Analysis of Road Traffic Crashes–Related Maxillofacial Injuries Severity and Concomitant Injuries in 201 Patients Seen at the UCH, Ibadan
Abstract
:Patients and Methods
Data Analysis
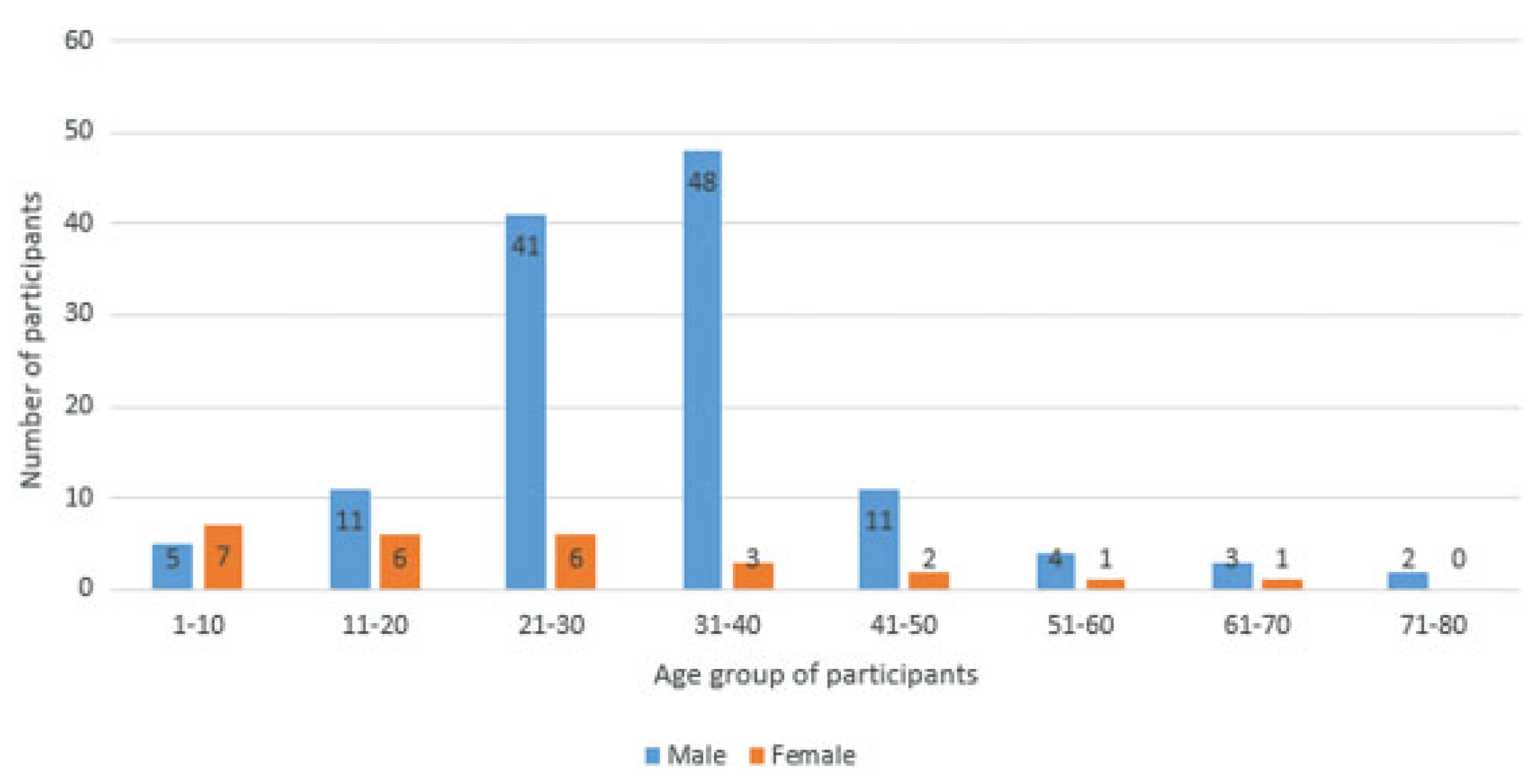
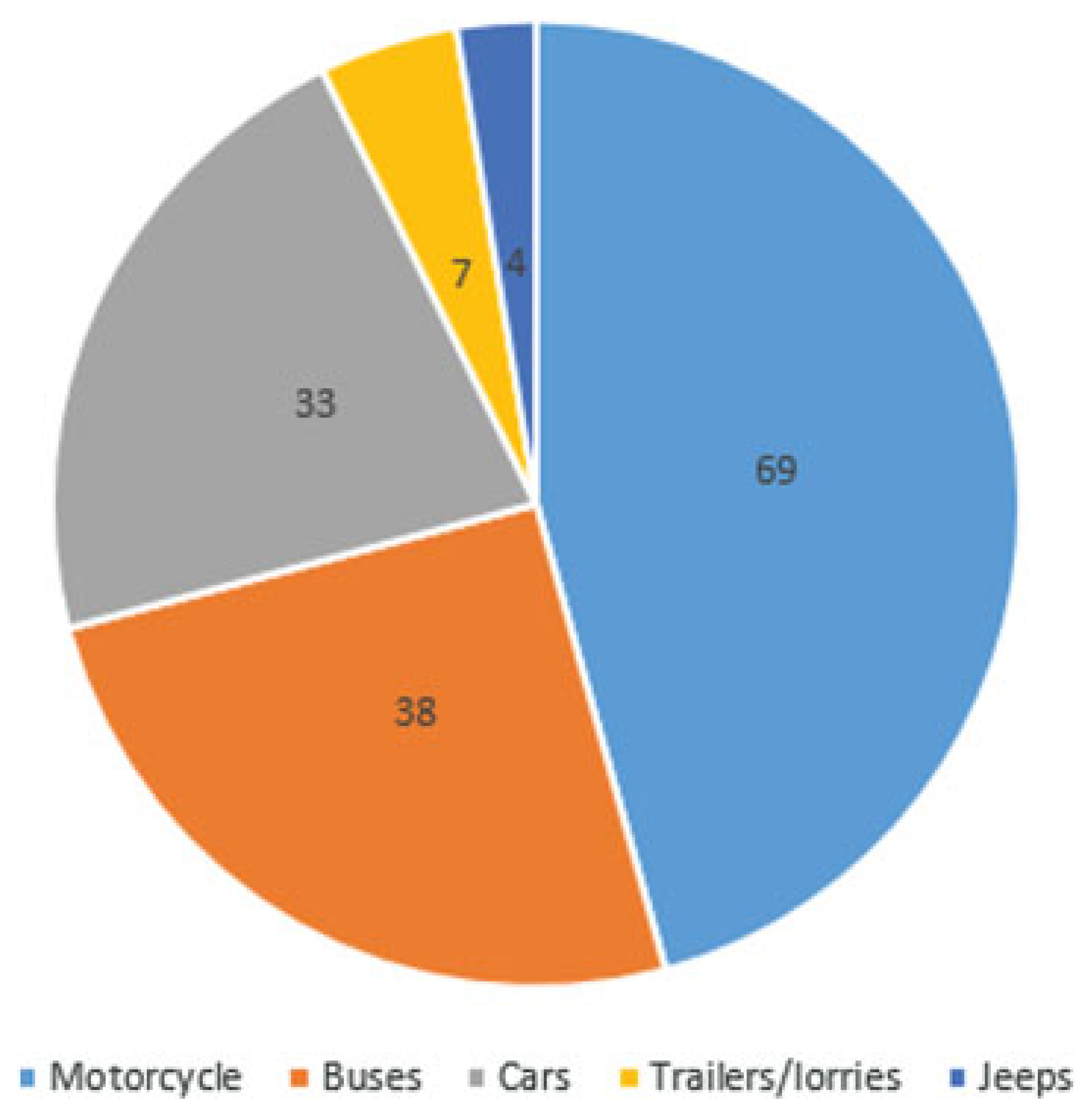
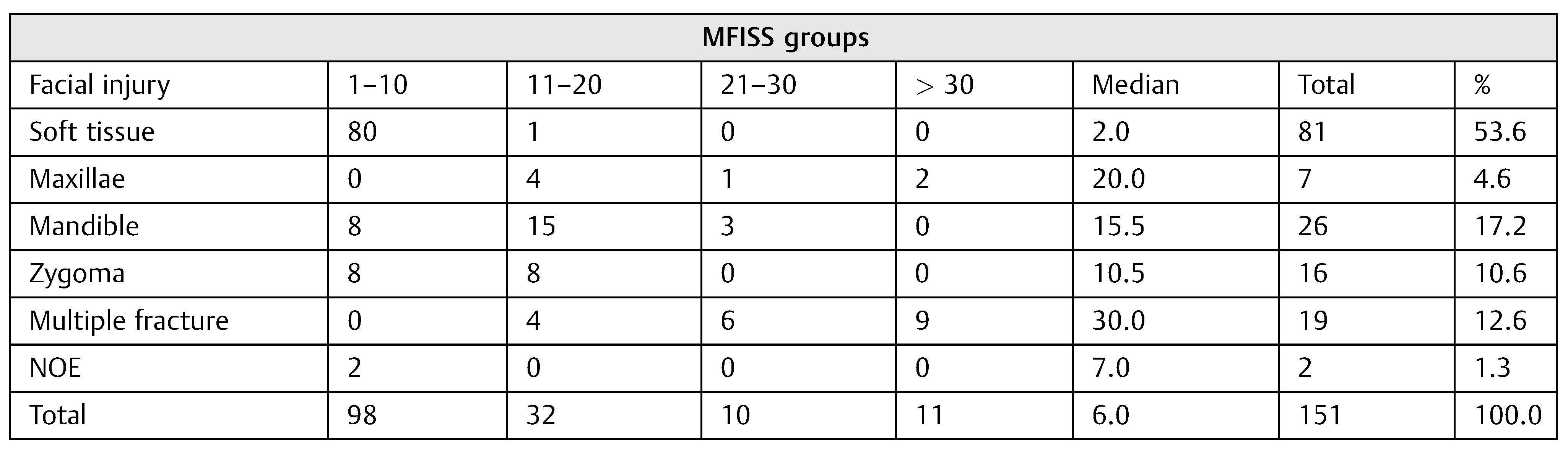
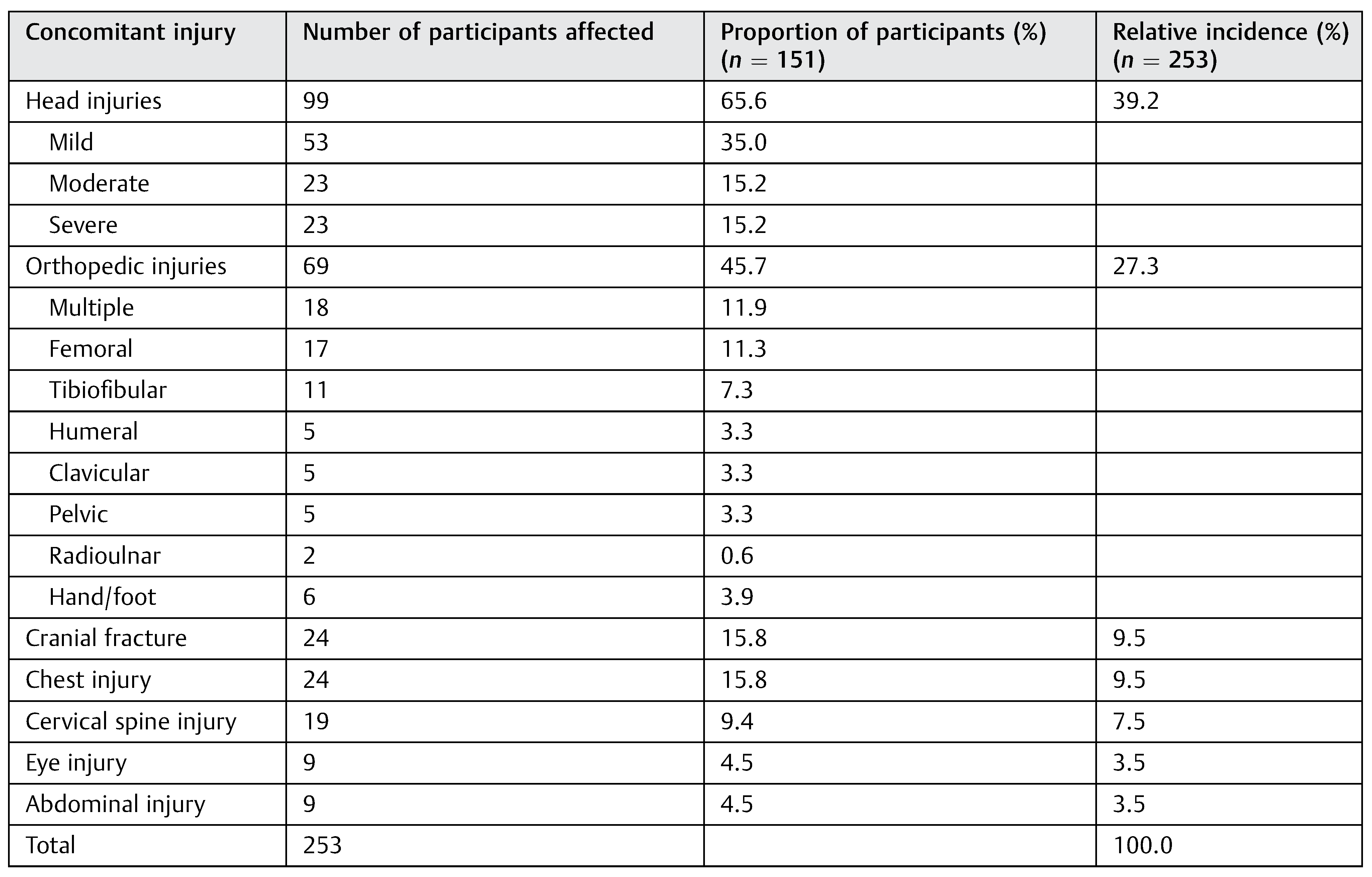
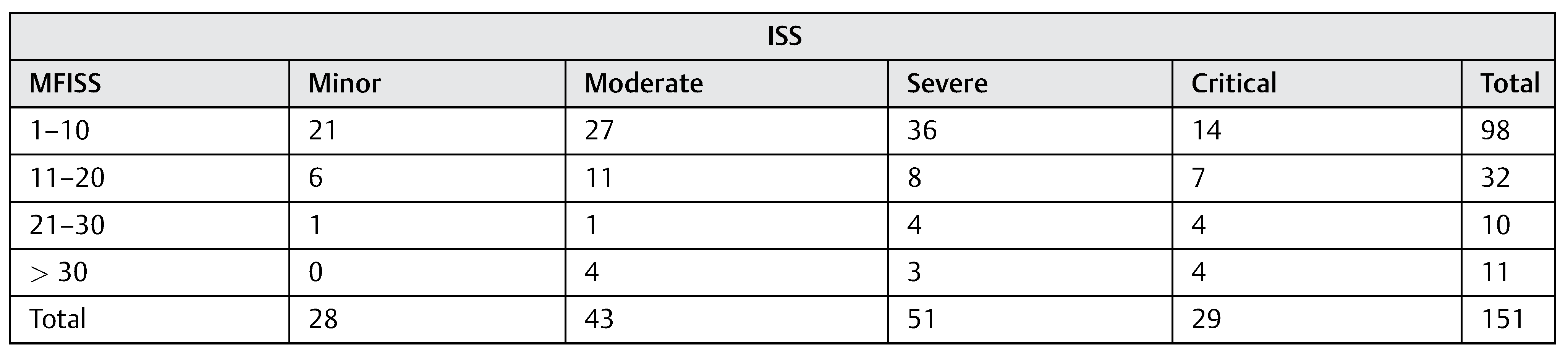
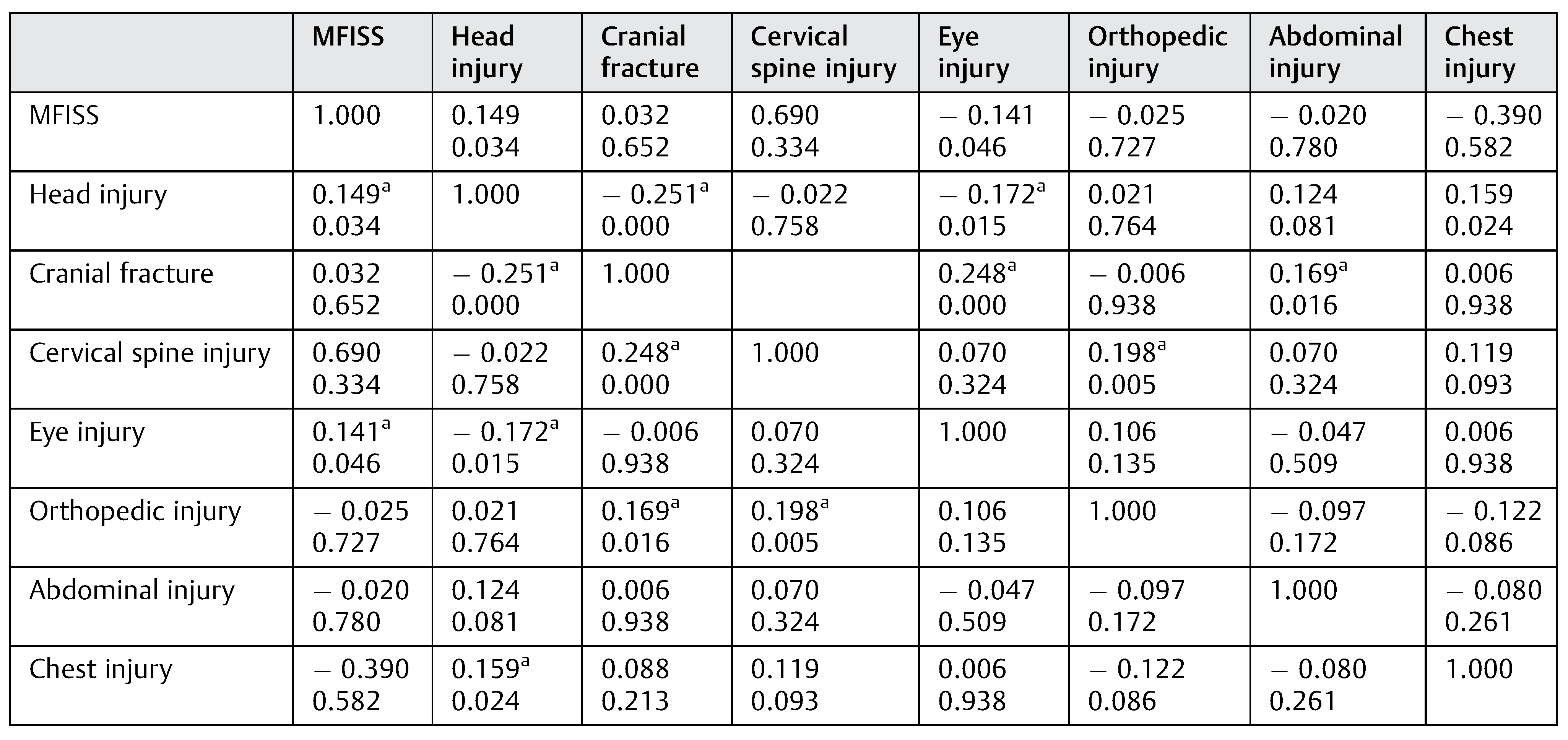
Results
Discussion
Conclusion
Note
References
- Adeyemo, W.L.; Ladeinde, A.L.; Ogunlewe, M.O.; James, O. Trends and characteristics of oral and maxillofacial injuries in Nigeria: a review of the literature. Head Face Med 2005, 1, 7. [Google Scholar] [CrossRef]
- Brooks, A.; Holroyd, B.; Riley, B. Missed injury in major trauma patients. Injury 2004, 35, 407–410. [Google Scholar] [CrossRef]
- Lawson, C.M.; Daley, B.J.; Ormsby, C.B.; Enderson, B. Missed injuries in the era of the trauma scan. J Trauma 2011, 70, 452–456, discussion 456–458. [Google Scholar] [CrossRef]
- Ugboko, V.I.; Udoye, C.; Olateju, S.O.; Amole, A.O. Blindness and visual impairment from severe midface trauma in Nigerians. Int J Oral Maxillofac Surg 2006, 35, 127–131. [Google Scholar] [CrossRef]
