Abstract
The aim of the study was to evaluate the efficacy and complication rate with use of 2.0-mm titanium three-dimensional (3D) curved angle strut plate for mandibular angle fractures. Twenty cases requiring internal fixation of the mandibular angle by 2.0-mm titanium 3D curved angle strut plates were evaluated. Postoperative clinical and radiological analyses were done on 1st, 2nd, 4th, and 6th weeks, which included wound healing, transmitted movements, difficulty in function and occlusion, and neurosensory changes, if any. Reasonable level of success in terms of immediate jaw function was noted in all cases. Transient inferior alveolar nerve dysfunction was observed in three cases, which recovered gradually in 2 months, and surgical site infection was observed in two cases, which resolved with appropriate course of antibiotics and wound care. Fixation of mandibular angle fractures with a 2.0-mm titanium 3D curved angle strut plate is predictable, expeditious, and has less complication rate.
Despite many advances in internal fixation, angle fracture remains among the most difficult and unpredictable fracture to treat compared with those of other areas of the mandible. Large number of studies on mandibular angle fracture treatment attests to the fact that no single approach has been shown to be ideal, and that treatment of mandibular angle fractures remains conceptually controversial, with a bothersome complication rate. During the past decade, significant attention has been placed on variety of plate fixations for mandibular angle fractures [1,2,3,4,5,6,7,8,9,10,11,12,13,14]. Fixation using miniplates has been shown to simplify surgery and reduce surgical morbidity, but failed to surpass the predictability of rigid fixation [15,16,17,18].
Although there have been several studies on linear and curvilinear plates for mandibular fracture fixation, only a few reports on the use of low profile three-dimensional (3D) strut or mesh plates are reported in the literature [1,6]. In fact, majority of studies on 3D strut plates are in vitro biomechanical studies. The geometry of 3D strut plate conceptually allows for an increased number of screws, stability in 3D, and resistance against torque forces while maintaining a low profile and malleability.
The 2.0-mm titanium 3D curved angle strut plate allows for almost no movement at the superior and inferior borders with manual torsional and bending forces, as opposed to when a single linear plate is applied to the superior border area. When only one linear plate is placed at the superior border, torsional and bending forces usually cause movement along the axis of the plate with buccal-lingual splaying and gap formation at the inferior border, respectively. Because the screws are placed in a box configuration of 2.0-mm titanium 3D curved angle strut plate on both sides of the fracture rather than on a single line, broad platforms are created that may increase the resistance to torsional forces along the axis of the plate.
Because the design of 2.0-mm titanium 3D curved angle strut plate is essentially that of 2 linear plates connected by reinforcing vertical struts, they may therefore provide greater resistance against gap opening at the inferior border with biting forces compared with when a single plate is applied at the external oblique ridge or superolateral border.
The aim of the study was to evaluate and describe clinical experience, stability, and complication rate with a 2.0-mm titanium 3D curved angle strut plate specifically designed for the mandibular angle fracture in 20 patients. Outcome parameters evaluated included infection rate, hardware failure rate, wound problems, and malocclusion. Information on fracture displacement, requirement of postoperative maxillomandibular fixation (MMF), and subjective inferior alveolar nerve status was also gathered.
