Safety and Immunogenicity of a Stable, Cold-Adapted, Temperature-Sensitive/Conditional Lethal Enterovirus A71 in Monkey Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Generation and Characterization of Temperature-Sensitive/Conditional Lethal EV-A71
2.1.1. Cell, Virus and Cold-Adaption Process
2.1.2. Virus Titration
2.1.3. Temperature-Sensitivity Phenotype Assay
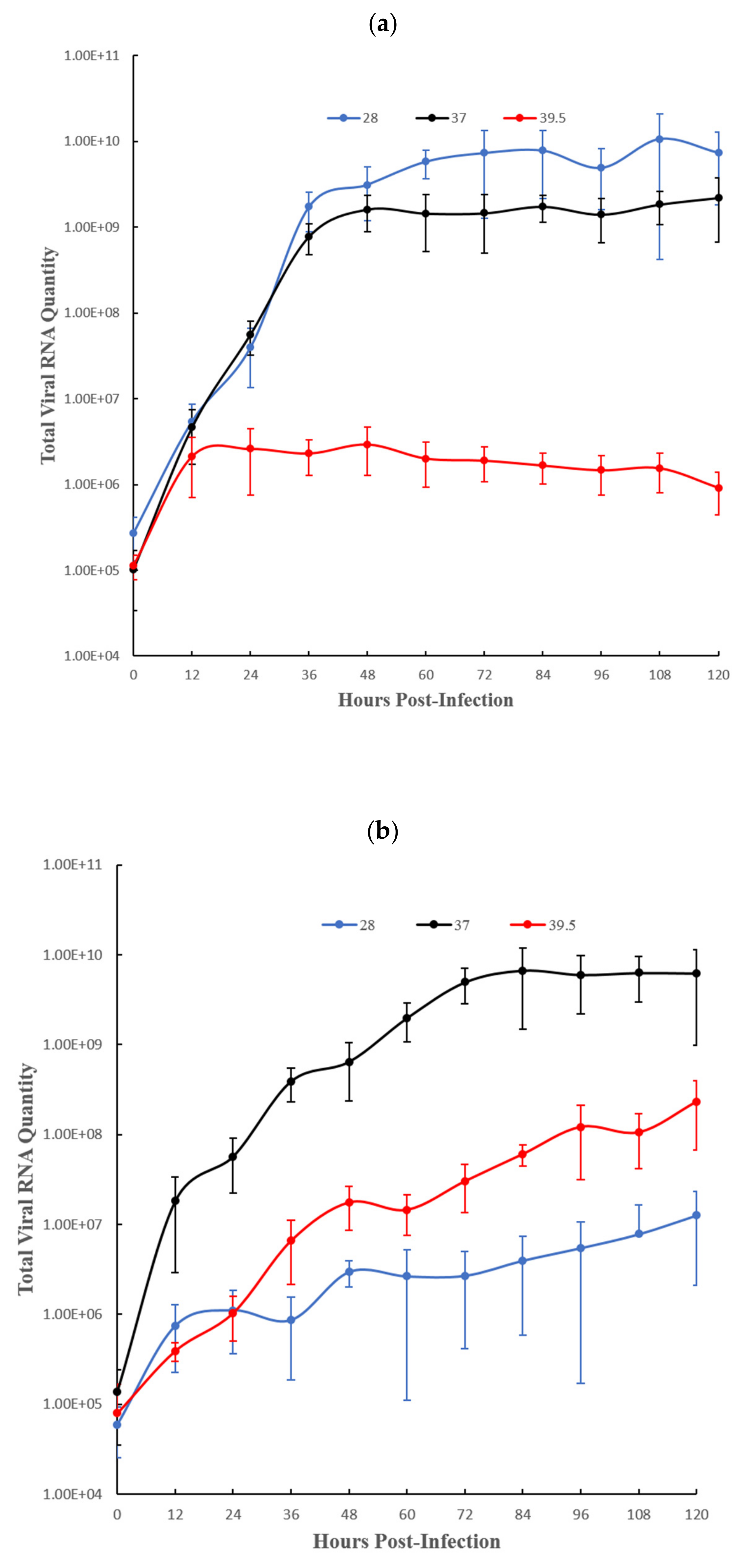
2.1.4. Virus Growth Kinetics by Total Viral RNA Quantity in the Culture Supernatant
2.1.5. Genetic Stability and Temperature Sensitivity Reversion Assay
2.1.6. RNA Extraction, RT-PCR and Sequencing
2.1.7. Molecular Cloning and Sequencing of Ambiguous Sequences
2.2. Monkey Study
2.2.1. Histology and Immunohistochemistry
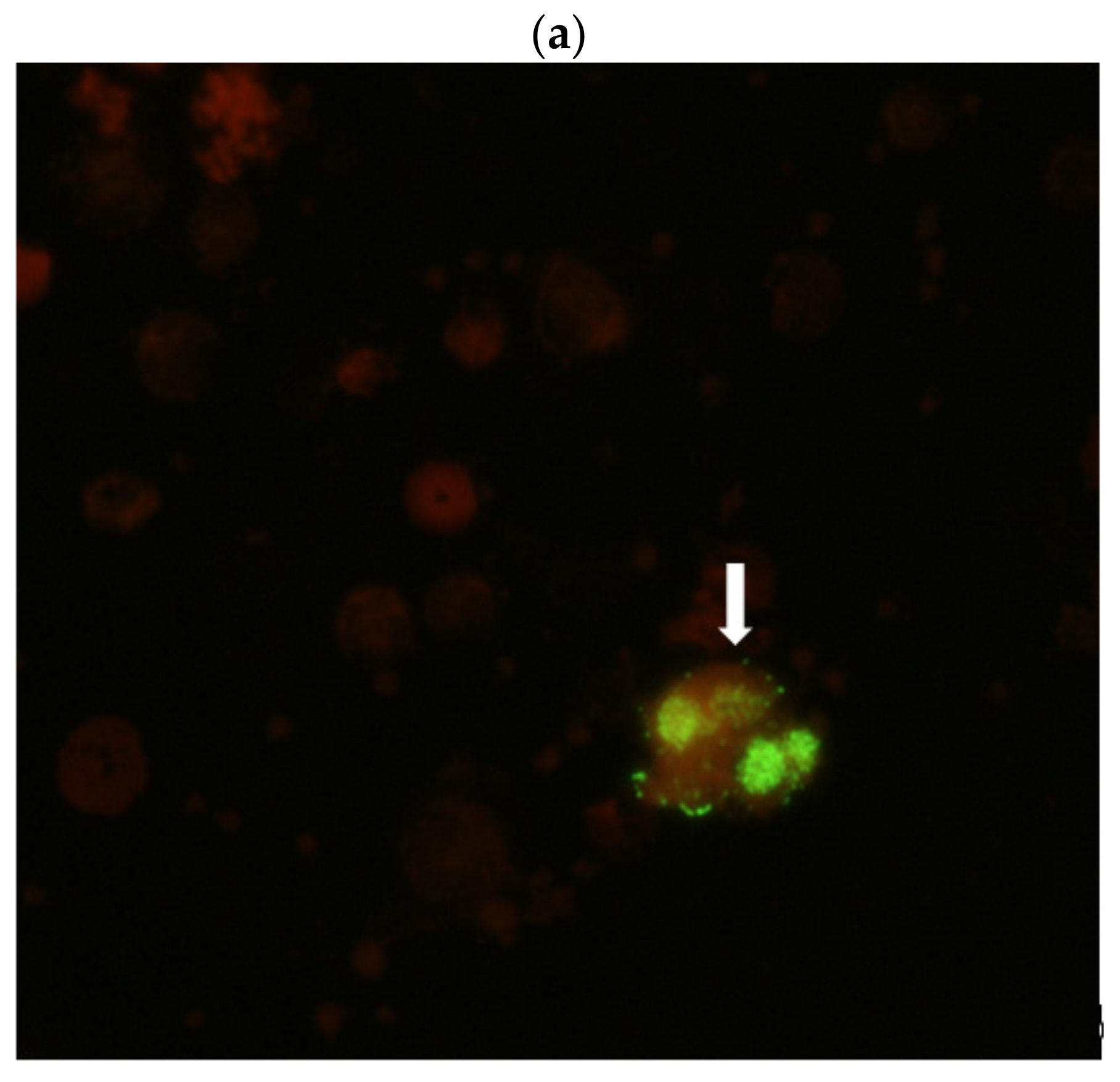
2.2.2. Antigen Detection and Virus Isolation from Monkey Specimens
2.2.3. Molecular Detection and Complete Genome Sequencing of Monkey Specimens
2.2.4. Serum Binding and Neutralizing Antibodies Assay
3. Results
3.1. Virus Phenotypic and Genotypic Characteristics in Cells
3.2. Monkey Study
3.2.1. Clinical Findings
3.2.2. Autopsy and Histological Findings
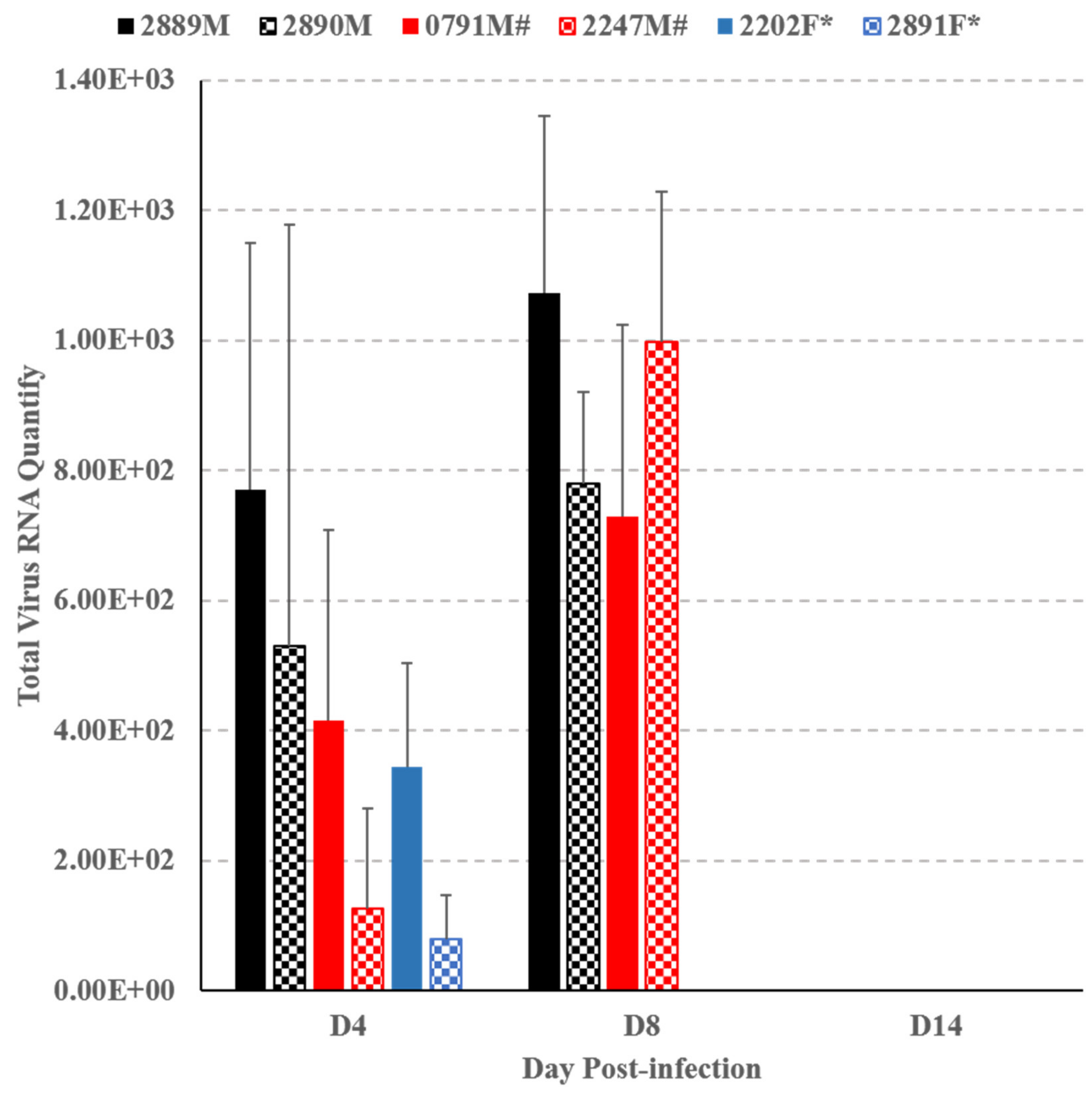
3.2.3. Virological Investigations
3.2.4. Monkeys’ Humoral Immune Response
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Alexander, J.P.; Baden, L.; Pallansch, M.A.; Anderson, L.J. Enterovirus 71 Infections and Neurologic Disease—United States, 1977–1991. J. Infect. Dis. 1994, 169, 905–908. [Google Scholar] [CrossRef] [PubMed]
- Melnick, J.L. Enteroviruses: Polioviruses, Coxsackieviruses, Echoviruses, and Newer Enteroviruses. In Fields Virology, 3rd ed.; Fields, B.N., Knipe, D.M., Howley, P.M., Eds.; Lippincott-Raven: Philadelphia, PA, USA, 1996; pp. 655–712. [Google Scholar]
- Blomberg, J.; Lycke, E.; Ahlfors, K.; Johnsson, T.; Wolontis, S.; Von Zeipel, G. New enterovirus type associated with epidemic of aseptic meningitis and/or hand, foot, and mouth disease. Lancet 1974, 304, 112. [Google Scholar] [CrossRef]
- Bible, J.M.; Iturriza-Gomara, M.; Megson, B.; Brown, D.; Pantelidis, P.; Earl, P.; Bendig, J.; Tong, C.Y.W. Molecular epidemiology of human entrovirus 71 in the United Kingdom from 1998 to 2006. J. Clin. Microbiol. 2008, 46, 3192–3200. [Google Scholar] [CrossRef] [PubMed]
