.L.; Sobral, A.P.T.; Motta, L.J.; Horliana, A.C.R.T.; Mesquita-Ferrari, R.A.; Rodriguez, V.S.; Prates, R.A.; et al. Comparative study of photodynamic therapy with LED and probiotics in the treatment of halitosis: Protocol for a randomised controlled clinical trial. BMJ Open 2025, 15, e095544. [Google Scholar] [CrossRef]
- Motta, P.d.B.; Motta, L.J.; Campos, T.M.; Gonçalves, M.L.L.; Santos, E.M.; Martimbianco, A.L.C.; de Andrade, D.J.C.; Mesquita-Ferrari, R.A.; Fernandes, K.P.S.; Horliana, A.C.R.T.; et al. Effect of Photodynamic Therapy on Halitosis: A Systematic Review of Randomized Controlled Trials. Sensors 2022, 22, 469. [Google Scholar] [CrossRef]
- Kellesarian, S.V.; Malignaggi, V.R.; Abduljabbar, T.; Vohra, F.; Malmstrom, H.; Romanos, G.E.; Javed, F. Efficacy of scaling and root planing with and without adjunct antimicrobial photodynamic therapy on the expression of cytokines in the gingival crevicular fluid of patients with periodontitis: A systematic review. Photodiagnosis Photodyn. Ther. 2016, 16, 76–84. [Google Scholar] [CrossRef] [PubMed]
- Niemczyk, W.; Żurek, J.; Niemczyk, S.; Kępa, M.; Zięba, N.; Misiołek, M.; Wiench, R. Antibiotic-Loaded Platelet-Rich Fibrin (AL-PRF) as a New Carrier for Antimicrobials: A Systematic Review of In Vitro Studies. Int. J. Mol. Sci. 2025, 26, 2140. [Google Scholar] [CrossRef]
| Source | Search Term | Filters | Number of Results |
|---|---|---|---|
| PubMed | ((“Halitosis”[MeSH] OR halitosis OR “oral malodor” OR “intraoral halitosis”) AND ((“Lasers”[MeSH] OR laser OR lasers) OR (“Photochemotherapy”[MeSH] OR “photodynamic therapy” OR aPDT OR “antimicrobial photodynamic therapy”)) AND (elimination OR treatment OR management OR efficacy OR effectiveness)) | 2015–2025 RCT | 13 |
| Embase | (‘halitosis’/exp OR halitosis:ti,ab,kw OR ‘oral malodor’:ti,ab,kw OR ‘intraoral halitosis’:ti,ab,kw) AND ((‘laser’/exp OR laser:ti,ab,kw OR lasers:ti,ab,kw) OR (‘photochemotherapy’/exp OR ‘photodynamic therapy’:ti,ab,kw OR apdt:ti,ab,kw OR ‘antimicrobial photodynamic therapy’:ti,ab,kw)) AND (elimination:ti,ab,kw OR treatment:ti,ab,kw OR management:ti,ab,kw OR efficacy:ti,ab,kw OR effectiveness:ti,ab,kw) | 2015–2025 | 77 |
| Scopus | (TITLE-ABS-KEY(halitosis OR “oral malodor” OR “intraoral halitosis”)) AND (TITLE-ABS-KEY(laser OR lasers OR “photodynamic therapy” OR aPDT OR “antimicrobial photodynamic therapy”)) AND (TITLE-ABS-KEY(elimination OR treatment OR management OR efficacy OR effectiveness)) | 2015–2025 | 73 |
| Cochrane | (halitosis OR “oral malodor” OR “intraoral halitosis”) AND (laser OR lasers OR “photodynamic therapy” OR aPDT OR “antimicrobial photodynamic therapy”) AND (elimination OR treatment OR management OR efficacy OR effectiveness) | 2015–2025 | 37 |
| Study | Randomization Process | Deviations From Intended Interventions | Missing Outcome Data | Measurement of the Outcome | Selection of the Reported Result | Overall Bias Judgment |
|---|---|---|---|---|---|---|
| Alshahrani et al., 2020 [41] | Some concerns | Low | Low | Low | Some concerns | Medium |
| Joseph et al., 2016 [42] | Low | Low | Low | Some concerns | Some concerns | Medium |
| Bruno et al., 2024 [43] | Low | Low | Low | Low | Low | Low |
| Ciarcia et al., 2019 [44] | Some concerns | Low | Low | Low | Low | Medium |
| Dereci et al., 2016 [45] | Low | Low | Low | Low | Low | Low |
| do Vale et al., 2021 [46] | Low | Low | Low | Low | Some concerns | Medium |
| Gonçalves et al., 2020 [47] | Some concerns | Low | Low | Low | Some concerns | Medium |
| Joseph et al., 2014 [48] | Low | Low | Low | Low | Some concerns | Low |
| Krespi et al., 2021 [49] | Some concerns | Low | Some concerns | Low | Some concerns | Medium |
| Lopes et al., 2014 [50] | Low | Low | Low | Low | Low | Low |
| Lopes et al., 2016 [51] | Some concerns | Low | Low | Low | Some concerns | Medium |
| da Mota et al., 2016 [52] | Low | Low | Low | Some concerns | Some concerns | Medium |
| Pinto et al., 2016 [53] | Low | Low | Low | Low | Some concerns | Medium |
| Romero et al., 2021 [54] | Low | Low | Low | Low | Low | Low |
| Study | Assessment Method | Objectivity | Evidence Strength |
|---|---|---|---|
| Alshahrani et al., 2020 [41] | Gas Chromatography | High | Strong |
| do Vale et al., 2021 [46] | Gas Chromatography | High | Strong |
| Ciarcia et al., 2019 [44] | Gas Chromatography + Microbiology | High | Strong |
