Abstract
The aim of the study was to investigate the incidence of the inferior alveolar nerve (IAN) injury in mandibular fractures. This study is based on two databases that have continuously recorded patients hospitalized with maxillofacial fractures in two departments—Department of Maxillofacial Surgery, Vrije Universiteit University Medical Center, Amsterdam, the Netherlands, and Division of Maxillofacial Surgery, San Giovanni Battista Hospital, Turin, Italy. Demographic, anatomic, and etiology variables were considered for each patient and statistically assessed in relation to the neurosensory IAN impairment. Statistically significant associations were found between IAN injury and fracture displacement (p = 0.03), isolated mandibular fractures (p = 0.01), and angle fractures (p = 0.004). A statistically significant association was also found between IAN injury and assaults (p = 0.03). Displaced isolated mandibular angle fractures could be considered at risk for increased incidence of IAN injury. Assaults seem to be the most important etiological factor that is responsible for IAN lesions.
The mandible is reported to be the most commonly fractured bone of the facial skeleton [1,2,3,4,5,6,7,8,9,10]. Mandibular fractures that occur between the mental and mandibular foramina frequently result in inferior alveolar nerve (IAN) injury [2,3,4,5]. As a consequence of nerve injury, an altered neurosensory function of the skin and mucous membrane within the distribution of mental nerve on the side of fracture may be observed, though usually such condition gradually improves with time [2,3,4,5]. Etiology of IAN injury may include indirect traumatic injury of nerve bundle, compression by soft tissue edema, or direct nerve involvement within fracture rimes with consequent dislocation, traction, or compression [7].
Posttraumatic disorders of IAN are troublesome sequelae of facial trauma, often determining a reduced quality of life for patients [7]. Nevertheless, the incidence and patterns of posttraumatic IAN sensory disturbances have been scarcely documented in the maxillofacial trauma literature [2,3,8].
The purpose of this study was to investigate the incidence of IAN injury at the time of presentation in mandibular fractures in a large two-center population of trauma patients. The investigators hypothesized that when the force of impact is completely absorbed by the mandible, the IAN is more frequently damaged. Therefore, the specific aims of the study were to estimate the role of some variables (patients’ age, gender, fractures site, displacement, and type of etiological mechanism) in determining IAN injury.
Materials and Methods
To address the research purpose, the investigators designed and implemented a retrospective cohort study that is based on two systematic computer-assisted databases that have continuously recorded patients hospitalized with maxillofacial fractures in the Division of Maxillofacial Surgery, San Giovanni Battista Hospital, Turin, Italy, and in the Department of Oral and Maxillofacial Surgery, Vrije Universiteit University Medical Center (VUMC), Amsterdam, the Netherlands.
The study population was composed of all patients who underwent surgical treatment for mandibular fractures placing the mandibular nerve at risk for injury (fractures extending from the mandibular foramen to the mental foramen) between January 1, 2001, and January 1, 2010. To be included in the study sample, patients had to present isolated unilateral mandibular fractures extending from the mandibular foramen to the mental foramen (ramus, angle, and body regions) (Figure 1) eventually in association with other maxillofacial fractures. Patients were excluded as study subjects if they presented with solitary condylar, subcondylar, coronoid, symphyseal, and parasymphyseal fractures or a combination thereof; patients with multiple mandibular fractures were excluded too.
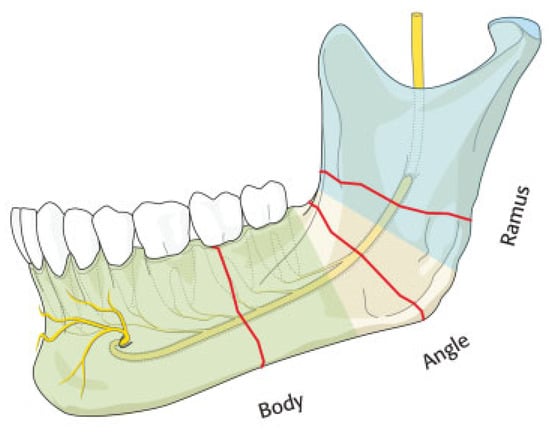
Figure 1.
The image would show the locations of injury of inferior alveolar nerve: ramus, angle, body. The mandible is seen from the lingual side.
The following data for the injured patients were considered: gender, age, site and severity (facial injury severity scale [FISS]) of facial fractures [9], etiology, associated dental injuries, and associated body injuries. Associated maxillofacial fractures were categorized as zygomatic fractures, nasal bone fractures, Le Fort I fractures, Le Fort II fractures, Le Fort III fractures, frontal bone fractures, nasal-orbit-ethmoid fractures, medial orbital wall fractures, orbital roof fractures, and dentoalveolar fractures.