- Brown, B.A.; Oberste, M.S.; Alexander, J.P., Jr.; Kennett, M.L.; Pallansch, M.A. Molecular epidemiology and evolution of enterovirus 71 strains isolated from 1970 to 1998. J. Virol. 1999, 73, 9969–9975. [Google Scholar] [CrossRef]
- Bessaud, M.; Razafindratsimandresy, R.; Nougairède, A.; Joffret, M.-L.; Deshpande, J.M.; Dubot-Pérès, A.; Héraud, J.-M.; De Lamballerie, X.; Delpeyroux, F.; Bailly, J.-L. Molecular Comparison and Evolutionary Analyses of VP1 Nucleotide Sequences of New African Human Enterovirus 71 Isolates Reveal a Wide Genetic Diversity. PLoS ONE 2014, 9, e90624. [Google Scholar] [CrossRef]
- Saxena, V.K.; Sane, S.; Nadkarni, S.S.; Sharma, D.K.; Deshpande, J.M. Genetic diversity of enterovirus A71, India. Emerg. Infect. Dis. 2015, 21, 123–126. [Google Scholar] [CrossRef]
- Chumakov, M.; Voroshilova, M.; Shindarov, L.; Lavrova, I.; Gracheva, L.; Koroleva, G.; Vasilenko, S.; Brodvarova, I.; Nikolova, M.; Gyurova, S.; et al. Enterovirus 71 isolated from cases of epidemic poliomyelitis-like disease in Bulgaria. Arch. Virol. 1979, 60, 329–340. [Google Scholar] [CrossRef]
- Shindarov, L.M.; Chumakov, M.P.; Voroshilova, M.K.; Bojinov, S.; Vasilenko, S.M.; Iordanov, I.; Kirov, I.D.; Kamenov, E.; Leshchinskaya, E.V.; Mitov, G.; et al. Epidemiological, clinical, and pathomorphological characteristics of epidemic poliomyelitis-like disease caused by enterovirus 71. J. Hyg. Epidemiol. Microbiol. Immunol. 1979, 23, 284–295. [Google Scholar]
- Nagy, G.; Takátsy, S.; Kukán, E.; Mihály, I.; Dömök, I. Virological diagnosis of enterovirus type 71 infections: Experiences gained during an epidemic of acute CNS diseases in Hungary in 1978. Arch. Virol. 1982, 71, 217–227. [Google Scholar] [CrossRef]
- Kennett, M.L.; Birch, C.J.; Lewis, F.A.; Yung, A.P.; Locarnini, S.A.; Gust, I.D. Enterovirus type 71 infection in Melbourne. Bull. EHO 1974, 51, 609–615. [Google Scholar]
- Deibel, R.; Gross, L.L.; Collins, D.N. Isolation of a New Enterovirus. Exp. Biol. Med. 1975, 148, 203–207. [Google Scholar] [CrossRef] [PubMed]