- Zhang, J.; Zhang, Y.; El-Maaytah, M.; Ma, L.; Liu, L.; Zhou, L.D. Maxillofacial injury severity score: proposal of a new scoring system. Int J Oral Maxillofac Surg 2006, 35, 109–114. [Google Scholar] [CrossRef]
- Champion, H.R. Trauma scoring. Scand J Surg 2002, 91, 12–22. [Google Scholar] [CrossRef]
- Adekeye, E.O. The pattern of fractures of the facial skeleton in Kaduna, Nigeria. A survey of 1,447 cases. Oral Surg Oral Med Oral Pathol 1980, 49, 491–495. [Google Scholar] [CrossRef]
- Ugboko, V.I.; Odusanya, S.A.; Fagade, O.O. Maxillofacial fractures in a semi-urban Nigerian teaching hospital. A review of 442 cases. Int J Oral Maxillofac Surg 1998, 27, 286–289. [Google Scholar] [CrossRef]
- Fasola, A.O.; Nyako, E.A.; Obiechina, A.E.; Arotiba, J.T. Trends in the characteristics of maxillofacial fractures in Nigeria. J Oral Maxillofac Surg 2003, 61, 1140–1143. [Google Scholar] [CrossRef]
- Ajike, S.O.; Adebayo, E.T.; Amanyiewe, E.U.; Ononiwu, C.N. An epidemiologic survey of maxillofacial fractures and concomitant injuries in Kaduna, Nigeria. Nig J Surg Res 2005, 7, 251–255. [Google Scholar] [CrossRef]