IAN sensory disturbances were defined when a loss or abnormal sensation over the V-3 distribution could be found by two-point discrimination test. The noninjured side served as an internal control in two-point discrimination [11]. Patients who reported to have anesthesia or hypoesthesia (numbness) of the lower lip region on the affected side were considered to have IAN injury [1].
Crown or root fracture, luxation, intrusion, and avulsion were considered in the “associated dental injuries” category, whereas dental concussions were not assessed. Concomitant injuries were classified as orthopedic, encephalic, spine, ocular, thoracic, and abdominal. Statistical analysis was used to search for associations among multiple variables. Statistical significance was determined using the X2 or Fisher exact test, if the sample sizes were too small. The retrospective series was exempted from review as a retrospective series by our institutional review board human studies committee. We followed Helsinki Declaration guidelines.
Results
During the considered time frame, 1,818 patients with maxillofacial fractures were admitted to the Division of Maxillofacial Surgery, San Giovanni Battista Hospital, Turin (UNITO), whereas 523 patients were admitted to the Department of Oral and Maxillofacial Surgery, VUMC, Amsterdam.
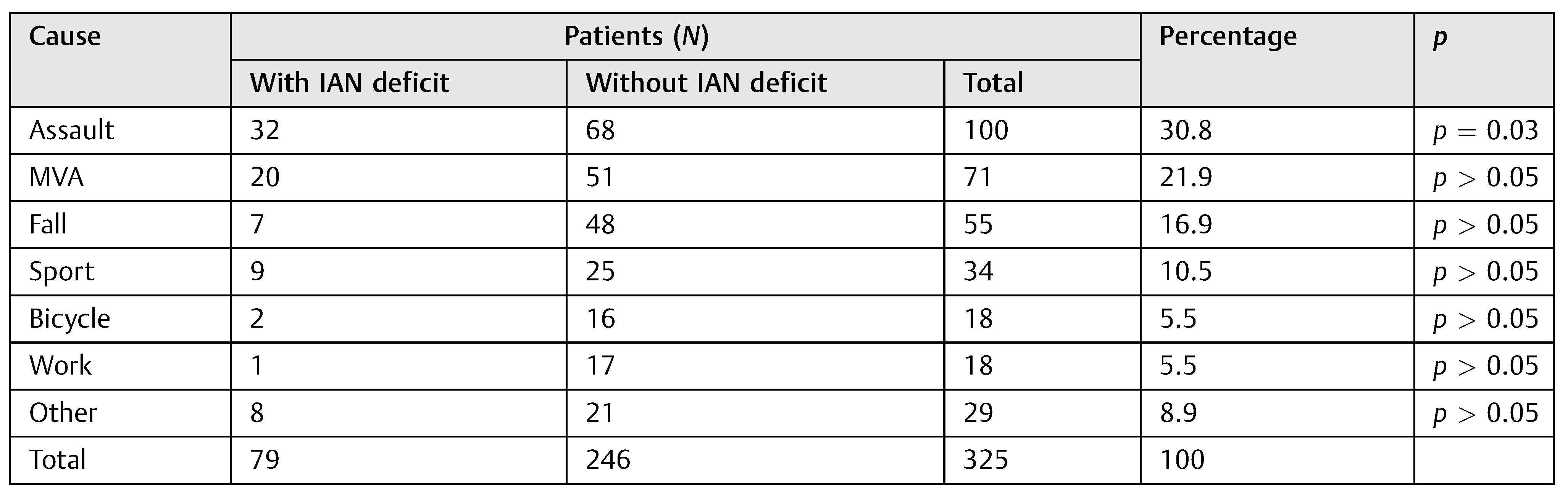
On the whole, 325 patients (255 males, 70 females; maleto-female ratio, 3.6:1) with surgically treated isolated unilateral mandibular fractures extending from the mandibular foramen to the mental foramen (i.e., ramus, angle, and body fractures) were included. The mean age of the patients was 34.4 years (range, 3–99 years; median, 25.5; standard deviation [SD], 8.1). The most common causes of the considered mandibular fractures were assaults (30.8%), followed by motor-vehicle accidents (21.9%), and falls (16.9%) (Table 1). The most frequent mandibular site of fracture with involvement of the IAN course was the angle (164 fractures), followed by body (156), and ramus (5). Out of the 325 considered mandibular fractures, 185 were found to be displaced, whereas 140 fractures were undisplaced. In 285 patients, a single mandibular fracture without any associated facial fracture was observed. In the remaining 40 cases, 67 associated facial fractures were diagnosed, with the zygoma being the most frequently involved site (10 fractures), followed by Le Fort II (9 fractures), dentoalveolar (8), Le Fort I (8), and palate fractures (7). The mean FISS score in the study population was 2.4 (range, 2–12; median, 2; SD, 1).