Materials and Methods
Twenty cases requiring internal fixation of the mandibular angle by 2.0-mm titanium 3D curved angle strut plates (Figure 1) were included in the study with detailed clinical and radiological analysis. All patients were provided with an information sheet detailing the procedure and materials used in this study. Institutional ethical committee approval and informed written consent from all the patients were obtained. Inclusion criteria were patients older than 18 years and patients who had sustained mandibular angle fracture requiring internal fixation. Exclusion criteria were patients younger than 18 years, immune compromised patients, and patients unwilling to be a part of the study or unable to come for follow-up. Preoperative evaluation included detailed case history, clinical examination, photographic records, and laboratory investigations. Preoperative radiographic analysis included posterior-anterior (PA) skull view, lateral oblique view of mandible, orthopantomogram (OPG) and computed tomographic scan to evaluate the site, nature of fractures, and need for internal fixation. All patients, either having isolated mandibular angle fracture or associated mandibular fractures, were treated under general anesthesia. For the mandibular angle fracture, either retromandibular or intraoral approach using transbuccal apparatus was used for reduction and fixation by 2.0-mm titanium 3D curved angle strut plate (Figure 2). Intraoperatively, intermaxillary fixation (IMF) was achieved in all patients. After achieving proper occlusion, fixation was completed using 2.0-mm titanium 3D curved angle strut plate with 2.0-mm × 6 mm titanium screws (Figure 3). IMF was released immediately after plate fixation and none of the patients were kept on IMF postoperatively. Postoperative radiographic evaluation was performed on immediate postoperative period (2nd postoperative day) and after 6 weeks, which included PA skull, lateral oblique view of mandible, and OPG (Figure 4). Postoperative clinical analyses were done on 1st, 2nd, 4th, and 6th weeks, which included wound healing, transmitted movements, difficulty in function and occlusion, and neurosensory changes, if any.
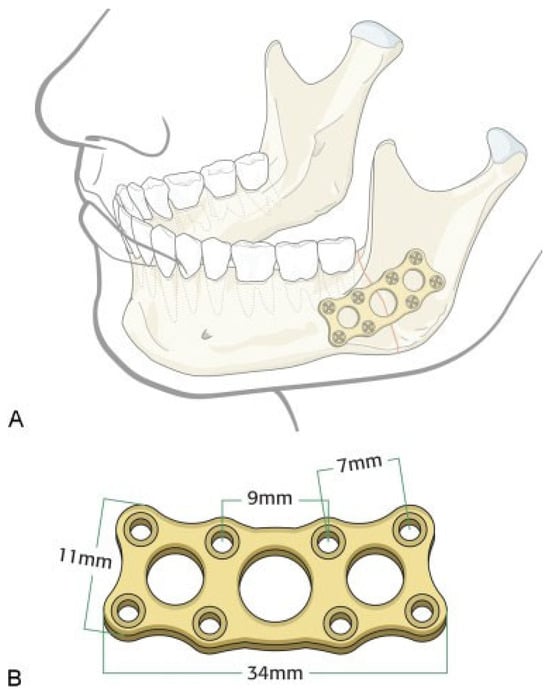
Figure 1.
(A) Adaptation of the strut plate at the mandibular angle region. (B) 2.0-mm titanium three-dimensional curved angle strut plate with detailed dimensions.
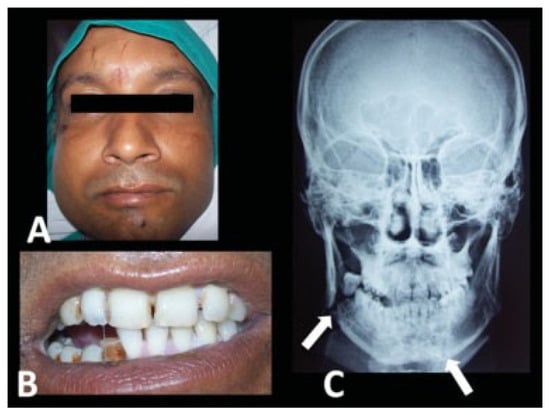
Figure 2.
Case of right angle and left parasymphysis of mandible fracture. (A) Extraoral view, (B) intraoral view showing the disturbed occlusion and step deformity, and (C) preoperative posterior-anterior skull view showing the displaced right angle and left parasymphysis fracture (arrows revealing the fracture sites).
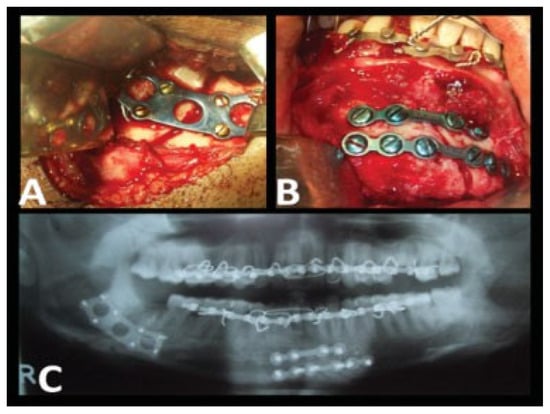
Figure 3.
