Abstract
Transcutaneous submandibular approaches are the preferred technique for the application of load-bearing mandibular osteosynthesis plates. However, an extraoral approach is associated with several shortcomings, like the risk of harming the facial nerve and scarring. This technical note presents a specializedmandibular reconstruction plate (MatrixMANDIBLE Preformed Reconstruction Plate [Synthes Maxillofacial, Paoli, PA]), simplifying the transoral application by its design with a preformed curvature along the lateral surface of the mandible. The application of wide-spanning plates reaching from the posterior margin of the ramus even into the contralateral body region is facilitated. Transoral application of preformed mandibular reconstruction plates seems to be a promising option to bypass external incisions and to reduce operating room time.
Load-bearing osteosynthesis plating of the mandible is regularly performed using a transcutaneous submandibular approach. This procedure, however, is associated with several drawbacks, which include the risk of harming the marginal mandibular branch of the facial nerve and large visible scarring. These disadvantages can be circumvented by a transoral approach. Although transoral application of mandibular reconstruction plates is known, clinical use and reports in the literature are sparse due to difficulties in handling and risk of damaging the mental nerve [1]. Therefore, we present a feasible and safe technique for transoral application of MatrixMANDIBLE Preformed Reconstruction Plates (MMPRPs; Synthes Maxillofacial, Paoli, PA). Due to the pre- formed shape, this novel plating system also facilitates transoral application for wide-stretching reconstruction plates. MMPRPs are based on a morphometric shape analysis of the mandible using more than 2000 computed tomography scans from two ethnic populations. It offers load-bearing plates that are preformed to the anatomy of the lateral mandible [2].
1. Technique
MMPRPs are commercially available osteosynthesis plates for the mandible, consisting of two bendable sections at the proximal and distal ends and a nonbendable section in the center. The preformed centerpiece corresponds to the ana- tomic curvature of the mandibular body and angle unit.
The posterior plate end is commonly fixed to the angle/ ramus. Depending on the dimension of the defect/fracture zone, the anterior plate end may be fixed to the symphyseal region, working around the mental nerve unilaterally (unilateral crossway situation; Figure 1A). Alternatively, bilateral handling of the mental nerves will be required if the anterior plate end crosses the symphysis into the contralateral parasymphyseal and body region past the contralateral mental foramen (bilateral crossway situation), for example, in ante- rolateral involvement of the mandible (Figure 1B).
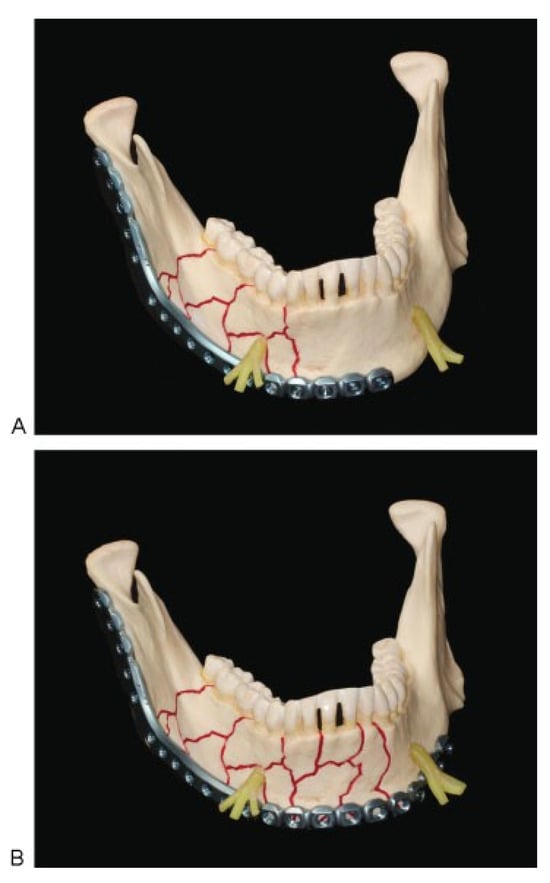
Figure 1.