- Chonmaitree, T.; Menegus, M.A.; Schervish-Swierkosz, E.M.; Schwalenstocker, E. Enterovirus 71 infection: A Report of an outbreak with two cases of paralysis and a review of the literature. Pediatrics 1981, 67, 489–493. [Google Scholar]
- Samuda, G.M.; Chang, W.K.; Yeung, C.Y.; Tang, P.S. Monoplegia caused by enterovirus 71: An outbreak in Hong Kong. Pediatr. Infect. Dis. 1987, 6, 206–208. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, G.L.; Dickson, K.E.; Waters, M.-J.; Kennett, M.L.; Land, S.A.; Sneddon, M. Outbreak of enterovirus 71 infection in Victoria, Australia, with a high incidence of neurologic involvement. Pediatr. Infect. Dis. J. 1988, 7, 484–487. [Google Scholar] [CrossRef]
- Hayward, J.C.; Gillespie, S.M.; Kaplan, K.M.; Packer, R.; Pallansch, M.; Plotkin, S.; Schonberger, L.B. Outbreak of poliomyelitis-like paralysis associated with enterovirus 71. Pediatr. Infect. Dis. J. 1989, 8, 611–615. [Google Scholar] [CrossRef]
- Hagiwara, A.; Tagaya, I.; Yoneyama, T. Epidemic of Hand, Foot and Mouth Disease Associated with Enterovirus 71 Infection. Intervirology 1978, 9, 60–63. [Google Scholar] [CrossRef]
- Tagaya, I.; Takayama, R.; Hagiwara, A. A large scale epidemic of hand, foot, mouth disease associated with enterovirus 71 infection in Japan in 1978. Jpn. J. Med. Sci. Biol. 1981, 34, 191–196. [Google Scholar] [CrossRef]
- Ishimaru, Y.; Nakano, S.; Yamaoka, K.; Takami, S. Outbreaks of hand, foot, mouth disease by enterovirus 71. High incidence of complication disorders of central nervous system. Arch. Dis. Child. 1980, 55, 583–588. [Google Scholar] [CrossRef]
- Lum, L.C.S.; Lam, S.K.; Wong, K.T.; Chua, K.B.; Goh, A.Y.T. Neurologic pulmonary oedema and enterovirus 71 encephalomyelitis. Lancet 1998, 352, 1391. [Google Scholar] [CrossRef]
- Lum, L.C.S.; Wong, K.T.; Lam, S.K.; Chua, K.B.; Goh, A.Y.T.; Lim, W.L.; Ong, B.B.; Paul, G.; AbuBakar, S.; Lambert, M. Fatal Enterovirus 71 encephalitis. J. Pediatr. 1998, 133, 795–798. [Google Scholar] [CrossRef]
- Lin, T.-Y.; Chang, L.-Y.; Huang, Y.-C. Fulminant neurogenic pulmonary oedema with hand, foot, and mouth disease. Lancet 1998, 352, 367–368. [Google Scholar] [CrossRef]
