Computational Analysis of Mechanical Performance for Composite Polymer Biodegradable Stents
Abstract
:1. Introduction
2. Materials and Methods
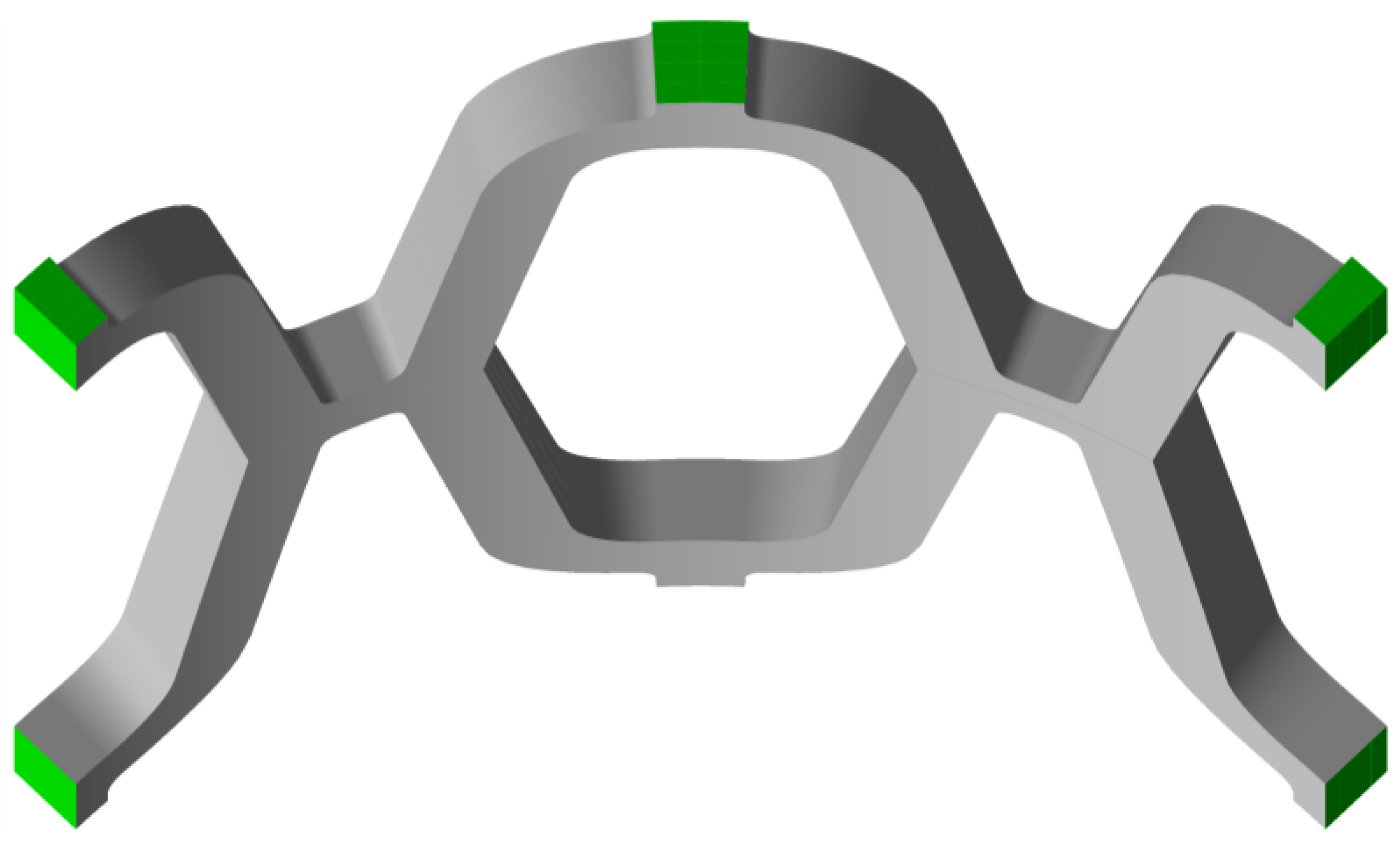
2.1. Modelling and Simulation
2.2. Radial Elastic Recoil and Foreshortening
3. Results
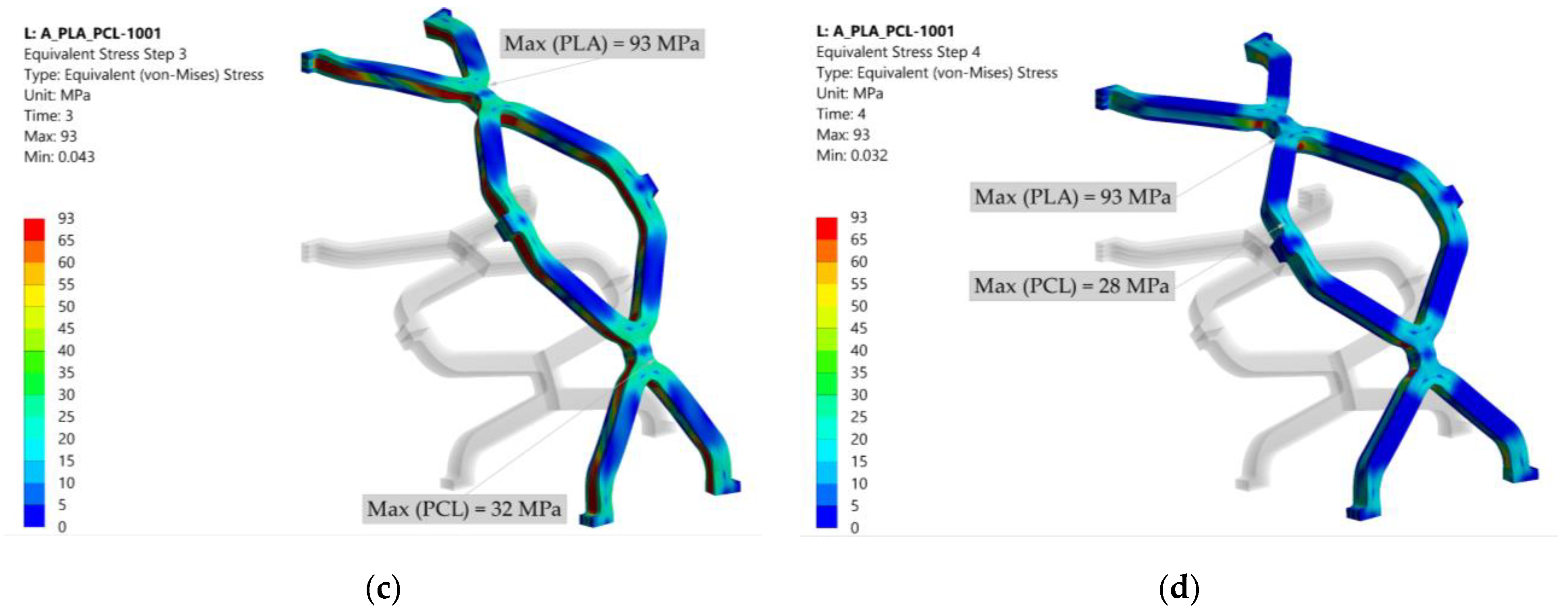
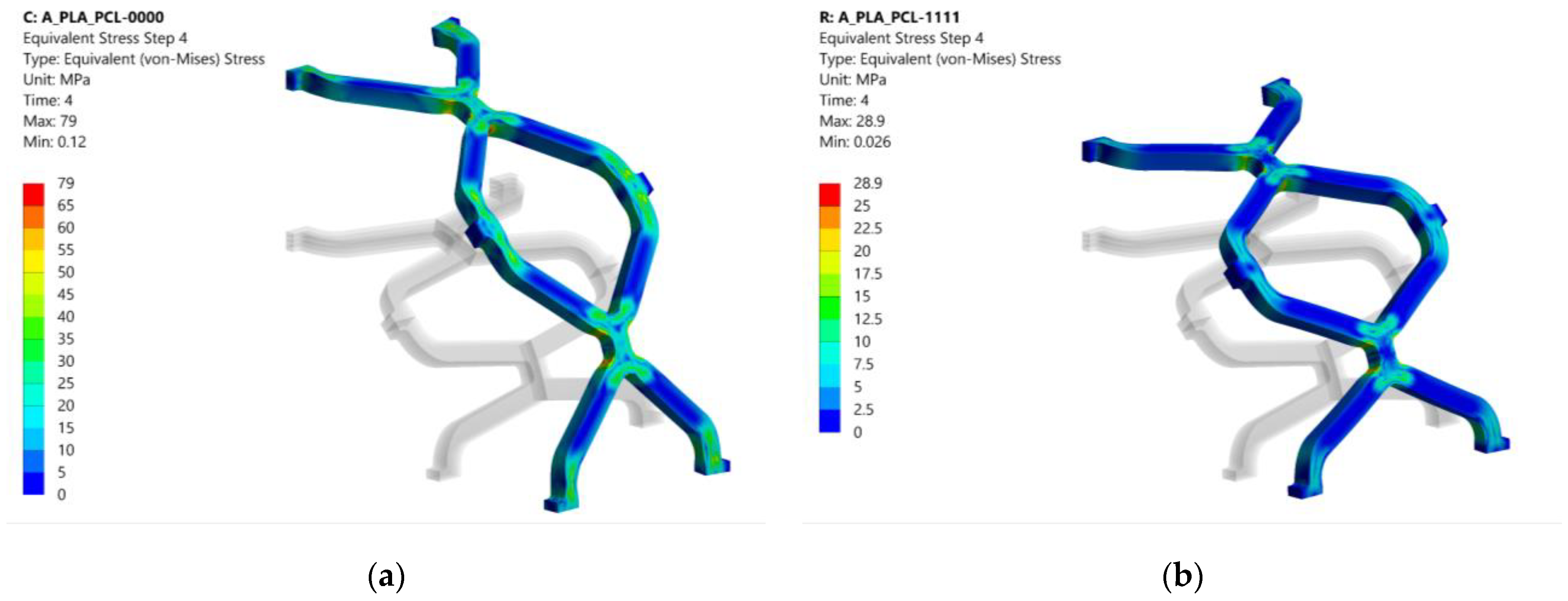
3.1. Equivalent Stress
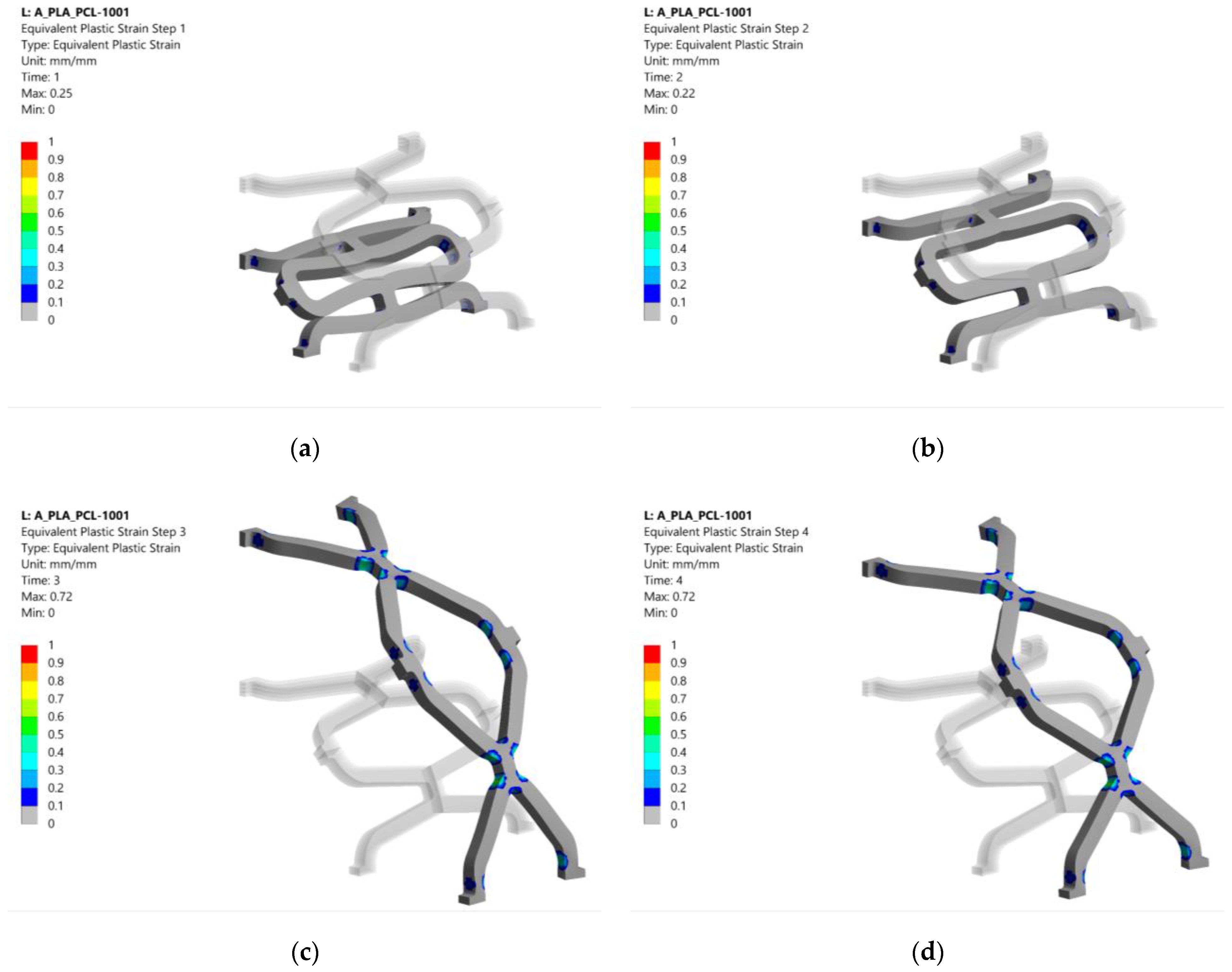
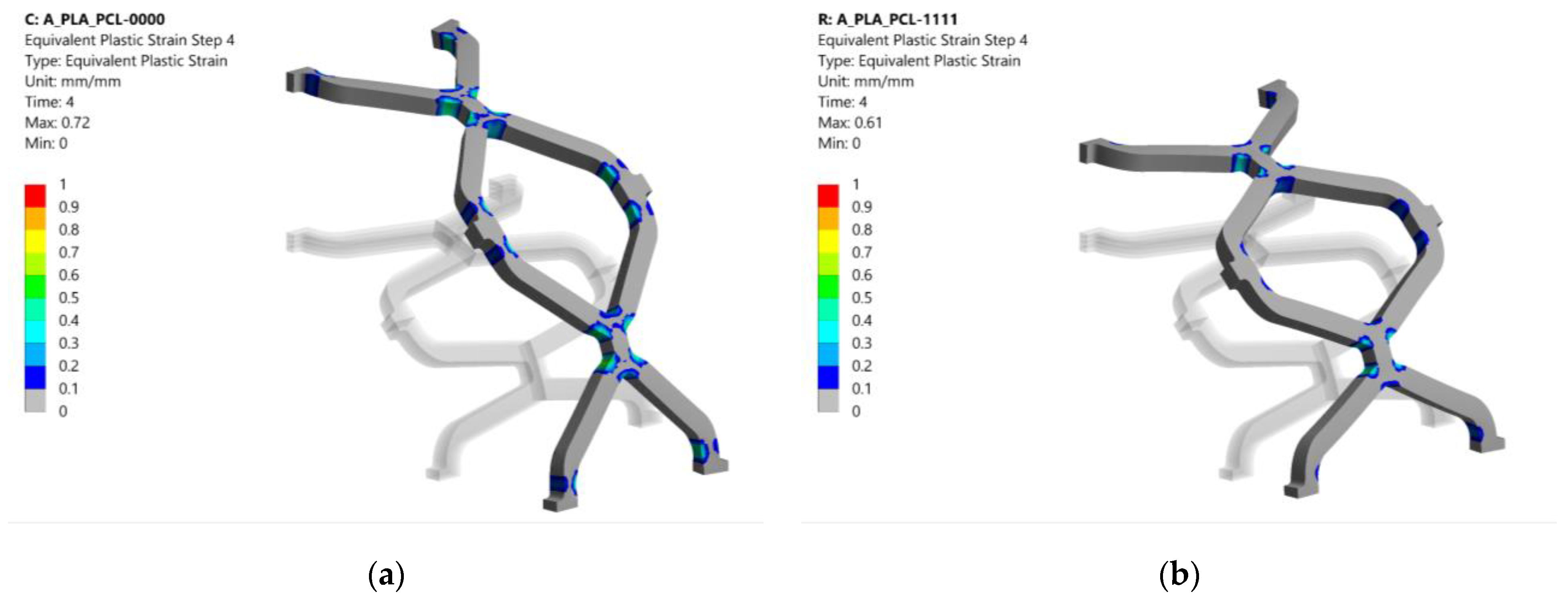
3.2. Equivalent Plastic Strain
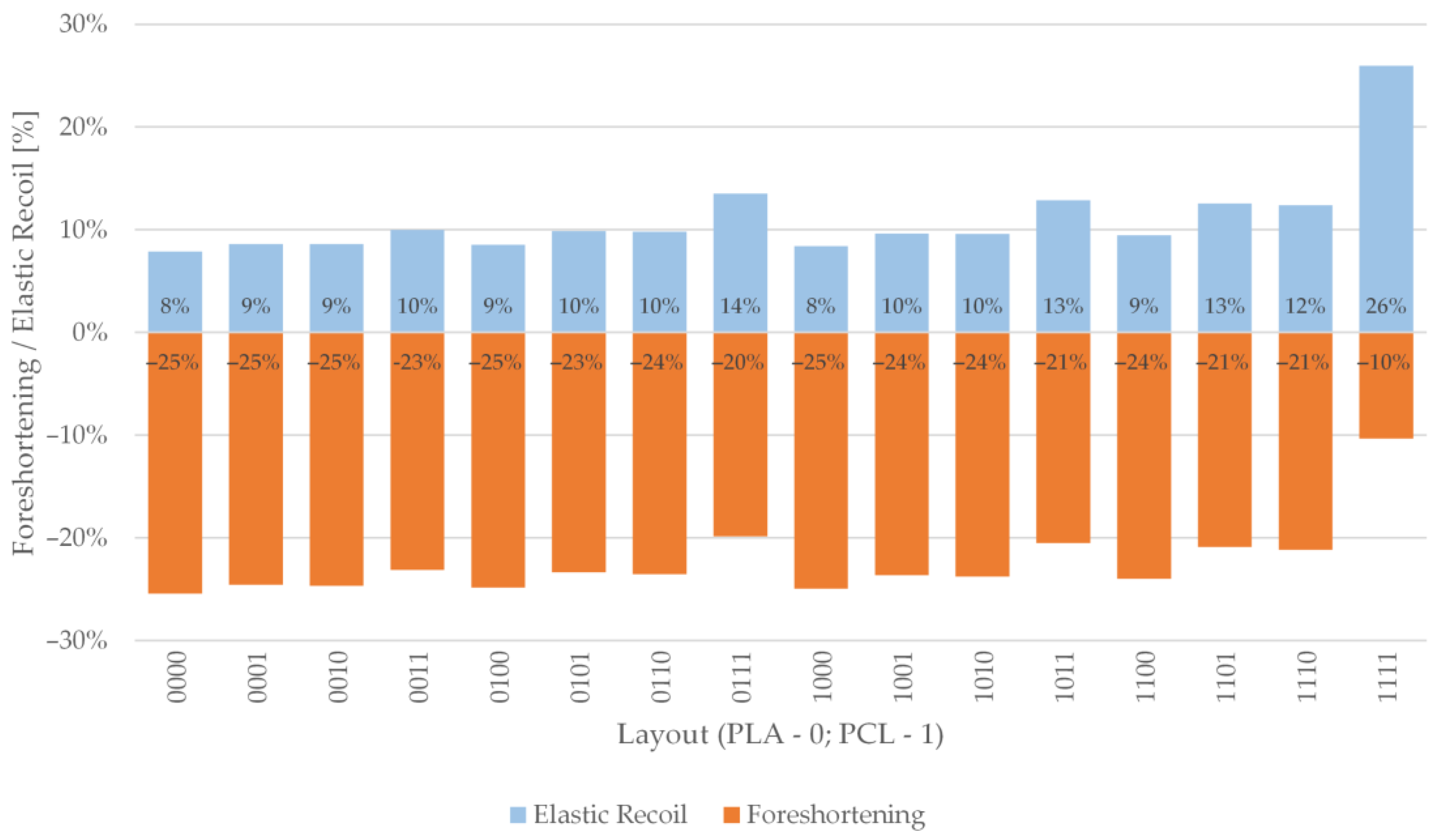
3.3. Radial Elastic Recoil and Foreshortening
4. Discussion
5. Conclusions
- The structures with the same number of layers per material show similar stress, plastic strain, foreshortening and elastic recoil.
- The order of layers only impacts plastic strains for configurations with three PCL layers and a single PLA layer. In other configurations, the layer arrangement does not play a significant role.
- The volumetric ratio of elements has a more significant influence on stent foreshortening and elastic recoil than layer arrangement.
- A combination of different materials in a composite stent could be useful for customizing mechanical properties along the length of the stent. Matching the compliance of the stent and the blood vessel could lower the risk of short-term complications after stent deployment.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mccormick, C. Overview of cardiovascular stent designs. In Functionalised Cardiovascular Stents; Woodhead Publishing: San Diego, CA, USA, 2018; pp. 3–26. [Google Scholar] [CrossRef]