(A) A 2.0-mm titanium three-dimensional curved angle strut plate fixed at right angle of mandible using 2 × 6 mm titanium screws; (B) miniplate fixation at parasymphysis region; (C) immediate postoperative orthopantomogram.
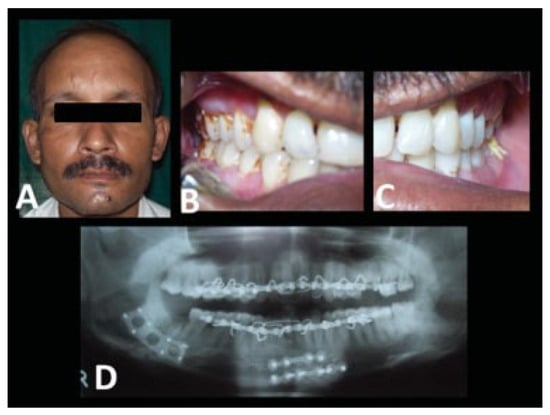
Figure 4.
(A) Postoperative extraoral view, (B and C) intact occlusion at 1 year postoperative follow-up, (D) 1 year postoperative follow-up orthopantomogram.
Results
Twenty patients (18 males, 2 females), aged between 21 and 50 years (mean 29 years), presenting with fractures of the angle of mandible and requiring open reduction and internal fixation (ORIF), were selected to evaluate the efficacy of 2.0-mm titanium 3D curved angle strut plates (Table 1).

Table 1.
Patient parameters.
A total of 21 angle fracture sites (19 unilateral and 1 bilateral) were treated using eight-holed 2.0-mm titanium 3D curved angle strut plates.
The causes of these fractures were road traffic accidents in 14 cases, fall in 3, assault in 2, and industrial accident in 1 case. In 15 cases, the mandibular angle fractures were grossly displaced and in 5 cases, the mandibular angle fractures were minimally displaced (Table 2).

Table 2.
Details of the fracture parameters.
Of the 21 mandibular angle fracture sites, 19 sites were approached extraorally and 2 sites were approached intraorally along with usage of transbuccal apparatus for fixation of 2.0-mm titanium 3D curved angle strut plate.
Among the cases selected, most of them were isolated mandibular angle fractures (12) while others were accompanied by mandibular parasymphysis (8) and mandibular body fractures (1). For mandibular angle fracture, either retromandibular or intraoral approach using transbuccal apparatus was used for reduction and fixation by 2.0-mm 3D curved angle strut plate using 2 mm × 6 mm titanium screws (Table 3). All associated fractures were approached intraorally for ORIF using titanium miniplates.

Table 3.
Details of the approaches used.
Intraoperatively, IMF was done in all cases and was released immediately after the fixation of 2.0-mm titanium 3D curved angle strut plate. The postoperative recovery was uneventful in all the cases.
Patients were able to achieve function immediately postoperatively with reasonable level of success. Malocclusion and nonunion were not noticed in any of the 20 cases. Transient inferior alveolar nerve dysfunction was observed in three cases (15%) postoperatively, which recovered gradually in 2 months. Surgical site infection was observed in two cases (10%), which resolved with appropriate course of antibiotics (Table 4).

Table 4.
Details of technique and complications.
Discussion
Mandibular angle fractures can be treated in a closed or open fashion. Closed treatment requires the patient to be in MMF for 4 to 6 weeks or even longer in older patients or patients with comminuted fractures. This prolonged MMF can be problematic in patients with psychiatric disorders or patients at risk of aspiration such as alcoholics or patients with altered mental status. Prolonged MMF can also lead to atrophy of masticatory muscles. ORIF can eliminate or reduce the period of MMF and facilitate an early return of jaw function.