- Yan, J.J.; Wang, J.R.; Liu, C.C.; Yang, H.B.; Su, I.J. An outbreak of enterovirus 71 infection in Taiwan 1998: A comprehensive pathological, virological, and molecular study on a case of fulminant encephalitis. J. Clin. Virol. 2000, 17, 13–22. [Google Scholar] [CrossRef]
- Liu, C.C.; Tseng, H.W.; Wang, S.M.; Wang, J.R.; Su, I.J. An outbreak of enteovirus 71 infection in Taiwan, 1998: Epidemiologic and clinical manifestations. J. Clin. Virol. 2000, 17, 23–30. [Google Scholar] [CrossRef]
- Wang, J.R.; Tsai, H.P.; Chen, P.F.; Lai, Y.J.; Yan, J.J.; Kiang, D.; Lin, K.H.; Liu, C.C.; Su, I.J. An outbreak of enteovirus 71 infection in Taiwan, 1998. II. Laboratory diagnosis and genetic analysis. J. Clin. Virol. 2000, 17, 91–99. [Google Scholar] [CrossRef]
- Chinese Center for Disease Control and Prevention; Office of the World Health Organization in China. Report on the Hand, Foot and Mouth Disease Outbreak in Fuyang City, Anhui Province and the Prevention and Control in China; World Health Organization: Beijing, China, 2008. [Google Scholar]
- Yang, F.; Zhng, T.; Hu, Y.; Wang, X.; Du, J.; Li YSun, S.; Sun, X.; Li, Z.; Jin, Q. Survey of enterovirus infections from hand, foot and mouth disease outbreak in China, 2009. Virol. J. 2011, 8, 508. [Google Scholar] [CrossRef]
- Zeng, M.; El Khatib, N.F.; Tu, S.; Ren, P.; Xu, S.; Zhu, Q.; Mo, X.; Pu, D.; Wang, X.; Altmeyer, R. Seroepidemiology of Enterovirus 71 infection prior to the 2011 season in children in Shanghai. J. Clin. Virol. 2012, 53, 285–289. [Google Scholar] [CrossRef]
- Wu, C.-N.; Lin, Y.-C.; Fann, C.; Liao, N.-S.; Shih, S.-R.; Ho, M.-S. Protection against lethal enterovirus 71 infection in newborn mice by passive immunization with subunit VP1 vaccines and inactivated virus. Vaccine 2001, 20, 895–904. [Google Scholar] [CrossRef]
- Chiu, C.-H.; Chu, C.; He, C.-C.; Lin, T.-Y. Protection of neonatal mice from lethal enterovirus 71 infection by maternal immunization with attenuated Salmonella enterica serovar Typhimurium expressing VP1 of enterovirus 71. Microbes Infect. 2006, 8, 1671–1678. [Google Scholar] [CrossRef]
- Tung, W.S.; Abu Bakar, S.; Sekawi, Z.; Rosli, R. DNA vaccine constructs against enterovirus 71 elicit immune response in mice. Genet. Vaccines Ther. 2007, 5, 6. [Google Scholar] [CrossRef]