- Grogan, J.A.; Leen, S.B.; Mchugh, P.E. Comparing coronary stent material performance on a common geometric platform through simulated bench testing. J. Mech. Behav. Biomed. Mater. 2012, 12, 129–138. [Google Scholar] [CrossRef] [Green Version]
- Mani, G.; Feldman, M.D.; Patel, D.; Agrawal, C.M. Coronary stents: A materials perspective. Biomaterials 2007, 28, 1689–1710. [Google Scholar] [CrossRef]
- Hu, T.; Yang., C.; Lin, S.; Yu, Q.; Wang, G. Biodegradable stents for coronary artery disease treatment: Recent advances and future perspectives. Mater. Sci. Eng. 2018, C91, 163–178. [Google Scholar] [CrossRef]
- Waksman, R. Promise and challenges of bioabsorbable stents. Catheter. Cardiovasc. Interv. 2007, 70, 407–414. [Google Scholar] [CrossRef]
- Polanec, B.; Kramberger, J.; Glodež, S. A review of production technologies and materials for manufacturing of cardiovascular stents. Adv. Prod. Eng. Manag. 2020, 15, 390–402. [Google Scholar] [CrossRef]
- Beshchasna, N.; Saqib, M.; Kraskiewicz, H.; Wasyluk, Ł.; Kuzmin, O.; Duta, O.C.; Ficai, D.; Ghizdavet, Z.; Marin, A.; Ficai, A.; et al. Recent Advances in Manufacturing Innovative Stents. Pharmaceutics 2020, 12, 349. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grabow, N.; Schlun, M.; Sternberg, K.; Hakansson, N.; Kramer, S.; Schmitz, K.P. Mechanical properties of laser cut poly (L-lactide) micro-specimens: Implications for stent design, manufacture, and sterilization. J. Biomech. Eng. 2005, 127, 25–31. [Google Scholar] [CrossRef]