Numerous methods of internal fixation for the fractured mandibular angle have been mentioned with varied results. Immobilization of fracture segments can be achieved via rigid fixation with dynamic compression plates (DCPs), reconstruction plates, lag screws, or via semirigid fixation with monocortical miniplate osteosynthesis [19]. DCP was one of the first methods of fixation used to treat angle fractures. Ideal placement of DCP is along the inferior border to prevent damage to the roots of the teeth in this region. This placement may cause distraction of the superior aspect of the mandible during jaw function, which can be negated with a small tension plate in the superior surface of the fracture site. The DCP system obviously does not work well in fractures that are oblique or comminuted or with continuity defect. In these instances, surgeons may consider reconstruction plates that are thicker and therefore provide greater strength that would resist functional load better. Ellis and Sinn [16] found that the infection rate associated with angle fractures fixated with reconstruction plate was relatively low (7.5%), which has served a benchmark for ORIF of the angle fracture.
Recently, many modifications have been brought about in the design of plates for fixation of fractured mandibular angle, of which 2.0-mm titanium 3D curved angle strut plate has shown promising results [19,20].
The 2.0-mm titanium 3D curved angle strut plate allows for almost no movement at the superior and inferior borders with manual torsional and bending forces, as opposed to when a single linear plate is applied to the superior border area. When only one linear plate is placed at the superior border, torsional and bending forces usually cause movement along the axis of the plate with buccal-lingual splaying and gap formation at the inferior border, respectively. Because the screws are placed in a box configuration of 2.0-mm titanium 3D curved angle strut plate on both sides of the fracture rather than on a single line, broad platforms are created that may increase the resistance to torsional forces along the axis of the plate.
Because the design of the 2.0-mm titanium 3D curved angle strut plate is conceptually that of two linear plates connected by reinforcing vertical struts, these may therefore provide greater resistance against gap opening at the inferior border with biting forces compared with when a single plate is applied at the external oblique ridge or superolateral border. Using sheep mandibles and a class 3 cantilever bending model, Wittenberg et al. [17] found that the gap and displacement values for the 3D strut plate were comparable with those of reconstruction plate.
Literature reveals numerous studies related to the fixation of fractured mandibular angle with their obvious advantages and disadvantages. When dealing with a linear fracture of the mandibular angle, surgeons may choose to place a miniplate along the external oblique ridge to neutralize the tensile force in the superior aspect of the mandible, which has been known as Champy technique. Placements of these plates require less dissection of tissue and theoretically lead to a reduction in infection rate and time of operation. Blood supply to the mandible is preserved and risk of root injury is eliminated. To minimize torsional forces, some authors recommend a second plate at the inferior border of the mandible, which negates the advantage of minimal dissection associated with the Champy technique and prolongs operative time. In addition, the complication rate is found to be much higher with the use of two miniplates in the treatment of the angle fractures (29%) [21]. Recently, 3D, 2.0-mm, eight-holed strut plate system has been used in several centers and has shown very promising data [20]. Guimond et al. [20] showed an infection rate associated with this system to be around 5.4%, which is relatively low.
In our study, we encountered two cases (10%) with surgical wound infection, which resolved with appropriate course of antibiotics and wound care.
Sensory abnormalities resulting from mandibular fractures and facial trauma in general have been understudied. This has been recognized by several authors [22,23,24] and becomes evident specially if compared with the number of studies on sensory deficits associated with elective orthognathic or dentoalveolar procedures. Some of the reasons for the lack of such studies include (1) the lack of pretreatment data collection such as fractured severity and mandibular canal involvement; (2) difficulty with the analysis and reporting of the variable treatment modalities which may by themselves cause nerve injury; (3) the sporadic reporting of the immediate postoperative sensory status; and (4) difficulty with follow-up because of poor patient compliance and, in addition, patients with mandibular fractures are rarely followed up for longer than 6 weeks after clinical union has been established. This issue has been recognized and numerous studies looking specifically at posttraumatic trigeminal sensory deficit have been brought into the literature [22,23,24,25,26].