- Chung, Y.-C.; Ho, M.-S.; Wu, J.-C.; Chen, W.-J.; Huang, J.-H.; Chou, S.-T.; Hu, Y.-C. Immunization with virus-like particles of enterovirus 71 elicits potent immune responses and protects mice against lethal challenge. Vaccine 2008, 26, 1855–1862. [Google Scholar] [CrossRef]
- Chen, H.-L.; Huang, J.-Y.; Chu, T.-W.; Tsai, T.-C.; Hung, C.-M.; Lin, C.-C.; Liu, F.-C.; Wang, L.-C.; Chen, Y.-J.; Lin, M.-F.; et al. Expression of VP1 protein in the milk of transgenic mice: A potential oral vaccine protects against enterovirus 71 infection. Vaccine 2008, 26, 2882–2889. [Google Scholar] [CrossRef]
- Ong, K.C.; Devi, S.; Cardosa, M.J.; Wong, K.T. Formaldehyde-Inactivated Whole-Virus Vaccine Protects a Murine Model of Enterovirus 71 Encephalomyelitis against Disease. J. Virol. 2010, 84, 661–665. [Google Scholar] [CrossRef]
- Chen, C.-W.; Lee, Y.-P.; Wang, Y.-F.; Yu, C.-K. Formaldehyde-inactivated human enterovirus 71 vaccine is compatible for co-immunization with a commercial pentavalent vaccine. Vaccine 2011, 29, 2772–2776. [Google Scholar] [CrossRef]
- Lee, M.-S.; Chang, L.-Y. Development of enterovirus 71 vaccines. Expert Rev. Vaccines 2010, 9, 149–156. [Google Scholar] [CrossRef]
- Zhang, D.; Lu, J.; Lu, J. Enterovirus 71 vaccine: Close but still far. Int. J. Infect. Dis. 2010, 14, e739–e743. [Google Scholar] [CrossRef] [PubMed]
- Sabin, A.B. Oral Poliovirus Vaccine: History of Its Development and Use and Current Challenge to Eliminate Poliomyelitis from the World. J. Infect. Dis. 1985, 151, 420–436. [Google Scholar] [CrossRef]
- Sutter, R.W.; Kew, O.M.; Cochi, S.L.; Aylward, R.B. Poliovirus vaccine-live. In Vaccines, 6th ed.; Plotkin, S.A., Orenstein, W.A., Offit, P.A., Eds.; Section 2; Elsevier Saunders: Philadelphia, PA, USA, 2012; Chapter 28; pp. 598–645. [Google Scholar]
- Chua, K.B.; Chua, B.H.; Lee, C.S.M.; Chem, Y.K.; Ismail, N.; Kiyu, A.; Kumarasamy, V. Genetic diversity of enterovirus 71 isolated from cases of hand, foot and mouth disease in the 1997, 2000 and 2005 outbreaks, Peninsular Malaysia. Malays. J. Pathol. 2007, 29, 69–78. [Google Scholar] [PubMed]