- Grabow, N.; Martin, H.; Schmitz, K.P. The impact of material characteristics on the mechanical properties of a poly(l-lactide) coronary stent. Biomech. Tech. 2002, 47, 503–505. [Google Scholar] [CrossRef] [PubMed]
- Welch, T.R.; Eberhart, R.C.; Reddy, S.V.; Wang, J.; Nugent, A.; Forbes, J. Novel Bioresorbable Stent Design and Fabrication: Congenital Heart Disease Applications. Cardiovasc. Eng. Technol. 2013, 4, 171–182. [Google Scholar] [CrossRef]
- Pauck, R.; Reddy, B. Computational analysis of the radial mechanical performance of PLLA coronary artery stents. Med. Eng. Phys. 2015, 37, 7–12. [Google Scholar] [CrossRef] [PubMed]
- De Beule, M. Finite Element Stent Design. Ph.D. Thesis, University of Gent, Ghent, Belgium, 2008. [Google Scholar]
- Guerra, A.J.; Ciurana, J. Fibre laser cutting of polymer tubes for stents manufacturing. Procedia Manuf. 2017, 13, 190–196. [Google Scholar] [CrossRef]
- Choudhury, I.A.; Shirley, S. Laser cutting of polymeric materials: An experimental investigation. Opt. Laser Technol. 2010, 42, 503–508. [Google Scholar] [CrossRef]
- Guerra, A.J.; Roca, A.; Ciurana, J. A novel 3D additive manufacturing machine to biodegradable stents. Procedia Manuf. 2017, 13, 718–723. [Google Scholar] [CrossRef]