Table 1.
Etiology of trauma in the study population.
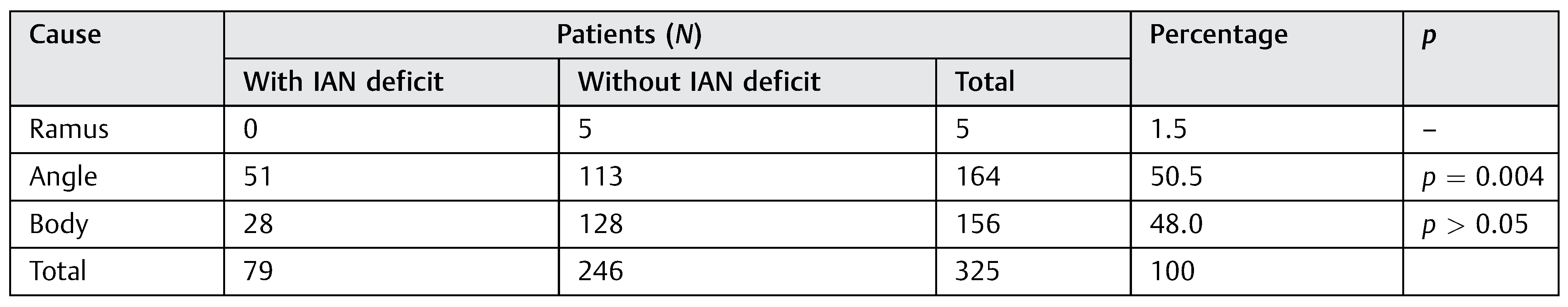
As for IAN injury, a sensory disturbance of the lower lip was evident in 79 patients (24.3%): 68 males and 11 females. Fifty-one patients had single fractures in the angle region and 28 in the body region (Table 2). Sixty-three patients presented associated dental injuries. Most frequently observed dental injuries were dental fractures (54 lesions), followed by avulsions (46), and luxations (41).

Table 2.
IAN injury and mandibular fracture location in the study population.
Finally, 41 patients were diagnosed with associated body injuries, with orthopedic injuries being the most frequently observed concomitant lesions (31 injuries), followed by encephalic (13), thoracic (11), spine (6 injuries), ocular (2), and abdominal (2). A statistically significant association was found between IAN injury and fracture displacement (p = 0.03; relative risk (RR), 1.8; intervals of confidence (IC) 95%, 1.04–3.02). Furthermore, statistically significant associations were also found between IAN sensory disturbances and a FISS value of 2, corresponding to isolated mandibular fractures (p = 0.01; RR, 3.2; IC 95%, 1.18–10.89), and between IAN sensory disturbances and angle fractures (p = 0.004) (Table 2). As for etiology (Table 1), a statistically significant association was found between IAN injury and assaults (p = 0.03).
Instead, no further statistically significant associations were observed between IAN deficit and age or gender.
Discussion
In literature, the prevalence of postinjury/pretreatment IAN deficit has been reported to range from 5.7 to 58.5% [3,8,11]. IAN injuries may be determined by indirect traumatic injury of nerve bundle, compression by soft tissue edema, or direct nerve involvement within fracture rimes with consequent dislocation, traction, or compression [7].
Nevertheless, features and factors associated with IAN injury have not been thoroughly investigated in the maxillofacial trauma literature. In our study population, a sensory disturbance of the lower lip was found in 79 patients (24.3%), thus confirming the frequency of this lesion when a mandibular fracture occurs. The presented case series showed a male-to-female ratio of 3.6:1, whereas the most common causes of mandibular fractures were assaults, followed by motor-vehicle accidents, and falls. In 285 patients, a single mandibular fracture without any associated facial fracture was observed. In the remaining 40 cases, 67 associated facial fractures were diagnosed, with the zygoma being the most frequently involved site, followed by Le Fort II, dentoalveolar, Le Fort I, and palate fractures.
Interestingly, statistically significant associations were found between IAN injury and fracture displacement (p = 0.03), between IAN sensory disturbances and a FISS value of 2, corresponding to isolated and unilateral mandibular fractures (p = 0.01), and between IAN sensory disturbances and angle fractures (p = 0.004) (Table 2). Furthermore, a statistically significant association was found between IAN injury and assaults (p = 0.03). As expected, these results confirm the obvious finding that displaced mandibular fractures are more frequently related to IAN injury, because of the direct nerve involvement within fracture rimes with consequent dislocation, traction, or compression [1,7,8,12].