- Dougherty, R.M. Animal virus titration technique. In Techniques in Experimental Virology; Harris, R.J.C., Ed.; Academic Press: London, UK; New York, NY, USA, 1964; Chapter 6; pp. 169–224. [Google Scholar]
- Reed, L.J.; Muench, H. A simple method of estimating fifty percent endpoints. Am. J. Hyg. 1938, 27, 493–497. [Google Scholar]
- Tan, E.L.; Chow, V.T.K.; Kumarasinghe, G.; Lin, R.T.P.; Mackay, I.M.; Sloots, T.P.; Poh, C.L. Specific detection of enterovirus 71 directly from clinical specimens using real-time RT-PCR hybridization probe assay. Mol. Cell. Probes 2006, 20, 135–140. [Google Scholar] [CrossRef]
- Li, Z.; Yu, M.; Zhang, H.; Wang, H.-Y.; Wang, L.-F. Improved rapid amplification of cDNA ends (RACE) for mapping both the 5′ and 3′ terminal sequences of paramyxovirus genomes. J. Virol. Methods 2005, 130, 154–156. [Google Scholar] [CrossRef]
- Rice, P.; Longden, I.; Bleasby, A. EMBOSS: The European Molecular Biology Open Software Suite. Trends Genet. 2000, 16, 276–277. [Google Scholar] [CrossRef]
- Hall, T. BioEdit: A user-friendly biological sequence alignment editor and analysis programme for Windows 95/98/NT. Nucleic Acids Symp. Res. 1997, 41, 95–98. [Google Scholar]
- Zhou, Y.; Li, J.-X.; Jin, P.-F.; Wang, Y.-X.; Zhu, F.-C. Enterovirus 71: A whole virion inactivated enterovirus 71 vaccine. Expert Rev. Vaccines 2016, 15, 803–813. [Google Scholar] [CrossRef] [PubMed]
- McGoldrick, A.; Macadam, A.J.; Dunn, G.; Rowe, A.; Burlison, J.; Minor, P.D.; Meredith, J.; Evans, D.J.; Almond, J.W. Role of mutations G-480 and C-6203 in the attenuation phenotype of Sabin type 1 poliovirus. J. Virol. 1995, 69, 7601–7605. [Google Scholar] [CrossRef] [PubMed]
- Arita, M.; Ami, Y.; Wakita, T.; Shimizu, H. Cooperative Effect of the Attenuation Deterrminants Derived from Poliovirus 1 Strain Is Essential for Attenuation of Enterovirus 71 in the NOD/SCID Mouse Infection Model. J. Virol. 2008, 82, 1787–1795. [Google Scholar] [CrossRef]
- Hagiwara, A.; Yoneyama, T.; Hashimoto, I. Isolation of a Temperature-sensitive Strain of Enterovirus 71 with Reduced Neurovirulence for Monkeys. J. Gen. Virol. 1983, 64, 499–502. [Google Scholar] [CrossRef]