- Guerra, A.J.; Ciurana, J. 3D-printed bioabsordable polycaprolactone stent: The effect of process parameters on its physical features. Mater. Des. 2018, 137, 430–437. [Google Scholar] [CrossRef]
- Guerra, A.J.; San, J.; Ciurana, J. Fabrication of PCL/PLA Composite Tube for Stent Manufacturing. Procedia CIRP 2017, 65, 231–235. [Google Scholar] [CrossRef]
- Carneiro, O.S.; Silva, A.F.; Gomes, R. Fused deposition modelling with polypropylene. Mater. Des. 2015, 83, 768–776. [Google Scholar] [CrossRef]
- Schiavone, A.; Qui, T.Y.; Zhao, L.G. Crimping and deployment of metallic and polymeric stents—Finite element modelling. Vessel Plus. 2017, 1, 12–21. [Google Scholar] [CrossRef] [Green Version]
- Wang, Q.; Fang, G.; Zhao, Y.; Wang, G.; Cai, T. Computational and experimental investigation into mechanical performances of Poly-L-Lactide Acid (PLLA) coronary stents. J. Mech. Behav. Biomed. Mater. 2017, 65, 415–427. [Google Scholar] [CrossRef] [Green Version]
- Migliavacca, F.; Petrini, L.; Colombo, M.; Auricchio, F.; Pietrabissa, R. Mechanical Behavior of Coronary Stents Investigated Through the Finite Element Method. J. Biomech. 2002, 35, 803–811. [Google Scholar] [CrossRef]
- Migliavacca, F.; Petrini, L.; Montanari, V.; Quagliana, I.; Auricchio, F.; Dubini, G. A predictive study of the mechanical behaviour of coronary stents by computer modelling. Med. Eng. Phys. 2005, 27, 13–18. [Google Scholar] [CrossRef]