In a recent review of the literature, the incidence of a postinjury/pretreatment inferior alveolar nerve sensory deficit ranges from 5.7 to 58% and that of a persistent sensory deficit ranges from 0.9 to 66.7% [24]. In other words, fractures with minimal displacement of 2 to 3 mm between the proximal and distal bone segments (using the total mandibular height as reference) are clearly more severe at the level of the nerve because they may cause crush and/or traction injuries of 50% of the nerve diameter. Classification of the degree of displacement using the height of the mandible versus the height of the mandibular canal must therefore be differentiated. The higher incidence of an immediate postinjury and a permanent inferior alveolar nerve deficit seen in the most severely displaced fractures has been previously reported [22,24,25].
It appears from our study that despite the large number and broad placement configuration of the screws, the use of strut plates may only cause a transient sensory deficit caused by fracture manipulation because all those patients (3% cases) who developed a new immediate postoperative sensory deficit regained normal sensation within a short span of time. Thus, 2.0-mm titanium 3D curved angle strut plate for fixation of fractured mandibular angle has relatively less or no postoperative complications compared with other techniques. Also they provide more stability and resist the torsional forces in mandibular angle fractures. Because of this distinctive stability, none of the patients in our series required postoperative MMF. Its low profile and malleability enable easy manipulation and adaptation during fixation, which is expeditious.
Sources of Support
None.
Conflicts of Interest
None declared.
References
- Michelet, F.X.; Deymes, J.; Dessus, B. Osteosynthesis with miniaturized screwed plates in maxillo-facial surgery. J Maxillofac Surg 1973, 1, 79–84. [Google Scholar] [CrossRef]
- Raveh, J.; Vuillemin, T.; Lädrach, K.; Roux, M.; Sutter, F. Plate osteosynthesis of 367 mandibular fractures. The unrestricted indication for the intraoral approach. J Craniomaxillofac Surg 1987, 15, 244–253. [Google Scholar] [CrossRef]
- Fridrich, K.L.; Pena-Velasco, G.; Olson, R.A. Changing trends with mandibular fractures: a review of 1,067 cases. J Oral Maxillofac Surg 1992, 50, 586–589. [Google Scholar] [CrossRef]
- Kroon, F.H.; Mathisson, M.; Cordey, J.R.; Rahn, B.A. The use of miniplates in mandibular fractures. An in vitro study. J Craniomaxillofac Surg 1991, 19, 199–204. [Google Scholar] [CrossRef] [PubMed]
- Ellis, E., III; Karas, N. Treatment of mandibular angle fractures using two mini dynamic compression plates. J Oral Maxillofac Surg 1992, 50, 958–963. [Google Scholar] [CrossRef]
- Farmand, M.; Dupoirieux, L. The value of 3-dimensional plates in maxillofacial surgery [in French]. Rev Stomatol Chir Maxillofac 1992, 93, 353–357. [Google Scholar] [PubMed]
- Ellis, E., III; Walker, L. Treatment of mandibular angle fractures using two noncompression miniplates. J Oral Maxillofac Surg 1994, 52, 1032–1036, discussion 1036–1037. [Google Scholar] [CrossRef]
- Choi, B.H.; Kim, K.N.; Kang, H.S. Clinical and in vitro evaluation of mandibular angle fracture fixation with the two-miniplate system. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1995, 79, 692–695. [Google Scholar] [CrossRef] [PubMed]
- Klotch, D.W.; Gal, R.L. Repair of mandibular fractures using the 2.0. mm system. A review. J Craniomaxillofac Trauma 1995, 1, 38–42. [Google Scholar]