- Hashimoto, I.; Hagiwara, A. Comparative studies on the neurovirulence of temperature-sensitive and temperature-resistant viruses of enterovirus 71 in monkeys. Acta Neuropathol. 1983, 60, 266–270. [Google Scholar] [CrossRef]
- Arit, C.M.; Shimizu, H.; Nagata, N.; Ami, Y.; Suzaki, Y.; Sata, T.; Iwasaki, T.; Miyamura, T. Temperature-sensitive mutants of enterovirus 71 show attenuation in cynomolgus monkeys. J. Gen. Virol. 2005, 86, 1391–1401. [Google Scholar] [CrossRef]
- Christopher, U.T. Hellen and Eckard Wimmer. Enterovirus Genetics. In Human Enterovirus Infections; Rotbart, H.H., Ed.; ASM Press: Washington, DC, USA, 2005; Chapter 2; pp. 25–72. [Google Scholar]
- Johnsonand, K.L.; Sarnow, P. Viral RNA Synthesis. In Human Enterovirus Infections; Rotbart, H.H., Ed.; ASM Press: Washington, DC, USA, 2005; Chapter 4; pp. 95–112. [Google Scholar]
- Sanders, B.P.; de Los Rios Oakes, I.; van Hoek, V.; Bockstal, V.; Kamphuis, T.; Uil, T.G.; Song, Y.; Cooper, G.; Crawt, L.E.; Martín, J.; et al. Cold-adapted viral attenuation (CAVA): Highly temperature sensitive polioviruses as novel vaccine strains for a next generation inactivated poliovirus vaccine. PLoS Pathog. 2016. [Google Scholar] [CrossRef]
- Hallerand, A.A.; Semler, B.L. Translation and Host Cell Shutoff. In Human Enterovirus Infections; Rotbart, H.H., Ed.; ASM Press: Washington, DC, USA, 2005; Chapter 5; pp. 113–133. [Google Scholar]
- Domingo, E.; Sheldon, J.; Perales, C. Viral Quasispecies Evolution. Microbiol. Mol. Biol. Rev. 2012, 76, 159–216. [Google Scholar] [CrossRef]
- Lauring, A.S.; Andino, R. Quasispecies Theory and the Behavior of RNA Viruses. PLoS Pathog. 2010, 6, e1001005. [Google Scholar] [CrossRef] [PubMed]


| Viral Gene Region/Protein | EV71:TLLα | EV71:TLLαP20 | |||
|---|---|---|---|---|---|
| NT | AA | NT | AA | ||
| 5′-UTR | “Cloverleaf” | ||||
| (1–747) | IRES | 1 | 2 | ||
| P1 | VP4 | 2 | 1 | 3 | 1 |
| (748–3333) | VP2 | 2 | 2 | 2 | 2 |
| VP3 | 2 | 2 | 3 | 3 | |
| VP1 | 2 | 2 | 4 | 3 | |
| P2 | 2A | 2 | 2 | 4 | 3 |
| (3334–5067) | 2B | 1 | 1 | ||
| 2C | 2 | 1 | 2 | 1 | |
| P3 | 3A | 1 | 1 | ||
| (5068–7326) | 3B | ||||
| 3C | 1 | 1 | 1 | 1 | |
| 3D | 3 | 1 | 3 | 1 | |
| 3′-UTR | |||||
| (7327–7412) | |||||
| Total | 18 | 12 | 26 | 16 | |
| Viral Gene Region/Protein | EV71:TLLβ | EV71:TLLβP20 | EV71:TLLβP40 | ||||