- Etave, F.; Finet, M.; Boivin, M.; Boyer, J.C.; Rioufol, G.; Thollet, G. Mechanical properties of coronary stents determined by using finite element analysis. J. Biomech. 2001, 34, 1065–1075. [Google Scholar] [CrossRef]
- Pant, S.; Bressloff, N.; Limbert, G. Geometry parameterization and multidisciplinary constrained optimization of coronary stents. Biomech. Model. Mechanobiol. 2012, 11, 61–82. [Google Scholar] [CrossRef] [PubMed]
- Jerold John Britto, J.; Venkatesh, R.; Prabhakaran, R.; Amudhan, K. Design optimization of biomedical stent under the influence of the radial pressure using FEM. Mater. Today 2020, in press. [Google Scholar] [CrossRef]
- Wei, Y.; Wang, M.; Zhao, D.; Li, H.; Jin, Y. Structural Design of Mechanical Property for Biodegradable Stent. Adv. Mater. Sci. Eng. 2019, 2019, 2960435. [Google Scholar] [CrossRef] [Green Version]
- Liu, R.; Mcginty, S.; Cui, F.; Luo, X.; Liu, Z. Modelling and simulation of the expansion of a shape memory polymer stent. Eng. Comput. 2019, 36, 2726–2746. [Google Scholar] [CrossRef]
- Liu, R.; Xu, S.; Luo, X.; Liu, Z. Theoretical and Numerical Analysis of Mechanical Behaviors of a Metamaterial-Based Shape Memory Polymer Stent. Polymers 2020, 12, 1784. [Google Scholar] [CrossRef]
- Yu, X.; Zhou, J.; Lianf, H.; Jiang, Z.; Wu, L. Mechanical metamaterials associated with stiffness, rigidity and compressibility: A brief review. Prog. Mater. Sci. 2018, 94, 114–173. [Google Scholar] [CrossRef]