- Ellis, E., III; Walker, L.R. Treatment of mandibular angle fractures using one noncompression miniplate. J Oral Maxillofac Surg 1996, 54, 864–871, discussion 871–872. [Google Scholar] [CrossRef]
- Haug, R.H.; Barber, J.E.; Reifeis, R. A comparison of mandibular angle fracture plating techniques. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1996, 82, 257–263. [Google Scholar] [PubMed]
- Potter, J.; Ellis, E., III. Treatment of mandibular angle fractures with a malleable noncompression miniplate. J Oral Maxillofac Surg 1999, 57, 288–292, discussion 292–293. [Google Scholar]
- Collins, C.P.; Pirinjian-Leonard, G.; Tolas, A.; Alcalde, R. A prospective randomized clinical trial comparing 2.0-mm locking plates to 2.0-mm standard plates in treatment of mandible fractures. J Oral Maxillofac Surg 2004, 62, 1392–1395. [Google Scholar] [PubMed]
- Ellis, E., III; Graham, J. Use of a 2.0-mm locking plate/screw system for mandibular fracture surgery. J Oral Maxillofac Surg 2002, 60, 642–645, discussion 645–646. [Google Scholar] [PubMed]
- Ellis, E., III. Treatment of mandibular angle fractures using the AO reconstruction plate. J Oral Maxillofac Surg 1993, 51, 250–254, discussion 255. [Google Scholar] [CrossRef]
- Ellis, E., III; Sinn, D.P. Treatment of mandibular angle fractures using two 2.4-mm dynamic compression plates. J Oral Maxillofac Surg 1993, 51, 969–973. [Google Scholar]
- Wittenberg, J.M.; Mukherjee, D.P.; Smith, B.R.; Kruse, R.N. Biomechanical evaluation of new fixation devices for mandibular angle fractures. Int J Oral Maxillofac Surg 1997, 26, 68–73. [Google Scholar] [CrossRef]
- Haug, R.H.; Fattahi, T.T.; Goltz, M. A biomechanical evaluation of mandibular angle fracture plating techniques. J Oral Maxillofac Surg 2001, 59, 1199–1210. [Google Scholar]
- Bui, P.; Demian, N.; Beetar, P. Infection rate in mandibular angle fractures treated with a 2.0-mm 8-hole curved strut plate. J Oral Maxillofac Surg 2009, 67, 804–808. [Google Scholar]
- Guimond, C.; Johnson, J.V.; Marchena, J.M. Fixation of mandibular angle fractures with a 2.0-mm 3-dimensional curved angle strut plate. J Oral Maxillofac Surg 2005, 63, 209–214. [Google Scholar]
- Siddiqui, A.; Markose, G.; Moos, K.F.; McMahon, J.; Ayoub, A.F. One miniplate versus two in the management of mandibular angle fractures: a prospective randomised study. Br J Oral Maxillofac Surg 2007, 45, 223–225. [Google Scholar] [CrossRef] [PubMed]
- Marchena, J.M.; Padwa, B.L.; Kaban, L.B. Sensory abnormalities associated with mandibular fractures: incidence and natural history. J Oral Maxillofac Surg 1998, 56, 822–825, discussion 825–826. [Google Scholar] [CrossRef]
- Schultze-Mosgau, S.; Erbe, M.; Rudolph, D.; Ott, R.; Neukam, F.W. Prospective study on post-traumatic and postoperative sensory disturbances of the inferior alveolar nerve and infraorbital nerve in mandibular and midfacial fractures. J Craniomaxillofac Surg 1999, 27, 86–93. [Google Scholar] [CrossRef] [PubMed]
- Thurmuller, P.; Dodson, T.B.; Kaban, L.B. Nerve injuries associated with facial trauma: Natural history, management, and outcome of treatment. OMFS Clin of N Amer 2001, 13, 283–293. [Google Scholar]
- Iizuka, T.; Lindqvist, C. Sensory disturbances associated with rigid internal fixation of mandibular fractures. J Oral Maxillofac Surg 1991, 49, 1264–1268. [Google Scholar] [CrossRef]
- Krakowiak, P.A.; Yamashita, D.D.; Yen, S. Recovery of inferior alveolar nerve function following open reduction internal fixation in traumatically induced mandibular fractures. J Oral Maxillofac Surg 2002, 60, 75–80. [Google Scholar]
© 2014 by the author. The Author(s) 2014.