- Oginni, F.O.; Ugboko, V.I.; Ogundipe, O.; Adegbehingbe, B.O. Motorcycle-related maxillofacial injuries among Nigerian intracity road users. J Oral Maxillofac Surg 2006, 64, 56–62. [Google Scholar] [CrossRef]
- Subhashraj, K.; Nandakumar, N.; Ravindran, C. Review of maxillofacial injuries in Chennai, India: a study of 2748 cases. Br J Oral Maxillofac Surg 2007, 45, 637–639. [Google Scholar] [CrossRef]
- Hashim, H.; Iqbal, S. Motorcycle accident is the main cause of maxillofacial injuries in the Penang Mainland, Malaysia. Dent Traumatol 2011, 27, 19–22. [Google Scholar] [CrossRef]
- Ramli, R.; Rahman, N.A.; Rahman, R.A.; Hussaini, H.M.; Hamid, A.L.A. A retrospective study of oral and maxillofacial injuries in Seremban Hospital, Malaysia. Dent Traumatol 2011, 27, 122–126. [Google Scholar] [CrossRef]
- Iribhogbe, P.E.; Osime, C.O. Compliance with seat belt use in Benin City, Nigeria. Prehosp Disaster Med 2008, 23, 16–19. [Google Scholar] [CrossRef]
- Obuekwe, O.N.; Ojo, M.A.; Akpata, O.; Etetafia, M. Maxillofacial trauma due to road traffic accidents in Benin City, Nigeria: a prospective study. Ann Afr Med 2003, 2, 58–63. [Google Scholar]