- Khosravi, A.; Bahreinizad, H.; Bani, M.S.; Karimi, A. A numerical study on the application of the functionally graded materials in the stent design. Mater. Sci. Eng. 2017, C73, 182–188. [Google Scholar] [CrossRef]
- De Beule, M.; Mortier, P.; Carlier, G.; Verhegghe, B.; Van Impe, R.; Verdonck, P. Realistic finite element-based stent design: The impact of balloon folding. J. Biomech. 2008, 41, 383–389. [Google Scholar] [CrossRef] [PubMed]
- Debusschere, N.; Segers, P.; Dubruel, P.; Verhegghe, B.; De Beule, M. A finite element strategy to investigate the free expansion behaviour of a biodegradable polymeric stent. J. Biomech. 2015, 48, 2012–2018. [Google Scholar] [CrossRef] [PubMed]
- Mortier, P.; De Beule, M.; Segers, P.; Verdonck, P.; Verhegghe, B. Virtual bench testing of new generation coronary stents. EuroIntervention. 2011, 7, 369–376. [Google Scholar] [CrossRef] [Green Version]
- Ju, F.; Xia, Z.; Sasaki, K. On the finite element modelling of balloon-expandable stents. J. Mech. Behav. Biomed. Mater. 2008, 1, 86–95. [Google Scholar] [CrossRef]
- Cabrera, M.M.; Sanders, B.; Goor, O.J.G.M.; Driessen-Mol, A.; Oomens, C.W.J.; Baaijens, F.P.T. Computationally designed 3D printed self-expandable polymer stents with biodegradation capacity for minimally invasive heart valve implantation: A proof-of-concept study. 3D Print. Addit. Manuf. 2017, 4, 19–29. [Google Scholar] [CrossRef]