(A) Hemimandibular MMPRP [Synthes Maxillofacial, Paoli, PA] placement for bridging the ramus and body region. The MMPRP underpasses the mental nerve unilaterally (unilateral crossway situa- tion). Screw fixation of the reconstruction plate at the ipsilateral ramus and parasymphysis/symphysis. (B) MMPRP placement for extended bridging of the ramus, the body, and the symphyseal region. The MMPRP underpasses both mental nerves (bilateral crossway situation). Screw fixation of the reconstruction plate at the ipsilateral ramus and contralateral body, past the mental foramen. Abbreviation: MMPRP, MatrixMANDIBLE Preformed Reconstruction Plate.
A vestibular mucoperiosteal incision is made superior to the mental nerve to access the ipsilateral ramus and angle, body, and parasymphyseal/symphyseal region [3]. To also access the contralateral parasymphyseal and body region in a bilat- eral crossway situation, an extended horseshoe-shaped vestibular mucoperiosteal incision is performed. To stay safely above the mental nerves, the incision in the canine and premolar region is placed directly along the transition be- tween attached gingival and mobile mucosa or along the alveolar crest in edentulous patients. The nerve trunks are exposed in a subperiosteal plane and the circumference of the mental foramina is stripped completely. A caveat to the skeletonization of the mental nerve is not to overstretch or disrupt any fascicles. With appropriate caution the pathways for the MMPRP underneath the overhanging mental nerve loops are widened.
Especially in cases of comminuted fractures, single frag- ments can be fixed after reduction by miniplates to simplify the fracture (Figure 2). Subsequent to the anatomical reduc- tion of fragments (comminuted fractures, nonunions), bone curettage, or partial resection (benign tumors, osteonecrosis), the best fitting MMPRP is selected. There are rigid metal sizers coming in three variants (small, medium, large) that serve as replicas to gauge the nonbendable centerpiece of the MMPRPs either for the left or right hemimandible. The most suitable sizer is introduced through the space below one of the two nerve loops posteriorly and aligned from the angle and ramus continuing over the body and the para- symphysis region to the mandibular midline to check for precise adaptation. It is removed afterward.
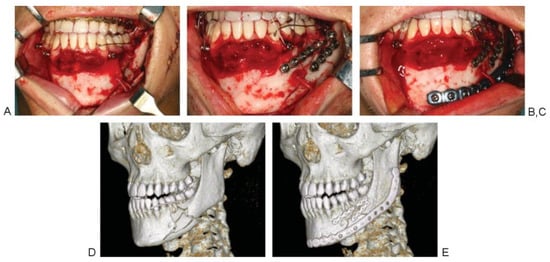
Figure 2.
Patient with a comminuted fracture of the left mandibular body, representing a unilateral crossway situation. (A) Operative findings. (B) MMF screws and wires provide for mandibulomaxillary fixation and the single fragments are fixed after reduction by using miniplates. (C) MMPRP [Synthes Maxillofacial, Paoli, PA] is finally applied after it is threaded underneath the mental nerve loop overhead the lateroinferior border of the mandible. (D) Preoperative CT imaging. (E) Postoperative CT imaging showing good adaption and fit of the plate. Abbreviations: CT, computed tomography; MMF, maxillomandibular fixation; MMPRP, MatrixMANDIBLE Preformed Reconstruction Plate.
The MMPRP implant corresponding to the gauge dimen- sion is chosen to prebend a malleable aluminum template on the side table. This prebent template is used to determine the required overall length, shape, and curvature of the MMPRP implant, in particular the bendable ends in situ.
In a unilateral crossway situation (MMPRP crosses the ipsilateral mental nerve) the length of the template is con- fined to the hemimandible and contralateral parasymphysis. It is threaded under the nerve loop in front of the defect/ fracture zone and formed against the bone surface by finger pressure.
In a bilateral crossway situation the aluminum template reaches over a hemimandible and the parasymphysis into the contralateral body region. First, the template underpasses the nerve loop within the anterolateral defect/fracture zone and is then moved further backward under upward rotation of its posterior end to bring the anterior plate end into a midline position. Second, the plate is slid forward again to thread the anterior plate end underneath the opposite nerve loop on its passage to the body region (Figure 3).