- Solagberu, B.A.; Ofoegbu, C.K.P.; Nasir, A.A.; Ogundipe, O.K.; Adekanye, A.O.; Abdur-Rahman, L.O. Motorcycle injuries in a developing country and the vulnerability of riders, passengers, and pedestrians. Inj Prev 2006, 12, 266–268. [Google Scholar] [CrossRef]
- Servadei, F.; Begliomini, C.; Gardini, E.; Giustini, M.; Taggi, F.; Kraus, J. Effect of Italy’s motorcycle helmet law on traumatic brain injuries. Inj Prev 2003, 9, 257–260. [Google Scholar] [CrossRef]
- Adebayo, E.T.; Ajike, O.S.; Adekeye, E.O. Analysis of the pattern of maxillofacial fractures in Kaduna, Nigeria. Br J Oral Maxillofac Surg 2003, 41, 396–400. [Google Scholar] [CrossRef]
- Fonseca, R.J.; Walker, R.V.; Betts, N.J.; Barber, H.D. (Eds.) Oral and Maxillofacial Surgery Trauma I, 2nd ed.; Philadelphia, PA: Saunders, 1997. [Google Scholar]
- Haug, R.H.; Prather, J.; Indresano, A.T. An epidemiologic survey of facial fractures and concomitant injuries. J Oral Maxillofac Surg 1990, 48, 926–932. [Google Scholar] [CrossRef]
- Fasola, A.O.; Obiechina, A.E.; Arotiba, J.T. Concomitant injuries in 531 patients with maxillofacial fractures. Afr J Med Med Sci 2002, 31, 101–105. [Google Scholar]