- Qiu, T.Y.; Song, M.; Zhao, L.G. A computational study of crimping and expansion of bioresorbable polymeric stents. Mech. Time-Depend. Mater. 2018, 22, 273–290. [Google Scholar] [CrossRef] [Green Version]
- Qiu, T.Y.; Zhao, L.G.; Song, M.A. Computational Study of Mechanical Performance of Bioresorbable Polymeric Stents with Design Variations. Cardiovasc. Eng. Tech. 2019, 10, 46–60. [Google Scholar] [CrossRef] [Green Version]
- Bobel, A.C.; Petisco, S.; Sarasua, J.R.; Wang, W.; McHugh, P.E. Computational Bench Testing to Evaluate the Short-Term Mechanical Performance of a Polymeric Stent. Cardiovasc. Eng. Tech. 2015, 6, 519–532. [Google Scholar] [CrossRef]
- Muliana, A.; Rajagopal, K.R. Modeling the response of nonlinear viscoelastic biodegradable polymeric stents. Int. J. Solids Struct. 2012, 49, 989–1000. [Google Scholar] [CrossRef] [Green Version]
- Guerra, A.J.; Cano, P.; Rabionet, M.; Puig, T.; Ciurana, J. 3D-Printed PCL/PLA Composite Stents: Towards a New Solution to Cardiovascular Problems. Materials 2018, 11, 1679. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ang, H.Y.; Huang, Y.Y.; Lim, S.T.; Wong, P.; Joner, M.; Foin, N. Mechanical behaviour of polymer-based vs. metallic-based bioresorbable stents. J. Thorac Dis. 2017, 9 (Suppl. 9), 923–934. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- ASTM F2079-09(2017), Standard Test Method for Measuring Intrinsic Elastic Recoil of Balloon-Expandable Stents; ASTM International: West Conshohocken, PA, USA, 2017.