Moreover, the results of the statistical analysis suggest that when the force of impact is completely absorbed by the mandible, the IAN is most frequently damaged. In fact, both the etiological category of assaults and a lower FISS value are associated with IAN injury, thus suggesting that a direct and single middle-energy trauma (such as a fist or a hitting object) that is often absorbed by the specific involved bone may more easily determine such neural lesion. Finally, a statistically significant association was also found between IAN sensory disturbances and angle fractures (p = 0.004) that seem to be a risk factor for IAN injury.
Conclusion
In conclusion, displaced, isolated, mandibular angle fractures could be considered at risk for an increased incidence of IAN injury. Assaults seem to be the most important etiological factor that is responsible for IAN lesions. Therefore, the etiology and the characteristics of mandibular fractures should be appropriately assessed, as they may reveal important factors for primary orientation. On the contrary, the finding of IAN sensory disturbances following facial trauma may remind the surgeon to accurately evaluate the mandible integrity.
References
- Bede, S.Y.; Ismael, W.K.; Al-Assaf, D.A.; Omer, S.S. Inferior alveolar nerve injuries associated with mandibular fractures. J Craniofac Surg 2012, 23, 1776–1778. [Google Scholar] [CrossRef] [PubMed]
- Brajdić, D.; Virag, M.; Uglešić, V.; Aljinović-Ratković, N.; Zajc, I.; Macan, D. Evaluation of sensitivity of teeth after mandibular fractures. Int J Oral Maxillofac Surg 2011, 40, 266–270. [Google Scholar] [CrossRef] [PubMed]
- Halpern, L.R.; Kaban, L.B.; Dodson, T.B. Perioperative neurosensory changes associated with treatment of mandibular fractures. J Oral Maxillofac Surg 2004, 62, 576–581. [Google Scholar] [CrossRef] [PubMed]
- van den Bergh, B.; van Es, C.; Forouzanfar, T. Analysis of mandibular fractures. J Craniofac Surg 2011, 22, 1631–1634. [Google Scholar] [CrossRef]
- van den Bergh, B.; Heymans, M.W.; Duvekot, F.; Forouzanfar, T. Treatment and complications of mandibular fractures: a 10-year analysis. J Craniomaxillofac Surg 2012, 40, e108–e111. [Google Scholar] [CrossRef] [PubMed]
- Gerbino, G.; Boffano, P.; Bosco, G.F. Symphyseal mandibular fractures associated with bicondylar fractures: a retrospective analysis. J Oral Maxillofac Surg 2009, 67, 1656–1660. [Google Scholar] [CrossRef]
- Renzi, G.; Carboni, A.; Perugini, M.; Giovannetti, F.; Becelli, R. Posttraumatic trigeminal nerve impairment: a prospective analysis of recovery patterns in a series of 103 consecutive facial fractures. J Oral Maxillofac Surg 2004, 62, 1341–1346. [Google Scholar] [CrossRef]
- Marchena, J.M.; Padwa, B.L.; Kaban, L.B. Sensory abnormalities associated with mandibular fractures: incidence and natural history. J Oral Maxillofac Surg 1998, 56, 822–825, discussion 825–826. [Google Scholar] [CrossRef]
- Bagheri, S.C.; Dierks, E.J.; Kademani, D.; et al. Application of a facial injury severity scale in craniomaxillofacial trauma. J Oral Maxillofac Surg 2006, 64, 408–414. [Google Scholar] [CrossRef] [PubMed]
- Vriens, J.P.; Moos, K.F. Morbidity of the infraorbital nerve following orbitozygomatic complex fractures. J Craniomaxillofac Surg 1995, 23, 363–368. [Google Scholar] [CrossRef] [PubMed]
- Schultze-Mosgau, S.; Erbe, M.; Rudolph, D.; Ott, R.; Neukam, F.W. Prospective study on post-traumatic and postoperative sensory disturbances of the inferior alveolar nerve and infraorbital nerve in mandibular and midfacial fractures. J Craniomaxillofac Surg 1999, 27, 86–93. [Google Scholar] [CrossRef]
- Roccia, F.; Diaspro, A.; Pecorari, G.C.; Bosco, G. Pneumomediastinum and cervical emphysema associated with mandibular fracture. J Trauma 2007, 63, 924–926. [Google Scholar] [CrossRef] [PubMed]
© 2014 by the author. The Author(s) 2014.