- Follmar, K.E.; Debruijn, M.; Baccarani, A.; et al. Concomitant injuries in patients with panfacial fractures. J Trauma 2007, 63, 831–835. [Google Scholar] [CrossRef]
- Allareddy, V.; Allareddy, V.; Nalliah, R.P. Epidemiology of facial fracture injuries. J Oral Maxillofac Surg 2011, 69, 2613–2618. [Google Scholar] [CrossRef]
- Gandhi, S.; Ranganathan, L.K.; Solanki, M.; Mathew, G.C.; Singh, I.; Bither, S. Pattern of maxillofacial fractures at a tertiary hospital in northern India: a 4-year retrospective study of 718 patients. Dent Traumatol 2011, 27, 257–262. [Google Scholar] [CrossRef]
- Haug, R.H.; Savage, J.D.; Likavec, M.J.; Conforti, P.J. A review of 100 closed head injuries associated with facial fractures. J Oral Maxillofac Surg 1992, 50, 218–222. [Google Scholar] [CrossRef]
- Plaisier, B.R.; Punjabi, A.P.; Super, D.M.; Haug, R.H. The relationship between facial fractures and death from neurologic injury. J Oral Maxillofac Surg 2000, 58, 708–712, discussion 712–713. [Google Scholar] [CrossRef]
- Roth, F.S.; Koshy, J.C.; Goldberg, J.S.; Soparkar, C.N.S. Pearls of orbital trauma management. Semin Plast Surg 2010, 24, 398–410. [Google Scholar] [CrossRef]