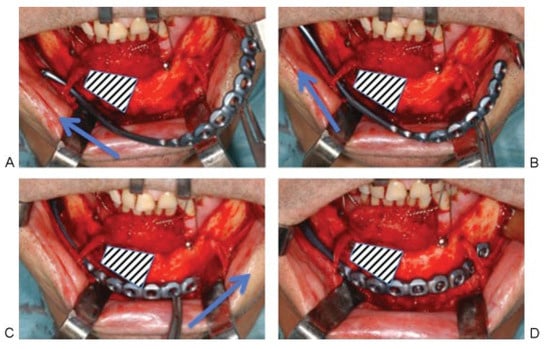
Figure 3.
Bilateral crossway situation with a defect area at the right parasymphyseal region. (A) MMPRP is threaded underneath the ipsilateral (right) mental nerve loop. The arrow indicates the initial backward movement of the posterior plate end. (B) The plate is moved further backward (arrow) under upward rotation of its posterior end. (C) After the anterior plate end nearly reaches a midline position, the plate is slid forward again to thread the anterior plate end underneath the contralateral (left) nerve loop (arrow) on its passage to the body region. (D) MMPRP [Synthes Maxillofacial, Paoli, PA] in its final position, reaching from posterior margin of the ipsilateral ramus into the contralateral body region.
After careful removal of the template in a reverse maneu- ver, the actual MMPRP implant is contoured accordingly on the side table. The final plate is positioned in the same way as the aluminum template, underpassing either one or both mental nerves. The plate is commonly fixed with bicortical angle-stable locking screws (2.4 or 2.9 mm in diameter and of proper length) using a transoral 90-degree angulated drill and screwdriver (Synthes Maxillofacial).
2. Discussion
This technical note describes a feasible technique for transoral application of mandibular reconstruction plates. The novel curve shape design of the MMPRPs improves convenient transoral application of wide-spanning reconstruction plates reaching from the posterior margin of the ramus even into the contralateral body region. The transoral route to the mandible obviates external skin incisions with potential conspicuous scarring. Lesions of the marginal mandibular branch of the facial nerve are to be expected with lower frequency when compared with extraoral approaches, whereas the risk of mental nerve lesions may become more relevant. However, maneuvering the sizers, templates, and implants around the mental nerves is limited due to the equipment’s anatomical preformation and by minimizing the need for intraoperative bending. Furthermore, the smooth continuous centerpiece without narrow neckings diminishes the direct risk of mental nerve injuries when the plates are threaded underneath the mental nerve loops. In cases of osteonecrosis with intraorally exposed bone, the option to circumvent external incisions seems advantageous to avoid wound healing problems end- ing up in a prolonged extra-intraoral fistula.
Though the process of transoral MMPRP application itself—dissecting subperiosteally and underpassing the mental nerves—may be rather time consuming, the time investment for the procedure is estimated to be lower than in an external submandibular approach with open reduction, bending, and internal fixation of a conventional flat reconstruction plate.
In conclusion, MMPRPs allow for transoral application of extended load-bearing osteosynthesis of the mandible. The transoral approach is an interesting option to bridge commi- nuted fractures, fractures in the atrophic edentulous mandi- ble, nonunions, or osteonecrosis. A transoral approach bypasses external incisions and associated risks and operating room time is estimated to be shorter compared with an extraoral approach.
References
- Lopes, N.; Oliveira, D.M.; Vajgel, A.; Pita, I.; Bezerra, T.; Vasconcellos, R.J. A new approach for reconstruction of a severely atrophic mandible. J Oral Maxillofac Surg 2009, 67, 2455–2459. [Google Scholar] [CrossRef] [PubMed]
- Metzger, M.C.; Vogel, M.; Hohlweg-Majert, B.; et al. Anatomical shape analysis of the mandible in Caucasian and Chinese for the produc- tion of preformed mandible reconstruction plates. J Craniomax- illofac Surg 2011, 39, 393–400. [Google Scholar] [CrossRef] [PubMed]
- Cienfuegos, R.; Cornelius, C.P.; Ellis, E.I.I.I.; Kushner, G. CMF Mandible: Surgical Approaches—AO Surgery Reference. AO Foundation. Available online: https://www2.aofoundation.org/wps/portal/surgery?showPage=diagnosis&bone=CMF&segment=Mandible (accessed on 22 May 2013).
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2008 by the author. The Author(s) 2008.