|---|---|---|---|---|---|---|---|
| NT | AA | NT | AA | NT | AA | ||
| 5′-UTR | “Cloverleaf” | 2 | 1 | 2 | |||
| (1–746) | IRES | 2 | 2 | 3 | |||
| P1 | VP4 | 1 | |||||
| (747–3332) | VP2 | 4 | 4 | 4 | |||
| VP3 | 2 | 2 | 2 | 2 | 2 | 2 | |
| VP1 | 9 | 8 | 8 | 8 | 8 | 8 | |
| P2 | 2A | 4 | 2 | 4 | 2 | 4 | 2 |
| (3333–5066) | 2B | 1 | 1 | 1 | 1 | 1 | 1 |
| 2C | 2 | 3 | 3 | ||||
| P3 | 3A | 1 | 1 | 1 | 1 | 1 | 1 |
| (5067–7325) | 3B | ||||||
| 3C | 2 | 2 | 2 | 2 | 2 | 2 | |
| 3D | 2 | 2 | 2 | 2 | 2 | 2 | |
| 3′-UTR | 1 | 1 | 1 | ||||
| (7326–7411) | |||||||
| Total | 31 | 18 | 30 | 18 | 33 | 18 | |
| Monkey | IgM titre | IgG titre | ||
|---|---|---|---|---|
| Day 14 PI | Day 30 PI | Day 14 PI | Day 30 PI | |
| 2889M | 1:20 | 1:10 | 1:160 | 1:320 |
| 2890M | 1:40 | 1:40 | 1:160 | 1:640 |
| EV71 Genotype | Monkey | |||
|---|---|---|---|---|
| 2889M | 2890M | |||
| Day 14 PI | Day 30 PI | Day 14 PI | Day 30 PI | |
| A (BrCr) | 1:20 | 1:40 | 1:40 | 1:80 |
| B3 | 1:160 | 1:640 | 1:160 | 1:640 |
| B4 | 1:160 | 1:640 | 1:160 | 1:320 |
| B5 | 1:80 | 1:320 | 1:160 | 1:320–640 |
| C1 | 1:40 | 1:160 | 1:40 | 1:160 |
| C5 | 1:20 | 1:40 | 1:20 | 1:40 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chua, K.B.; Ng, Q.; Meng, T.; Jia, Q. Safety and Immunogenicity of a Stable, Cold-Adapted, Temperature-Sensitive/Conditional Lethal Enterovirus A71 in Monkey Study. Viruses 2021, 13, 438. https://doi.org/10.3390/v13030438
Chua KB, Ng Q, Meng T, Jia Q. Safety and Immunogenicity of a Stable, Cold-Adapted, Temperature-Sensitive/Conditional Lethal Enterovirus A71 in Monkey Study. Viruses. 2021; 13(3):438. https://doi.org/10.3390/v13030438
Chicago/Turabian StyleChua, Kaw Bing, Qimei Ng, Tao Meng, and Qiang Jia. 2021. "Safety and Immunogenicity of a Stable, Cold-Adapted, Temperature-Sensitive/Conditional Lethal Enterovirus A71 in Monkey Study" Viruses 13, no. 3: 438. https://doi.org/10.3390/v13030438
APA StyleChua, K. B., Ng, Q., Meng, T., & Jia, Q. (2021). Safety and Immunogenicity of a Stable, Cold-Adapted, Temperature-Sensitive/Conditional Lethal Enterovirus A71 in Monkey Study. Viruses, 13(3), 438. https://doi.org/10.3390/v13030438