| Gonçalves et al., 2020 [47] | Gas Chromatography | High | Strong |
| Lopes et al., 2014 [50] | Gas Chromatography | High | Strong |
| Lopes et al., 2016 [51] | Gas Chromatography + sulfide monitor | High | Strong |
| Romero et al., 2021 [54] | Gas Chromatography | High | Strong |
| da Mota et al., 2016 [52] | Gas Chromatography | High | Strong |
| Dereci et al., 2016 [45] | Halimeter (sulfur monitor) | Medium | Moderate |
| Krespi et al., 2021 [49] | Organoleptic + Halimeter | Medium | Moderate |
| Bruno et al., 2024 [43] | Organoleptic + Breath Alert™ | Medium | Moderate |
| Joseph et al., 2014 [48] | Microbiology + Questionnaire | Medium | Moderate |
| Pinto et al., 2016 [53] | Microbiology + Gas Chromatography | Medium | Moderate |
| Study | Laser Details |
|---|---|
| Alshahrani et al., 2020 [41] | Diode laser (660 nm), continuous mode, power density: 3527 mW/cm2, average radiant power: 100 mW, energy density: 317.43 J/cm2, beam spot size: 0.028 cm2. |
| Joseph et al., 2016 [42] | Diode laser (655 nm, 1 W, continuous wave), 60 s duration at 60 mW/cm2 intensity, methylene blue photosensitizer at 10 mg/mL concentration. |
| Bruno et al., 2024 [43] | Blue LED combined with 20% annatto-based dye (Bixa orellana extract). |
| Ciarcia et al., 2019 [44] | Red LED (660 nm), continuous wave, average radiant power: 400 mW, energy density: 93.5 J/cm2, radiant energy: 36 J, beam spot size: 0.38 cm2, irradiation duration: 90 s per point, 4 irradiated points. |
| Dereci et al., 2016 [45] | Er,Cr:YSGG laser (2.78 μm wavelength), 1.5 W, 30 Hz pulse rate, 11% air, 20% water, pulse duration: 140 µs, 360° firing tip (Waterlase MD, Biolase, Irvine, CA, USA). |
| do Vale et al., 2021 [46] | Diode laser (THERAPY XT-EC®, DMC, São Paulo, Brazil); 660 nm wavelength; 0.005% methylene blue photosensitizer; irradiation at 6 points. |
| Gonçalves et al., 2020 [47] | Blue-violet LED (395–480 nm), energy: 9.6 J, radiant energy: 6.37 J/cm2 per point, irradiated six points on tongue dorsum with 20 s duration per point, 20% annatto-based extract. |
| Joseph et al., 2014 [48] | Diode laser (655 nm, 1 W, continuous wave), 60 s duration at 60 mW/cm2 intensity, methylene blue photosensitizer at 10 mg/mL concentration. |
| Krespi et al., 2021 [49] | Er,Cr:YSGG solid-state laser with pulsed water specifically for targeting oral biofilms. |
| Lopes et al., 2014 [50] | THERAPY XT-ES™; 660 nm wavelength; 100 mW power; continuous wave; fluence of 320 J/cm2; irradiance of 3537 mW/cm2; 9 J per point; 90 s exposure per point. |
| Lopes et al., 2016 [51] | THERAPY XT-EC® (DMC ABC Equipamentos Médicos e Odontológicos, SP, Brazil); red diode laser; 660 nm wavelength; 0.005% methylene blue photosensitizer; direct contact method; irradiation of 6 sites. |
| da Mota et al., 2016 [52] | THERAPY XT-EC® (DMC ABC Equipamentos Médicos e Odontológicos, São Paulo, Brazil); red diode laser; 660 nm wavelength; 100 mW output power; fluence 320 J/cm2; irradiance 3537 mW/cm2; energy 9 J per point; direct contact; irradiation at 6 points. |
| Pinto et al., 2016 [53] | Red diode laser (660 nm); methylene blue photosensitizer; combined with scaling and root planing. |
| Romero et al., 2021 [54] | Diode laser (THERAPY XT-EC®, DMC, São Paulo, Brazil); 660 nm wavelength; 100 mW power; fluence 318 J/cm2; irradiance 3537 mW/cm2; energy 9 J per point; irradiations at 6 points. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wiench, R.; Fiegler-Rudol, J.; Zięba, N.; Misiołek, M. Laser Interventions for Intraoral Halitosis: A Systematic Review of Randomized Controlled Trials. Pharmaceutics 2025, 17, 1046. https://doi.org/10.3390/pharmaceutics17081046
Wiench R, Fiegler-Rudol J, Zięba N, Misiołek M. Laser Interventions for Intraoral Halitosis: A Systematic Review of Randomized Controlled Trials. Pharmaceutics. 2025; 17(8):1046. https://doi.org/10.3390/pharmaceutics17081046
Chicago/Turabian StyleWiench, Rafał, Jakub Fiegler-Rudol, Natalia Zięba, and Maciej Misiołek. 2025. "Laser Interventions for Intraoral Halitosis: A Systematic Review of Randomized Controlled Trials" Pharmaceutics 17, no. 8: 1046. https://doi.org/10.3390/pharmaceutics17081046
APA StyleWiench, R., Fiegler-Rudol, J., Zięba, N., & Misiołek, M. (2025). Laser Interventions for Intraoral Halitosis: A Systematic Review of Randomized Controlled Trials. Pharmaceutics, 17(8), 1046. https://doi.org/10.3390/pharmaceutics17081046