- Nagase, D.Y.; Courtemanche, D.J.; Peters, D.A. Facial fractures - association with ocular injuries: A 13-year review of one practice in a tertiary care centre. Can J Plast Surg 2006, 14, 167–171. [Google Scholar] [CrossRef]
- Okoje, V.N.; Malomo, A.O.; Obiechina, A.E. Concomitant craniospinal injuries with maxillofacial trauma—a review of 266 cases. Afr J Med Med Sci 2006, 35, 165–168. [Google Scholar] [PubMed]
- Kraft, A.; Abermann, E.; Stigler, R.; et al. Craniomaxillofacial trauma: synopsis of 14,654 cases with 35,129 injuries in 15 years. Cranio-maxillofac Trauma Reconstr 2012, 5, 41–50. [Google Scholar] [CrossRef] [PubMed]
- Down, K.E.; Boot, D.A.; Gorman, D.F. Maxillofacial and associated injuries in severely traumatized patients: implications of a regional survey. Int J Oral Maxillofac Surg 1995, 24, 409–412. [Google Scholar] [CrossRef]
- Hayter, J.P.; Ward, A.J.; Smith, E.J. Maxillofacial trauma in severely injured patients. Br J Oral Maxillofac Surg 1991, 29, 370–373. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2014 by the author. The Author(s) 2014.
Share and Cite