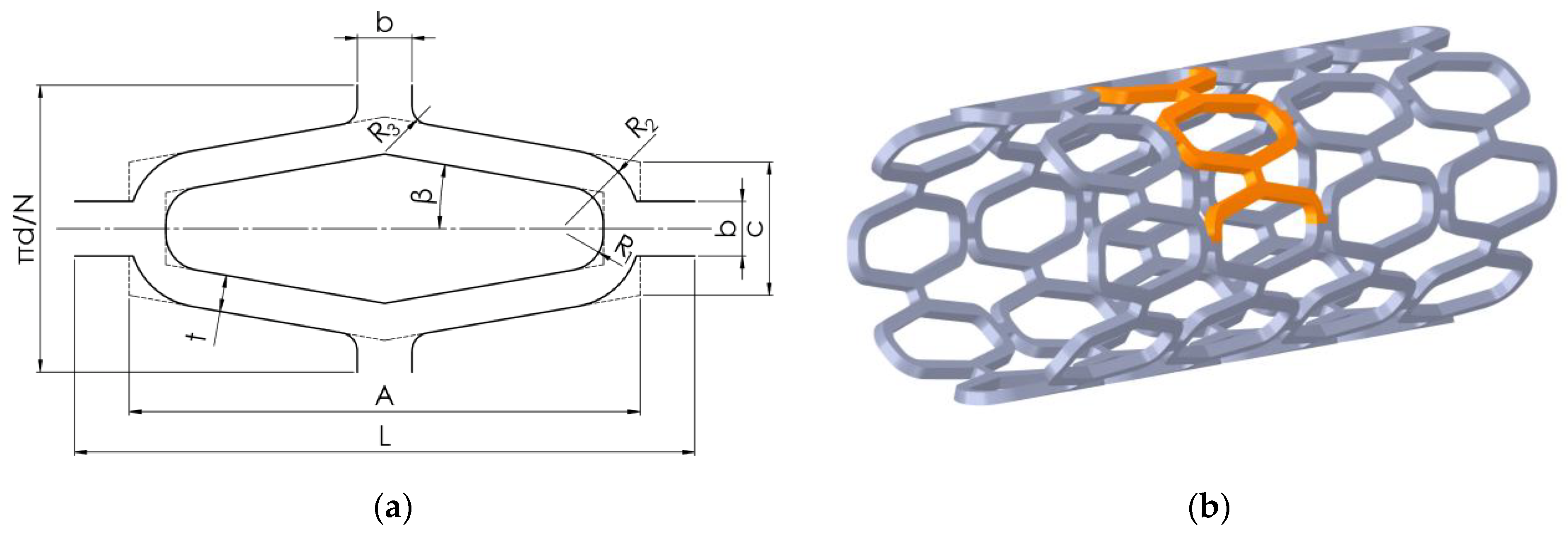




| Parameter | Symbol | Value |
|---|---|---|
| Outer stent diameter | D | 4.4 mm |
| Inner stent diameter | d | 4 mm |
| Total cell length | L | 3.2 mm |
| Cell length | A | 2.8 mm |
| Cell height | c | 0.73 mm |
| Number of cells per circumference | N | 8 mm |
| Strut width | t | 0.2 mm |
| Stent thickness | ts | 0.2 mm |
| Connecting strut width | b | 0.3 mm |
| Radius 1 | R1 | 0.2 mm |
| Radius 2 | R2 | 0.41 mm |
| Material | Density [kg/m3] | Poisson’s Ratio [–] | Young’s Modulus [MPa] | Yield Strength [MPa] | Tangent Modulus [MPa] | Material Model |
|---|---|---|---|---|---|---|
| PLA | 1250 | 0.33 | 3000 | 65 | 30 | Bilinear |
| PCL | 1100 | 0.33 | 350 | 25 | 10 | Bilinear |
| Part | Element Type | Element Order | Number of Nodes | Number of Elements |
|---|---|---|---|---|
| Stent | Hex20 (SOLID186) | Quadratic | 28,632 | 5120 |
| Crimper | Quad4 (SHELL181) | Linear | 25 | 16 |
| Balloon | Quad4 (SHELL181) | Linear | 168 | 140 |
| Configuration (0-PLA; 1-PCL) | Equivalent Plastic Strain [mm/mm] | Configuration (0-PLA; 1-PCL) | Equivalent Plastic Strain [mm/mm] |
|---|---|---|---|
| 0000 | 0.72 | 1000 | 0.74 |
| 0001 | 0.72 | 1001 | 0.72 |
| 0010 | 0.71 | 1010 | 0.72 |
| 0011 | 0.71 | 1011 | 0.68 |
| 0100 | 0.72 | 1100 | 0.73 |
| 0101 | 0.71 | 1101 | 0.69 |
| 0110 | 0.71 | 1110 | 0.71 |
| 0111 | 0.65 | 1111 | 0.61 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Donik, Ž.; Nečemer, B.; Vesenjak, M.; Glodež, S.; Kramberger, J. Computational Analysis of Mechanical Performance for Composite Polymer Biodegradable Stents. Materials 2021, 14, 6016. https://doi.org/10.3390/ma14206016
Donik Ž, Nečemer B, Vesenjak M, Glodež S, Kramberger J. Computational Analysis of Mechanical Performance for Composite Polymer Biodegradable Stents. Materials. 2021; 14(20):6016. https://doi.org/10.3390/ma14206016
Chicago/Turabian StyleDonik, Žiga, Branko Nečemer, Matej Vesenjak, Srečko Glodež, and Janez Kramberger. 2021. "Computational Analysis of Mechanical Performance for Composite Polymer Biodegradable Stents" Materials 14, no. 20: 6016. https://doi.org/10.3390/ma14206016
APA StyleDonik, Ž., Nečemer, B., Vesenjak, M., Glodež, S., & Kramberger, J. (2021). Computational Analysis of Mechanical Performance for Composite Polymer Biodegradable Stents. Materials, 14(20), 6016. https://doi.org/10.3390/ma14206016