Aladelusi, T.; Akinmoladun, V.; Olusanya, A.; Akadiri, O.; Fasola, A. Analysis of Road Traffic Crashes–Related Maxillofacial Injuries Severity and Concomitant Injuries in 201 Patients Seen at the UCH, Ibadan. Craniomaxillofac. Trauma Reconstr. 2014, 7, 284-289. https://doi.org/10.1055/s-0034-1378183
Aladelusi T, Akinmoladun V, Olusanya A, Akadiri O, Fasola A. Analysis of Road Traffic Crashes–Related Maxillofacial Injuries Severity and Concomitant Injuries in 201 Patients Seen at the UCH, Ibadan. Craniomaxillofacial Trauma & Reconstruction. 2014; 7(4):284-289. https://doi.org/10.1055/s-0034-1378183
Chicago/Turabian StyleAladelusi, Timothy, Victor Akinmoladun, Adeola Olusanya, Oladimeji Akadiri, and Abiodun Fasola. 2014. "Analysis of Road Traffic Crashes–Related Maxillofacial Injuries Severity and Concomitant Injuries in 201 Patients Seen at the UCH, Ibadan" Craniomaxillofacial Trauma & Reconstruction 7, no. 4: 284-289. https://doi.org/10.1055/s-0034-1378183
APA StyleAladelusi, T., Akinmoladun, V., Olusanya, A., Akadiri, O., & Fasola, A. (2014). Analysis of Road Traffic Crashes–Related Maxillofacial Injuries Severity and Concomitant Injuries in 201 Patients Seen at the UCH, Ibadan. Craniomaxillofacial Trauma & Reconstruction, 7(4), 284-289. https://doi.org/10.1055/s-0034-1378183



